Abstract
Purpose
PTEN is an important tumor suppressor in breast cancer. Here, we examined the prognostic and predictive value of PTEN and PTEN pseudogene (PTENP1) gene expression in patients with locally advanced breast cancer given neoadjuvant chemotherapy.
Methods
The association between pretreatment PTEN and PTENP1 gene expression, response to neoadjuvant chemotherapy, and recurrence-free and disease-specific survival was assessed in 364 patients with locally advanced breast cancer given doxorubicin, 5-fluorouracil/mitomycin, or epirubicin versus paclitaxel in three phase II prospective studies. Further, protein expression of PTEN or phosphorylated Akt, S6 kinase, and 4EBP1 was assessed in a subgroup of 187 tumors.
Results
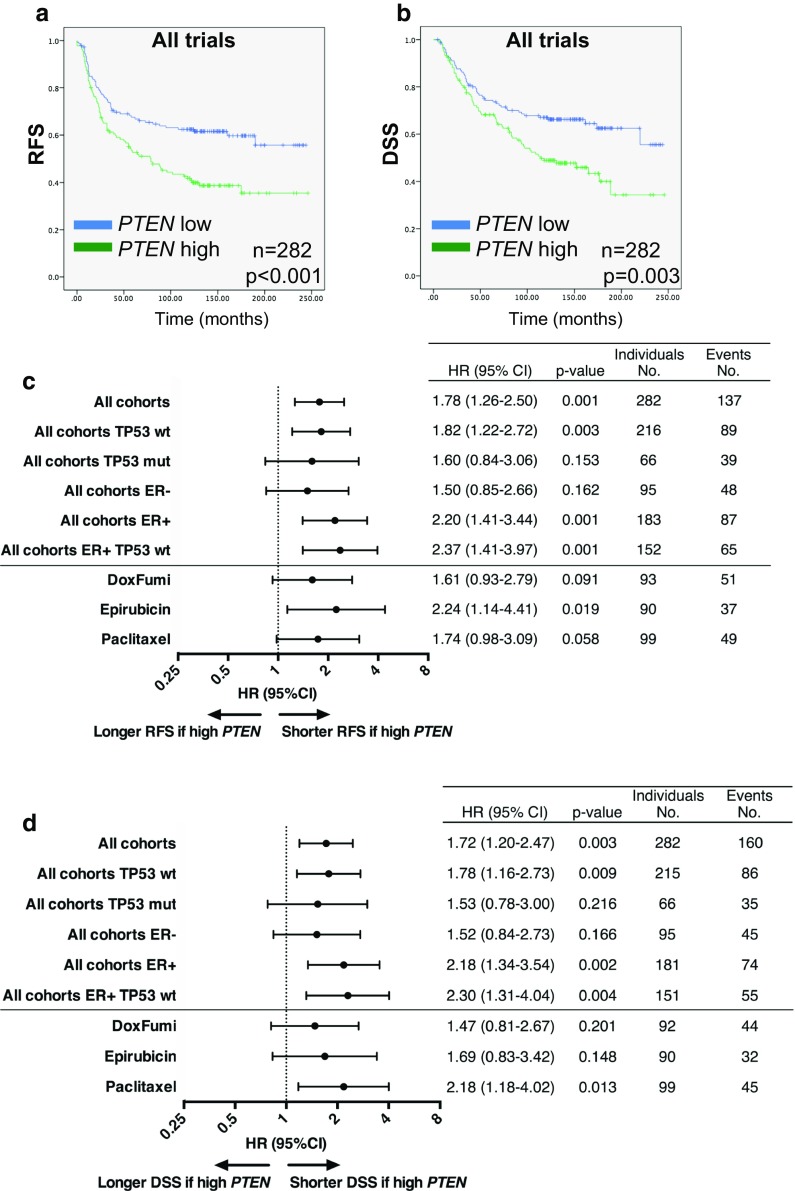
Neither PTEN nor PTENP1 gene expression level predicted response to any of the chemotherapy regimens tested (n = 317). Among patients without distant metastases (n = 282), a high pretreatment PTEN mRNA level was associated with inferior relapse-free (RFS; p = 0.001) and disease-specific survival (DSS; p = 0.003). Notably, this association was limited to patients harboring TP53 wild-type tumors (RFS; p = 0.003, DSS; p = 0.009). PTEN mRNA correlated significantly with PTENP1 mRNA levels (r s = 0.456, p < 0.0001) and PTEN protein staining (r s = 0.163, p = 0.036). However, no correlation between PTEN, phosphorylated Akt, S6 kinase or 4EBP1 protein staining, and survival was recorded. Similarly, no correlation between PTENP1 gene expression and survival outcome was observed.
Conclusion
High intratumoral PTEN gene expression was associated with poor prognosis in patients with locally advanced breast cancers harboring wild-type TP53.
Electronic supplementary material
The online version of this article (doi:10.1007/s10549-017-4160-5) contains supplementary material, which is available to authorized users.
Keywords: Locally advanced breast cancer, PTEN, p53, Prognosis, Predictive factors
Introduction
Mutations in the TP53 tumor suppressor gene, encoding the p53 protein, are associated with lack of response to anthracycline- and mitomycin-containing chemotherapy as well as poor prognosis in breast cancer [1–7]. However, some patients experience lack of response to these chemotherapeutic compounds despite a preserved tumor p53 function, pointing to additional resistance mechanisms [8]. Apart from p53, PTEN is an important tumor suppressor which is frequently inactivated in breast cancer, thus enabling increased signaling of the crucial growth-promoting PI3K-Akt-mTOR pathway [9, 10]. PI3K-Akt-mTOR signaling is involved in resistance to endocrine- and HER2-directed therapy clinically [9, 11], as well as resistance to chemotherapy in preclinical trials [12, 13]. This suggests that PTEN expression may influence response to cancer treatment.
While PTEN somatic mutations are rare, PTEN protein expression is frequently lost in breast carcinomas, pointing to transcriptional and post-transcriptional regulation as possible mechanisms [14, 15]. Of notice, PTEN and p53 reciprocally interact to preserve each other’s protein levels [16]. Further, in vitro data from prostate cancer cell lines suggest that PTEN pseudogene (PTENP1) mRNA transcripts may regulate the PTEN expression level by competing for PTEN-degrading micro RNAs (miRNAs) [17].
The aim of the present study was to assess the prognostic role of pretreatment PTEN and PTENP1 gene expression levels in patients with locally advanced breast cancer, stratified by TP53 mutations status, and the predictive role of PTEN and PTENP1 gene expression levels toward chemotherapy response. In addition, we examined protein expression levels of PTEN as well as key signaling molecules in the PI3K-Akt-mTOR pathway [9]. For this purpose, we used tumor material collected from patients with locally advanced breast cancer treated with different chemotherapy regimens in phase II trials conducted between 1991 and 2007 [1–5].
