Abstract
Purpose
Patients’ trust in health care is increasingly recognized as important to quality care, yet questions remain about what types of health care experiences erode trust. The current study assessed the prevalence and impact of institutional betrayal on patients’ trust and engagement in health care.
Participants and methods
Participants who had sought health care in the US in October 2013 were recruited from an online marketplace, Amazon’s Mechanical Turk. Participants (n = 707; 73% Caucasian; 56.8% female; 9.8% lesbian, gay, or bisexual; median age between 18 and 35 years) responded to survey questions about health care use, trust in health care providers and organizations, negative medical experiences, and institutional betrayal.
Results
Institutional betrayal was reported by two-thirds of the participants and predicted disengagement from health care (r = 0.36, p < 0.001). Mediational models (tested using bootstrapping analyses) indicated a negative, nonzero pathway between institutional betrayal and trust in health care organizations (b = −0.05, 95% confidence interval [CI] = [−0.07, −0.02]), controlling for trust in physicians and hospitalization history. These negative effects were not buffered by trust in one’s own physician, but in fact patients who trusted their physician more reported lower trust in health care organizations following negative medical events (interaction b = −0.02, 95%CI = [−0.03, −0.01]).
Conclusion
Clinical implications are discussed, concluding that institutional betrayal decreases patient trust and engagement in health care.
Keywords: USA, social science, self-report, cross-sectional, engagement, adherence, healthcare systems
Introduction
Medicine has long looked to patients’ trust in physicians as an important metric of care quality.1 It is in the best interest of health care systems that patients trust their physicians because trust predicts outcomes that directly benefit these systems. Trust in physicians is associated with following treatment recommendations2 and seeking care in a timely manner3 – both of which are associated with reduced health care costs4 and faster recovery.5 Trust is powerful; it may mediate clinical outcomes such as placebo effects and explain some of the variance in responses to nontraditional treatments.6,7 Establishing trust creates a feedback loop where trust begets better care, which increases trust and satisfaction.3 Sometimes lost in the discussion of trust and health care is the fact that patients are dependent on health care institutions to meet their needs for care, a vulnerability that can prove uncomfortable if they mistrust those institutions.7 Very little research has focused on the types of health care experiences that are likely to degrade trust in health care institutions. The question of trust, or broken trust (which sometimes, but not always, is the result of a betrayal), has been addressed in research on interpersonal and institutional contexts,8 and this research is brought to bear on this discussion, with an emphasis on institutional betrayal. In this paper, I describe a study that tests hypotheses about the roles of negative medical experiences, institutional betrayal, and individual characteristics in predicting trust in physicians and health care systems. The results of this study are discussed in terms of their contribution to the existing medical and social science literature as well as potential applications for health care institutions and professionals.
Trust and betrayal
Defining trust
Patients’ trust in their individual health care providers (e.g., doctor, nurse, etc.) encompasses several distinct but related concepts. Most closely aligned with the definition of trust used in the current study is fiduciary trust (derived from fidelity), which has been defined as the belief that health care providers will act in patients’ best interests and not take advantage of their vulnerability.7 This is critically different from confidence, which involves a calculated prediction of a positive outcome based on measurable characteristics (e.g., specialized training, past success9). Fiduciary trust, in contrast, is primarily about the patients’ beliefs regarding their physicians’ motivation and intention rather than concrete outcomes of treatment.7 It is perhaps unsurprising that a central tenet of medical ethics is the principle beneficence, which instructs physicians to act in the interest of their patients and is aimed at intention rather than outcome. Trust is also readily distinguished from satisfaction, although the two are related (e.g., patients who trust their doctor are more likely to be satisfied with their care7). The primary difference is that trust captures a belief about an on-going relationship and optimism about future interactions, whereas satisfaction is limited to describing past interactions.10 Although trust, satisfaction, and confidence in a physician may be aligned, they can also be independent: patients may believe their physicians to be competent in general but doubt their physician’s personal commitment to their own care.11
Recognizing betrayal
Because trust, in its most basic fiduciary form, has a strong emotional component, it is not always easily changed by experiences that might otherwise affect more cognitive qualities such as confidence and satisfaction.10 Trust plays an insulating role in that it allows for mistakes or errors to be made in the provision of health care without disastrous consequences. Patients can tolerate doubt about a physician’s competence or infallibility without necessarily having to adjust their beliefs about the physician’s motivations and intentions toward them – fiduciary trust can remain intact.7,12 In part, this may be because trust has a strong influence on patients’ perceptions of treatment, such that patients describe the quality of their treatment as more positive when trust is high13 and more negative when trust is low,7 regardless of the objective quality of that treatment. This is consistent with research on the role of trust in attribution of positive or negative intent in relationship research.14
Betrayal occurs when an individual is harmed by someone they trust or depend upon. Themes of betrayal arise in the context of medical research on trust: when patients realize that their physician has acted counter to their best interests or taken advantage of them (a betrayal of fiduciary trust), their reaction is closer to moral outrage and indignation than mere disappointment.7,12 These types of reactions to betrayal compel an individual to either confront the transgression or leave the relationship as a means to protect against further harm. Because both of these actions compromise the continuation of the relationship, in cases where need or dependency is particularly high (e.g., between a caregiver and child), the self-preservation of responding to betrayal may be outweighed by the immediate need for protection provided by the relationship.8 In these situations, unawareness of betrayal may occur.15 Thus, understanding not just how trust is built in health care but also how it may be undone by betrayal is key to fully understand patients’ experiences.
