Abstract
Background and aims
Previous analyses have highlighted significant associations between gambling disorder (GD)/subsyndromal GD and increased rates of anxiety symptoms and anxiety disorders relative to the general population. However, less is known about how anxiety symptoms influence the clinical presentation of gambling problems. The objective of this study was to evaluate the association between anxiety symptoms, gambling activity, and neurocognition across the spectrum of gambling behavior.
Methods
The sample consisted of 143 non-treatment-seeking young adults (aged 18–29 years), in which 63 individuals (44.1%) were classified as recreational gamblers, 47 (32.9%) as having subsyndromal GD, and 33 (23.1%) met criteria for GD.
Results
The main findings were: (a) there was a positive correlation between anxiety severity and gambling severity measured by the number of DSM-5 GD criteria met; (b) there was a positive correlation between anxiety severity and attentional impulsiveness; (c) subjects with suicidality presented higher levels of anxiety; and (d) the severity of anxiety symptoms was negatively correlated with the quality of life.
Discussion and conclusions
This study suggests that anxiety may be associated with relevant clinical variables in the broad spectrum of gambling activity. Therefore, proper management of anxiety symptoms might improve the clinical presentation of gamblers in different areas.
Keywords: gambling disorder, subsyndromal gambling, problem gambling, anxiety, neurocognition
Introduction
Gambling disorder (GD) is associated with high rates of depression, substance-use disorders, and suicidality; as well as occupational and legal problems (Bland, Newman, Orn, & Stebelsky, 1993; Cunningham-Williams, Cottler, Compton, & Spitznagel, 1998; Muelleman, DenOtter, Wadman, Tran, & Anderson, 2002; Petry & Kiluk, 2002; Petry, Stinson, & Grant, 2005; Toce-Gerstein, Gerstein, & Volberg, 2003). The annual cost of GD is approximately 5 billion US dollars within the United States alone (National Gambling Impact Study Commission & James, 1999). Subsyndromal gambling is also a notable concern, and is defined as a significant gambling activity that does not meet full DSM-5 criteria for GD (Grant, Derbyshire, Leppink, & Chamberlain, 2014). Subsyndromal gamblers also show high rates of depression, anxiety disorders, substance-use disorders, financial, legal, family, and professional problems (Cunningham-Williams et al., 1998; Desai, 2004; Gerstein et al., 1999; Grall-Bronnec et al., 2012; Potenza, Maciejewski, & Mazure, 2006; Shaffer & Korn, 2002; Welte, Barnes, Wieczorek, Tidwell, & Parker, 2001). Therefore, it is likely that gambling symptoms present on a continuum, and that symptoms should be assessed across the spectrum of gambling behavior (Cunningham-Williams et al., 1998; Eisen et al., 2001; Gerstein et al., 1999; Grant et al., 2014; Shaffer, Hall, & Vander Bilt, 1999; Shaffer & Korn, 2002; Slutske et al., 2000; Toce-Gerstein et al., 2003; Welte et al., 2001).
The previous analyses have highlighted significant associations between GD/subsyndromal GD and increased rates of anxiety symptoms and anxiety disorders relative to the general population (Black & Moyer, 1998; Bland et al., 1993; Cunningham-Williams et al., 1998; Desai & Potenza, 2008; Petry et al., 2005). One large epidemiological study found a lifetime prevalence of anxiety disorders of 41.3% among disordered gamblers (Petry et al., 2005). A systematic review of epidemiological studies corroborated these findings, with 37% of gamblers reporting a history of a comorbid anxiety disorder (Lorains, Cowlishaw, & Thomas, 2011). In another analysis, Desai and Potenza (2008) also found a high prevalence of panic disorder, generalized anxiety, and social phobia in subsyndromal GD.
Although anxiety symptoms are common in gamblers, less is known about how anxiety symptoms influence the clinical presentation of gambling problems. Various lines of research suggest that anxiety could be a powerful contributor to gambling behavior. First, the research in other addictions (alcohol-use disorder and substance-use disorder) suggests that the behavior may be a way to cope with anxiety (Sher, Trull, Bartholow, & Vieth, 1999). The relief of the anxiety, however, tends to be short-lived, and the symptoms may often reappear more intensely. As a result, a harmful cycle is created, and the anxious individual may therefore present with a more frequent and severe form of the addictive behavior. Second, attentional bias toward threatening elements is a well-characterized phenomenon in anxious individuals and, as a result of this, other non-threatening elements tend to be less perceived (Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg, & Van Ijzendoorn, 2007; Bishop, Duncan, Brett, & Lawrence, 2004; Koster, Crombez, Van Damme, Verschuere, & De Houwer, 2004; Koster, Crombez, Verschuere, Van Damme, & Wiersema, 2006; MacLeod, Mathews, & Tata, 1986; Mogg & Bradley, 1998; Schofield, Johnson, Inhoff, & Coles, 2012). Therefore, an anxious individual who gambles may have a reduced focus on the gambling behavior (i.e., how to bet and how much to bet). This attentional deficit may be another factor leading to a worse severity of GD. Finally, anxiety symptoms decrease some dimensions of quality of life (Spitzer et al., 1995). In this context, the increased emotional suffering and the lower level of life satisfaction could also increase the risk of suicide.
In light of this background, the objective of this study was to evaluate the association between anxiety symptoms, gambling activity, and neurocognition across the spectrum of gambling behavior (recreational gamblers, subsyndromal GD, and GD) in a non-treatment-seeking sample. We assessed the current severity of anxiety symptoms and associations between anxiety symptom severity, gambling symptoms, impulsiveness, and neurocognition. We predicted that anxiety symptoms would be associated with: (a) worse overall severity of GD, measured by increased gambling activity and more losses due to gambling and (b) higher impulsivity measured with clinical and neurocognitive tasks. In addition, we expected that anxiety would be correlated with: (c) worse clinical and neurocognitive attentional performance; (d) lower quality of life; and (e) higher levels of suicidality. If our hypotheses are correct, anxiety symptoms would be associated with variables correlated with poor prognosis and poor overall functioning. Therefore, proper management of anxiety should receive greater attention in clinical practice since it could improve the clinical presentation of gamblers in multiple domains. If our hypotheses are not supported, constant assessment and treatment of anxiety would be a secondary approach in the management of GD.
Methods
Sample
The sample consisted of 143 non-treatment-seeking young adults (aged 18–29 years) [n = 75 (52.1%) male; mean age 24.8 (±2.9) years] with varying levels of gambling severity. Participants were recruited through media advertising (“have you ever gambled?”), and had gambled at least five times during the past year. Also, 63 individuals (44.1%) were classified as recreational gamblers (see later for definitions), 47 (32.9%) as having subsyndromal GD, and 33 (23.1%) met criteria for GD.
