Summary
Background
Bronchial artery aneurysm (BAA) is a rare condition with a reported prevalence of less than 1% of all selective bronchial arterial angiograms. Despite its low incidence, BAA represents a potential cause of hemoptysis.
Case Report
We describe the case of a 63-year-old man suffering from chronic obstructive pulmonary disease (COPD), who presented with non-massive hemoptysis.
CT angiography revealed a single bronchial artery aneurysm of 9 mm in diameter, abutting the esophageal wall.
Other CT findings included hypertrophy of the bronchial arteries along the mediastinal course, diffuse thickening of the walls of numerous bronchial branches and a “ground glass” opacity in the anterior segment of the right upper pulmonary lobe suggestive of alveolar hemorrhage.
The final diagnosis was established based on selective angiography, which was followed by transcatheter arterial embolization (TAE) of the BAA and of the pathological bronchial circulation.
Follow-up CT scans revealed a total exclusion of the aneurysm from the systemic circulation, resolution of the parenchymal “ground glass” opacity and absence of further episodes of hemoptysis over a period of two years.
Conclusions
An incidental finding of a bronchial artery aneurysm necessitates prompt treatment.
CT angiography and TAE represent the methods of choice for an appropriate diagnosis and treatment, respectively.
In case of a BAA associated with chronic inflammatory diseases, such as COPD, in patients with hemoptysis, TAE of the BAA and of the pathological bronchial circulation, in association with the treatment of the underlying disease, represents a valid approach that can improve the pulmonary status and prevent further episodes of hemoptysis.
MeSH Keywords: Aneurysm; Bronchial Arteries; Embolization, Therapeutic; Hemoptysis; Multidetector Computed Tomography
Background
Bronchial artery aneurysms (BAA) are very rare with a reported prevalence of less than 1% of all selective bronchial arterial angiograms [1] but can represent a potential cause of life-threatening hemoptysis. Thus, it is usually accepted in the literature that treatment of every bronchial artery aneurysm should be initiated as soon as the diagnosis is made [1,2]. We report an uncommon case of a bronchial artery aneurysm in a COPD patient presenting with non-massive hemoptysis and the CT finding of a “ground glass” opacity.
Case Report
A 63-year-old man was admitted to our department because of a sudden onset of non-massive hemoptysis. He was a current smoker (50 packs per year), suffering from chronic obstructive pulmonary disease (COPD), without any occupational exposure factors but with a positive family history of cancer in first-degree relatives. Past medical history included a mild degree of mitral valve insufficiency, sliding hiatal hernia and gastroesophageal reflux. No abnormalities were detected on the physical examination or in laboratory tests.
Furthermore, chest radiography did not show any abnormal findings.
Chest CT angiography was performed and a single bronchial artery aneurysm, 9 mm in diameter, was seen originating from the aortic arch and abutting the posterolateral left wall of the middle-third of the esophagus with hypertrophy of bronchial arteries along their mediastinal course (Figures 1, 2). In addition, there was a diffuse thickening of the walls of many bronchial branches – without evident bronchiectasis, and “ground glass” opacity in the anterior segment of the right upper lobe suggestive of alveolar hemorrhage (Figure 3).
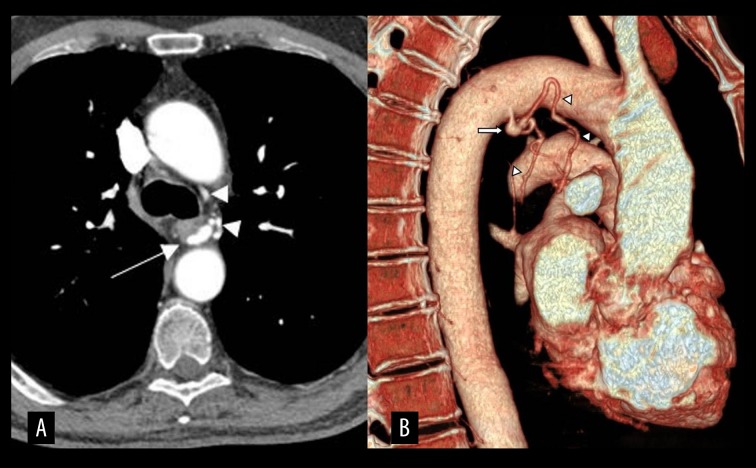
Figure 1.
