1. Introduction – delayed presentation and STEMI pathways
Optimal treatment of acute ST-elevation myocardial infarction (STEMI) in developing countries may require a novel approach on account of the numerous infrastructure, personnel, financial and logistic constraints.
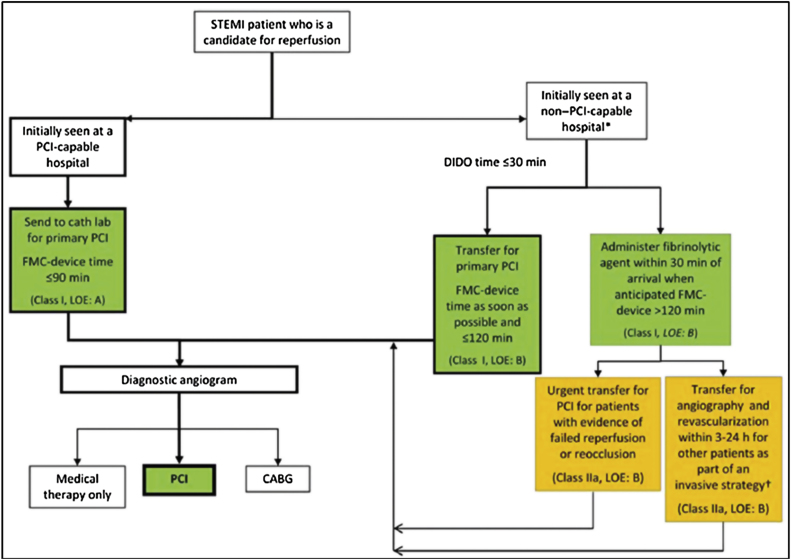
The prevalent pathways of STEMI care, which exist in North America and in Europe, face hurdles in low and middle-income countries. The American College of Cardiology Foundation/American Heart Association (ACCF/AHA) and the Stent for Life STEMI Guidelines recommendation to develop regional systems of STEMI care (Fig. 1) is extremely challenging to adopt in developing countries.1, 2 This occurs due to numerous reasons – hospitals have not been clearly identified as PCI and non-PCI institutions and the network and transfer policies between these hospitals have not been wellestablished. Another important drawback is the general lack of ambulance-based emergency medical services in many developing countries, which means that a major component of regional STEMI networks are completely missing. In a similar manner, the recommendations of Mission: Lifeline, an AHA initiative launched in 2007, to improve health system readiness and response to STEMI, with the focus on the continuum of care from EMS activation to primary PCI, cannot function in environments that lack sophisticated prehospital care.3 The endorsements of the other remarkable ACCF initiative, the D2B Alliance, whose goal was for participating PCI-capable hospitals to achieve a D2B time of <90 min, is also a major challenge in developing countries related to resource constraints that have been listed above. Most importantly, there are no guidelines for late presenters with in countries with system delays and non-existent STEMI networks. This manuscript is specifically designed to offer pragmatic solutions for improving STEMI care in low and middle-income countries.4, 5
Fig. 1.
STEMI Systems of Care – ACCF/AHA Recommended Pathways.
Delayed presentation is the single biggest global challenge for patients presenting with STEMI and this issue is far worse in developing countries for a variety of reasons. These include the traditional patient-related delays that are also seen in North America and in Europe and which include women, the elderly and the diabetics.6 In low and middle-income countries, there are additional and distinctive process delays, such as stoppages as a result of payment and consent issues. Alexander and Mullasari reported a time to presentation in India of 300 min, in stark contrast to in the U.S. where patients calling 9-1-1 now have EMS personnel arrive at their sides in less than 50 min after symptom onset.7, 8 The delayed presentation in India (and in several other low and middle-income countries) has critical implications for instituting pragmatic guidelines. Delayed presentation is the Achilles heel of STEMI care in these countries and a rethink of this subject is critical.
