Abstract
Background/Purpose
The implications of childhood obesity on pediatric trauma outcomes are not clearly established. Anthropomorphic data were recently added to the National Trauma Data Bank (NTDB) Research Datasets, enabling a large, multicenter evaluation of the effect of obesity on pediatric trauma patients.
Methods
Children ages 2 to 19 years who required hospitalization for traumatic injury were identified in the 2013–2014 NTDB Research Datasets. Age and gender-specific body mass indices (BMI) were calculated. Outcomes included injury patterns, operative procedures, complications, and hospital utilization parameters.
Results
Data from 149,817 pediatric patients were analyzed; higher BMI percentiles were associated with significantly more extremity injuries, and fewer injuries to the head, abdomen, thorax and spine (p values <0.001). On multivariable analysis, higher BMI percentiles were associated with significantly increased likelihood of death, deep venous thrombosis, pulmonary embolus and pneumonia; although there was no difference in risk of overall complications.
Obese children also had significantly longer lengths of stay and more frequent ventilator requirement.
Conclusions
Among children admitted after trauma, increased BMI percentile is associated with increased risk of death and potentially preventable complications. These findings suggest that obese children may require different management than non-obese counterparts to prevent complications.
Keywords: trauma, pediatric, obesity, body mass index, outcomes, complications
1. BACKGROUND
In children, unintentional injury and obesity are leading causes of morbidity. Multiple studies show that obese children have similar injury severity and mortality to non-overweight children(1–4), but they sustain distinct anatomic patterns of injury. Obese children had a greater frequency of extremity injuries than normal-weight children among Level I trauma admissions(1), Emergency Department (ED) evaluations(5), and after motor vehicle crashes(2, 4, 6); some studies show that obese children presenting to an ED or level I trauma center were less likely to have head injuries(1, 3, 5). Still, literature regarding complications following trauma in obese children consists primarily of single-institution studies, limiting generalizability of findings. Prior studies have demonstrated conflicting results regarding effect of obesity on complications and hospital resource utilization such as ICU needs(1, 7)
Given that complications are uncommon in children, larger sample sizes are needed to adequately evaluate the association of BMI with trauma outcomes. Furthermore, single-center studies may not be representative of trauma patients nationwide. Finally, existing studies largely dichotomize obesity, which may not adequately capture the risk of patients with the highest body mass indices (BMIs). Beginning in 2013, the National Trauma Data Bank (NTDB) added height and weight parameters to the research datasets, enabling a nationwide assessment of the impact of pediatric obesity on pediatric trauma. Specific aims of this study were to evaluate injury patterns and outcomes across a broader spectrum of BMIs, determine if injury patterns seen in previous studies are also observed in this nationwide dataset, characterize the impact of obesity on healthcare utilization such as LOS and procedures, and assess the impact of obesity on complications. We hypothesized that obese children would have different injury patterns, greater morbidity and greater hospital resource utilization, compared to normal-weight children.
2. METHODS
This was a retrospective study of pediatric trauma patients, and met the University of Washington Institutional Review Board’s criteria to be exempt from review.
The NTDB, maintained by the American College of Surgeons Committee on Trauma(8) is the largest compilation of trauma registry data in the world and contains data on more than 6,000,000 cases from over 900 registered trauma centers. Data are collected by trained registrars with common inclusion criteria and field definitions across centers. We queried the 2013–2014 Research Datasets for all patients ages 2 to 19 who sustained traumatic injuries. We excluded patients who had isolated burns, died prior to arrival, or were discharged home from the ED.
The CDC’s gender-specific growth tables and their associated SAS program(9) were used to determine BMI percentile for age. For categorical analysis, the CDC’s established pediatric BMI categories were used: obese (≥95th percentile), overweight (85th to <95th percentile), and normal-weight (5th to <85th percentile). Patients >99th percentile for BMI were categorized as morbidly obese. Given our intent to evaluate obesity, we excluded patients <5th percentile.
The initial pediatric cohort included 211,604 patients. Gender was missing for 103 patients; these were excluded given that gender is needed for selection of growth table parameters. Eighteen percent of patients in the initial cohort were missing weight values; since most patients missing weight values were also missing height values, these 37,157 patients were excluded from the analysis.
