ABSTRACT
Introduction: Fifty years after the discovery of Δ9-tetrahydrocannabinol (THC) as the psychoactive component of Cannabis, we are assessing the possibility of translating this herb into clinical treatment of inflammatory bowel diseases (IBDs). Here, a discussion on the problems associated with a potential treatment is given. From first surveys and small clinical studies in patients with IBD we have learned that Cannabis is frequently used to alleviate diarrhea, abdominal pain, and loss of appetite. Single ingredients from Cannabis, such as THC and cannabidiol, commonly described as cannabinoids, are responsible for these effects. Synthetic cannabinoid receptor agonists are also termed cannabinoids, some of which, like dronabinol and nabilone, are already available with a narcotic prescription.
Areas covered: Recent data on the effects of Cannabis/cannabinoids in experimental models of IBD and in clinical trials with IBD patients have been reviewed using a PubMed database search. A short background on the endocannabinoid system is also provided.
Expert commentary: Cannabinoids could be helpful for certain symptoms of IBD, but there is still a lack of clinical studies to prove efficacy, tolerability and safety of cannabinoid-based medication for IBD patients, leaving medical professionals without evidence and guidelines.
KEYWORDS: Cannabinoids, Crohn’s disease, dronabinol, inflammatory bowel disease, medical marijuana, nabilone, nabiximols, ulcerative colitis, Cannabis
1. Introduction
Inflammatory bowel diseases (IBDs), i.e. Crohn’s disease (CD) and ulcerative colitis (UC), are chronic inflammatory conditions of the gastrointestinal (GI) tract with increasing prevalence in Westernized countries [1]. Although their etiology is still unknown, these diseases are thought to comprise misdirected attacks of the immune system against gut microbiota or their products [2]. Defects in the epithelial barrier function and in mucosal wound healing are of paramount importance in the progression of IBD [1,2]. The endocannabinoid system (ECS) has been recognized to play an important role in the maintenance of gut homeostasis since it quickly responds to disturbances by de novo synthesis of its effector molecules and is, therefore, of particular interest in the management of IBD [3].
The ECS consists of lipid mediators, so-called endocannabinoids, their synthesizing and degrading enzymes, and of G protein-coupled cannabinoid receptors (CBs) that mediate the endocannabinoid effects (Figure 1). Components of the ECS have been found to be expressed throughout the GI tract and have been reviewed in detail elsewhere [4,5]. Briefly, the ECS has been described to comprise two CBs, i.e. cannabinoid receptor 1 (CB1) and 2 (CB2). CBs can be activated by a variety of synthetic or plant-derived cannabinoids, as well as by the endocannabinoids anandamide (arachidonoylethanolamine [AEA]) and 2-arachidonoylglycerol (2-AG). Synthesizing enzymes include N-acyl phosphatidylethanolamine phospholipase D (NAPE-PLD) for AEA and diacylglycerol lipase for 2-AG, respectively.
Figure 1.
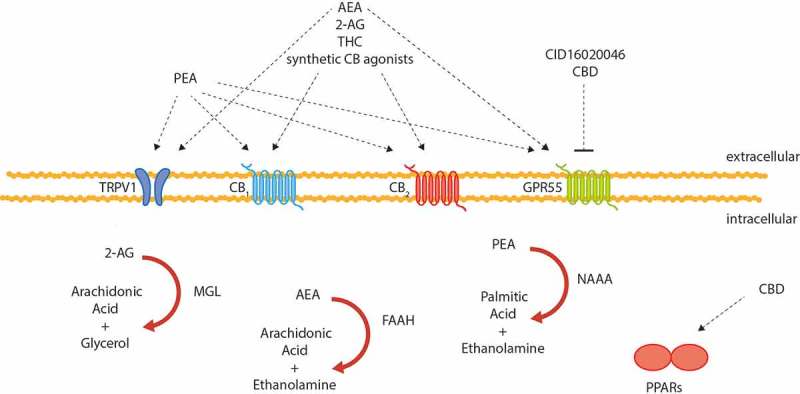
A schematic overview of cannabinoid receptors, cannabinoid-responsive non-cannabinoid receptors, their ligands and degrading enzymes of the endocannabinoid system as described in murine IBD. 2-AG, 2-arachidonoylglycerol; AEA, anandamide; CB, cannabinoid receptor; CBD, cannabidiol; FAAH, fatty acid amide hydrolase; GPR55, G protein-coupled receptor 55; NAAA, N-acylethanolamine-hydrolyzing acid amidase; PEA, palmitoylethanolamide; PPARs, peroxisome proliferator-activated nuclear receptors; THC, Δ9-tetrahydrocannabinol; TRPV1, transient receptor potential of vanilloid-type 1.
Degradation of AEA is facilitated mainly by fatty acid amide hydrolase (FAAH), whereas 2-AG is degraded mostly by monoacylglycerol lipase (MGL or MAGL). However, the notion of the ECS being a confined physiological entity with CB receptors in its center has been challenged by the discovery of receptors responsive to cannabinoids other than CB1/2, such as G protein-coupled receptor 55 (GPR55), transient receptor potential of vanilloid-type 1 (TRPV1), and peroxisome proliferator-activated nuclear receptors (PPARs) [6]. Furthermore, it has been found that the ECS does not only consist of the aforementioned biosynthetic and degrading components, but also in fact shares many enzymes with other pathways, e.g. cyclooxygenase-2 which oxidizes AEA and thus provides a link between the ECS and prostaglandin synthesis [7]. While the complexity of the interactions of all molecules involved in (endo-) cannabinoid signaling represents a large obstacle in understanding the endocannabinoids’ role in (patho-)physiology, research on the ‘expanded ECS’ or ‘endocannabinoidome’ [7] may very well open doors for new treatment options. After all, it is desirable to discover cannabinoid based drugs that exert their actions without causing psychotropic effects that arise from activation of central CB1 receptors.