CT-angiography image showing a bronchial artery aneurysm (white arrow) that arises at the origin of the left bronchial artery and some dilated bronchial arteries (arrowheads), posteriorly and laterally to the trachea (A). Three-dimensional volume-rendering technique (VRT) image depicts the aneurysm (white arrow) and the enlarged bronchial arteries (arrowheads) more clearly (B).
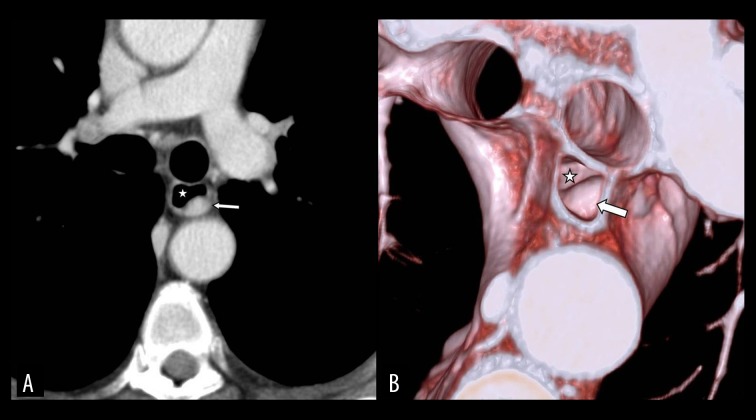
Figure 2.
Axial CT image (A) and VRT image (B) showing aneurysm (arrow) compression on the posterolateral left wall of the middle-third of the esophagus (star).
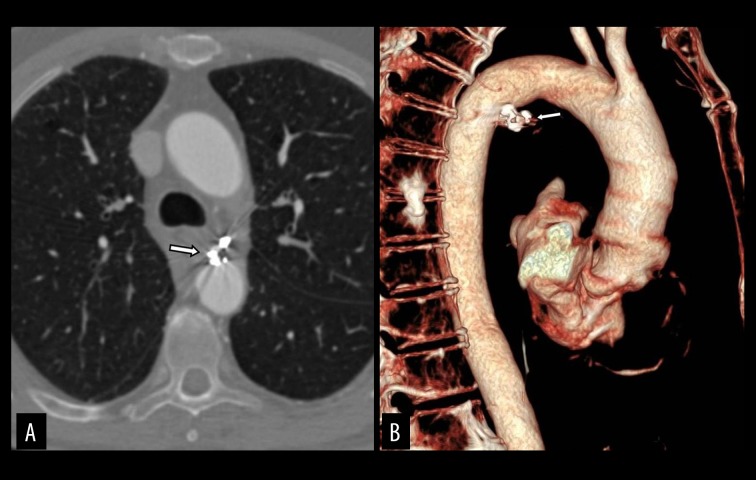
Figure 3.

Axial CT image (lung window) showing a “ground glass” opacity in the anterior segment of the right upper lobe.
Fiberoptic bronchoscopy confirmed the presence of blood clots inside the bronchial tree of the same lobe.
Although there was no rupture of the BAA, transcatheter arterial embolization (TAE) of the detected lesion was performed.
Selective angiography of the bronchial artery system showed the presence of two ectatic branches of the bronchial arteries in addition to the aneurysm. Subsequently, TAE of the aneurysm and of the pathological bronchial circulation was carried out with the use of 5 coils.
After the procedure, no complications occurred. The patient had an uneventful recovery and was discharged after 5 days of hospitalization.
