Abstract
Objectives:
To examine the associations between sleep duration and a variety of demographic and clinical variables in a sample of Saudi adults.
Methods:
A cross-sectional study among 2,095 participants was conducted at King Abdulaziz Medical City, Riyadh, Kingdom of Saudi Arabia, between May and October 2014. A questionnaire was administered to collect data related to clinical health outcomes and demographic characteristics. Participants were asked to report their average sleep duration per night in hours.
Results:
One-third (33.8%) reported short sleep duration of less than 7 hours/night. Short sleep duration was more prevalent in females (37.3% versus 31.4%, p=0.004). The most common medical problems reported were obesity with body mass index of >30 Kg/m2 (39.1%), hypertension (33.9%), diabetes mellitus (20.8%), depression (4.3%), asthma (17.3%), COPD (6.6%), and hyperlipidemia (2.7%). Diabetes mellitus was associated with long sleep of more than 9 hours/night (25.4%, p=0.011) and hypertension (54.2%, p=0.001). The linear regression model tend to reduce their sleep duration by roughly 22 minutes in female gender, 66 minutes in participants with hyperlipidemia, and 70 minutes in participants with poor sleep quality.
Conclusions:
Short sleep duration per night was prevalent, it affects one in every 3 Saudi adults. Long sleep duration of more than 9 hours was associated with increased comorbid conditions.
The recommended amount of sleep for healthy adults is between 7-8 hours per night in order to feel rested with optimal sleep quality.1-3 However, sleep deprivation and short sleep duration are very common. In the past decades, accumulating evidence has shown that quantity and duration of sleep are important factors associated with health and mortality.4-8 Irregular or sleep loss may be associated with an increased risk of morbidity and mortality.3,7-15 Studies reported that both shortened sleep (<7 hours per night) and long sleep duration (>8 hours per night) are associated with increased mortality and morbidity. According to several epidemiological studies, the risk of all-cause mortality occurs among individuals with long duration of sleep (≥8 hours sleep per day) and short durations of sleep (<7 hours sleep per day).13,16-22 However, few studies explore factors that predict an individual’s sleep duration per day. Furthermore, published studies corroborate that there is an association between sleep deprivation, short sleep duration, the chances of developing obesity,23-26 type 2 diabetes,18,27-29 hyperlipidemia,30-32 high blood pressure,33-36 motor vehicle accidents,37,38 and increased risk of dying of coronary artery disease.39-41 A study investigating the relationship between sleeping hours and adjusted injury risk revealed that the odds ratio (OR) for a worker sleeping a total of <5 hours/day was 2.65, 1.79 for 5-5.9 hours/day, 1.40 for 6-6.9 hours/day and 1.82 for >10 hours of usual daily sleep.37
Another study investigating the relationship between sleeping hours and self-related health (fair/poor) revealed the OR for sleeping a total of <5 hours/day was 2.29, 1.68 for 6 hours/day, 1.38 for 8 hours/day, and 1.98 for >9 hours of usual daily sleep.42 Older age, depression, anxiety, night or shift work, heavy smoking, and lower levels of income were associated with short sleep duration, while younger age, underweight, widowed, being divorced, heavy smoking, anxiety, depression, and poorer self-reported health were associated with long sleep duration.43 Studies also reported correlation between low socioeconomic status, depression, and long sleep duration.42-45 The epidemiological studies on sleep duration and its relation to comorbid conditions among different societies and cultures are limited. There are no studies on sleep duration and its relation to comorbid conditions among Saudi adults. This study proposed to investigate the relationship between several risk factors, morbidities, and sleep duration per night among the Saudi population. We also intended to develop a model to predict sleep duration, using a variety of demographic and clinical variables.
