Abstract
Background and objective
Ischemic heart disease is the leading cause of death in India. In high-income countries, pre-hospital systems of care have been developed to manage acute manifestations of ischemic heart disease, such as acute coronary syndrome (ACS). However, it is unknown whether guidelines, policies, regulations, or laws exist to guide pre-hospital ACS care in India. We undertook a nation-wide document analysis to address this gap in knowledge.
Methods and results
From November 2014 to May 2016, we searched for publicly available emergency care guidelines and legislation addressing pre-hospital ACS care in all 29 Indian states and 7 Union Territories via Internet search and direct correspondence. We found two documents addressing pre-hospital ACS care.
Conclusion
Though India has legislation mandating acute care for emergencies such as trauma, regulations or laws to guide pre-hospital ACS care are largely absent. Policy makers urgently need to develop comprehensive, multi-stakeholder policies for pre-hospital emergency cardiovascular care in India.
Keywords: Acute coronary syndromes, Pre-hospital, Guidelines, Healthcare infrastructure, Emergency
1. Introduction
Cardiovascular disease (CVD) is the number one cause of death in India and accounted for approximately 21% of deaths in 2010, with 11% of all deaths due to ischemic heart disease.1 A frequent, acute manifestation of ischemic heart disease is acute coronary syndrome (ACS), which includes ST-segment elevation myocardial infarction (STEMI), non-ST-segment elevation myocardial infarction (NSTEMI), and unstable angina. Deaths due to acute coronary syndromes often occur suddenly and outside of the hospital setting. In high-income countries, short-term case fatality rates for acute coronary syndromes, including acute myocardial infarction, have fallen dramatically from approximately 25% in the early 1980s to as low as 4% in the current era, due at least in part to a combination of medical therapy, reperfusion, and better overall intensive care, including availability of defibrillation.2, 3, 4, 5 However, treatment of patients with acute coronary syndromes in India is highly variable and often suboptimal,6 with increased symptom-to-presentation (pain-to-door) times and increased presentation-to-treatment (door-to-drug) times compared to high-income countries.7
Early recognition of acute coronary syndrome symptoms by patients through public education campaigns and use of emergency medical services have been demonstrated to be effective ways to reduce time to first medical contact in patients with acute coronary syndrome. A 2014 study in Dublin, Ireland showed that among acute coronary syndrome patients, two individualized educational sessions compared with no educational sessions reduced patient-level symptom-to-first medical contact delays (1.7 vs. 7.1 h, p < 0.001).8 Use of a pre-hospital electrocardiogram (ECG) has also been associated with reduced pre-hospital delay time, increased use of reperfusion interventions, earlier diagnosis, and faster time to treatment.9 In England and Wales, analysis of a large national registry including nearly 290,000 patients with acute myocardial infarction demonstrated that a pre-hospital ECG was associated with more timely initiation of reperfusion and lower 30-day mortality rates (7.4% vs. 8.2%, adjusted OR 0.94, 95% CI 0.91–0.96) compared to those who did not have a pre-hospital ECG.10 Thus, a combination of public education, increased use of emergency medical services, expeditious arrival at an equipped medical facility, and initiation of diagnostic and therapeutic measures in the pre-hospital setting improve outcomes in patients with acute coronary syndromes.
Despite the potential utility of these individual interventions, it is unclear if there are local, regional, or national guidelines, policies, regulations, or laws in place to guide pre-hospital acute coronary syndrome care in many low- and middle-income countries, including India. 80% of CVD-related deaths, including those due to ischemic heart disease and stroke, occur in low- and middle-income countries (LMICs),1 and this number is projected to rise so that if current trends continue to the year 2030, then 85% of cardiovascular disease-related deaths will occur in LMICs.11, 12 Given the sheer number of lives lost in India due to CVD, there is a pressing need to understand the current state of the Indian health system, particularly for the World Health Organization (WHO) to reach its goal of reducing the risk of premature mortality related to noncommunicable diseases (NCDs) by 25% by the year 2025.13
The WHO describes health systems framework in terms of six “building blocks”: service delivery, health workforce, information, medicines, financing and governance.14 In recent years, the Government of India has begun to address these “blocks” through the formation of the National Rural Health Mission, National Urban Health Mission, and the development of government-sponsored insurance schemes for individuals who live below the poverty line.15 Furthermore, the establishment of laws requiring the emergency medical treatment of patients suffering trauma as a result of motor vehicle accidents16 sets a precedent that could potentially be extended to individuals suffering from other acutely life-threatening conditions, like acute coronary syndromes. The implementation of pre-hospital acute coronary syndrome policies through these avenues may be important to ensure equitable and accessible emergency care, taking into account potential barriers to emergency care, including infrastructure and cost. A nation-wide documentary analysis of pre-hospital acute coronary syndromes systems of care policies was undertaken to address this existing gap in knowledge.