Multiple imputation using multivariate normal regression with 20 iterations was performed for remaining patients. Imputed parameters included height, LOS, ICU LOS, ventilator days, and ISS (missing <5% for variables other than height, which was missing in 30% of the included patients). The mean BMI percentile in the imputed and complete case analysis (non-imputed) datasets was similar (non-imputed mean 63.4, SD 31.5; imputed mean 63.6, SD 32.9); however, multivariable analyses were conducted using both versions of the dataset. The CDC algorithm flags biologically implausible BMI percentiles; these patients (7%) were also excluded. The final study population included 149, 817 patients after applying the above exclusion criteria.
For analysis of Injury Severity Scores, hospital-submitted values were used when available (96%), and otherwise substituted with AIS or ICD9-derived codes. Frequency of operative procedures was assessed among patients with AIS ≥3 injury to the associated body region in each BMI category. Given that older adolescents may be at greater risk for certain in-hospital complications, a subanalysis was performed to assess adjusted risk of complications among children under 13 years of age.
Univariate analyses assessed differences in outcomes across BMI strata using Chi Square and ANOVA tests. Poisson and linear regression with robust variance were used for multivariable analyses. The category of any complication included death as well as non-fatal complications. Potential confounding variables were included if they resulted in a ≥10% change in the coefficient for BMI or were clinically important. Multivariable regression models for operative procedures also included presence of severe injuries (AIS≥3) in the associated anatomic region. Analysis was performed using Stata version 14.1 (StataCorp LP, College Station, TX). The CDC algorithm was applied using SAS (SAS Institute, Cary, NC).
3. RESULTS
3.1 Descriptive and univariate analyses
Data from 149, 817 pediatric patients were analyzed (Table 1). Mean age was 12.1 years (SD5.2) and 66% of included patients were male. Overall mortality was 1.9%, and 86.0% of patients were discharged home after hospitalization. Relevant patient comorbidities were tabulated across BMI categories (Table 2). Documented obesity was underreported: only 11.2% of the morbidly obese patients had a diagnosis of obesity recorded.
Table 1.
Characteristics of the population by body mass index category
| Normal weight (n=87,780) | Overweight (n=27,119) | Obese (n=23,784) | Morbidly obese (n=11,134) | |
|---|---|---|---|---|
| Mean age, years (SD) | 12.2 (5.4) | 12.4 (4.9) | 11.9 (4.7) | 10.3 (5.2) |
| Mean BMI percentile (SD) | 51.3 (23.7) | 90.6 (2.9) | 97.3 (1.2) | 99.5 (0.3) |
| Female gender | 33.2% | 34.2% | 34.8% | 33.1% |
| Race | ||||
| White | 64.2% | 62.0% | 61.6% | 58.1% |
| Black | 16.6% | 17.2% | 17.4% | 18.6% |
| Asian | 1.9% | 1.6% | 1.3% | 1.4% |
| Other/unknown | 17.4% | 19.1% | 19.8% | 21.9% |
| Hispanic ethnicity | 14.8% | 16.5% | 17.5% | 18.8% |
| Mechanism | ||||
| MVC or other transport | 37.8% | 38.8% | 39.5% | 37.0% |
| Fall | 32.3% | 30.8% | 31.6% | 36.1% |
| Firearm, suicide or assault | 10.0% | 9.6% | 8.3% | 6.8% |
| Struck by or against object | 11.0% | 11.6% | 10.9% | 9.6% |
| ISS; median (IQR) | 5 (4–10) | 5 (4–10) | 5 (4–9) | 5 (4–9) |
| Maximum AIS; median (IQR) | 2 (2–3) | 2 (2–3) | 2 (2–3) | 2 (2–3) |
| Hospital disposition | ||||
| Home | 86.8% | 85.4% | 84.8% | 84.6% |
| Intermediate care facility | 0.8% | 0.8% | 0.9% | 0.8% |
| Inpatient rehabilitation | 3.0% | 3.5% | 3.3% | 2.9% |
| Deceased or hospice | 1.2% | 1.3% | 1.2% | 1.1% |
| Medicaid or other government insurance | 33.5% | 35.4% | 37.0% | 42.0% |
Abbreviations: SD = standard deviation, BMI = body mass index, MVC = motor vehicle collision, IQR = interquartile range, ISS = Injury Severity Score, AIS = Abbreviated Injury Score
Table 2.