After a week, follow-up CT angiography displayed exclusion of the bronchial artery aneurysm from the systemic circulation (Figure 4) with occlusion of all efferent vessels and resolution of the parenchymal “ground glass” opacity (Figure 5).Over a period of two years, the patient did not have any further episodes of hemoptysis.
Figure 4.
Axial CT image (A) and VRT image (B) obtained after endovascular embolization, demonstrate a complete occlusion of the aneurysm (arrow) and the disappearance of bronchial artery enlargement.
Figure 5.
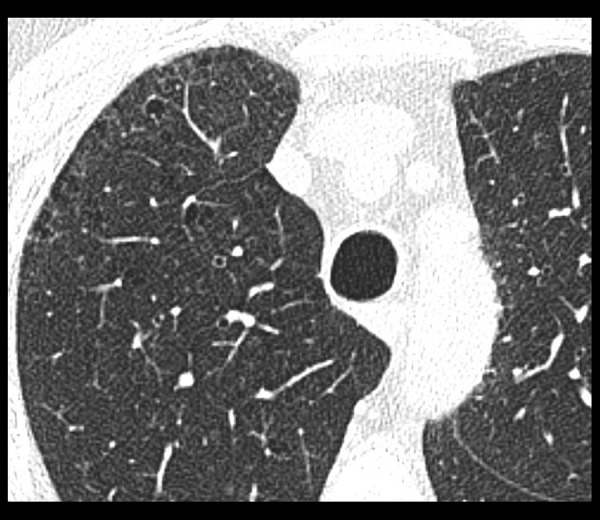
Axial CT image (lung window) shows a resolution of the “ground glass” opacity.
Discussion
In cases of severe hemoptysis requiring treatment, the source of bleeding originates from bronchial arteries in 90% of cases [3].
Under normal conditions, the diameter of the bronchial arteries is smaller than 1.5 mm at the origin and smaller than 0.5 mm more distally.
Although there is no clear correlation between arterial dilatation and the risk of hemorrhage, BAs with a diameter above 2 mm are considered ectatic[4], and when the enlargement is localized, this condition is referred to as a bronchial artery aneurysm (BAA).
Bronchial artery aneurysms (BAA) occur rarely and are detected in fewer than 1% of all patients who undergo selective bronchial arteriography. They can be classified as mediastinal, intrapulmonary or both [1].
Our patient presented with a mediastinal BAA associated with hypertrophy of the bronchial arteries and a “ground glass” opacity.
Bronchial artery aneurysms have been associated with congenital conditions such as double aortic arch [5], pulmonary artery agenesis [6] or defective embryonic development of the bronchial artery wall, or with acquired causes [1] including atherosclerosis, inflammatory lung disease, bronchiectasis, Osler-Weber-Rendu disease, trauma and tuberculosis [7].
The BAA observed in our case was probably secondary to COPD. An increase in systemic arterial blood flow to the lungs, as is typically observed in chronic inflammatory diseases, could be a mechanism of bronchial artery dilation and subsequent aneurysm formation [8].
Chronic inflammatory disorders are also associated with the release of angiogenetic growth factors that lead to neovascularization, vascular remodeling and increased collateral supply from the nearby systemic arteries [9].
Such formed anastomotic vessels usually have weak walls that can easily rupture into the alveoli or the airways causing hemoptysis.
The presence of these findings in a COPD patient corroborates the hypothesis that the chronic inflammatory state can lead to the formation of aneurysms and other disorders of the bronchial circulation, which ultimately results in hemoptysis even before aneurysm rupture.
It is likely that in our case, where the BAA was not identified as the primary site of bleeding, the presence of hypertrophy of the bronchial artery and the alveolar hemorrhage suggest that the bleeding originated from the pathological circulation.
Bronchial artery aneurysms are often asymptomatic, representing an incidental finding during CT angiography.
