Abstract
Objectives:
Obesity is an important risk factor for the development of colorectal cancer (CRC). Although the impact of bariatric surgery on CRC is conflicting, its impact on precursor lesions is unknown. The aim of this study was to determine whether bariatric surgery before index screening colonoscopy is associated with decreased development of colorectal adenomas.
Methods:
We performed a retrospective cohort study of bariatric surgery patients who had undergone index, screening colonoscopy at an academic center from 2001 to 2014. Patients who had bariatric surgery at least 1 year before index colonoscopy were compared with those who had surgery after colonoscopy, using multivariable logistic regression to control for presurgical body mass index, sex, gender, race, type of surgery, aspirin use, metformin use, smoking, and age at colonoscopy.
Results:
One hundred and twenty-five obese individuals who had bariatric surgery before colonoscopy were compared with 223 individuals who had colonoscopy after surgery. Adenomatous polyps were found in 16.8% of individuals who had surgery first vs. 35.5% who had colonoscopy before bariatric surgery (unadjusted odds ratio (OR) 0.37, 95% confidence interval (CI): 0.21–0.64, P=0.0003). After multivariable adjustment, bariatric surgery before index screening colonoscopy was associated with a decreased risk of adenomas at index colonoscopy (adjusted OR 0.37, 95% CI: 0.19–0.69, P=0.002).
Conclusions:
Bariatric surgery is associated with a decreased risk of colorectal adenomas in obese individuals without a family history of CRC.
Introduction
Both obesity and cancer, debilitating diseases, carry an increasingly heavy burden on patients and the health-care system.1 A significant fraction of colorectal cancer is attributable to modifiable risk factors such as obesity.2, 3 The link between increased body mass index (BMI) and cancer is under an area of heavy investigation, and several publications have addressed the epidemiological link.4, 5 Mechanisms for the causal link have also been proposed, with the American Society of Clinical Oncology advocating the development of strategies to reduce the impact of obesity on cancer.4, 6, 7 In relation to colorectal adenomas specifically, previous work has shown an increased risk of colorectal adenomas in both men and women who are obese compared with non-obese.8 Although it is widely accepted that colorectal cancer develops as a consequence of accumulation of genetic alterations during which normal epithelium is transformed into adenomas, which eventually progress to cancer, the exact mechanism of obesity on these steps is yet to be fully characterized.9
Patients who undergo bariatric surgery have the potential to achieve significant weight loss, accompanied by a significant reduction in mortality rates for those with severe obesity.10 Currently, there is controversy as to whether bariatric surgery increases or decreases the risk of colorectal cancer.11, 12 Furthermore, guidelines for screening of individuals with obesity for colorectal cancer are undeveloped.13 The assumption that bariatric surgeries reduce CRC risk has been recently tested. In a large cohort study of colorectal cancer incidence after bariatric surgery, standardized incidence ratio for CRC following bariatric surgery increased with time (95% confidence interval [CI]: 1.48–2.64) 10 years after surgery.11 Other studies have refuted this claim, showing a reduction in cancer-related mortality in bariatric patients.12, 14, 15 Given the fact that adenomas are precursor lesions of colorectal cancer, we sought to investigate whether bariatric surgery is associated with change in the proportion of individuals who harbor colorectal adenomas. To that end, we conducted a retrospective chart review of bariatric surgery patients without a family history of CRC, who had index screening colonoscopies at our institution.
Methods
Study population
Records from Massachusetts General Hospital (MGH) were reviewed to identify patients who had bariatric surgery at the institution between the years 2000 and 2014 using the Research Patient Data Registry, a Partners Healthcare query database.16 The study was approved by MGH Institutional Review Board (protocol number 2015P002548). All data were collected by detailed review of electronic medical records to identify patients who had bariatric surgery performed after evaluation by the MGH Weight Center. Cases were defined as patients without a family history of CRC who had bariatric surgery before their index screening colonoscopy, which were performed at an MGH or its affiliates, with full records available for analysis. Controls were defined as patients who underwent their bariatric surgery after their index screening colonoscopy. Bariatric surgery was defined as open or laproscopic Roux-en-Y gastric bypass (RYGB), gastric sleeve, and banding aimed at invoking weight loss and its accompanying metabolic changes.
