Abstract
We conducted a cross-sectional, Internet-based survey with a nationally representative sample of Japanese adults to assess the prevalence and characteristics of failed back surgery syndrome (FBSS). Data regarding the residual symptoms and patient satisfaction from an online survey of 1842 lumbar surgery patients revealed the prevalence of FBSS to be 20.6% (95% confidence interval [CI], 18.8–22.6). The prevalence of low back pain, dull ache, numbness, cold sensations, and paresthesia after surgery was 94.0%, 71.1%, 69.8%, 43.3%, and 35.3%, respectively. With a logistic regression model, severe residual low back pain (numerical rating scale 8–10), higher pain intensity, and multiple low back surgeries were strongly associated with FBSS, with odds ratios of 15.21 (95% CI, 7.79–29.7), 1.40 (95% CI, 1.32–1.49), and 1.87 (95% CI, 1.25–2.81), respectively. Respondents with FBSS had significantly lower EuroQol-5D (P<0.001) values and significantly higher scores on the Kessler six-item psychological distress scale (P<0.001), compared with the non-FBSS group. Our findings indicate that residual sensations have a significant effect on patient quality of life, similar to that of chronic low back pain. Precise presurgical provision of prognoses based on comprehensive epidemiologic data, as well as scrupulous attention to patient satisfaction and clinical progress may help reduce the incidence of FBSS.
Keywords: failed back surgery syndrome, patient satisfaction, prevalence, residual symptom, numbness
Introduction
Failed back surgery syndrome (FBSS) refers to a subset of patients who experience residual symptoms, such as chronic back pain, leg pain, or numbness, following one or more spinal surgeries.1,2 Indeed, a patient complaint or dissatisfaction due to residual symptoms after spinal surgery is essential for an FBSS diagnosis.
The most common symptom associated with FBSS is significant, long-lasting back pain. Dvorak et al3 studied 575 patients with symptomatic lumbar disc herniation (LDH) who underwent surgical procedures and found that 255 (70%) still complained of back pain, with 83 (23%) reporting constant heavy pain and 172 patients (45%) presenting with residual sciatica. Although many studies have investigated postoperative low back pain, data regarding the characteristics of the pain and abnormal sensations, such as numbness, coldness, or paresthesia in the lower extremities, and a dull ache in the lower back, are very limited. Indeed, symptoms aside from pain tend to be ignored, despite being frequently observed after spine surgery. To provide patients with comprehensive information about the residual symptoms that may occur after surgery, it is necessary to determine the prognosis of all symptoms, including low back pain as well as other abnormal sensations. Thus, our current research trajectory is focused on the collection of data regarding the characteristics of pain and abnormal sensations following spine surgery, with the goal of characterizing the outcome of these symptoms and their contribution to the onset or development of FBSS.
Previous reports have stated that FBSS affects approximately 10%–40% of patients who undergo back surgery.4–6 However, most prevalence rates were calculated based on the incidence of residual back and/or leg pain or the rate of reoperation. Malter et al also reported that 18% of 6376 patients in the USA who underwent lumbar fusion surgery for degenerative conditions underwent reoperation within the following 5 years.7 Kim et al conducted a cohort study of the incidence of reoperation, sourced from a national health insurance database. Among the 11,027 patients who had undergone lumbar spine surgery, 14.2% required reoperation at a 5-year follow-up assessment.8 Since not all surgical patients who experienced an unsuccessful outcome following a spine operation chose to undergo reoperation, the estimated incidence rate of FBSS could significantly exceed 20%.
It is impossible to estimate the prevalence of FBSS accurately using studies that focused on clinical features but did not address patient perspectives. To our knowledge, few studies have estimated the prevalence of FBSS based on both the presence of residual symptoms and patient satisfaction with low back surgery. North et al defined a successful surgical procedure for low back pain as one where at least 50% of patients experienced sustained pain relief and felt satisfied with the results. They reported that in a single facility, 34% of patients experienced a successful outcome after correction.1 In the present study, we assessed the prevalence of FBSS after low back surgery conducted in multiple facilities, based on various residual symptoms and patient satisfaction assessed by a nationwide Internet survey.
Our investigation had three aims: 1) to estimate the prevalence of FBSS based on both residual symptoms and patient perspectives; 2) to determine the characteristics of residual symptoms such as low back pain, dull ache, numbness, and cold sensations after lumbar spine surgery; and 3) to evaluate the negative impact of such residual symptoms on patient satisfaction with the surgery, health-related quality of life (HRQOL), and mental health. These epidemiologic data could provide new information about the experience of FBSS patients, and may lead to countermeasures in clinical medicine and public health.
Perspectives
We conducted a nationwide Internet survey in Japan to assess the relationships between various residual symptoms after low back surgery and FBSS. Numbness, dull ache, cold sensations, and paresthesia significantly affected patient quality of life (QOL), satisfaction, and mental health. The prevalence of FBSS was 20.6% in 1842 respondents.
Materials and methods
Participants and procedures
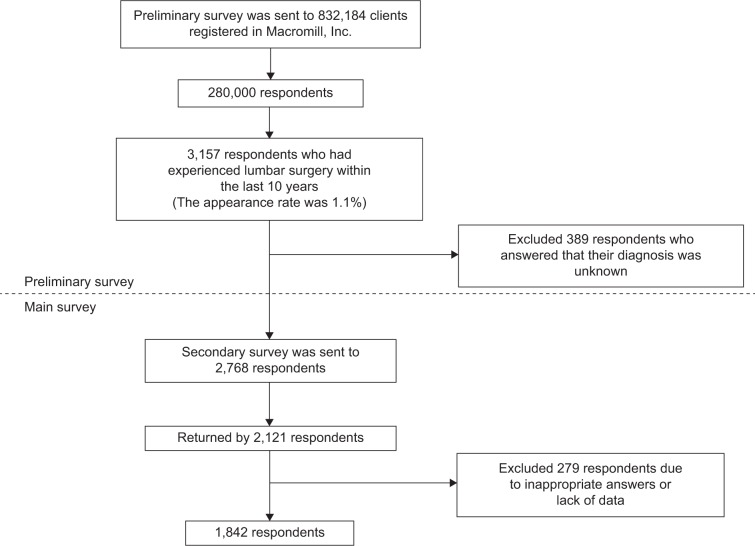
This Internet-based survey was initiated in December 2012 in Japan. The survey was performed by Macromill Inc., which is a leading Internet research company in Japan and has over 2,600,000 clients. We carried out a preliminary survey for the selection of participants and an in-depth investigation to gather detailed information. A total of 1842 participants were selected, as detailed in Figure 1.
Figure 1.
Flowchart of participant recruitment.