Documented comorbidities by body mass index category
| Normal weight (n=87,780) | Overweight (n=27,119) | Obese (n=23,784) | Morbidly obese (n=11,134) | P value | |
|---|---|---|---|---|---|
| Bleeding disorder | 0.3% | 0.3% | 0.2% | 0.2% | 0.35 |
| Congenital anomaly | 0.8% | 0.7% | 0.6% | 0.8% | 0.04 |
| Diabetes | 0.4% | 0.5% | 0.5% | 0.6% | <0.001 |
| Obesity (documented) | 0.1% | 0.4% | 6.0% | 11.2% | <0.001 |
| Prematurity | 0.4% | 0.3% | 0.3% | 0.3% | 0.01 |
| Respiratory disease | 5.0% | 5.4% | 5.9% | 6.3% | <0.001 |
| Steroid use | 0.1% | 0.1% | 0.0% | 0.1% | 0.20 |
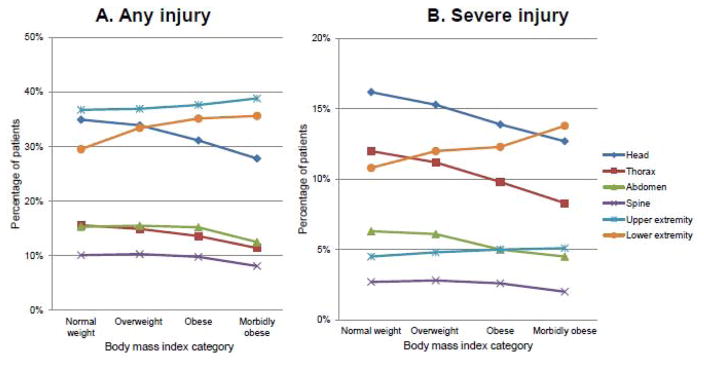
The frequencies of any injuries and severe (AIS≥3) injuries by body region were assessed, as shown in Figure 1 (quantitative results available in Supplementary Table 1). Increased BMI category was associated with significantly greater frequency of upper and lower extremity injuries, and lower frequency of head, thorax, abdomen, spine and external injuries. Among severe regional injuries, these trends in head, thorax and lower extremity injuries were particularly pronounced.
Figure 1.
Associations between body mass index category and Abbreviated Injury Scale by major body region. Panel A shows the trends for injury of any severity to each body region; Panel B shows the trends for severe injury to each body region (Abbreviated Injury Scale of 3 or greater).
Univariate analyses of hospital utilization and complications across BMI categories are presented in Table 3. Mean hospital LOS was significantly higher among overweight and obese patients; however, patients in higher BMI categories were also more frequently admitted for only one day.
Table 3.
Unadjusted association of body mass index categories with in-hospital trauma outcomes
| Normal weight (n=87,780) | Overweigh t (n=27,119) | Obese (n=23,784) | Morbidly obese (n=11,134) | P value | |
|---|---|---|---|---|---|
| Any in-hospital complication | 17.4% | 17.4% | 16.9% | 15.9% | <0.001 |
| Death | 1.9% | 2.1% | 2.0% | 1.8% | 0.22 |
| Any specified complication excludes “unspecified” complications |
4.2% | 4.7% | 4.5% | 4.4% | 0.01 |
| Acute kidney injury | 0.1% | 0.1% | 0.1% | 0.1% | 0.08 |
| Superficial surgical site infection | 0.1% | 0.1% | 0.1% | 0.1% | 0.93 |
| Deep surgical site infection | 0.1% | 0.1% | 0.1% | 0.1% | 0.15 |
| Organ space surgical site infection | 0.1% | 0.1% | 0.1% | 0.1% | 0.001 |
| Sepsis | 0.1% | 0.1% | 0.1% | 0.0% | 0.30 |
| Deep venous thrombosis or thrombophlebitis | 0.2% | 0.3% | 0.3% | 0.2% | 0.01 |
| Pulmonary embolism | 0.0% | 0.1% | 0.1% | 0.1% | <0.001 |
| Pneumonia | 0.7% | 0.8% | 0.7% | 0.7% | 0.86 |
| Acute respiratory distress syndrome | 0.3% | 0.3% | 0.3% | 0.3% | 0.74 |
| Urinary tract infection | 0.4% | 0.4% | 0.4% | 0.4% | 0.98 |
| Other unspecified complication | 14.2% | 13.9% | 13.6% | 12.9% | <0.001 |
| LOS (days); mean (SD) | 3.3 (5.1) | 3.5 (6.0) | 3.4 (5.9) | 3.3 (6.5) | <0.001 |
| Percent admitted only 1 day | 38.5% | 38.6% | 39.7% | 41.6% | <0.001 |
| Percent requiring ICU | 22.6% | 22.5% | 20.5% | 18.1% | <0.001 |
| Percent requiring ventilator | 7.8% | 8.2% | 7.5% | 6.3% | <0.001 |
| ICU LOS, mean (SD) | 4.0 (5.7) | 4.3 (6.2) | 4.5 (6.9) | 4.7 (8.9) | <0.001 |
Abbreviations: LOS = length of stay, IQR = interquartile range, SD = standard deviation, ICU = intensive care unit.