Methods
A cross-sectional study was conducted at King Abdulaziz Medical City-Riyadh (KAMC-R), Kingdom of Saudi Arabia, between January and July 2014. The study was approved by the King Abdullah International Medical Research Center (KAIMRC) Research Ethics Committee. The study sample was chosen from pre-employment clinics, blood bank donors, visitors to KAMC-R, and employees. We include all adults 18 years old or older who was willing to participate. In order to overcome possible sources of bias in this convenience sample, we excluded individuals with night-shift work, time-zone travel during the last 4 weeks, or use of any sleep medications. Three research assistants distributed the questionnaire after participants’ verbal agreement to participate in the study. Of the 2,500 people asked to participate in the study, 2,095 agreed to complete the questionnaire. These 2,095 participants (ages 18-100 years) were recruited from the study population (pre-employment clinics, blood bank donors, visitors to KAMC-R, and employees). The survey was assessed based on a self-administered questionnaire; research assistants reviewed the questionnaires for completeness. We used the validated Arabic version of the Berlin Questionnaire (BQ) to assess the presence of risk of obstructive sleep apnea (OSA) among participants.46,47 The BQ consisted of 10 items related to sleep apnea risk that include: snoring behavior, wake time, sleepiness or fatigue, history of obesity or hypertension, and body mass index (BMI).47 Participants were classified as having a high risk of OSA if there were 2 or more categories where the score was positive.47 We also used the Epworth Sleepiness Scale (ESS) Arabic version to assess excessive daytime sleepiness (EDS).48 A score of 11 or more (ESS ≥11) is considered EDS. We also used the International Classification of Sleep Disorders-2 (ICSD-2), which defines insomnia as difficulty in falling asleep, waking up too early, frequent awakening with difficulty in falling asleep again, and secondary daytime impairment related to nighttime sleep difficulties.49 The sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI).50 The PSQI version was translated and validated by Suleiman et al.51 The questionnaire included demographic characteristics such as age, gender, education, self-reported weight, and height. Participants were asked whether they smoked or consumed coffee or tea. The questionnaire included clarification on medical conditions based on history, including asthma, diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), hypertension, and depression. Self-reported sleep duration was collected from each respondent by asking to report the average sleep duration hours of sleep per night. Informed consent was obtained from all individual participants included in the study.
Statistical analysis
Statistical analyses were conducted using IBM SPSS® version 22 (Chicago, Illinois: SPSS Inc, USA). Self-report of sleep duration as measured by average hours of sleep per night was expressed as mean (±SD) with 25th and 75th percentiles. Differences in sleep duration across participants’ characteristics were tested using independent samples t-tests. Analysis of variance (ANOVA) test was used to test differences in BMI across 3 categories of sleep duration: short sleep (<7 hours), normative (7-9 hours), and long (>9 hours). Chi-square tests were used to examine associations between short/long sleep duration and demographic characteristics. Also, Chi-square tests were used to examine the associations between short/long sleep duration and the presence of comorbid medical conditions. The short sleep duration was based on American Academy of Sleep Medicine (AASM) parameters.30 We used stepwise linear regression to develop a model to predict sleep duration, using a variety of demographic and clinical variables. The following variables were entered in the model: age, gender, obesity, coffee intake, tea intake, smoke status, asthma, diabetes, chronic obstructive pulmonary, hypertension, depression, hyperlipidemia, quality of sleep, high risk of sleep apnea, difficulty falling asleep, frequent awakening, wake up too early, feel tired/fatigued, and change in mood because of sleep issues. We used multiple linear models to compare predictors of sleep duration in 2 predictive models according to age groups (<40 and ≥40 years). All statistical tests were 2-tailed and the level of significance was set at p=0.05.
Results
A total of 2,095 participants were included in the analysis. The age range was 18-100 years, with a mean age of 42.3±15.5 years.
Table 1 shows the sample characteristics. The sample consisted of 59.3% males, 17.1% elderly (>60 years), 72.1% coffee consumers, and 63.6% tea consumers. The most common medical problems reported were obesity (Table 1). On average, participants reported 6.4±1.7 hours sleep per night, 33.8% reported short sleep duration of less than 7 hours per night. As per the PSQI, the majority (78.3%) of the sample reported poor sleep quality. High risk for sleep apnea using the BQ was reported in 31.9%. Most participants reported trouble falling asleep, had frequent awakening, waking up too early, and felt tired during the day due to lack of sleep. Table 1 also showed differences in sleep duration across participants’ characteristics as tested using independent samples t-test (bivariate analyses). The average sleep duration decreased among participants with poor sleep quality as per PSQI score. Sleep duration was longer among participants who reported: difficulty falling asleep, frequent awakening, waking up too early, obesity, DM, HTN, and COPD. Sleep duration was shorter among participants with sleep loss affecting mood and participants with hyperlipidemia (Table 1).
Table 1.
Sleep duration by the sample characteristics.