Methods
Patient material
Pretreatment tumor samples were available from patients with locally advanced breast cancer (T3/T4 and/or N2/N3) included in three neoadjuvant phase II trials described in detail previously [1, 3–5, 18] and outlined in Fig. 1. Dates of enrollment of the first participants to the trials were 18/1-91 (Study 1), 1/6-93 (Study 2), and 24/11-97 (Study 3). In Study 1, patients were given neoadjuvant doxorubicin, 14 mg/m2 qW for 16 weeks. In Study 2, each patient received 5-fluorouracil 1000 mg/m2 and mitomycin 6 mg/m2 (FUMI) q3w for 12 weeks. In Study 3, patients were randomized to either epirubicin 90 mg/m2 (Arm A) or paclitaxel 200 mg/m2 q3w (Arm B), administered in 4–6 courses. Further, in Study 3, patients with suboptimal tumor response to either drug switched to the opposite chemotherapy regimen [5, 18].
Fig. 1.
Flow chart depicting the number of patients with locally advanced breast cancer recruited in Studies 1–3, and the number of samples available from each trial for RNA and immunohistochemistry (IHC) analysis. In Study 3, patients randomized to either epirubicin or paclitaxel were switched to the opposite regimen if tumor regression on the first regimen was insufficient; survival analysis was performed for all patients randomized to each regimen (intention-to-treat) and separately for those patients without crossover (w/o cross) to the opposite regimen. aPatients with stage IV disease were excluded from survival analysis. bOne patient with progressive disease (PD) never became tumor-free, and recurrence-free or disease-free survival could therefore not be assessed. FFPE formalin-fixed paraffin-embedded tissue, IHC immunohistochemistry
Response rates (according to the The Union for International Cancer Control criteria), TNM status, estrogen receptor (ER), and TP53 mutation data have been reported previously [1, 5, 18], and are summarized in Table 1, along with the current assessment of PIK3CA and HER2 status. Follow-up data were available for >10 years or up to time of death for all patients in the trials. A total of 317 patients were assessed for chemotherapy response with respect to gene and protein expression. Among these, 282 patients with stage 3 disease at diagnosis were used for survival analysis.
Table 1.
Baseline patient and tumor characteristics
| Treatment | Study 1a | Study 2a | Study 3Ab | Study 3Bb |
|---|---|---|---|---|
| Doxorubicin | FUMI | Epirubicin | Paclitaxel | |
| Patients | 90 | 34 | 119 | 121 |
| Accrual | 1991–1997 | 1993–2001 | 1997–2003 | 1997–2003 |
| Age (years) | ||||
| Range | 32–88 | 37–82 | 28–70 | 25–70 |
| Median | 64 | 67 | 49 | 48 |
| T stage | ||||
| T2c | 3 | 2 | 1 | 1 |
| T3 | 54 | 15 | 99 | 90 |
| T4 | 33 | 17 | 18 | 30 |
| N stage | ||||
| N0d | 30 | 9 | 52 | 45 |
| N1 | 34 | 14 | 48 | 59 |
| N2 | 26 | 11 | 17 | 17 |
| N3 | 0 | 0 | 1 | 0 |
| M stage | ||||
| M0 | 78 | 24 | 109 | 106 |
| M1 | 12 | 10 | 10 | 15 |
| ER | ||||
| Negative | 13e | 11e | 52 | 49 |
| Positive | 77 | 23 | 66 | 69 |
| Unknown | 0 | 0 | 1 | 3 |
| HER2 | ||||
| Negativef | 24 | 27 | 63 | 66 |
| Positive | 6 | 6 | 30 | 28 |
| Unknown | 60 | 1 | 26 | 27 |
| TP53 | ||||
| TP53 wtg | 64 | 16 | 84 | 89 |
| TP53 mut. | 26 | 18 | 23 | 25 |
| Unknown | 0 | 0 | 12 | 7 |
| Responseh | ||||
| PD | 5 | 9 | 10 | 14 |
| SD | 45 | 13 | 49 | 47 |
| PR | 31 | 10 | 56 | 47 |
| CR | 0 | 0 | 4 | 5 |
| Unknown | 0 | 0 | 0 | 8 |
| TMAi | ||||
| Stage 3 | 0 | 0 | 88 | 81 |
| Stage 4 | 0 | 0 | 7 | 11 |
| RNA/DNAj | ||||
| Stage 3 | 71 | 22 | 90 | 99 |
| Stage 4 | 10 | 10 | 9 | 14 |
| PTEN k | ||||
| PTEN wt | 0 | 0 | 80 | 99 |
| PTEN mut. | 0 | 0 | 2 | 2 |
| Unknown | 0 | 0 | 27 | 4 |
| PIK3CA l | ||||
| PIK3CA wt | 26 | 20 | 82 | 92 |
| PIK3CA mut. | 4 | 12 | 25 | 22 |
| Unknown | 51 | 0 | 12 | 7 |
aData from Studies 1–2 were pooled for statistical analysis due to a low number of patients in Study 2
bData from Study 3 were split into Study 3a (epirubicin) and 3b (paclitaxel), based on the primary chemotherapy given
cT2 tumors only included if axilla stage N2. T stage and all subsequent tumor characteristics given for stage 3 and 4 combined
dN stage by clinical assessment alone
eER negative if tumor ER concentration <10 fmol/mg in Study 1–2. ER assessed by standard IHC in Study 3
fFor Studies 1–2; HER2 assessment available from a subset of the tumors by in situ hybridization only. For Study 3: HercepTest IHC was performed on all tumors, and HER2 in situ hybridization for tumors with staining score 2 by IHC
g TP53 mutation status, whole exome assessed by Sanger sequencing. wt wild-type, mut mutation
hProgressive disease (PD), stable disease (SD), partial response (PR), complete response (CR)
iSubset of patients from whom formalin-fixed paraffin-embedded (FFPE) tumor tissue was available for protein analysis to correlate against gene expression results (PTEN), response rates (stage 3 and 4 disease), or survival (stage 3 only)
jSubset of patients from whom tumor RNA was available for gene expression analysis to correlate against response rates (stage 3 and 4 disease) or survival (stage 3 only)
kSubset of patients from whom tumor DNA was available for PTEN mutation analysis
lSubset of patients from whom tumor DNA was available for PIK3CA mutation analysis to correlate against response rates (stage 3 and 4 disease) or survival (stage 3 only)
Tumor samples
In each protocol, tumor samples were collected by incisional biopsies prior to commencing cancer therapy. Samples were snap frozen and stored in liquid nitrogen until DNA/RNA analysis. In the present investigation, tumor RNA was available from 325 patients; 81 patients from Study 1, 32 patients from Study 2, and 212 patients from Study 3. Among patients with tumor RNA available, seven lacked response data and 43 had primary metastatic disease, leaving 318 patients for response evaluation and 282 patients for survival analysis with respect to gene expression results (Fig. 1).
Pretreatment formalin-fixed paraffin-embedded (FFPE) tumor tissue was available from 193 patients in Study 3 as tissue microarrays (TMAs), but due to the lack of tumor tissue in some core biopsies or staining artifacts, incl. missing cores, only 187 patients could be evaluated for any particular protein. Among patients with TMA tumor tissue available, seven lacked response data, 18 had primary metastatic disease, whereas one patient did not undergo breast surgery and was unfit for calculation of recurrence-free survival, leaving 179 patients for response evaluation and 169 patients for survival analysis with respect to protein staining results (Fig. 1).
Basic genomic procedures
Procedures, primers, and antibodies used for RNA and DNA analysis are described in detail in Online Resource 1.