Higher BMI categories were associated with lower frequency of ICU admission, but among patients requiring intensive care, ICU LOS was longer in patients in higher BMI strata. Increased BMI category was associated with lower frequency of ventilator requirement. The overall frequency of complications (including death) was 17.2%; univariate analysis showed a slightly, but significantly, lower rate of complications in higher BMI strata.
The unadjusted frequencies of operative procedures among patients with severe injury to the associated body region is shown in Table 4; statistically significant differences were noted only for tube thoracostomy and fixation of femur fractures.
Table 4.
Operative interventions for patients with severe injury to body region by body mass index category
| Normal weight | Overweight | Obese | Morbidly obese | P value | |
|---|---|---|---|---|---|
|
Exploratory laparotomy
(if severe abdominal injury) |
18.8% | 20.6% | 18.6% | 18.3% | 0.39 |
|
Tube thoracostomy (if severe chest injury) |
20.3% | 19.3% | 17.8% | 17.5% | 0.01 |
|
Thoracotomy (if severe chest injury) |
1.5% | 1.4% | 1.0% | 1.3% | 0.28 |
|
Craniotomy/craniectomy (if severe head injury) |
7.2% | 8.0% | 7.7% | 7.2% | 0.36 |
|
Spine fixation (if severe spine injury) |
26.5% | 26.3% | 23.6% | 27.2% | 0.50 |
|
Tibia, fibula, patella fixation (if severe lower extremity injury) |
16.7% | 17.4% | 16.5% | 15.8% | 0.52 |
|
Femur fixation (if severe lower extremity injury) |
45.0% | 46.9% | 47. 8% | 46.5% | 0.03 |
|
Humerus, radius, ulna fixation (if severe upper extremity injury) |
60.2% | 58.0% | 58.0% | 61.2% | 0.28 |
Within each category, the denominator is patients of a given BMI category who sustained a severe (AIS ≥ 3) injury to the body region of the operation. For example, for exploratory laparotomy, the denominator for each BMI category is patients with AIS ≥ 3 abdominal injuries.
3.2 Multivariable analyses
Multivariable analysis was performed, as shown in Table 5. The final model included BMI percentile as a continuous variable, maximum AIS in any body region, presence of ED hypotension (<70+2*age), ED Glasgow Coma Score motor response, age, Hispanic ethnicity, presence of any comorbidity, and insurance type. Patients in the 99th percentile for BMI had a 50% increase in acute kidney injury (AKI), 89% increase in deep venous thrombosis (DVT), and 2.66 times the risk of pulmonary embolism (PE), compared to patients in the 50th percentile for BMI. The association between BMI and both DVT and PE persisted when the presence of any or severe lower extremity injury was added to the model. The same multivariable analyses were also conducted using the complete case analysis (non-imputed) dataset. The estimates were similar overall; however confidence intervals for superficial surgical site infection, organ space surgical site infection and acute respiratory distress syndrome became statistically significant. A table analogous to Table 5, but with estimates from the complete case analysis dataset, is available as Supplementary Table 2.
Table 5.
