1. Case report
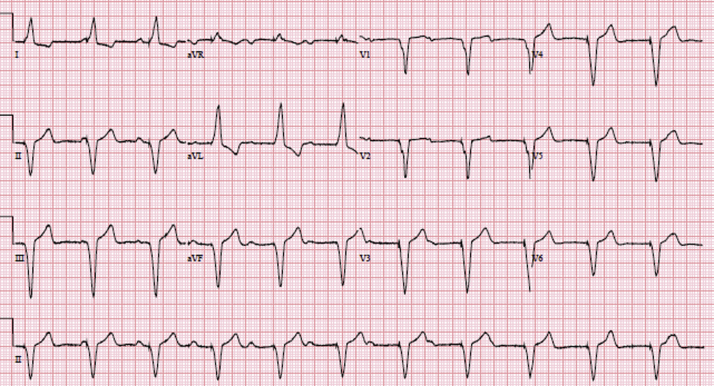
A 56-year-old woman with prior history of dual-chamber permanent pacemaker (PPM) implantation (ELA Medical Symphony DR 2550, ELA Medical, Montrouge, France) for symptomatic complete heart block presented to the Cardiac Rhythm Device Clinic because of increased shortness of breath. A surface 12-lead electrocardiogram (ECG) showed no pacing activity in the atrium (Fig. 1). What is the mechanism?
Fig. 1.
Twelve-lead ECG showing ventricular pacing and complete heart block.
2. Comments
The device is a dual-chamber PPM in rate-modulate (DDDR) mode. The 12-lead ECG depicts fixed ventricular pacing in the context of complete heart block. Loss of atrial sensing and pacing is clearly revealed by the ECG and possible causes include:
-
1.
Atrial oversensing due to lead integrity failure (fracture, insulation failure) or connector problems between the header and the lead.
-
2.
Atrial lead displacement: no evidence of micro- or macro-displacement was found on chest radiography.
-
3.
Asynchronous mode of pacing (VOO) due to magnet or programming: device interrogation ruled out this differential diagnosis. The device was fully functional in DDDR mode.
-
4.
Battery end of life triggering VVI mode with underlying complete heart block.
Differential diagnoses such as atrial oversensing and lead failures can manifest together, since lead or connector problems can cause oversensing of non-physiologic cardiac signals. In this particular case, all other possible causes were ruled out.
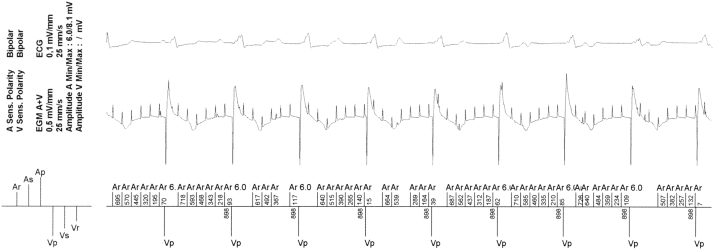
Pacemaker interrogation was performed (Fig. 2) and showed atrial mode switch (AMS) due to atrial oversensing. Appropriate AMS refers to the ability of the pacemaker to change automatically from one mode to another in response to atrial tachyarrhythmia. The atrial lead revealed no capture at 5.0 V/1.5 ms, P-wave sensing of 0.7 mV, and an impedance level above 3000 Ω.
Fig. 2.
Intracardiac electrocardiograms obtained from the pacemaker interrogation showing atrial oversensing due to atrial noise and the consequently activated mode switch.
The patient had DDD pacing when we performed PM interrogation. Diagnosis obtained from the device revealed atrial arrhythmia and mode switches due to atrial tachyarrhythmia. In addition, the asynchronous pacing mode or magnet mode was adjusted to 80 ppm. However, in our patient, VP rate was 898 ms (66 ppm), and no magnet mode was noted in the device log that was consistent with the AMS rate.
This pacemaker is made by Sorin (ELA Medical Symphony DR 2550, ELA Medical, Montrouge, France) and is equipped with a rate response function that is regulated by a minute ventilation sensor. In ELA devices, minute ventilation is measured by using the RA lead with an 8-Hz low-amplitude current. If the RA lead is fractured, the pacemaker automatically increases voltage to maintain the current, and the sensing of this high voltage output prompts an auto-mode switch. In fact, the regular noise in this case was 8 Hz. Therefore, we believe that this was the actual cause of the auto-mode switch.
In conclusion, 12-lead ECG interpretation is important in recognizing possible PPM-related problems.
Conflict of interest and disclosure of funding
All authors declare that the manuscript, as submitted or its content in another version, is not under consideration for publication elsewhere and will not be submitted elsewhere, until a final decision is made by the editors of the Journal of Arrhythmia. All authors declare no conflict of interest related to this study. All authors have made substantive contributions to the study, and all authors endorse the data and conclusions. Nevertheless, confirmation of informed patient consent for publication was obtained.