Specifically, the delayed presentation affects the STEMI pathways in three possible manners:
-
1)
Delayed presentation fundamentally alters a fibrinolytic strategy as the door to needle times (D2N) are significantly prolonged and the benefits associated with early and pre-hospital administration of thrombolytic therapy are reduced
-
2)
The longer time window of opportunity for primary PCI in patients with delayed presentation may be the most effective way to treat many patients with STEMI despite the lack of PCI facilities.
-
3)
Delayed presentation requires a novel look at pharmaco-invasive strategies that may prolong the window of opportunity for reperfusion therapy.
2. Alternate STEMI pathway for low and middle-income countries
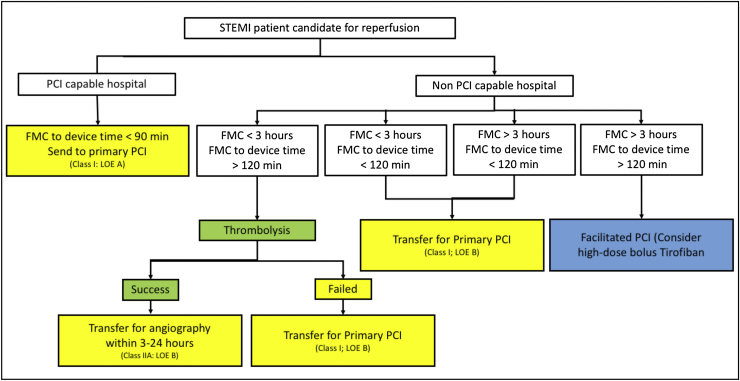
In order to incorporate delayed presentation and lack of STEMI networks, we recommend a new pathway that is pragmatic and efficient and that may be cost-effective (Fig. 2).
Fig. 2.
Alternate Pathway for Developing Countries.
In this methodology, the construct for PCI hospitals remains unchanged. The overwhelming benefits of primary PCI support this recommendation where this modality remains the cornerstone of superior STEMI care. These PCI hospitals need to continually improve the three essential components of a D2B intervention: door to electrocardiogram (ECG) time, ECG to Cardiac Catheterization Laboratory (CCL) time, and CCL Arrival to Device time. As per the guidelines, the over-arching goal remains rapid first medical contact (FMC) to device times.
It is for the care of the majority of patients that present at non-PCI capable hospitals that there are the new considerations in our recommended pathway. To incorporate the delayed presentation and lack of STEMI networks, the non-PCI-Capable hospital pathway utilizes two critical time parameters that differentiate treatment strategies: 1) Symptom onset to first medical contact (FMC), with a cut off of less than 3 h, the time during which thrombolytic therapy is most effective; 2) FMC to device time of 120 min or less, an ACC/AHA Guideline Class I-B recommendation that has been shown to result in excellent outcomes for the transferred STEMI patient. Beyond this logistic difference that is used for triage of STEMI patients at non-PCI-capable hospitals, the practice may alter the use of thrombolytic therapy (due to delayed presentation) and that of GPIIb/IIIa therapy, and in particular high-dose tirofiban (delayed presentation, cost-effectiveness).
2.1. High dose tirofiban
Upfront, high-dose tirofiban presents intriguing possibilities for the pathway with delayed presentation and with long transfer times. The original concept of facilitated PCI involved administration of pharmacotherapy (fibrinolytic agents and/or glycoprotein IIb/IIIa inhibitors) to initiate reperfusion while the patient was en route to the catheterization laboratory. Following ASSENT – 4 PCI and FINESSE trial, the use of glycoprotein inhibitors was largely abandoned.9, 10
More recently, a few events have renewed interest in the use of this therapy. First, a reexamination of previous data, including results of a meta-analysis has exposed several limitations in the analysis. In particular, the studies were not designed to address the optimal strategy in patients with expected delays of greater than 120 min to PCI.11 The authors noted that only a small minority of patients actually fit the target population for which facilitated PCI was designed. Simultaneously, another meta-analysis by Valgimigli et al. showed improved initial patency and ST resolution in patients with upfront IIb/IIIa blockers.12 Recently other studies have suggested a beneficial effect of early initiation of a glycoprotein IIb/IIIa blocker as well. Ortolani and co-workers found that pretreatment with a IIb/IIIa blocker in patients referred to a PCI center was associated with a better clinical outcome.