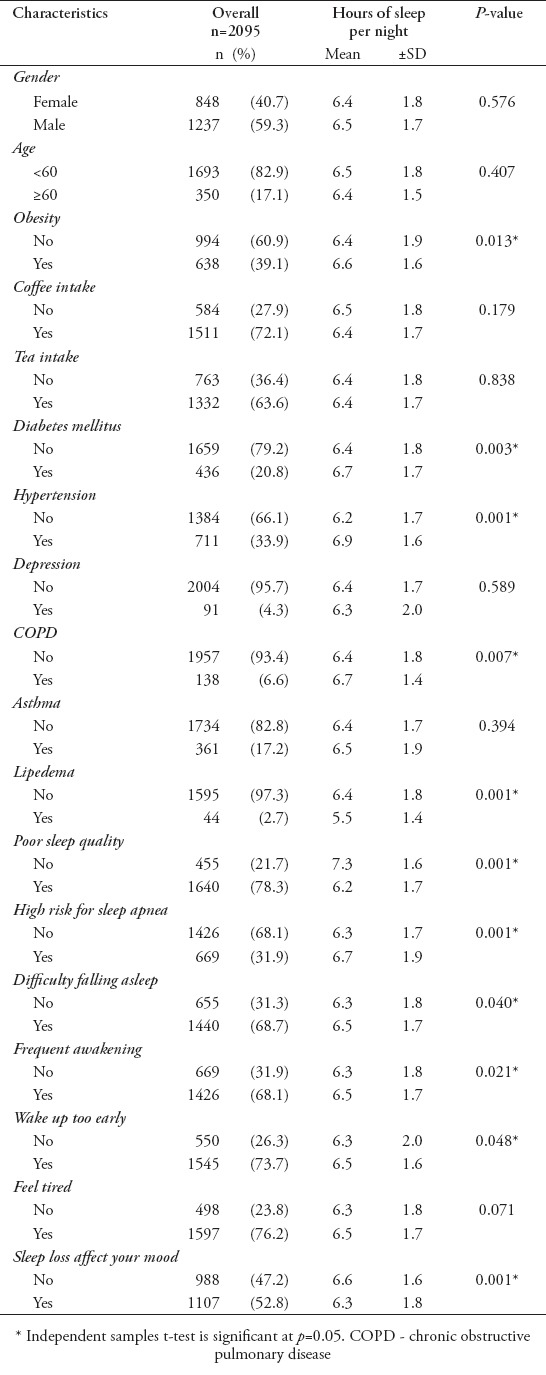
Table 2 shows the associations between sleep duration and demographic characteristics. The female gender had a higher percentage of short sleep duration than the male gender. The prevalence of short sleep duration was significantly higher among participants who consumed coffee than those who did not consume coffee.
Table 2.
Sleep duration and its relation to demographic characteristics.
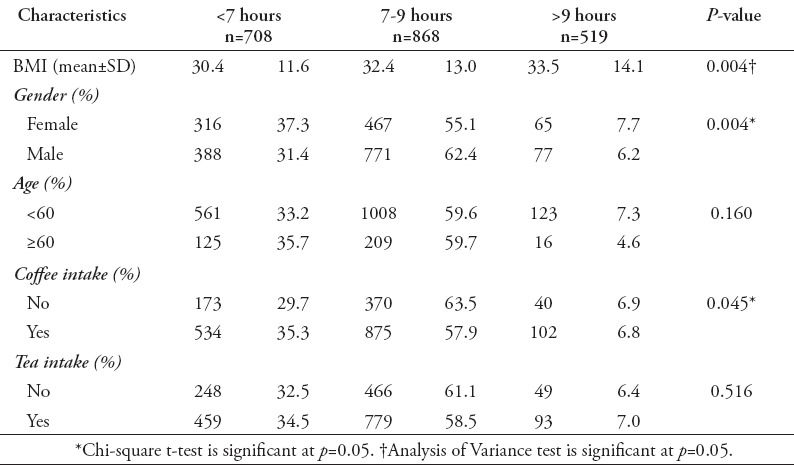
Table 3 illustrates short/long sleep duration and their association with comorbid conditions. Hyperlipidemia was more common in those with short sleep duration. Poor sleep quality was very prevalent in those with short sleep duration. Participants with sleep loss affects mood were significantly more likely to have short sleep duration. Diabetes mellitus was more common in participants with long sleep duration. Participants with hypertension were significantly more likely to have long sleep duration. Participants with high risk of sleep apnea tend to have a long sleep duration. Stepwise analysis (multivariate analysis) was used to build a multiple linear regression model to explain the variation in sleep duration among participants (Table 4). Controlling for all confounders, the analysis revealed that the sleep duration was predicted by the following characteristics: being female, poor sleep quality, COPD, hyperlipidemia, and HTN (p<0.05). The multiple correlation coefficient of this model was 0.32 with adjusted R square of 10%.