Adjusted relative risk of in-hospital complications as a function of body mass index
| Adjusted relative risks: 85th percentile for BMI relative to 50th percentile | Adjusted relative risks: 95th percentile for BMI relative to 50th percentile | Adjusted relative risks: 99th percentile for BMI relative to 50th percentile | |
|---|---|---|---|
| Any in-hospital complication | 0.99 (0.97–1.00) | 0.98 (0.96–1.00) | 0.98 (0.96–1.00) |
| Death | 1.09 (1.03–1.14) | 1.11 (1.05–1.18) | 1.12 (1.05–1.20) |
| Any specified complication | 1.10 (1.07–1.14) | 1.13 (1.08–1.18) | 1.14 (1.09–1.20) |
| Acute kidney injury | 1.34 (1.00–1.79) | 1.45 (1.00–2.11) | 1.50 (1.00–2.25) |
| Superficial surgical site infection | 1.23 (0.95–1.58) | 1.30 (0.94–1.80) | 1.33 (0.94–1.90) |
| Organ space surgical site infection | 1.27 (0.96–1.69) | 1.36 (0.94–1.96) | 1.40 (0.94–2.08) |
| Sepsis | 1.31 (0.97–1.76) | 1.42 (0.97–2.09) | 1.46 (0.96–2.23) |
| Deep venous thrombosis, thrombophlebitis | 1.57 (1.31–1.88) | 1.79 (1.42–2.26) | 1.89 (1.46–2.43) |
| Pulmonary embolus | 2.01 (1.30–3.10) | 2.45 (1.40–4.29) | 2.66 (1.45–4.88) |
| Pneumonia | 1.11 (1.01–1.21) | 1.14 (1.02–1.28) | 1.15 (1.02–1.30) |
| Acute respiratory distress syndrome | 1.12 (0.97–1.29) | 1.15 (0.96–1.39) | 1.17 (0.95–1.44) |
| Any ICU admission | 0.98 (0.97–0.99) | 0.97 (0.96–0.99) | 0.97 (0.95–0.99) |
| Ventilator requirement | 1.05 (1.02–1.07) | 1.06 (1.03–1.09) | 1.07 (1.03–1.10) |
Abbreviations: BMI = body mass index, OR = operating room, ICU = intensive care unit. Adjusted relative risks are shown for outcomes based on the multivariable model, for patients in the 85th, 95th and 99th percentile for BMI, with the reference category being patients in the 50th percentile for BMI. Variables for any in-hospital complication and any specified complication included death. Estimates are based on imputed dataset as described in the methods.
Subanalysis was performed to assess risks of complications in children younger than 13 years. Overall results were similar to those presented in Table 5; however, the association between BMI percentile and acute kidney injury and ventilator need were not statistically significant. Notably, the association between DVT risk and BMI percentile remained positive; wherein children <13 years in the 99th percentile for BMI had an adjusted relative risk of DVT of 2.77 (95% CI 1.33, 5.75), relative to children <13 years in the 50th percentile. Pulmonary embolism was rare so the confidence interval was wide, however, the estimated risk for children <13 years in the 99th percentile for BMI was 9.8 (95% CI 0.5, 187.7), compared to children <13 years in the 50th percentile.
On adjusted analyses of hospital utilization parameters, there was a small positive association between BMI percentile and hospital LOS (0.04 days longer per 10-point increase in BMI percentile; 95% CI=0.03–0.05 days). There were minor differences across BMI categories regarding need for ICU admission; however, among patients who did require intensive care, patients with higher BMIs had longer ICU LOS (0.1 day per 10 point increase in BMI percentile; 95% CI 0.06–0.11 days). Higher BMI percentile was associated with a slightly greater likelihood of ventilator requirement as shown in Table 6, and there was a positive association between BMI percentile and ventilator days among patients requiring ventilator support (0.1 day longer per 10-point increase in BMI percentile; 95% CI=0.06–0.15). These estimates were similar in the complete case analysis dataset.
Frequency of operative intervention was also assessed using multivariable analysis. In addition to the variables described above, these models also included presence of severe injury in the body region associated with the operation. The only operations for which a statistically significant difference in adjusted relative risk was observed was for tibia/fibula/patella fixation and femur fixation. For tibia/fibula/patella fixation, a 10-point increase in BMI percentile was associated with an 8% increase in risk of operation (adjusted relative risk 1.08, 95% CI=1.07–1.09); results from complete case analysis dataset were similar. For femur fixation, a 10-point increase in BMI percentile was associated with a 1% increase in risk of operation (adjusted relative risk 1.01, 95% CI=1.00–1.01); results from complete case analysis dataset were not statistically significant.