Higher efficacy of pre-hospital tirofiban with longer pretreatment time to primary PCI may provide protection for the negative impact of time delay.13 Heestermans et al. demonstrated that pre-treatment with tirofiban may compensate for longer time delay to PCI (i.e. >55 mins vs. ≤55 mins). It was also observed that STEMI patients who received early administration of tirofiban had significantly lower mortality than patients who did not. The lower mortality was attributed to increased patency associated with tirofiban. A comparison between upfront high-dose tirofiban versus provisional use in the real world of non-selected STEMI patients undergoing primary PCI was reported from the Zwolle Acute Myocardial Infarction Registry. The experience at this center demonstrated improved ST-segment resolution and subsequent clinical outcome with pre-hospital initiated high dose therapy as compared with provisional tirofiban therapy. In the upfront tirofiban arm, the total ischemia time was >3 h. The Zwolle experience also illustrates that in routine daily practice, delays to reperfusion are longer and consequently pretreatment times, with potent antithrombotic and antiplatelet drugs when given upfront, are longer. The 94 min of pre- treatment time is much longer than the 55 min of pretreatment time seen in the On-TIME 2 trial. The results of this analysis confirm the results of the On-TIME 2 trial which demonstrated improved ST-segment resolution and clinical outcome with prehospital initiated tirofiban therapy on top of dual antiplatelet therapy (aspirin/clopidogrel) as compared with provisional IIb/IIIa therapy.13, [14]
2.2. Reduced dose lytics
Primary PCI has made remarkable progress in the last two decades. Still, fibrinolytic therapy remains the most frequently used method of reperfusion worldwide. This is as result of the majority of patients presenting at non-PCI capable hospitals. In low and middle-income countries, this situation of low use of primary PCI is worsened by delayed presentation and lack of STEMI networks. Larson et al. demonstrated the safety and efficacy of a pharmaco-invasive reperfusion study in rural STEMI patients with expected delays due to long-distance transfers.15 In a recent issue of the Journal of American College of Cardiology (JACC): Cardiovascular Interventions, Rashid et al. presented an analysis from a retrospective registry of 1216 STEMI patients comparing the efficacy and safety of a pharmaco-invasive versus a primary PCI strategy.16 Despite the significantly longer D2B time, there was no difference in the primary composite endpoint (mortality, re-infarction or stroke) which occurred in 6.4% of the pharmaco-invasive group and 7.0% of the primary PCI group. These results are similar to the STREAM (Strategic Reperfusion Early after Myocardial Infarction) trial that also reported no difference in outcome between the two strategies.17
In “The Choice is Reperfusion Therapy, But Which One?” Timothy Henry and Paul Armstrong provided a poignant appraisal.18 They opined that one of the major benefits resulting from modern fibrinolytic therapy is prompt pre-hospital administration removing any door-to-needle delay. When this delay occurs, as it commonly happens in low and middle-income countries, late presenters may expect less benefit from a pharmaco-invasive strategy given the decline of efficacy of fibrinolytics over time.
What is the preferred regimen for a fibrinolytic strategy? The choice of fibrinolytic (full dose or half dose), the best P2Y12 inhibitor and the ideal antithrombin regimen remain uncertain. The most experience is with Tenecteplase and there is some evidence that one half dose may decrease major bleeding – in particular hemorrhagic stroke in the elderly, without a sacrifice in efficacy.
