Abstract
We report the case of a 51-year-old patient with Brugada syndrome (BrS) who experienced inappropriate shock due to T-wave oversensing (TWOS) during exercise when the optimal sensing vector was selected based on the automatic analysis by a subcutaneous implantable cardioverter-defibrillator (S-ICD). After selecting another vector during exercise testing, TWOS did not re-occur. Selection of appropriate sensing vector based on analyses under various conditions, including during exercise after S-ICD implantation, should be considered for patients with BrS.
Keywords: Subcutaneous implantable cardioverter-defibrillator, Inappropriate shock, Brugada syndrome
1. Introduction
Subcutaneous implantable cardioverter-defibrillator (S-ICD) is a novel treatment modality to prevent sudden cardiac death that does not require lead implantation in or on the heart. S-ICD automatically analyzes optimal sensing vectors, and the optimal sensing vector is usually selected based on this analysis [1]. This analysis is usually performed in the supine position at rest.
In patients with Brugada syndrome (BrS), ICD is the main treatment modality to prevent sudden cardiac death, and S-ICD is a therapeutic option designed to avoid complications related to the transvenous system. However, the BrS-pattern electrocardiogram (ECG) is known to show dynamic changes, and evaluation of ECGs after S-ICD implantation in patients with BrS should be undertaken in various situations [2]. Moreover, little is known about the method of selection of the optimal sensing vector in patients with BrS based only on the automatic analysis of the S-ICD at rest. Here, we report the case of a patient with BrS who experienced inappropriate shock (IAS) due to T-wave oversensing (TWOS) during exercise.
2. Case report
A 51-year-old man with BrS was referred to our hospital to be evaluated for indications for ICD. He exhibited a spontaneous type 1 baseline ECG and had a family history of sudden cardiac death. Ventricular fibrillation was induced during an electrophysiological study, and ICD implantation was recommended. After ECG screening, all three vectors were recognized as acceptable. S-ICD (EMBLEM, Boston Scientific, Marlborough, Massachusetts) was successfully implanted in the standard position using a standard technique (Fig. 1A), and the secondary vector was selected as the optimal sensing vector based on automatic S-ICD analysis at rest. The patient experienced a strong impact during exercise 30 days after the S-ICD implantation. Evaluation revealed that IAS had occurred due to TWOS (Fig. 2A). The secondary vector was still acceptable as the optimal sensing vector, again based on automatic re-analysis by the S-ICD at that time. He therefore underwent an exercise test to confirm whether the secondary vector was appropriate. During exercise, the ECG ST segment changed remarkably (Fig. 1B), and TWOS was observed in the primary and secondary vectors on the cardiac signals of the S-ICD (Fig. 2B and C). However, TWOS was not observed when we selected the alternate vector (Fig. 2D), which was then selected as the optimal sensing vector of S-ICD instead of the secondary vector. After changing the sensing vector, the patient was free from IAS.
Fig. 1.
(A) Chest radiography findings of the BrS patient with an S-ICD A pulse generator was implanted subcutaneously in the left lateral position. (B) 12-lead ECG of BrS patient before and during exercise ST segment changed remarkably during exercise.
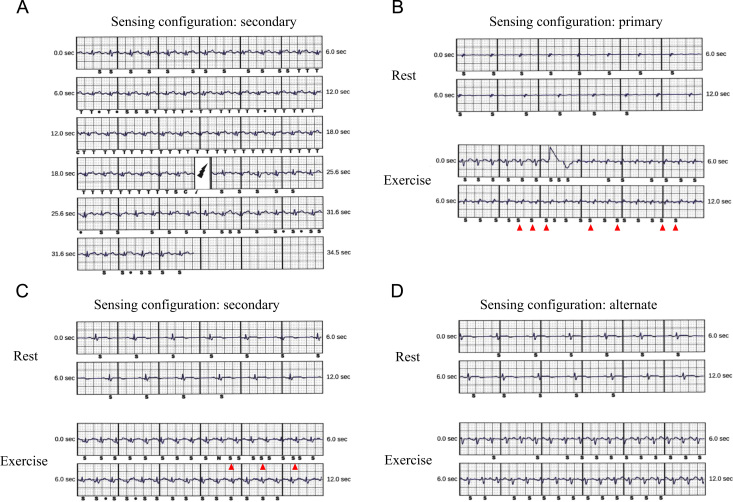
Fig. 2.
