1. Preamble
It is well appreciated that the lay public and even first medical contact (FMC) physicians remain in denial about myocardial infarction (heart attack). Patients frequently ignore signs and symptoms of a heart attack and even FMC may fail to pay as much attention to it as otherwise warranted. On the other hand appropriate management of this condition including primary PCI are among the few therapeutic modalities in cardiology that actually save life.1 Medical profession should play a central role in overcoming this void and provide clear cut guidance to emergency personnel, FMC physician, even physicians manning the local clinics and even casualty services. Of-course, the guidance provided should be based on expert analysis of available data (on drugs, devices and strategies), careful dissection of risk benefit ratio of therapeutic modalities but also a scrutiny of the cost of these strategies. Health economics while playing a mere supportive role in the developed world certainly plays a central part in the internal decision-making process in emerging economies. From patients perspective all these considerations can improve the quality of care, optimize patient outcomes, and favorably affect costs by focusing resources on the most effective strategies.
In many emerging economies there is a wide disparity in the delivery of health-care from big metropolitan cities, to urban center, semi-urban township to rural villages. While primary PCI is easily available in metro and urban areas (although limited by cost of the procedure and traffic congestion), suburban town hospitals may find some of these issues not relevant to them because of limited availability of PCI capable centers. Furthermore even smaller hospitals in urban areas have fewer cardiologists who are involved in responding to STEMI emergencies 24/7 and even fewer interventional cardiologists on call.
2. Methods
Considering that this is a health-care issue of vital importance we have contacted 9351 cardiologists and cardiologist physicians regarding their interest and proficiency in developing STEMI algorithms. Out of them 62 physicians from diverse background responded. In developing these algorithms we have undertook an organized and directed approach to thoroughly review evidence and place it into a perspective which should assist physicians in selecting the best management strategy for an individual patient. The protocols were developed after considerable review of medical literature, currently available guidelines and active scientific and practice inputs from 16 of the previously mentioned cardiology professionals.