Table 3.
Short/long sleep duration and their association with sleep pattern and comorbid conditions
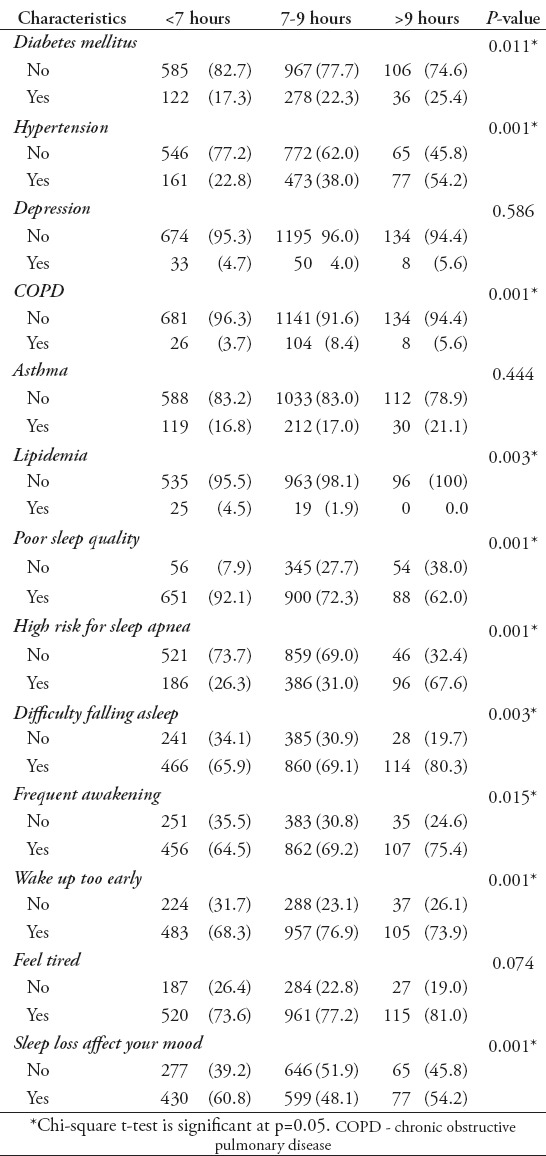
Table 4.
Stepwise analysis: predictors of sleep duration.
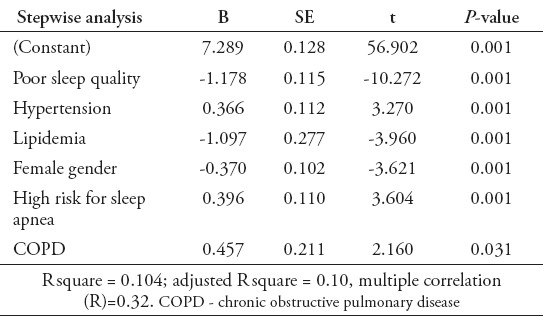
Table 5.
Predictive models of sleep duration by age groups.