Procedures
All assessments were completed as a part of an ongoing study of gambling behavior in young adults. Participants were compensated with a US$50 gift card to a local department store. Subjects were recruited in Chicago/IL and Minneapolis/MN metropolitan areas. Exclusion criteria included the inability to complete the study procedures, inability/unwillingness to provide voluntary written informed consent, and gambling frequency of less than five times in the past year. No medications were administered as a part of this study. Subjects taking medications were allowed to take part in the research.
Measurements
Demographics
Age, gender, marital status, educational status, professional status, ethnicity, and sexual orientation were recorded.
Severity of anxiety symptoms
The Hamilton Anxiety Scale (HAM-A) is a valid and reliable instrument that assesses cross-sectional severity of anxiety symptoms (Hamilton, 1969; Maier, Buller, Philipp, & Heuser, 1988; Snaith, Baugh, Clayden, Husain, & Sipple, 1982). The HAM-A consists of 14 items (score range 0–56) that evaluate a variety of anxiety symptoms (Beck & Steer, 1991). HAM-A total score presents an intra-class coefficient of 0.74 and a concurrent validity between 0.63 and 0.75 (Maier et al., 1988). The HAM-A has shown good internal consistency (Cronbach’s alpha = .893) (Kummer, Cardoso, & Teixeira, 2010). It is probably the most used and accepted scale to evaluate anxiety symptoms.
Clinical variables
-
1.
Gambling behavior: we evaluated the age at the start of regular gambling, the amount of money lost with gambling in the last year, and the average gambling frequency (times per week).
-
2.
Overall severity of GD: we assessed the total number of DSM-5 GD criteria using the Structured Clinical Interview for Gambling Disorder (SCI-PG) (Grant, Steinberg, Kim, Rounsaville, & Potenza, 2004). SCI-PG was first validated using the criteria of the Fourth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-4). Test–retest reliability on the number of GD criteria endorsed showed r = .97 (p = .006) (Grant et al., 2004). We retrospectively processed the electronic saved DSM-4 criteria for a proper adaptation to DSM-5. This procedure was performed deleting the criterion “committed illegal acts such as forgery, fraud, theft, or embezzlement to finance gambling regarding illegal acts,” which was present in the previous manual, DSM-4. Moreover, we lowered the diagnostic threshold from five to four, consistent with DSM-5. Remaining criteria were unchanged. Severity was divided in three categories: recreational gambling (meets 0 DSM-5 criteria), subsyndromal GD (meets 1–3 DSM-5 criteria) and GD (meets 4 or more DSM-5 criteria).
In addition, we investigated the overall gambling severity with the Pathological Gambling Yale-Brown Obsessive-Compulsive Scale (PG-YBOCS). It is a 10-item scale that showed high validity (r = .895) and reliability (Cronbach’s α = .970) (Pallanti, DeCaria, Grant, Urpe, & Hollander, 2005). This scale provides a total score (overall severity) as well as scores in two subscales (urges and behavior subscales).
-
3.
Impulsiveness: evaluated by the Barratt Impulsiveness Scale, version 11 (BIS-11) (Patton & Stanford, 1995), a scale that has been largely used to investigate impulsiveness (Steinberg, Sharp, Stanford, & Tharp, 2013). This scale has shown good internal consistency (Cronbach’s α between .79 and .83) (Patton & Stanford, 1995). BIS-11 provides scores in three different dimensions, based on previous factor analyses: attentional impulsiveness, motor impulsiveness, and non-planning impulsiveness (Patton & Stanford, 1995).
-
4.
Prevalence of illegal acts: the commitment of illegal acts to finance gambling activity has been associated with higher severity of GD (Granero et al., 2015; Strong & Kahler, 2007; Toce-Gerstein et al., 2003). It was evaluated using an open question using previous DSM-4 criteria: “Have you committed illegal acts such as forgery, fraud, theft, or embezzlement to finance gambling?”
-
5.
Suicidality and psychiatric comorbidity: evaluated by the Mini-International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998).
-
6.
Quality of life (quality of life inventory): a 17-item scale that evaluates the subject’s overall quality of life (Frisch, 1994). Alpha coefficients and test–retest correlations for this questionnaire have ranged, respectively, from 0.77 to 0.89 and from 0.80 to 0.91 (Mendlowicz & Stein, 2014).
-
7.
Use of nicotine: assessed by a 20-cigarette pack per day equivalent.
Neurocognitive testing
Individuals with GD tend to present with several neurocognitive deficits such as poorer response inhibition, low cognitive flexibility, worse decision making, and problems with sustained attention and executive functioning (Clark, 2010; Van Holst, van den Brink, Veltman, & Goudriaan, 2010). This study evaluated whether anxiety symptoms affected any of these neuropsychological variables. In this context, participants undertook selected tests from the computerized Cambridge Neuropsychological Test Automated Battery (CANTABeclipse, version 3, Cambridge Cognition Ltd., Cambridge, UK) (Cambridge Cognition, 2015). Task order was fixed and the total duration of cognitive testing was approximately 50 min.
-
1.
Response inhibition: assessed by the stop-signal task, which assesses the subject’s ability to inhibit/suppress motor responses. Individuals react to an arrow stimulus, by touching either a left or right key depending on the direction in which the arrow points. When an audio tone occurs, the participant attempts to suppress their motor response for the particular trial (Morein-Zamir & Sahakian, 2010). The outcome measure of interest is the stop-signal reaction time, an index of the time taken for the person’s brain to stop a response that would normally be made.
-
2.
Cognitive flexibility: investigated with the intra-dimensional/extra-dimensional set shifting test, which evaluates rule learning, reversal, and shifting of attentional focus across stimulus dimensions. The test uses visual stimuli (colorful shapes and white lines) and gives feedback to the individual so that they are able to learn an underlying “rule” about which stimulus is correct, based on trial and error. The underlining rule that determines what is “correct” and “incorrect” changes several times and assesses the individual’s ability to respond with flexibility (Cambrigde Cognition, 2015). The adjusted total number of errors is an overall score of performance.
-
3.
Decision making: assessed using the Cambridge Gamble Task, a test that assesses decision making and risk taking (Cambridge Cognition, 2015; Deakin, Aitken, Robbins, & Sahakian, 2004; Lawrence, Luty, Bogdan, Sahakian, & Clark, 2009). The task simulates gambling activity but uses points for bets, rather than “real” rewards. The main outcome measures in this test are: quality of decision making, proportion of points gambled, and risk adjustment.
-
4.