When symptomatic, they may have different clinical presentations, albeit non-specific, depending on their location. Hemoptysis represents the most common symptom both in intrapulmonary and mediastinal BAAs. Mediastinal BAAs may also present with other symptoms related to the extrinsic compression or rupture into contiguous structures. If the aneurysm ruptures, the clinical presentation may include acute thoracic pain mimicking such conditions as aortic dissection, and it eventually leads to a hypovolemic shock [1].Rarely, a BAA may rupture into the esophagus, causing hematemesis [10].
Patients with hemoptysis should be managed based on the rate and severity of bleeding (massive or non-massive) and the clinical condition of the patient.
Chest radiography is considered as the initial examination, but its sensitivity is low. The combined use of CT angiography and bronchoscopy provides the best accuracy in assessing the etiology and potential source of bleeding [11].
It has been widely reported in the literature that CT can help predict the site of bleeding as accurately as bronchoscopy by detecting the underlying disease with high sensitivity. Moreover, it provides a detailed “road map” of the thoracic vasculature for both the interventional radiologist (arterial embolization) and the thoracic surgeon (open surgery) [9,12].
An incidental finding of a BAA is a condition that should prompt immediate treatment, regardless of the diameter of the aneurysm or the presence of symptoms, as rupture can be life-threatening and the diameter is not an incremental risk factor [1,2].
The treatment of bronchial artery aneurysms consists of open surgery or endovascular procedures [1].
Transcatheter arterial embolization (TAE) is usually the treatment of choice [13], and different embolic materials have been used successfully [14]. During TAE, it is necessary to occlude not only the feeding vessels but also the efferent branches in order to eliminate a backward filling of the aneurysm.
However, it is not possible to occlude the feeding vessels when the segment between the thoracic aorta and the aneurysm is short.
In our patient, TAE of the aneurysm and of the pathological bronchial circulation was performed with 5 coils. After a week, follow-up CT angiography showed a resolution of the parenchymal “ground glass” opacity. This supports the hypothesis that the episode of hemoptysis in our patient originated from the pathological bronchial arterial circulation beyond the aneurysm.
In acquired cases of BAAs, it is also essential to treat any underlying inflammatory, pulmonary or vascular disease to reduce the future risk of revascularization, development of collateral circulation and bronchial artery wall damage, especially in predisposed patients [15].
After management of both the BAA and COPD, the patient did not present further episodes of hemoptysis over a period of two years.
Conclusions
Bronchial arterial aneurysms represent a very rare condition, but may cause potentially fatal complications. They most commonly present with hemoptysis.
In most cases, BAAs are asymptomatic and therefore it is reasonable to assess bronchial circulation in every patient with hemoptysis (even non-massive).
Fiberoptic bronchoscopy and CT angiography should be considered as first-choice studies for an appropriate diagnosis.
Trans-catheter embolization is considered as the gold standard of treatment in hemodynamically stable patients because of its safety, selectivity, efficacy and low invasiveness.
An incidental finding of BAA in an asymptomatic patient should prompt treatment independently of the aneurysm’s diameter or the patient’s condition, since rupture can be life-threatening.
When the BAA is associated with other disorders of the bronchial circulation, especially in patients suffering from chronic inflammatory diseases, such as COPD, and present with hemoptysis, TAE should be performed. TAE enables not only the visualization of the BAA and of the pathological bronchial circulation, but can also improve the patient’s pulmonary status and prevent further episodes of hemoptysis, even when the BAA does not represent the primary site of bleeding.
In such conditions, it is equally important to treat the underlying inflammatory disease in order to reduce bronchial arterial overflow and reduce a future risk of revascularization with the development of collateral circulation.
