Abstract
Introduction
β Blockers are important treatment for ischaemic heart disease and heart failure; however, there has long been concern about their use in people with chronic obstructive pulmonary disease (COPD) due to fear of symptomatic worsening of breathlessness. Despite growing evidence of safety and efficacy, they remain underused. We examined the effect of β-blockade on lung function, exercise performance and dynamic hyperinflation in a group of vascular surgical patients, a high proportion of who were expected to have COPD.
Methods
People undergoing routine abdominal aortic aneurysm (AAA) surveillance were sequentially recruited from vascular surgery clinic. They completed plethysmographically measured lung function and incremental cardiopulmonary exercise testing with dynamic measurement of inspiratory capacity while taking and not taking β blocker.
Results
48 participants completed tests while taking and not taking β blockers with 38 completing all assessments successfully. 15 participants (39%) were found to have, predominantly mild and undiagnosed, COPD. People with COPD had airflow obstruction, increased airway resistance (Raw) and specific conductance (sGaw), static hyperinflation and dynamically hyperinflated during exercise. In the whole group, β-blockade led to a small fall in FEV1 (0.1 L/2.8% predicted) but did not affect Raw, sGaw, static or dynamic hyperinflation. No difference in response to β-blockade was seen in those with and without COPD.
Conclusions
In people with AAA, β-blockade has little effect on lung function and dynamic hyperinflation in those with and without COPD. In this population, the prevalence of COPD is high and consideration should be given to case finding with spirometry.
Trial registration number
Keywords: Lung Physiology, Exercise, COPD Pharmacology
Introduction
β Blockers represent an important treatment for heart failure and have been shown to reduce mortality and symptoms.1 In addition, β blockers are an important part of treatment postmyocardial infarction (MI) where again they are associated with reduced mortality including in people with chronic obstructive pulmonary disease (COPD).2 However, there has long been concern that β blockers may worsen lung function3 and could be associated with increased mortality in people with severe COPD.4 Heart failure guidelines recommend their use stating that COPD is not a contraindication to β-blockade5 and a body of evidence now exists suggesting that cardioselective β blockers are not detrimental to people with COPD rather their prescription is associated with a survival benefit post-MI,6 in chronic heart failure7 and overall.8 There is also a suggestion that the use of β blockers is associated with fewer disease exacerbations.8–11 However, it is clear that β blockers are still underused in people with COPD12 because of fears of worsening lung function, associated with increased symptoms, secondary to parasympathetic bronchoconstriction.
A number of studies, using a variety of cardioselective and non-cardioselective β blockers, have assessed the short-term effect of β-blockade on FEV1 and meta-analyses show no effect or small, but relatively insignificant, falls in FEV1.13 14 However, most studies report the effect of β blockers on spirometry only and there is a lack of data on other lung function measures, in particular body plethysmographic data. To the best of our knowledge, only one prospective study has examined the effect of β blockers on dynamic hyperinflation and peak exercise capacity.15 This is important because there is a relatively weak relationship between FEV1, symptoms and exercise capacity, in people with COPD, which may explain the reluctance to prescribe. Moreover, it is recognised that COPD is underdiagnosed16 and this may contribute to reluctance to use β blockers in long-term cigarette smokers.
We have recently published a study examining the effect of perioperative β-blockade on cardiopulmonary exercise performance in people with abdominal aortic aneurysm (AAA) awaiting surgery.17 We showed improvement in exercise performance when people were taking β blockers. As a ‘real life’ study, a significant number of participants had (mainly undiagnosed and relatively mild) COPD. As part of this study, we examined the effect of β-blockade on lung function, including body plethysmography and dynamic hyperinflation, during exercise testing. We hypothesised that β-blockade would have little effect on these parameters in the overall group, but there would be a greater effect on airway resistance, specific conductance and dynamic hyperinflation in those participants with COPD.