Sustained attention: evaluated by the Rapid Visual Information Processing paradigm. This task investigates the ability to detect unpredictable target sequences over prolonged period of time (Sarter, Givens, & Bruno, 2001). The task consists of a white box in the center of the computer screen, inside which numbers, from 2 to 9, show up in a pseudo-random manner, at the frequency of 100 digits/min. A′ was used as a measure of sustained attention.
-
5.
Executive functioning: assessed using the One touch stockings of Cambridge task. This test, a variant of a variation of the Tower of London (Owen et al., 1995), investigates goal-directed planning (Cambridge Cognition, 2015). The task presents visual problems to the subject and evaluates the individual’s ability to plan a solution and answer these problems.
Statistical analysis
We analyzed the association between the severity of anxiety symptoms and demographic, clinical, and neurocognitive variables of the participants using Spearman’s coefficients for continuous elements and Mann–Whitney tests for categorical variables.
To control for multiple comparisons, we divided the usual level of significance (p = .05) by the number of variables evaluated in each group of assessments (i.e., clinical variables and neurocognitive testing). Consequently, significance was defined as p ≤ .004 (.05/13 = .004) for clinical variables and p ≤ .007 (.05/7 = .007) for neurocognitive variables.
To reduce the likelihood of confounding variables contributing to the above analyses, we controlled for current major-depressive disorder, alcohol-use disorder, substance-use disorder, and nicotine use. These controls were included, as all four variables have demonstrated significant overlap with anxiety symptoms and several clinical/neurocognitive variables investigated in this study, in prior work (Clark, 2010; Maier et al., 1988).
Ethics
This research was approved by the Institutional Review Boards of the University of Chicago and the University of Minnesota. The study procedures were explained to the participants prior to providing consent, and all participants were given time to ask questions. All participants provided written informed consent.
Results
Table 1 describes the demographics and main clinical variables of our sample.
Table 1.
Description of demographics and main clinical variables of non-treatment-seeking gamblers (n = 143)
| Demographics | % (n) or mean (SD) |
| Age | 24.8 (±2.9) |
| Gender | |
| Male | 52.4 (75) |
| Female | 47.6 (68) |
| Marital status | |
| With partner | 79.7 (114) |
| Without partner | 20.3 (29) |
| Educational status | |
| Less than college | 53.8 (77) |
| College or more | 46.2 (66) |
| Occupational status | |
| Studying or working | 81.8 (117) |
| Unemployed | 18.2 (26) |
| Ethnicity | |
| Caucasian | 43.3 (61) |
| Non-Caucasian | 56.7 (80) |
| Sexual orientation | |
| Heterosexual | 83.9 (120) |
| Other | 16.1 (23) |
| Clinical variables | |
| Anxiety symptoms severity (Hamilton Anxiety Scale) | 6.1 (±6.3) |
| Age at the start of regular gambling | 18.9 (±3.0) |
| Money lost with gambling (last year) | 2,221 (±4,325) |
| Average gambling frequency (times per week) | 2.9 (±2.9) |
| Number of DSM-5 gambling disorder criteria | 2.0 (±2.6) |
| PG-YBOCS total score | 7.9 (±8.1) |
Note. SD, standard deviation; DSM-5, Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition; PG-YBOCS, gambling adaptation of the Yale-Brown Obsessive-Compulsive Scale.
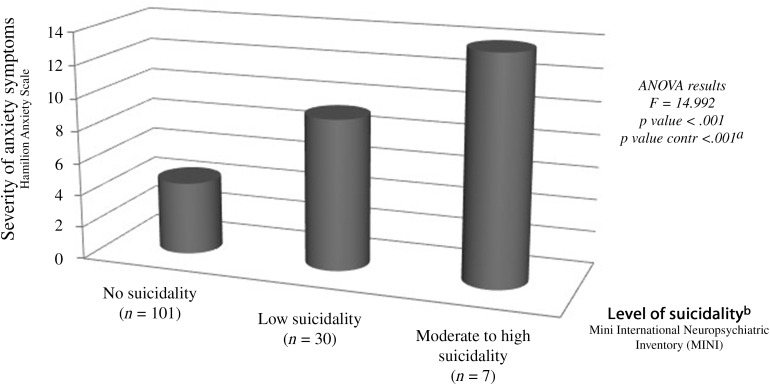
There was a significant positive correlation between the severity of anxiety symptoms and the number of current DSM-5 GD criteria. In addition, the quality of life was negatively correlated with the severity of anxiety symptoms. The presence of suicidality in gamblers was also associated with significantly higher scores on HAM-A, even after controlling for major depression, alcohol-use disorders, substance-use disorder, and use of nicotine (see also the findings using ANOVA, Figure 1). The analysis also showed a direct correlation between anxiety symptoms in gamblers and higher scores on the attentional impulsivity dimension of BIS (i.e., higher attentional impulsiveness) (see Table 2).
Figure 1.
Association between the severity of anxiety symptoms and the level of suicidality in non-treatment-seeking gamblers (n = 138). ap value controlled for major depressive disorder, alcohol-use disorder, substance-use disorder, and smoking. bThe level of suicidality was defined by the MINI-score that accesses the risk of suicide in the past month. Suicidality is considered low (scores between 1 and 8 points), moderate (scores between 9 and 16 points), and high (scores ≥ 17)
Table 2.
Association between clinical variables and anxiety levels in non-treatment-seeking gamblers (n = 143)
| Clinical variables | Spearman’s correlation coefficient or mean HAM-A (SD) | p valuea | Adjusted correlation coefficientb or effect size | Adjusted p valueb |
| Age started gambling regularly | −.170 | .043 | −.135 | .146 |
| Money lost with gambling (last year) | .222 | .008 | .122 | .186 |
| Average gambling frequency (times per week) | .110 | .192 | .048 | .604 |
| Number of DSM-5 gambling disorder criteria | .374 | <.001 | .363 | <.001 |
| PG-YBOCS total score | .345 | <.001 | .213 | .019 |
| PG-YBOCS urges subscale | .341 | <.001 | .183 | .046 |
| PG-YBOCS gambling behavior subscale | .307 | <.001 | .229 | .012 |
| Barratt Impulsiveness Scale | ||||
| Attentional | .328 | <.001 | .290 | .001 |
| Motor | .250 | .003 | .198 | .032 |
| Lack of planning | .236 | .005 | .088 | .344 |
| Legal problems due to gambling (yes/no) | 2.5 (±2.1)/6.2 (±6.4) | .437 | −.036 | .439 |
| Suicidality in the past month (yes/no) | 10.1 (±7.2)/4.5 (±5.2) | <.001 | .040 | <.001 |
| Quality of life (quality of life inventory) | −.343 | <.001 | −.292 | .001 |
Note. HAM-A, Hamilton Anxiety Scale; SD, standard deviation; DSM-5, Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition; PG-YBOCS, gambling adaptation of the Yale-Brown Obsessive-Compulsive Scale.