Preliminary survey
We administered a preliminary survey to a subset of 1,100,000 members aged 20 or over who had registered with the Internet monitor system (the Macromill research monitor, www.macromill.com/global/index.html) and agreed to participate in health-related surveys upon registration. Recruitment was conducted with the goal of sampling a wide range of diverse participants living in different areas across Japan, to avoid an institutional or regional bias. Individuals were invited to participate in this survey by email. They received an email containing the details of the survey, and if they agreed to participate and provided informed consent by clicking a corresponding link, a screening survey began immediately.
Individuals who answered “yes” to the following three questions were included in the study: “Have you undergone lumbar surgery with a skin incision under general anesthesia?”, “If so, was this surgery within the last 10 years?”, and “Was the disease that led to the operation one of the following eight diseases: lumbar disc herniation (LDH), lumbar spinal canal stenosis, lumbar spondylolisthesis, lumbar infection, lumbar fracture, tumor, low back pain, lumbar scoliosis?” Of the 832,184 registrants whom we contacted, 280,000 persons agreed to participate in this survey and 3157 respondents answered “yes” to all three questions (an appearance rate of 1.1%). We excluded 389 respondents who answered “Disease unknown” or “Other disease”. Based on the preliminary survey, 2768 participants fulfilled our inclusion criteria.
Main survey
We asked the 2768 participants to complete an in-depth questionnaire. Before administering the main survey, we verified that the participants were interested in participation by telephone. A total of 2121 people (response rate 76.6%) returned the questionnaire. We carefully evaluated the responses and excluded 274 respondents due to insufficient comprehension of the questions, inappropriate answers, or lack of data. Valid responses were eventually obtained from 1842 participants (1321 females and 521 males). All participants who had registered to the main survey received a book coupon worth about US$5 as compensation.
Questionnaire
We surveyed the participants with a self-completed questionnaire that was administered through the Internet. The survey was developed through piloting and validation. The questionnaire included items regarding patient background characteristics (i.e., age, sex, indication for surgery, preoperative symptoms), ratings of changes in symptoms after the surgery, satisfaction with the surgery, and current QOL and mood. The questions regarding residual symptoms addressed five symptom types: low back pain (including buttock pain), low back dul ache, numbness in the legs, coldness, and paresthesia in the feet. The intensity of low back pain was reported using an eleven-point numerical rating scale (0=no pain, 10=worst pain imaginable). Low back pain scores were divided into four groups based on pain intensity as follows: numerical rating scale (NRS) 0, none; NRS 1–4, mild pain; NRS 4–7, moderate pain; NRS 8–10, severe pain.9
Outcome score
The outcome of each residual symptom was ranked using four categories (disappeared, completely cured; improved, partially cured; no change, unchanged or very little change; worsened, aggravated compared with the preoperative degree) before and after the surgical operation. To compare the symptoms before vs. after surgery, we calculated the outcome scores based on the presence of preoperative symptoms and the course of symptoms, as shown in Table 1.
Table 1.
Outcome scores
| Preoperative | Change after surgery | Outcome scores |
|---|---|---|
| Symptom+ | Disappeared | +2 |
| Improved | +1 | |
| No change | −1 | |
| Worsened | −2 | |
| No symptom | Disappeared | – |
| Improved | – | |
| No change | – | |
| Worsened | −2 |
Patient satisfaction
Respondents were asked to rate their level of satisfaction for each item (i.e., very dissatisfied, somewhat dissatisfied, somewhat satisfied, or very satisfied). We created a two-category satisfaction outcome by organizing the respondents into two groups based on their response to the overall satisfaction question. Specifically, we grouped respondents who answered “very dissatisfied” or “somewhat dissatisfied” into the dissatisfaction group, and those who answered “somewhat satisfied” or “very satisfied” into the satisfaction group.
HRQOL: EuroQol-5 dimensions
Our questionnaire measured the QOL and levels of distress. Specifically, we assessed subjective HRQOL using the “EuroQol-5 dimensions” (EQ-5D) scale.10 This instrument contains descriptions of health status in five dimensions: “mobility”, “self-care”, “usual activities”, “pain/complaints”, and “anxiety/depression”. Each dimension has three degrees of response or severity (no problems, some problems, extreme problems). The combination of responses enables the description of 243 different health states, with a set of values ranging from 1 (no problem in any dimension) to −0.111 (severe problems in all five dimensions) anchored by 0 (death) and 1 (full health), with a higher score indicating greater health. The Japanese version of the instrument was developed by the Japanese EuroQol Translation Team.11
Psychological distress: the Kessler psychological distress scale
Our questionnaire included the six-item Kessler psychological distress scale (K6) to assess psychological status.12 The K6 includes items that measure the presence of nervousness, hopelessness, irritability, negative affect, fatigue, and worthlessness experienced over the past 30 days. Items are rated on a five-point scale, with 0 indicating the absence of a symptom and 4 indicating that the symptom was present all of the time during the past 30 days. The final K6 score can range from 0 to 24, with higher scores indicating higher levels of psychological distress. A K6 score over 5 is considered to be a risk factor for a mood disorder in the Japanese population.13
Statistical analyses
The data were analyzed using IBM SPSS Statistics for Windows, Version 21.0 for Windows (IBM Corp., Armonk, NY, USA). Continuous data were reported as the mean ± standard deviation (SD) if normally distributed and as the median and interquartile range if not normally distributed. Analyses of variance, Student’s unpaired t-tests, and Mann–Whitney U tests were used where appropriate. Categorical data were represented as n (%) and analyzed using Fisher’s exact test. We calculated the Spearman correlation coefficient to test the relationships between variables.
We performed simultaneous logistic regression analysis to evaluate the effect of specific demographic characteristics and social factors, as well as disease variables, on pain status. The analysis produced odds ratios and their 95% confidence intervals (CIs). Values of P <0.05 were considered statistically significant in all analyses.
The present study was carried out in accordance with the latest version of the Declaration of Helsinki and approved by the Institutional Review Board at Aichi Medical University, Aichi, Japan. All participants provided informed consent online after receiving a complete description of the study.
Results
Demographic background data
We obtained a total of 1842 useable questionnaires from validated respondents, making the overall corrected response rate 66.5% for the main survey. The respondents consisted of 1321 males and 521 females, with a mean age of 42.6 years (range 20–89 years). The demographic characteristics of the respondents are shown in Table 2. The most common diagnosis leading to surgery (only one answer was allowed) was LDH (69.1%), followed by lumbar canal stenosis (14.1%), and spondylolisthesis (4.7%). In total, 412 respondents (22.4%) underwent fixation surgery and the remaining 1294 respondents (70.2%) underwent decompression surgery without fixation. Nearly one in five respondents (18.4%) reported receiving multiple back surgeries.
Table 2.