4. DISCUSSION
This study demonstrated that among pediatric patients admitted to US trauma centers, anatomic distribution of injuries varies with BMI. Additionally, the overall risk of complications was similar across BMI categories; however, obese children had higher adjusted risks of certain complications, including thromboembolic complications and death.
While both DVT and PE are rare in children, obese children in our cohort were at significantly elevated risk compared to normal-weight children. These findings persisted upon subanalysis of children younger than 13 years, although the finding for PE in this population was not statistically significant given a wide confidence interval. Although extremity injuries and need for orthopedic operations are known risk factors for pediatric venous thromboembolism(10–12), the association we observed persisted after controlling for presence of any and severe lower extremity injuries. This finding may relate to insulin resistance(13), greater difficulty detecting early signs of infection, or from decreased mobility in obese children. Our result suggests that providers should have high clinical suspicion and be vigilant in caring for these patients. Thrombotic complications may be reduced by greater focus on mobilization, early engagement of physical therapy, consideration of chemical venous thromboembolic prophylaxis in some patients, and more frequent use of lower extremity duplex ultrasound in the setting of potential DVT symptoms.
Obese patients in our cohort had a small but significant increase in risk of in-hospital mortality after adjustment for injury severity and sociodemographic factors. Since this trend was not present in univariate analysis, we hypothesize that it may relate differences in injury severity across exposure groups, and to observed complication risks. Despite this increase in in-hospital mortality, the adjusted risk of complications overall was not significantly increased in patients with higher BMI percentiles. Children in higher BMI categories had lower frequencies of complications on univariate analysis but no difference after adjustment for injury severity and sociodemographics.
Our results also show that higher BMI percentile is associated with higher adjusted risk of pneumonia. The complete case analysis dataset, but not the imputed dataset, also showed increased risk of infectious complications such as superficial surgical site infection, organ space surgical site infection and acute respiratory distress syndrome; these differences may relate to differences in sample sizes and confidence intervals, or to selection bias in these methods. While our study is not conclusive regarding the risk of infectious complications, existing literature has also been conflicting(1, 7). Thus, we encourage providers to continue to ensure adequate dosing of prophylactic antibiotics for body weight, and appropriate glycemic control when indicated.
Relating to hospital resource utilization, our study demonstrated that obese children were more likely than normal-weight children to require operative repair of lower extremity injuries after controlling for regional injury severity. Additionally, higher BMI percentile was associated with greater likelihood of ventilator requirement and slightly longer hospital and ICU lengths of stay.
There were some limitations to our study. Anthropomorphic values were missing in a sizable proportion; we addressed this problem by excluding patients with missing weight, and imputing heights only in patients with weight data available. We recognize that this process may introduce some selection bias; however, using a combination of exclusion and imputation provides the most robust analysis, instead of either excluding all cases with missing data or imputing a large portion of key exposure variables. We also presented multivariable estimates based on both imputed and complete case analysis datasets. Further, we recognize that the centers participating in NTDB might underreport complications(14), which could affect our results if there was differential reporting across BMI percentiles. Additionally, we lack anesthesia and clinical data to comment on how care of the obese child may differ, such as in affecting admission, thromboprophylaxis or other clinical decisions.
In conclusion, this large, nationwide study of pediatric trauma patients demonstrated that obesity is associated with mortality and increased risk of certain potentially-preventable complications. While it is encouraging that the overall risk of complications is similar across BMI categories, these results identify specific areas, such as thromboembolic disease, that may be useful in quality assurance and benchmarking. Ultimately, our results support the need for thoughtful management of obese children, with attention to appropriate prophylactic measures.
Acknowledgments
Thank you to Alex Quistberg and Hao He for data management and statistical assistance. Funding support for this study was from the National Institute of Health, Institute of Child Health and Human Development [2T32HD057822-06; Drs. Frederick Rivara and Monica Vavilala].