2. Objectives
-
1.
To assess the presence of and describe any central government or any Indian state and Union Territory published guideline, policy, regulation, or law for emergency, pre-hospital acute coronary syndrome care.
-
2.
To analyze the content of the existing policies for pre-hospital acute coronary syndrome care and compare to existing established recommendations by the WHO and international cardiovascular professional societies, such as the European Society of Cardiology, American College of Cardiology, or American Heart Association (Fig. 1, Fig. 2).17, 18
Fig. 1.
2012 ESC Prehospital and In-hospital Guideline to the management of ST-elevation myocardial infarction.
Fig. 2.
2013 ACCF/AHA Guideline for the management of ST-elevation myocardial infarction. Reperfusion therapy for patients with STEMI. The bold arrows and boxes are the preferred strategies. Performance of PCI is dictated by an anatomically appropriate culprit stenosis. *Patients with cardiogenic shock or severe heart failure initially seen at a non-PCI capable hospital should be transferred for cardiac catheterization and revascularization as soon as possible, irrespective of time delay from MI onset (Class I, LOE: B). †Angiography and revascularization should not be performed within the first 2–3 h after administration of fibrinolytic therapy. CABG indicates coronary artery bypass graft; DIDO, door-in–door-out; FMC, first medical contact; LOE, Level of Evidence; MI, myocardial infarction; PCI, percutaneous coronary intervention; and STEMI, ST-elevation myocardial infarction.
3. Methods
3.1. Design
We attempted to conduct a policy document analysis of publicly available pre-hospital acute coronary syndrome care guidelines, policies, regulations, or laws. One author with expertise in library science (MB) developed the search strategies and conducted searches of the health department websites for all Indian states (n = 29) and Union Territories (UT, n = 7) using the search terms “acute coronary”, “heart attack”, and “infarction”. We also searched the websites of the Cardiological Society of India and the Indian College of Cardiology. Because 29 of the 44 websites investigated offered limited or no search functionality, we also browsed the websites and used Google site search for all the websites (e.g., “acute coronary” OR “heart attack” OR infarction site: http://www.accindia.org/). In addition, we searched the Legal Information Institute of India and India Code websites using the search terms “emergency care” OR “emergency department” OR “emergency room” OR “pre-hospital” OR “pre hospital” OR “acute coronary” OR “heart attack” OR infarction, in an attempt to locate legislation. See Appendix 1 for a full list of websites and search strategies. All hits were screened for potential relevance. When unable to retrieve a policy through the initial website searches, we sent an official email requesting the policy documents that are relevant to this study from Northwestern University and the Centre for Chronic Disease Control to respective parties as outlined above (N = 37). If we did not find any official documents after the performance of these steps, then we documented the state or UT as not having publicly available policies. We registered our protocol, including our search strategy, though PROSPERO (http://www.crd.york.ac.uk/PROSPERO/; registration no. CRD42015016439) and performed our search from November 2014 to May 2016. We complemented our document search by seeking input from local, regional, and national experts.
3.1.1. Inclusion criteria
We used the following inclusion criteria:
-
-
Officially approved guideline, policy, regulation, or law published by a public health or cardiovascular organization.
-
-
Publicly available document.
-
-
Be related to pre-hospital or early hospital (emergency) acute coronary syndrome care through local, state-level, or national-level guidelines, policies, regulations, or laws.
-
-
Published in English or any official Indian language.
The definitions of policy, guideline, action plan, program, regulation, and law vary in the literature and among the local, statewide, or territory-wide documents. In this analysis, we planned to include all documents that include the objectives and guidelines for action in the domain of pre-hospital acute coronary syndrome care. We planned to retrieve all pre-hospital acute coronary syndrome policies that were publicly available for each state or UT that were related to the following key concepts:
-
-
Acute coronary syndromes (ACS).
-
-
Pre-hospital care (including emergency care).
3.1.2. Methods for comparative analysis
State and UT policies eligible for the study were to be analyzed as follows using previously described methods19:
-
1.