Characteristics of all respondents, including those with and without FBSS
| Social and demographic characteristics | Overall, N=1842 (%) | Non-FBSS, n=1462 (%) | FBSS, n=380 (%) | P-value |
|---|---|---|---|---|
| Sex | ||||
| Male | 1321 (71.7) | 1041 (71.2) | 280 (73.7) | 0.371a |
| Female | 521 (28.3) | 421 (28.8) | 100 (26.3) | |
| Age, years (mean±SD) | ||||
| <65 (%) | 1679 (91.2) | 1349 (92.3) | 330 (86.8) | <0.005a |
| ≥65 (%) | 163 (8.8) | 113 (7.7) | 50 (13.2) | |
| Average±SD | 42.6±14.4 | 41.7±14.0 | 45.8±15.3 | <0.001c |
| Severity of low back pain | ||||
| None | 146 (7.9) | 135 (9.2) | 11 (2.9) | <0.001b |
| Mild pain (1–3) | 667 (36.2) | 577 (39.5) | 90 (23.7) | |
| Moderate pain (4–7) | 803 (43.6) | 616 (42.1) | 187 (49.2) | |
| Severe pain (8–10) | 226 (12.3) | 134 (9.2) | 92 (24.2) | |
| Pain intensity (NRS 0–10) (average±SD) | 4.3±2.6 | 4.0±2.6 | 5.4±2.5 | <0.001c |
| Surgical diagnosis (n) | ||||
| Disc herniation | 1273 (69.1) | 1045 (71.5) | 228 (60.0) | <0.001a |
| Canal stenosis | 260 (14.1) | 183 (12.5) | 77 (20.3) | <0.001a |
| Spondylolisthesis | 87 (4.7) | 59 (4.0) | 28 (7.4) | <0.01a |
| Low back pain | 68 (3.7) | 59 (4.0) | 9 (2.4) | 0.168a |
| Fracture | 52 (2.8) | 41 (2.8) | 11 (2.9) | 0.863a |
| Tumor | 27 (1.5) | 21 (1.4) | 6 (1.6) | 0.812a |
| Spondylolysis | 27 (1.5) | 19 (1.3) | 8 (2.1) | 0.236a |
| Infection | 16 (1.1) | 10 (0.7) | 6 (1.6) | 0.116a |
| Scoliosis | 12 (0.9) | 10 (0.7) | 2 (0.5) | >0.999a |
| Others | 20 (0.7) | 15 (1.0) | 5 (1.3) | 0.584a |
| Number of operations | ||||
| 1 | 1503 (81.6) | 1233 (84.3) | 270 (71.1) | <0.001a |
| ≥2 | 339 (18.4) | 229 (15.7) | 110 (28.9) | |
| Period from surgery, weeks (average±SD) | 167.9±132.9 | 167.7±133.0 | 168.8±133.0 | 0.879c |
| Surgery | ||||
| Fusion | 412 (22.4) | 308 (21.1) | 104 (27.4) | <0.01a |
| Decompression | 1294 (70.2) | 1046 (71.5) | 248 (65.3) | |
| Unknown | 136 (7.4) | 108 (7.4) | 28 (7.4) | |
| Utility value of EQ-5D (average±SD) | 0.79±0.19 | 0.83±0.17 | 0.65±0.17 | <0.001c |
| K6 score (average±SD) | 5.7±4.9 | 5.2±4.7 | 7.7±5.2 | <0.001c |
Notes: P-value:
Fisher’s exact test;
Mann–Whitney U test;
unpaired t-test. Participants were considered FBSS if they fulfilled two conditions: “dissatisfied” or “somewhat dissatisfied” with their surgery on a four-grade scale and the existence of at least one symptom in any residual symptoms (low back pain, low back dull ache, numbness in legs, coldness in feet, or paresthesia on the sole).
Abbreviations: EQ-5D, EuroQol-5 dimensions; FBSS, failed back surgery syndrome; K6, Kessler psychological distress scale; SD, standard deviation.
We found no significant differences in the sex ratio of individuals with vs. without FBSS. However, FBSS was more likely to occur in individuals who were older than 65 years (P=0.002). The mean intensity of residual low back pain was significantly higher in the FBSS group. Also, FBSS was more frequent in respondents with spinal fusion and those who had undergone multiple operations, compared with the respondents with decompression and those who had received a single operation. Respondents with FBSS had significantly lower EQ-5D values (0.65±0.17) compared with those without FBSS (0.83±0.17, P<0.001), as well as significantly higher K6 scores (7.7±5.2, P<0.001), with a mean that was above the threshold for anxiety disorder (i.e., a score of 5).14
Prevalence and characteristics of residual symptoms
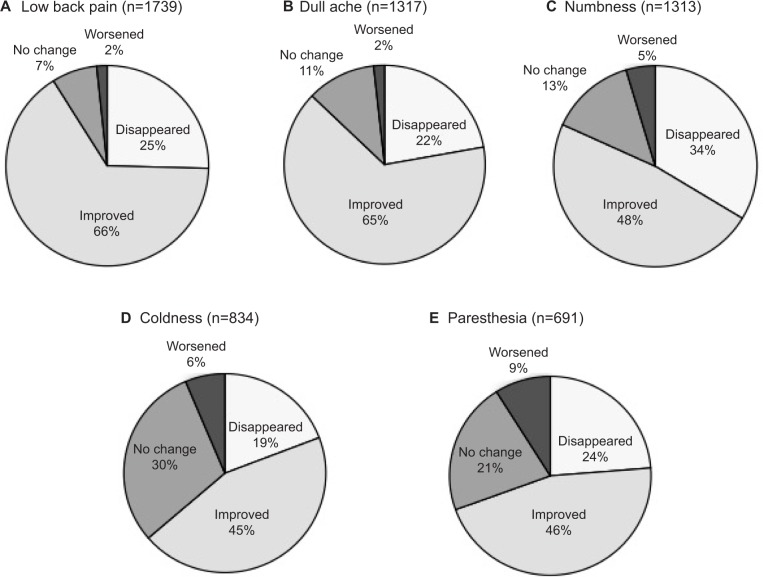
The preoperative prevalence rates of low back pain, low back dull ache, numbness, coldness, and paresthesia before surgery were 94.0% (95% CI, 92.8–95.0), 71.1% (95% CI, 68.9–73.1), 69.8% (95% CI, 67.7–71.9), 43.3% (95% CI, 41.0–45.6), and 35.3% (95% CI, 33.2–37.6), respectively. The outcomes of the five preoperative symptoms are shown in Figure 2. The percentage of respondents who answered that low back pain, dull ache, numbness, coldness, and paresthesia disappeared after surgery was 25.4% (95% CI, 23.4–27.5), 22.2% (95% CI, 20.0–24.5), 33.7% (95% CI, 31.1–36.3), 19.2% (95% CI, 16.6–22.0), and 23.7% (95% CI, 20.6–27.1), respectively. Respondents were more likely to report “no symptom change” or that the symptom “worsened” for coldness and paresthesia compared with the other three symptoms.
Figure 2.
Clinical outcomes of five preoperative symptoms.