Significance was defined as p ≤ .004 (.05/13 = .004) for clinical variables.
Adjusted for current major-depressive, alcohol-use disorder, substance-use disorder, and nicotine use.
We did not find significant correlations between neurocognitive variables and anxiety symptoms (see Table 3).
Table 3.
Association between neurocognitive variables and anxiety level in non-treatment-seeking gamblers (n = 143)
| Neurocognitive variables | Spearman’s correlation coefficient | p valuea | Adjusted correlation coefficientb | Adjusted p valueb |
| Response inhibition (delay at the stop-signal test)c | .051 | .546 | .047 | .617 |
| Decision making (Cambridge gamble task) | ||||
| Quality of decision making | −.093 | .273 | −.109 | .243 |
| Overall proportion bet | .124 | .141 | .128 | .172 |
| Risk adjustment | −.131 | .120 | −.169 | .070 |
| Cognitive flexibility (intra–extra-dimensional set shifting test) | .170 | .044 | .158 | .091 |
| Sustained attention (rapid visual information processing) | −.235 | .005 | −.153 | .101 |
| Executive functioning (one touch stockings of Cambridge) | −.209 | .014 | −.102 | .274 |
Significance was defined as p ≤ .007 (.05/7 = .007) for neurocognitive variables.
Adjusted for current major-depressive, alcohol-use disorder, substance-use disorder, and nicotine use.
The following measures were used: [delay at stop-signal test] = stop-signal reaction time (ms); [intra–extra dimensional set shifting test] = total errors (adjusted); [rapid visual information processing] = proportion of targets detected; [one touch stockings of Cambridge] = problems solved in minimum possible number of moves.
Discussion and Conclusions
This study analyzed the association of anxiety symptoms, gambling clinical variables, and neurocognitive variables in non-treatment-seeking gamblers. We evaluated subjects with a wide range of gambling severity (individuals who meet 0–9 DSM-5 GD criteria) and with different levels of anxiety (HAM-A scores from 0 to 28). The use of a non-treatment-seeking sample was important to achieve this spread of disease severities, to maximize the ability to detect the relationships between variables. Treatment-seeking gamblers tend to be more severe than gamblers in the general population (Petry et al., 2005) and therefore, the range of different levels of gambling activity is narrower in treatment-seeking samples. In addition, treatment-seeking gamblers may present a significant selection bias. Therefore, the use of a non-treatment-seeking sample enabled us to assess the association between anxiety, gambling, and neurocognition throughout a broad spectrum of gambling and anxiety levels.
This study found that the severity of anxiety symptoms was associated with several important clinical variables, even when controlling for major depression, alcohol-use disorder, substance-use disorder, and use of nicotine. There was a positive correlation between anxiety and gambling severities measured by the number of DSM-5 GD criteria met. There was also a positive correlation between anxiety severity and attentional impulsiveness. Participants with suicidality presented with higher levels of anxiety. Finally, the severity of anxiety symptoms was negatively correlated with the quality of life.
The number of DSM-5 criteria endorsed showed a positive correlation with anxiety levels. There was no significant correlation, however, between gambling severity, as measured by PG-YBOCS, and anxiety. The DSM-5 criteria assess the symptoms over the past year, whereas the PG-YBOCS was designed to evaluate severity during the past 7 days. Given that the anxiety is often a chronic condition; the DSM-5 criteria may more accurately capture the impact of these symptoms on gambling behavior.
A large epidemiological study suggested that anxiety disorders usually precede GD and appear to trigger gambling problems (Kessler et al., 2008). The longitudinal relationship between anxiety symptoms and gambling activity, after gambling has started, remains unclear. In this context, important questions remain: do gamblers have a more harmful gambling activity due to higher anxiety levels? Or, does having severe gambling problems and, therefore more negative consequences, make gamblers feel more anxious? Future longitudinal studies should address this point.
The finding that anxiety levels were positively correlated with gambling severity is clinically important, and proper management of anxiety may improve treatment outcomes in gambling problems. Psychological therapies should address anxiety while identifying the reasons for gambling or for worsening of bets. Relaxation techniques and alternative ways to deal with anxiety (other than gambling) might be useful. Pharmacological approaches, such as the use of selective serotonin re-uptake inhibitors, may also enhance the control of anxiety. Grant and Potenza (2006) found that the use of escitalopram in a sample of disordered gamblers with co-occurring anxiety significantly improved gambling and anxiety symptoms. Future clinical trials looking specifically at anxious gamblers are needed.
This study observed a positive correlation between attentional impulsiveness as indexed by the Barratt questionnaire, and severity of anxiety symptoms; and between worse sustained attention on a computerized task, and severity of anxiety symptoms. Attentional impulsiveness has been described as an inability to keep attention/concentration (Stanford et al., 2009). When the BIS was first developed, attentional impulsiveness was believed to be an isolated dimension together with motor impulsiveness and lack of planning (Barratt, 1959). Later research suggested that it is an underlying construct that interacts with motor impulsiveness and lack of planning (Patton & Stanford, 1995). Therefore, attentional impulsiveness may be considered as a dimension that is correlated with impulsiveness in several levels (Patton & Stanford, 1995).
Attentional bias is a well-characterized phenomenon in anxious individuals, who preferably allocate attention/focus on threatening stimuli rather than on neutral stimuli (Bar-Haim et al., 2007; MacLeod et al., 1986; Mogg & Bradley, 1998). This attentional bias to threat also leads to slower disengagement from threatening elements and, as a result of this, other non-threatening elements tend to be less perceived (Bishop et al., 2004; Koster et al., 2004, 2006; Schofield et al., 2012). Therefore, an anxious individual who gambles may have a reduced focus on the gambling behavior (i.e., how to bet and how much to bet). Future studies might further investigate how the attentional bias interferes in gambling activity and could, particularly, look at possible threatening stimuli that are over-perceived during gambling behavior.
This study also observed that the severity of anxiety symptoms was positively associated with the presence of suicidality (Figure 1).
This is an important finding for several reasons. First, suicide has a huge economic impact in the United States. For example, in 2010, the financial losses associated with suicide were estimated at 44 billion US dollars/year (American Foundation for Suicide Prevention, 2010). Second, suicide is a top 2 leading cause of death in the United States for subjects aged 15–34 years (Centers for Disease Control and Prevention, 2011), the population evaluated by this study. Third, GD and subsyndromal GD have been associated with higher rates of suicide ideation/attempts (Bland et al., 1993; Hodgins, Mansley, & Thygesen, 2006; Newman & Thompson, 2007). Therefore, young gamblers appear to have a substantially elevated risk for suicide (age + gambling activity).