2. The ECS as a therapeutic target in IBD
To investigate the role of cannabinoids in IBD, mostly animal models that rely on chemically induced mucosal inflammation are used. Dextran sulfate sodium (DSS)-induced colitis, for instance, causes the influx of macrophages, neutrophils, and a Th2-mediated immune response [8–10], whereas trinitrobenzene sulfonic acid (TNBS)-induced colitis is more dominated by a Th1-response [8,10]. Analysis of expression levels of ECS components in inflamed rodent colonic tissue revealed enhanced cannabinoid signaling under inflammatory conditions as compared to healthy tissue. Thus, CB1 and CB2 receptors, as well as AEA, were found to be upregulated in experimental IBD models [11,12]. Upregulation of AEA, however, was only found in certain layers of the colon (e.g. in the submucosa but not the mucosa) [11]. On the other hand, the AEA-degrading enzyme FAAH was expressed to a lesser extent in the initial stage of colitis but returned to control levels as the disease progressed [13]. Pharmacological strategies to enhance endocannabinoid levels in the inflamed colon of rodents through inhibition of the degrading enzymes FAAH or MGL, respectively, ameliorated the inflammation [14,15]. Accordingly, it has been reported that activation of CB1 or CB2 with synthetic agonists protected from colitis [12,16] and that treatment with Δ9-tetrahydrocannabinol (THC), the main psychoactive constituent of Cannabis sativa, reduced TNBS-induced inflammation as well as myeloperoxidase (MPO) activity and motility disturbances in the in rat colon [17]. These findings prompted the investigation of other nonpsychoactive components of Cannabis in IBD models. It has been shown that cannabidiol (CBD), a cannabinoid with very low affinity for CB1 and CB2, has protective effects in murine colitis as observed by a reduction of colon injury, inducible nitric oxide synthase expression, reactive oxygen species production, MPO activity, and tumor necrosis factor alpha (TNF-α) levels [17–21]. CBD has also been reported to inhibit FAAH activity [22] and could thus alter endocannabinoid levels. Other non-psychotropic cannabinoids, shown to be beneficial in colitis models, include the plant cannabinoid cannabigerol [23] and the synthetic atypical cannabinoid O-1602, which has been shown to inhibit neutrophil recruitment [24]. Cannabigerol reduced nitric oxide production in macrophages and this effect was modulated by the CB2 receptors [23]. While the molecular targets of cannabigerol and O-1602 have not been fully elucidated yet, extensive evidence exists that CBD exerts its functions, at least partly, through PPARs [21]. CBD has also been reported to act as an antagonist to GPR55, a receptor that plays a crucial role in intestinal inflammation [25]. Another molecule of interest in IBD is palmitoylethanolamide (PEA), a structural relative of anandamide that acts via multiple targets including CB1, CB2, GPR55, PPARα, and TRPV1 and that has been reported to reduce inflammation and intestinal permeability in mice [26–28]. With regard to the ECS, beneficial effects of PEA in experimental IBD involved an increase in colonic CB1 receptor expression and activation of CB2 and GPR55 [26]. Another plant cannabinoid with anti-inflammatory properties in murine colitis is cannabichromene [29] which inhibited endocannabinoid inactivation [30].
Taken together, a huge amount of preclinical data strongly support the ECS as a therapeutic target in IBD (as previously reviewed by Refs. [3,31–33]).
2.1. Components of the ECS are differentially expressed in human IBD
The altered regulation of the ECS in IBD patients has been addressed in various reports with rather contradictory outcomes (summarized in Table 1). Although AEA levels were found to be increased in UC patients (n = 8) [11], some studies reported an overall reduced AEA signaling in IBD patients, as observed through decreased activity and/or levels of the synthesizing enzyme NAPE-PLD [34,35], as well as through increased activity of the degrading enzyme FAAH [34,35], and through reduced levels of AEA [34]. Enhanced CB2 immunoreactivity has been observed in the colonic epithelium and some cells of the inflammatory cell infiltrate in CD and UC specimens, suggesting that CB2 might be a relevant target for IBD treatment [34–36]. In fact, activation of CB2 has shown protection in experimental models of colitis [16,37]. Also in a human colonic explant model, where colitis-like damage was induced with pro-inflammatory cytokines, activation of CB2 led to reduced damage of mucosal crypts and the epithelial lining [38].
Table 1.
Differential expression of ECS components in human IBD compared to controls as described in the literature.
| IBD |
||||
|---|---|---|---|---|
| ECS component | UC | CD | References | |
| Receptors | CB1 | No change, downregulation, or upregulation | Upregulation | [26–28] |
| CB2 | Upregulation | [27,30] | ||
| Upregulation (protein) or no change (mRNA, protein) | [26,28] | |||
| Ligands | AEA | Upregulation | [10] | |
| Downregulation | [26] | |||
| 2-AG | No change | [10,26] | ||
| Synthesizing enzymes | NAPE-PLD | Downregulation or reduced activity | [26,27] | |
| DAGL | Upregulation | [27] | ||
| Degrading enzymes | FAAH | No change (epithelium) or upregulation (immune cells) or increased activity | [26,27] | |
| MGL | Upregulation | [27] | ||
CB1: cannabinoid receptor 1; CB2: cannabinoid receptor 2; AEA: anandamide; 2-AG: 2-arachidonoylglycerol; ECS: endocannabinoid system; IBD: inflammatory bowel disease; NAPE-PLD: N-acyl phosphatidylethanolamine phospholipase D; DAGL: diacylglycerol lipase; FAAH: fatty acid amide hydrolase; MGL: monoacylglycerol lipase.
Furthermore, treatment with methanandamide, a non-hydrolysable analog of AEA, reduced interferon-γ and TNF-α secretion from cultured biopsy specimens and from lamina propria cells isolated from IBD specimens [34].