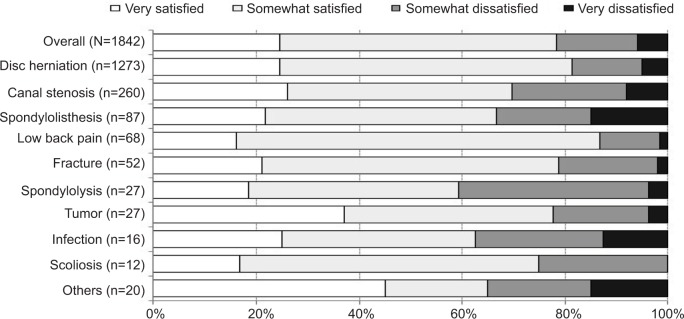
Patient satisfaction
In total, 78.4% of all respondents expressed satisfaction (very satisfied or somewhat satisfied) with their lumbar surgery (Figure 3). Across all nine surgical diagnoses, surgery for low back pain and disc herniation had the highest satisfaction rate. Respondents who underwent surgery for spondylolysis (40.7%) and infection (37.5%) reported relatively low satisfaction rates.
Figure 3.
Patient satisfaction with lumbar spine surgery by surgical diagnosis.
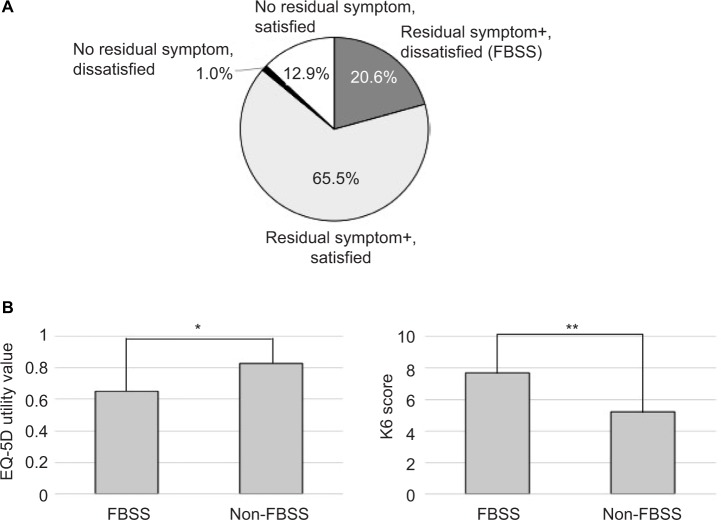
Prevalence of FBSS
Respondents were considered to have FBSS if they fulfilled the following two conditions: 1) they answered that they were very dissatisfied or somewhat dissatisfied in terms of their patent satisfaction with the surgery and 2) they reported at least one unpleasant abnormal sensation after the operation. The overall prevalence rate of FBSS was 20.6% (95% CI, 18.8–22.6) after all types of low back surgery combined (Figure 4A). When the participants were classified into FBSS and non-FBSS groups, the EQ-5D health status of the FBSS group was significantly lower than that in the non-FBSS group (Figure 4B). K6 scores in the FBSS group were also significantly higher than those in the non-FBSS group, suggesting that individuals with FBSS are more likely to experience psychological distress or depression (Figure 4B).
Figure 4.
(A) Patient satisfaction with lumbar spine surgery by surgical diagnosis. (B) Prevalence of FBSS in a Japanese population; and influence of FBSS on health-related quality of life and psychological distress. P-values by unpaired t-test: *P<0.001; **P<0.05.
Abbreviations: EQ-5D, EuroQol-5 dimensions; FBSS, failed back surgery syndrome; K6, Kessler psychological distress scale.
The burden of residual low back pain
Respondents had undergone surgery at an average of 3.4 years prior to our assessment, and reported a mean intensity of residual low back pain of 4.3±2.6. A total of 226 respondents reported experiencing severe pain (12.3%), 803 reported moderate pain (43.6%), and 667 reported mild pain (36.2%). A total of 146 respondents (7.9%) reported no pain in the low back.
The outcome score
The estimated outcome scores for abnormal residual symptoms (pain, dull ache, numbness, coldness, and paresthesia) are shown in Figure 5. The overall outcome scores for low back pain, low back dull ache, numbness, coldness, and paresthesia were 1.0±0.8, 0.7±0.9, 0.7±1.0, 0.2±0.9, and 0.2±0.8, respectively. This indicates that coldness and paresthesia showed the smallest improvement after low back surgery. The outcome score varied somewhat according to the surgical diagnosis. Respondents who had surgery due to a fracture, tumor, or infection had relatively lower outcome scores for all symptoms, compared with the overall average.
Figure 5.
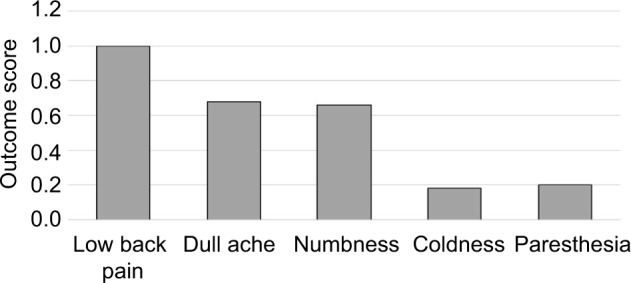
Average outcome scores of residual symptoms.
Table 3 shows the correlations between residual symptoms and patient satisfaction in terms of the mean EQ-5D health status and mean K6 scores. We observed direct correlations between patient satisfactions and outcome scores for all residual symptoms. The correlations between patient satisfaction and outcome scores for each residual symptom were as follows: low back pain: Spearman’s ρ=0.537, P<0.001; low back dull ache: Spearman’s ρ=0.464, P<0.001; numbness in the legs: Spearman’s ρ=0.448, P<0.001; coldness in the feet: Spearman’s ρ=0.373, P<0.001; and paresthesia in the feet: Spearman’s ρ=0.427, P<0.001. Compared with the other symptoms, the increase in the outcome score for low back pain after surgery was more strongly related to the increase in EQ-5D health status (Spearman’s ρ=0.420, P<0.001). In terms of mental status, the increase in the outcome score for dull pain was more strongly related to the increase in K6 score, compared with the other symptoms.
Table 3.
Spearman rank-order correlations of outcome variables with patient satisfaction, EQ-5D, and K6 scores
| Outcome score | FBSS
|
Patient satisfaction
|
EQ-5D
|
K6
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Correlation (Q) | P-value | n | Correlation (Q) | P-value | n | Correlation (Q) | P-value | n | Correlation (Q) | P-value | n | |
| Low back pain | −0.407 | <0.001 | 1739 | 0.537 | <0.001 | 1739 | 0.420 | <0.001 | 1739 | −0.240 | <0.001 | 1739 |
| Dull ache | −0.351 | <0.001 | 1317 | 0.464 | <0.001 | 1317 | 0.410 | <0.001 | 1317 | −0.271 | <0.001 | 1317 |
| Numbness | −0.380 | <0.001 | 1313 | 0.448 | <0.001 | 1313 | 0.379 | <0.001 | 1313 | −0.223 | <0.001 | 1313 |
| Coldness | −0.304 | <0.001 | 834 | 0.373 | <0.001 | 834 | 0.313 | <0.001 | 834 | −0.200 | <0.001 | 834 |
| Paresthesia | −0.364 | <0.001 | 691 | 0.427 | <0.001 | 691 | 0.324 | <0.001 | 691 | −0.119 | <0.001 | 691 |
Notes: Whole sample, N=1842. We excluded participants with outcome scores of 0. Connections between abnormal sensory symptoms (i.e., pain, dull ache, numbness, coldness, and paresthesia) and patient satisfaction, as well as EQ-5D and K6 scores were calculated using Spearman’s rank correlations.