Unlike this research, the majority of previous studies that assessed suicide/risk of suicide in gamblers did not report a significant correlation between anxiety and suicidality. Two facts may explain this as follows: (a) some studies failed to assess the relationship between anxiety symptoms/anxiety disorders and suicide (see Hodgins et al., 2006) and (b) this study evaluated only young adults (aged 18–29 years), a group with higher anxiety symptoms, and higher suicidality (Centers for Disease Control and Prevention, 2011; Martin, 2003). Therefore, anxiety symptoms may present a higher impact on suicidality in young gamblers and we evaluated a broad spectrum of gambling activity.
In fact, Grant et al. (2014) used a subsyndromal GD sample and found an association between suicidality and anxiety disorders. However, the assessment of suicidality did not control for other mental disorders as this study did. As the correlation between GD and suicide ideation/attempts has been strongly attributed to co-occurring major depressive disorder and alcohol-/substance-use disorders (Crockford & el-Guebaly, 1998; Hodgins et al., 2006), our study strengthens the possible separate association of anxiety symptoms and suicidality in gamblers.
A meta-analysis of 42 studies conducted by Kanwar et al. (2013) suggested that anxiety disorders are associated with higher suicidality (Kanwar et al., 2013). Better assessment of anxiety symptoms, particularly in gamblers with suicidality seems to be important in clinical practice. As anxiety symptoms/disorders are considered relatively treatable (Hofmann & Smits, 2008), a more focused management in anxious gamblers may possibly reduce suicide risk.
Our study found that severity of anxiety was negatively correlated with the quality of life. This finding is consistent with previous epidemiological and clinical studies that have shown that anxiety disorders and subthreshold forms of anxiety disorders are associated with significantly reduced quality of life (Kessler et al., 1994; Markowitz, Weissman, Ouellette, Lish, & Klerman, 1989; Mendlowicz & Stein, 2014; Spitzer et al., 1995; Weissman, 1991; Wittchen, 2002; Wittchen, Carter, Pfister, Montgomery, & Kessler, 2000; Zatzick et al., 2014). On the other hand, subsyndromal GD and GD have also been associated with poorer life satisfaction when compared with the general population (Black, Moyer, & Schlosser, 2003; Grant & Kim, 2005). Therefore, this study reinforces the negative correlation between anxiety and decreased quality of life in a non-treatment-seeking sample of impulsive patients.
Quality of life is a core dimension in psychiatry treatments and, as a result of this, this variable has been increasingly recognized as a main outcome measure in clinical trials (Group for the Advancement of Psychiatry Committee on Psychopathology, 1994; Johnson & Temple, 1985; Pietersma, de Vries, & van den Akker-van, 2014; Spitzer et al., 1995; Wilson & Cleary, 1995). Anxiety may selectively affect some areas of quality of life. Spitzer et al. suggested that patients with anxiety disorders presented decreased scores particularly in role functioning. Further research should look at the effects of anxiety in specific dimensions. Cognitive-behavioral therapy focusing on training of social skills may benefit anxious gambling individuals.
This study should be interpreted in light of its limitations. First, this research used a cross-sectional analysis and, therefore, causal relationships cannot be confirmed. However, the analysis provides reliable measures of association. Second, some of the data collected (age at the start of recreational gambling and money lost with gambling in the last year) may be subject to potential recall bias, as it was collected in hindsight. Third, our sample consisted of a convenience sample of young adults (individuals aged 18–29 years). Therefore, caution is needed when generalizing our findings to broader segments of the population. Finally, our study used a low significance level [i.e., .004 for (clinical variables) and .007 for (neurocognitive variables)]. Therefore, we increased the likelihood of committing Type II error. On the other hand, we reduced the risk of finding false-positive results.
This study suggests that anxiety may be associated with relevant clinical variables in the broad spectrum of gambling activity. Therefore, proper management of anxiety symptoms might improve the clinical presentation of gamblers in different areas: (a) reducing the overall gambling severity; (b) improving the attentional deficits and attempting to reduce attentional impulsiveness; (c) reducing the risk/severity of suicidality; and (d) improving the quality of life.
Authors’ contribution
We confirm that all persons designated as authors qualified for authorship. Each author participated sufficiently in the work to take public responsibility for the content. The corresponding author affirms that he had access to all data from the study, both what is reported and what is unreported, and also that he had complete freedom to direct its analysis and its reporting, without influence from the sponsors. The corresponding author also affirms that there was no editorial direction or censorship from the sponsors. GCM conducted the literature searches, the statistical analysis, and wrote the first draft of the manuscript. DGS performed the literature searches and wrote the first draft of the manuscript. EWL and SRC wrote the protocol and made edits and amendments to the first draft of the manuscript. JEG designed the study, wrote the protocol, supervised the literature searches and statistical analysis, and reviewed the final version of this paper. All authors contributed to and have approved the final manuscript.
Conflict of interest
GCM, DGS, and EWL have no conflict of interest to report. SRC consults for Cambridge Cognition. His involvement in this research was supported by a grant from the Academy of Medical Sciences (AMS, UK). JEG has received research grants from National Center for Responsible Gaming, American Foundation for Suicide Prevention, Brainsway, and Forest, Takeda, and Psyadon Pharmaceuticals. He receives yearly compensation from Springer Publishing for acting as Editor-in-Chief of the Journal of Gambling Studies and has received royalties from Oxford University Press, American Psychiatric Publishing, Inc., Norton Press, McGraw Hill, and Johns Hopkins University Press.
Funding Statement
Funding sources: This study was funded by the National Center for Responsible Gaming (specific grant type: Center of Excellence grant).