Methods
Participants
Between April 2012 and August 2013, participants were recruited from a cohort attending our vascular laboratory for routine AAA surveillance (<5.5 cm aneurysm). We approached all patients >18 years who were able to perform a cardiopulmonary exercise test (CPET) and excluded patients who had a known contraindication to β blockers, severe ischaemic heart disease, stage IV–V chronic kidney disease, uncontrolled hypertension, those unable to consent and absolute contraindications to CPET based on the ATS/ACCP guidelines.18 Participants were neither selected for the presence or absence of COPD nor use of β blockers. Written informed consent was obtained from all patients.
Study design
Patients were divided into two groups based on whether they were normally taking β blockers (chronic β blockade) or not (acute β blockade). All patients completed the study protocol both ‘on’ and ‘off’ β blockers. Patients already taking β blockers completed tests at visit 1 taking their usual prescription and repeated tests at visit 2 having stopped β blocker for at least 7 days. Patients not normally taking β blockers completed tests at visit 1 ‘off’ β blockers and then started bisoprolol, a cardioselective β blocker, once daily—1.25 mg if weight 50–75 kg, 2.5 mg if 76–100 kg and 3.75 mg if 101 kg or heavier. Doses were not titrated to achieve a target heart rate. Participants then repeated tests at visit 2 at least 48 hours after starting bisoprolol. All participants were advised of the potential risks of alteration of their medical therapy at the time of consent.
Demographics details and health and medication information was collected. At each visit, participants completed lung function measurements, including spirometry, lung volumes, gas transfer and airway resistance using body plethysmography (Zan Messgerate, nSpire Health 530). The small number of participants already diagnosed with airway disease were asked to omit short-acting bronchodilators for 6 hours and long-acting bronchodilators (β-agonists and antimuscarinics) for 12 or 24 hours, according to the bronchodilator taken normally. All measurements were performed according to ERS/ATS guidelines.19 Study participants performed incremental CPET, following a standard protocol, and these results have been published previously.17 Inspiratory capacity (IC) was measured before exercise and then every minute during exercise with a final IC measurement at peak exercise.20 Isotime IC was used for analysis. Borg score of breathlessness and leg fatigue was also measured at rest and then every minute during exercise and recovery.21
Assessment of the impact of β-blockade on lung function parameters and dynamic hyperinflation (dynamic IC measurements) was a predefined study outcome. Subgroup analysis according to the presence or absence of COPD was performed post hoc when it was established that a significant number of study participants had (predominantly undiagnosed) COPD.
In the absence of postbronchodilator measures of lung function and to avoid overdiagnosis of COPD in older participants (particularly men), the diagnosis of COPD was based on a minimum 10 pack years cigarette smoking and a prebronchodilator FEV1/FVC ratio exceeding the lower limit of normal using GLI-2012 equations.22 Airflow obstruction was defined as a standard residual z-score of below −1.64.
Statistical methods
Patient demographics have been summarised as mean (SD) for continuous variables or median (IQR) if non-normal and as frequency (%) for categorical variables. Pair plots were produced for each variable to graphically visualise the difference between on and off measurements for each patient and to identify any relationship between the outcome variables and being on/off β blockers for those with normal lung function and those with COPD. Variables were summarised by β blocker status (on/off) and for normal lung function compared with COPD and a comparison performed using a paired t-test or a Mann-Whitney U-test when non-normal and for categorical variables using a χ2 test or a Fisher's exact test when cell frequencies were insufficient. A p value of <0.05 was considered significant.
Study power was based on change in VO2 peak at anaerobic threshold (AT) which was the primary outcome in our previous publication17 where we estimated that 32 patients were required to detect a 10% difference in VO2 at AT with 90% power and allowing for 25% drop out. Separate study power was not calculated for the outcomes described here. All statistical analyses were performed using Stata V.13 (StataCorp., 2013. Stata Statistical Software: release 13. College Station).
