Abstract
In May 2013, an internationally renowned celebrity—Angelina Jolie—disclosed her receipt of BRCA1/BRCA2 (BRCA) testing and subsequent double mastectomy in a highly publicized editorial. Publicity surrounding celebrity health services use increases awareness of important health issues and demand for health services. We aimed to describe BRCA testing trends before and after Jolie’s disclosure, breast cancer-related services use following testing, and test reimbursement trends. MarketScan Commercial Claims data were used to compare trends in BRCA testing before and after Jolie’s health disclosure using an interrupted time series model among women aged 18–64. We used modified Poisson regression to estimate risks for health services use (surgical consult, mastectomy, mammography, magnetic resonance imaging, genetic counseling) following BRCA testing. BRCA testing rates increased from 12.5 to 19.0 tests/100,000 women between January 2013 and October 2014. Immediately following Jolie’s disclosure, testing increased by approximately 37% (p < 0.001). Although BRCA testing increased, use of post-testing follow-up services declined after Jolie’s disclosure. Mean insurance reimbursement and patient out-of-pocket spending on the test decreased by 3 and 36%, respectively. While genetic testing uptake increased following Jolie’s disclosure, subsequent health services use associated with BRCA mutations declined, suggesting that celebrity disclosures may be associated with potential genetic testing overuse.
Keywords: Genetic testing, Breast cancer, Costs, Health services use
Introduction
Approximately 10% of invasive breast cancers can be attributed to hereditary breast cancer, most commonly resulting from deleterious mutations in BRCA1 and BRCA2 (BRCA) genes (King et al. 2003). Known mutations in these genes confer increased risks of both breast and ovarian cancers, as well as other malignancies. On average by the age of 70, women with BRCA1 and BRCA2 mutations have a 57 and 49% cumulative risk of breast cancer and a 40 and 18% risk of ovarian cancer, respectively. This is in contrast to women in the general population, where the risk of breast and ovarian cancers is 12 and 1.3% (Chen and Parmigiani 2007). Evidence demonstrates that enhanced screening, risk-reducing medications, and prophylactic mastectomy/oophorectomy are effective strategies for reducing cancer incidence and stage at diagnosis among women with deleterious BRCA mutations (Moyer and Force 2014). As such, testing women at high risk for BRCA mutations—specifically, those with a personal or family history of breast and/or ovarian cancer—has been shown to be cost-effective (Anderson et al. 2006; Guillem et al. 2006). Given this body of evidence, guidelines have been established and recommend testing for women with significant personal or family history (Berliner et al. 2013); however, use of these genetic tests remains low. In a sample of high-risk breast cancer patients, only 19% of women received genetic testing (Jagsi et al. 2015). Low rates of uptake may be partially due to lack of awareness (Lacour et al. 2008) or costs (Finlay et al. 2008).
On May 14, 2013, an internationally renowned celebrity—Angelina Jolie—brought public awareness to BRCA testing through a widely publicized editorial in the New York Times (Jolie 2013). In this editorial, Jolie described both her decision to undergo BRCA testing due to her family history of breast and ovarian cancer, and her decision to have prophylactic double mastectomy upon learning she had a known deleterious BRCA1 mutation. In the week following this publication, information seeking for genetic testing and procedures increased significantly, (Noar et al. 2015) and visits to The National Cancer Institute’s Preventive Mastectomy and the Physician Data Query Genetics of Breast and Ovarian Cancer webpages increased 795- and 5-fold, respectively (Juthe et al. 2015). This suggests that her editorial increased awareness and information seeking regarding BRCA mutations, testing, and subsequent risk reduction strategies. In the USA, similar trends have occurred following celebrity health disclosures. For example, in March 2000, a journalist (Katie Couric) brought awareness to colorectal cancer screening by undergoing a colonoscopy on national television, and was also credited with increasing rates of colonoscopy following her procedure (Cram et al. 2003). This demonstrates that celebrity health disclosures have the power not only to change awareness but also to change health services use.
While several studies have documented increased awareness of prophylactic mastectomy following Jolie’s disclosure (Juthe et al. 2015; Borzekowski et al. 2014; Lebo et al. 2015), population-level BRCA testing trends and receipt of BRCA-related follow-up health services before and after Jolie’s disclosure have not been described. The objective of this study was to examine the uptake of BRCA testing and subsequent health services use following the 2013 Jolie’s editorial, among commercially insured women.