References
- American Foundation for Suicide Prevention. (2010). Facts and figures. Available from https://www.afsp.org/understanding-suicide/facts-and-figures
- Bar-Haim Y., Lamy D., Pergamin L., Bakermans-Kranenburg M. J., Van Ijzendoorn M. H. (2007). Threat-related attentional bias in anxious and non-anxious individuals: A meta-analytic study. Psychological Bulletin, 133(1), 1–24. doi:10.1037/0033-2909.133.1.1 [DOI] [PubMed] [Google Scholar]
- Barratt E. S. (1959). Anxiety and impulsiveness related to psychomotor efficiency. Perceptual and Motor Skills, 9(3), 191–198. doi:10.2466/pms.1959.9.3.191 [Google Scholar]
- Beck A. T., Steer R. A. (1991). Relationship between the Beck Anxiety Inventory and the Hamilton Anxiety Rating Scale with anxious outpatients. Journal of Anxiety Disorders, 5(3), 213–223. doi:10.1016/0887-6185(91)90002-B [Google Scholar]
- Bishop S., Duncan J., Brett M., Lawrence A. D. (2004). Prefrontal cortical function and anxiety: Controlling attention to threat-related stimuli. Nature Neuroscience, 7(2), 184–188. doi:10.1038/nn1173 [DOI] [PubMed] [Google Scholar]
- Black D. W., Moyer T. (1998). Clinical features and psychiatric comorbidity of subjects with pathological gambling behavior. Psychiatric Services, 49, 1434–1439. doi:10.1176/ps.49.11.1434 [DOI] [PubMed] [Google Scholar]
- Black D. W., Moyer T., Schlosser S. (2003). Quality of life and family history in pathological gambling. The Journal of Nervous and Mental Disease, 191(2), 124–126. doi: 10.1097/00005053-200302000-00011 [DOI] [PubMed] [Google Scholar]
- Bland R. C., Newman S. C., Orn H., Stebelsky G. (1993). Epidemiology of pathological gambling in Edmonton. Canadian Journal of Psychiatry, 38(2), 108–112. [DOI] [PubMed] [Google Scholar]
- Cambridge Cognition. (2015). Executive function test (CANTAB batteries). Available from http://www.cambridgecognition.com/academic/cantabsuite/executive-function-tests
- Centers for Disease Control and Prevention (CDC). (2011). Web-based Injury Statistics Query and Reporting System [WISQARS]. National Center for Injury Prevention and Control, CDC (producer).
- Clark L. (2010). Decision-making during gambling: An integration of cognitive and psychobiological approaches. Philosophical Transactions of the Royal Society B: Biological Sciences, 365(1538), 319–330. doi:10.1098/rstb.2009.0147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crockford D. N., el-Guebaly N. (1998). Psychiatric comorbidity in pathological gambling: A critical review. Canadian Journal of Psychiatry, 43(1), 43–50. doi: 10.1177/070674379804300104 [DOI] [PubMed] [Google Scholar]
- Cunningham-Williams R. M., Cottler L. B., Compton W. M., III, Spitznagel E. L. (1998). Taking chances: Problem gamblers and mental health disorders – Results from the St. Louis Epidemiologic Catchment Area Study. American Journal of Public Health, 88, 1093–1096. doi:10.2105/AJPH.88.7.1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deakin J., Aitken M., Robbins T., Sahakian B. J. (2004). Risk taking during decision-making in normal volunteers changes with age. Journal of the International Neuropsychological Society, 10(4), 590–598. doi:10.1017/S1355617704104104 [DOI] [PubMed] [Google Scholar]
- Desai R. A. (2004). Older adults. In Pathological gambling: A clinical guide to treatment (pp. 83–96). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Desai R. A., Potenza M. N. (2008). Gender differences in the associations between past-year gambling problems and psychiatric disorders. Social Psychiatry and Psychiatric Epidemiology, 43(3), 173–183. doi:10.1007/s00127-007-0283-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen S. A., Slutske W. S., Lyons M. J., Lassman J., Xian H., Toomey R. E. E. A., Chantarujikapong S., Tsuang M. T. (2001). The genetics of pathological gambling. Seminars in Clinical Neuropsychiatry, 6(3), 195–204. doi:10.1053/scnp.2001.22931 [DOI] [PubMed] [Google Scholar]
- Frisch M. B. (1994). QOLI: Quality of life inventory: Manual and treatment guide. New York, NY: Pearson. [Google Scholar]
- Gerstein D., Murphy S., Toce M., Hoffmann J., Palmer A., Johnson R., Larison C., Chuchro L., Bard A., Engelman L., Hill M. A., Buie T., Volberg R., Harwood H., Tucker A., Christiansen E., Cummings W., Sinclair S. (1999). Gambling impact and behavior study. Chicago, IL: National Opinion Research Center, University of Chicago. [Google Scholar]
- Grall-Bronnec M., Wainstein L., Feuillet F., Bouju G., Rocher B., Vénisse J. L., Sébille-Rivain V. (2012). Clinical profiles as a function of level and type of impulsivity in a sample group of at-risk and pathological gamblers seeking treatment. Journal of Gambling Studies, 28(2), 239–252. doi:10.1007/s10899-011-9258-9 [DOI] [PubMed] [Google Scholar]
- Granero R., Fernández-Aranda F., Aymamí N., Gómez-Peña M., Fagundo A. B., Sauchelli S., Del Pino-Gutiérrez A., Moragas L., Savvidou L. G., Islam M. A., Tàrrega S., Menchón J. M., Jiménez-Murcia S. (2015). Subtypes of pathological gambling with concurrent illegal behaviors. Journal of Gambling Studies, 31, 1161–1178. doi:10.1007/s10899-014-9499-5 [DOI] [PubMed] [Google Scholar]
- Grant J. E., Derbyshire K., Leppink E., Chamberlain S. R. (2014). Suicidality in non-treatment seeking young adults with subsyndromal gambling disorder. Psychiatric Quarterly, 85(4), 513–522. doi:10.1007/s11126-014-9312-8 [DOI] [PubMed] [Google Scholar]
- Grant J. E., Kim S. W. (2005). Quality of life in kleptomania and pathological gambling. Comprehensive Psychiatry, 46(1), 34–37. doi:10.1016/j.comppsych.2004.07.022 [DOI] [PubMed] [Google Scholar]
- Grant J. E., Potenza M. N. (2006). Escitalopram treatment of pathological gambling with co-occurring anxiety: An open-label pilot study with double-blind discontinuation. International Clinical Psychopharmacology, 21(4), 203–209. doi:10.1097/00004850-200607000-00002 [DOI] [PubMed] [Google Scholar]
- Grant J. E., Steinberg M. A., Kim S. W., Rounsaville B. J., Potenza M. N. (2004). Preliminary validity and reliability testing of a structured clinical interview for pathological gambling. Psychiatry Research, 128(1), 79–88. doi:10.1016/j.psychres.2004.05.006 [DOI] [PubMed] [Google Scholar]