2.3. Choice of high dose bolus tirofiban or half dose lytics?
Even before answering this critical question, two fundamental observations must be made. In every circumstances, short D2N times must remain an absolute goal and non-PCI capable hospitals should have the same mandatory pathways in place to achieve D2N times <30 min, as do PCI-capable hospitals, that must strive to achieve D2B times. Second, as must be evident from the data, no size fits all, and every community should develop a clear strategy of its treatment pathway. For low and middle-income countries, with late presenters and no STEMI networks, Fig. 2 can create an effective STEMI system of care for every community.
Therefore, for the late presenter, what should a community choose – high dose tirofiban or half dose lytic? We feel that the true cut off point is 3 h. Based upon convincing data, these patients will benefit from lytic therapy, particularly, if it is accompanied with D2N time <30 min. As mentioned previously, “no size fits all”, it is better to select HDT if the only lytic available is Streptokinase, on the other hand, half dose TNK is an excellent alternative if no tirofiban is available. Moreover, if transfer for subsequent PCI is not available, then fibrinolytic therapy would be preferred. These decisions should be made upfront such that each hospital has a plan. They are key constituents of a STEMI network in middle and low-income countries.
The alternate STEMI pathway, in summary, makes the following considerations: a) Thrombolysis is recommended for the narrow subset of patients who present very early, have no contraindication to thrombolytic therapy and for whom the FMC to device time exceeds 120 min; b) For even the group of very early presenting patients, with FMC <3 h, but with a proven ability for early transfer and short Door-in/Door-out (DIDO) times, we recommend Primary PCI as the preferred modality; c) High dose tirofiban is recommended to be considered for patients with FMC >3 h and longer transfer times.
We believe our strategy will have the following and noteworthy implications on the care of STEMI patients in low and middle-income countries. It is the expectation of these improvements and a yearning to advance better STEMI care that we deliberated on the strategy of creating the alternate strategy for developing countries.
-
1)
Fewer patients may be treated with fibrinolytic therapy considering a large number of patients that are presently receiving this therapy are presenting late and may not be achieving adequate reperfusion rates with late-administered fibrinolytic therapy. We believe that patients treated with first generation fibrinolytic will comprise the majority of these patients. It appears a superior strategy to transfer for primary PCI, than administer streptokinase, even with modestly longer delays to PCI, for a patient who presents with 8 h of chest pain.
-
2)
Complications, including bleeding, immunologic reactions, stroke and hypotension may be reduced as a result of the above strategy. Once again, this is a particular problem with older generation lytic agents.
-
3)
Costs will be reduced from the use of a single, definitive procedure – several of these agents are fairly expensive, despite the availability of generics.
-
4)
A single, definitive procedure will be implemented for this cohort. Often, several patients in low and middle-income countries have exhausted their financial resources after paying for the thrombolytic therapy and they end up abandoning the follow up coronary angiography and PCI.
-
5)
Costs of PCI hardware have come down strikingly in low and middle-income countries and it is possible to perform extremely cost-effective primary PCI. This provides further rational to expand the use of primary PCI in poor countries.
-
6)
The present strategy of thrombolysis for all patients that have long transfer times, irrespective of their FMC, has lead to the nascent practice of “thrombolysis during the night, PCI during the day”. This pattern is increasingly prevalent at PCI capable hospitals and this is truly unfortunate. In 2016, PCI-capable hospitals have a moral obligation to provide 24/7 primary PCI for all patients that present with STEMI. In addition to being detrimental to patient care, such practices have hampered development of STEMI programs, and of STEMI networks, in developing countries. Such unethical practices also encourage the performance of two expensive treatments for treating STEMI – this is a most dishonorable practice in a cost-constrained environment.
