Abstract
The aim of this study is to assess the difficulty of intracorporeal suturing in single-port surgery, using experimental suturing model in dry box. Subjects were divided for three groups: seven experienced laparoscopic surgeons, seven surgical residents, and seven interns. An experimental suturing model is developed, and working angle was set from 0° to 90°. The completion rate in 0° was significantly lower than that in the other angles. Completion rate of group A was higher than that of the other groups. Precision of task in group A was significantly higher than that of group B and group C in 0° and 60°. Stress score in 0° were significantly higher than that in the other angles. Our study demonstrated that intracorporeal suturing in single-port surgery seems to be more difficult than conventional laparoscopic surgery. Our data should be taken the institution under consideration for introduction of single-port surgery.
Keywords: Single-port surgery, Intracorporeal suturing, Objective and subjective assessment, Reduced port laparoscopic surgery
Main Text
The use of single-port surgery (SPS) is rapidly increasing. SPS was first reported by Navarra et al. [1], who performed a cholecystectomy using SPS in 1997. At our institution, SPS has been performed since July 2008 and is now used for appendectomy, cholecystectomy, colectomy, and gastrectomy.
Several clinical studies have reported on the increased difficulty of SPS compared with standard laparoscopic surgery, based on operative time and surgeon perception [2–5].
The aim of this study was to assess the difficulty of intracorporeal suturing in SPS using an experimental suturing model in a dry box. Suturing is considered to be one of the most difficult laparoscopic skills due to its complexity and intricacy but is required in various advanced laparoscopic procedures [6, 7]. In clinical settings, measurements of differences in technical performance between procedures may be complicated by variations in patient anatomy, case difficulty, interactions between the surgeon and assistant, rater bias, and other factors. In contrast, a laboratory setting allows standardized tasks to be compared in a controlled, safe environment. There are currently few reports of studies that objectively or subjectively evaluated the difficulty of SPS in this way. We assessed the difficulty of intracorporeal suturing in SPS.
Materials and Methods
Subjects
This study was conducted in the Department of Gastroenterological Surgery at the Ishikawa Prefectural Central Hospital, Japan. A total of 21 surgeons were divided into the three groups according to their experience as an operator in laparoscopic surgery: seven experienced laparoscopic surgeons (group A), seven surgical residents (group B), and seven interns (group C). Surgeons in group A had obtained the laparoscopic surgery certification of the Japan Society for Endoscopic Surgery. Surgical residents had been enrolled in postgraduate courses for 3 to 15 years. The interns had not performed laparoscopic surgery before. None of the subjects had any previous experience with the task in the specialized dry box. Consent was obtained from all subjects before inclusion in the study.
Apparatus
The subjects performed tasks in a specialized dry box (Richard Wolf, Knittlingen, Germany) using conventional needle drivers (Karl Storz, Tuttlingen, Germany). The specialized box had a custom-made cover containing a single 3.0-cm opening positioned between the usual port positions, through which an EZ Access (70 × 70 mm, Hakko Co., Nagano, Japan) was inserted. Two conventional needle drivers were used through the EZ Access trocar port (5 mm, Hakko Co.) Visualization was provided through an Excel port (120 mm, Echicon Endo-Surgery Inc., Cincinnati, OH) using a 10 mm, standard length, 30° laparoscope fitted with a 90° light cord adapter (Karl Storz). The monitor was placed directly facing the surgeon at a distance of 1 m with the center of the monitor at eye level. The elevation angle was fixed at 60°, and manipulation angles of 0°, 30°, 45°, 60°, and 90° were assessed. The manipulation angle was the angle between the two instruments (active and assisting). The elevation angle was the angle between the instrument and the horizontal plane.
Task
Each subject performed the intracorporeal suturing task in the specialized dry box three times at each of the manipulation angles. The task consisted of grasping a needle, penetrating the suture pad with the needle at the marked point, and tying a knot in the 150-mm length of 2/0 Vicryl (Ethicon) inserted through the suture pad. The time limit was 5 min per task. If the subjects could not perform the task, the execution time was recorded as 5 min.
Endpoints
The endpoints were the completion rate, execution time, precision, and stress experienced by the surgeon. Precision was evaluated by whether the stitch penetrated the marked point. Stress experienced by the surgeon was evaluated using a questionnaire, which asked subjects to rate each procedure on the following scale: 1, very easy; 2, easy; 3, neutral; 4, difficult; or 5, very difficult.