- Group for the Advancement of Psychiatry Committee on Psychopathology. (1994). Taking issue: Outcomes assessment and psychiatric services (editorial). Psychiatric Services, 45, 1165–1165. doi:10.1176/ps.45.12.1165 [PubMed] [Google Scholar]
- Hamilton M. (1969). Diagnosis and rating of anxiety. British Journal of Psychiatry, 3(Special issue), 76–79. [Google Scholar]
- Hodgins D. C., Mansley C., Thygesen K. (2006). Risk factors for suicide ideation and attempts among pathological gamblers. American Journal on Addictions, 15(4), 303–310. doi:10.1080/10550490600754366 [DOI] [PubMed] [Google Scholar]
- Hofmann S. G., Smits J. A. (2008). Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. The Journal of Clinical Psychiatry, 69(4), 621–632. doi:10.4088/JCP.v69n0415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson J. R., Temple R. (1985). Food and Drug Administration requirements for approval of new anticancer drugs. Cancer Treatment Reports, 69(10), 1155–1159. [PubMed] [Google Scholar]
- Kanwar A., Malik S., Prokop L. J., Sim L. A., Feldstein D., Wang Z., Murad M. H. (2013). The association between anxiety disorders and suicidal behaviors: A systematic review and meta‐analysis. Depression and Anxiety, 30(10), 917–929. doi: 10.1002/da.22074 [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Hwang I., LaBrie R., Petukhova M., Sampson N. A., Winters K. C., Shaffer H. J. (2008). DSM-IV pathological gambling in the National Comorbidity Survey replication. Psychological Medicine, 38(9), 1351–1360. doi:10.1017/S0033291708002900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. C., McGonagle K. A., Zhao S., Nelson C. B., Hughes M., Eshleman S., Wittchen H. U., Kendler K. S. (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Archives of General Psychiatry, 51(1), 8–19. doi:10.1001/archpsyc.1994.03950010008002 [DOI] [PubMed] [Google Scholar]
- Koster E. H., Crombez G., Van Damme S., Verschuere B., De Houwer J. (2004). Does imminent threat capture and hold attention? Emotion, 4(3), 312–317. doi:10.1037/1528-3542.4.3.312 [DOI] [PubMed] [Google Scholar]
- Koster E. H., Crombez G., Verschuere B., Van Damme S., Wiersema J. R. (2006). Components of attentional bias to threat in high trait anxiety: Facilitated engagement, impaired disengagement, and attentional avoidance. Behaviour Research and Therapy, 44(12), 1757–1771. doi:10.1016/j.brat.2005.12.011 [DOI] [PubMed] [Google Scholar]
- Kummer A., Cardoso F., Teixeira A. L. (2010). Generalized anxiety disorder and the Hamilton Anxiety Rating Scale in Parkinson’s disease. Arquivos de Neuro-Psiquiatria, 68(4), 495–501. doi:10.1590/S0004-282X2010000400005 [DOI] [PubMed] [Google Scholar]
- Lawrence A. J., Luty J., Bogdan N. A., Sahakian B. J., Clark L. (2009). Problem gamblers share deficits in impulsive decision‐making with alcohol‐dependent individuals. Addiction, 104(6), 1006–1015. doi:10.1111/add.2009.104.issue-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorains F. K., Cowlishaw S., Thomas S. A. (2011). Prevalence of comorbid disorders in problem and pathological gambling: Systematic review and meta‐analysis of population surveys. Addiction, 106(3), 490–498. doi:10.1111/add.2011.106.issue-3 [DOI] [PubMed] [Google Scholar]
- MacLeod C., Mathews A., Tata P. (1986). Attentional bias in emotional disorders. Journal of Abnormal Psychology, 95(1), 15–20. doi:10.1037/0021-843X.95.1.15 [DOI] [PubMed] [Google Scholar]
- Maier W., Buller R., Philipp M., Heuser I. (1988). The Hamilton Anxiety Scale: Reliability, validity and sensitivity to change in anxiety and depressive disorders. Journal of Affective Disorders, 14(1), 61–68. doi:10.1016/0165-0327(88)90072-9 [DOI] [PubMed] [Google Scholar]
- Markowitz J. S., Weissman M. M., Ouellette R., Lish J. D., Klerman G. L. (1989). Quality of life in panic disorder. Archives of General Psychiatry, 46(11), 984–992. doi:10.1001/archpsyc.1989.01810110026004 [DOI] [PubMed] [Google Scholar]
- Martin P. (2003). The epidemiology of anxiety disorders: A review. Dialogues in Clinical Neuroscience, 5(3), 281–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendlowicz M. V., Stein M. B. (2000). Quality of life in individuals with anxiety disorders. American Journal of Psychiatry, 157(5), 669–682. [DOI] [PubMed] [Google Scholar]
- Mogg K., Bradley B. P. (1998). A cognitive-motivational analysis of anxiety. Behaviour Research and Therapy, 36(9), 809–848. doi:10.1016/S0005-7967(98)00063-1 [DOI] [PubMed] [Google Scholar]
- Morein-Zamir S., Sahakian B. J. (2010). Stop-signal task. In Encyclopedia of psychopharmacology (p. 1285). Berlin, Heidelberg: Springer. [Google Scholar]
- Muelleman R. L., DenOtter T., Wadman M. C., Tran T. P., Anderson J. (2002). Problem gambling in the partner of the emergency department patient as a risk factor for intimate partner violence. The Journal of Emergency Medicine, 23(3), 307–312. doi:10.1016/S0736-4679(02)00543-7 [DOI] [PubMed] [Google Scholar]
- National Gambling Impact Study Commission, & James K. C. (1999). National gambling impact study commission final report. Washington, D.C.: The Commission. [Google Scholar]
- Newman S. C., Thompson A. H. (2007). The association between pathological gambling and attempted suicide: Findings from a national survey in Canada. Canadian Journal of Psychiatry, 52(9), 605–612. doi: 10.1177/070674370705200909 [DOI] [PubMed] [Google Scholar]
- Owen A. M., Sahakian B. J., Hodges J. R., Summers B. A., Polkey C. E., Robbins T. W. (1995). Dopamine-dependent frontostriatal planning deficits in early Parkinson’s disease. Neuropsychology, 9(1), 126–140. doi:10.1037/0894-4105.9.1.126 [Google Scholar]
- Pallanti S., DeCaria C. M., Grant J. E., Urpe M., Hollander E. (2005). Reliability and validity of the pathological gambling adaptation of the Yale-Brown Obsessive-Compulsive Scale (PG-YBOCS). Journal of Gambling Studies, 21(4), 431–443. doi:10.1007/s10899-005-5557-3 [DOI] [PubMed] [Google Scholar]
- Patton J. H., Stanford M. S. (1995). Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology, 51(6), 768–774. doi:10.1002/(ISSN)1097-4679 [DOI] [PubMed] [Google Scholar]