3. System delays – barriers and solutions
Several pioneering studies conducted in India have explored the epidemiology of STEMI. In addition to highlighting the problems of delayed presentation, they reveal several other important features. The CREATE Registry demonstrated that the symptom to hospital time was 6 h and the hospital to needle time was 50 min, with 58% of these patients treated with thrombolysis, and 8% with PCI.19 Mohanan et al. reported in the Kerala ACS Registry, almost identical time to presentation, with a higher proportion of patients (13%) being treated with PCI.20 Two recent ACS studies reveal disconcerting statistics and they also highlighted tremendous regional variations. Negi reported a symptom to presentation time of 13 h with 38.2% patients receiving reperfusion (36% lysis, 2.2% PCI) in the hilly region of Himachal Pradesh (HP). Iqbal, reporting findings from the North East Registry, found symptom to presentation times of 10 h, with 39% treated with lysis and 1.8% with PCI.21, 22 The HP Registry explored the causes of delay, and interestingly found that poor patient education and physician awareness contributed to nearly 80% of delay in presentation, and not travel delay, as would have been expected. In an editorial S Mishra succinctly explained that physician awareness is a very important variable of health-care delivery.23 These recent registries bring out an important clue, that while socio-economic status does play a role but the effect is perhaps not as pronounced as that of physician awareness. Comparing the data available from the affluent and educated parts of India (CREATE and Kerala Registry) with the less developed regions reported by Negi and Iqbal, there seems to be a huge discordance. It seems that within the same state (India) there are two different countries, divided not by economy but by educational status. Thus among other initiatives another need of the hour is a Physician Awareness Program so that they can be made aware of state of art regimens and adhere to guidelines.
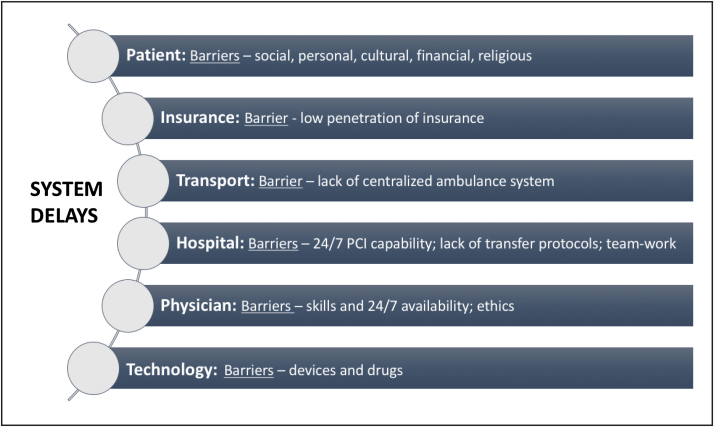
With respect to the critical aspect of reducing system delays, Fig. 3 depicts our compilation of six aspects that we believe cause process and procedural delays in most low and middle-income countries. Some of the specific barriers that cause delays are also listed. Between the process and the procedure, indisputably it is process delays that largely affect all the three parameters of D2N, D2B and Door In Door Out (DIDO) times. So far as solutions are concerned to reduce system delays, there is considerable regional variation. Beyond these provincial differences, our 10 top strategies to reduce system delays are the following:
-
1.
Treat STEMI Interventions as a public health initiative in which there are numerous stakeholders that can be engaged to seek financial, logistic, structural and medical support.
-
2.
Improve ambulance care, qualitatively and quantitatively, with the goal being to ensure a centralized, intelligent ambulance system, both for community emergency response and for inter-hospital transfers.
-
3.
Increase 24/7 STEMI facilities, including the ability to perform primary PCI with or without the capability for on site cardiac surgery.
-
4.
Create regional STEMI networks and systems of care for each community with a reperfusion protocol for every hospital.
-
5.
Develop prehospital alert whenever possible and ECG transmission using Internet, Fax, or smartphone applications such as WhatsApp.
-
6.
Establish unambiguous payment policies and systems that are clearly understood by payers, hospital and patient. Payment delays notoriously cause delays in obtaining consents. Penalize refusal to provide life-saving STEMI care.
-
7.
Use single call activation to engage the catheterization laboratory, with team work and quality improvement (QI) feedback.