Results
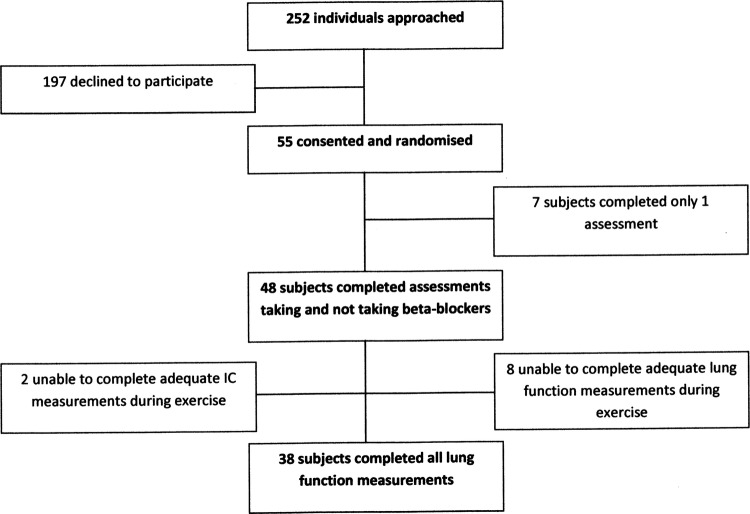
We screened 252 participants, 55 completed the first assessment but 7 people then dropped out leaving 48 who completed both visits. No participant dropped out due to symptoms possibly or likely related to β-blockade—five performed the first test taking β blockers but all were taking them long term and two performed the first test not taking β blockers. From these 48 patients, 2 were unable to perform IC at peak exercise reliably and a further 8 did not produce guideline defined lung function tests, so were excluded from this analysis leaving 38 participants. This is shown in figure 1. Six participants already had a diagnosis of COPD.
Figure 1.
Consort diagram describing study flow.
From the 38 patients that completed all study methods, 16 patients were already taking β blockers (chronic group) and 22 were not taking β blockers (acute group). Patients in the chronic group were taking bisoprolol (8 participants), atenolol (5), propranolol (1), carvedilol (1) and metoprolol (1) for hypertension (9 participants), ischaemic heart disease (5) and atrial fibrillation (1) with the indication being unclear in one participant. The CPET results have been published previously.17
Baseline characteristics of the whole group (n=38) and split into those with (n=15) and without (n=23) COPD are shown in table 1. The lung function parameters presented were recorded at the visit off β blockers. There were no significant differences between the COPD group and non-COPD group in age, gender, height, weight or BMI. As expected, there were significant differences in smoking and pack years. People with COPD not only had a lower FEV1 and greater airflow obstruction but were also more hyperinflated, had lower airway specific conductance and showed dynamic hyperinflation with exercise (a significant fall in IC at peak exercise).
Table 1.
Patient demographics and lung function recorded when they were not taking β blockers in the 38 participants and split according to the presence or absence of chronic obstructive pulmonary disease
| Whole group (n=38) | Non-COPD (n=23) | COPD (n=15) | p Value | |
|---|---|---|---|---|
| Age (years) | 70 (5) | 69 (6) | 72 (4) | 0.16 |
| Male | 33 (87%) | 19 (83%) | 14 (93%) | 0.35 |
| Female | 5 (13%) | 4 (17%) | 1 (7%) | |
| BMI (kg/m2) | 29.1 (4.3) | 29.3 (4) | 28.6 (5) | 0.72 |
| Smoking | ||||
| Current | 10 (26%) | 5 (22%) | 5 (33%) | <0.01 |
| Ex-smoker | 19 (50%) | 9 (39%) | 10 (67%) | |
| Non-smoker | 9 (24%) | 9 (39%) | 0 | |
| Pack years | 31 (0–100) | 23(0–80) | 43.5 (12–100) | 0.02 |
| Current β blocker | ||||
| No | 22 (58%) | 10 (43%) | 12 (80%) | 0.83 |
| Yes | 16 (42%) | 13 (57%) | 3 (20%) | |
| FEV1 (L) | 2.57 (0.69) | 2.86 (0.61) | 2.03 (0.55) | <0.01 |
| FEV1 (%) | 94.8 (22.4) | 105.4 (17.9) | 75.0 (16.1) | <0.01 |
| FEV1/FVC | 0.69 (0.12) | 0.75 (0.05) | 0.56 (0.08) | <0.01 |
| FVC (L) | 3.68 (0.76) | 3.71 (0.8) | 3.61 (0.8) | 0.68 |
| FVC (%) | 107.3 (18.7) | 110 (19.9) | 103.0 (16.8) | 0.31 |
| RV/TLC | 46.2 (15) | 42.4 (16.7) | 52.5 (10.3) | <0.01 |