Immunohistochemistry (IHC) and in situ hybridization (ISH)
Procedures used for IHC and ISH analysis are described in detail in Online Resource 1. The antibodies used for protein analysis were monoclonal anti-Akt (phosphorylated Ser 473), monoclonal anti-HER2 (4B5, Dako), polyclonal anti-PTEN, polyclonal anti-S6 kinase (S6K, phosphorylated Ser 371, Abcam), mouse monoclonal anti-S6K (phosphorylated Thr 389), and polyclonal anti-4EBP1 (phosphorylated Thr 70). All antibodies were developed in rabbit, and purchased from Cell Signaling unless specified otherwise. Immunostaining was evaluated by two independent researchers, and given a semi-quantitative score of 0 (no staining) to 3 (strong staining). Whereas both nuclear and cytoplasmic staining were assessed for PTEN, cytoplasmic staining was scored for 4EBP1, and nuclear staining for Akt and S6K. In a combined PI3K pathway analysis, absent PTEN protein staining, phosphorylated Akt staining, phosphorylated S6K staining, and PIK3CA mutation were each given a score of one each, and “PI3K pathway activation” was defined as a score of two or higher.
Statistics
Correlation analysis between PTEN mRNA expression level and PTEN staining was performed using Spearman's rho. Mann–Whitney test was used for comparison of mRNA or protein staining levels between tumor subgroups. The Chi-square test was used to assess the correlations between PIK3CA mutation status and phosphorylation status of Akt, S6 K, 4EBP1 proteins or between PIK3CA mutations and response to chemotherapy. Chi-square test was also used to assess the correlation between IHC staining and chemotherapy response. Survival data were assessed by Cox regression analysis calculating hazard ratios for each parameter. For Kaplan–Meier plots, patient subgroups were compared by the log-rank test. Due to a smaller number of patients, the survival data from Studies 1 to 2 were analyzed in concert, as described previously [1]. Recurrence-free (RFS) and disease-specific survival (DSS) were defined as time from inclusion in the trial until breast cancer recurrence or death due to breast cancer, respectively. Deaths for reasons other than breast cancer, or patients still alive at the time of analysis, were treated as censored observations. PTEN and PTENP1 gene expression values were sorted for each of the three trials separately and divided by the median value into two groups defined as PTEN or PTENP1 “low” (i.e., below the median) and “high” (i.e., above the median). Multivariate analysis was performed using Cox regression to evaluate the independent prognostic impact of PTEN, PTENP1, TP53, PIK3CA, HER2, and ER status in this cohort of locally advanced breast cancers. Statistical analyses were performed using the SPSS 22/PASW 17.0 and Graph Pad Prism v6 software packages. All p-values reported are two-tailed, and p < 0.05 was considered statistically significant.
Results
PTEN, PTENP1, and TP53 gene expression
Baseline patient and breast cancer characteristics from Studies 1-3 are summarized in Table 1. PTEN gene expression by quantitative/real-time PCR (qPCR) was detectable in all 318 tumors with a defined treatment response (Fig. 2a). In contrast, PTENP1 expression was undetectable in 96 tumors (30%; Fig. 2b). There was a significant, albeit not uniform correlation between PTEN and PTENP1 mRNA expression levels (r s = 0.456, p < 0.0001; Fig. 2c). Whereas PTEN mutations were identified in four out of 183 breast cancers (2.2%), PIK3CA mutations were found in 63 out of 220 (29%), and TP53 mutations in 92 out of 253 (36%) tumors analyzed (Table 1). Among the four tumors with PTEN mutations, two had PTEN gene expression above and two below the median (data not shown). No significant differences in PTEN or PTENP1 gene expression were observed in subgroups stratified by ER, HER2, PIK3CA, or TP53 mutation status or by comparison of triple-negative breast cancer (ER/PGR/HER2 negative; TNBC) vs. non-TNBC (data not shown). TP53 gene expression was undetectable in seven out of 273 tumors (2.5%), and a significant correlation was observed between TP53 and PTEN gene expression in these 273 tumors from Studies 1 to 3 where both transcripts were measured (r s = 0.227, p < 0.0002). This correlation between TP53 and PTEN mRNA levels remained significant (r s = 0.150, p < 0.05), if 47 out 212 tumors with known TP53 or PTEN mutations (Study 3) were excluded from the analysis.
Fig. 2.
a Gene expression of PTEN in locally advanced human breast cancers prior to starting neoadjuvant epirubicin, paclitaxel, doxorubicin, or 5-FU/mitomycin (FUMI), Studies 1–3 combined. Sorted by response group and increasing PTEN levels. b Gene expression of PTEN pseudogene (PTENP1) in locally advanced human breast cancers prior to starting neoadjuvant chemotherapy, sorted by response group and increasing PTEN levels (same as a). c Scatter plot depicting the correlation between PTEN and PTENP1 gene expression in breast cancers from the epirubicin/paclitaxel, doxorubicin, FUMI trials combined. d Scatter plot depicting the correlation between PTEN gene expression and PTEN protein expression in breast cancers from the epirubicin/paclitaxel, doxorubicin, FUMI trials combined. PTEN and PTENP1 mRNA levels in a–d are depicted as the mean gene expression of three separate real-time RT-PCR runs, as a fraction of RPLP2 expression, and corrected for cDNA pool. Gene expression in a–b is not depicted beyond eight times the RPLP2 expression to visualize better differences between the tumor samples. PD progressive disease, SD stable disease, PR partial response, CR complete response
PTEN and PI3K pathway protein expression
IHC staining results for PTEN, and phosphorylated Akt (Ser 473), S6K (Ser 371 or Thr 389), and 4EBP1 (Thr 70) are summarized in Online Resource 2. High-quality immunostaining was observed for all antibodies used, apart from phosphorylated S6K (Thr 389) which yielded poor staining of the tissue microarrays. At the same time, it has been established previously that phosphorylation at the S6K Ser371 phosphorylation site is essential for Thr389 phosphorylation [19], indicating that the staining results for Ser371 should correlate to Thr389 staining. A weak correlation (r s = 0.163, p = 0.036) was established between PTEN gene expression and the corresponding PTEN protein staining level in 166 tumors from which both RNA and TMA tissue blocks were available (Fig. 2d). However, there was no correlation between a low PTEN gene expression level and increased Akt (Ser 473) or S6K (Ser 371 or Thr 389) phosphorylation in breast cancers from which both RNA and IHC tissue samples were available for such comparisons (n = 163). Also, there was no correlation between the absence of PTEN protein staining and increased Akt (Ser 473) or S6K (Ser 371 or Thr 389) phosphorylation by comparison of IHC tissue samples (data not shown). “PI3K pathway activation,” defined as two or more of the following: absent PTEN staining, phosphorylated Akt, phosphorylated S6K, and/or PIK3CA mutations, was observed in 117 out of 159 breast cancers in Study 3. PTEN gene expression was significantly higher (p = 0.028) in tumors with pathway activation, compared to tumors without pathway activation (data not shown). However, if split into ER-positive or ER-negative tumors, PTEN gene expression was not significantly higher in neither group in tumors with pathway activation. Akt phosphorylation was significantly more prevalent in tumors harboring PIK3CA mutations (27 out of 38 tumors), as compared to PIK3CA wild-type tumors (55 out of 132 tumors; p = 0.002, data not shown). However, there was no correlation between PIK3CA mutation status and the proportion of tumors with phosphorylation of S6K (Ser371), S6K (Thr389), or 4EBP1 further downstream in the PI3K pathway. In TNBC, a high frequency of absent PTEN staining, and low level of Akt-S6K-4EBP1 phosphorylation was observed, as expected for this breast cancer subtype (Online Resource 2). However, there was no significant difference in PTEN staining between TNBC and non-TNBC tumors (data not shown).