2.2. Could Cannabis be used as a treatment for IBD?
Thousands of years ago, Cannabis was traditionally used for the treatment of inflammation of the gut. Nowadays, the use of medicinal Cannabis is being legalized in a growing number of countries but clinical studies on the effects of Cannabis in IBD are scarce. Questionnaires conducted in Canada, USA, and Israel so far revealed that patients commonly use the drug as a self-medication to relieve IBD-related symptoms, including abdominal pain, diarrhea, and loss of appetite [39–43]. A retrospective observational study on 30 patients with CD found that 21 subjects significantly benefited from Cannabis consumption as seen through a significant reduction of the average Harvey Bradshaw Index as well as through a reduced need for other medication [44]. A prospective pilot study with 13 IBD patients, who were instructed to inhale Cannabis when they were in pain, concluded that the treatment significantly improved the patients’ quality of life [42]. Finally, a small randomized placebo-controlled clinical trial suggested beneficial effects of Cannabis treatment in CD patients [45]. In this study, 11 patients received Cannabis cigarettes containing 115 mg THC twice daily, while the placebo group (n = 10) received Cannabis flowers that were devoid of THC. The duration of the study was 8 weeks with an additional wash out phase of 2 weeks. Because of the small sample sizes, a statistical difference in remission (a Crohn’s disease and activity index [CDAI] < 150) between treatment (5/11) and placebo group (1/10) was not achieved. A clinical response (a reduction in CDAI > 100), however, was observed in 10/11 subjects in the treatment group (4/10 in the placebo group). Additionally, in the Cannabis group, three patients were weaned from steroids and two from opiates. Patients of the treatment group further reported an increase in quality of life (as assessed by SF-36). A difference in objective markers of inflammation, i.e. C-reactive protein, however, was not observed between the two groups [45]. A summary of clinical studies on the benefit of Cannabis medication in IBD conducted to date is given in Table 2. It should be kept in mind, however, that most of these clinical studies are statistically underpowered and also lack methodological quality. Another critical point is the use of the right placebo in these studies as central effects of Cannabis/cannabinoids are hard to conceal.
Table 2.
An overview of clinical studies on Cannabis treatment in IBD patients.
| Patient number (n) |
||||||
|---|---|---|---|---|---|---|
| Study type | UC | CD | Treatment | Investigated parameters | Findings | Reference |
| Questionnaire | 100 | 191 | – | Cannabis use, SIBDQ | 33% of UC and 50% of CD patients used Cannabis for symptom relief | [31] |
| Questionnaire | 63 | 231 | – | Cannabis use, subjective assessment, users vs. nonusers | 17.6% of patients used Cannabis for symptom relief, surgery prediction | [33] |
| Retrospective observational study | – | 30 | Cannabis use (unspecified) | HBI, need for surgery and hospitalization | HBI reduced from 14 ± 6.7 to 7 ± 4.7 | [36] |
| Prospective study | 2 | 11 | Cannabis use for 3 months (not standardized) | HBI, partial Mayo score | HBI reduced from 11.36 ± 3.17 to 5.72 ± 2.68 | [34] |
| Prospective study | – | 21 | 115 mg THC twice daily or placebo for 8 weeks | CDAI, life quality (SF-36) | Remission (5/11), CDAI reduction (10/11), increased life quality | [37] |
| Prospective survey | 102 | 177 | – | Cannabis use | 16.4% of patients used Cannabis for symptom relief | [32] |
| Prospective survey | 18 | 35 | – | Cannabis use, SIBDQ in young adults | 45% of patients (18–21 years old) used Cannabis for symptom relief | [35] |
HBI: Harvey Bradshaw index; IBD: inflammatory bowel disease; THC: Δ9-tetrahydrocannabinol; CDAI: Crohn’s disease and activity index; SIBDQ: short-inflammatory bowel disease questionnaire.
2.3. CBD for the treatment of IBD?
As outlined above, several preclinical studies have indicated that CBD is protective in intestinal inflammation [17–20]. A study in an lipopolysaccharide-induced model suggested that CBD, which is known to act as GPR55 antagonist [46], inhibits GI inflammation by controlling the inflammatory response and the activation of enteric glial cells [21]. Parts of the beneficial effects by CBD were mediated via PPARγ raising the possibility that GPR55 could have been involved in the beneficial effect [21]. Furthermore, CBD could be supportive in maintaining a healthy intestinal barrier. In a CaCo-2 cell monolayer model stimulated by EDTA, CBD recovered the intestinal barrier in a concentration and CB1-dependent manner [47]. The results of a clinical trial on CBD in IBD (ClinicalTrials.gov ID NCT01037322), however, have not been published so far. The anti-inflammatory potential of CBD has been also recently reviewed elsewhere [48].
3. Conclusion
Experimental evidence gathered from preclinical IBD models and conducted in rodents point to a strong potential of the ECS components to serve as drug targets in inflammatory diseases of the intestine. Data suggest a homeostatic role of the ECS in the gut. Accordingly, it is believed that the enhancement of endocannabinoid signaling, as observed through the increased levels of endocannabinoids and their receptors, and the decrease in endocannabinoid degrading enzymes, is a response to disturbances of the homeostatic system and is aimed at restoring the balance. This is further supported by the finding that the manipulation of the ECS toward a further increase of endocannabinoid signaling is protective against IBD. On the other hand, analysis of biopsies from UC and CD patients paints a rather complex picture in terms of differential expression of ECS components. Most likely, owing to the small sample sizes in the studies, a conclusion on the meaning of this has not yet been reached. Most evidence points toward an involvement of CB1 and also CB2 receptors, especially with regard to immune cell recruitment. Further research in this direction, preferably on human IBD material, such as explants, cultured biopsies, etc. is highly warranted.
4. Expert commentary
IBDs pose a high burden on patients and health-care systems alike. Current therapy includes anti-inflammatory agents like aminosalicylic acid, immunomodulators, steroids, and biological agents, such as anti-TNF-α antibodies and vedolizumab (an anti-α4β7 integrin antibody that specifically targets adhesion and migration of leukocytes to the GI tract) [49]. Vedolizumab has shown its ability and effectiveness in the induction therapy of IBD, in particular, in patient’s refractory to anti-TNF-α antibody treatment [50]. Biologicals are first-line alternative treatment options in severe IBD and are powerful tools to change the course of the disease [49,51]. However, they come at the prize, as in the case of anti-TNF-α antibodies, of causing severe adverse effects, such as infections, malignancies, and injection/infusion reactions [52]. For Vedolizumab, cases of arthritis and sarcoiliitis have been recently reported [53]. Conventional treatment is often little effective leaving many patients dissatisfied [54]. Because of failing standard therapy, willingness and desire of IBD patients to use complementary and alternative medicine (CAM) are understandably high and an alternative treatment with Cannabis is, therefore, often sought.
Not surprisingly, a New Zealand Survey of 1370 patients with IBD revealed that 44.1% of IBD patients self-medicated with CAM, including Cannabis [55]. Additionally, a large population-based study, using data from the NHANES database (National Center for Health Statistics) showed that IBD patients had a higher incidence (67.3% vs. 60.0%) and an earlier onset in age (15.7 vs. 19.6 years) for Cannabis use as compared to control subjects [56]. Judging from these data, Cannabis has long been used by IBD patients as a form of ‘self-treatment’ to control their symptoms. In the US prospective cohort survey of IBD patients, Ravikoff Allegretti reported that half of the patients, who had never used Cannabis before, expressed their interest in Cannabis for treatment, in particular, against abdominal pain [40].