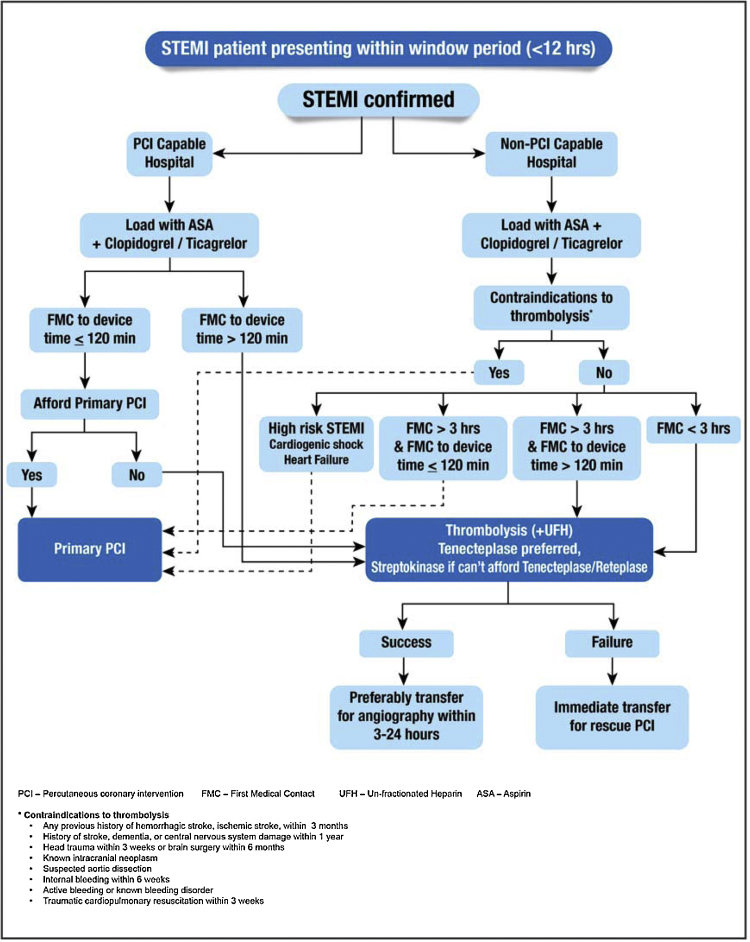
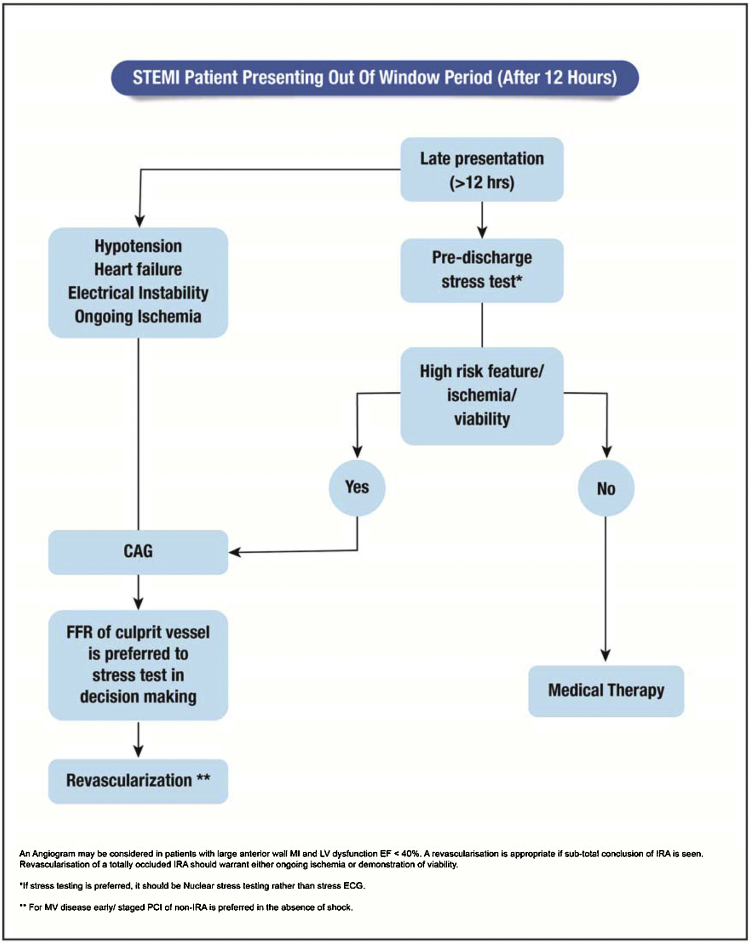
2.1. Patients presenting within window period and out of window period
In context of STEMI in less industrialized counties a major factor in delay in revascularization issue is time from onset of ischemia to presentation to a health-care facility (capable of revascularizing – PCI or thrombolysis). A delay by the patient and FMC physicians often contributes to patient presenting out of the window period (12 h after the chest pain).2, 3, 4 To address this issue we have developed an algorithm to manage patients presenting out of window period (12 h) (Fig. 1). We have taken a cut-off of 12 h because maximum benefit of revascularization strategy occurs during this time period and after this time period benefit of revascularization in uncomplicated STEMI is pretty low if any. Within the group of patients presenting in the window period we have clearly categorized them into presenting in PCI capable centers versus non PCI capable centers. An interesting part of our algorithm is that besides considering transfer times or other delays we have also considered affordability, a particularly relevant issue in emerging economies. Another interesting concept in this algorithm, is that if patient presents to a non-PCI capable center we have stretched the Golden Hour to 3 h, wherein thrombolysis may be the best option keeping in mind the huge transfer times and limited availability of cath labs especially in rural areas.5 Finally, while tissue plasminogen inhibitor (tenecteplase or alternately reteplase) is the preferred fibrinolytic agent in many far flung and resource compromised areas it may not be available and in this case streptokinase is a reasonable alternative.6 Out of window period protocol is a unique feature of our algorithms particularly relevant to far flung areas, low resource setting and low education levels (Fig. 2). Based on available evidence we have given a lot of importance to demonstration of viability or ischemia rather than routine angiography to conserve monetary resources and use it in those situations where benefit is more as also avoid overuse of treatment.
Fig. 1.
Patient with STEMI presenting within window period.
Fig. 2.
Patient with STEMI presenting within window period.