-
8.
Bypass the ED, when possible, relying on pre-hospital alert and single call activation
-
9.
Consider telemedicine to increase access, accuracy and remote guidance of comprehensive STEMI management.24, 25
-
10.
Educate the patient – this is the hardest assignment and it requires a multi-pronged approach, including empowering the general physician.
Fig. 3.
System Delays in Developing Countries.
4. Conclusions
STEMI care is challenging in low and middle-income countries because of resource constraints, delayed patient presentation, and system delays. Late presentation and lack of STEMI networks make management more problematic. There are no clear guidelines to optimally care for these patients given these deficiencies. We propose a novel STEMI pathway for these late presenting patients that reconfigures the management strategies at non-PCI capable hospitals by incorporating a 3-h symptom duration as cutoff to use reduced dose lytics (with short D2N times) or to consider high dose tirofiban.
System delays in STEMI care have multiple triggers and regional barriers. We present a multi-pronged approach to overcome these glitches.
Conflicts of interest
None.
References
- 1.Antman E.M., Anbe D.T. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction) J Am Coll Cardiol. 2004;44(3):E1–E211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 2.Kaifoszova Z., Kala P., Wijns W. The stent for life initiative: quo vadis? EuroIntervention. 2016;12(May (1)):14–17. doi: 10.4244/EIJV12I1A3. [DOI] [PubMed] [Google Scholar]
- 3.Jollis J.G., Granger C.B., Henry T.D. Systems of care for ST-segment-elevation myocardial infarction: a report from the American Heart Association’s Mission: lifeline. Cir Cardiovasc Qual Outcomes. 2012;5(4):423–428. doi: 10.1161/CIRCOUTCOMES.111.964668. [DOI] [PubMed] [Google Scholar]
- 4.Jacobs A.K., Antman E.M., Faxon D.P. Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation. 2007;116(2):217–230. doi: 10.1161/CIRCULATIONAHA.107.184043. [DOI] [PubMed] [Google Scholar]
- 5.Krumholz H.M., Bradley E.H., Nallamothu B.K. A campaign to improve the timeliness of primary percutaneous coronary intervention: door-to-balloon: an alliance for quality. JACC Cardiovasc Interv. 2008;1:97–104. doi: 10.1016/j.jcin.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg R.J., Spencer F.A., Fox K.A.A. Prehospital delay in patients with acute coronary syndromes (from the Global Registry of Acute Coronary Events [GRACE]) Am J Cardiol. 2009;103:598–603. doi: 10.1016/j.amjcard.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 7.Alexander T., Mullasari A.S., Kaifoszova Z. Framework for a national STEMI program: consensus document developed by STEMI INDIA, cardiological society of india and association physicians of India. Indian Heart J. 2015;67(5):497–502. doi: 10.1016/j.ihj.2015.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Larson D.M., McKavanagh P., Henry T.D., Cantor W. Reperfusion options for STEMI patients with expected delays to PCI. Interv Cardiol Clin. 2016;5(4):439–450. doi: 10.1016/j.iccl.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 9.Ellis S.G., Armstrong P., Betriu A. Facilitated percutaneous coronary intervention versus primary percutaneous coronary intervention: design and rationale of the Facilitated Intervention with Enhanced Reperfusion Speed to Stop Events (FINESSE) trial. Am Heart J. 2004;147:E16. doi: 10.1016/j.ahj.2003.07.025. [DOI] [PubMed] [Google Scholar]
- 10.Primary versus tenecteplase-facilitated percutaneous coronary intervention in patients with ST-segment elevation acute myocardial infarction (ASSENT-4 PCI): randomized trial. Lancet. 2006;367:569–578. doi: 10.1016/S0140-6736(06)68147-6. [DOI] [PubMed] [Google Scholar]