The broad interest for alternative medicine often puts medical professionals in a situation in which patients express their wish to use Cannabis medicinally, but at the same time, they also face legal and administrative boundaries for its prescription. Unlike in Canada, Israel, and some states in the United States, ‘medical marijuana’ is not legally available in most European countries (only after seeking permission from the government) although cannabinoid-based drugs, such as nabiximols (Sativex®), dronabinol, and nabilone, can be obtained (Table 3). Prescription of these drugs has to follow strict indications or may be given off-label with a narcotic prescription, a situation many physicians are reluctant to deal with.
Table 3.
Currently available cannabinoids for human treatment.
| Dronabinol ((–)-Δ9-trans-tetrahydrocannabinol) |
| Application: oral |
| Trade name: Marinol® |
| Nabilone (THC analog) |
| Application: oral |
| Trade name: Cesamet® |
| Nabiximols (combination of THC and cannabidiol) |
| Application: sublingual spray |
| Trade name: Sativex® |
|
Medical Marijuana (dried leaves and buds from Cannabis) Application: oral, by inhalation, topical |
| Traded as ‘Medical Marijuana’ or ‘Medical Cannabis’ |
THC: Δ9-tetrahydrocannabinol.
4.1. Basic versus clinical research with Cannabis/cannabinoids
A surge of preclinical data on cellular mechanisms of CB receptors and other components of the ECS have recently come forward. However, more information on in vivo mechanisms of cannabinoids and the ECS in inflammatory diseases like IBD is necessary, despite existing reports [19–21,23,25,26,57]. Although we can assume that anti-inflammatory actions of cannabinoids employ peripherally as well as centrally located CB receptors [58,59], a broader picture on how cannabinoids improve severity of inflammation in IBD is needed. Most likely, the ECS concerts a holistic anti-inflammatory response linking endocannabinoids with CB receptors and non-CB1/CB2 cannabinoid-responsive receptors, such as GPR55 [25] and PPARα [26]. Thus, the ECS exerts profound effects on the GI-immune system, intestinal barrier, motility, and brain areas that control gut homeostasis [58].
As to clinical research, data on human trials with Cannabis/cannabinoids in IBD unfortunately lag behind. The medical practitioner has no evidence or guidelines when confronted with questions whether and how to use Cannabis/cannabinoids for the treatment of IBD. Exactly this is of critical importance as the general public is becoming increasingly interested in trying medical treatment with Cannabis. With the availability of medical marijuana and the lack of guidelines for treatment, people may tend to apply Cannabis with the help of a whole range of unprofessional advice and views, an extremely undesirable situation.
4.2. Clinical evidence, efficacy, and safety of cannabinoid-based treatment in IBD
Evidence that Cannabis/cannabinoids provide benefit for IBD patients is still sparse. Apart from anecdotal reports and some small clinical trials [42,44,45], as well as a handful of questionnaires [39–41,43], not much is known regarding a benefit for IBD patients by Cannabis. After reviewing the small amount of literature available on Cannabis/cannabinoids and human IBD, some indication can be seen for the use of Cannabis against abdominal pain, nausea, and loss of appetite in CD but treatment should only be considered after careful assessment of risks and after failure of standard medication. With regard to UC, indication that Cannabis may provide benefit for patients mainly derives from anecdotes and surveys [39–41]. Altogether, clinical trials are urgently warranted to determine the efficacy of Cannabis/cannabinoids in IBD and to draw a comprehensive conclusion. Cannabis/cannabinoids have been considered generally safe as a short-time medication for adults but as a meta-review recently pointed out, there is also a risk of serious adverse events in short-term treatment [60]. High odds for side effects include psychiatric, nervous system, and hepatobiliary disorders; however, short-term treatment mostly causes not only dry mouth, dizziness, somnolence, euphoria, but also hallucinations [60]. These psychotropic-adverse effects are caused by activation of CB1 receptors in the brain. A possibility to circumvent this obstacle could be the use of cannabinoids that do not enter the blood–brain barrier or that only act peripherally.
4.3. Risks of long-term treatment with Cannabis/cannabinoids in IBD
Many questions arise when considering long-term treatment with Cannabis/cannabinoids which is likely necessary in diseases like IBD. Long-term treatment is a strong caveat in adolescent people, given the young age of 20 years for the onset of CD [61]. Prolonged use of Cannabis has shown neurological changes in adolescents including a decrease in gray matter volume in certain brain areas [62]. This aspect needs close attention because a new survey in young adults with IBD (from 18 to 21 years) reported that 70% of these patients did not discuss marijuana use with their gastroenterologist and only half of them had knowledge of possible adverse effects [43]. A further aspect to be considered when using Cannabis for medical treatment is pregnancy. A recent study suggests an increase in stillbirth by long-term use of Cannabis [63]. Since IBD is frequently accompanied by comorbidities, such as cardiovascular disease [64], patients taking Cannabis should be aware of the risk of myocardial infarction and stroke [65].
Long-term treatment with Cannabis/cannabinoids may also have pronounced effects on gut permeability. While THC and CBD have shown permeability-preserving and CB1-dependent properties in CaCo-2 monolayers, the opposite was observed for the endocannabinoids AEA and 2-AG [47,66]. Treatment with FAAH inhibitors that raise endocannabinoid levels may therefore unfavorably affect gut leakiness that is associated with IBD. To minimize risks of adverse effects by cannabinoids, which are caused by activation of CB1 receptors in the brain, the CB2 receptor may be an alternative and valuable target to treat IBD. Unlike with the CB1 receptor, activation of CB2 does not lead to psychotropic effects. In addition, experimental data point to a crucial role of CB2 in the protection against colitis [16,37]. New compounds have been recently described as selective CB2 agonists capable of ameliorating inflammation during DSS colitis [67] but it remains to be evaluated whether CB2 agonists are also anti-inflammatory in human IBD.