Predictive variables toward chemotherapy response
No association was recorded between pretreatment PTEN or PTENP1 gene expression and response to neither of the chemotherapies given (n = 320 patients with stage 3/4 disease), irrespective of TP53 mutation, PIK3CA mutation, HER2 or ER status (data not shown). Furthermore, no association between PIK3CA mutation status and response to chemotherapies was detected across the three trials (n = 267). Finally, the protein staining intensity for PTEN (n = 179), phosphorylated Akt (n = 178), S6K (Ser 371, n = 173), S6K (Thr 389, n = 183), and 4EBP1 (n = 175), yielded no predictive information toward chemotherapy response among patients in Study 3.
Prognostic impact of PTEN gene expression
Excluding patients with stage 4 disease from the analysis, high PTEN gene expression, defined as a PTEN mRNA level above the median, was associated with significantly shorter RFS (hazard ratio (HR) for recurrence 1.78, 95% confidence interval (CI) 1.26–2.50, p = 0.001), and DSS (HR for breast cancer-specific death 1.72, 95% CI 1.20–2.47, p = 0.003) across the pooled cohort of patients with stage 3 disease (n = 282, Fig. 3a–d). Among tumors wild-type for TP53, a high PTEN level remained a negative prognostic marker, with inferior RFS as well as DSS (HR 1.82, 95% CI 1.22–2.72, p = 0.003 and HR 1.78, 95% CI 1.16–2.73, p = 0.009, respectively; Figs. 3c, d, 4a, b). In contrast, no significant association between outcome and PTEN gene expression level was observed in patients with tumors harboring TP53 mutations (Fig. 3c, d, 4c, d). These findings were consistent across each individual trial (Online Resource 3).
Fig. 3.
a–b Recurrence-free (RFS) and disease-specific survival (DSS) after neoadjuvant chemotherapy in patients with locally advanced breast cancer after neoadjuvant epirubicin, paclitaxel, doxorubicin, or 5-FU/mitomycin (FUMI), Studies 1–3 combined. Groups are split by PTEN gene expression above or below the median. Censored values are marked with +. n indicates the number of patients used for the survival analysis. c–d Forest plot for the association between tumor PTEN gene expression level and recurrence-free (c) or disease-free survival (d) in patients with locally advanced breast cancer. Results are presented as individual hazard ratios (HRs) with corresponding 95% confidence intervals (CIs). HR > 1 indicates that the survival of patients with tumor PTEN gene expression above the median (PTEN high) is shorter than that of patients with PTEN low tumors, while HR < 1 indicates the opposite. RFS recurrence-free survival, DSS disease-specific survival, wt wild-type, mut mutated, ER estrogen receptor
Fig. 4.

a–d Recurrence-free (RFS) and disease-specific survival (DSS) after neoadjuvant chemotherapy in patients with locally advanced breast cancer after neoadjuvant epirubicin, paclitaxel, doxorubicin, or 5-FU/mitomycin (FUMI), Studies 1–3 combined. Groups are split by PTEN gene expression above or below the median, and stratified by TP53 mutation status. Censored values are marked with +. n indicates the number of patients used for the survival analysis. e–f Forest plot for the association between tumor PTEN gene expression level and recurrence-free (e) or overall survival (f) in patients with early breast cancer with data extracted from the The Cancer Genome Atlas (TCGA) Breast Invasive Carcinoma (Cell, 2015) cohort. Results are presented as individual hazard ratios (HRs) with corresponding 95% confidence intervals (CIs). HR > 1 indicates that the survival of patients with tumor PTEN gene expression above the median (PTEN high) is shorter than that of patients with PTEN low tumors, while HR < 1 indicates the opposite. RFS recurrence-free survival, OS overall survival, wt wild-type, mut mutated
If stratified by ER status, high intratumoral PTEN gene expression was associated with inferior RFS (HR 2.20, 95% CI 1.41–3.44, p = 0.001) and DSS (HR 2.18, 95% CI 1.34–3.54, p = 0.002) among patients with ER-positive tumors only; no effect was observed among patients harboring ER negative tumors (Fig. 3c, d). Moreover, the negative prognostic impact of a high PTEN level was evident only in ER-positive tumors harboring wild-type TP53 (Fig. 3c, d), with inferior RFS (HR 2.37, 95% CI 1.41–3.97, p = 0.001) and DSS (HR 2.30, 95% CI 1.31–4.04, p = 0.004). No prognostic impact of PTEN mRNA level was recorded in patients with ER-negative tumors, irrespective of TP53 status (Fig. 3c, d). In contrast, PTEN gene expression above the median was associated with inferior survival outcome among both HER2 negative (RFS; HR 1.69, 95% CI 1.07–2.69, p = 0.026, DSS; HR 1.63, 95% CI 0.99–2.65, p = 0.053) and HER2-positive tumors (RFS; HR 2.52, 95% CI 1.07–5.91, p = 0.034, DSS; HR 3.16, 95% CI 1.19–8.39, p = 0.021, Fig. 3c, d).
Finally, the negative prognostic impact of high PTEN mRNA levels was observed exclusively for PIK3CA wild-type tumors (RFS; HR 1.89, 95% CI 1.23–2.91, p = 0.004, DSS; HR 1.94, 95% CI 1.33–3.07, p = 0.005), with no impact of PTEN level in PIK3CA mutated tumors (Online Resource 3).
Patients with stage 4 disease (n = 44) were excluded from the above survival analysis. However, a high PTEN gene expression was associated with significantly shorter DSS (HR for breast cancer-specific death 2.06, 95% CI 1.08–3.01, p = 0.027) also for patients with primary metastatic disease (data not shown).
Validation using the cancer genome atlas (TCGA) public dataset
To validate our findings in another patient cohort, PTEN gene expression data were extracted from the cBioPortal database [20, 21], and normalized to RPLP2 expression in the same dataset. These gene expression data are based on RNA sequencing in the Breast Invasive Carcinoma (Cell 2015) analysis [22], which are in whole based upon data generated by the TCGA Research Network: http://cancergenome.nih.gov/. Patient outcome for 816 patients with primary breast cancer was compared for tumors with PTEN mRNA levels above or below the median. A negative prognostic impact of high PTEN gene expression was observed for overall survival (OS) (HR 1.59, 95% CI 1.10–2.29, p = 0.014), but not for RFS (Fig. 4e, f). Among tumors wild-type for TP53, a high PTEN level remained a negative prognostic marker, with inferior OS (HR 2.03, 95% CI 1.25–3.30, p = 0.004; Fig. 4e, f). In contrast, no prognostic value was established for PTEN gene expression in tumors harboring TP53 mutations. DNA sequencing data from the same cohort identified PTEN mutations in 42 tumors (5.1%), and 13 tumors thereof exhibited PTEN gene expression above and 29 tumors exhibited PTEN gene expression below the median. A weak negative correlation (r s = −0.090, p = 0.010) was established between the presence of PTEN mutations and the corresponding PTEN gene expression level in the 816 tumors from the TCGA dataset.