Statistical Analysis
Statistical analysis was performed using Y-Stat version 7.0 (2008). As the execution times, precision scores, and stress scores were not normally distributed, nonparametric tests were used to compare these data, including the Kruskal-Wallis one-way analysis of variance and the Mann-Whitney U test with Bonferroni correction. Data are expressed as the median. Completion rates were compared using the Pearson χ 2 test. Statistical significance was set at P < 0.05.
Results
Comparisons Among Manipulation Angles
The completion rate was significantly lower at a manipulation angle of 0° than at 30°, 45°, 60°, and 90° (P < 0.05). There were no significant differences in completion rates among the angles of 30°, 45°, 60°, and 90° (P > 0.05).
At a manipulation angle of 0°, the suturing task was completed within the allotted time of 5 min by 19 % of the subjects. The 0° manipulation angle had the longest execution time, but there were no significant differences in execution times among any of the angles (P > 0.05). The precision score was significantly higher at manipulation angles of 30° and 45° than at 0° (P < 0.05). The stress score was significantly higher at a manipulation angle of 0° than at 30°, 45°, 60°, and 90° (P < 0.05) (Table 1).
Table 1.
Effect of manipulation angles of the task
| Angle | ||||||
|---|---|---|---|---|---|---|
| 90° | 60° | 45° | 30° | 0° | P value | |
| Completion rate | 16/21 (76.2 %) | 20/21 (95 %) | 20/21 (95 %) | 20/21 (95 %) | 4/21 (19 %) | P < 0.05b |
| Execution time | 59.5 | 45.9 | 42.6 | 46.2 | 210 | P = 0.003a |
| Precision | 4 | 3 | 5 | 5 | 2 | P < 0.05a |