4.4. Application of Cannabis/cannabinoids in IBD
Medical marijuana is preferably applied via inhalation. Bioavailability levels of THC average at about 30% [68]. Oral THC has been shown to be effective in chemotherapy-induced nausea at a dose of 5–15 mg/m2 [69]. Most variabilities in THC bioavailability are due to the individual itself and the different content of THC in marijuana plants, a general problem of phytotherapy [68]. These obstacles can be circumvented by using purified ingredients of Cannabis or combinations of purified ingredients, as in nabiximols (THC and CBD), which is applied as a sublingual spray. Each milliliter of nabiximols contains 27 mg THC and 25 mg CBD and a meta-review summarized that the most common maximum dose was 8 sprays/3 h or 48 sprays/24 h in studies of spasticity, pain, nausea, and vomiting [60]. A possibility for IBD patients to undergo treatment with Cannabis/cannabinoids may be by intrarectal (IR) application. Preclinical studies in mice have shown an anti-inflammatory effect after IR application of CBD [18]. The IR route could reduce first pass effects and would allow cannabinoids to act also locally at receptors of the ECS which is highly represented in the bowel mucosa [35]. Doses of CBD have been evaluated in clinical studies of psychosis and anxiety and range between 200 and 800 mg/d [60]. Most common doses for dronabinol and nabilone were 5–30 mg/d (1–2 doses/d) and 2 mg 2× d, respectively, in studies of spasticity, pain, nausea, and vomiting [60].
5. Five-year view
Since the beginning of cannabinoid research, which is marked by the cloning of the CB1 receptor [70], the field has rapidly expanded, in particular, during the past decade. In 2011, the search term ‘cannabinoid’ yielded over 7000 hits in PubMed, the US National Library of Medicine, while this number has soared above 20,000 in 2016. However, for the gastroenterologist, it is sobering to realize that not even a 100 hits pop up when using the terms ‘cannabinoid’ and ‘inflammatory bowel disease'.
With increasing interest of the public and the attention of funding agencies, this will hopefully change in the years to come. By implementation of clinical trials on Cannabis/cannabinoids in IBD and the search for potential mechanisms of action in humans, the topic will certainly shift into the focus of the research community. On the preclinical side, we will gain more information on relevant basic mechanisms of cannabinoids in experimental IBD, for instance, on the role of CB receptors in the interaction of the microbiome with the gut epithelial barrier [71]. Although preliminary data on the efficacy of CBD in human CD do not appear to be promising [72], CBD still may find a way into treatment of IBD, after carefully evaluating dose and mode of application. From experimental data, FAAH inhibitors could hold high promise in the treatment of IBD [14,73,74]. However, human trials have failed to provide efficacy of these inhibitors [75]. In addition, the tragic incidence during the phase I trial for the FAAH inhibitor BIA 10-2474 has now hampered the translation of these drugs into humans, although up to that incident, other FAAH inhibitors were generally safe in human trials [76,77]. Here, we may have to come back to preclinical research to better understand the (patho-)physiological role of FAAH, and the mechanisms and caveats of these inhibitors.
The future will shed more light on drugs that directly target enzymes of the ECS to raise levels of endocannabinoids and other lipid compounds, such as PEA. Thus, exogenous PEA has been shown to reduce severity of experimental colitis [26]. Levels of PEA can be also increased endogenously in the colon via inhibition of N-acylethanolamine-hydrolyzing acid amidase leading to an improvement of experimental inflammation of the colon [27]. Certainly, inhibitors of MGL that raise endogenous levels of 2-AG will be in the focus during the years to come. IBD patients could benefit from such drugs through their antinociceptive and anti-inflammatory potential [78]. On the clinical side, we expect to see an increase in clinical studies (observational, controlled, and prospective) evaluating the efficacy of cannabinoid compounds in IBD. Some of the key questions are not answered yet, e.g. which patients would benefit the most from a treatment with cannabinoids and what the appropriate dosages and modes of application are. Other questions include the risks of long-term treatment and which group of patients should be excluded from treatment with cannabinoids.
There is an almost unanimous request in the current literature to conduct larger clinical trials to find out whether treatment with Cannabis/cannabinoids could provide benefit to the IBD patient. Cannabis is still rated as an illegal drug in most countries. However, because of the high public interest in cannabinoid-based medication, health-care providers, political institutions, and funding agencies hopefully will promote these kinds of studies by providing financial support and by easing legal barriers that still put patients and physicians in a semi-illegal position. For the researcher, one thing is certain: apart from THC and CBD, other anti-inflammatory compounds of the Cannabis plant are still waiting to be explored offering a vast and promising research area. However, physicians need definite proof that Cannabis/cannabinoids are effective in human IBD as well as guidelines for potential use. Fifty years after the discovery of THC by Raphael Mechoulam [79], the time is more than ripe.
Key issues
The GI tract accommodates all the relevant components of the endocannabinoid system and is therefore highly amenable to treatment with Cannabis/cannabinoids
Preclinical data in mouse models show that Cannabis/cannabinoids reduce the severity of colitis and relax intestinal hypercontractility through cannabinoid receptors and other components of the endocannabinoid system
Cannabis/cannabinoids not only act via classical cannabinoid receptors but also via GPR55, TRPV1, and PPAR receptors
To circumvent side effects of cannabinoid compounds, levels of endocannabinoids can be raised by inhibitors of endocannabinoid-degrading enzymes, such as FAAH and MGL. These enzymes are important drug targets in IBD.
Translation of preclinical data on cannabinoids in experimental IBD into humans has been insufficiently investigated warranting large clinical trials
Cannabis may be helpful in Crohn’s disease to ease abdominal pain but should be only considered after failure of standard medication and assessment of risks
Short term treatment with cannabinoids may cause common adverse effects like dry mouth, fatigue and dizziness but also serious adverse effects occur.
Until clinical trials do not provide evidence that IBD patients will benefit from a treatment with Cannabis/cannabinoids and before the questions of safety and tolerability are not solved, treatment with Cannabis/cannabinoids for IBD should not be recommended
Funding Statement
The authors were supported by the Austrian Science Fund (KLI 521-B31).
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
References
Papers of special note have been highlighted as either of interest (•) or of considerable interest (••) to readers.
- 1. Cosnes J, Gowerrousseau C, Seksik P, et al. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140(6):1785–1794. [DOI] [PubMed] [Google Scholar]
- 2. Engel MA, Neurath MF.. New pathophysiological insights and modern treatment of IBD. J Gastroenterol. 2010;45(6):571–583. [DOI] [PubMed] [Google Scholar]
- 3. Hasenoehrl C, Taschler U, Storr M, et al. The gastrointestinal tract - a central organ of cannabinoid signaling in health and disease. Neurogastroenterol Motil. 2016;28(12):1765–1780. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Good overview of the endocannabinoid system in the gastrointestinal tract and its role in functional and inflammatory bowel disorders as well as in colon cancer.