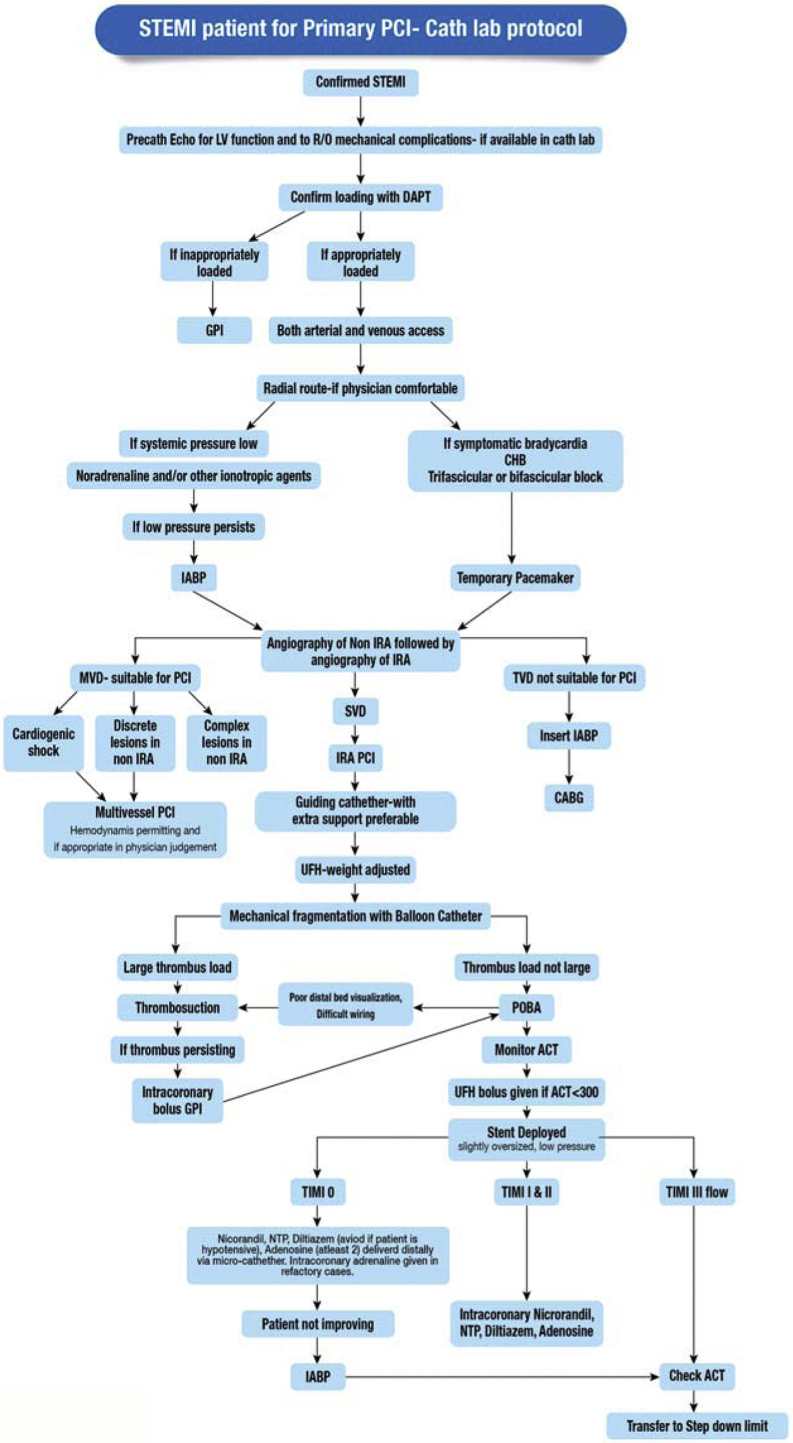
2.2. Primary PCI cath lab protocol
In countries like India where significant volume of PCI is in context of acute MI; primary PCI, delayed PCI or rescue PCI, standardized cath protocols, once the patient has been taken up for primary PCI are very important.7 Unfortunately, these standardized protocols for less industrialized nations are not available. In this context we have developed an algorithm and outlined a suggested procedure protocol for the cardiac cath labs. Within the algorithm we have made provisions for doing complicated, high-risk PCI procedures. We have made suggestions depending on the hospital set-up, for example in some large hospitals cardiologists may have the choice to choose a guiding catheter with support (a strategy which might be useful in especially in complex cases) while this option may not be available to physicians in smaller hospitals where only one type of guide – catheter may exist. We have also adapted the protocol to practice environments in countries like India where often not only Echocardiography (echo) equipment is easily available in cath labs but also interventional cardiologists are trained to do basic echo. We recommend a baseline echo exam while initiating the catheterization procedure; for left ventricular function assessment but also to rule out mechanical complications, as sometimes due to poor patient education status and rural background even the time of onset of ischemia is not very clear (Fig. 3). We recommend that hospital set-ups use this protocol to set up a standard inventory of guiding catheters, wires, and a couple of balloons that could fit on one moveable cart, which can be dedicated to primary PCI program.
Fig. 3.
Patient presenting with STEMI − Cath lab Protocol.