Other prognostic variables
No survival difference was observed between patients with tumor PTENP1 gene expression above or below the median within the pooled cohort of patients with stage 3 disease, nor within any of the subgroups (Online Resource 4). Also, there was no prognostic impact of PTENP1 mRNA level in patients with stage 4 disease (data not shown). Similarly, no prognostic impact of either PIK3CA mutation status (n = 238), PTEN protein expression level (n = 168), phosphorylated Akt (n = 167), S6K (n = 162), or 4EBP1 (n = 165) assessed by immunohistochemistry was recorded with respect to RFS and DSS for patients with stage 3 disease (Online Resource 5). Further, in patients with stage 4 disease where tissue was available for IHC (n = 18), no correlation was observed between PTEN protein expression and DSS (data not shown).
Multivariate analysis
Multivariate analysis revealed PTEN expression level and TP53 mutation status to be independent prognostic variables for RFS as well as DSS (Table 2). No significant interaction between PTEN mRNA level and TP53 status with respect to outcome was recorded (Table 2).
Table 2.
Prognostic indicators of survival by multivariate analysis
| Variable | Recurrence-free survival | Disease-specific survival | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | p value | Events/patients | HR (95% CI) | p value | Events/patients | |
| PTEN low | 1.00 | 0.040 | 57/147 | 1.00 | 0.005 | 51/146a |
| PTEN high | 1.48 (1.02–2.14) | 80/135 | 1.69 (1.17–2.42) | 70/135 | ||
| TP53 wt | 1.00 | 0.001 | 98/216 | 1.00 | 0.040 | 86/215a |
| TP53 mut | 1.75 (1.24–2.46) | 39/66 | 1.51 (1.02–2.24) | 35/66 | ||
| Interaction PTEN*TP53 | 0.927 | 0.776 | ||||
The parameters included in the multivariate analysis were PTEN gene expression (high vs. low) and TP53 mutation status (wild-type vs. mutated)
wt wild-type, mut mutated, HR hazard ratio, CI confidence interval
aOne case censored before the earliest event in a stratum for disease-free survival
Discussion
TP53 inactivating mutations are associated with resistance to anthracycline- and mitomycin-containing chemotherapy and poor prognosis in patients with locally advanced breast cancer [1–7]. Among TP53 wild-type breast cancers revealing primary resistance to anthracyclines, mutations in the p53 upstream activator CHEK2 [23] or low expression levels of ATM [24] have been observed. Yet, additional factors are known to influence p53 activation in response to genotoxic stress [25, 26]. One such factor is the PTEN protein encoded by the PTEN gene [10]. In the present work, we provide data demonstrating the negative prognostic role of high PTEN gene expression levels in tumor tissue from patients with locally advanced breast cancer. Notably, the prognostic role of PTEN was observed exclusively in patients whose tumors contain preserved TP53 wild-type status, in accordance with the known functional crosstalk between PTEN and p53 [16, 25, 27–29]. Moreover, our data suggest that the biological impact of PTEN in human breast cancer is mediated via mRNA interactions, given a lack of prognostic impact of PTEN protein staining, and a lack of correlation between PTEN and PI3K-Akt-mTOR signaling activity.
To the best of our knowledge, the prognostic role of PTEN gene expression by qPCR has not been assessed in patients with breast cancer previously. In a study of 70 patients with stage 2 breast cancer, a gene expression profile of “PTEN loss,” including reduced PTEN gene expression, was predictive of poor survival, whereas PTEN protein staining had no prognostic value [30]. However, PTEN gene expression was categorized only as up- or downregulated in this microarray analysis, with no further quantification [30]. Another study found PTEN gene expression to be significantly higher in 93 human breast cancer samples as compared to healthy breast tissue; however, the potential impact on survival was not assessed [31].
While our clinical data are provocative to suggest a negative prognostic role of high intratumoral PTEN gene expression in patients with stage 3 breast cancer, our findings were confirmed by mining the TCGA dataset, to extract RNA sequencing data from 816 patients with stage 1–3 breast cancer [22]. Again, inferior overall survival was observed among patients with high intratumoral PTEN mRNA levels, and in particular, for patients with TP53 wild-type tumors. In this validation cohort, recurrence-free survival did not differ for patients with high versus low PTEN levels, as opposed to our findings. This could be attributed to a high proportion of stage 1–2 breast cancer in the TCGA cohort (74%), with a better prognosis, regardless of PTEN gene expression, compared to patients with high-risk stage 3 disease in our trials.
The biological reason why high PTEN gene expression was associated with an inferior prognosis in our clinical material remains to be elucidated. While a weak correlation between PTEN gene expression and PTEN protein staining was observed, PTEN protein levels had no prognostic impact, pointing to biological interactions at the mRNA level as a probable reason.
Firstly, PTEN and p53 influence each other at the transcriptional level as well as through protein interaction [25]. Apart from binding to and stabilizing the p53 protein [16], PTEN inhibits MDM2 transcription, thus reducing MDM2-mediated p53 degradation [27]. Furthermore, p53 binds to the genomic PTEN locus and increases PTEN transcription [28, 29]. Notably, while we found PTEN and TP53 to correlate at the mRNA expression level, this was observed among tumors harboring wild-type TP53 only. Similar, PTEN expression correlated to outcome only among TP53 wild-type tumors. Interestingly, in vitro data indicate that nuclear PTEN modulates the response to genotoxic stress by control of DNA repair in cancer cells with preserved p53 function [32]. While the role of PTEN as a regulator of PI3K cytoplasmic signaling has been extensively studied, the role of nuclear PTEN to influence cell cycle arrest and DNA repair remains less defined [33, 34]. However, the prognostic impact of PTEN protein staining did not differ if nuclear staining was assessed separately, as opposed to combined nuclear and cytoplasmic staining in the current patient cohort.
Secondly, PTEN mRNA share miRNA binding sites with multiple gene transcripts implicated in cancer progression [35], and high PTEN gene expression could skew the balance between these transcripts in a pro-tumorigenic manner by adsorbing miRNAs which would otherwise target and degrade important oncogenes [36]. Moreover, PTEN and the protein non-coding PTEN pseudogene (PTENP1) share multiple miRNA binding sites [17], and altering the PTEN mRNA level could influence PTENP1 degradation by competing for the same miRNAs [17, 35]. PTEN and PTENP1 could even interact via PTENP1 antisense transcripts which bind to the PTEN promoter and reduce PTEN mRNA expression [37]. While being protein non-coding, PTENP1 transcripts are biologically active and tumor suppressive in various solid cancers [17, 38–40]. Loss of PTENP1 on chromosome 9p was identified in 11 out of 118 human breast cancers in data extracted from array-based comparative genomic hybridization databases by Poliseno et al. [17].