Data coding
We planned to divide and assign categories to data in the policy documents. Two researchers (AP, MDH) planned to code these documents to minimize subjective coding results. For this study, we planned to code the contents of the eligible policy documents in two phases:-
•Phase 1: Keyword codingWe planned to scan policy documents for pre-identified keywords that are relevant to the study objectives (Table 1). We would choose the keywords based on the elements that are deemed to be important in the framework of a policy document with focus on the diagnosis and management of patients with acute coronary syndrome in the pre-hospital setting. The coding would be done using Dedoose data analysis software v4.12 (Manhattan Beach, USA).
-
•Phase 2: Assessment of coded text in phase 1After coding the documents in phase 1, we planned to assess the text retrieved in the process to determine the context in which the keyword was used and whether or not it corresponded to a pre-hospital system of care component within the policy. We planned to code the text using Dedoose to identify and name the different components of the policy in which the keywords were found. We would then merge these free nodes into the following tree nodes:
-
•Background: the text gives an introduction, context or background for the policy.
-
•Axis: the text describes the principles that determined the content of the policy.
-
•Objectives: the text states the aims, goals, vision, expected outcomes, and/or objectives of the policy.
-
•Strategies: the text describes the different strategies described in the policy to achieve other professional cardiology society recommendations. Actions, participating stakeholders, and law production are included in this category.
-
•Other context: text was included here when the keywords were used in a context other than the systems for pre-hospital acute coronary syndrome care.
-
•
-
•
-
2.
Mapping of policy availability of the States and Union Territories
This step is related with study objective 1. For this purpose, we planned to construct a consolidated policy database containing all the eligible policy documents and a produce a map. This map would provide an overview of availability of a regional policy on pre-hospital acute coronary syndrome care published by any Indian state or UT.
-
3.
Analysis of eligible policy documents with established pre-hospital emergency acute coronary syndrome care recommendations by public health and international cardiovascular societies organizations
This step is related with study objective 2. We planned to construct a table to assist the comparison and analysis purposes. This table would be constructed with the data sourced from the coded eligible documents.
Table 1.
Guideline for keywords used for phase 1 coding.
| Keyword | Dedoose query |
|---|---|
| Acute coronary syndrome | acute coronary syndrome OR ACS |
| Analgesic | analgesic |
| Antiplatelet | antiplatelet |
| Ambulance | ambulance |
| Aspirin | aspirin |
| Beta blocker | beta blocker |
| Clopidogrel | clopidogrel |
| Defibrillator | defibrillator OR AED |
| Electrocardiogram | electrocardiogram OR ECG OR EKG |
| Emergency | emergency |
| Medication | medication OR medicine |
| Nitroglycerin | nitroglycerin |
| Non-ST segment elevation myocardial infarction | non-ST segment elevation myocardial infarction OR NSTEMI |
| Oxygen | oxygen |
| Paramedic | paramedic |
| Payment | payment |
| Policy | policy or policies |
| Pre-hospital | pre-hospital |
| ST segment elevation myocardial infarction | ST segment elevation myocardial infarction OR STEMI |
| Telemetry | telemetry OR cardiac monitoring |
| Thrombolysis/fibrinolysis | thrombolysis OR thrombolytic OR fibrinolysis OR fibrinolytic |
| Unstable angina | unstable angina |
3.2. Ethical considerations
Because all information used for this report lie in the public domain, we received an Institutional Review Board exemption from Northwestern University. The Northwestern University Institutional Review Board approved the request of information letter that was sent to each office or organization if the initial Internet search yielded no results.