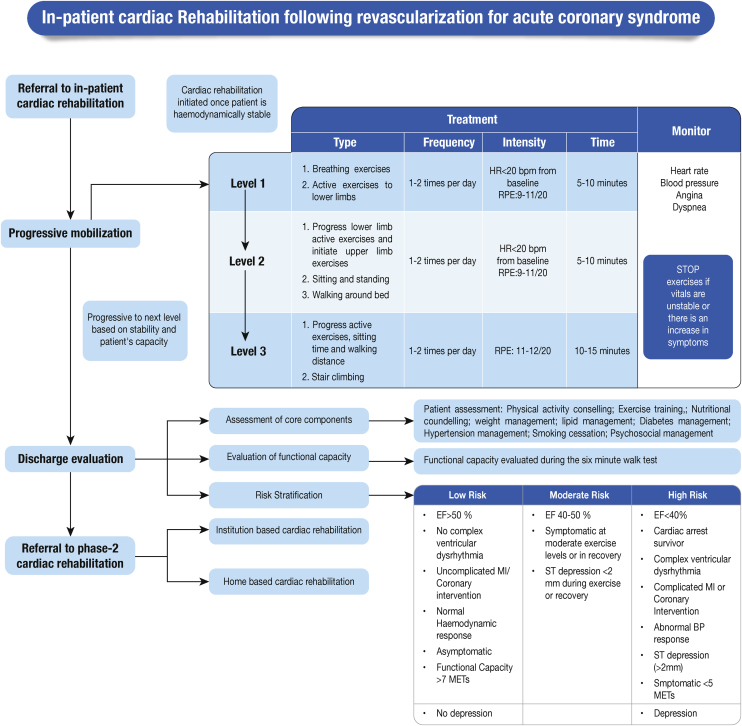
2.3. Cardiac rehabilitation
Cardiac rehabilitation is an integral but often neglected component of post STEMI care. Often even physicians are unaware of level of activity permitted after STEMI and the concept behind this protocol. We have given a simple, scientific algorithm for post MI care and risk stratification keeping in mind low resource settings8, 9 (Fig. 4).
Fig. 4.
Patient presenting with STEMI − Cardiac rehabilitation.
3. Conclusions
In conclusion, these algorithms have been developed keeping in mind practice environments in less industrialized areas and low resource and rural settings and maybe very useful for decision making for STEMI patients within these practice environments. They should also help address issues of physician awareness and decision making and help set up a standardized STEMI programs at various centers. Ultimately they could impact many health-care delivery indices like mean door-to-balloon/needle time and even pain to door time.
References
- 1.Mishra S. Does modern medicine increase life-expectancy: quest for the moon rabbit? Indian Heart J. 2016;68:19–27. doi: 10.1016/j.ihj.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Negi P.C., Merwaha R., Panday D., Chauhan V., Guleri R. Multicenter HP ACS registry. Indian Heart J. 2016;68(2):118–127. doi: 10.1016/j.ihj.2015.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iqbal F., Barkataki J.C. Spectrum of acute coronary syndrome in North Eastern India—a study from a major center. Indian Heart J. 2016;68(2):128–131. doi: 10.1016/j.ihj.2015.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mehta S., Granger C.B., Henry T.D. Reducing system delays in treatment of st elevation myocardial infarction and confronting the challenges of late presentation in low and middle—income countries. Indian Heart J. 2016;69(S1):S1–S5. doi: 10.1016/j.ihj.2016.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boersma E., Maas A.C., Deckers J.W. Simoons ML Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996;348:771–775. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- 6.Melandri G., Vagnarelli F., Calabrese D., Semprini F., Nanni S., Branzi A. Review of tenecteplase (TNKase) in the treatment of acute myocardial infarction. Vasc Health Risk Manag. 2009;5:249–256. doi: 10.2147/vhrm.s3848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramakrishnan S., Mishra S., Chakraborty R., Chandra K.S., Mardikar H.M. The report on the Indian coronary intervention data for the year 2011—National Interventional Council. Indian Heart J. 2013;65(5):518–521. doi: 10.1016/j.ihj.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grace S.L., Bennett S., Ardern C.I., Clark A. cardiac rehabilitation series: Canada. Prog Cardiovasc Dis. 2014;56(5):530–535. doi: 10.1016/j.pcad.2013.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Babu A.S., Noone M.S., Haneef M., Naryanan S.M. Protocol-guided phase-1 cardiac rehabilitation in patients with ST-Elevation myocardial infarction in a rural hospital. Heart Views. 2010;11:52–56. doi: 10.4103/1995-705X.73209. [DOI] [PMC free article] [PubMed] [Google Scholar]