| Stress | 3 | 2 | 2 | 2 | 5 | P < 0.05a |
aANOVA Mann-Whitney U test with Bonferroni correction
bResult of mxn chi-squared test and Fischer’s test
Comparisons Within Groups
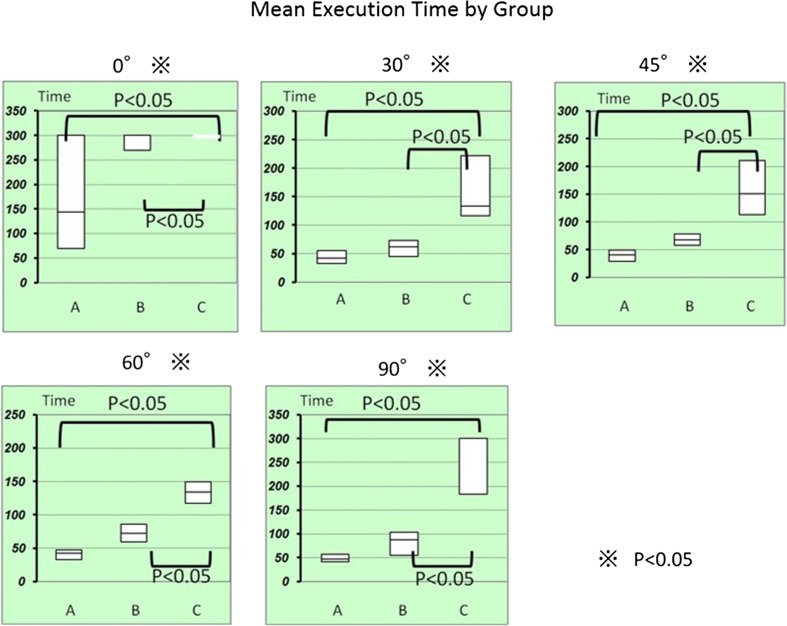
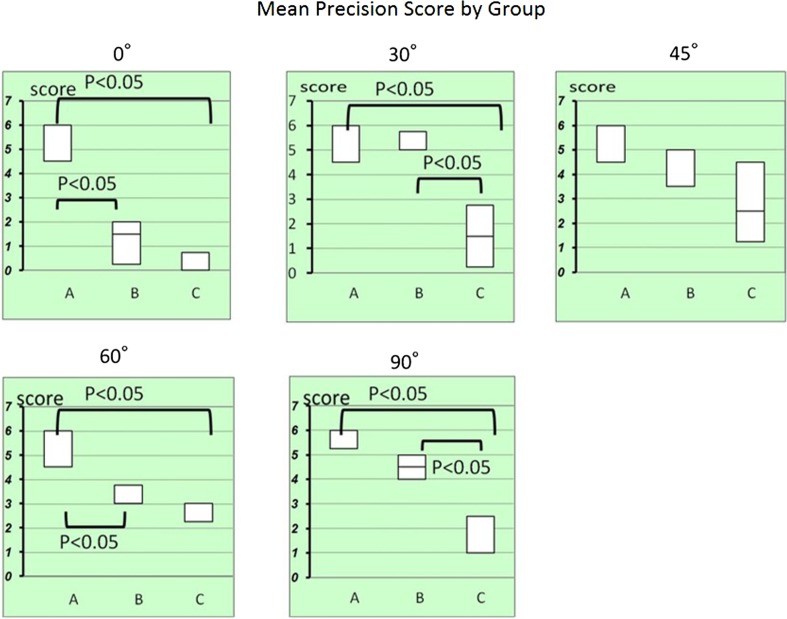
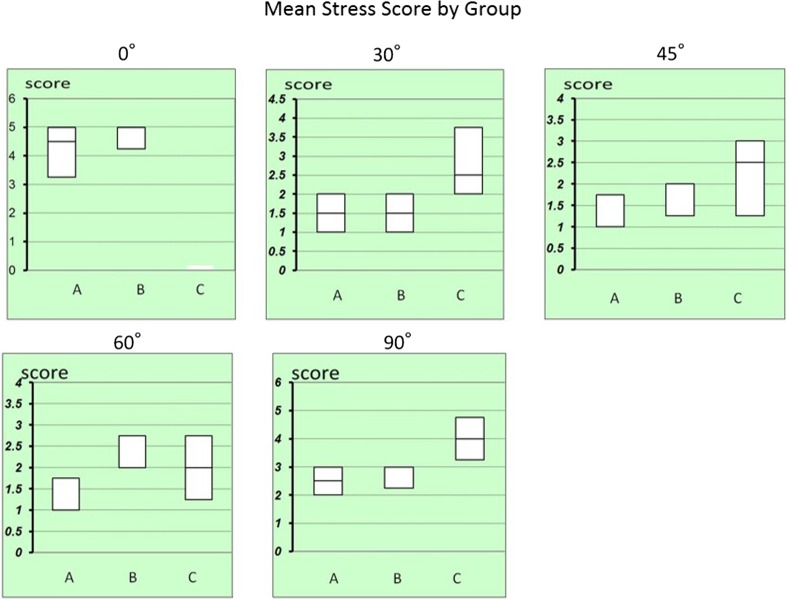
Group A had the highest completion rate (A, 42.8 %; B, 14.2 %; C, 0 %) (P < 0.05) (Table 1). The execution time was significantly shorter in groups A and B than in group C at manipulation angles of 30°, 45°, 60°, and 90° (90°, P = 0.0008; 60°, P = 0.001; 45°, P = 0.001; 30°, P = 0.002) (Fig. 1). The precision score was significantly higher in group A than in groups B and C at manipulation angles of 0° and 60° (60°, P = 0.01; 0°, P = 0.001) (Fig. 2). The precision score at 45° was significantly higher in groups A and B than in group C (P = 0.028) (Fig. 2). There were no significant differences in stress scores among the three groups (P > 0.05) (Fig. 3).
Fig. 1.
Mean execution time (P values significant by post hoc comparison are indicated)
Fig. 2.
Mean precious score (P values significant by post hoc comparison are indicated)
Fig. 3.
Mean stress score (no significant difference)
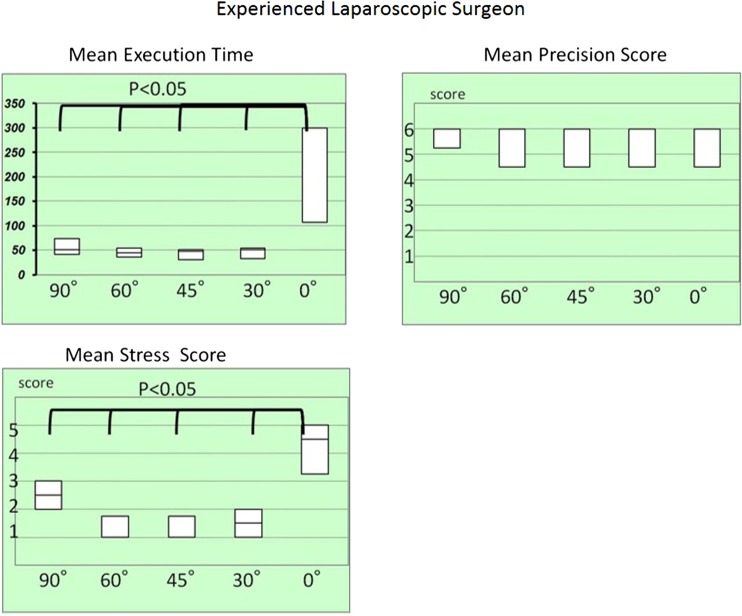
Experienced Laparoscopic Surgeons
Among laparoscopic surgeons, the completion rate was 42.8 % (3/7). The execution time was significantly longer at a manipulation angle of 0° than at 30°, 45°, 60°, and 90° (P < 0.05). The manipulation angle of 0° had significantly higher stress scores than 30°, 45°, 60°, and 90° (P < 0.05). There were no significant differences in precision scores among the different angles (P > 0.05) (Fig. 4).