Methods
Study sample
We used 2012–2014 TruvenHealth MarketScan Commercial Claims and Encounters data for this study. These data represent the healthcare experience of non-retired employees and their dependents enrolled in commercial health insurance plans and include monthly enrollment, inpatient and outpatient medical claims, and outpatient prescription drug claims. The MarketScan data is one of the largest convenience samples available in proprietary U.S. claims databases (Truven Health Analytics 2015).
We identified women (ages 18–64) from January 2013 to December 2014 who received BRCA testing (Healthcare Common Procedure Classification (HCPCS) codes: 81211–81217, S3818–S3820, S3822–S3823). Among women who received BRCA testing, we further restricted to those who were enrolled in their insurance plan for 1 year prior to their BRCA testing date to measure comorbidity. For evaluating follow-up health services receipt, we restricted this sample to women with 3 months of enrollment following BRCA testing. There were 50,557 women meeting these criteria.
In addition to the primary sample, we also identified the number of women enrolled in the health plan by month in 2013 and 2014 who were between the ages of 18 and 64 to evaluate use of the test per 100,000 enrollees in the health plan, controlling for potential changes in enrollment by month.
Time periods of interest
The event of interest was the May 14, 2013 New York Times editorial publication authored by Angelina Jolie, an internationally known celebrity (Jolie 2013). This publication documented Ms. Jolie’s decisions to undergo BRCA testing and, subsequent to learning her BRCA status, to pursue a prophylactic double mastectomy due to her high-risk status and family history of breast and ovarian cancer.
Measures
Outcomes of interest were receipt of BRCA testing and, among women who received testing, receipt of follow-up services within the 3 months following test receipt. Services of interest included health care visits to a surgeon (surgeon listed as the specialist on any inpatient or outpatient claim), receipt of a mastectomy (HCPCS codes: 19303 and 19304, and International Classification of Diseases, Ninth Edition (ICD-9) procedure codes: 85.33–85.36 and 85.41–85.44), and receipt of a breast MRI (HCPCS code: 77059). In addition, we were interested in receipt of genetic counseling within 3 months prior to or after BRCA1/2 testing (HCPCS codes: 96040, S0265). Of note, the genetic counseling HCPCS codes are not specific to cancer-related genetic counseling. We examined these health services, as women with deleterious BRCA1/BRCA2 mutations would be eligible for prophylactic surgery, mammography, and breast MRI, and should attend genetic counseling.
Control variables included in our models were age, region (northeast, south, west, and north central), relationship to plan holder (employee, spouse, or child), and health plan type (Health Maintenance Organization (HMO), Preferred Provider Organization (PPO), or other). These variables were included as covariates, as they were available in the MarketScan dataset and may be related to need for health services use (i.e., age, relationship to plan holder) or access to health services (i.e., region and health plan type) (Andersen 1995). For example, individuals with HMOs often have more closely coordinated care managed through a primary care physician and may be less likely to receive unnecessary services or could have delays in receipt of specialty services due to the need for referrals in most HMO settings.
Statistical analysis
We summarize baseline characteristics of women who received BRCA testing and plotted monthly trends in the proportion of women receiving BRCA testing during 2013 and 2014 per 100,000 women enrolled during each month.
To estimate the impact of Ms. Jolie’s editorial on BRCA testing rates, we used an interrupted time series analysis to compare trends in the number of BRCA tests received prior to May 2013, the level change in testing during May 2013, and the change in trend following May 2013 through the remainder of the study period (Wagner et al. 2002). As an exploratory analysis, we examined bivariate relationships between covariates and uptake of genetic testing using interrupted time series analyses to estimate changes in the number of tests received by month. We also estimated bivariate and multivariate adjusted models using generalized estimating equations with a normal distribution and identity link. Multivariate models controlled for patient and plan covariates noted above.
Next, we estimate subsequent health services use during the 3 months following BRCA testing among women receiving BRCA testing before and after the Jolie’s editorial. We also estimated estimates genetic counseling receipt during 3 months before or following BRCA testing. Separate models were estimated for each of the following binary outcomes: inpatient or outpatient claims submitted by a surgeon, receipt of mastectomy, breast MRI, receipt of mammography or genetic counseling). We used generalized estimating equations with a binomial distribution and log link to estimate risks and risk ratios with 95% confidence intervals for each comparison.