Abbreviations: EQ-5D, EuroQol-5 dimensions; FBSS, failed back surgery syndrome; K6, Kessler psychological distress scale.
Risk factors for developing FBSS
Table 4 shows the results of our multivariate logistic regression analysis of independent risk factors for developing FBSS. After adjusting for age and sex, the logistic regression model revealed that severe low back pain (NRS 8–10) was most strongly associated with FBSS, with an odds ratio of 15.21 (95% CI, 7.79–29.7; P<0.001). Each successive category in the NRS showed an increasingly larger significant correlation with FBSS in terms of low back pain intensity, with an odds ratio of 1.40 (95% CI, 1.32–1.49; P<0.001). In addition, a history of multiple low back surgeries was the strongest independent factor associated with FBSS, with an odds ratio of 1.87 (95% CI, 1.25–2.81; P<0.001). Spinal fusion surgery (vs. decompression surgery) was correlated with a risk of FBSS with an odds ratio of 1.12 (95% CI, 0.8–1.57; P<0.001), but this was not a significantly independent risk factor (P=0.496).
Table 4.
Multivariable logistic regression analyses of characteristics associated with FBSS after low back surgery
| FBSS
|
||||||
|---|---|---|---|---|---|---|
| Univariate
|
Adjusted for age and sex
|
|||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Sex | ||||||
| Female (vs. male) | 0.883 | 0.684–1.139 | 0.339 | – | – | – |
| Age | ||||||
| Age ≥65 (vs. <65) | 1.809 | 1.270–2.577 | <0.002 | – | – | – |
| Age (10 per year old) | 1.214 | 1.124–1.311 | <0.001 | – | – | – |
| Currently married (vs. unmarried) | 1.167 | 0.919–1.483 | 0.206 | 0.877 | 0.671–1.147 | 0.338 |
| The intensity of residual low back pain | ||||||
| None | 1.000 | Ref | 1.000 | Ref | ||
| Mild | 1.914 | 0.996–3.680 | 0.051 | 2.187 | 1.132–4.223 | <0.02 |
| Moderate (vs. mild) | 3.726 | 1.972–7.037 | <0.001 | 4.684 | 2.459–8.924 | <0001 |
| Severe (vs. mild) | 8.426 | 4.314–6.457 | <0.001 | 10.068 | 5.115–19.820 | <0.001 |
| NRS of residual low back pain (per 1) | 1.231 | 1.176–1.288 | <0.001 | 1.250 | 1.194–1.308 | <0.001 |
| The outcome of low back pain | ||||||
| Disappeared | 0.121 | 0.070–0.210 | <0.001 | 0.110 | 0.063–0192 | <0.001 |
| Improved | 1.000 | Ref | 1.000 | Ref | ||
| No change | 7.186 | 5.053–10.218 | <0.001 | 6.848 | 4.792–9.787 | <0.001 |
| Worsened | 7.412 | 3.402–16.146 | <0.001 | 6.843 | 3.110–15.056 | <0.001 |
| The outcome of dull ache in low back | ||||||
| Disappeared | 0.372 | 0.246–0.562 | <0.001 | 0.350 | 0.231–0.531 | <0.001 |
| Improved | 1.000 | Ref | 1.000 | Ref | ||
| No change | 2.743 | 2.131–3.530 | <0.001 | 2.632 | 2.040–3.395 | <0.001 |
| Worsened | 5.083 | 2.206–11.708 | <0.001 | 5.097 | 2.183–11.902 | <0.001 |
| The outcome of numbness in legs | ||||||
| Disappeared | 0.324 | 0.227–0.463 | <0.001 | 0.317 | 0.221–0.455 | <0.001 |
| Improved | 1.000 | Ref | 1.000 | Ref | ||
| No change | 1.488 | 1.147–1.930 | <0.003 | 1.575 | 1210–2.051 | <0.001 |
| Worsened | 4.356 | 2.350–7.440 | <0.001 | 4.087 | 2.375–7.035 | <0.001 |
| The outcome of coldness in feet | ||||||
| Disappeared | 0.607 | 0.396–0.931 | <0.03 | 0.585 | 0.380–0.899 | <0.02 |
| Improved | 1.000 | Ref | 1.000 | Ref | ||
| No change | 1.540 | 1.158–2.047 | <0.003 | 1.476 | 1.108–1.966 | <0.01 |
| Worsened | 5.995 | 3.311–10.854 | <0.001 | 5.600 | 3.072–10.209 | <0.001 |
| The outcome of paresthesia in feet | ||||||
| Disappeared | 0.354 | 0.227–0.554 | <0.001 | 0.347 | 0.222–0.543 | <0.001 |
| Improved | 1.000 | Ref | 1.000 | Ref | ||
| No change | 1.029 | 0.775–1.366 | 0.842 | 0.993 | 0.746–1320 | 0.959 |
| Worsened | 5.071 | 2.897–8.877 | <0.001 | 4.636 | 2.622–8.197 | <0.001 |
| Multiple low back surgery (vs. single low back surgery) | 2.194 | 1.687–2.853 | <0.001 | 2.337 | 1.789–3.053 | <0.001 |
| Spinal fusion surgery (vs. decompression surgery) | 1.424 | 1.096–1.850 | <0.01 | 1.380 | 1.059–1.798 | <0.02 |
| EQ-5D utility value (per 0.1) | 0.563 | 0.521–0.609 | <0.001 | 0.557 | 0.514–0.603 | <0.001 |
| K6 score (per 1) | 1.099 | 1.075–1.124 | <0.001 | 1.117 | 1.091–1.143 | <0.001 |
Note: Participants were considered satisfied with their low back surgery if they replied that they were “satisfied” or “somewhat satisfied” on a four-grade scale. Dash (–) means not applicable.
Abbreviations: CI, confidence interval; EQ-5D, EuroQol-5 dimensions; FBSS, failed back surgery syndrome; K6, Kessler psychological distress scale; OR, odds ratio; Ref, reference.
Logistic regression analysis of patient satisfaction
To further identify the predictors of patient satisfaction, we performed logistic regression analysis, after adjusting for age and sex, to estimate the odds ratio and 95% CI (Table 5). In the logistic regression model, patient satisfaction after low back surgery was associated with age, the intensity of residual low back pain, the outcome scores for all residual symptoms, a history of multiple low back surgeries, and spinal fusion surgery. Patient satisfaction was also associated with EQ-5D health status and K6 score (P<0.001).