4. Results
4.1. Website searches
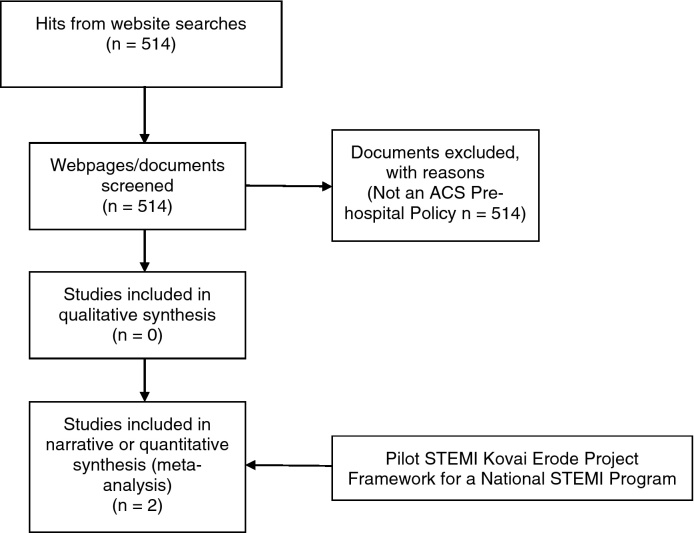
The website searches returned 514 hits, but no results contained pre-hospital acute coronary syndrome policies from any of the 29 Indian states or 7 UTs. Additionally, the two major Indian cardiology professional organizations (the Cardiological Society of India and the Indian College of Cardiology) had no published pre-hospital acute coronary syndrome policies available on their websites (Fig. 3).
Fig. 3.
Flow of information through different phases of our policy document analysis.
4.2. Request of information letters
Because we found no results during our initial Internet search, we sent emails to each state and UT Director of the National Rural Health Mission requesting information on pre-hospital acute coronary syndrome policies in their respective states (N = 36). We received responses from three states (response rate = 8%). An email response was received from the state of Uttarakhand, stating it has no pre-hospital acute coronary syndrome policy in place and from the state of Karnataka, saying that it follows the Stanford Emergency Medicine guidelines for pre-hospital care. A published copy of these guidelines was provided on request, and the algorithm that is used for emergency evaluation of chest pain is shown in Fig. 4. A phone call was received from the state of Punjab, also stating that they have no pre-hospital acute coronary syndrome policies in place. No response was received from the remaining states and UTs.
Fig. 4.
Chest pain protocol used by the Indian state of Karnataka for emergency acute coronary syndrome care (GVK Emergency Management and Research Institute, 2012).
Request of information letters were also sent to two major cardiology professional organizations of India, the Cardiological Society of India and the Indian College of Cardiology, but no response was received to indicate evidence of published pre-hospital acute coronary syndrome guidelines by either organization. However, the Cardiological Society of India is currently in the process of writing a consensus statement on pre-hospital acute coronary syndrome systems of care.
Through our search of gray or unpublished literature and experts, we sent an email invitation requesting information from the director of a regional ST-elevation myocardial infarction system of care in Tamil Nadu, Dr. Thomas Alexander. Dr. Alexander is also co-founder of STEMI India, a non-governmental organization with the goal of improving ST-elevation myocardial infarction care by developing locally collaborative systems of care.20 To aid our search, Dr. Alexander shared a consensus statement published in 2013 by the Association of Physicians of India in collaboration with STEMI India that recommends the use of a pharmaco-invasive approach to STEMI treatment (i.e., administration of fibrinolytics agents followed by percutaneous coronary intervention) in areas where the facilities or resources for primary percutaneous coronary intervention are not readily available.21 Based on this work, an additional consensus statement was published in September 2015, outlining the partners, management, and infrastructure needed to implement a STEMI system of care in India.22
Further communications allowed us to find information on the protocol for the pilot STEMI Kovai Erode Project, a regional ST-elevation myocardial infarction (STEMI) model of care in India. The project is a collaboration between STEMI India, private technology partners, an ambulance network, and the state government of Tamil Nadu. The Pilot STEMI Kovai Erode Project was instituted in Erode district in the south Indian state of Tamil Nadu in 2010.23 In 2010, Erode district had only one hospital with a cardiac catheterization lab. This hospital was designated as the hub hospital to a network of several smaller referral hospitals in the district. Patients with ST-elevation myocardial infarction were treated either with primary percutaneous coronary intervention or a pharmaco-invasive approach based on their distance from the hub hospital on presentation. Eighty-four patients received care under this model from May 2010 to December 2010. The mean time of arrival from symptom onset was 170 min with 77% of patients arriving by ambulance (transport time: 5–99 min; mean: 44 min).23 The mean time to percutaneous coronary intervention after fibrinolytic therapy in the pharmaco-invasive strategy was 480 min compared with 69 min from the first medical contact to percutaneous coronary intervention in patients undergoing primary percutaneous coronary intervention.23 Plans are underway to expand the program to the entire state of Tamil Nadu with the primary objective of reducing time from first medical contact to reperfusion in patients with ST-elevation myocardial infarction.