- 4. Izzo AA, Sharkey KA. Cannabinoids and the gut: new developments and emerging concepts. Pharmacol Ther. 2010;126(1):21–38. [DOI] [PubMed] [Google Scholar]
- 5. Schicho R, Storr M. Targeting the endocannabinoid system for gastrointestinal diseases: future therapeutic strategies. Expert Rev Clin Pharmacol. 2010;3(2):193–207. [DOI] [PubMed] [Google Scholar]
- 6. Di Marzo V. Targeting the endocannabinoid system: to enhance or reduce? Nat Rev Drug Discov. 2008;7:438–455. [DOI] [PubMed] [Google Scholar]
- 7. Di Marzo V, Piscitelli F. The endocannabinoid system and its modulation by phytocannabinoids. Neurotherapeutics. 2015;12(4):692–698. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Elegant overview of how the components of the endocannabinoid system could serve as drug targets in various diseases, such as depression, gastrointestinal inflammation, liver diseases, osteoporosis, neurogenereative disorders, and cancer.
- 8. Wirtz S, Neufert C, Weigmann B, et al. Chemically induced mouse models of intestinal inflammation. Nat Protoc. 2007;2(3):541–546. [DOI] [PubMed] [Google Scholar]
- 9. Stevceva L, Pavli P, Husband AJ, et al. The inflammatory infiltrate in the acute stage of the dextran sulphate sodium induced colitis: B cell response differs depending on the percentage of DSS used to induce it. BMC Clin Pathol. 2001;1(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alex P, Zachos NC, Nguyen T, et al. Distinct cytokine patterns identified from multiplex profiles of murine DSS and TNBS-induced colitis. Inflamm Bowel Dis. 2009;15 (3):341-352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. D’Argenio G, Valenti M, Scaglione G, et al. Up-regulation of anandamide levels as an endogenous mechanism and a pharmacological strategy to limit colon inflammation. FASEB J. 2006;20:568–570. [DOI] [PubMed] [Google Scholar]
- 12. Kimball ES, Schneider CR, Wallace NH, et al. Agonists of cannabinoid receptor 1 and 2 inhibit experimental colitis induced by oil of mustard and by dextran sulfate sodium. Am J Physiol Gastrointest Liver Physiol. 2006;291(2):G364–G371. [DOI] [PubMed] [Google Scholar]
- 13. Storr MA, Keenan CM, Emmerdinger D, et al. Targeting endocannabinoid degradation protects against experimental colitis in mice: involvement of CB1 and CB2 receptors. J Mol Med. 2008;86(8):925–936. [DOI] [PubMed] [Google Scholar]
- 14. Salaga M, Mokrowiecka A, Zakrzewski PK, et al. Experimental colitis in mice is attenuated by changes in the levels of endocannabinoid metabolites induced by selective inhibition of fatty acid amide hydrolase (FAAH). J Crohn’s Colitis. 2014;8(9):998–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alhouayek M, Lambert DM, Delzenne NM, et al. Increasing endogenous 2-arachidonoylglycerol levels counteracts colitis and related systemic inflammation. FASEB J. 2011;25 (8):2711-2721. [DOI] [PubMed] [Google Scholar]; •• Important study showing that blockade of MGL has protective effects against experimental colitis and endotoxemia.
- 16. Storr MA, Keenan CM, Zhang H, et al. Activation of the cannabinoid 2 receptor (CB2) protects against experimental colitis. Inflamm Bowel Dis. 2009;15(11):1678–1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jamontt JM, Molleman A, Pertwee RG, et al. The effects of d9-tetrahydrocannabinol and cannabidiol alone and in combination on damage, inflammation and in vitro motility disturbances in rat colitis. Br J Pharmacol. 2010;160(3):712–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Schicho R, Storr M. Topical and systemic cannabidiol improves trinitrobenzene sulfonic acid colitis in mice. Pharmacology. 2012;89(3–4):149–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Borrelli F, Aviello G, Romano B, et al. Cannabidiol, a safe and non-psychotropic ingredient of the marijuana plant Cannabis sativa, is protective in a murine model of colitis. J Mol Med. 2009;87(11):1111–1121. [DOI] [PubMed] [Google Scholar]
- 20. Pagano E, Capasso R, Piscitelli F, et al. An orally active Cannabis extract with high content in cannabidiol attenuates chemically-induced intestinal inflammation and hypermotility in the mouse. Front Pharmacol. 2016;7(341):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. De Filippis D, Esposito G, Cirillo C, et al. Cannabidiol reduces intestinal inflammation through the control of neuroimmune axis. PLoS One. 2011;6(12):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bisogno T, Hanus L, De Petrocellis L, et al. Molecular targets for cannabidiol and its synthetic analogues: effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br J Pharmacol. 2001;134(4):845–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Borrelli F, Fasolino I, Romano B, et al. Beneficial effect of the non-psychotropic plant cannabinoid cannabigerol on experimental inflammatory bowel disease. Biochem Pharmacol. 2013;85 (9):1306-1316. [DOI] [PubMed] [Google Scholar]
- 24. Schicho R, Bashashati M, Bawa M, et al. The atypical cannabinoid O-1602 protects against experimental colitis and inhibits neutrophil recruitment. Inflamm Bowel Dis. 2011;17(8):1651–1664. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Interesting study showing that cannabinoid-related compounds, such as O-1602, have protective effects in experimental forms of colitis independently of cannabinoid receptors and GPR55.
- 25. Stancic A, Jandl K, Hasenoehrl C, et al. The GPR55 antagonist CID16020046 protects against intestinal inflammation. Neurogastroenterol Motil. 2015;27(10):1432–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Borrelli F, Romano B, Petrosino S, et al. Palmitoylethanolamide, a naturally occurring lipid, is an orally effective intestinal anti-inflammatory agent. Br J Pharmacol. 2015;172:142–158. [DOI] [PMC free article] [PubMed] [Google Scholar]; •• Important study showing the effects of PEA in experimental IBD.