Distinguishing individuals from institutions
Trustworthy qualities are more readily apparent in individual physicians than in institutions, but institutions can embody these trustworthy traits as well. For example, insurance plans that provide a choice in doctors promote fidelity because patients’ treatment preferences are respected and they are able to change providers if they are not getting the care they need.11 These institutional characteristics may become suddenly clear when there is a break down in functioning (e.g., a data breach at a hospital that exposes many patients’ personal information). In fact, it appears that one reason why patients are more aware of potential conflicts of interest that exist in their health care systems is due to increased media exposure of health care system failings.11,12 More informed patients may push health care systems to be more responsive, but, taken to an extreme, skepticism may tip to suspicion and undermine the trust necessary to hold health care relationships together.
Trust in an individual physician and trust in a larger health care institution may be interrelated; patients may generalize their trust in a physician to doctors in general or the health care system in which the physician is located,7,11 or patients may base their trust in a physician on their trust in the health care system or their attitudes about doctors in general (more likely in new treatment relationships).16 Patients may vary in how much they distinguish their individual doctor from a broader health care system. Some systems are highly visible and distinct from individual providers (e.g., the Veterans Health Administration), which may make systemic limitations on physicians’ behaviors more clear and serve to create a “common foe” against which both doctor and patient must petition for services.17 In other cases, individual physicians may be very strongly identified with their institution. For example, the reputation of prestigious medical centers such as the Mayo Clinic may inform patients’ attributions of competence and, by extension, trustworthiness of an individual physician, even if they are unknown to the patient.12 Organizations’ understanding of this bidirectional influence can be seen in public assurances of their personnel selection process or advertising prestigious awards of their staff.11 Some research suggests that patients’ trust in health care systems is changing independently of their trust in physicians,18 which implies that patients are able to distinguish institutional barriers to ideal care from physician qualities.
Adverse medical events
A landmark report released by the Institute of Medicine (IOM) in 1999 reported that medical errors are responsible for between 44,000 and 98,000 deaths annually.19 This report defined medical errors as the failure of a planned action to be taken or the use of the wrong plan to achieve an aim. In keeping with prior research,20 the IOM assessed diagnostic errors (e.g., wrong or delayed diagnosis), treatment errors (e.g., pertaining to operations, treatments, tests, or medications), preventative errors (e.g., failing to provide prophylactic treatment or monitoring), and other errors (e.g., related to facilities, equipment). The report further notes that 90% of these errors were due to system failures, rather than individual provider error. At the time of the report, the IOM found that, in spite of the huge financial costs associated with these errors, health care systems are resistant to change and cite the medical liability system as an impediment to understand and prevent medical errors.19 Yet, public discussions of the report often focused on individual physician behaviors as the problem, obscuring the fact that most recommendations in the report were aimed at the system level, rather than providers.21 Further, IOM linked these errors to reduced patient trust in physicians and health care systems, patients’ mental and physical health declines, and frustration and lost morale for health care providers. Since this report was released, some systemic changes have occurred (e.g., incentivizing physicians to prevent errors, creating patient safety initiatives).22 Yet in a 2015 report, the IOM again pointed to systemic, environmental, and cultural factors in medicine as leading causes of diagnostic errors, highlighting the need to look beyond individual providers and patients.23
Measuring institutional betrayal in health care
At first glance, the results of the IOM report may seem contradictory to research indicating that patients who trust their physicians perceive their treatment more positively. What types of experiences may puncture the protective barrier of this trust? One potential explanation may be the co-occurrence of institutional action or inactions that contribute to these experiences: institutional betrayal. For institutional betrayal to occur, there must first exist trust in or dependency upon an institution.24 In the case of health care systems, both of these are likely to exist – it is in a state of vulnerability that patients seek health care.7,25 In order to measure institutional betrayal, it is also necessary that the institution itself is clearly identifiable and has a defined purpose that organizes its functioning. This feature allows for individuals to consider interactions they may have with individual representatives of the institution (e.g., a claims processor at an insurance company) as indicative of broader institutional values (e.g., declining to cover an expensive but effective medication due to its price reflects prioritizing profits over patient health). Institutional betrayal is theoretically and structurally consistent with the existing framework trust in health care. For example, fiduciary trust, defined as the belief that health care providers will act in patients’ best interests and not take advantage of their vulnerability,7 can be betrayed at the institutional level when patients are made to feel like less valuable members of the institution or when bringing up negative experiences is discouraged or punished, both forms of institutional betrayal.26
Examining institutional betrayal may not only add a new dimension to understanding trust in health care but also clarify why some negative medical experiences impact patients’ trust in health care providers and organizations while others do not – it may be that the initial error is not necessarily harmful but institutional responses to these errors is where the problem lies.27 This is particularly important as trust in organizations and individual physicians is interrelated.7,11 Therefore, even if the primary impact of institutional betrayal in health care is on trust in organizations, it may affect trust in physicians.
Hypotheses of the current study
The goal of the current study is to describe the effect of institutional betrayal in health care on patients’ reported behaviors and attitudes. In keeping with this goal and the literature reviewed above, the following three hypotheses are tested:
Hypothesis 1: Institutional betrayal will occur in health care settings related to, but distinct from, negative medical experiences (i.e., not all participants who report negative medical experiences will also report institutional betrayal related to those experiences).
Hypothesis 2: Institutional betrayal will predict disengagement from health care in the form of decreased adherence to health care advice as well as less frequent visits to the doctor even when needed.
Hypothesis 3: Institutional betrayal will mediate the relationship between negative medical experiences and decreased trust in health care systems and professionals, even controlling for overall exposure to health care systems.