Finally, again through email communication with an expert, we found two documents, the “Guidelines for the Management of Cardiovascular Diseases” published by the Government of India, Ministry of Health and Family Welfare, and the “Clinical Management Guidelines for Coronary Artery Disease for National Programme for Prevention and Control of Diabetes, Cardiovascular Disease and Stroke”, published by the Post-Graduate Institute of Medical Education and Research. These documents do not address pre-hospital acute coronary syndrome care specifically, but do recommend that the facility to perform an electrocardiogram be available at the primary healthcare level as a standard of care.24, 25
5. Discussion
5.1. Summary of findings
In this policy document analysis of pre-hospital acute coronary syndrome systems of care, we found no guidelines, policies, regulations, or laws specifically guiding pre-hospital acute coronary syndrome care by government offices or cardiology professional organizations in India, aside from the Association of Physicians of India document. The only information found in our review was not readily accessible and was primarily obtained through targeted personal communication with research contacts. This dearth of systematic guidelines, policies, regulations, or laws in India pertaining to emergency acute coronary syndrome care is concerning given the country's epidemic proportions of ischemic heart disease, the prohibitively high cost of procedures and medications for a large portion of the population, and the presence of disparities in equitable access to healthcare services based on socioeconomic status.23 Similar concerns exist for pre-hospital care for patients with acute strokes as well.26
The only formal model of pre-hospital acute coronary syndrome care our search yielded was the Pilot STEMI Kovai Erode Project. This project was established by STEMI India in collaboration with partners in the private and public sectors, and incorporates a number of factors that have been crucial to its initial success. These factors include the establishment of a hub-and-spoke model of care, the use of standardized treatment protocols, and the leveraging of recent developments of emergency medical service systems and social insurance programs within Tamil Nadu. The integration of each of these components requires a collaborative effort and investment from a multitude of stakeholders. If pre-hospital systems of care for acute coronary syndromes were implemented within and across other Indian states, then a similar infrastructure, which takes into account the individualized resources of the specific region, may facilitate more optimal delivery of services to the population.23, 27
5.2. Policies/laws addressing other emergencies in India
While there are no guidelines, policies, regulations, or laws pertaining specifically to pre-hospital acute coronary syndrome care in India, aside from the Association of Physicians of India statement, the Law Commission of India, an executive central government body that works for legal reform, issued a report in 2006 that aimed to mandate emergency care be given to victims of accidents, during emergency medical conditions, and women under labor.28 The report states that a patient should not be refused care for an accident or an emergency condition if he/she is not able to pay immediately or if he/she has no medical insurance or other reimbursement facilities. The determination of what is defined as an emergency condition is left to the evaluating clinician. If care is refused without justifiable reason, then the report proposes penalties as follows: (1) for any person responsible for management of a hospital, medical practitioner, or ambulance company that refuses care, imprisonment for a period which may extend up to six months and a fine which may extend up to Rs. 10,000 (approximately USD $150), (2) for a hospital refusing to provide care, suspension or cancelation of any of its licenses in addition to the aforementioned penalty, which may be imposed on the persons owning or managing the hospital, and (3) for any medical practitioner attached to a hospital, in addition to imprisonment and fines already mentioned, the practitioner will be subject to such disciplinary action as may be determined by the State Medical Council.28 The delineation of these penalties are drawn from the Indian Motor Vehicles Act of 1988, which states that if a registered medical practitioner or doctor does not immediately attend to the victim of a motor vehicle accident and render medical aid or treatment, then he/she “shall be punishable with imprisonment for a term which may extend to three months, or with [a fine] which may extent to Rs. 500 (approximately USD $8) or with both.”
The Law Commission's Draft Model Law on Emergency Medical Care to Victims of Accidents and During Emergency Medical Condition and Women Under Labour was reviewed by the Board of Governors of the Medical Council of India in September 2012 and, after consulting physician associations, doctors, and state governments, the model law was fully backed by the Medical Council in December 2012. However, despite this endorsement, each individual state was left to bear the responsibility of developing a framework to provide such emergency care and compensate private hospitals and doctors. As our search has demonstrated, the creation and implementation of such health services delivery arrangements has not yet come to fruition. In India, with regard to acute coronary syndrome care in particular, limited staff, such as cardiologists; resources, such as electrocardiogram machines and reliable transportation; and facilities, such as coronary care units and cardiac catheterization laboratories hinder, but do not prohibit, the application of this law for patients requiring emergency cardiovascular care.