| TLCO (mmol/min/kPa) | 6.28 (1.84) | 6.44 (1.53) | 6.04 (2.28) | 0.52 |
| TLCO (% predicted) | 78.2 (20.1) | 80.4 (16.5) | 74.8 (24.9) | 0.52 |
| KCO (units/min) | 1.17 (0.28) | 1.24 (0.22) | 1.06 (0.33) | 0.41 |
| KCO (% predicted) | 91.3 (22.8) | 94.9 (20.1) | 85.7 (26.3) | 0.23 |
| Raw (kPa/s/L) | 2.31 (0.88) | 2.17 (0.74) | 2.63 (1.05) | 0.31 |
| sGaw (kPa/s) | 0.12 (0.05) | 0.14 (0.05) | 0.08 (0.03) | <0.01 |
| sRaw (kPa/s) | 9.23 (3.62) | 7.61 (3.12) | 11.71 (2.76) | <0.01 |
| Resting IC (L) | 2.91 (0.39) | 2.71 (0.48) | 2.99 (0.48) | 0.28 |
| Change in IC (L)—dynamic hyperinflation | −0.09 (0.25) | −0.02 (0.24) | −0.20 (0.23) | 0.02 |
Results are shown as mean±SD with the exception of pack years which is presented as mean (range).
FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; IC, inspiratory capacity; KCO, transfer coefficient for carbon monoxide; Raw, airway resistance; RV, residual volume; sGaw, specific airway conductance; sRaw, specific airway resistance; TLC, total lung capacity; TLCO, diffusing capacity for carbon monoxide.
Effect of β blocker
Significant β blockade was achieved with a fall in heart rate by 18 bpm.
The effect of β-blockade on cardiorespiratory parameters is shown in table 2. β-Blockade led to a small but significant fall in FEV1 in the whole group by a mean 100 mL (2.8% of predicted value), but there was no further significant change in any other lung function measure.
Table 2.
Change in lung function and heart rate on and off β blockers in the whole group of 38 participants
| Lung function or heart rate measurement | Change | p Value |
|---|---|---|
| FEV1 (L) | −0.10 (0.23) | 0.01 |
| FEV1 (% predicted) | −2.8 (5.9) | <0.01 |
| FVC (L) | −0.10 (0.28) | 0.98 |
| FVC (% predicted) | −0.8 (6.7) | 0.45 |
| FEV1/FVC | −0.01 (0.05) | 0.12 |
| RV/TLC (% pred.) | −0.8 (9) | 0.63 |
| Raw (kPa/s/L) | 0.15 (0.67) | 0.17 |
| sGaw (kPa/s) | 0 (0.03) | 0.73 |
| sRaw (kPa/s) | 0.91 (1.89) | <0.01 |
| Resting IC (L) | −0.01 (0.79) | 0.96 |
| Change in IC (L)—dynamic hyperinflation | −0.03 (0.29) | 0.5 |
| Heart rate (bpm) | −18 (19) | <0.01 |
FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; IC, inspiratory capacity; Raw, airway resistance; RV, residual volume; sGaw, specific airway conductance; sRaw, specific airway resistance; TLC, total lung capacity.
There was no difference in the effect of β-blockade according to whether the β blocker was already prescribed (chronic group) or not normally prescribed (acute group).
Effect of β blocker according to COPD status
In this unselected group, we found 15 people had COPD. Six were previously diagnosed (3 already treated with a β blocker) and 9 newly diagnosed (3 already treated with a β blocker).
There was no difference in the effect of β-blockade on lung function or dynamic hyperinflation when patients with COPD were compared with those without COPD as shown in table 3. In particular, the small change seen in FEV1 was seen in people with and without COPD. Only the COPD participants showed a fall in IC with exercise (dynamic hyperinflation) and β-blockade had no significant impact on this.