- Petry N. M., Kiluk B. D. (2002). Suicidal ideation and suicide attempts in treatment-seeking pathological gamblers. The Journal of Nervous and Mental Disease, 190(7), 462–469. doi:10.1097/00005053-200207000-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry N. M., Stinson F. S., Grant B. F. (2005). Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: Results from the National Epidemiologic Survey on alcohol and related conditions. Journal of Clinical Psychiatry, 66(5), 564–574. [DOI] [PubMed] [Google Scholar]
- Pietersma S., de Vries M., van den Akker-van M. E. (2014). Domains of quality of life: Results of a three-stage Delphi consensus procedure among patients, family of patients, clinicians, scientists and the general public. Quality of Life Research, 23(5), 1543–1556. doi: 10.1007/s11136-013-0578-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potenza M. N., Maciejewski P. K., Mazure C. M. (2006). A gender-based examination of past-year recreational gamblers. Journal of Gambling Studies, 22(1), 41–64. doi:10.1007/s10899-005-9002-4 [DOI] [PubMed] [Google Scholar]
- Sarter M., Givens B., Bruno J. P. (2001). The cognitive neuroscience of sustained attention: Where top-down meets bottom-up. Brain Research Reviews, 35(2), 146–160. doi:10.1016/S0165-0173(01)00044-3 [DOI] [PubMed] [Google Scholar]
- Schofield C. A., Johnson A. L., Inhoff A. W., Coles M. E. (2012). Social anxiety and difficulty disengaging threat: Evidence from eye-tracking. Cognition & Emotion, 26(2), 300–311. doi:10.1080/02699931.2011.602050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer H. J., Hall M. N., Vander Bilt J. (1999). Estimating the prevalence of disordered gambling behavior in the United States and Canada: A research synthesis. American Journal of Public Health, 89(9), 1369–1376. doi:10.2105/AJPH.89.9.1369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer H. J., Korn D. A. (2002). Gambling and related mental disorders: A public health analysis. Annual Review of Public Health, 23(1), 171–212. doi:10.1146/annurev.publhealth.23.100901.140532 [DOI] [PubMed] [Google Scholar]
- Sheehan D. V., Lecrubier Y., Sheehan K. H., Amorim P., Janavs J., Weiller E., Hergueta T., Baker R., Dunbar G. C. (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(Suppl 20), 22–33. [PubMed] [Google Scholar]
- Sher K. J., Trull T. J., Bartholow B. D., Vieth A. (1999). Personality and alcoholism: Issues, methods, and etiological processes. In Leonard K. E., Blane H. T. (Eds.), Psychological theories of drinking and alcoholism (2nd ed., pp. 54–105). New York, NY: Guilford. [Google Scholar]
- Slutske W. S., Eisen S., True W. R., Lyons M. J., Goldberg J., Tsuang M. (2000). Common genetic vulnerability for pathological gambling and alcohol dependence in men. Archives of General Psychiatry, 57(7), 666–673. doi:10.1001/archpsyc.57.7.666 [DOI] [PubMed] [Google Scholar]
- Snaith R. P., Baugh S. J., Clayden A. D., Husain A., Sipple M. A. (1982). The Clinical Anxiety Scale: An instrument derived from the Hamilton Anxiety Scale. The British Journal of Psychiatry, 141, 518–523. [DOI] [PubMed] [Google Scholar]
- Spitzer R. L., Kroenke K., Linzer M., Hahn S. R., Williams J. B., deGruy F. V., Brody D., Davies M. (1995). Health-related quality of life in primary care patients with mental disorders: Results from the PRIME-MD 1000 Study. JAMA, 274(19), 1511–1517. doi:10.1001/jama.1995.03530190025030 [PubMed] [Google Scholar]
- Stanford M. S., Mathias C. W., Dougherty D. M., Lake S. L., Anderson N. E., Patton J. H. (2009). Fifty years of the Barratt Impulsiveness Scale: An update and review. Personality and Individual Differences, 47(5), 385–395. doi:10.1016/j.paid.2009.04.008 [Google Scholar]
- Steinberg L., Sharp C., Stanford M. S., Tharp A. T. (2013). New tricks for an old measure: The development of the Barratt Impulsiveness Scale-Brief (BIS-Brief). Psychological Assessment, 25(1), 216–226. doi:10.1037/a0030550 [DOI] [PubMed] [Google Scholar]
- Strong D. R., Kahler C. W. (2007). Evaluation of the continuum of gambling problems using the DSM‐IV. Addiction, 102(5), 713–721. doi:10.1111/add.2007.102.issue-5 [DOI] [PubMed] [Google Scholar]
- Toce-Gerstein M., Gerstein D. R., Volberg R. A. (2003). A hierarchy of gambling disorders in the community. Addiction, 98, 1661–1672. doi:10.1111/add.2003.98.issue-12 [DOI] [PubMed] [Google Scholar]
- van Holst R. J., van den Brink W., Veltman D. J., Goudriaan A. E. (2010). Why gamblers fail to win: A review of cognitive and neuroimaging findings in pathological gambling. Neuroscience & Biobehavioral Reviews, 34(1), 87–107. doi:10.1016/j.neubiorev.2009.07.007 [DOI] [PubMed] [Google Scholar]
- Weissman M. M. (1991). Panic disorder: Impact on quality of life. Journal of Clinical Psychiatry, 52, 6–9. [PubMed] [Google Scholar]
- Welte J., Barnes G., Wieczorek W., Tidwell M. C., Parker J. (2001). Alcohol and gambling pathology among US adults: Prevalence, demographic patterns and comorbidity. Journal of Studies on Alcohol, 62(5), 706–712. doi:10.15288/jsa.2001.62.706 [DOI] [PubMed] [Google Scholar]
- Wilson I. B., Cleary P. D. (1995). Linking clinical variables with health-related quality of life: A conceptual model of patient outcomes. JAMA, 273(1), 59–65. doi:10.1001/jama.1995.03520250075037 [PubMed] [Google Scholar]
- Wittchen H. U. (2002). Generalized anxiety disorder: Prevalence, burden, and cost to society. Depression and Anxiety, 16(4), 162–171. doi:10.1002/(ISSN)1520-6394 [DOI] [PubMed] [Google Scholar]
- Wittchen H. U., Carter R. M., Pfister H., Montgomery S. A., Kessler R. C. (2000). Disabilities and quality of life in pure and comorbid generalized anxiety disorder and major depression in a national survey. International Clinical Psychopharmacology, 15(6), 319–328. doi:10.1097/00004850-200015060-00002 [DOI] [PubMed] [Google Scholar]
- Zatzick D. F., Marmar C. R., Weiss D. S., Browner W. S., Metzler T. J., Golding J. M., Stewart A., Schlenger W. E., Wells K. B. (1997). Posttraumatic stress disorder and functioning and quality of life outcomes in a nationally representative sample of male Vietnam veterans. American Journal of Psychiatry, 154(12), 1690–1695. [DOI] [PubMed] [Google Scholar]