To the best of our knowledge, we present the first analysis of PTENP1 gene expression in human breast cancer. We found PTENP1 to be expressed in 222 out of 318 human breast cancer samples analyzed. However, the positive correlation between PTEN and PTENP1 transcript levels established in the current report, and the known tumor inhibitory role of PTENP1, do not indicate that the negative prognostic impact of high PTEN levels is mediated via its pseudogene. Accordingly, no prognostic impact of PTENP1 was observed in univariate analysis in our patient cohort.
Thirdly, methodological issues associated with immunohistochemistry, such as formalin fixation, antigen retrieval, antibody specificity, and inter-observer variability could explain the lack of strong correlation between PTEN mRNA and PTEN protein levels. In comparison, PTEN mRNA analysis was performed using a standardized qPCR assay with specific primers and validated PCR products which were quantified independently of the observers.
PTEN is a known inhibitor of the growth-promoting PI3 K-Akt-mTOR pathway [9, 41], and lack of PTEN protein expression is generally associated with increased PI3K-Akt-mTOR signaling [9, 42]. While a significant association between PTEN and phosphorylated Akt by IHC was established previously in 655 breast cancers [43], such an association was not observed in another patient cohort [44], and there was no correlation between the loss of PTEN staining and increased Akt phosphorylation in neither of these two trials [43, 44]. In our current TMA analysis, negative PTEN staining was not associated with increased Akt or S6K phosphorylation levels in 163 locally advanced breast cancers, clearly indicating a lack of biological interaction between PTEN and the PI3K-Akt-mTOR pathway in this setting.
The lack of prognostic impact of PTEN protein expression among 168 patients in the current study is in accordance with several large clinical trials in early breast cancer [30, 43–46]. In the recent CLEOPATRA trial in HER2-positive metastatic breast cancer, a low PTEN protein expression was associated with worse OS, but at the same time an improved progression-free survival, whereas the presence of PIK3CA mutations was a definite negative prognostic marker [47]. In the BOLERO-2 trial, patients with ER-positive metastatic breast cancer experienced the same survival benefit from adding the mTOR inhibitor everolimus to exemestane, regardless of “PI3K activation”, defined as low PTEN staining, or AKT1, PIK3CA, PIK3R1 or PTEN mutations [48]. Finally, the prognostic impact of PIK3CA in breast cancer is not well established [49], and our data are consistent with the findings in a recent study, reporting no influence of PIK3CA mutation status on survival outcome among 1008 patients with breast cancer at high risk of relapse [50].
Conclusions
We establish that high PTEN gene expression in locally advanced human breast cancers is a marker of poor prognosis, across three neoadjuvant trials with 282 patients. Furthermore, the prognostic impact of PTEN gene expression is evident only among patients with TP53 wild-type breast cancers. This should be examined further to assess whether the outcome of patients with these breast cancer characteristics could be improved by alternative therapeutic measures in the future.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors are grateful to the patients who participated in the clinical trials which the current study is based upon. Furthermore, the trials could not have been conducted without the skillful expertise of colleagues in the participating Norwegian study centers, and the technical assistance from Elise de Faveri, Nhat Kim Duong, and Beryl Leirvaag in Mohn Cancer Research Laboratory. The authors would also like to acknowledge the TCGA Research Network for making publicly available the breast cancer genomic data used in the current work, and the patients who donated samples for the TCGA breast cancer analysis.
Funding
This work was supported by generous grants from Helse Vest, Bergen Medical Research Foundation, the Norwegian Cancer Society and the Rieber Foundation, Norway. The study sponsors had no involvement in the design of this study, the literature review, data interpretation, writing of the manuscript, or the decision to submit it for publication.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
The study protocols were approved by the Regional Committee for Medical and Health Research Ethics West, reference numbers 192/91-69.91, 39/92-69.91, 06/597, and 082.96. All patients provided informed consent before inclusion in the protocols, which also included future studies on prognostic and predictive factors.
Footnotes
Availability of data and materials
Apart from patient data presented in the article, the full data set is not made publicly available due to ongoing scientific work.
Contributor Information
Synnøve Yndestad, Email: synnove.yndestad@k2.uib.no.
Eilin Austreid, Email: e.austreid@gmail.com.
Stian Knappskog, Email: stian.knappskog@k2.uib.no.
Ranjan Chrisanthar, Email: ranjch@ous-hf.no.
Peer Kåre Lilleng, Email: peer.lilleng@helse-bergen.no.
Per Eystein Lønning, Email: per.lonning@helse-bergen.no.
Hans Petter Eikesdal, Phone: +4755972010, Email: hans.eikesdal@k2.uib.no.
References
- 1.Eikesdal HP, Knappskog S, Aas T, Lonning PE. TP53 status predicts long-term survival in locally advanced breast cancer after primary chemotherapy. Acta Oncol. 2014;53:1–9. doi: 10.3109/0284186X.2014.922215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aas T, Borresen AL, Geisler S, Smith-Sorensen B, Johnsen H, Varhaug JE, Akslen LA, Lonning PE. Specific P53 mutations are associated with de novo resistance to doxorubicin in breast cancer patients. Nat Med. 1996;2:811–814. doi: 10.1038/nm0796-811. [DOI] [PubMed] [Google Scholar]
- 3.Geisler S, Borresen-Dale AL, Johnsen H, Aas T, Geisler J, Akslen LA, Anker G, Lonning PE. TP53 gene mutations predict the response to neoadjuvant treatment with 5-fluorouracil and mitomycin in locally advanced breast cancer. Clin Cancer Res. 2003;9:5582–5588. [PubMed] [Google Scholar]
- 4.Geisler S, Lonning PE, Aas T, Johnsen H, Fluge O, Haugen DF, Lillehaug JR, Akslen LA, Borresen-Dale AL. Influence of TP53 gene alterations and c-erbB-2 expression on the response to treatment with doxorubicin in locally advanced breast cancer. Cancer Res. 2001;61:2505–2512. [PubMed] [Google Scholar]