- 11.Keeley E.V., Boura J.A., Grines C.L. Comparison of primary and facilitated percutaneous coronary interventions for ST-elevation myocardial infarction: quantitative review of randomized trials. Lancet. 2006;367(9510):579–588. doi: 10.1016/S0140-6736(06)68148-8. [DOI] [PubMed] [Google Scholar]
- 12.Valgimigli M., Biondi-Zoccai G. Tirofiban as adjunctive therapy for acute coronary syndromes and percutaneous coronary intervention: a meta-analysis of randomized trials. Eur Heart J. 2010;31:35–49. doi: 10.1093/eurheartj/ehp376. [DOI] [PubMed] [Google Scholar]
- 13.Ten Berg J.M., Van’t Hof A.W. Effect of early, pre-hospital initiation of high bolus dose tirofiban in patients with ST-segment elevation myocardial infarction on short- and long-term clinical outcome. JACC. 2010;55(2) doi: 10.1016/j.jacc.2009.11.091. [DOI] [PubMed] [Google Scholar]
- 14.Heestermans Higher efficacy of pre-hospital tirofiban with longer pretreatment time to primary PCI: protection for the negative impact of time delay. EuroIntervention. 2011;7:442–448. doi: 10.4244/EIJV7I4A73. [DOI] [PubMed] [Google Scholar]
- 15.Larson D.M., Duval S., Sharkey S.W. Safety and efficacy of a pharmaco-invasive reperfusion strategy in rural ST-elevation myocardial infarction patients with expected delays due to long distance transfers. Eur Heart J. 2012;33(May (10)):1232–1240. doi: 10.1093/eurheartj/ehr403. [DOI] [PubMed] [Google Scholar]
- 16.Rashid M.K., Guron N., Bernick J. Safety and efficacy of a pharmacoinvasive strategy in ST-segment elevation myocardial infarction: a patient population study comparing a pharmacoinvasive strategy with a primary percutaneous coronary intervention strategy within a regional system. J Am Coll Cardiol Interv. 2016;9:2014–2020. doi: 10.1016/j.jcin.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Sinnaeve P.R., Armstrong P.W. ST-segment-elevation myocardial infarction patients randomized to a pharmaco-invasive strategy or primary percutaneous intervention: strategic reperfusion early after myocardial infarction (STREAM) 1 year mortality follow-up. Circulation. 2014;130(14):1139–1145. doi: 10.1161/CIRCULATIONAHA.114.009570. [DOI] [PubMed] [Google Scholar]
- 18.Henry D., Armstrong P. The choice is reperfusion therapy but which one? J Am Coll Cardiol Interv. 2016;9(19):2021–2023. doi: 10.1016/j.jcin.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 19.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371(April (9622)):1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 20.Mohanan P.P., Mathews S., Harikrishnana Presentation, Management, and outcomes of 25748 acute coronary syndrome admissions in Kerala, India: results from Kerala ACS registry. Eur Heart J. 2013;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Negi C.P., Merwaha P. Multicenter HP ACS registry. Indian Heart J. 2016;68(2):118–127. doi: 10.1016/j.ihj.2015.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iqbal F., Barkataki J.C. Spectrum of acute coronary syndrome in North Eastern India–a study from a major center. Indian Heart J. 2016;68(2):128–131. doi: 10.1016/j.ihj.2015.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mishra M. Do medical conferences have a role to play? Sharpen the saw. Indian Heart J. 2016;68(2):111–113. doi: 10.1016/j.ihj.2016.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehta S., Reynbakh O., Kostela J.C. Building population-based AMI management systems using telemedicine as a foundation pillar. Eur Heart J. 2014;35:1172–1176. [Google Scholar]
- 25.Mehta S., Botelho R., Rodriguez D. A tale of two cities: STEMI interventions in developed and developing countries and the potential of telemedicine to reduce disparities in care. J Interv Cardiol. 2014;27(2):155–166. doi: 10.1111/joic.12117. [DOI] [PubMed] [Google Scholar]