5.3. Comparison with policies/laws for pre-hospital emergency care in other countries
The European community has long acknowledged the fundamental right to health care services through the European Social Charter of 1961.29 European legislation addressing the right to health services dates at least as far back as 19th century Germany,30, 31 while legislation pertaining specifically to emergency medical services is a more recent development, with the majority of European Union states enacting emergency medical services legislation in the 1990s and 2000s.32
In 1986, the United States Congress passed the Emergency Medical Treatment and Active Labor Act (EMTALA) as part of the Consolidated Omnibus Budget Reconciliation Act. EMTALA requires hospitals that accept payments from the Centers for Medicare and Medicaid Services (CMS) to provide emergency medical treatment to anyone who needs it, regardless of citizenship, legal status, or ability to pay.33 There are no reimbursement provisions included in the legislation, which also states that participating hospitals may not transfer or discharge patients needing emergency treatment except with the informed consent or stabilization of the patient or when their condition requires transfer to a hospital better equipped to administer the treatment.33 In 2003, CMS published its “Final Rule” regarding EMTALA, stating that hospitals with emergency departments are not required to guarantee specialist coverage at all times after many community hospitals had reported difficulty in providing such coverage.34, 35
Because EMTALA applies to all hospitals in the United States that accept payments from CMS, the implementation of a similar law in India, where there is a lack of widespread government insurance programs, may not be translatable. Virtually all hospitals in the United States accept CMS reimbursements. However, in India most healthcare services, providers, and hospitals are positioned in the private sector. The majority of India's population avails healthcare services either exclusively from private sources or from a combination of private and public sources: less than 3% of the population from either urban or rural areas utilizes exclusively public government-funded care.36 Services provided by private hospitals are typically paid for by patients out-of-pocket37 or, less often, by private insurance schemes.38, 39 Thus, because the vast majority of the Indians are at least partial consumers of predominantly private healthcare services, applying government rules and regulations to private hospitals may be less enforceable. However, to ensure equitable access to standard-of-care management for all individuals with acute coronary syndromes in India, invoking regulations like those outlined in EMTALA, may prove beneficial.
5.4. Strengths and limitations
Our analysis has both strengths and limitations. Our findings comprise the first ever nation-wide policy document analysis of pre-hospital acute coronary syndrome policies in India. We hope that the paucity of results to address this major public health problem spurs state and central governments and public health and cardiovascular professional organizations to collaborate and develop guidelines, policies, regulations, or laws to deliver equitable pre-hospital acute coronary syndrome care.
Though novel, our study also has limitations. First, our search methods may have failed to identify all existing pre-hospital acute coronary syndrome policies. Of the websites investigated, 29 of 44 had either no or limited search capabilities. Further, the impermanent nature of these websites calls into question the reproducibility the searches. Though our protocol of Internet searches followed up with targeted letters to request information included key stakeholders we believed to be involved in pre-hospital acute coronary syndrome healthcare delivery and guideline development, any policies, guidelines, regulation or laws at the local level could have been potentially missed. The pertinent information we gathered was obtained through personal communication with thought leaders in the field of pre-hospital acute coronary syndrome care, though this strategy was not included in our initial search protocol. Second, the response rate to individualized emails sent to directors of the National Rural Health Mission of each state and UT was low, introducing the possibility of reporting bias. Third, contact was made with government offices electronically, under the assumption that each state and UT would have Internet access. Finally, the consensus statement addressing pre-hospital acute coronary syndrome systems of care by the Cardiological Society of India will be published in the near future, but the contents of that statement were unavailable to include in this analysis.
6. Conclusion
In conclusion, this nation-wide policy document analysis of pre-hospital acute coronary syndrome guidelines, policies, regulations, and laws is the first ever of its kind. Our methods can be applied for similar document analyses in other low- and middle-income countries. Further, though no state- or nation-wide guidelines, policies, regulations, or laws were found addressing pre-hospital acute coronary syndrome care, our search provides useful insights when considering strategies to create organized frameworks for the optimal delivery of acute cardiovascular care in the future. Successful pilot projects confirm that for pre-hospital acute coronary syndrome care to be successful, a strong partnership is essential among all stakeholders, including state government authorities, ambulance networks, cardiology professional organizations, and the general public. Using a multi-pronged, interdisciplinary approach that incorporates these key players is most likely to result in a system that allows for the equitable and optimal delivery of care.
Conflicts of interest
The authors have none to declare.