- 5.Chrisanthar R, Knappskog S, Lokkevik E, Anker G, Ostenstad B, Lundgren S, Risberg T, Mjaaland I, Skjonsberg G, Aas T, Schlichting E, Fjosne HE, Nysted A, Lillehaug JR, Lonning PE. Predictive and prognostic impact of TP53 mutations and MDM2 promoter genotype in primary breast cancer patients treated with epirubicin or paclitaxel. PLoS ONE. 2011;6:e19249. doi: 10.1371/journal.pone.0019249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kandioler-Eckersberger D, Ludwig C, Rudas M, Kappel S, Janschek E, Wenzel C, Schlagbauer-Wadl H, Mittlbock M, Gnant M, Steger G, Jakesz R. TP53 mutation and p53 overexpression for prediction of response to neoadjuvant treatment in breast cancer patients. Clin Cancer Res. 2000;6:50–56. [PubMed] [Google Scholar]
- 7.Bergh J, Norberg T, Sjogren S, Lindgren A, Holmberg L. Complete sequencing of the p53 gene provides prognostic information in breast cancer patients, particularly in relation to adjuvant systemic therapy and radiotherapy. Nat Med. 1995;1:1029–1034. doi: 10.1038/nm1095-1029. [DOI] [PubMed] [Google Scholar]
- 8.Lonning PE. Study of suboptimum treatment response: lessons from breast cancer. Lancet Oncol. 2003;4:177–185. doi: 10.1016/S1470-2045(03)01022-2. [DOI] [PubMed] [Google Scholar]
- 9.Baselga J. Targeting the phosphoinositide-3 (PI3) kinase pathway in breast cancer. Oncologist. 2011;16(Suppl 1):12–19. doi: 10.1634/theoncologist.2011-S1-12. [DOI] [PubMed] [Google Scholar]
- 10.Song MS, Salmena L, Pandolfi PP. The functions and regulation of the PTEN tumour suppressor. Nat Rev Mol Cell Biol. 2012;13:283–296. doi: 10.1038/nrm3330. [DOI] [PubMed] [Google Scholar]
- 11.Pandolfi PP. Breast cancer—loss of PTEN predicts resistance to treatment. N Engl J Med. 2004;351:2337–2338. doi: 10.1056/NEJMcibr043143. [DOI] [PubMed] [Google Scholar]
- 12.Clark AS, West K, Streicher S, Dennis PA. Constitutive and inducible Akt activity promotes resistance to chemotherapy, trastuzumab, or tamoxifen in breast cancer cells. Mol Cancer Ther. 2002;1:707–717. [PubMed] [Google Scholar]
- 13.Wallin JJ, Guan J, Prior WW, Edgar KA, Kassees R, Sampath D, Belvin M, Friedman LS. Nuclear phospho-Akt increase predicts synergy of PI3K inhibition and doxorubicin in breast and ovarian cancer. Sci Transl Med. 2010;2:48ra66. doi: 10.1126/scitranslmed.3000630. [DOI] [PubMed] [Google Scholar]
- 14.Hollander MC, Blumenthal GM, Dennis PA. PTEN loss in the continuum of common cancers, rare syndromes and mouse models. Nat Rev Cancer. 2011;11:289–301. doi: 10.1038/nrc3037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leslie NR, Foti M. Non-genomic loss of PTEN function in cancer: not in my genes. Trends Pharmacol Sci. 2011;32:131–140. doi: 10.1016/j.tips.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Freeman DJ, Li AG, Wei G, Li HH, Kertesz N, Lesche R, Whale AD, Martinez-Diaz H, Rozengurt N, Cardiff RD, Liu X, Wu H. PTEN tumor suppressor regulates p53 protein levels and activity through phosphatase-dependent and -independent mechanisms. Cancer Cell. 2003;3:117–130. doi: 10.1016/S1535-6108(03)00021-7. [DOI] [PubMed] [Google Scholar]
- 17.Poliseno L, Salmena L, Zhang J, Carver B, Haveman WJ, Pandolfi PP. A coding-independent function of gene and pseudogene mRNAs regulates tumour biology. Nature. 2010;465:1033–1038. doi: 10.1038/nature09144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chrisanthar R, Knappskog S, Lokkevik E, Anker G, Ostenstad B, Lundgren S, Berge EO, Risberg T, Mjaaland I, Maehle L, Engebretsen LF, Lillehaug JR, Lonning PE. CHEK2 mutations affecting kinase activity together with mutations in TP53 indicate a functional pathway associated with resistance to epirubicin in primary breast cancer. PLoS ONE. 2008;3:e3062. doi: 10.1371/journal.pone.0003062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shin S, Wolgamott L, Yu Y, Blenis J, Yoon SO. Glycogen synthase kinase (GSK)-3 promotes p70 ribosomal protein S6 kinase (p70S6K) activity and cell proliferation. Proc Natl Acad Sci USA. 2011;108:E1204–E1213. doi: 10.1073/pnas.1110195108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, Jacobsen A, Byrne CJ, Heuer ML, Larsson E, Antipin Y, Reva B, Goldberg AP, Sander C, Schultz N. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–404. doi: 10.1158/2159-8290.CD-12-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, Sun Y, Jacobsen A, Sinha R, Larsson E, Cerami E, Sander C, Schultz N. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal. 2013;6:p11. doi: 10.1126/scisignal.2004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ciriello G, Gatza ML, Beck AH, Wilkerson MD, Rhie SK, Pastore A, Zhang H, McLellan M, Yau C, Kandoth C, Bowlby R, Shen H, Hayat S, Fieldhouse R, Lester SC, Tse GM, Factor RE, Collins LC, Allison KH, Chen YY, Jensen K, Johnson NB, Oesterreich S, Mills GB, Cherniack AD, Robertson G, Benz C, Sander C, Laird PW, Hoadley KA, King TA, Network TR, Perou CM. Comprehensive molecular portraits of invasive lobular breast cancer. Cell. 2015;163:506–519. doi: 10.1016/j.cell.2015.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Staalesen V, Falck J, Geisler S, Bartkova J, Borresen-Dale AL, Lukas J, Lillehaug JR, Bartek J, Lonning PE. Alternative splicing and mutation status of CHEK2 in stage III breast cancer. Oncogene. 2004;23:8535–8544. doi: 10.1038/sj.onc.1207928. [DOI] [PubMed] [Google Scholar]
- 24.Knappskog S, Chrisanthar R, Lokkevik E, Anker G, Ostenstad B, Lundgren S, Risberg T, Mjaaland I, Leirvaag B, Miletic H, Lonning PE. Low expression levels of ATM may substitute for CHEK2/TP53 mutations predicting resistance towards anthracycline and mitomycin chemotherapy in breast cancer. Breast Cancer Res. 2012;14:R47. doi: 10.1186/bcr3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trotman LC, Pandolfi PP. PTEN and p53: who will get the upper hand? Cancer Cell. 2003;3:97–99. doi: 10.1016/S1535-6108(03)00022-9. [DOI] [PubMed] [Google Scholar]
- 26.Lonning PE, Knappskog S. Mapping genetic alterations causing chemoresistance in cancer: identifying the roads by tracking the drivers. Oncogene. 2013;32:5315–5330. doi: 10.1038/onc.2013.48. [DOI] [PubMed] [Google Scholar]
- 27.Chang CJ, Freeman DJ, Wu H. PTEN regulates Mdm2 expression through the P1 promoter. J Biol Chem. 2004;279:29841–29848. doi: 10.1074/jbc.M401488200. [DOI] [PubMed] [Google Scholar]
- 28.Stambolic V, MacPherson D, Sas D, Lin Y, Snow B, Jang Y, Benchimol S, Mak TW. Regulation of PTEN transcription by p53. Mol Cell. 2001;8:317–325. doi: 10.1016/S1097-2765(01)00323-9. [DOI] [PubMed] [Google Scholar]