Finally, we estimated mean health plan reimbursement and patient out-of-pocket spending on BRCA testing by month. We compare changes in spending before and after the Jolie’s editorial, using a generalized estimating equation with a normal distribution and log link. We used SAS 9.4 for all analyses and adjusted spending estimates for medical inflation using the medical component of the Consumer Price Index.
Results
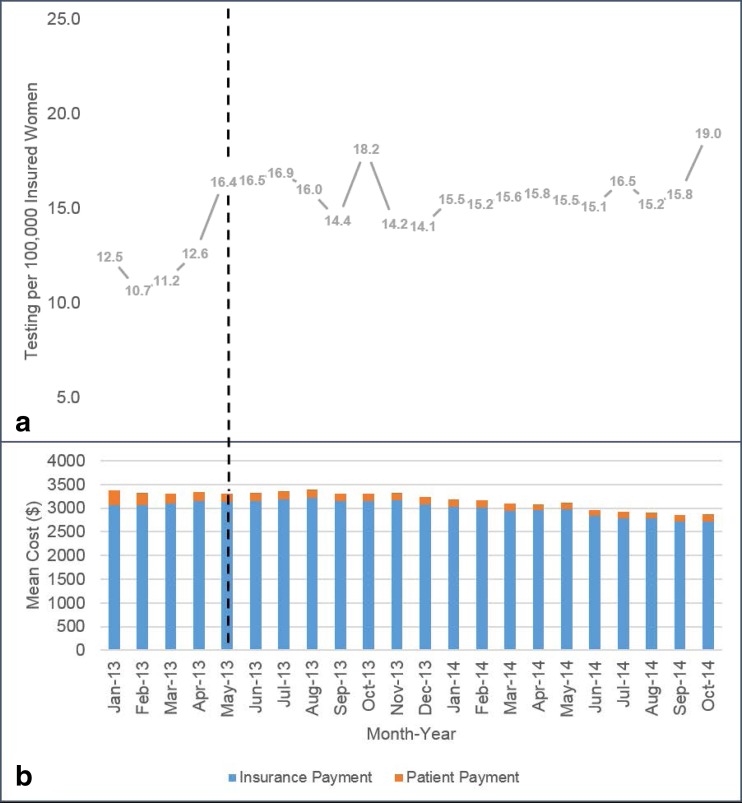
On average, women receiving BRCA testing in this commercially insured population were 46.8 years old (Table 1 online only). The majority of women had a PPO health plan and received insurance through their employer; 44.3% were between the ages of 35 and 49. BRCA testing increased between April and May (the month of Jolie’s editorial publication) from 12.6 to 16.4 tests per 100,000 women (Fig. 1a). When evaluating trends in testing over time, women received approximately 93.6 tests/month at baseline, and there was a non-significant increase in testing of 2.2 tests/month over the entire study period (p = 0.33). However, in May 2013, there was a large and statistically significant increase in testing by 31.1 tests—a 36% increase in testing from the prior month (p < 0.001) (Table 2). We found no difference in testing over time by covariates (i.e., age, region, relationship to the plan holder, and health insurance type) in bivariate analyses (data not shown).
Table 1.
(Online only). Characteristics of commercially insured adult women (aged 18–64) who received BRCA testing in 2013 or 2014
| Total (n = 50,557) | Percentage (%) | |
|---|---|---|
| Variable | ||
| Age, mean/SD | 46.8 | 10.2 |
| Age category (years) | ||
| 18–34 | 6455 | 12.8 |
| 35–49 | 22,406 | 44.3 |
| 50–64 | 21,697 | 42.9 |
| Region | ||
| Northeast | 12,214 | 24.2 |
| North Central | 9413 | 18.6 |
| South | 16,954 | 33.5 |
| West | 10,708 | 21.2 |
| Relationship to plan holder | ||
| Employee | 29,159 | 57.7 |
| Spouse | 20,204 | 40.0 |
| Child/other | 1194 | 2.4 |
| Plan type | ||
| HMO | 5809 | 11.5 |
| PPO | 30,658 | 60.6 |
| Other | 14,090 | 27.9 |
HMO Health Maintenance Organization, PPO Preferred Provider Organization
Fig. 1.
a Unadjusted proportion of women who received BRCA1/2 testing for the management of breast cancer risk, by year. b BRCA1/2 test mean costs by patients and payers, by year. Comparison of mean insurance reimbursement and patient out-of-pocket spending was estimated using a generalized estimating equation with log link and normal distribution for before and after Jolie’s announcement in 05/2013
Table 2.