All patients enrolled in the study were required to have had their index screening colonoscopy performed by gastroenterologists at MGH or a Partners Healthcare-affiliated institution with colonoscopy and pathology reports available for review. Patients with known family history of adenomas or colon cancer were excluded, as well as those with incomplete exams, poor prep, or indications other than screening. In addition, to account for undocumented indications other than screening, we selected individuals who underwent index colonoscopy at age 49–60 years. Patients who had a colonoscopy less than a year after bariatric surgery also were excluded given that the maximal weight loss may not have been fully achieved. Three hundred and twenty-eight patients were eligible for analysis.
Covariates
Based on the pre-existing literature, the following variables were included in regression models as potential confounders in the association between bariatric surgery before index screening colonoscopy and adenoma development: age at the time of index screening colonoscopy, sex, race (white vs. non-white), presurgical BMI, type of bariatric surgery, smoking status, metformin use, and aspirin use. Exploratory analyses were conducted where we corrected for BMI at the time of colonoscopy, as well as any interaction between BMI at the time of colonoscopy and bariatric surgery before colonoscopy.
Statistical analysis
For univariate analyses, means and standard deviations were calculated for continuous variables, and analyzed using unpaired Student's t-tests. Categorical variables were analyzed with either χ2 or two-tailed Fisher's exact tests. P<0.05 were considered significant.
To correct for potential confounders in the association of tubular adenoma development with bariatric surgery before colonoscopy, we performed a binomial logistic regression additionally incorporating age at index screening colonoscopy, sex, race, presurgical BMI, bariatric surgery type, any aspirin use within 10 years, smoking status, and any metformin use. Regression coefficients with P<0.05 were considered significant. R 3.1.0 × 64 was used to perform all statistical tests.
Results
Among the 328 eligible study participants, 125 individuals underwent bariatric surgery before their index screening colonoscopy (Table 1). Concordantly, the mean age at the time of bariatric surgery between both groups was statistically significant (47.3 vs. 56.5 years, P<0.0001), as well as BMI at index colonoscopy (31.6 vs. 42.7 kg/m2, P<0.0001). Although age at index colonoscopy of individuals who had bariatric surgery before colonoscopy appeared significantly younger (52.4 vs. 53.7 years, P<0.0001), the magnitude of the difference appeared small. Both groups appeared to be predominantly female and were non-smokers.
Table 1. Demographic characteristics of bariatric surgery cohort.
| Cohort (n=328) | Bariatric surgery before colonoscopy—125 (38.1%) | Bariatric surgery after colonoscopy—203 (61.9%) | P value |
|---|---|---|---|
| Age at surgery | 47.3±0.3 | 56.5±0.3 | <0.0001 |
| Age at colonoscopy | 52.4±0.2 | 53.7±0.20 | <0.0001 |
| Female sex—no. (%) | 92 (73.60%) | 45 (56.25%) | 0.0963 |
| BMI before surgery (kg/m2) | 48.6±0.7 | 44.5±0.5 | <0.0001 |
| BMI 1 year after surgery (kg/m2) | 30.9±1.0 | 33.1±0.6 | 0.0904 |
| Time from surgery to colonoscopy (years) | 5.0± 3.1 | N/A | |
| Type of surgery | 0.9999 | ||
| Lap Roux-en-Y | 79 (63.20%) | 143 (70.40%) | |
| Lap sleeve | 6 (4.80%) | 43 (21.20%) | |
| Lap gastric banding | 5 (4.00%) | 4 (2.00%) | |
| Open Roux-en-Y | 35 (28.00%) | 13 (6.40%) | |
| BMI at Colo (kg/m2) | 31.55±1.24 | 42.74±0.89 | <0.0001 |
| Race—no. (%) | 0.5348 | ||
| White | 102 (81.60%) | 171(84.24%) | |
| Black | 9 (7.20%) | 18(14.40%) | |
| Hispanic | 12 (9.60%) | 13(10.40%) | |
| Native American | 1 (0.80%) | 1(0.08%) | |
| Asian | 1 (0.80%) | 0(0%) | |
| Smokers—no. (%) | 23 (18.40%) | 34(16.75%) | 0.7015 |
| Metformin use—no.(%) | 40 (32.00%) | 50(24.63%) | 0.1463 |
| Aspirin use—no.(%) | 40 (32.00%) | 83(40.89%) | 0.1064 |
| Adenoma—no.(%) | 21 (16.80%) | 72(35.47%) | 0.0003 |
BMI, body mass index; NA, not available.