- 27. Alhouayek M, Bottemanne P, Subramanian KV, et al. N-acylethanolamine-hydrolyzing acid amidase inhibition increases colon N-palmitoylethanolamine levels and counteracts murine colitis. FASEB J. 2015;29(2):650–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Esposito G, Capoccia E, Turco F, et al. Palmitoylethanolamide improves colon inflammation through an enteric glia/toll like receptor 4-dependent PPAR-α activation. Gut. 2013;63(8):1300–1312. [DOI] [PubMed] [Google Scholar]; •• Another important study on the mechanisms of PEA in IBD also using human tissue.
- 29. Romano B, Borrelli F, Fasolino I, et al. The cannabinoid TRPA1 agonist cannabichromene inhibits nitric oxide production in macrophages and ameliorates murine colitis. Br J Pharmacol. 2013;169(1):213–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. De Petrocellis L, Ligresti A, Moriello AS, et al. Effects of cannabinoids and cannabinoid-enriched Cannabis extracts on TRP channels and endocannabinoid metabolic enzymes. Br J Pharmacol. 2011;163(7):1479–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Alhouayek M, Muccioli GG. The endocannabinoid system in inflammatory bowel diseases: from pathophysiology to therapeutic opportunity. Trends Mol Med. 2012;18(10):615–625. [DOI] [PubMed] [Google Scholar]
- 32. Izzo AA, Camilleri M. Cannabinoids in intestinal inflammation and cancer. Pharmacol Res. 2009;60:117–125. [DOI] [PubMed] [Google Scholar]
- 33. Leinwand KL, Gerich ME, Hoffenberg EJ, et al. Manipulation of the endocannabinoid system in colitis. Inflamm Bowel Dis. 2017;23(2):192–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Di Sabatino A, Battista N, Biancheri P, et al. The endogenous cannabinoid system in the gut of patients with inflammatory bowel disease. Mucosal Immunol. 2011;4(5):574–583. [DOI] [PubMed] [Google Scholar]
- 35. Marquéz L, Suárez J, Iglesias M, et al. Ulcerative colitis induces changes on the expression of the endocannabinoid system in the human colonic tissue. PLoS One. 2009;4(9):e6893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Stintzing S, Wissniowski TT, Lohwasser C, et al. Role of cannabinoid receptors and RAGE in inflammatory bowel disease. Histol Histopathol. 2011;26:735–745. [DOI] [PubMed] [Google Scholar]
- 37. Singh UP, Singh NP, Singh B, et al. Cannabinoid receptor-2 (CB2) agonist ameliorates colitis in IL-10−/- mice by attenuating the activation of T cells and promoting their apoptosis. Toxicol Appl Pharmacol. 2012;258(2):256–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Harvey BS, Nicotra LL, Vu M, et al. Cannabinoid CB2 receptor activation attenuates cytokine-evoked mucosal damage in a human colonic explant model without changing epithelial permeability. Cytokine. 2013;63(2):209–217. [DOI] [PubMed] [Google Scholar]
- 39. Lal S, Prasad N, Ryan M, et al. Cannabis use amongst patients with inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2011;23(10):891–896. [DOI] [PubMed] [Google Scholar]
- 40. Ravikoff Allegretti J, Courtwright A, Lucci M, et al. Marijuana use patterns among patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19(13):2809–2814. [DOI] [PMC free article] [PubMed] [Google Scholar]; • Comprehensive survey on the use of marijuana in IBD patients suggesting that marijuana is helpful in Crohn’s disease and also in ulceratice colitis.
- 41. Storr M, Devlin S, Kaplan GG, et al. Cannabis use provides symptom relief in patients with inflammatory bowel disease but is associated with worse disease prognosis in patients with Crohn’s disease. Inflamm Bowel Dis. 2014;20(3):472–480. [DOI] [PubMed] [Google Scholar]; • Survey on a large cohort of IBD patients who used Cannabis for the alleviation of pain and diarrhea. The study also highlights caveats for long-term use of Cannabis in IBD.
- 42. Lahat A, Lang A, Ben-Horin S. Impact of cannabis treatment on the quality of life, weight and clinical disease activity in inflammatory bowel disease patients: a pilot prospective study. Digestion. 2012;85(1):1–8. [DOI] [PubMed] [Google Scholar]
- 43. Phatak UP, Rojas-Velasquez D, Porto A, et al. Prevalence and patterns of marijuana use in young adults with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2017;64(2):261–264. [DOI] [PubMed] [Google Scholar]
- 44. Naftali T, Lev LB, Yablekovitz D, et al. Treatment of Crohn’s disease with cannabis: an observational study. Isr Med Assoc J. 2011;13(8):455–458. [PubMed] [Google Scholar]
- 45. Naftali T, Bar-Lev Schleider L, Dotan I, et al. Cannabis induces a clinical response in patients with Crohn’s disease: a prospective placebo-controlled study. Clin Gastroenterol Hepatol. 2013;11(10):1276–1280.e1. [DOI] [PubMed] [Google Scholar]; • First prospective and controlled clinical trial on THC and Crohn’s disease.