Interrupted time series results for trends in BRCA testing in 2013 and 2014
| Estimate | p value | |
|---|---|---|
| Coefficient | ||
| Intercept | 93.6 | – |
| Time (months 1–22) | 2.2 | 0.30 |
| Intervention period (May 14, 2013) | 31.1 | <0.001 |
| Months post intervention (5–17) | −0.07 | 0.74 |
Model adjusted for age, region, relationship to plan holder, and insurance type
Rates of post-testing health services use declined following the Jolie’s editorial date (Table 3). Specifically, visits to a surgeon declined from 35.6% of women tested to 31.0% (adjusted risk ratio (aRR) 0.87, 95% confidence interval (CI) 0.84, 0.90), mastectomy from 10.1 to 7.2% (aRR 0.71, CI 0.84, 0.90), and MRI from 12.4 to 9.7% (aRR 0.78, CI 0.73, 0.84). We found a slight increase in mammography from 11.4 to 12.1% (aRR 1.18, CI 1.11, 1.26) and no significant difference in genetic counseling from 7.3 to 7.7% (aRR 1.05, CI 0.97, 1.15). Overall, costs for BRCA testing declined over time (Fig. 1b). After accounting for inflation, mean reimbursement by plans decreased by 3% over the study period (RR 0.97, CI 0.96, 0.98) from $3101 to $3011 per test. For patients, mean out-of-pocket spending decreased by 36% (RR 0.64, CI 0.60, 0.68), from $234 to $150 per test.
Table 3.
Comparing health services use in the 90 days following BRCA testing before and after the Jolie’s announcement
| Unadjusted risk | Adjusted risk ratio | 95% confidence interval | ||
|---|---|---|---|---|
| Tested before (%) | Tested after (%) | |||
| Outcome | ||||
| Any claim submitted by a surgeon | 35.6 | 31.0 | 0.87 | (0.84, 0.90) |
| Any mastectomy | 10.1 | 7.2 | 0.71 | (0.66, 0.77) |
| Any MRI | 12.4 | 9.7 | 0.78 | (0.73, 0.84) |
| Any claim submitted for genetic counselinga | 7.3 | 7.7 | 1.05 | (0.97, 1.15) |
| Any mammogram | 11.4 | 12.1 | 1.18 | (1.11, 1.26) |
Model adjusted for age, region, relationship to plan holder and insurance type
aGenetic counseling claims were captured during 90 days before and after the test. All other outcomes were measured in the 90 days following testing
Discussion
Overall, we found that BRCA genetic testing increased following Jolie’s editorial; furthermore, we observed a lower probability of receiving several health services associated with a deleterious BRCA test result following Jolie’s editorial. BRCA1/2 testing increased following Jolie’s editorial, supporting findings from a recent study conducted in 12 family history clinics and 9 regional genetics services in the United Kingdom showing a 2.5-fold increase in genetic testing referrals and increased inquiries about prophylactic mastectomy following publication of the article (Evans et al. 2014). On the one hand, increased use of BRCA testing may reflect improved access to care; however, increased use of genetic testing may reflect inappropriate screening, as current US Preventative Services Task Force guidelines recommend against BRCA testing among women who are at low risk of having a deleterious BRCA mutation, as the harms of genetic testing may outweigh the benefits (Moyer and Force 2014). This complements recent findings by Borzekowski et al. demonstrating that awareness of Jolie’s story was not associated with improved understanding about genetic testing (Borzekowski et al. 2014). Increased use of the genetic test among women for whom it is not guideline-recommended may reflect overuse of care and exposure to unnecessary costs and harms associated with unnecessary testing. Also, among those who received a genetic test, few had claims indicating receipt of genetic counseling, suggesting that the majority of women who are tested do not receive counseling from a genetic counselor. This may reflect low return of positive BRCA results and/or underuse of genetic counseling services, as recently reported by Armstrong et al. (Armstrong et al. 2015). Within the study period, we also observed a decrease in BRCA testing costs following Jolie’s disclosure; this may partially have contributed to an increase in testing within the study period. In addition to seeing an increase in BRCA testing among all women, women were less likely to receive health services that are associated with having a deleterious BRCA mutation following Jolie’s health disclosure. One possible explanation for this drop in such health services use could be that the additional women who received BRCA testing following the health disclosure were less likely to harbor a deleterious BRCA mutation that necessitates additional prophylactic and/or screening services. Thus, it is possible that increased uptake in testing within this group did not confer increased identification of women with deleterious BRCA mutations.