Acknowledgements
This work was supported by the National Institutes of Health/National Heart, Lung, and Blood Institute through the Fogarty International Clinical Research Scholars and Fellows Program at Vanderbilt University (R24 TW007988) and the American Recovery and Reinvestment Act.
Footnotes
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.ihj.2016.06.012.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Lozano R., Naghavi M., Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study. Lancet. 2010 doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gillum R.F. Trends in acute myocardial infarction and coronary heart disease death in the United States. J Am Coll Cardiol. 1994;23(6):1273–1277. doi: 10.1016/0735-1097(94)90367-0. [DOI] [PubMed] [Google Scholar]
- 3.Krumholz H.M., Normand S.-L.T., Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation. 2014;130(12):966–975. doi: 10.1161/CIRCULATIONAHA.113.007787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flynn A., Moscucci M., Share D. Trends in door-to-balloon time and mortality in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Arch Intern Med. 2010;170(20):1842–1849. doi: 10.1001/archinternmed.2010.381. [DOI] [PubMed] [Google Scholar]
- 5.de Vreede J.J., Gorgels A.P., Verstraaten G.M. Did prognosis after acute myocardial infarction change during the past 30 years? A meta-analysis. J Am Coll Cardiol. 1991;18(3):698–706. doi: 10.1016/0735-1097(91)90792-8. [DOI] [PubMed] [Google Scholar]
- 6.Huffman M.D., Prabhakaran D., Abraham A.K. Optimal in-hospital and discharge medical therapy in acute coronary syndromes in Kerala: results from the Kerala acute coronary syndrome registry. Circ Cardiovasc Qual Outcomes. 2013;6(4):436–443. doi: 10.1161/CIRCOUTCOMES.113.000189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karthikeyan G., Xavier D., Prabhakaran D. Perspectives on the management of coronary artery disease in India. Heart (British Cardiac Society) 2007;93(11):1334–1338. doi: 10.1136/hrt.2007.131193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mooney M., McKee G., Fealy G. A randomized controlled trial to reduce prehospital delay time in patients with acute coronary syndrome (ACS) J Emerg Med. 2014;46(4):495–506. doi: 10.1016/j.jemermed.2013.08.114. [DOI] [PubMed] [Google Scholar]
- 9.Zègre Hemsey J.K., Drew B.J. Prehospital electrocardiography: a review of the literature. J Emerg Nurs. 2012;38(1):9–14. doi: 10.1016/j.jen.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quinn T., Johnsen S., Gale C.P. Effects of prehospital 12-lead ECG on processes of care and mortality in acute coronary syndrome: a linked cohort study from the Myocardial Ischaemia National Audit Project. Heart (British Cardiac Society) 2014;100(12):944–950. doi: 10.1136/heartjnl-2013-304599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joshi R., Jan S., Wu Y. Global inequalities in access to cardiovascular health care: our greatest challenge. J Am Coll Cardiol. 2008;52(23):1817–1825. doi: 10.1016/j.jacc.2008.08.049. [DOI] [PubMed] [Google Scholar]
- 12.Mathers C.D., Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. WHO Member States Make Progress on Noncommunicable Diseases. WHO. http://www.who.int/mediacentre/news/notes/2012/ncd_20121109/en/.
- 14.WPRO. The WHO Health Systems Framework. WPRO. http://www.wpro.who.int/health_services/health_systems_framework/en/.
- 15.Virk A.K., Atun R. Towards universal health coverage in India: a historical examination of the genesis of Rashtriya Swasthya Bima Yojana – the health insurance scheme for low-income groups. Public Health. 2015;129(6):810–817. doi: 10.1016/j.puhe.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 16.The Motor Vehicles Act, 1988. http://www.tn.gov.in/sta/Mvact1988.pdf.
- 17.Steg P.G., James S.K., Atar D. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33(20):2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 18.O’Gara P.T., Kushner F.G., Ascheim D.D. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78–e140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 19.Lachat C., Otchere S., Roberfroid D. Diet and physical activity for the prevention of noncommunicable diseases in low- and middle-income countries: a systematic policy review. PLoS Med. 2013;10(6):e1001465. doi: 10.1371/journal.pmed.1001465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Management of ST Elevation Myocardial Infarction. http://www.stemiindia.com; Accessed 26.06.15.