Data are presented as the mean plus/minus s.e. or number. P values were calculated by Student's t-test, two-tailed Fisher's exact test, or χ2 test. P values less than 0.05 are in bold.
Regarding obesity-related metrics, study participants demonstrated a reduction in BMI 1 year following their bariatric procedure from their preoperative BMI. The mean preoperative BMI was higher for those who underwent bariatric surgery before colonoscopy compared with those who underwent surgery after colonoscopy (48.6 vs. 44.5 kg/m2, P<0.0001, and following the surgery, BMI decreased in both groups to similar levels (30.9 vs. 33.1 kg/m2, P=0.09). Laparoscopic RYGB was the most common procedure performed in both groups.
Univariate analysis of adenoma risk demonstrated a statistically significant fewer number of individuals with polyps in those who had bariatric surgery before index colonoscopy (16.8% vs. 35.5%, P=0.0003). To account for any potential confounding factors, we performed a multivariable logistic regression analysis of our data set with the outcome defined as the presence or absence of adenomatous polyps (Table 2). We also included well-established risk factors for the development of adenomas including sex, race, smoking, aspirin use, metformin use, and age at colonoscopy. In addition, we included obesity-related metrics including presurgical BMI and type of bariatric surgery. From this analysis, we observed bariatric surgery before index screening colonoscopy was still significantly associated with decreased in the proportions with adenomas (adjusted odds ratio (OR) 0.37, 95% confidence interval (CI): 0.19–0.69, P=0.002). In addition, age at index colonoscopy (adjusted OR 1.10, 95% CI: 1.00–1.21, P=0.03) and use of open RYGB (adjusted OR 2.71, 95% CI: 1.23–5.98, P=0.01) were significant factors.
Table 2. Factors affecting likelihood of adenomatous polyps at index screening colonoscopy using multivariable logistic regression analysis (n=328).
| Parameter | P value | Odds ratio | 95% CI for odds ratio |
|---|---|---|---|
| Intercept | 0.0341 | ||
| Bariatric surgery after index screening colonoscopy | 1 (reference) | ||
| Bariatric surgery before index screening colonoscopy | 0.0024 | 0.37 | 0.19, 0.69 |
| Aspirin use | 0.6514 | 1.13 | 0.66, 1.94 |
| Metformin use | 0.4018 | 1.30 | 0.70, 2.40 |
| Sex (male) | 0.6240 | 1.15 | 0.65, 2.05 |
| Race (non-white) | 1 (reference) | ||
| Race (white) | 0.2189 | 1.61 | 0.77, 3.57 |
| Procedure (laparoscopic RYGB) | 1 (reference) | ||
| Procedure (laparoscopic gastric sleeve) | 0.4161 | 1.34 | 0.65, 2.67 |
| Procedure (laparoscopic gastric banding) | 0.9583 | 1.05 | 0.14, 5.08 |
| Procedure (open RYGB) | 0.0131 | 2.71 | 1.23, 5.98 |
| Smoking | 0.1653 | 1.52 | 0.84, 2.73 |
| Presurgical BMI | 0.1842 | 0.97 | 0.94, 1.01 |
| Age at colonoscopy | 0.0349 | 1.10 | 1.01, 1.21 |
BMI, body mass index; CI, confidence interval; RYGB, Roux-en-Y gastric bypass.