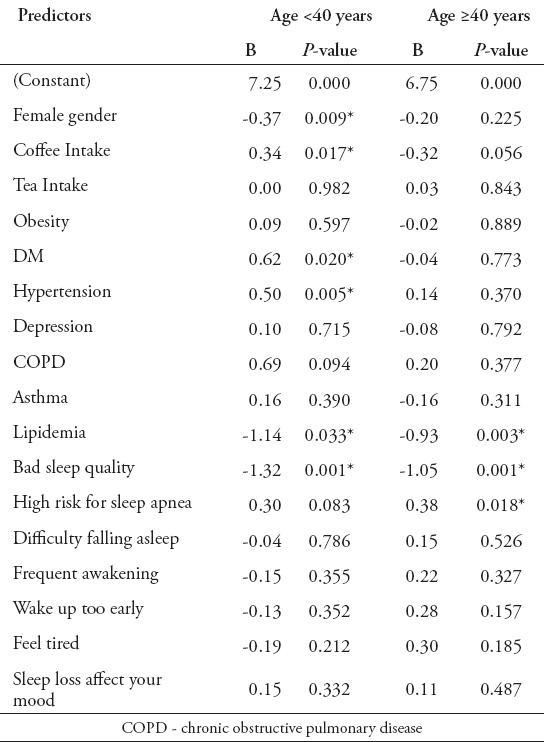
The following is the estimated equation: predicted sleep duration/hours = 7.289-0.370 × female - 1.178 x bad sleep quality + 0.396 × high risk for sleep apnea + 0.366 × hypertension - 1.097 lipidemia + 0.457 COPD. Controlling for the other 3 predictors, this model implies that the female gender, participants with hyperlipidemia, and participants with poor sleep quality tend to experience reduced sleep duration by roughly 22, 66, and 70 minutes, respectively. In contrast, controlling for being female, and having poor sleep quality and hyperlipidemia, the predicted sleep duration tends to increase by 22 in participants with HTN. Also, for participants with COPD the sleep duration was predicted to increase by 27 minutes and high risk of sleep apnea in 23 minutes. In young age group (<40 years), independent predictors for sleep duration were gender, coffee intake, DM, HTN, lipidemia, and bad sleep quality. However, in older age (≥40 years), sleep duration was significantly predicted by lipidemia, bad sleep quality, and high risk for sleep apnea. In the first model (young age group <40 years), the predictors explained 13.1% of the variation in sleep duration. The second model (older age group ≥40 years), the predictors explained 14.9% of the variation in sleep duration.
Discussion
The current study investigated the associations between short/long sleep duration and the presence of comorbid medical conditions in a sample of Saudi adults. In addition, this study also analyzed the factors that can be used to explain the variation in duration of sleep. A study conducted in northeast China reported an average sleep duration of 6.9±1.6 hours per night.24 Another study reported an average sleep duration of 6.5±1.7 hours.27 The self-reported mean of sleep duration in our sample was found to be 6.4±1.7 hours per night with a 25th percentile of 5 hours, a 75th percentile of 7.5 hours, and a median of 6 hours. Our study reported a high prevalence of short sleep duration <7 hours in one-third (33.8%), which is similar to many other reported studies (24.1%-41.6%).28,29 The USA general population reported sleep duration of less than 7 hours in approximately a third of the population.41 We found no studies on sleep duration among adults in our Saudi population. Most studies regarding sleep habits and duration were conducted among children, adolescents, and medical students. Al-Hazzaa et al26 reported short sleep duration (<7 hours) in approximately 31% of 15 to 19 year-old in Saudi Arabia with no difference in sleep duration between males and females. Recent studies have shown that sleep duration is associated with HTN.15 The relationship between HTN and sleep duration has also been discussed in our research. Our findings are similar to other studies that found sleep duration is associated with HTN,52 obesity,53 hyperlipidemia,31 and DM.54 We noted that 24.8% of our population reported long sleep hours. This could be due to some other considerations, such as BMI, HTN, and DM, all of which have shown association with long sleep duration. Although our study shows sleep duration was associated with increased BMI (Figure 1), both factors may be related to sleep breathing disorders. Longitudinal studies are needed to investigate the effect of sleep duration on clinical management of diabetes, obesity, and hypertension.
Figure 1.
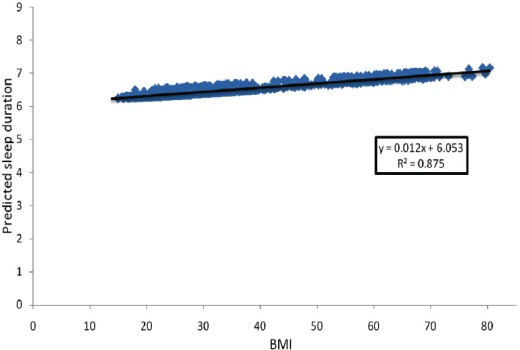
Relationship between body mass index (BMI) and predicted sleep duration, adjusted for age and gender.
