Abstract
Interdural hematomas are primarily observed in infants, and adult interdural hematomas are rare. We describe a 54-year-old woman with a round, well-defined mass. The mass was an interdural hematoma that was misdiagnosed as an epidural hematoma. Unlike an epidural hematoma, interdural hematomas are located between the two layers of the dura mater, and the dural tail sign can be observed.
Keywords: interdural hematoma, epidural hematoma, epidermoid cyst, extra axial tumor
Introduction
The cerebral dura mater consists of two layers. The inner ‘meningeal’ layer and outer ‘periosteal’ layer are connected, and a hematoma between the two layers is termed an ‘interdural hematoma’.1) We present a case of interdural hematoma that was misdiagnosed as a subacute epidural hematoma.
Case Report
A 54-year-old woman was admitted to the emergency room with a scalp laceration wound. The patient reported that the head contusion was caused by dizziness. She was alert and had no neurologic deficits. She did not take any medication and had no medical history. She denied any previous history of trauma. Blood examination including coagulation testing showed no abnormalities. Computed tomography (CT) scan of her brain revealed a mass (diameter: 3.2 cm) in the left pterion (Fig. 1A), and no skull fracture (Fig. 1B). Subsequent magnetic resonance imaging (MRI) revealed a convex, well-defined mass with a homogenous high signal intensity lesion on T1-weighted images (Fig. 1C) and iso signal intensity on T2-weighted images in the left pterion (Fig. 1D). The mass was not enhanced with gadolinium contrast (Fig. 1E) and low signal intensity on Gradient-recalled echo (GRE) image. But the dural tail sign was observed at the superior portion of the mass (Fig. 1F). Although the radiologic images were collected due to head trauma, the stage of hematoma was not associated with the trauma. These unusual appearances prompted a differential diagnosis that included subacute epidural hematoma. An epidermoid cyst seemed unlikely. Because there was no break in the skin at that time, we underestimated the possibility of an epidermoid cyst.
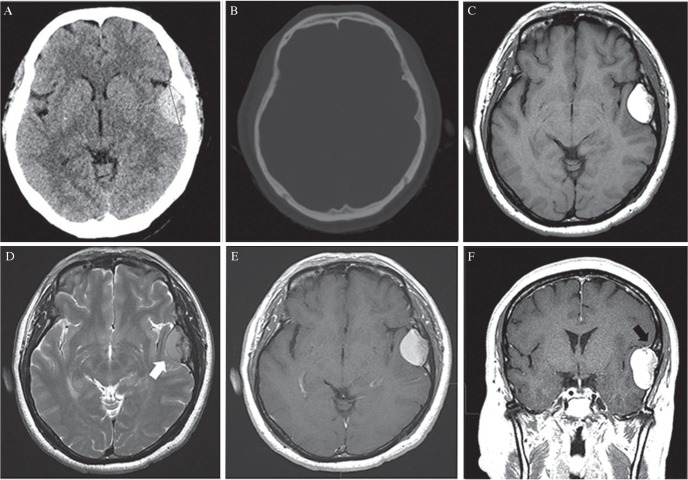
Fig. 1.
(A) CT imaging revealed a mass (diameter: 3.2 cm) in the left temporal convexity. (B) Bone imaging of CT revealed no skull fracture. (C) Axial T1-weighted MR imaging revealed a convex, well-defined mass with homogenous high signal intensity. (D) Axial T2-weighted MR imaging revealed a cerebrospinal fluid (CSF) cleft (white arrow) along the medial boundary. (E) The mass did not show significant enhancement. (F) Coronal, post-gadolinium, T1-weighted MR imaging revealed the dural tail sign (black arrow) at the superior portion of the lesion.