P value less than 0.05 is in bold.
As an exploratory analysis, we explored whether the effect of bariatric surgery on the risk of adenoma development was solely attributable to changes in BMI (Table 3). After incorporating BMI at the time of colonoscopy into logistic regression models, we observed that the effect size of bariatric surgery before colonoscopy was preserved. In addition, we tested a model where a possible interaction exists between bariatric surgery timing and BMI at the time of colonoscopy. Both bariatric surgery and the interaction term became significant.
Table 3. Exploratory analyses incorporating BMI at the time of colonoscopy (n=328).
| Parameter | P value | Odds ratio | 95% CI for odds ratio |
|---|---|---|---|
| Model 1 | |||
| Intercept | 0.0142 | ||
| Bariatric surgery after index screening colonoscopy | 1 (reference) | ||
| Bariatric surgery before index screening colonoscopy | 0.0028 | 0.33 | 0.16, 0.67 |
| Aspirin use | 0.6438 | 1.14 | 0.66, 1.94 |
| Metformin use | 0.4077 | 1.29 | 0.70, 2.38 |
| Sex (male) | 0.6946 | 1.12 | 0.63, 1.98 |
| Race (non-white) | 1 (reference) | ||
| Race (white) | 0.2001 | 1.63 | 0.79, 3.60 |
| Procedure (laparoscopic RYGB) | 1 (reference) | ||
| Procedure (laparoscopic gastric sleeve) | 0.4382 | 1.32 | 0.65, 2.67 |
| Procedure (laparoscopic gastric banding) | 0.8784 | 1.14 | 0.16, 5.49 |
| Procedure (open RYGB) | 0.0267 | 2.40 | 1.10, 5.24 |
| Smoking | 0.1470 | 1.55 | 0.85, 2.78 |
| BMI at colonoscopy | 0.9223 | 1.00 | 0.96, 1.03 |
| Age at colonoscopy | 0.0417 | 1.10 | 1.00, 1.20 |
| Model 2 | |||
| Intercept | 0.0669 | ||
| Bariatric surgery after index screening colonoscopy | 1 (reference) | ||
| Bariatric surgery before index screening colonoscopy | 0.0053 | 0.02 | 0.009, 0.28 |
| Aspirin use | 0.6530 | 1.13 | 0.66, 1.94 |
| Metformin use | 0.4155 | 1.29 | 0.69, 2.37 |
| Sex (male) | 0.5838 | 1.17 | 0.66, 2.09 |
| Race (non-white) | 1 (reference) | ||
| Race (white) | 0.2187 | 1.61 | 0.77, 3.55 |
| Procedure (laparoscopic RYGB) | 1 (reference) | ||
| Procedure (laparoscopic gastric sleeve) | 0.5686 | 1.23 | 0.60, 2.46 |
| Procedure (laparoscopic gastric banding) | 0.9920 | 0.99 | 0.14, 4.84 |
| Procedure (open RYGB) | 0.0364 | 2.31 | 1.05, 5.07 |
| Smoking | 0.0953 | 1.67 | 0.91, 3.03 |
| BMI at colonoscopy | 0.1840 | 0.97 | 0.93, 1.01 |
| Age at colonoscopy | 0.0525 | 1.09 | 1.00, 1.20 |
| Bariatric surgery before colonoscopy × BMI at colonoscopy (interaction) | 0.0326 | 1.08 | 1.01, 1.16 |
BMI, body mass index; CI, confidence interval; RYGB, Roux-en-Y gastric bypass.
P values less than 0.05 are in bold.