Study limitations
The measurement of sleep duration similar to many other studies relied upon self-report, which may not be accurate,55,56 and we did not assess all other confounders such as work or home environments, shift work, sleep patterns in working days and weekends, and cognitive function of participants. Also, chronic disease was based on information provided by the patients and could not be confirmed. Although our sample is large and may present a wide spectrum of the Saudi population, the results cannot be generalized to the entire Saudi population as it merely represents one facility’s experience. This is a cross-sectional study, and therefore we examined the correlations, not causations. Possible sources of sampling bias might exist in this convenience sample as visitors to the hospital may have short sleep duration if a close family member is ill. In order to overcome this limitation, we included a relatively large sample size. Despite these limitations, this study represents one of the few explorations into predictive factors for sleep duration in Saudi adults, and considers both the bivariate and multivariate approach in determining important predictors of sleep duration.
In conclusion, short sleep duration per night is very prevalent and affects one in every 3 Saudi adults. Female gender and bad sleep quality negatively contributed to the sleep duration times in our study population. Further studies are needed to better understand the effects of environmental factors and cultures on sleep duration. This study can contribute further to attempts by medical practitioners to educate their patients on lifestyle factors that could affect sleep health.
Acknowledgment
This study was funded by King Abdullah International Medical Research Center, Riyadh, Kingdom of Saudi Arabia which provided financial support in the form of study coordinators, data entry support, secretarial support, and other logistics. The sponsor had no role in the design or conduct of this research.
Footnotes
Copyright.
Whenever a manuscript contains material (tables, figures, etc.) which is protected by copyright (previously published), it is the obligation of the author to obtain written permission from the holder of the copyright (usually the publisher) to reproduce the material in Saudi Medical Journal. This also applies if the material is the authors own work. Please submit copies of the material from the source in which it was first published.
References
- 1.Ferrie JE, Shipley MJ, Cappuccio FP, Brunner E, Miller MA, Kumari M, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30:1659–1666. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–528. [PMC free article] [PubMed] [Google Scholar]
- 3.Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. J Clin Sleep Med. 2015;11:931–952. doi: 10.5664/jcsm.4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ryu SY, Kim KS, Han MA. Factors associated with sleep duration in Korean adults: results of a 2008 community health survey in Gwangju metropolitan city, Korea. J Korean Med Sci. 2011;26:1124–1131. doi: 10.3346/jkms.2011.26.9.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim WH, Kim BS, Kim SK, Chang SM, Lee DW, Cho MJ, et al. Sleep duration and associated factors in a community sample of elderly individuals in Korea. Psychogeriatrics. 2014 Dec 17; doi: 10.1111/psyg.12072. [DOI] [PubMed] [Google Scholar]
- 6.Hoefelmann LP, Lopes Ada S, da Silva KS, Moritz P, Nahas MV. Sociodemographic factors associated with sleep quality and sleep duration in adolescents from Santa Catarina, Brazil: what changed between 2001 and 2011? Sleep Med. 2013;14:1017–1023. doi: 10.1016/j.sleep.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res. 2009;18:148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 8.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33:585–592. doi: 10.1093/sleep/33.5.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aurora RN, Kim JS, Crainiceanu C, O’Hearn D, Punjabi NM. Habitual Sleep Duration and All-Cause Mortality in a General Community Sample. Sleep. 2016 Jul 19; doi: 10.5665/sleep.6212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kripke DF, Simons RN, Garfinkel L, Hammond EC. Short and long sleep and sleeping pills. Is increased mortality associated? Arch Gen Psychiatry. 1979;36:103–116. doi: 10.1001/archpsyc.1979.01780010109014. [DOI] [PubMed] [Google Scholar]
- 11.Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6:102–107. doi: 10.1093/sleep/6.2.102. [DOI] [PubMed] [Google Scholar]