Participants and methods
Participants and procedure
This research was approved by the University of Oregon’s institutional review board (IRB protocol number: 08212014.023). The study was advertised on Amazon’s Mechanical Turk as a Human Intelligent Task (HIT) titled “Healthcare Survey” that would take approximately 45 minutes to complete. Any of the approximately 500,000 registered “workers” on Mechanical Turk could have seen the posting. Potential participants saw a brief description of the study that read, “Describe your personal experiences accessing health care along with information about your health.” Participation eligibility was limited to individuals who were at least 18 years old and who had used health care in the USA. No cutoff date for accessing these services was mentioned, but potential participants were encouraged to consider whether they could remember experiences well enough to describe them before agreeing to participate. Participants were paid a flat rate of $5 credited to their Mechanical Turk account for completing the survey. The consent form also stated that only complete participation would result in compensation of $5, which included spending sufficient time on each page to ensure that instructions and items could be read and answered. Participants chose a single item that read, “I agree to participate,” in order to proceed to the survey.
The survey was available for a total of 10 days. A total of 759 individuals participated in the study and 707 provided valid responses (i.e., providing valid responses to four of five items such as, “Check this box to indicate you are reading each item”). This strategy has been demonstrated to reduce “noise” of careless or inattentive responding, increasing the validity of self-report data and power, particularly where small effects are concerned.28 Fewer than 20 individuals work was rejected for failing to meet this cutoff. In order to assess the representativeness of the sample compared to the US population, several demographic variables for which national statistics are available were collected. The sample was 73% Caucasian, 10.3% Black or African American, 6.2% Asian American, 2.7% Native American, 6.5% Hispanic or Latino/a, and 1.3% mixed race. Many of these demographics are within 5% points of the 2013 US Census figures representing the USA (exception was Hispanic or Latino/a, which was 17.1% in 2013 Census). The sample was 42.2% male, 56.8% female, and 1% indicated they were genderqueer or gender nonconforming. Approximately 10% of the sample (9.8%) identified as nonheterosexual. The median range was 18–35 years; participants reported their age by choosing a 10-year increment beginning at 25–35 years (exceptions were the spans from 18 to 25 years and 76 and older). Almost all of participants (99.3%) were below 65 years of age (compared to 75.9% of the population of the USA per the 2013 US Census) and many (91.6%) were below 55 years of age. All participants had exposure to US health care systems and a range of health care experiences and needs. Most reported choosing health care professionals who were covered by insurance (75.5%) or near to their home (52.5%). Approximately half (46.5%) reported taking a prescribed medication daily. Almost all (93.2%) had been hospitalized fewer than seven times in their life. Most (95.1%) reported visiting the doctor once per month or less.
Materials
Hospitalization history
Respondents were asked several different questions that assessed their exposure to a variety of health care systems, including how many times in their life they had been hospitalized (on a four-point scale, with response options ranging from 0 to 3, 4 to 7, 8 to 11, and 12 or more times).
Health care disengagement
Underutilization and nonadherence related to health care in the past 12 months were measured with a checklist that included five items used in previous studies of health care disengagement (Table 1). Each of these items has been previously found to be associated with mistrust of health care institutions (e.g., “A physician gave me advice that I did not take; I did not seek medical care at all even when I felt I needed it”;25 “I delayed seeking healthcare that I thought I needed.”3) These five items were summed to create an indicator of overall disengagement from health care.
Table 1.
Disengagement from health care behaviors
| Item content | Participants endorsing (%) |
|---|---|
| In the past year Ia… | |
| Ignored a doctor’s advice | 23.9 |
| Did not keep a follow-up appointment | 26.7 |
| Postponed/delayed needed care | 40.7 |
| Did not seek needed care at all | 30.8 |
| Did not fill a prescription | 17.3 |
| Took a prescription not as prescribed | 20.1 |
Note:
M items endorsed = 1.5, standard deviation = 1.43.
Wake Forest Trust in Physician Scale
This scale contains five items that assess agreement with positively and negatively worded statements about trusting one’s own physician (e.g., “I completely trust my doctor’s decisions about which medical treatments are best for me”) with response options on a five-point scale ranging from strongly disagree to strongly agree. Responses on this scale are averaged to create a composite variable representing trust in one’s own physician (range = 1–5). This scale demonstrated good internal consistency in the current sample (alpha = 0.92) and prior studies demonstrated validity via positive correlations with other measures of trust, physician competence, and adherence to medical advice.29
Medical Mistrust Inventory
This scale contains 17 items that assess agreement with positively and negatively worded statements about mistrust of medical institutions (e.g., “when healthcare organizations make mistakes, they usually cover it up”) with response options on a five-point scale ranging from strongly disagree to strongly agree.25 Responses on this scale are averaged to create a composite variable representing mistrust medical institutions (range = 1–5). This scale demonstrated good internal consistency (test–retest correlation coefficients ranging from 0.35 to 0.70; current study alpha = 0.90) and prior studies indicated validity via correlations with underutilization of health care (e.g., failure to keep a health care appointment, failure to fill a prescription, and failure to take medical advice). To facilitate comparison with other scales of trust, the negatively worded items were reverse scored so the composite score reflects the degree to which a respondent trusts medical organizations.
