Abstract
Malignant gastrointestinal neuroectodermal tumor (GNET), a rare soft tissue sarcoma, is a recently described distinct clinicopathological entity. With only a few cases reported in literature till date, there is limited knowledge about the behavior as well as diagnosis of this tumor. GNET mimics several other tumors and hence presents as a diagnostic challenge to clinicians and pathologists alike. We report a case of gastrointestinal neuroectodermal tumors with liver metastasis.
Keywords: Malignant gastrointestinal neuroectodermal tumor, Soft tissue sarcoma, Liver metastasis, Small intestine
Introduction
Malignant gastrointestinal neuroectodermal tumor, previously known as clear cell sarcoma of gastrointestinal tract, is a rare soft tissue sarcoma. There is limited knowledge about the clinical presentation, diagnosis, and behavior of this tumor due to its rarity as well as recent recognition as a distinct clinical entity.
Case Report
A 37-year-old lady presented to us with abdominal pain 2 years back. She was diagnosed with an ileal mass and a 4-cm solitary right lobe liver cystic lesion. She underwent small bowel resection and was diagnosed with neuroendocrine tumor grade 2 with nodal metastasis. Immunohistochemistry showed positivity for chromogranin and synaptophysin, while negative for cytokeratin, CD34, C-kit, and CEA. Mib-1 index was 15–20 %. She presented a year later with suspected anastomotic site recurrence. A contrast-enhanced computed tomography scan showed well-defined liver lesions in segments 6 and 8, with predominantly cystic component and a hypodense lesion in the ileal anastomotic site. 99mTc-HYNIC DOTATOC scan showed abnormal tracer uptake in the ileal region but none in the liver. She underwent resection of the anastomotic site mass, which revealed no evidence of disease. Repeat CT scan done prior to surgery showed no change in the size or character of the liver lesion in segment 6, and no evidence of new lesions; hence, the liver lesion was not addressed. After 9 months, CECT scan showed significant increase in size of the liver lesions. Serial chromogranin levels showed a rising trend from 128 to 326 over 2 years. PET scan showed FDG avid cystic liver lesion measuring 16 × 9.5 cm. DOTATOC scan showed no abnormal uptake. She underwent a right hepatectomy. Histopathology report showed metastatic poorly differentiated carcinoma with diffuse positivity for S100; negative for c-kit, DOG-1, CD34, chromogranin, synaptophysin, CD56, CD10, and PR, MIB1 labeling index was 20 %, suggestive of metastatic GNET. In view of the discrepancy with the existing diagnosis of a NET, the previous bowel specimen was reviewed and found compatible with GNET. Molecular genetic studies (EWSR1 break-apart studies) confirm chromosomal rearrangement in favor of GNET (Fig. 1). She is currently controlled following chemotherapy (EFT 2001 protocol).
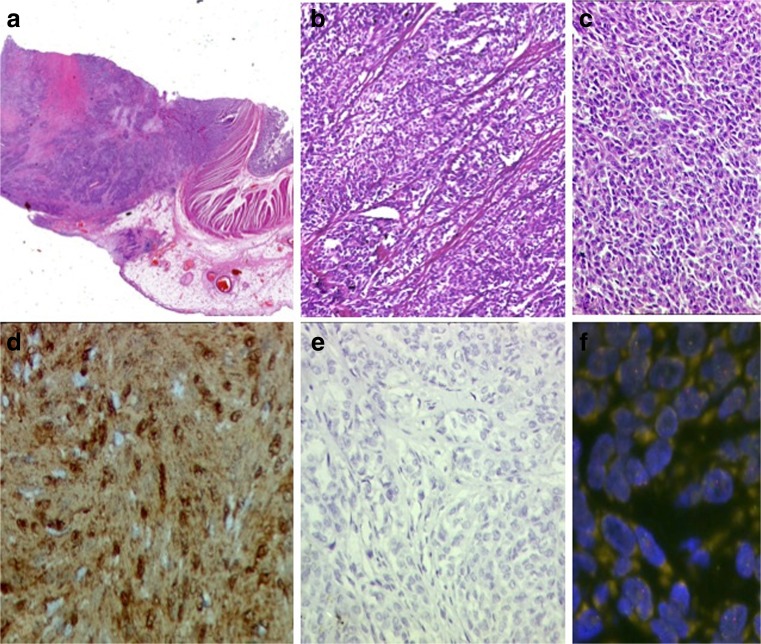
Fig. 1.