Discussion
The epidemic proportions of obesity in the United States, and its increasing rates around the world, have aroused considerable concern about a downstream impact on cancer incidence and mortality.1 Obesity is a modifiable risk factor, which makes it an attractive target for reducing the burden of colorectal cancer. Several studies have linked adult weight change with the risk of colorectal cancer.17, 18 The hypothesis that a reduction in obesity may result in a subsequent decrease in colon cancer incidence is rooted in the biological effects of obesity on insulin resistance, adipokine levels, and gut microbiota—all of which have been independently implicated in cancer incidence and progression.19, 20, 21, 22
Although the successful effects of bariatric surgery in reducing known obesity-related comorbidities such as insulin resistance, hypertension, and cardiovascular disease are well established, its impact on colorectal cancer-related outcomes thus far have been mixed. Most notably, a large Swedish study of over 15,000 bariatric patients demonstrated an increase in the incidence of CRC.11, 23, 24 Other studies, including a retrospective cohort mortality study and a recent meta-analysis, have shown that bariatric surgery appears to decrease CRC risk.12, 15 Given these conflicting findings, we sought to explore whether bariatric surgery is associated with a reduction in the proportion of individuals with colorectal adenomas found during index screening colonoscopy. By selecting patients from the same weight loss center who had bariatric surgery either before or after index screening colonoscopy, we attempted to minimize unaccounted confounders, as all study participants were medically fit to undergo bariatric surgery.
In a model for the development of adenomatous polyps, bariatric surgery before index screening colonoscopy was significantly associated with decreased risk of colorectal adenomas. This association is particularly notable given the higher presurgical BMI observed in those who received surgery before colonoscopy. Reasons that previously well-established risk factors such as sex and smoking were not statistically significant include sample size, the large fraction of women in the cohort, as well as the unknown impact of traditional risk factors in the context of severe obesity. Moreover, we could not ascertain exact duration and dosages for medications such as aspirin and metformin because of limitations in the electronic health record. The relatively higher risk seen in open RYGB compared with other bariatric surgeries may reflect other unaccounted, accompanying comorbidities, given the strong preference for laparoscopic approaches by surgeons and patients.
Exploratory analyses suggest that some of the protective effects of bypass may be more than a simple consequence of weight loss, particularly given that the magnitude of the effect was preserved in logistic regression models after adjusting for BMI at colonoscopy. Observational and basic science studies support weight-independent effects of bariatric surgery. Physiologically, insulin resistance is markedly reduced in RYGB and gastric sleeve procedures in the immediate postoperative period.25, 26 Insulin resistance has been linked to an increased rate of advanced adenomas27 through activation of the insulin–insulin-like growth factor signaling axis—which can upregulate Wnt signaling, expression of antiapoptotic proteins, and Akt protein activation.28 Adiponectin, a systemic adipokine, is increased after RYGB.29 In vitro, adiponectin has been demonstrated to inhibit colon cancer cell line proliferation through the regulation of signal transducer and activator of transcription 3 signaling.30 Reproducible shifts in the microbiome have been observed in RYGB patients can alter host metabolism, and evident through microbiome transfer experiments to germ-free mice.31 Mechanistic studies to examine the effects of these microbial shifts on cancer prevention are underway. Future studies with larger cohorts will be required to elucidate the effect of these weight-independent factors.
The key strength of our work is that unlike previous epidemiological studies that examined whether bariatric surgery affects CRC risk, we focused on precursor lesions with extensive patient level data derived from an electronic medical record. Our study is limited to a single-academic center, as well as a population that is primarily Caucasian and female. Given differences in body fat deposition and risks for metabolic disorders among races, validation of these findings in larger and more diverse cohorts will also be required.
In conclusion, we have demonstrated that bariatric surgery before index screening colonoscopy is associated with a decreased risk of adenomas in individuals without family history of CRC. Our work further strengthens the hypothesis that obesity is contributing to the appearance of precancerous colorectal lesions, and offers the suggestion that the benefits of bariatric surgery may extend to primary cancer prevention.