Medical Errors, Adverse Consequences, Unexpected, or Lasting Pain Assessment (MEACULPA)
The 15-item MEACULPA was created for this study in order to assess negative medical experiences that are notable but not necessarily egregious (i.e., most people were expected to have experienced at least one of the items at some point). The items themselves were drawn from examples in the medical literature of commonly experienced adverse medical events.30 The items are presented as a checklist that encompasses a participant’s lifetime experiences of health care systems (Table 2). Respondents were also given the option to write in an experience. Because the MEACULPA is a checklist, rather than a scale designed to measure an underlying state or trait, responses are summed to reflect the total number of different types of events they have experienced (the number of times each event happened is not captured). This type of scoring is consistent with other checklists of adverse life events (e.g., the PTSD Cheklist).31
Table 2.
Negative Medical Experiences, Adverse Consequences, and Unexpected or Lasting Pain Assessment (MEACULPA)
| MEACULPA item | Particpants, n=707
|
|
|---|---|---|
| n | % | |
| I was prescribed an unnecessary medication | 198 | 28 |
| I was given an incorrect diagnosis | 191 | 27 |
| I was not notified of test results | 174 | 24.6 |
| I had an allergic reaction to medication | 173 | 24.5 |
| I underwent an unnecessary procedure or test. | 159 | 22.5 |
| I had a procedure was more painful than I expected | 155 | 21.9 |
| I experienced unexpected side effects of a procedure or medication | 149 | 21.1 |
| I received inaccurate insurance information | 136 | 19.2 |
| My personal information (e.g., name, diagnosis, schedule) was incorrect | 96 | 13.6 |
| I needed to return to hospital after discharge for emergency care | 83 | 11.7 |
| I had postsurgical complications | 78 | 11 |
| I found the medical facilities were old, run down, or in disrepair | 75 | 10.6 |
| I was prescribed an incorrect medication dosage | 72 | 10.2 |
| I developed an infection related to a medical procedure | 58 | 8.2 |
| Other medical error, adverse experience, or lasting/unexpected pain | 51 | 7.2 |
| I was prescribed a medication that interacted with existing medication | 50 | 7.1 |
Institutional Betrayal Questionnaire – Health Care (IBQ-H)
The IBQ-H is a 15-item modified version of the IBQ26 that assesses institutional betrayal specifically in health care settings. Presented directly following the MEACULPA to respondents who endorsed any MEACULPA items, respondents were asked to indicate whether a health care institution played a role in their MEACULPA experiences. The instructions orient respondents to the range of institutions that would be appropriate to consider, from the US health care system as a whole to a staff within a single doctor’s office. Additionally, they are instructed to report on any institutional betrayal they have experienced related to the MEACULPA item or items they endorsed, even if it means reporting about different institutions. The main content of the items (e.g., not taking proactive steps to prevent, responding inadequately to, etc.) mirrors the original IBQ, but “negative” or “unpleasant” health care experiences (rather than the more general “experience” of the original scale) are referred to throughout and the examples provided for each item are health care related (e.g., not taking proactive steps to prevent unpleasant healthcare experiences was followed by the example by explaining procedures, side effects, etc.). Following a checklist of 12 such items, respondents are asked to identify the health care institution or institutions involved in these experiences by typing into a field, to indicate the degree to which they trusted this institution prior to their experience (on a four-point scale from not at all to very much), and to indicate whether they have continued to seek health care from this institution following these experiences (response options are yes or no). Full measure can be accessed in the Supplementary material or by request from the author.
Data analysis plan
Multivariate path analyses are tested using ordinary least squares regression via PROCESS software, a macro available within SPSS 22. PROCESS is designed to test complex models of multiple mediation and moderation, where each direct (i.e., where x predicts y) and indirect pathway (i.e., the total effect of x predicting y and y predicting z) is specified and tested.32 PROCESS differs from traditional mediational process (e.g., Baron and Kenny’s popular four-step process that uses multiple regression) in two important ways. First, it does not depend upon the assumption that any variable (much less the combined effects of two or more variables) is normally distributed in the population as in standard regression. Instead, PROCESS uses bootstrapping to estimate standard error (SE), which in effect creates an empirical distribution by repeatedly “sampling” the data with replacement (10,000 times in the current study). This distribution is then used to test inferential hypotheses by computing regression coefficients and 95% confidence intervals (CIs) that indicate the likelihood that the observed effects differ from zero (reported as upper limit CI [ULCI]and lower limit CI [LLCI]). The second difference arises from this method: because the sample data are not expected to conform to normal assumptions, irregularly distributed variables are not as disruptive to inferential tests and thus real indirect effects are more likely to be observed – yielding higher powered tests.
The outcome variables in these path analyses are trust in health care organizations and physicians. In order to make the strongest statement about the unique effects of the predictor variables (negative medical experiences and institutional betrayal), it may be necessary to also control for other variables that are related to the outcome variables. Although research is inconsistent in regard to individual characteristics that predict trust in health care systems and providers,7 socioeconomic characteristics are often discussed as potential mediators of trust. However, in the current sample, no differences in trust were observed across racial groups or income level. All of the measures of exposure to health care systems (e.g., number of visits to any health care provider) were positively correlated with trust. The number of hospitalizations was used as an indicator of health care exposure, as it showed the strongest relationship with other items assessing health care use and outcome measures. Beyond the predictor variables of interest, only hospitalization history was included as a control variable.
Results
Hypothesis 1: negative medical experiences and institutional betrayal
Negative medical experiences were reported by 80.1% of participants, and the average number of MEACULPA items endorsed was 3.35 (SD = 2.53). The rates of each type of experience are shown in Table 2. Each item on the MEACULPA was endorsed by at least 50 participants, indicating that this construct assessed meaningful and relatively common negative medical experiences.