Table 5.
Multivariable logistic regression of factors associated with patient satisfaction after low back surgery
| Patient satisfaction
|
||||||
|---|---|---|---|---|---|---|
| Univariate
|
Adjusted for age and sex
|
|||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Sex | ||||||
| Female (vs. male) | 1.129 | 0.879–1.450 | 0.341 | – | – | – |
| Age, years | ||||||
| Age ≥65 (vs. <65) | 0.591 | 0.415–0.841 | <0.005 | – | – | – |
| Age (10 per year old) | 0.841 | 0.779–0.907 | <0.001 | – | – | – |
| Currently married (vs. unmarried) | 0.920 | 0.729–1.163 | 0.487 | 1.205 | 0.927–1.566 | 0.163 |
| The intensity of residual low back pain | ||||||
| None | 1.000 | Ref | 1.000 | Ref | ||
| Mild | 0.485 | 0.253–0.930 | <0.05 | 0.429 | 0.223–0.826 | <0.05 |
| Moderate (vs. mild) | 0.252 | 0.134–0.476 | <0.001 | 0.205 | 0.108–0.390 | <0.001 |
| Severe (vs. mild) | 0.112 | 0.058–0.219 | <0.001 | 0.096 | 0.049–0.188 | <0.001 |
| NRS of residual low back pain (per 1) | 0.816 | 0.780–0.853 | <0.001 | 0.804 | 0.769–0.841 | <0.001 |
| The outcome of low back pain | ||||||
| Disappeared | 5.003 | 3.216–7.785 | <0.001 | 5403 | 3.462–8.432 | <0.001 |
| Improved | 1.000 | Ref | 1.000 | Ref | ||
| No change | 0.120 | 0.083–0.171 | <0.001 | 0.125 | 0.087–0.180 | <0.001 |
| Worsened | 0.137 | 0.063–0.298 | <0.001 | 0.148 | 0.067–0.324 | <0.001 |
| The outcome of dull ache in low back | ||||||
| Disappeared | 2.103 | 1.444–3.062 | <0.001 | 2.210 | 1.514–3.226 | <0.001 |
| Improved | 1.000 | Ref | 1.000 | Ref | ||
| No change | 0.348 | 0.271–0.448 | <0.001 | 0.362 | 0.281–0.466 | <0.001 |
| Worsened | 0.201 | 0.087–0.463 | <0.001 | 0.201 | 0.086–0.467 | <0.001 |
| The outcome of numbness in legs | ||||||
| Disappeared | 2.560 | 1.829–3.583 | <0.001 | 2.601 | 1.856–3.647 | <0.001 |
| Improved | 1.000 | Ref | 1.000 | Ref | ||
| No change | 0.642 | 0.496–0.831 | <0.001 | 0.610 | 0.470–0.792 | <0.001 |
| Worsened | 0.234 | 0.137–0.399 | <0.001 | 0.248 | 0.144–0.425 | <0.001 |
| The outcome of coldness in feet | ||||||
| Disappeared | 1.572 | 1.037–2.382 | <0.005 | 1.624 | 1.070–2.466 | <0.005 |
| Improved | 1.000 | Ref | 1.000 | Ref | ||
| No change | 0.637 | 0.482–0.844 | <0.005 | 0.662 | 0.499–0.877 | <0.005 |
| Worsened | 0.175 | 0.097–0,316 | <0.001 | 0.185 | 0.102–0.337 | <0.001 |
| The outcome of paresthesia in feet | ||||||
| Disappeared | 2.527 | 1.655–3.860 | <0.001 | 2.571 | 1.681–3.932 | <0.001 |
| Improved | 1.000 | Ref | 1.000 | Ref | ||
| No change | 0.982 | 0.743–1.298 | 0.900 | 1.014 | 0.766–1.342 | 0.922 |
| Worsened | 0.209 | 0.120–0.366 | <0.001 | 0.227 | 0.129–0.400 | <0.001 |
| Multiple low back surgeries (vs. single low back surgery) | 0.460 | 0.355–0.596 | <0.001 | 0.435 | 0.334–0.566 | <0.001 |
| Spinal fusion surgery (vs. decompression surgery) | 0.710 | 0.548–0.920 | <0.05 | 0.731 | 0.563–0.949 | <0.05 |
| EQ-5D utility value (per 0.1) | 1.787 | 1.653–1.932 | <0.001 | 1.804 | 1.668–1.952 | <0.001 |
| K6 score (per 1) | 0.912 | 0.892–0.932 | <0.001 | 0.899 | 0.879–0.919 | <0.001 |
Note: Participants were considered satisfied with their low back surgery if they replied that they were “satisfied” or “somewhat satisfied” on a four-grade scale. Dash (–) means not applicable.
Abbreviations: CI, confidence interval; EQ-5D, EuroQol-5 dimensions; K6, Kessler psychological distress scale; OR, odds ratio; Ref, reference.
Discussion
This is the first nationwide survey of the prevalence and characteristics of residual low back pain, low back dull ache, numbness in the legs, and coldness and paresthesia in the feet following low back surgery. Although many studies have investigated residual symptoms after low back surgery, these have mainly focused on residual pain in the low back and/or legs.15–17 Thus, cross-sectional epidemiologic data regarding residual unpleasant sensations such as low back dull ache, numbness in the legs, and coldness and paresthesia in the feet, are lacking. According to our outcome scores, low back pain was the symptom that was expected to show the greatest improvement after surgery. Conversely, abnormal sensations, especially coldness and paresthesia, were less likely to subside and tended to sustain for a long period after surgery.
Huang and Sengupta followed the course of recovery of different sensory symptoms (pain, numbness, and paresthesia) after lumbar nerve root decompression. They found that numbness and paresthesia improved at a much slower speed compared with pain.18 Pathologically, paresthesia and abnormal sensations or discomfort are thought to arise from damage or oversensitization of A-delta fibers, which are myelinated, relatively larger fibers that convey touch, pressure, and pain sensations. Alternatively, pain is mainly transmitted by C-fibers, which are smaller sensory fibers without myelin sheaths.19 The recovery rate of small, unmyelinated nerve fibers (C-fibers) involved in pain is faster and more complete than that of the myelinated nerve fibers (A-delta) involved in numbness and tingling symptoms.20 Thus, to ensure that patients have realistic expectations about surgery outcomes; surgeons should inform patients preoperatively about the difficulty of recovery with respect to these particular symptoms.