- 21.Dalal J.J., Alexander T., Mullasari A. 2013 Consensus Statement for early reperfusion and pharmaco-invasive approach in patients presenting with chest pain diagnosed as STEMI (ST elevation myocardial infarction) in an Indian Setting. J Assoc Phys India. 2014;62:473–483. [PubMed] [Google Scholar]
- 22.Alexander T., Mullasari A.S., Kaifoszova Z. Framework for a National STEMI Program: consensus document developed by STEMI INDIA, Cardiological Society of India and Association Physicians of India. Indian Heart J. 2015;67(5):497–502. doi: 10.1016/j.ihj.2015.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alexander T., Mullasari A.S., Narula J. Developing a STEMI system of care for low- and middle-income countries: the STEMI-India model. Glob Heart. 2014;9(4):419–423. doi: 10.1016/j.gheart.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Sharma S, Bhargava B, Mullasari A, et al. Guidelines for the Management of Cardiovascular Diseases in India. New Delhi. file:///Users/ajp158/Downloads/IND%20Guideline.pdf.
- 25.Talwar KK, Sharma YP, Thakur JS, et al. PostGraduate Institute of Medical Education and Research. Clinical Management Guidelines for Coronary Artery Disease for National Programme for Prevention and Control of Diabetes, Cardiovascular Disease and Stroke. file:///Users/ajp158/Downloads/CAD%20Guidelines.pdf.
- 26.Saddichha S., Saxena M.K., Vibha P. Neurological emergencies in India – lessons learnt and strategies to improve outcomes. Neuroepidemiology. 2009;33(3):280–285. doi: 10.1159/000235640. [DOI] [PubMed] [Google Scholar]
- 27.Alexander T., Mehta S., Mullasari A. Systems of care for ST-elevation myocardial infarction in India. Heart (British Cardiac Society) 2012;98(1):15–17. doi: 10.1136/heartjnl-2011-301009. [DOI] [PubMed] [Google Scholar]
- 28.Victims of Accidents and During Emergency Medical Condition and Women Under Labour. http://lawcommissionofindia.nic.in/reports/rep201.pdf.
- 29.European Social Charter of 1961 (Revised). http://conventions.coe.int/treaty/en/Treaties/Html/163.htm.
- 30.Altenstetter C. Insights from health care in Germany. Am J Public Health. 2003;93(1):38–44. doi: 10.2105/ajph.93.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Platz E., Bey T., Walter F.G. International report: current state and development of health insurance and emergency medicine in Germany. The influence of health insurance laws on the practice of emergency medicine in a European country. J Emerg Med. 2003;25(2):203–210. doi: 10.1016/s0736-4679(03)00173-2. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization . 2008. Regional Office for Europe, Union E. Emergency medical services systems in the European Union: report of an assessment project co-ordinated by the World Health Organization. http://www.who.int/iris/handle/10665/107916#sthash.DqzYnCX8.dpuf. [Google Scholar]
- 33.42 U.S.C. 1395DD – Examination and Treatment for Emergency Medical Conditions and Women in Labor. http://www.gpo.gov/fdsys/granule/USCODE-2010-title42/USCODE-2010-title42-chap7-subchapXVIII-partE-sec1395dd.
- 34.Kao D.P., Martin M.H., Das A.K. Consequences of federal patient transfer regulations: effect of the 2003 EMTALA revision on a tertiary referral center and evidence of possible misuse. Arch Intern Med. 2012;172(11):891–892. doi: 10.1001/archinternmed.2012.1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Medicare program; clarifying policies related to the responsibilities of Medicare-participating hospitals in treating individuals with emergency medical conditions. Final rule. Fed Regist. 2003;68(174):53222–53264. [PubMed] [Google Scholar]
- 36.Kumar C., Prakash R. Public-private dichotomy in utilization of health care services in India. Consilience: J Sustain Dev. 2011;5(1):25–52. [Google Scholar]
- 37.Huffman M.D., Rao K.D., Pichon-Riviere A. A cross-sectional study of the microeconomic impact of cardiovascular disease hospitalization in four low- and middle-income countries. PLoS ONE. 2011;6(6):e20821. doi: 10.1371/journal.pone.0020821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tung E., Bennett S. Private sector, for-profit health providers in low and middle income countries: can they reach the poor at scale? Glob Health. 2014;10:52. doi: 10.1186/1744-8603-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sharma D.C. Concern over private sector tilt in India's new health policy. Lancet. 2015;385(9965):317. doi: 10.1016/s0140-6736(15)60103-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.