Fig. 4.
Experienced laparoscopic surgeon (P values significant by post hoc comparison are indicated)
Discussion
The aim of this study was to assess the difficulty of intracorporeal suturing in SPS using an experimental suturing model in a dry box. The recent consensus is that laparoscopic suturing should be an important part of a surgical training program [8]. It has been reported that assessment of laparoscopic suturing is useful for overall assessment of laparoscopic skills [9]. Furthermore, a recent study using a conventional needle driver in a surgical simulator demonstrated that laparoscopic suturing is superior to suturing in SPS [10].
We hypothesized that intracorporeal suturing is more technically challenging in SPS than in standard laparoscopic surgery. We expected that performance would be significantly lower at a manipulation angle of 0° than at 30°, 45°, 60°, and 90°. We also hypothesized that even though intracorporeal suturing in SPS is difficult, experienced laparoscopic surgeons would be able to adapt their training and experience to this new technique. We compared performance among interns, surgical residents, and experienced laparoscopic surgeons.
In this study, we found that the completion rate was much lower at a manipulation angle of 0° than at 30°, 45°, 60°, and 90°. Group A had the highest completion rate.
The execution time was the longest at 0°. Although there were no significant differences between groups A and B at manipulation angles of 30°, 45°, 60°, and 90°, there were significant differences between groups A and B at a manipulation angle of 0°. These results indicate that completion and precision are difficult at a manipulation angle of 0°. Completion of tasks with a manipulation angle of 0° requires a highly skilled and experienced operator.
SPS poses unique challenges in terms of triangulation, retraction, instrument crowding, and visibility. Yang et al. [11] demonstrated that the tasks used for standard laparoscopic surgery training are insufficient for SPS and that SPS training requires specialized tasks. In this study, we found that subjects with specific SPS training had superior outcomes to the other subjects. We therefore consider that SPS is difficult but that surgeons with specific training or experience in laparoscopic surgery can adapt their skills to perform SPS. Specific SPS training is more useful for improving SPS performance than standard laparoscopic surgery training alone [12]. SPS suturing is a difficult task to learn; techniques such as the Thumbs up! Knot and Tornado Knot can be adapted for SPS [13]. In our study, three of four people who had completed all tasks used these techniques. We suggested that these techniques made SPS easily for surgeon.
On the other hand, additional ports should be inserted in a minimally invasive manner. We suggest that surgeons should not hesitate to use them when performing minimally invasive surgery. Additional ports can be easily inserted without causing postoperative pain or an unsatisfactory cosmetic outcome. Additional ports are helpful for obtaining the proper manipulation angle in the laparoscopic view.
We acknowledge that the findings of this study are limited by the laboratory setting. This setting allowed us to control many aspects of the experiment, such as fixing the elevation at 60°, which is the recommended angle for SPS. Other limitations include the choice of trocar, instrument type, and laparoscope. Although there are several port types available for SPS, we used the EZ Access because this is the port that we use in the operating room. Other commercially available, multichannel, single-incision ports or multiple low-profile ports could have been used. Our choice of laparoscope could have affected performance, as we did not use a laparoscope specifically designed to provide an in-line view of the instruments to avoid intracorporeal and extracorporeal instrument collisions, transposed instrument viewing, and loss of triangulation. We kept the laparoscope position fixed, which may not occur in the operating room. As the number of subjects was small, the study did not have the power needed to detect statistically significant differences in all the parameters evaluated.
In summary, intracorporeal suturing is more technically challenging in SPS than in standard laparoscopic surgery. At a manipulation angle of 0°, experienced laparoscopic surgeons can achieve good outcomes; however, they do experience more stress and require longer execution times for 0° than for other angles. We therefore conclude that highly skilled laparoscopic surgeons can perform SPS satisfactorily. However, the associated increased stress and prolonged execution times may result in longer operation times and carry a higher risk of inadvertent injuries, anastomotic complications, and other technical problems. Surgeons should therefore obtain specific SPS training.