Cardiac signals of the S-ICD at the time of IAS (A) and during the exercise test (B, C, D) . Inappropriate shock was observed during exercise due to TWOS (A). TWOS (red arrows) was observed during the exercise test in the primary (B) and secondary vectors (C) on the cardiac signals of S-ICD. TWOS was not observed using the alternate vector (D). S = Sense, N = Noise, T = Tachy Detection, C = Charge Start, • = Discard.
3. Discussion
This is the first report of IAS due to TWOS in a Japanese patient with BrS after S-ICD implantation. A previous registry revealed that the incidence of IAS with S-ICD was 13.1% at 3 years after implantation [3]. The most common cause of IAS was oversensing of the cardiac signal, such as TWOS, apart from heart rate increase due to supraventricular tachycardia in the shock zone [4]. A recent report showed that patients exhibiting an ST segment change during exercise, including patients with hypertrophic cardiomyopathy, were at risk for TWOS [5]. BrS ECG patterns show dynamic changes that affect the QRS complex and ST segment amplitude and morphology. A recent report showed that the acceptable sensing vector in S-ICD could be changed by injecting ajmaline [2]. ECG changes in BrS occur not only due to drugs but also during exercise; therefore, specific attention to TWOS is needed in this population. While S-ICD is a therapeutic option for patients with BrS, it is important to pay close attention to the selection of the optimal sensing vector in S-ICD. Furthermore, if all sensing vectors are not available, we cannot use S-ICD appropriately. In that case, we have to change the lead location or extract the S-ICD system and implant transvenous ICD. From this point of view, it is still important to adequately evaluate the acceptability of the sensing vector in S-ICD before implantation.
4. Conclusion
Exercise testing shortly after S-ICD implantation should be considered for patients with BrS to evaluate the acceptability of the sensing vector in S-ICD.
Conflicts of interest
All authors declare no conflict of interest related to this study.
Acknowledgments
None.
References
- 1.Bruce L.W., Laurent F., Martin K.S. HRS/EHRA/APHRS/SOLAECE expert consensus statement on optimal implantable cardioverter-defibrillator programming and testing. J Arrhythm. 2015;2016(32):1–28. doi: 10.1016/j.joa.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conte G., Regoli F., Moccetti T. Subcutaneous implantable cardioverter-defibrillator and drug-induced Brugada syndrome: the importance of repeat morphology analysis during ajmaline challenge. Eur Heart J. 2016;(37):1498. doi: 10.1093/eurheartj/ehv572. [DOI] [PubMed] [Google Scholar]
- 3.Burke M.C., Gold M.R., Knight B.P. Safety and efficacy of the totally subcutaneous implantable defibrillator. 2-year results from a pooled analysis of the IDE study and EFFORTLESS registry. J Am Coll Cardiol. 2015;65:1605–1615. doi: 10.1016/j.jacc.2015.02.047. [DOI] [PubMed] [Google Scholar]
- 4.Louise R.A.O.N., Tom F.B., Craig Barr. Inappropriate shocks in the subcutaneous ICD: incidence, predictors and management. Int J Cardiol. 2015;195:126–133. doi: 10.1016/j.ijcard.2015.05.135. [DOI] [PubMed] [Google Scholar]
- 5.Kirsten M.K., Reinoud E.K., Louise O.N. Inappropriate subcutaneous implantable cardioverter-defibrillatior shocks due to T-wave oversensing can be prevented: implantations for management. Heart Rhythm. 2014;11:426–434. doi: 10.1016/j.hrthm.2013.12.007. [DOI] [PubMed] [Google Scholar]