Institutional betrayal was reported by 66.1% of participants, and the average number of IBQ-H items endorsed was 3.01 (SD = 2.23). The most common types of institutional betrayal reported were failure to take steps to prevent an unpleasant health care experience (31.5% of participants), responding inadequately to concerns or reports of a negative experience (24.8%), denying negative medical experiences (24.8%), making it difficult to report a negative health care experience or share concerns (21.4%), and creating an environment where negative experiences seemed more likely to occur (21.1%). Institutional betrayal was distinct from negative medical experiences as 17.5% of participants who reported such an experience did not report institutional betrayal.
Hypothesis 2: institutional betrayal and disengagement
Disengagement from health care was correlated with negative medical experiences (as well as trust in physicians and health care institutions; Table 3). Institutional betrayal was positively correlated with disengagement from health care (r = 0.36, p < 0.001). This relationship remained significant and positive, even when MEACULPA scores were controlled for via a partial correlation (r = 0.11, p = 0.004).
Table 3.
Correlations between negative medical experiences, institutional betrayal, noncompliance, and trust
| Scale | MEACULPA | IBQ-H | Disengagementa |
|---|---|---|---|
| Trust in own physicianb | −0.36** | −0.40** | −0.24** |
| Trust in health care organizationsc | −0.43** | −0.45** | −0.22** |
| Disengagement | 0.41** | 0.36** | – |
Notes:
Disengagement = total number of health care behaviors endorsed.
Wake Forest Trust in Physician Scale.
Medical Mistrust Inventory.
p < 0.001.
Abbreviations: MEACULPA, Medical Experiences, Adverse Consequences, and Unexpected or Lasting Pain Assessment; IBQ-H, Institutional Betrayal Questionnaire – Health Care.
Hypothesis 3: institutional betrayal and trust
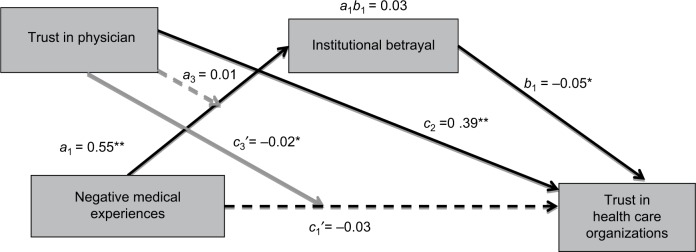
A moderated mediation analysis revealed several important direct and indirect effects. As shown in Figure 1 and Table 4, the direct effect of negative medical experiences (measured via the MEACULPA) on trust in health care organizations is fully mediated by institutional betrayal and trust in one’s own physician (c1′ = 0.02, p = 0.34). Specifically, negative medical experiences were stronger predictors of decreased trust in health care organizations for participants who reported more trust in their own physician compared to individuals who reported less trust in their own physician (i.e., for an individual who was 1 SD above the mean on the Trust in Physician scale, the effect was c1 = −0.06, p < 0.001 compared to an individual who was 1 SD below the mean on the Trust in Physician scale for whom the effect was c1 = −0.02, p = 0.001). However, trust in one’s own physician did not affect the relationship between negative medical experiences and institutional betrayal (a3 = 0.01, p = 0.672) and the indirect effect of negative medical experiences on trust in health care organizations (through institutional betrayal) did not depend on trust in one’s physician, the coefficients for this pathway were in fact identical for individuals with high and low trust in their physician (c3′ = 0.03, SE = 0.01).
Figure 1.
Effect of negative medical experiences on trust in health care organizations moderated by trust in physician and mediated by institutional betrayal.
Note: Bolded coefficients indicate nonzero indirect effects of negative medical experiences on trust health care organizations. Covariates of the mediator and outcome in this model are hospitalization history. Refer Table 4 for further statistics for each pathway and description of coefficients. *p < 0.01; **p < 0.001.
Table 4.
Regression coefficients for the effect of negative medical experiences on trust in health care organizations moderated by trust in physician and mediated by institutional betrayal
| Predictor | Path coefficients | Outcome: M (IBQ-H)
|
||||
|---|---|---|---|---|---|---|
| Coeff. | SE | p | LLCI | ULCI | ||
| Constant | 2.62 | 0.48 | <0.0001 | 1.69 | 3.56 | |
| MEACULPA | a1 | 0.55 | 0.08 | <0.0001 | 0.39 | 0.70 |
| Trust in phys.a | a2 | −0.55 | 0.12 | <0.0001 | −0.79 | −0.31 |
| MEACULPA × trust in phys. | a3 | 0.01 | 0.02 | 0.6716 | −0.03 | 0.05 |
| Hospitalizationb | −0.12 | 0.09 | 0.1933 | −0.29 | 0.06 | |
|
| ||||||
| Predictor |
Outcome: Y (trust in health care orgs.c)
|
|||||
| Coeff. | SE | p | LLCI | ULCI | ||
|
| ||||||
| Constant | 1.52 | 0.16 | <0.0001 | 1.21 | 1.87 | |
| MEACULPA | c′ | 0.02 | 0.03 | 0.4000 | −0.03 | 0.08 |
| IBQ-H | b1 | −0.05 | 0.01 | 0.0001 | −0.07 | −0.02 |
| Trust in phys. | b2 | 0.39 | 0.04 | <0.0001 | 0.31 | 0.47 |
| MEACULPA × trust in phys. | b3 | −0.02 | 0.01 | 0.006 | −0.03 | −0.01 |
| Hospitalization | 0.06 | 0.03 | 0.0426 | 0.002 | 0.12 | |
|
| ||||||
| MEACULPA |
Outcome: Y (trust in health care orgs.) at moderator
|
|||||
| Coeff. | SE | p | LLCI | ULCI | ||
|
| ||||||
| −1 SDd trust in physician | −0.03 | 0.01 | 0.0012 | −0.05 | −0.01 | |
| +1 SDd trust in physician | −0.06 | 0.01 | <0.0001 | −0.09 | −0.04 | |
Notes:
Wake Forest Trust in Physician Scale.