Our data indicate that both residual pain and abnormal sensations can decrease patient satisfaction regarding surgery outcomes, as shown in Table 4. Our adjusted multivariable logistic regression analysis of overall patient satisfaction revealed that the odds ratio of a respondent indicating “no change” in a symptom after surgery was the lowest (0.125) for pain and the highest for paresthesia (1.014). Also, as residual pain intensity increased, the odds ratio of patient satisfaction decreased substantially. This suggests that residual low back pain is the symptom, most closely related to patient satisfaction. However, as shown in Table 3, the outcome score for residual paresthesia after surgery is also correlated with patient satisfaction (ρ=0.427), indicating that this symptom should be thoroughly discussed with patients before surgery. Overall, when the symptoms increased in severity, patient satisfaction decreased markedly, regardless of the type of symptom. It has been well established that excessive expectations regarding surgery outcome can have a significant impact on the outcome and patient satisfaction.21,22 Also, patient expectations of surgical outcome generally exceed the actual outcome.23 For instance, Mannion et al reported that many patients were overoptimistic concerning the outcome of their surgery.21 Given these reports, along with our findings, it appears that the prevention of FBSS may rely on preoperative presentation of precise information about the realistic outcomes and residual symptoms. This may help to adjust the gap between patient expectations and their prospective prognosis. Realistic expectations prior to surgery are likely to have an important impact on patient satisfaction. Although satisfaction regarding surgery in our data was roughly correlated with the outcome scores, some patients were not satisfied even after a symptom was greatly improved or even disappeared, whereas other patients were satisfied despite reporting residual symptoms. This supports the notion that effective patient–provider communication can affect patient satisfaction and health outcomes.24 Indeed, communication has been correlated with improved physiologic status, functional outcomes, mental health, and symptom resolution.25 To reduce the prevalence of FBSS after surgery, it appears that more emphasis should be placed on preoperatively establishing an effective patient–provider relationship.
We found that residual symptoms were not only closely related to satisfaction with surgery, but also to the patient QOL and psychological status. Indeed, chronic low back pain has repeatedly been found to decrease QOL in both clinical26 and general populations.27–29 However, aside from this study, the impact of residual abnormal sensations after back surgery on patient QOL has not been investigated. Indeed, the experience of such abnormal sensations, especially when they were not major complaints prior to surgery, may have an important detrimental effect on patient QOL and mental health, and thus should be considered seriously in pre- and postsurgical practice.
We estimated an FBSS prevalence rate of 21.6% in our 1842 participants, based on the existence of residual symptoms and patient ratings of satisfaction. The general prevalence of FBSS has not been estimated clearly, possibly because the definition is somewhat ambiguous. Most reports have estimated the prevalence of FBSS based on the incidence rate of residual symptoms, the reoperation rate,1 or the success rate of clinical outcomes.30,31 Generally, FBSS refers to persistent or recurrent back and/or leg pain following one or more spinal surgeries, including cases involving anatomically successful spinal surgery. The International Neuromodulation Society defined FBSS as referring to a subset of patients who have new or persistent pain after spinal surgery for back or leg pain. Turner et al performed a meta-analysis of 74 journal articles and reported that, on average, 64% of patients who underwent surgery for lumbar spinal stenosis had good or excellent results.30 Javid and Hadar reviewed seven prospective studies, and reported an average success rate of 67.8% in a total of 983 patients who underwent lumbar spinal surgery.31 Based on these reports, FBSS is estimated to affect nearly 30 % of patients who undergo low back surgery. However, all patients who experience residual symptoms after low back surgery do not necessarily have FBSS. In this study, we found a lower rate of FBSS compared with other studies because we used patient satisfaction to estimate the FBSS prevalence. Not all patients with residual symptoms reported being dissatisfied with their surgery. Indeed, 76% of respondents in our study who had more than one residual symptom answered that they were satisfied with their surgery. Therefore, our prevalence data might represent a more accurate rate of FBSS in the general community.
With the goal of reducing surgeon bias, we distributed this Internet survey through a third-party company. Voorhies et al found significant differences between measurements of success or satisfaction collected by a surgeon vs. those collected by another patient, even for relatively simple lumbar surgery.32 One report from Japan indicated that only 27 of 89 patients (30.3%) showed residual leg pain/numbness 2 years after surgery for lumbar spinal stenosis.33 However, our data indicate that low back pain and leg numbness disappeared in only 25% and 34% of patients, respectively. As discussed, this large discrepancy regarding surgery outcome may be due to differences in patient willingness to accurately report their residual symptoms and the level of satisfaction to the physicians who performed the surgery or to the researchers at the same institution. Recently, the aim of many health care services has shifted from curing disease to improving QOL outcomes in individuals by assessing patient-reported outcomes measures. An accurate measurement of “patient satisfaction” with a given health care service is an important element of patient-reported outcomes measures, and has become increasingly accepted as an indicator of the quality of health care. Thus, Internet surveys using an anonymous third party may represent an effective way to assess the degree of patient satisfaction with the overall treatment outcomes.
Limitations
Although investigations using the Internet are relatively of low cost, anonymous, and convenient for participants to complete, there are several limitations to this method: 1) some individuals may submit inaccurate responses to receive compensation for the study; 2) it may not be possible to verify the accuracy of patient medical records; and 3) it may be difficult to obtain accurate answers from elderly people with degenerative diseases. These disadvantages are indeed limitations of the present study. Regarding the reliability of the Internet survey, we excluded respondents with conflicts or contradictions in their answers as a way to limit the number of dishonest respondents. As a result, we excluded 274 respondents (13.2%) in the main survey, thus increasing the accuracy and reliability of the present study. Also, in an attempt to avoid any confusion or misunderstandings regarding the contents of the study, especially with respect to participants who were elderly or who had limited medical knowledge, we minimized our use of medical terms.
Conclusion
The data from our nationwide online survey of 1842 lumbar surgery patients revealed new information about the prevalence and sociodemographic characteristics of FBSS. We found that residual abnormal sensations such as numbness, coldness, or paresthesia in the lower extremities and dull ache in the low back were highly associated with patient satisfaction and QOL following low back surgery. Also, these residual symptoms were significantly correlated with the development of FBSS. Our findings indicate that FBSS may be reduced by emphasizing the delivery of precise pre-surgical prognostic information, based on comprehensive epidemiologic data, to patients and by conducting clinical procedures, preparations, and follow-up assessments with a strong focus on patient satisfaction.