Pathologic findings in GNET. a Solid sheets of tumor involving small intestine transmurally (H&E, ×10). b Epithelioid morphology of neoplastic cells with trabecular arrangement (Hematoxylin and Eosin, ×100). c Spindle tumor cells arranged as diffuse sheets (Hematoxylin and Eosin, ×200). d Diffuse S100 immunoreactivity in tumor cells (indirect immunoperoxidase, ×400). e Tumor cells are negative for cKit (indirect immunoperoxidase, ×200). f FISH for EWSR1 break-apart gene shows split signals in tumor cells
Discussion
Malignant GNET is a rare tumor of the gastrointestinal tract. GNET is described as a distinctive tumor, presenting with abdominal symptoms such as pain, obstruction, or an incidentaloma [1]. Lymph nodal (>50 %) and hepatic metastases appear to be common at the time of presentation, or subsequently develop liver metastasis (32 %) on follow-up [1–3]. The small intestine is the most common site [1, 4]. GNET is a highly malignant tumor with poor prognosis and mean survival of 32 months [1]. She is alive and symptom free at 30 months and disease free since the last 6 months. Histopathologically, GNET lacks melanocytic features and exhibit neural differentiation, such as positivity for S100 protein, SOX10, NSE, synaptophysin, CD56, and NB84 [1]. GIST and NET were ruled out as c-kit, DOG-1, chromogranin, and synaptophysin were negative, and S100 was diffusely positive. The differential diagnoses of a GNET are GIST, alveolar rhabdomyosarcoma, synovial sarcoma, and malignant peripheral nerve sheath tumor. Each of these tumors has characteristic IHC and molecular features [4]. GNET is associated with EWSR1 gene rearrangements. Other tumors that exhibit EWSR1 gene rearrangements are Ewing’s sarcoma, angiomatoid fibrous histiocytoma, primary pulmonary myxoid sarcoma, and hyalinizing clear cell carcinoma of the salivary gland [5]. Unlike NETs where functional scans aid in the diagnosis and treatment, there are no reports on the use of imaging and functional scans in GNET. Further studies are needed to evaluate the use of imaging.
Conclusion
GNET is a rare and recently described entity. With better diagnostic tools, in particular IHC and molecular studies, we would be able to study the behavior of this tumor in greater detail. Hence, clinicians and pathologists need to be aware of this entity and consider GNET as a differential diagnosis for gastrointestinal soft tissue tumors with neural features.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no competing interests.
Contributor Information
Keduovinuo K. Keditsu, Phone: +91 9819819709, Email: kkeditsu@gmail.com
Mahesh Goel, Phone: +91 9820504492, Email: drmaheshgoel@gmail.com.
References
- 1.Stockman DL, Miettinen M, Suster S, et al. Malignant gastrointestinal neuroectodermal tumor: clinicopathologic, immunohistochemical, ultrastructural, and molecular analysis of 16 cases with a reappraisal of clear cell sarcoma-like tumors of the gastrointestinal tract. Am J Surg Pathol. 2012;36:857–68. doi: 10.1097/PAS.0b013e31824644ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taminelli L, Zaman K, Gengler C, et al. Primary clear cell sarcoma of the ileum: an uncommon and misleading site. Virchows Arch. 2005;447:772–777. doi: 10.1007/s00428-005-0019-y. [DOI] [PubMed] [Google Scholar]
- 3.Konstantinos LK, Protonotarios A, Lazarou V, et al. Clear cell sarcoma of the jejunum: a case report. World J Surg Oncol. 2013;11:1–4. doi: 10.1186/1477-7819-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kong J, Li N, Wu S et al (2014) Malignant gastrointestinal neuroectodermal tumor: a case report and review of the literature. Oncology letters:1–4. doi:10.3892/ol.2014.2524 [DOI] [PMC free article] [PubMed]
- 5.Thway K, Fisher C. Tumours with EWSR1-CREB1 and EWSR1-ATF1 fusions: the current status. Am J Surg Pathol. 2012;36:1–11. doi: 10.1097/PAS.0b013e31825485c5. [DOI] [PubMed] [Google Scholar]