- 12.Hammond EC. Some Preliminary Findings on Physical Complaints from a Prospective Study of 1,064,004 Men and Women. Am J Public Health Nations Health. 1964;54:11–23. doi: 10.2105/ajph.54.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27:51–54. [PubMed] [Google Scholar]
- 14.Cai H, Shu XO, Xiang YB, Yang G, Li H, Ji BT, et al. Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep. 2015;38:529–536. doi: 10.5665/sleep.4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall MH, Smagula SF, Boudreau RM, Ayonayon HN, Goldman SE, Harris TB, et al. Association between sleep duration and mortality is mediated by markers of inflammation and health in older adults: the Health, Aging and Body Composition Study. Sleep. 2015;38:189–195. doi: 10.5665/sleep.4394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leng Y, Cappuccio FP, Wainwright NW, Surtees PG, Luben R, Brayne C, et al. Sleep duration and risk of fatal and nonfatal stroke: a prospective study and meta-analysis. Neurology. 2015;84:1072–1079. doi: 10.1212/WNL.0000000000001371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 18.Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 19.Castro-Costa E, Dewey ME, Ferri CP, Uchoa E, Firmo JO, Rocha FL, et al. Association between sleep duration and all-cause mortality in old age:9-year follow-up of the Bambui Cohort Study, Brazil. J Sleep Res. 2011;20:303–310. doi: 10.1111/j.1365-2869.2010.00884.x. [DOI] [PubMed] [Google Scholar]
- 20.Hublin C, Partinen M, Koskenvuo M, Kaprio J. Sleep and mortality: a population-based 22-year follow-up study. Sleep. 2007;30:1245–12453. doi: 10.1093/sleep/30.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–444. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 22.Youngstedt SD, Kripke DF. Long sleep and mortality: rationale for sleep restriction. Sleep Med Rev. 2004;8:159–174. doi: 10.1016/j.smrv.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 23.Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. Am J Epidemiol. 2006;164:947–954. doi: 10.1093/aje/kwj280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xiao Q, Arem H, Moore SC, Hollenbeck AR, Matthews CE. A large prospective investigation of sleep duration, weight change, and obesity in the NIH-AARP Diet and Health Study cohort. Am J Epidemiol. 2013;178:1600–1610. doi: 10.1093/aje/kwt180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hasler G, Buysse DJ, Klaghofer R, Gamma A, Ajdacic V, Eich D, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27:661–666. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 26.Al-Hazzaa HM, Musaiger AO, Abahussain NA, Al-Sobayel HI, Qahwaji DM. Prevalence of short sleep duration and its association with obesity among adolescents 15- to 19-year olds: A cross-sectional study from three major cities in Saudi Arabia. Ann Thorac Med. 2012;7:133–139. doi: 10.4103/1817-1737.98845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zizi F, Pandey A, Murrray-Bachmann R, Vincent M, McFarlane S, Ogedegbe G, et al. Race/ethnicity, sleep duration, and diabetes mellitus: analysis of the National Health Interview Survey. Am J Med. 2012;125:162–167. doi: 10.1016/j.amjmed.2011.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Resnick HE, Redline S, Shahar E, Gilpin A, Newman A, Walter R, et al. Diabetes and sleep disturbances: findings from the Sleep Heart Health Study. Diabetes Care. 2003;26:702–709. doi: 10.2337/diacare.26.3.702. [DOI] [PubMed] [Google Scholar]
- 29.Tuomilehto H, Peltonen M, Partinen M, Seppa J, Saaristo T, Korpi-Hyovalti E, et al. Sleep duration is associated with an increased risk for the prevalence of type 2 diabetes in middle-aged women - The FIN-D2D survey. Sleep Med. 2008;9:221–227. doi: 10.1016/j.sleep.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 30.Zhan Y, Chen R, Yu J. Sleep duration and abnormal serum lipids: the China Health and Nutrition Survey. Sleep Med. 2014;15:833–839. doi: 10.1016/j.sleep.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 31.Sabanayagam C, Shankar A. Sleep duration and hypercholesterolaemia: Results from the National Health Interview Survey 2008. Sleep Med. 2012;13:145–150. doi: 10.1016/j.sleep.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gangwisch JE, Malaspina D, Babiss LA, Opler MG, Posner K, Shen S, et al. Short sleep duration as a risk factor for hypercholesterolemia: analyses of the National Longitudinal Study of Adolescent Health. Sleep. 2010;33:956–961. doi: 10.1093/sleep/33.7.956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li Y, Vgontzas AN, Fernandez-Mendoza J, Bixler EO, Sun Y, Zhou J, et al. Insomnia with physiological hyperarousal is associated with hypertension. Hypertension. 2015;65:644–650. doi: 10.1161/HYPERTENSIONAHA.114.04604. [DOI] [PubMed] [Google Scholar]