Footnotes
Level of evidence: Level III; prognosis study
AUTHOR CONTRIBUTION
Dr. Witt participated in literature search, study design, data collection, data analysis, data interpretation, writing and critical revision. Dr. Arbabi, Dr. Nathens, Dr. Vavilala and Dr. Rivara participated in study design, data interpretation and critical revision.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rana AR, Michalsky MP, Teich S, Groner JI, Caniano DA, Schuster DP. Childhood obesity: a risk factor for injuries observed at a level-1 trauma center. J Pediatr Surg. 2009 Aug;44(8):1601–5. doi: 10.1016/j.jpedsurg.2008.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zonfrillo MRNK, Durbin DR, Kallan MJ. The association of weight percentile and motor vehicle crash injury among 3 to 8 year old children. Ann Adv Automot Med. 2010;54:193–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Alselaim N, Malaekah H, Saade M, Hussein M, Altokhais T, Albedah K, et al. Does obesity impact the pattern and outcome of trauma in children? J Pediatr Surg. 2012 Jul;47(7):1404–9. doi: 10.1016/j.jpedsurg.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 4.Pollack KM, Xie D, Arbogast KB, Durbin DR. Body mass index and injury risk among US children 9–15 years old in motor vehicle crashes. Inj Prev. 2008 Dec;14(6):366–71. doi: 10.1136/ip.2008.019208. [DOI] [PubMed] [Google Scholar]
- 5.Pomerantz WJ, Timm NL, Gittelman MA. Injury patterns in obese versus nonobese children presenting to a pediatric emergency department. Pediatrics. 2010 Apr;125(4):681–5. doi: 10.1542/peds.2009-2367. [DOI] [PubMed] [Google Scholar]
- 6.Haricharan RN, Griffin RL, Barnhart DC, Harmon CM, McGwin G. Injury patterns among obese children involved in motor vehicle collisions. J Pediatr Surg. 2009 Jun;44(6):1218–22. doi: 10.1016/j.jpedsurg.2009.02.029. discussion 22. [DOI] [PubMed] [Google Scholar]
- 7.Brown CV, Neville AL, Salim A, Rhee P, Cologne K, Demetriades D. The impact of obesity on severely injured children and adolescents. J Pediatr Surg. 2006 Jan;41(1):88–91. doi: 10.1016/j.jpedsurg.2005.10.012. discussion 88–91. [DOI] [PubMed] [Google Scholar]
- 8.Committee on Trauma ACoS. National Trauma Data Bank. Chicago, IL: 2013–2014. [Google Scholar]
- 9.A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 years) Center for Disease Control: Center for Disease Control; 2015. [updated Apr; cited 2015 Aug]. Available from: http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. [Google Scholar]
- 10.Connelly CR, Laird A, Barton JS, Fischer PE, Krishnaswami S, Schreiber MA, et al. A Clinical Tool for the Prediction of Venous Thromboembolism in Pediatric Trauma Patients. JAMA Surg. 2016 Jan 1;151(1):50–7. doi: 10.1001/jamasurg.2015.2670. Epub 2015/10/01. eng. [DOI] [PubMed] [Google Scholar]
- 11.Allen CJ, Murray CR, Meizoso JP, Ray JJ, Neville HL, Schulman CI, et al. Risk factors for venous thromboembolism after pediatric trauma. J Pediatr Surg. 2016 Jan;51(1):168–71. doi: 10.1016/j.jpedsurg.2015.10.033. Epub 2015/11/09. eng. [DOI] [PubMed] [Google Scholar]
- 12.Hanson SJ, Punzalan RC, Greenup RA, Liu H, Sato TT, Havens PL. Incidence and risk factors for venous thromboembolism in critically ill children after trauma. J Trauma. 2010 Jan;68(1):52–6. doi: 10.1097/TA.0b013e3181a74652. Epub 2010/01/13. eng. [DOI] [PubMed] [Google Scholar]
- 13.Ljungqvist O. Insulin resistance and outcomes in surgery. J Clin Endocrinol Metab. 2010 Sep;95(9):4217–9. doi: 10.1210/jc.2010-1525. Epub 2010/09/09. eng. [DOI] [PubMed] [Google Scholar]
- 14.Hemmila MR, Jakubus JL, Wahl WL, Arbabi S, Henderson WG, Khuri SF, et al. Detecting the blind spot: complications in the trauma registry and trauma quality improvement. Surgery. 2007 Oct;142(4):439–48. doi: 10.1016/j.surg.2007.07.002. discussion 48–9 Epub 2007/10/24.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]