Table 3.
The effect of β-blockade on change in lung function, dynamic hyperinflation and peak exercise according to whether the individual had chronic obstructive pulmonary disease
| Change; non-COPD (n=23) | Change; COPD (n=15) | p Value | |
|---|---|---|---|
| FEV1 (L) | −0.09 (0.32) | −0.11 (0.18) | 0.76 |
| FEV1 (% predicted) | −1.9 (5.9) | −4.2 (6.5) | 0.24 |
| FVC (L) | 0.01 (0.35) | −0.09 (0.29) | 0.30 |
| FVC (% predicted) | 0.2 (5.7) | −2.2 (8.3) | 0.32 |
| FEV1/FVC | −0.01 (0.06) | −0.02 (0.06) | 0.49 |
| RV/TLC (% predicted) | −2.1 (3.5) | 0.5 (5.1) | 0.27 |
| Raw (kPa/s/L) | −0.15 (0.66) | −0.13 (0.84) | 0.90 |
| sGaw (kPa/s) | 0.01 (0.05) | 0 (0.01) | 0.78 |
| sRaw (kPa/s) | 0.74 (1.89) | 1.17 (1.87) | 0.5 |
| IC (L) at rest | 0 (1.10) | −0.05 (0.62) | 0.46 |
| VO2 at LT (mL/min) | −0.21 (1.34) | −0.54 (1.40) | 0.54 |
| VO2 at peak (mL/min) | 0.11 (2.31) | 0.21 (2.11) | 0.90 |
| Oxygen pulse (mL/beat) | −1.52 (2.23) | −2.17 (2.09) | 0.42 |
| VE/VO2 | 0.97 (3.90) | 0.48 (3.63) | 0.70 |
| VE/VCO2 | 1.27 (2.33) | 0.23 (1.72) | 0.45 |
| Workload (W) | −1.1 (7.7) | 4.3 (9.5) | 0.08 |
| Heart rate (bpm) | −17 (11) | −17 (7) | 0.60 |
| Change in IC (L)—dynamic hyperinflation | 0.02 (0.24) | −0.07 (0.30) | 0.09 |
FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; IC, inspiratory capacity; LT, lactate threshold; Raw, airway resistance; RV, residual volume; sGaw, specific airway conductance; sRaw, specific airway resistance; TLC, total lung capacity; VCO2, maximal carbon dioxide output; VE, minute ventilation; VO2, maximal oxygen uptake.
No significant difference was seen in peak exercise measures when the COPD and non-COPD groups were compared.
Discussion
We have shown that β-blockade has a minimal effect on lung function and dynamic hyperinflation, in vascular surgical patients, regardless of the presence of mild to moderate COPD. Combined with our published cardiopulmonary exercise testing results,17 this provides further reassurance that the use of β blockers remains safe in people with COPD. The high prevalence of COPD suggests that vascular surgical clinics may represent a good place for COPD case finding using spirometry.