References
- 1.Tanaka K, Ihaya A, Horiuci T, et al. Giant mediastinal bronchial artery aneurysm mimicking benign esophageal tumor: A case report and review of 26 cases from literature. J Vasc Surg. 2003;38:1125–29. doi: 10.1016/s0741-5214(03)00707-9. [DOI] [PubMed] [Google Scholar]
- 2.Lin J, Wood DE. Bronchial artery aneurysm refractory to transcatheterembolization. Ann Thorac Surg. 2008;86(1):306–8. doi: 10.1016/j.athoracsur.2008.01.033. [DOI] [PubMed] [Google Scholar]
- 3.Yoon W, Kim JK, Kim YH, et al. Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: A comprehensive review. Radiographics. 2002;22:1395–409. doi: 10.1148/rg.226015180. [DOI] [PubMed] [Google Scholar]
- 4.Yildiz AE, Ariyurek OM, Akpinar E, et al. Multidetector CT of bronchial and non-bronchial systemic arteries. Diagn Interv Radiol. 2011;17:10–17. doi: 10.4261/1305-3825.DIR.2694-09.1. [DOI] [PubMed] [Google Scholar]
- 5.Mahmood RD, Chen ZY, Low TB, Ng KS. A rare case of multiple bronchial artery aneurysms associated with a double aortic arch. Singapore Med J. 2015;56(3):e42–45. doi: 10.11622/smedj.2015050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Dominicis F, Leborgne L, Raymond A, Berna P. Right pulmonary artery agenesis and coronary-to-bronchial artery aneurysm. Interact Cardiovasc Thorac Surg. 2011;12(3):507–9. doi: 10.1510/icvts.2010.250795. [DOI] [PubMed] [Google Scholar]
- 7.Karmakar S, Nath A, Neyaz Z, et al. Bronchial artery aneurysm due to pulmonary tuberculosis: Detection with multidetector Computed Tomographic Angiography. J Clin Imaging Sci. 2011;1:26. doi: 10.4103/2156-7514.81293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim HJ, Son HS, Cho SB, Kim KT. Development of a life-threatening mediastinal hematoma from a ruptured bronchial artery aneurysm. J Thorac Cardiovasc Surg. 2013;146(5):e47–49. doi: 10.1016/j.jtcvs.2013.07.034. [DOI] [PubMed] [Google Scholar]
- 9.Bruzzi JF, Rémy-Jardin M, Delhaye D, et al. Multi-detector row CT of hemoptysis. Radiographics. 2006;26:3–22. doi: 10.1148/rg.261045726. [DOI] [PubMed] [Google Scholar]
- 10.Kim JS, Lee SY, Son KH, et al. Bronchial artery aneurysm presenting as hematemesis and mediastinal hemorrhage. Korean J Thorac Cardiovasc Surg. 2015;48:298–301. doi: 10.5090/kjtcs.2015.48.4.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abal AT, Nair PC, Cherian J. Haemoptysis: Aetiology, evaluation and outcome – a prospective study in a third-world country. Respir Med. 2001;95:548–52. doi: 10.1053/rmed.2001.1053. [DOI] [PubMed] [Google Scholar]
- 12.Walker CM, Rosado-de-Christenson ML, Martínez-Jiménez S, et al. Bronchial arteries: Anatomy, function, hypertrophy, and anomalies. Radiographics. 2015;35(1):32–49. doi: 10.1148/rg.351140089. [DOI] [PubMed] [Google Scholar]
- 13.Sanchez E, Alados P, Zurera L, et al. Bronchial artery aneurysm treated with aortic stent graft and fibrin sealant. Ann Thorac Surg. 2007;83:693–95. doi: 10.1016/j.athoracsur.2006.06.082. [DOI] [PubMed] [Google Scholar]
- 14.Izaaryene J, Vidal V, Bartoli JM, Gaubert JY. Multiple bronchial artery aneurysms: Successful treatment with ethylene-vinyl alcohol copolymer (Onyx®) Diagn Interv Imaging. 2016;97(1):125–27. doi: 10.1016/j.diii.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 15.Swanson KL, Johnson CM, Prakash UBS, et al. Bronchial artery embolization. Experience with 54 patients. Chest. 2002;121:789–95. doi: 10.1378/chest.121.3.789. [DOI] [PubMed] [Google Scholar]