Because the histology was required to confirm a diagnosis, hematoma evacuation was performed via a left frontotemporal craniotomy. After craniotomy, a hematoma was removed with the periosteal layer, because this was adhered to the bone flap (Fig. 2A, B). The hematoma was encapsulated, fibrous and dark with blood (Fig. 2C). No arteries or veins were identified as sources of the hemorrhage within the lesion. After dissection from the skull, the hematoma was curetted en bloc, including around the dura mater. No skull fracture had occurred, but thinning of the abutting skull bone was observed. Based on the pathology of the specimen, the patient was diagnosed with an intracranial hematoma (Fig. 2D–F). There was no evidence of abnormal vessels or tumor cells (Fig. 2G, H). With hematoma evacuation and duroplasty (Neuro-Patch, B. Braun Melsungen AG, Germany), the patient recovered without any neurologic deficits. Seven days later, the patient was discharged without complications. She had no difficulties performing usual activities of daily living.
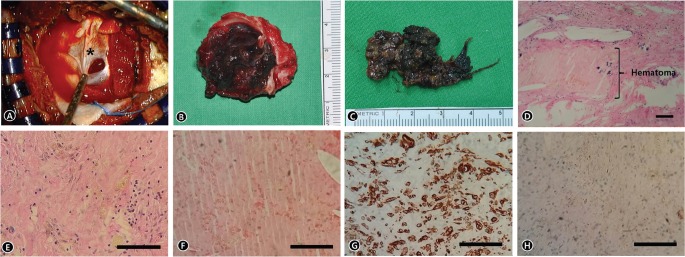
Fig. 2.
(A) Intraoperative photograph showing the meningeal layers (asterisk) of the dura mater after the craniotomy. (B) The hematoma was removed with the periosteal layer of the dura matter because this was adhered to the bone flap. (C) The hematoma was an encapsulated, fibrous, dark-colored, bloody mass. (D) Microphotography of the dura matter revealed a fibrocollagenous tissue (periosteal layer of dura matter and meningeal layer of dura matter) with interdural hematoma (H&E, ×40). (E) Microphotography of the dura matter revealed an eosinophilic lining and scattered inflammatory cells in the lesion (H&E, ×100). (F) Magnified microphotography of the hematoma (H&E, ×100). (G) Immunohistochemical staining for epithelial membrane antigen (EMA) revealed negative in the specimen (×100). (H) Immunohistochemical staining for Vimentin revealed positive in the specimen (×100).
Discussion
In our case, the hematoma was in the subacute stage, and the convex shape was similar to the appearance of an epidural hematoma. However, the epidural hematoma does not have the dural tail sign (as observed with extra-axial tumor, such as meningioma).2) A definitive diagnosis requires the confirmation of pathology because radiological examinations are frequently not helpful during the diagnosis. A dural tail sign that is an unusual finding in an epidural hematoma was present because the hematoma was located between the two dura mater layers.
Interdural hematomas are primarily observed in infants, and adult interdural hematomas are rare.3) Only six cases of interdural hematomas in adults have been reported. Five cases occurred in the supratentorial convexity, and one case occurred in the posterior fossa. One case had coagulopathy previously, two cases were related with the previous operation or trauma, and two cases were related to a ruptured aneurysm. Though the etiology of the interdural hematoma is unknown, because most reported cases were related trauma, the injury of middle meningeal artery by external impact is considered to be the beginning of the hematoma.
Conclusively, a convex shaped hematoma with dural tail sign should be considered as the possibility of interdural hematoma.
Footnotes
Conflict of Interests Disclosure
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
References
- 1). Babayev R, Ekşi MŞ: A blackhole over brain: interdural hematoma – a challenging diagnosis. Neurol Neurochir Pol 49: 189– 192, 2015. [DOI] [PubMed] [Google Scholar]
- 2). Matsui H, Imagama S, Ito Z, Ando K, Hirano K, Tauchi R, Muramoto A, Matsumoto T, Ishiguro N: Chronic spontaneous lumbar epidural hematoma simulating extradural spinal tumor: a case report. Nagoya J Med Sci 76: 195– 201, 2014. [PMC free article] [PubMed] [Google Scholar]
- 3). Miyajima K, Hayashi N, Kurimoto M, Kuwayama N, Hirashima Y, Endo S: Idiopathic interdural hematoma looking like a “Chinese dumpling”, case report. Neuro Med Chir (Tokyo) 44: 75– 76, 2004. [DOI] [PubMed] [Google Scholar]