It is known that bronchodilators, including β-agonists, produce relatively rapid relaxation of airway smooth muscle and improve expiratory flow rate, but it is questionable whether this is the mechanism by which they act in people with COPD where the prominent abnormalities are increased peripheral resistance and loss of lung elastic recoil.23 In COPD patients, β-agonists have been shown to reduce tidal inspiratory resistance,24 but their main effect is by reducing end-expiratory lung volume which allows the individual to exercise for longer before they reach a critical and exercise limiting inspiratory reserve volume.25 Hence, drugs that antagonise airway β receptors and consequently reduce airway calibre through their effect on airway smooth muscle may have little effect on measures of airway function in COPD patients as this is not predominantly determined by airway smooth muscle. Our results are consistent with this. There was a small effect on expiratory flow measured by FEV1, which is consistent with previous studies,14 but no effect on airflow assessed by FEV1/FVC. Airway resistance and specific conductance were unchanged, something which has not been published previously, and β-blockade did not lead to a significant change in end-expiratory lung volume and magnitude of dynamic hyperinflation during exercise. These results are consistent with the minimal impact of perioperative β-blockade on cardiopulmonary exercise parameters, despite the high proportion of people with COPD in the study.17
The study was designed, and powered, to establish the effect of β-blockade on exercise parameters at AT and peak ventilation.17 Participants were not selected because they had COPD. The high prevalence of COPD was higher than expected and exceeded 50% if only current or ex-smokers were considered, so provided an opportunity to compare the response to β-blockade of people with COPD compared with a non-COPD population. It is striking that no difference in group response was seen in any measure of lung function. The majority of people had mild COPD, but it has been shown previously these individuals have significant ventilatory impairment and gas exchange abnormalities during exercise.26 Our results are consistent with this work and our participants with generally mild COPD showed significant dynamic hyperinflation (IC fell by an average of about 200 mL at peak exercise) and poorer ventilatory function at AT and peak exercise before β-blockade. However, β-blockade did not significantly worsen this. Ours is only the second study to examine the effect of β-blockade on dynamic hyperinflation in COPD patients and, along with the previous study, has shown no significant impact.15 However, our participants had less severe COPD (FEV1 75% vs 52% predicted) and fall in IC was greater in the previous study probably due to greater disease severity and measurement during endurance rather than incremental testing. Consequently, although β-blockade did not lead to a significant difference in change in dynamic IC, when comparing participants with and without COPD, we cannot exclude this being apparent in a population with more severe airway disease.
AAA is a recognised comorbidity in people with COPD as is peripheral vascular disease with a prevalence of 7% aged 55 years or younger increasing to 17% in those 65 years or older.27 Six people were diagnosed with COPD but after spirometry, a further nine current or ex-smokers had significant airflow obstruction; a COPD prevalence of 39%. Although we were unable to present full lung function results from a further 10 participants, they all completed resting spirometry and 21 of the 48 participants in this larger group had airflow obstruction; a COPD prevalence of 44%. This is >50% of only current or ex-smokers are considered. Although our sample size is modest, this figure is higher than many screening studies of high-risk individuals who had chronic respiratory symptoms28 and spirometry screening in our local population29 and provides an opportunity for COPD case finding.
The study has a number of weaknesses, the foremost of which being that participants were not selected because they had COPD (or cardiac disease including heart failure) and the study was powered to assess a difference in VO2 at AT in the whole group rather than the outcomes we present. Hence, this is a post hoc analysis and worthy of prospective confirmation. Notwithstanding, the results add to the evidence base supporting the use of β blockers in people with COPD, present data on plethysmographic lung function for the first time and add to the only previous publication looking at the effect of β-blockade on dynamic hyperinflation because our population had only modest spirometric impairment.15 The other core limitation is we cannot exclude more significant dynamic hyperinflation if the participants had more severe COPD and more complete β blockade. We achieved significant β-blockade with a mean fall in resting pulse of 18 bpm, but the protocol was pragmatic and the aim was not to reduce heart rate to a level of 60–70 bpm promoted in clinical cardiology practice.30 This is also reflected in the modest fall in whole group systolic blood pressure of 3 and 1 mm Hg diastolic. However, it seems unlikely this would significantly impact other lung function parameter considering the lack of effect shown. The time that the participant was taking β blockers was often relatively short (excepting those individuals taking β blockers chronically) but is consistent with many previous studies addressing the impact of β-blockade in COPD patients. We did not switch individuals normally taking β blockers from their usual therapy to bisoprolol in order to mirror perioperative practice and to reduce the time that β blockers were withdrawn from people taking them chronically. This meant that participants were not all taking a cardioselective β blocker, but we do not believe there was a significant impact on study results as 30/38 participants were taking bisoprolol.
In summary, perioperative β blockade in people undergoing vascular surgery appears safe generally and more specifically in patients with coexistent mild to moderate COPD. The impact on lung function is minimal and there is no change in airway resistance, specific conductance or dynamic hyperinflation. However, the prevalence of undiagnosed COPD is high and consideration should be made to spirometric case finding screening in this population.