In conclusion, our study demonstrated that intracorporeal suturing is more difficult in SPS than in standard laparoscopic surgery. Our results suggested that additional ports should be inserted in a manipulation angle of 30° or 45°, which can keep the cosmetic and make the procedure easy in minimally invasive surgery. However, further and more extensive studies are necessary to confirm of the same assessment for subjects with the technique for SPS.
Acknowledgments
The authors thank Karl Storz for providing the laparoscopy during the study. Furthermore, we acknowledge the surgeons and resident surgeons and interns who performed the task in this study. This study was presented during SAGES in San Diego, March 2011.
Compliance with Ethical Standards
Conflict of Interest
Yasuhiro Ishiyama, Noriyuki Inaki, Hiroyuki Bando, and Tetsuji Yamada have no conflicts of interest or financial ties to disclose.
References
- 1.Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopi cholecystectomy. Br J Surg. 1997;84:695. doi: 10.1002/bjs.1800840536. [DOI] [PubMed] [Google Scholar]
- 2.Galvani CA, Gallo AS, Gorodner MV. Single-incision and dual-incision laparoscopic adjustable gastric band: evaluation of initial experience. Surg Obes. 2012;8(2):194–200. doi: 10.1016/j.soard.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 3.Philipp SR, Miedema BW, Thaler K. Single-incision laparoscopic cholecystectomy using conventional instrumenets:early experience in comparison with the gold standard. J Am Coll Surg. 2009;209:632–637. doi: 10.1016/j.jamcollsurg.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 4.Tang B, Hou S, Cuschieri SA. Ergonomics of and technologies for single-port lapaxroscopic surgery. Minim Invasive Ther Allied Technol. 2012;21(1):46–54. doi: 10.3109/13645706.2011.627924. [DOI] [PubMed] [Google Scholar]
- 5.Champion JK, Hunter J, Trus T, Laycock W. Teaching basic video skills as an aid in laparoscopic suturing. Surg Endosc. 1996;10:23–25. doi: 10.1007/s004649910004. [DOI] [PubMed] [Google Scholar]
- 6.Aggarwal R, Hance J, Undre S, Ratnasothy J, Moorthy K, Chang A, et al. Training junior operative residents in laparoscopic suturing skills is feasible and efficacious. Surgery. 2006;139:729–734. doi: 10.1016/j.surg.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen NT, Mayer KL, Bold RJ, Larson M, Foster S, Ho HS, et al. Laparoscopic suturing evaluation among surgical residents. J Surg Res. 2000;93:133–136. doi: 10.1006/jsre.2000.5969. [DOI] [PubMed] [Google Scholar]
- 8.Cuschieri A, Francis N, Crosby J, Hanna GB. What do master surgeons think of surgical competence and revalidation? Am J Surg. 2001;182:110–116. doi: 10.1016/S0002-9610(01)00667-5. [DOI] [PubMed] [Google Scholar]
- 9.Yamaguchi S, Yoshida D, Kenmotsu H, Yasunaga T, Konishi K, Ieiri S, et al. Objective assessment of laparoscopic suturing skills using a motion-tracking system. Surg Endosc. 2011;25:771–775. doi: 10.1007/s00464-010-1251-3. [DOI] [PubMed] [Google Scholar]
- 10.Santos BF, Enter D, Soper NJ, Hungness ES. Single-incision laparoscopic surgery (SILSTM) versus standard laparoscopic surgery: a comparison of performance using a surgical simulator. Surg Endosc. 2011;25:483–490. doi: 10.1007/s00464-010-1197-5. [DOI] [PubMed] [Google Scholar]
- 11.Yang B, Xu B, Zeng Q, Altunrende F, Wang H, Xiao L, et al. A specialized course of basic skills training for single-port laparoscopic surgery. Surgery. 2011;149:766–775. doi: 10.1016/j.surg.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Santos BF, Reif TJ, Soper NJ, Hungness ES. Effective of training and instrument type on performance in single-incision laparoscopy: results of a randomized comparison using a surgical simulator. Surg Endosc. 2011;25:3798–3804. doi: 10.1007/s00464-011-1791-1. [DOI] [PubMed] [Google Scholar]
- 13.Uchida K, Haruta N, Okajima M, Matsuda D, Yamamoto M. Multimedia article, the keys to the new laparoscopic world Thumbs up! Knot and Tornado Knot. Surg Endosc. 2005;19(6):859. doi: 10.1007/s00464-004-6007-5. [DOI] [PubMed] [Google Scholar]