Number of hospitalizations.
Medical Mistrust Inventory.
Coefficients for individuals low and high in trust (1 SD below and above the mean) on the Trust in Physician scale. Refer figure 1 for coefficient paths.
Abbreviations: IBQ-H, Institutional Betrayal Questionnaire – Health Care; coeff., coefficient; SE, standard error; LLCI, lower level confidence interval; ULCI, upper level confidence interval; MEACULPA, Medical Errors, Adverse Consequences, Unexpected, or Lasting Pain Assessment; phys., physician; orgs., organizations.
Discussion
This study expands the discussion of trust in health care beyond individual patient or doctor characteristics by measuring the impact of institutional betrayal. Consistent with hypotheses, the current study found that 1) institutional betrayal is common in health care (two-thirds of the participants reported experiencing at least one item on the IBQ-H) and distinct from adverse medical events (17.5% of individuals who reported negative medical experiences did not report institutional betrayal); 2) institutional betrayal was associated with disengagement from health care; and 3) institutional betrayal, over and above negative medical experiences, predicted trust in health care organizations.
Disengagement
Institutional betrayal is occurring both before negative medical experiences and in the aftermath; some of the most common forms of betrayal reported were institutional failure to prevent these negative experiences and responding inadequately to reports of negative experiences. Both point to a lack of responsiveness that does not match the needs of patients who may be at their most vulnerable. Unsurprisingly, this betrayal appears to be a contributor to patient behaviors that undermine treatment effectiveness, including not seeking medical care when it is necessary and not complying with treatment recommendations. This is consistent with previous research on institutional betrayal where withdrawal from the institution was a common outcome of institutional betrayal.26 Although this reaction is entirely understandable, one consequence is that these systems do not always get feedback that something they did contributed to a patient’s disengagement or even complete departure. What this means for health care professionals can be considered both good and bad news. The good news is that it is not completely up to doctors alone to establish and protect patients’ trust in the broader health care system and thereby keep patients engaged in their care. The bad news is that the broader institutional environment may be undoing some of the hard work that goes into treating patients and affecting doctors’ ability to deliver effective care.
Institutional betrayal and trust in health care organizations
Given the multiple forms of trust measured, it was possible to begin to understand how institutional betrayal might “spread” from physician to institution or vice versa as predicted by previous research.11,33 Indeed, trust in physicians was positively correlated with trust in organizations, even controlling for negative medical experiences and institutional betrayal. However, when negative medical experiences occurred, participants with more trust in their own physician actually demonstrated greater decreases in trust in health care organizations – potentially indicating that they are attributing these errors to systemic issues rather than doctor error.
Critically, trust in one’s own physician did not affect the relationship between negative medical experiences and institutional betrayal. This is another piece of evidence that differentiates negative medical experiences from institutional betrayal as well as underscores the importance of focusing interventions on institutional problems rather than the doctor–patient relationship alone. It further suggests that institutional betrayal may be undermining some of the potentially protective aspects of trust in health care providers as even participants with apparently good relationships with their physicians were just as vulnerable to experiencing institutional betrayal.
Clinical implications
The most important clinical implication from these findings is that asking about negative medical experiences and institutional betrayal – and listening to the answer – is critical. These are not rare occurrences; the majority of participants in this study had experienced both negative medical experiences and institutional betrayal. Although patients may be hesitant to bring up medical errors or institutional betrayal,30 it is likely that the mere act of a physician or health care system asking about these experiences could be a means to restore lost trust.34 Prior research has characterized decisions not to report documented medical mistakes as a hesitancy to question medical professionals,30,34 but the results of this study suggest that patients’ reasons may be more complex. It may be threatening to acknowledge that a trusted medical professional or institution has contributed to a negative health care experience or it may be difficult voice concerns with an incomplete memory of one’s experience. When patients do report negative medical experiences, it is critical to validate and respond to these reports. Many participants reported inadequate responses to their reports or outright denials of their experience. This type of invalidation is particularly harmful coming from a depended upon institution at a time of vulnerability.35
What response would be best in these situations? The most basic answer is an apology. Yet this very human reaction is one that many doctors have been implicitly or explicitly advised against given the potential for malpractice suits that may follow an admission of guilt.36 In the majority of states, however, the framework for encouraging apologies in medical settings is already in place in the form of “I’m Sorry” laws.37 These laws are based on research on the motivations of patients who file medical malpractice suits – in many cases, the patients reported being motivated not by the medical error itself but by the insensitivity of the physician and a lack of accountability for the mistake.36 I’m Sorry laws protect doctors who apologize (i.e., including admitting fault, expressing regret for the injurious action, and expressing sympathy for the other’s injury) from later having that apology used in litigation. These laws have been associated with fewer lawsuits, lower settlement amounts, and shorter litigation.37 There is still some risk in apologizing but there is clear risk in having patients lose trust as well. Even when the individual health care provider is not directly responsible, an apology for the pain, distress, or uncertainty the patient has experienced could contribute to restoring trust.38
Strengths and limitations
This study is the first to examine the role of institutional betrayal in health care. As such, the hypotheses were broad and the primary goals were accomplished by collecting a large number of responses at a single time point. This also represents a methodological limitation as the temporal precedence of events could not be established. The described models had strong theoretical rationales for testing directional hypotheses (e.g., that institutional betrayal would lead to decreased trust, rather than the other way around), but the manner in which the data were collected did not truly allow for establishing the order of events as all variables were measured at the same time.