- 34.Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006;47:833–839. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 35.Wang Y, Mei H, Jiang YR, Sun WQ, Song YJ, Liu SJ, et al. Relationship between Duration of Sleep and Hypertension in Adults: A Meta-Analysis. J Clin Sleep Med. 2015;11:1047–1056. doi: 10.5664/jcsm.5024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cappuccio FP, Stranges S, Kandala NB, Miller MA, Taggart FM, Kumari M, et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II Study. Hypertension. 2007;50:693–700. doi: 10.1161/HYPERTENSIONAHA.107.095471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lombardi DA, Folkard S, Willetts JL, Smith GS. Daily sleep, weekly working hours, and risk of work-related injury: US National Health Interview Survey (2004-2008) Chronobiol Int. 2010;27:1013–1030. doi: 10.3109/07420528.2010.489466. [DOI] [PubMed] [Google Scholar]
- 38.Marshall NS, Bolger W, Gander PH. Abnormal sleep duration and motor vehicle crash risk. J Sleep Res. 2004;13:177–178. doi: 10.1111/j.1365-2869.2004.00402.x. [DOI] [PubMed] [Google Scholar]
- 39.Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med. 2002;251:207–216. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- 40.Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: results from the National Health Interview Survey. Sleep. 2010;33:1037–1042. doi: 10.1093/sleep/33.8.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of Healthy Sleep Duration among Adults--United States 2014. MMWR Morb Mortal Wkly Rep. 2016;65:137–141. doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- 42.Shankar A, Charumathi S, Kalidindi S. Sleep duration and self-rated health: the national health interview survey 2008. Sleep. 2011;34:1173–1177. doi: 10.5665/SLEEP.1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37:601–611. doi: 10.5665/sleep.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bouscoulet LT, Vazquez-Garcia JC, Muino A, Marquez M, Lopez MV, de Oca MM, et al. Prevalence of sleep related symptoms in four Latin American cities. J Clin Sleep Med. 2008;4:579–585. [PMC free article] [PubMed] [Google Scholar]
- 45.Patel SR, Sotres-Alvarez D, Castaneda SF, Dudley KA, Gallo LC, Hernandez R, et al. Social and Health Correlates of Sleep Duration in a US Hispanic Population: Results from the Hispanic Community Health Study/Study of Latinos. Sleep. 2015;38:1515–1522. doi: 10.5665/sleep.5036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Saleh AB, Ahmad MA, Awadalla NJ. Development of Arabic version of Berlin questionnaire to identify obstructive sleep apnea at risk patients. Ann Thorac Med. 2011;6:212–216. doi: 10.4103/1817-1737.84775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–491. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 48.Ahmed AE, Fatani A, Al-Harbi A, Al-Shimemeri A, Ali YZ, Baharoon S, et al. Validation of the Arabic version of the Epworth sleepiness scale. J Epidemiol Glob Health. 2014;4:297–302. doi: 10.1016/j.jegh.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.American Academy of Sleep Medicine. International Classification of Sleep Disorders. Rochester (MN): American Academy of Sleep Medicine; 1997. [Google Scholar]
- 50.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 51.Suleiman KH, Yates BC, Berger AM, Pozehl B, Meza J. Translating the Pittsburgh Sleep Quality Index into Arabic. West J Nurs Res. 2010;32:250–268. doi: 10.1177/0193945909348230. [DOI] [PubMed] [Google Scholar]
- 52.Tsai TC, Wu JS, Yang YC, Huang YH, Lu FH, Chang CJ. Long sleep duration associated with a higher risk of increased arterial stiffness in males. Sleep. 2014;37:1315–1320. doi: 10.5665/sleep.3920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014;15:1456–1462. doi: 10.1016/j.sleep.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 54.Lou P, Zhang P, Zhang L, Chen P, Chang G, Zhang N, et al. Effects of sleep duration and sleep quality on prevalence of type 2 diabetes mellitus: A 5-year follow-up study in China. Diabetes Res Clin Pract. 2015;109:178–184. doi: 10.1016/j.diabres.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 55.Gale C, Martyn C. Larks and owls and health, wealth, and wisdom. BMJ. 1998;317:1675–1677. doi: 10.1136/bmj.317.7174.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lan TY, Lan TH, Wen CP, Lin YH, Chuang YL. Nighttime sleep, Chinese afternoon nap, and mortality in the elderly. Sleep. 2007;30:1105–1110. doi: 10.1093/sleep/30.9.1105. [DOI] [PMC free article] [PubMed] [Google Scholar]