- 46. Kargl J, Andersen L, Hasenöhrl C, et al. GPR55 promotes migration and adhesion of colon cancer cells indicating a role in metastasis. Br J Pharmacol. 2016;173(1):142–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Alhamoruni A, Lee AC, Wright KL, et al. Pharmacological effects of cannabinoids on the Caco-2 cell culture model of intestinal permeability. J Pharmacol Exp Ther. 2010;335(1):92–102. [DOI] [PubMed] [Google Scholar]
- 48. Esposito G, Filippis DD, Cirillo C, et al. Cannabidiol in inflammatory bowel diseases: a brief overview. Phytother Res. 2013;27(5):633–636. [DOI] [PubMed] [Google Scholar]
- 49. Mowat C, Cole A, Windsor A, et al. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2011;60(5):571–607. [DOI] [PubMed] [Google Scholar]
- 50. Amiot A, Grimaud J-C, Peyrin-Biroulet L, et al. Effectiveness and safety of vedolizumab induction therapy for patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2016;14(11):1593–1601.e2. [DOI] [PubMed] [Google Scholar]
- 51. Armuzzi A, Gionchetti P, Daperno M, et al. Expert consensus paper on the use of vedolizumab for the management of patients with moderate-to-severe inflammatory bowel disease. Dig Liver Dis. 2016;48(4):360–370. [DOI] [PubMed] [Google Scholar]
- 52. Stallmach A, Hagel S, Bruns T. Adverse effects of biologics used for treating IBD. Best Pract Res Clin Gastroenterol. 2010;24(2):167–182. [DOI] [PubMed] [Google Scholar]
- 53. Varkas G, Thevissen K, De Brabanter G, et al. An induction or flare of arthritis and/or sacroiliitis by vedolizumab in inflammatory bowel disease: a case series. Ann Rheum Dis. 2016. DOI: 10.1136/annrheumdis-2016-210233 [DOI] [PubMed] [Google Scholar]
- 54. Hung A, Kang N, Bollom A, et al. Complementary and alternative medicine use is prevalent among patients with gastrointestinal diseases. Dig Dis Sci. 2015;60(7):1883–1888. [DOI] [PubMed] [Google Scholar]
- 55. Koning M, Ailabouni R, Gearry RB, et al. Use and predictors of oral complementary and alternative medicine by patients with inflammatory bowel disease: a population-based, case-control study. Inflamm Bowel Dis. 2013;19(4):767–778. [DOI] [PubMed] [Google Scholar]
- 56. Weiss A, Friedenberg F. Patterns of cannabis use in patients with inflammatory bowel disease: a population based analysis. Drug Alcohol Depend. 2015;156:84–89. [DOI] [PubMed] [Google Scholar]
- 57. Wallace JL, Flannigan KL, McKnight W, et al. Pro-resolution, protective and anti-nociceptive effects of a cannabis extract in the rat gastrointestinal tract. J Physiol Pharmacol. 2013;64(2):167–175. [PubMed] [Google Scholar]
- 58. Schicho R, Storr M. Cannabis finds its way into treatment of Crohn’s disease. Pharmacology. 2014;93(1–2):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Fichna J, Bawa M, Thakur GA, et al. Cannabinoids alleviate experimentally induced intestinal inflammation by acting at central and peripheral receptors. PLoS One. 2014;9(10):2–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456–2473. [DOI] [PubMed] [Google Scholar]
- 61. Polito JM, Childs B, Mellits ED, et al. Crohn’s disease: influence of age at diagnosis on site and clinical type of disease. Gastroenterology. 1996;111(3):580–586. [DOI] [PubMed] [Google Scholar]
- 62. Battistella G, Fornari E, Annoni J-M, et al. Long-term effects of cannabis on brain structure. Neuropsychopharmacology. 2014;39(9):2041–2048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Varner MW, Silver RM, Rowland Hogue CJ, et al. Association between stillbirth and illicit drug use and smoking during pregnancy. Obstet Gynecol. 2014;123(1):113–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Schicho R, Marsche G, Storr M. Cardiovascular complications in inflammatory bowel disease. Curr Drug Targets. 2015;16(3):181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Thomas G, Kloner RA, Rezkalla S. Adverse cardiovascular, cerebrovascular, and peripheral vascular effects of marijuana inhalation: what cardiologists need to know. Am J Cardiol. 2014;113(1):187–190. [DOI] [PubMed] [Google Scholar]
- 66. Alhamoruni A, Wright KL, Larvin M, et al. Cannabinoids mediate opposing effects on inflammationinduced intestinal permeability. Br J Pharmacol. 2012;165(8):2598–2610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Tourteau A, Andrzejak V, Body-Malapel M, et al. 3-Carboxamido-5-aryl-isoxazoles as new CB2 agonists for the treatment of colitis. Bioorganic Med Chem. 2013;21(17):5383–5394. [DOI] [PubMed] [Google Scholar]
- 68. McGilveray IJ. Pharmacokinetics of cannabinoids. Pain Res Manag. 2005;10 Suppl A:15A–22A. [DOI] [PubMed] [Google Scholar]
- 69. Voth EA, Schwartz RH. Medicinal applications of delta-9-tetrahydrocannabinol and marijuana. Ann Intern Med. 1997;126(10):791–798. [DOI] [PubMed] [Google Scholar]
- 70. Matsuda LA, Lolait SJ, Brownstein MJ, et al. Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature. 1990;346(6284):561–564. [DOI] [PubMed] [Google Scholar]
- 71. Cani PD, Plovier H, Van Hul M, et al. Endocannabinoids — at the crossroads between the gut microbiota and host metabolism. Nat Rev Endocrinol. 2016;12(3):133–143. [DOI] [PubMed] [Google Scholar]; • Excellent review discussing possible links between endocannabinoid system, gut microbiome, and metabolism.
- 72. Naftali T, Mechulam R, Lev LB, et al. Cannabis for inflammatory bowel disease. Dig Dis. 2014;32(4):468–474. [DOI] [PubMed] [Google Scholar]
- 73. Andrzejak V, Muccioli GG, Body-Malapel M, et al. New FAAH inhibitors based on 3-carboxamido-5aryl-isoxazole scaffold that protect against experimental colitis. Bioorg Med Chem. 2011;19(12):3777–3786. [DOI] [PubMed] [Google Scholar]
- 74. Shamran H, Singh NP, Zumbrun EE, et al. Fatty acid amide hydrolase (FAAH) blockade ameliorates experimental colitis by altering microRNA expression and suppressing inflammation. Brain Behav Immun. 2017;59:10–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Huggins JP, Smart TS, Langman S, et al. An efficient randomised, placebo-controlled clinical trial with the irreversible fatty acid amide hydrolase-1 inhibitor PF-04457845, which modulates endocannabinoids but fails to induce effective analgesia in patients with pain due to osteoarthritis of the knee. Pain. 2012;153(9):1837–1846. [DOI] [PubMed] [Google Scholar]
- 76. Bisogno T, Maccarrone M. Latest advances in the discovery of fatty acid amide hydrolase inhibitors. Expert Opin Drug Discov. 2013;8(5):509–522. [DOI] [PubMed] [Google Scholar]
- 77. Kaur R, Sidhu P, Singh S. What failed BIA 10-2474 phase I clinical trial? Global speculations and recommendations for future phase I trials. J Pharmacol Pharmacother. 2016;7(3):120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Mulvihill MM, Nomura DK. Therapeutic potential of monoacylglycerol lipase inhibitors. Life Sci. 2013;92(8–9):492–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mechoulam R, Gaoni Y. A total synthesis of DL-delta-1-tetrahydrocannabinol, the active constituent of hashish. J Am Chem Soc. 1965;87:3273–3275. [DOI] [PubMed] [Google Scholar]