- 29.Agrawal S, Eng C. Differential expression of novel naturally occurring splice variants of PTEN and their functional consequences in Cowden syndrome and sporadic breast cancer. Hum Mol Genet. 2006;15:777–787. doi: 10.1093/hmg/ddi492. [DOI] [PubMed] [Google Scholar]
- 30.Saal LH, Johansson P, Holm K, Gruvberger-Saal SK, She QB, Maurer M, Koujak S, Ferrando AA, Malmstrom P, Memeo L, Isola J, Bendahl PO, Rosen N, Hibshoosh H, Ringner M, Borg A, Parsons R. Poor prognosis in carcinoma is associated with a gene expression signature of aberrant PTEN tumor suppressor pathway activity. Proc Natl Acad Sci USA. 2007;104:7564–7569. doi: 10.1073/pnas.0702507104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang Y, Liu M, Yang H, Wang J, Liu H, Li X, Li J, Xu J, Li X. PIK3CA mutations are a predictor of docetaxel plus epirubicin neoadjuvant chemotherapy clinical efficacy in breast cancer. Neoplasma. 2014;61:461–467. doi: 10.4149/neo_2014_057. [DOI] [PubMed] [Google Scholar]
- 32.Bassi C, Ho J, Srikumar T, Dowling RJ, Gorrini C, Miller SJ, Mak TW, Neel BG, Raught B, Stambolic V. Nuclear PTEN controls DNA repair and sensitivity to genotoxic stress. Science. 2013;341:395–399. doi: 10.1126/science.1236188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bassi C, Stambolic V. PTEN, here, there, everywhere. Cell Death Differ. 2013;20:1595–1596. doi: 10.1038/cdd.2013.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Milella M, Falcone I, Conciatori F, Cesta Incani U, Del Curatolo A, Inzerilli N, Nuzzo CM, Vaccaro V, Vari S, Cognetti F, Ciuffreda L. PTEN: multiple functions in human malignant tumors. Front Oncol. 2015;5:24. doi: 10.3389/fonc.2015.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poliseno L, Pandolfi PP. PTEN ceRNA networks in human cancer. Methods. 2015 doi: 10.1016/j.ymeth.2015.01.013. [DOI] [PubMed] [Google Scholar]
- 36.Salmena L, Poliseno L, Tay Y, Kats L, Pandolfi PP. A ceRNA hypothesis: the Rosetta Stone of a hidden RNA language? Cell. 2011;146:353–358. doi: 10.1016/j.cell.2011.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johnsson P, Ackley A, Vidarsdottir L, Lui WO, Corcoran M, Grander D, Morris KV. A pseudogene long-noncoding-RNA network regulates PTEN transcription and translation in human cells. Nat Struct Mol Biol. 2013;20:440–446. doi: 10.1038/nsmb.2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen CL, Tseng YW, Wu JC, Chen GY, Lin KC, Hwang SM, Hu YC. Suppression of hepatocellular carcinoma by baculovirus-mediated expression of long non-coding RNA PTENP1 and MicroRNA regulation. Biomaterials. 2015;44:71–81. doi: 10.1016/j.biomaterials.2014.12.023. [DOI] [PubMed] [Google Scholar]
- 39.Guo X, Deng L, Deng K, Wang H, Shan T, Zhou H, Liang Z, Xia J, Li C. Pseudogene PTENP1 suppresses gastric cancer progression by modulating PTEN. Anti-Cancer Agents Med Chem. 2015;16(4):456–464. doi: 10.2174/1871520615666150507121407. [DOI] [PubMed] [Google Scholar]
- 40.Yu G, Yao W, Gumireddy K, Li A, Wang J, Xiao W, Chen K, Xiao H, Li H, Tang K, Ye Z, Huang Q, Xu H. Pseudogene PTENP1 functions as a competing endogenous RNA to suppress clear cell renal cell carcinoma progression. Mol Cancer Ther. 2014 doi: 10.1158/1535-7163.MCT-14-0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cantley LC. The phosphoinositide 3-kinase pathway. Science. 2002;296:1655–1657. doi: 10.1126/science.296.5573.1655. [DOI] [PubMed] [Google Scholar]
- 42.Carracedo A, Pandolfi PP. The PTEN-PI3 K pathway: of feedbacks and cross-talks. Oncogene. 2008;27:5527–5541. doi: 10.1038/onc.2008.247. [DOI] [PubMed] [Google Scholar]
- 43.Panigrahi AR, Pinder SE, Chan SY, Paish EC, Robertson JF, Ellis IO. The role of PTEN and its signalling pathways, including AKT, in breast cancer; an assessment of relationships with other prognostic factors and with outcome. J Pathol. 2004;204:93–100. doi: 10.1002/path.1611. [DOI] [PubMed] [Google Scholar]
- 44.Bose S, Chandran S, Mirocha JM, Bose N. The Akt pathway in human breast cancer: a tissue-array-based analysis. Mod Pathol. 2006;19:238–245. doi: 10.1038/modpathol.3800525. [DOI] [PubMed] [Google Scholar]
- 45.Lazaridis G, Lambaki S, Karayannopoulou G, Eleftheraki AG, Papaspirou I, Bobos M, Efstratiou I, Pentheroudakis G, Zamboglou N, Fountzilas G. Prognostic and predictive value of p-Akt, EGFR, and p-mTOR in early breast cancer. Strahlenther Onkol. 2014;190:636–645. doi: 10.1007/s00066-014-0620-6. [DOI] [PubMed] [Google Scholar]
- 46.Perez EA, Dueck AC, McCullough AE, Chen B, Geiger XJ, Jenkins RB, Lingle WL, Davidson NE, Martino S, Kaufman PA, Kutteh LA, Sledge GW, Harris LN, Gralow JR, Reinholz MM. Impact of PTEN protein expression on benefit from adjuvant trastuzumab in early-stage human epidermal growth factor receptor 2-positive breast cancer in the north central cancer treatment group N9831 trial. J Clin Oncol. 2013;31:2115–2122. doi: 10.1200/JCO.2012.42.2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Baselga J, Cortes J, Im SA, Clark E, Ross G, Kiermaier A, Swain SM. Biomarker analyses in CLEOPATRA: a phase III, placebo-controlled study of pertuzumab in human epidermal growth factor receptor 2-positive, first-line metastatic breast cancer. J Clin Oncol. 2014;32:3753–3761. doi: 10.1200/JCO.2013.54.5384. [DOI] [PubMed] [Google Scholar]
- 48.Hortobagyi GN, Chen D, Piccart M, Rugo HS, Burris HA, 3rd, Pritchard KI, Campone M, Noguchi S, Perez AT, Deleu I, Shtivelband M, Masuda N, Dakhil S, Anderson I, Robinson DM, He W, Garg A, McDonald ER, 3rd, Bitter H, Huang A, Taran T, Bachelot T, Lebrun F, Lebwohl D, Baselga J. Correlative analysis of genetic alterations and everolimus benefit in hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer: results from bolero-2. J Clin Oncol. 2015;34:419–426. doi: 10.1200/JCO.2014.60.1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pang B, Cheng S, Sun SP, An C, Liu ZY, Feng X, Liu GJ. Prognostic role of PIK3CA mutations and their association with hormone receptor expression in breast cancer: a meta-analysis. Sci Rep. 2014;4:6255. doi: 10.1038/srep06255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Papaxoinis G, Kotoula V, Alexopoulou Z, Kalogeras KT, Zagouri F, Timotheadou E, Gogas H, Pentheroudakis G, Christodoulou C, Koutras A, Bafaloukos D, Aravantinos G, Papakostas P, Charalambous E, Papadopoulou K, Varthalitis I, Efstratiou I, Zaramboukas T, Patsea H, Scopa CD, Skondra M, Kosmidis P, Pectasides D, Fountzilas G. Significance of PIK3CA mutations in patients with early breast cancer treated with adjuvant chemotherapy: a Hellenic Cooperative Oncology Group (HeCOG) Study. PLoS ONE. 2015;10:e0140293. doi: 10.1371/journal.pone.0140293. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.