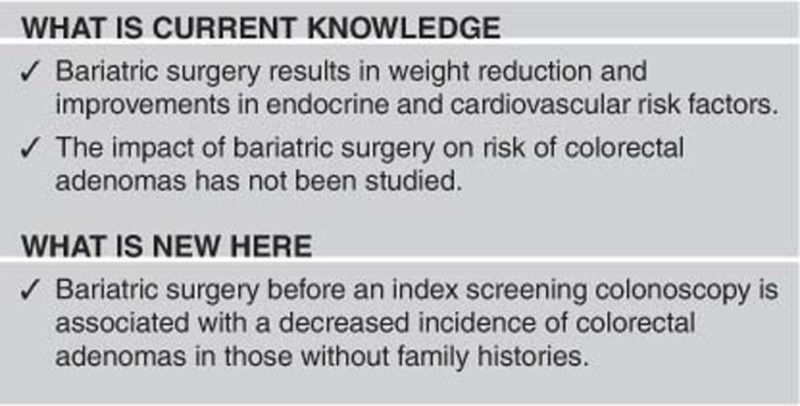
Study Highlights
Footnotes
Guarantor of the article: Manish Gala, MD.
Specific author contributions: D.K., O.Y., and M.G. designed the study. Data collection was performed by D.K., S.G., M.W., K.C., and F.S. Data analysis was performed by D.K., H.K., and M.G. All authors contributed to the writing of the manuscript and providing concepts.
Financial support: This study was supported by the National Institutes of Health (T32 DK007191 to D.K.; R00 AG045144 to Ö.H.Y; K23 DK103119 to M.G.) and the American College of Gastroenterology (Junior Faculty Development Award to M.G.).
Potential competing interests: M.G. has equity interest in New Amsterdam Genomics.
References
- Arnold M, Pandeya N, Byrnes G et al. Global burden of cancer attributable to high body-mass index in 2012: a population-based study. Lancet Oncol 2015; 16: 36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardou M, Barkun AN, Martel M. Obesity and colorectal cancer. Gut 2013; 62: 933–947. [DOI] [PubMed] [Google Scholar]
- Renehan AG, Tyson M, Egger M et al. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 2008; 371: 569–578. [DOI] [PubMed] [Google Scholar]
- Ligibel JA, Alfano CM, Courneya KS et al. American Society of Clinical Oncology position statement on obesity and cancer. J Clin Oncol 2014; 32: 3568–3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhaskaran K, Douglas I, Forbes H et al. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet 2014; 384: 755–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khandekar MJ, Cohen P, Spiegelman BM. Molecular mechanisms of cancer development in obesity. Nat Rev Cancer 2011; 11: 886–895. [DOI] [PubMed] [Google Scholar]
- Iyengar NM, Hudis CA, Dannenberg AJ. Obesity and cancer: local and systemic mechanisms. Annu Rev Med 2015; 66: 297–309. [DOI] [PubMed] [Google Scholar]
- Omata F, Deshpande GA, Ohde S et al. The association between obesity and colorectal adenoma: systematic review and meta-analysis. Scand J Gastroenterol 2013; 48: 136–146. [DOI] [PubMed] [Google Scholar]
- Fearon ER, Vogelstein B. A genetic model for colorectal tumorigenesis. Cell 1990; 61: 759–767. [DOI] [PubMed] [Google Scholar]
- Sjostrom L, Narbro K, Sjostrom CD et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007; 357: 741–752. [DOI] [PubMed] [Google Scholar]
- Derogar M, Hull MA, Kant P et al. Increased risk of colorectal cancer after obesity surgery. Ann Surg 2013; 258: 983–988. [DOI] [PubMed] [Google Scholar]
- Afshar S, Kelly SB, Seymour K et al. The effects of bariatric surgery on colorectal cancer risk: systematic review and meta-analysis. Obes Surg 2014; 24: 1793–1799. [DOI] [PubMed] [Google Scholar]
- Al Hadad M, Dehni N, Alakhras A et al. Screening colonoscopy in the initial workup of bariatric surgery patients: guidelines are needed. Surg Endosc 2014; 28: 1607–1612. [DOI] [PubMed] [Google Scholar]
- Sjostrom L. Bariatric surgery and reduction in morbidity and mortality: experiences from the SOS study. Int J Obes (Lond) 2008; 32 (Suppl 7): S93–S97. [DOI] [PubMed] [Google Scholar]
- Adams TD, Stroup AM, Gress RE et al. Cancer incidence and mortality after gastric bypass surgery. Obesity (Silver Spring, MD) 2009; 17: 796–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalichowski R, Keogh D, Chueh HC et al. Calculating the benefits of a Research Patient Data Repository. AMIA Annu Symp Proc 2006; 2006: 1044. [PMC free article] [PubMed] [Google Scholar]