Future studies could examine the association of negative medical experiences, institutional betrayal, and the outcomes reported in this study in real time quite easily – particularly if researchers are associated with a medical institution with access to patients seeking treatment. Additionally, the results could have been influenced by participants self-selecting into the study based on their interest in the topic – either because they had a strong opinion on health care or because they had had particularly egregious experiences they hoped to describe. However, several hundred people completed this survey within 10 days, which suggests that the $5 payment was motivation enough. It is still the case that participants knew the topic of the study from the description and from potentially communicating with one another. This limitation could be addressed in future studies if these measures were embedded in a larger study or on-going health care research that could obscure the research aims more readily and depend upon debriefing to fully inform participants of the purpose of the research.
Future directions
There are at least two clear future directions suggested by these results. The first is to assess the effects of institutional betrayal on physicians and other health care providers. The way that the current study posed questions about institutional betrayal to participants asked them to consider larger health care institutions rather than individual providers. These are the same institutions in which health care providers work and they are likely to also experience institutional betrayal.35 However, it is not clear that their experiences would be the same ones as patients’ or what outcomes (behavioral or emotional) would be associated with working alongside of institutional betrayal. The second future direction is one of intervening on institutional betrayal, either before it happens or addressing and repairing its effects. These interventions could operate at two levels: at a provider level, where individual physicians or other professionals are educated about institutional betrayal and how to prevent or ask about it, and at an institutional level where risk factors contributing to institutional betrayal are addressed.
Conclusion
Institutional betrayal in health care frequently accompanies negative medical experiences. This betrayal is associated with disengagement from health care and lower trust in health care organizations. Although many negative medical experiences may never be entirely preventable (e.g., adverse reactions to medications), institutional betrayal is preventable. But first, health care institutions must know about the harm their patients face. This study provides insight into the form and impact of institutional betrayal in health care.
Supplementary materials
Institutional Betrayal Questionnaire – Healthcare.
Note: Reproduced from Smith SP. First, Do No Harm: Institutional Betrayal in Healthcare [dissertation]. Eugene, OR: University of Oregon; 2016. Creative Commons license and disclaimer available from: http://creativecommons.org/licenses/by/4.0/legalcode.1
References
- 1.Smith SP. First, Do No Harm: Institutional Betrayal in Healthcare [dissertation] Eugene, OR: University of Oregon; 2016. [Google Scholar]
Footnotes
Disclosure
The author reports no conflicts of interest in this work.
References
- 1.Peabody FW. The care of the patient. J Am Med Assoc. 1927;88(12):877–882. [Google Scholar]
- 2.Altice FL, Mostashari F, Friedland GH. Trust and the acceptance of and adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;28(1):47–58. doi: 10.1097/00042560-200109010-00008. [DOI] [PubMed] [Google Scholar]
- 3.Mollborn S, Stepanikova I, Cook KS. Delayed care and unmet needs among health care system users: when does fiduciary trust in a physician matter? Health Serv Res. 2005;40(6 Pt 1):1898–1917. doi: 10.1111/j.1475-6773.2005.00457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tidkikis F, Strasen L. Patient-focused care units improve service and financial outcomes. Healthc Financial Manag. 1994;48(9):38. [PubMed] [Google Scholar]
- 5.Bowling A, Rowe G, Lambert N, et al. The measurement of patients’ expectations for health care: a review and psychometric testing of a measure of patients’ expectations. Health Technol Assess. 2012;16(30):i–xii. 1–509. doi: 10.3310/hta16300. [DOI] [PubMed] [Google Scholar]
- 6.Branch WT. Is the therapeutic nature of the patient-physician relationship being undermined? Arch Intern Med. 2000;160:2257–2260. doi: 10.1001/archinte.160.15.2257. [DOI] [PubMed] [Google Scholar]
- 7.Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79(4):613–639. doi: 10.1111/1468-0009.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freyd JJ. Betrayal Trauma: The Logic of Forgetting Childhood Abuse. Boston: Harvard University Press; 1996. [Google Scholar]
- 9.Heimer CA. Solving the problem of trust. In: Cook KS, editor. Trust and Society. New York: Russell Sage; 2001. pp. 40–88. [Google Scholar]
- 10.Murray SL, Holmes JG. A leap of faith? Positive illusions in romantic relationships. Pers Soc Psychol Bull. 1997;23:586–604. doi: 10.1037//0022-3514.71.6.1155. [DOI] [PubMed] [Google Scholar]
- 11.Mechanic D. Changing medical organization and the erosion of trust. Milbank Q. 1996;74(2):171–189. [PubMed] [Google Scholar]
- 12.Mechanic D. The functions and limitations of trust in the provision of medical care. J Health Politic Policy Law. 1998;23(4):661–686. doi: 10.1215/03616878-23-4-661. [DOI] [PubMed] [Google Scholar]