Finally, BRCA genetic testing also increased in October, breast cancer awareness month, which supports other research indicating temporal trends for increased screening and diagnosis rates during this month (Jacobsen and Jacobsen 2011), likely due to increased cues to action throughout the month, reminding women to “think pink” and attend breast cancer screening (Thackeray et al. 2013).
While this study is among the first to describe trends in genetic testing and health services use following Angelina Jolie’s health disclosure (Desai and Jena 2016), the study is not without limitations. We were unable to examine whether BRCA testing was guideline concordant due to a lack of reliable personal/family history of breast cancer data and lack of BRCA test results. Also, we were unable to include socioeconomic variables, which likely contribute to uptake of genetic testing (Armstrong et al. 2005). Several direct-to-consumer BRCA tests were available to women in 2013; this analysis is unable to account for trends in screening using these tests. Finally, in June of 2013, the United States Supreme Court ruled against patenting of genes; this decision removed the patent on BRCA1/BRCA2 gene tests by Myriad and thus allowed other companies to conduct BRCA testing, increasing access to testing (Kesselheim et al. 2013). Our analysis cannot disentangle effects of the editorial and the court ruling on increased screening following the June 13th ruling. This is particularly important, as we did find that costs of BRCA testing decreased.
Conclusions
This study demonstrates that a celebrity health disclosure can impact health services use, specifically BRCA testing increased following an editorial article by Angelina Jolie. While such disclosures increase awareness and uptake of genetic testing, uptake of health services related to having a deleterious BRCA mutations decreased, suggesting that increased BRCA use did not confer higher identification of women with BRCA mutations. This points to the importance of pairing celebrity disclosure with specific recommendations from health providers to ensure that potential surges in health seeking do not result in unnecessary services use that may not benefit patients at low risk.
Acknowledgements
This project was unfunded. Dr. Roberts was funded by the UNC Lineberger Cancer Control Education Program (CCEP) (R25 CA57726). Dr. Dusetzina receives salary support from the BIRCWH K12 Program and the North Carolina Translational and Clinical Sciences Institute (UL1TR001111).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
This article does not contain any studies with human or animal subjects performed by the any of the authors.
References
- Andersen M (1995) Revisiting the behavioral model and access to medical care: does it matter?. Journal of health and social behavior: 1–10 [PubMed]
- Anderson K, Jacobson JS, Heitjan DF, Zivin JG, Hershman D, Neugut AI, Grann VR. Cost-effectiveness of preventive strategies for women with a BRCA1 or a BRCA2 mutation. Ann Intern Med. 2006;144:397–406. doi: 10.7326/0003-4819-144-6-200603210-00006. [DOI] [PubMed] [Google Scholar]
- Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005;293:1729–1736. doi: 10.1001/jama.293.14.1729. [DOI] [PubMed] [Google Scholar]
- Armstrong J et al. (2015) Utilization and outcomes of BRCA genetic testing and counseling in a national commercially insured population: the ABOUT study JAMA oncology:1–10 doi:10.1001/jamaoncol.2015.3048 [DOI] [PubMed]
- Berliner JL, Fay AM, Cummings SA, Burnett B, Tillmanns T. NSGC practice guideline: risk assessment and genetic counseling for hereditary breast and ovarian cancer. J Genet Couns. 2013;22(2):155–163. doi: 10.1007/s10897-012-9547-1. [DOI] [PubMed] [Google Scholar]
- Borzekowski DL, Guan Y, Smith KC, Erby LH, Roter DL. The Angelina effect: immediate reach, grasp, and impact of going public. Genetics in medicine : official journal of the American College of Medical Genetics. 2014;16:516–521. doi: 10.1038/gim.2013.181. [DOI] [PubMed] [Google Scholar]
- Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2007;25:1329–1333. doi: 10.1200/JCO.2006.09.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cram P, Fendrick AM, Inadomi J, Cowen ME, Carpenter D, Vijan S. The impact of a celebrity promotional campaign on the use of colon cancer screening: the Katie Couric effect. Arch Intern Med. 2003;163:1601–1605. doi: 10.1001/archinte.163.13.1601. [DOI] [PubMed] [Google Scholar]
- Desai S, Jena AB (2016) Do celebrity endorsements matter? Observational study of BRCA gene testing and mastectomy rates after Angelina Jolie’s New York Times editorial BMJ 355: i6357 doi.org/10.1136/bmj.i6357 [DOI] [PMC free article] [PubMed]
- Evans DG et al. (2014) The Angelina Jolie effect: how high celebrity profile can have a major impact on provision of cancer related services Breast Cancer Res 16:442 doi:10.1186/s13058-014-0442-6 [DOI] [PMC free article] [PubMed]
- Finlay E, et al. Factors determining dissemination of results and uptake of genetic testing in families with known BRCA1/2 mutations. Genet Test. 2008;12:81–91. doi: 10.1089/gte.2007.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillem JG, et al. ASCO/SSO review of current role of risk-reducing surgery in common hereditary cancer syndromes. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2006;24:4642–4660. doi: 10.1200/JCO.2005.04.5260. [DOI] [PubMed] [Google Scholar]
- Jacobsen GD, Jacobsen KH. Health awareness campaigns and diagnosis rates: evidence from National Breast Cancer Awareness Month. J Health Econ. 2011;30:55–61. doi: 10.1016/j.jhealeco.2010.11.005. [DOI] [PubMed] [Google Scholar]
- Jagsi R, et al. Concerns about cancer risk and experiences with genetic testing in a diverse population of patients with breast cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2015;33:1584–1591. doi: 10.1200/JCO.2014.58.5885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolie A. My medical choice. New York: The New York Times Company; 2013. [Google Scholar]
- Juthe RH, Zaharchuk A, Wang C. Celebrity disclosures and information seeking: the case of Angelina Jolie. Genetics in medicine : official journal of the American College of Medical Genetics. 2015;17:545–553. doi: 10.1038/gim.2014.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesselheim AS, Cook-Deegan RM, Winickoff DE, Mello MM. Gene patenting—the supreme court finally speaks. N Engl J Med. 2013;369:869–875. doi: 10.1056/NEJMhle1308199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King MC, Marks JH, Mandell JB, New York Breast Cancer Study Group Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science. 2003;302:643–646. doi: 10.1126/science.1088759. [DOI] [PubMed] [Google Scholar]
- Lacour RA, et al. What women with ovarian cancer think and know about genetic testing. Gynecol Oncol. 2008;111:132–136. doi: 10.1016/j.ygyno.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebo PB, Quehenberger F, Kamolz LP, Lumenta DB. The Angelina effect revisited: exploring a media-related impact on public awareness. Cancer. 2015;121:3959–3964. doi: 10.1002/cncr.29461. [DOI] [PubMed] [Google Scholar]
- Moyer VA, USPSTF Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women: U.S. Preventive Services Task Force recommendation statement Annals of internal medicine. 2014;160:271–281. doi: 10.7326/M13-2747. [DOI] [PubMed] [Google Scholar]
- Noar SM, Althouse BM, Ayers JW, Francis DB, Ribisl KM. Cancer information seeking in the digital age: effects of Angelina Jolie’s prophylactic mastectomy announcement. Medical decision making : an international journal of the Society for Medical Decision Making. 2015;35:16–21. doi: 10.1177/0272989X14556130. [DOI] [PubMed] [Google Scholar]
- Thackeray R, Burton SH, Giraud-Carrier C, Rollins S, Draper CR (2013) Using Twitter for breast cancer prevention: an analysis of breast cancer awareness month Bmc Cancer 13 doi:Unsp 50810.1186/1471-2407-13-508 [DOI] [PMC free article] [PubMed]
- Truven Health Analytics (2015) Databases and online tools. http://truvenhealth.com/your-healthcare-focus/life-sciences/data-databases-and-online-tools. Accessed 11 Sep 2015
- Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27:299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]