Footnotes
Contributors: MAW, SJ, ND and FT contributed to study conception and design. AK, MP and MAW contributed to data acquisition. AK, MAW, RA, SJ, ND, FT and PPW contributed to data analysis and interpretation. AK and PPW contributed to manuscript drafting. AK, MP, MAW, RA, SJ, ND, FT and PPW contributed to critical manuscript revision and final manuscript approval. PPW has overall responsibility for the manuscript and is the guarantor
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: North West—Liverpool East Research and Ethics Committee (11/NW/0810).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.NICE, August 2010. Chronic heart failure in adults: management. NICE guidelines [CG108]. https://www.nice.org.uk/guidance/CG108 (accessed 27 Jul 2016).
- 2.Gottlieb SS, McCarter RJ, Vogel RA. Effect of beta-blockade on mortality among high-risk and low-risk patients after myocardial infarction. N Engl J Med 1998;339:489–97. doi:10.1056/NEJM199808203390801 [DOI] [PubMed] [Google Scholar]
- 3.van der Woude HJ, Zaagsma J, Postma DS et al. . Detrimental effects of beta-blockers in COPD: a concern for nonselective beta-blockers. Chest 2005;127:818–24. doi:10.1378/chest.127.3.818 [DOI] [PubMed] [Google Scholar]
- 4.Ekström MP, Hermansson AB, Ström KE. Effects of cardiovascular drugs on mortality in severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2013;187:715–20. doi:10.1164/rccm.201208-1565OC [DOI] [PubMed] [Google Scholar]
- 5.Dickstein K, Cohen-Solal A, Filippatos G et al. . ESC Committee for Practice Guidelines (CPG). ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 2008;29:2388–442. doi:10.1093/eurheartj/ehn309 [DOI] [PubMed] [Google Scholar]
- 6.Quint K, Herrett E, Bhaskaran K et al. . Effect of β blockers on mortality after myocardial infarction in adults with COPD: population based cohort study of UK electronic healthcare records. BMJ 2013;347:f6650 doi:10.1136/bmj.f6650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mentz RJ, Wojdyla D, Fiuzat M et al. . Association of beta-blocker use and selectivity with outcomes in patients with heart failure and chronic obstructive pulmonary disease (from OPTIMIZE-HF). Am J Cardiol 2013;111:582–7. doi:10.1016/j.amjcard.2012.10.041 [DOI] [PubMed] [Google Scholar]
- 8.Short PM, Lipworth SI, Elder DH et al. . Effect of beta blockers in treatment of chronic obstructive pulmonary disease: a retrospective cohort study. BMJ 2011;342:d2549 doi:10.1136/bmj.d2549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farland MZ, Peters CJ, Williams JD et al. . β-Blocker use and incidence of chronic obstructive pulmonary disease exacerbations. Ann Pharmacother 2013;47:651–6. doi:10.1345/aph.1R600 [DOI] [PubMed] [Google Scholar]
- 10.Rutten FH, Zuithoff NP, Hak E et al. . Beta-blockers may reduce mortality and risk of exacerbations in patients with chronic obstructive pulmonary disease. Arch Intern Med 2010;170:880–7. doi:10.1001/archinternmed.2010.112 [DOI] [PubMed] [Google Scholar]
- 11.Bhatt SP, Wells JM, Kinney GL et al. . COPD Gene Investigators. β-Blockers are associated with a reduction in COPD exacerbations. Thorax 2016;71:8–14. doi:10.1136/thoraxjnl-2015-207251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puente-Maestu L, Calle M, Ortega-González A et al. . GEMEPOC Group. Multicentric study on the beta-blocker use and relation with exacerbations in COPD. Respir Med 2014;108:737–44. doi:10.1016/j.rmed.2014.02.009 [DOI] [PubMed] [Google Scholar]
- 13.Hawkins NM, MacDonald MR, Petrie MC et al. . Bisoprolol in patients with heart failure and moderate to severe chronic obstructive pulmonary disease: a randomized controlled trial. Eur J Heart Fail 2009;11:684–90. doi:10.1093/eurjhf/hfp066 [DOI] [PubMed] [Google Scholar]