Acknowledgments
This study was funded by the grants from the Ministry of Health, Labour and Welfare (MHLW) of Japan (H23-Itami-Shitei-001) and by the 2014 Japanese Orthopaedic Association through the Committee on the Study of Musculoskeletal Pain Research Grant for population-based studies of neuropathic pain.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.North RB, Campbell JN, James CS, et al. Failed back surgery syndrome: 5-year follow-up in 102 patients undergoing repeated operation. Neurosurgery. 1991;28(5):685–691. discussion 690–691. [PubMed] [Google Scholar]
- 2.Chan CW, Peng P. Failed back surgery syndrome. Pain Med. 2011;12(4):577–606. doi: 10.1111/j.1526-4637.2011.01089.x. [DOI] [PubMed] [Google Scholar]
- 3.Dvorak J, Gauchat MH, Valach L. The outcome of surgery for lumbar disc herniation. I. A 4-17 years’ follow-up with emphasis on somatic aspects. Spine (Phila Pa 1976) 1988;13(12):1418–1422. doi: 10.1097/00007632-198812000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Oaklander AL, North RB. Failed Back Surgery Syndrome. 4th ed. Philadelphia, PA: Lippincott Williams & Williams; 2010. [Google Scholar]
- 5.Wilkinson HA. The Failed Back Syndrome: Etiology and Therapy. 2nd ed. New York, NY: Springer; 1991. [Google Scholar]
- 6.Benzon HT. Essentials of Pain Medicine and Regional Anesthesia. New York, NY: Churchill Livingstone; 2005. [Google Scholar]
- 7.Malter AD, McNeney B, Loeser JD, Deyo RA. 5-year reoperation rates after different types of lumbar spine surgery. Spine (Phila Pa 1976) 1998;23(7):814–820. doi: 10.1097/00007632-199804010-00015. [DOI] [PubMed] [Google Scholar]
- 8.Kim CH, Chung CK, Park CS, et al. Reoperation rate after surgery for lumbar spinal stenosis without spondylolisthesis: a nationwide cohort study. Spine J. 2013;13(10):1230–1237. doi: 10.1016/j.spinee.2013.06.069. [DOI] [PubMed] [Google Scholar]
- 9.Boonstra AM, Schiphorst Preuper HR, Balk GA, Stewart RE. Cutoff points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain. 2014;155(12):2545–2550. doi: 10.1016/j.pain.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 10.EuroQol Group EuroQol – a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 11.Ikeda S, Ikegami N. The QOL Measurement Handbook. Tokyo: Igaku-Shoin; 2001. Preference-based measure. [Google Scholar]
- 12.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 13.Furukawa TA, Kawakami N, Saitoh M, et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int J Methods Psychiatr Res. 2008;17(3):152–158. doi: 10.1002/mpr.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sakurai K, Nishi A, Kondo K, Yanagida K, Kawakami N. Screening performance of K6/K10 and other screening instruments for mood and anxiety disorders in Japan. Psychiatry Clin Neurosci. 2011;65(5):434–441. doi: 10.1111/j.1440-1819.2011.02236.x. [DOI] [PubMed] [Google Scholar]
- 15.Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K. Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine (Phila Pa 1976) 2001;26(6):652–657. doi: 10.1097/00007632-200103150-00019. [DOI] [PubMed] [Google Scholar]
- 16.Loupasis GA, Stamos K, Katonis PG, Sapkas G, Korres DS, Hartofilakidis G. Seven- to 20-year outcome of lumbar discectomy. Spine. 1999;24(22):2313–2317. doi: 10.1097/00007632-199911150-00005. [DOI] [PubMed] [Google Scholar]
- 17.Kornblum MB, Fischgrund JS, Herkowitz HN, Abraham DA, Berkower DL, Ditkoff JS. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective long-term study comparing fusion and pseudarthrosis. Spine. 2004;29(7):726–733. doi: 10.1097/01.brs.0000119398.22620.92. [DOI] [PubMed] [Google Scholar]
- 18.Huang P, Sengupta DK. How fast pain, numbness, and paresthesia resolves after lumbar nerve root decompression: a retrospective study of patient’s self-reported computerized pain drawing. Spine. 2014;39(8):E529–E536. doi: 10.1097/BRS.0000000000000240. [DOI] [PubMed] [Google Scholar]
- 19.Waxman SG, Kocsis JD. The Axon: Structure, Function, and Pathophysiology. New York, NY: Oxford University Press; USA; 1995. [Google Scholar]
- 20.Nygaard O, Kloster R, Mellgren S. Recovery of sensory nerve fibres after surgical decompression in lumbar radiculopathy: use of quantitative sensory testing in the exploration of different populations of nerve fibres. J Neurol Neurosurg Psychiatry. 1998;64(1):120–123. doi: 10.1136/jnnp.64.1.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mannion AF, Junge A, Elfering A, Dvorak J, Porchet F, Grob D. Great expectations: really the novel predictor of outcome after spinal surgery? Spine (Phila Pa 1976) 2009;34(15):1590–1599. doi: 10.1097/BRS.0b013e31819fcd52. [DOI] [PubMed] [Google Scholar]
- 22.Stambough JL. Matching patient and physician expectations in spine surgery leads to improved outcomes. Spine J. 2001;1(3):234. doi: 10.1016/s1529-9430(01)00088-2. [DOI] [PubMed] [Google Scholar]
- 23.McGregor AH, Doré CJ, Morris TP. An exploration of patients’ expectation of and satisfaction with surgical outcome. Eur Spine J. 2013;22(12):2836–2844. doi: 10.1007/s00586-013-2971-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(Suppl 3):S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 25.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 26.Ekman M, Jonhagen S, Hunsche E, Jonsson L. Burden of illness of chronic low back pain in Sweden: a cross-sectional, retrospective study in primary care setting. Spine (Phila Pa 1976) 2005;30(15):1777–1785. doi: 10.1097/01.brs.0000171911.99348.90. [DOI] [PubMed] [Google Scholar]
- 27.Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333. doi: 10.1016/j.ejpain.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 28.Inoue S, Kobayashi F, Nishihara M, et al. Chronic pain in the Japanese community–prevalence, characteristics and impact on quality of life. PLoS One. 2015;10(6):e0129262. doi: 10.1371/journal.pone.0129262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pellisé F, Balagué F, Rajmil L, et al. PRevalence of low back pain and its effect on health-related quality of life in adolescents. Arch Pediatr Adolesc Med. 2009;163(1):65–71. doi: 10.1001/archpediatrics.2008.512. [DOI] [PubMed] [Google Scholar]
- 30.Turner JA, Ersek M, Herron L, Deyo R. Surgery for lumbar spinal stenosis. Attempted meta-analysis of the literature. Spine (Phila Pa 1976) 1992;17(1):1–8. doi: 10.1097/00007632-199201000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Javid MJ, Hadar EJ. Long-term follow-up review of patients who underwent laminectomy for lumbar stenosis: a prospective study. J Neurosurg. 1998;89(1):1–7. doi: 10.3171/jns.1998.89.1.0001. [DOI] [PubMed] [Google Scholar]
- 32.Voorhies RM, Jiang X, Thomas N. Predicting outcome in the surgical treatment of lumbar radiculopathy using the Pain Drawing Score, McGill Short Form Pain Questionnaire, and risk factors including psychosocial issues and axial joint pain. Spine J. 2007;7(5):516–524. doi: 10.1016/j.spinee.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 33.Hara N, Oka H, Yamazaki T, et al. Predictors of residual symptoms in lower extremities after decompression surgery on lumbar spinal stenosis. Eur Spine J. 2010;19(11):1849–1854. doi: 10.1007/s00586-010-1374-1. [DOI] [PMC free article] [PubMed] [Google Scholar]