- 13.Mechanic D, Schlesinger M. The impact of managed care on patients’ trust in medical care and their physicians. J Am Med Assoc. 1996;275(21):1693–1697. [PubMed] [Google Scholar]
- 14.Rempel JK, Ross M, Holmes JG. Trust and communicated attributions in close relationships. J Pers Soc Psychol. 2001;81:57–64. [PubMed] [Google Scholar]
- 15.Freyd J, Birrell P. Blind to Betrayal: Why We Fool Ourselves We Aren’t Being Fooled. New Jersey: John Wiley & Sons; 2013. [Google Scholar]
- 16.Buchanan AE. Trust in managed care organizations. Kennedy Inst Ethics J. 2000;10(3):189–212. doi: 10.1353/ken.2000.0018. [DOI] [PubMed] [Google Scholar]
- 17.Budzi D, Lurie S, Singh K, Hooker R. Veterans’ perceptions of care by nurse practitioners, physician assistants, and physicians: a comparison from satisfaction surveys. J Am Acad Nurse Pract. 2010;22(3):170–176. doi: 10.1111/j.1745-7599.2010.00489.x. [DOI] [PubMed] [Google Scholar]
- 18.Rose A, Peters N, Shea JA, Armstrong K. Development and testing of the Health Care System Distrust Scale. J Gen Intern Med. 2004;19(1):57–63. doi: 10.1111/j.1525-1497.2004.21146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Institute of Medicine [webpage on the Internet] To Err Is Human: Building a Safe Health System. 1999. [Accessed February 17, 2017]. Retrieved from: http://www.nap.edu/books/0309068371/html/
- 20.Leape L, Lawthers AG, Brennan TA, Johnson WG. Preventing medical injury. Q Rev Bull. 1993;19(5):144–149. doi: 10.1016/s0097-5990(16)30608-x. [DOI] [PubMed] [Google Scholar]
- 21.Donaldson MS [webpage on the Internet] An overview of to err is human: re-emphasizing the message of patient safety. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality (US); 2008. [Accessed February 17, 2017]. Retrieved from: http://www.ncbi.nlm.nih.gov/books/NBK2673/ [Google Scholar]
- 22.Fernandez B, Sarata AK. Medical Malpractice: The Role of Patient Safety Initiatives. Domestic Social Policy Division: Library of Congress; 2006. [Accessed February 17, 2017]. pp. 1–23. Available from: https://www.americanbar.org/content/dam/aba/images/medical_liability/CRS_SI.pdf. [Google Scholar]
- 23.National Academies of Sciences, Engineering, and Medicine . Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015. [Google Scholar]
- 24.Smith CP, Freyd JJ. Institutional betrayal. Am Psychol. 2014;69(6):575–587. doi: 10.1037/a0037564. [DOI] [PubMed] [Google Scholar]
- 25.LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009;44(6):2093–2105. doi: 10.1111/j.1475-6773.2009.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith CP, Freyd JJ. Dangerous safe havens: institutional betrayal exacerbates sexual trauma. J Trauma Stress. 2013;26(1):119–124. doi: 10.1002/jts.21778. [DOI] [PubMed] [Google Scholar]
- 27.Mattox EA. Identifying vulnerable patients at heightened risk for medical error. Crit Care Nurse. 2010;30(2):61–70. doi: 10.4037/ccn2010102. [DOI] [PubMed] [Google Scholar]
- 28.Oppenheimer DM, Meyvis T, Davidenko N. Instructional manipulation checks: detecting satisficing to increase statistical power. J Exp Soc Psychol. 2009;45(4):867–872. [Google Scholar]
- 29.Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev. 2002;59(3):293–318. doi: 10.1177/1077558702059003004. [DOI] [PubMed] [Google Scholar]
- 30.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York: Guilford Press; 2013. [Google Scholar]
- 31.King A, Daniels J, Lim J, Cochrane DD, Taylor A, Ansermino JM. Time to listen: a review of methods to solicit patient reports of adverse events. Q Safety Health Care. 2010;19(2):148–157. doi: 10.1136/qshc.2008.030114. [DOI] [PubMed] [Google Scholar]
- 32.Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD checklist: reliability, validity, and diagnostic utility; Paper presented at: Annual Meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- 33.Armstrong DK, Rose A, Peters N, Long JA, McMurphy S, Shea JA. Distrust of the health care system and self-reported health in the United States. J Gen Intern Med. 2006;21:292–297. doi: 10.1111/j.1525-1497.2006.00396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schwappach DL. “Against the silence”: development and first results of a patient survey to assess experiences of safety-related events in hospital. BMC Health Serv Res. 2008;20(8):59. doi: 10.1186/1472-6963-8-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kahn WA. Holding Fast: The Struggle to Create Resilient Caregiving Organizations. New York: Brunner Routledge Psychology Press; 2005. [Google Scholar]
- 36.Jesson L, Knapp PB. My Lawyer Told Me to Say I'm Sorry: Lawyers, Doctors, and Medical Apologies. William Mitchell Law Review. 2009;35(2):1–46. [Google Scholar]
- 37.Ho B, Liu E. Does Sorry Work? The Impact of Apology Laws on Medical Malpractice (SSRN Scholarly Paper No. ID 1744225) Rochester, NY: Social Science Research Network; 2010. [Accessed February 17, 2017]. webpage on the Internet. Retrieved from: http://papers.ssrn.com/abstract=1744225. [Google Scholar]
- 38.Brooks AW, Dai H, Schweitzer ME. I’m sorry about the rain! Superfluous apologies demonstrate empathic concern and increase trust. Soc Psychol Pers Sci. 2014;5:467–474. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Institutional Betrayal Questionnaire – Healthcare.
Note: Reproduced from Smith SP. First, Do No Harm: Institutional Betrayal in Healthcare [dissertation]. Eugene, OR: University of Oregon; 2016. Creative Commons license and disclaimer available from: http://creativecommons.org/licenses/by/4.0/legalcode.1