- Renehan AG, Flood A, Adams KF et al. Body mass index at different adult ages, weight change, and colorectal cancer risk in the National Institutes of Health-AARP Cohort. Am J Epidemiol 2012; 176: 1130–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleksandrova K, Pischon T, Buijsse B et al. Adult weight change and risk of colorectal cancer in the European Prospective Investigation into Cancer and Nutrition. Eur J Cancer 2013; 49: 3526–3536. [DOI] [PubMed] [Google Scholar]
- Song M, Zhang X, Wu K et al. Plasma adiponectin and soluble leptin receptor and risk of colorectal cancer: a prospective study. Cancer Prev Res (Phila) 2013; 6: 875–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byers T, Sedjo RL. Body fatness as a cause of cancer: epidemiologic clues to biologic mechanisms. Endocr Relat Cancer 2015; 22: R125–R134. [DOI] [PubMed] [Google Scholar]
- Aleksandrova K, Jenab M, Boeing H et al. Circulating C-reactive protein concentrations and risks of colon and rectal cancer: a nested case–control study within the European Prospective Investigation into Cancer and Nutrition. Am J Epidemiol 2010; 172: 407–418. [DOI] [PubMed] [Google Scholar]
- Louis P, Hold GL, Flint HJ. The gut microbiota, bacterial metabolites and colorectal cancer. Nat Rev Microbiol 2014; 12: 661–672. [DOI] [PubMed] [Google Scholar]
- Schauer PR, Bhatt DL, Kirwan JP et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med 2014; 370: 2002–2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang SH, Stoll CR, Song J et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg 2014; 149: 275–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickremesekera K, Miller G, Naotunne TD et al. Loss of insulin resistance after Roux-en-Y gastric bypass surgery: a time course study. Obes Surg 2005; 15: 474–481. [DOI] [PubMed] [Google Scholar]
- Meydan C, Goldstein N, Weiss-Shwartz E et al. Immediate metabolic response following sleeve gastrectomy in obese diabetics. Obes Surg 2015; 25: 2023–2029. [DOI] [PubMed] [Google Scholar]
- Chiu HM, Lee YC, Tu CH et al. Effects of metabolic syndrome and findings from baseline colonoscopies on occurrence of colorectal neoplasms. Clin Gastroenterol Hepatol 2015; 13: 1134–42.e8. [DOI] [PubMed] [Google Scholar]
- Aleman JO, Eusebi LH, Ricciardiello L et al. Mechanisms of obesity-induced gastrointestinal neoplasia. Gastroenterology 2014; 146: 357–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Illan-Gomez F, Gonzalvez-Ortega M, Orea-Soler I et al. Obesity and inflammation: change in adiponectin, C-reactive protein, tumour necrosis factor-alpha and interleukin-6 after bariatric surgery. Obes Surg 2012; 22: 950–955. [DOI] [PubMed] [Google Scholar]
- Fenton JI, Birmingham JM. Adipokine regulation of colon cancer: adiponectin attenuates interleukin-6-induced colon carcinoma cell proliferation via STAT-3. Mol Carcinogen 2010; 49: 700–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liou AP, Paziuk M, Luevano JM Jr et al. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci Transl Med 2013; 5: 178ra41. [DOI] [PMC free article] [PubMed] [Google Scholar]