- 14.Salpeter S, Ormiston T, Salpeter E. Cardioselective beta-blockers for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2005;4:CD003566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mainguy V, Girard D, Maltais F et al. . Effect of bisoprolol on respiratory function and exercise capacity in chronic obstructive pulmonary disease. Am J Cardiol 2012;110:258–63. doi:10.1016/j.amjcard.2012.03.019 [DOI] [PubMed] [Google Scholar]
- 16.British Thoracic Society, 2006. The burden of lung disease. 2nd edn, 2006. http://www.brit-thoracic.org.uk/delivery-of-respiratory-care/burden-of-lung-disease-reports (accessed 26 Jul 2016). [Google Scholar]
- 17.West MA, Parry M, Asher R et al. . The effect of beta-blockade on objectively measured physical fitness in patients with abdominal aortic aneurysms—a blinded interventional study. Br J Anaesth 2015;114:878–85. doi:10.1093/bja/aev026 [DOI] [PubMed] [Google Scholar]
- 18.Weisman IM, Marciniuk D, Martinez FJ et al. . ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 2003;167:211–77. doi:10.1164/rccm.167.2.211 [DOI] [PubMed] [Google Scholar]
- 19.Brusasco V, Crapo R, Viegi G. Coming together: the ATS/ERS consensus on clinical pulmonary function testing. Eur Respir J 2005;26:1–2. doi:10.1183/09031936.05.00034205 [DOI] [PubMed] [Google Scholar]
- 20.Dolmage TE, Goldstein RS. Repeatability of inspiratory capacity during incremental exercise in patients with severe COPD. Chest 2002;121:708–14. [DOI] [PubMed] [Google Scholar]
- 21.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982;14:377. [PubMed] [Google Scholar]
- 22.Quanjer PH, Stanojevic S, Cole TJ et al. , ERS Global Lung Function Initiative. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 2012;40:1324–43. doi:10.1183/09031936.00080312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Calverley PM, Albert P, Walker PP. Bronchodilator reversibility in chronic obstructive pulmonary disease: use and limitations. Lancet Respir Med 2013;1:564–73. doi:10.1016/S2213-2600(13)70086-9 [DOI] [PubMed] [Google Scholar]
- 24.Dellaca RL, Pompilio PP, Walker PP et al. . Effect of bronchodilation on expiratory flow limitation and resting lung mechanics in COPD. Eur Respir J 2009;33:1329–37. doi:10.1183/09031936.00139608 [DOI] [PubMed] [Google Scholar]
- 25.O'Donnell DE, Voduc N, Fitzpatrick M et al. . Effect of salmeterol on the ventilatory response to exercise in chronic obstructive pulmonary disease. Eur Respir J 2004;24:86–94. doi:10.1183/09031936.04.00072703 [DOI] [PubMed] [Google Scholar]
- 26.Elbehairy AF, Ciavaglia CE, Webb KA et al. , Canadian Respiratory Research Network. Pulmonary gas exchange abnormalities in mild chronic obstructive pulmonary disease. Implications for dyspnea and exercise intolerance. Am J Respir Crit Care Med 2015;191:1384–94. doi:10.1164/rccm.201501-0157OC [DOI] [PubMed] [Google Scholar]
- 27.Divo MJ, Casanova C, Marin JM et al. , BODE Collaborative Group. COPD comorbidities network. Eur Respir J 2015;46:640–50. doi:10.1183/09031936.00171614 [DOI] [PubMed] [Google Scholar]
- 28.Van Schayck CP, Loozen JM, Wagena E et al. . Detecting patients at a high risk of developing chronic obstructive pulmonary disease in general practice: cross sectional case finding study. BMJ 2002;324:1370 doi:10.1136/bmj.324.7350.1370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walker PP, Mitchell P, Diamantea F et al. . Effect of primary-care spirometry on the diagnosis and management of COPD. Eur Respir J 2006;28:945–52. doi:10.1183/09031936.06.00019306 [DOI] [PubMed] [Google Scholar]
- 30.Swedberg K, Komajda M, Böhm M et al. , SHIFT Investigators. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 2010;376:875–85. [DOI] [PubMed] [Google Scholar]