Abstract
Internalizing disorders co-occur with alcohol use disorder (AUD) at a rate that exceeds chance and compromise conventional AUD treatment. The “vicious cycle” model of comorbidity specifies drinking to cope (DTC) as a link between these disorders that, when not directly addressed, undermines the effectiveness of conventional treatments. Interventions based on this model have proven successful but there is no direct evidence for how and to what extent DTC contributes to the maintenance of comorbidity. In the present study, we used network analysis to depict associations between syndrome-specific groupings of internalizing symptoms, alcohol craving, and drinking behavior, as well as DTC and other extradiagnostic variables specified in the vicious cycle model (e.g., perceived stress and coping self-efficacy). Network analyses of 362 individuals with comorbid anxiety and AUD assessed at the beginning of residential AUD treatment indicated that while internalizing conditions and drinking elements had only weak direct associations, they were strongly connected with DTC and perceived stress. Consistent with this, centrality indices showed that DTC ranked as the most central/important element in the network in terms of its “connectedness” to all other network elements. A series of model simulations—in which individual elements were statistically controlled for—demonstrated that DTC accounted for all the relationships between the drinking-related elements and internalizing elements in the network; no other variable had this effect. Taken together, our findings suggest that DTC may serve as a “keystone” process in maintaining comorbidity between internalizing disorders and AUD.
Keywords: network analysis, comorbidity, alcohol use disorder, drinking to cope
The observation that high levels of negative affect characterize a large subgroup of those who abuse alcohol predates the modern study of alcohol use disorders (Babor, 1996), and is manifest in the modern epidemiological finding of a two- to four-fold increase in the prevalence of various anxiety and mood (“internalizing”) disorders among those with an alcohol use disorder (AUD; “comorbidity;” Kushner et al., 2012; Kushner, Krueger, Frye, & Peterson, 2008). Outcome studies demonstrate the adverse impact of comorbidity in AUD and highlight the complexity of the problem. For example, the presence of clinically significant anxiety or depression approximately doubles the risk for AUD treatment failure (Cornelius et al., 1997; Greenfield et al., 1998; Haver, 2003; Heizer & Pryzbeck, 1988; Kushner et al., 2005; Regier et al., 1990; Tómasson & Vaglum, 1995). Surprisingly, however, providing a standard psychiatric treatment for anxiety or depression disorder alone (Book, Thomas, Randall, & Randall, 2008) or in combination with standard AUD treatment (see meta-analysis by Hobbs, Kushner, Lee, Reardon, & Maurer, 2011), does not appreciably improve AUD outcomes in comorbid individuals. This suggests that other conditions and/or processes (i.e., beyond the internalizing disorders) contribute to the elevated relapse risk of those with co-occurring anxiety/depressive disorders and AUD.
In the early literature, pathological alcohol use was proposed by Freud to develop and persist as a defense against “intra-psychic distress” (Kushner, 2014). While Freudian theory has been largely supplanted in psychology and psychiatry, the notion of drinking to cope (DTC) with negative affect remains an essential constituent of cognitive-behavioral models of comorbidity such as self-medication (Khantzian, 1985; Quitkin, Rifkin, Kaplan, & Klein, 1972), tension reduction (Conger, 1956), and stress-response dampening (Sher, 1987; Sher & Levenson, 1982). Broadly speaking, these models hold that problematic drinking develops and escalates when the experience of strong negative affect (anxiety, depression, stress) is coupled with (a) low self-efficacy to resist drinking when experiencing negative affect, and (b) the belief that drinking is the most viable coping option available. While such models were initially causally unidirectional (i.e., it was presumed that anxiety leads to drinking via DTC motives and negatively reinforced drinking), more recent models have identified positive feedback influences. These models implicate neurobiological adaptations (Koob & Le Moal, 2001) and negative psychosocial consequences associated with chronic drinking in exacerbating negative affect and DTC (Koob & Le Moal, 2001; Kushner, Abrams, Thuras, & Hanson, 2000; Kushner et al., 2006). These processes describe a vicious cycle (or mutual maintenance) model of comorbid internalizing problems and pathological drinking in which DTC simultaneously functions as a (a) relay between a feedforward process (internalizing problems → DTC → AUD); and (b) an outcome of a feedback process (DTC ← internalizing problems ←AUD).
This vicious cycle model (and the earlier unidirectional models in which DTC is also central) provides an explanation of why successful treatment of internalizing disorders fails to improve AUD outcomes among comorbid individuals. Namely, these treatments fail to address DTC, which remains available to maintain or reinitiate the vicious cycle (Kushner, Abrams, & Borchardt, 2000) in response to even moderate (e.g., subclinical) negative affect. Consistent with this view, Kushner et al. (2013) found that adding a cognitive–behavioral treatment aimed at reducing both negative affectivity and DTC to a standard AUD treatment improved alcohol outcomes to a greater degree than adding a treatment aimed at reducing negative affectivity alone. This supports the notion that DTC can maintain comorbidity, even when internalizing conditions are treated. Additional support for DTC’s central role in comorbidity comes from previous findings demonstrating that level of DTC is a key predictor of AUD development (Crum, Mojtabai et al., 2013; Menary, Kushner, Maurer, & Thuras, 2011) and a robust moderator of AUD relapse risk among individuals with internalizing disorders (Anker, Kushner, Thuras, Menk, & Unruh, 2016). Taken together, these findings are consistent with a conceptualization of comorbidity, not as two distinct conditions, but as a single dynamic system maintained through processes such as DTC.
Using Network Analysis to Visualize Elements of the Vicious Cycle Model
In the present study, we use a novel application of network analysis (Newman, 2010) to visually characterize the direct and indirect associations among variables relevant to the vicious cycle model in comorbid individuals. Network analysis has been used extensively to depict complex systems in disciplines as diverse as material science (Bhadeshia, 1999), computer networking (Wellman, 2001), information science (Otte & Rousseau, 2002), public health (Luke & Harris, 2007), sociology (Borgatti, Mehra, Brass, & Labianca, 2009), and neuroscience (Sepulcre, Sabuncu, & Johnson, 2012). The basic components of networks include nodes that represent variables and edges that represent the association (or lack of association) between the variables. Within the correlational space of a network, variables with strong direct relationships tend to cluster, while variables with weak relationships tend to separate. Network elements (nodes) with strong direct relationships (single edges) to several other elements have a central location in the graphical network. Centrality indices are used to quantify the importance of individual elements within the network in terms of interrelatedness with other elements. High centrality for an element indicates its importance in maintaining network connectivity.
The network approach has only recently been applied in the area of psychopathology, where it has been used primarily to characterize mental health problems in terms of the relationships between individual symptoms (Borsboom & Cramer, 2013; Cramer, Waldorp, van der Maas, & Borsboom, 2010; De Schryver, Vindevogel, Rasmussen, & Cramer, 2015; Frewen, Schmittmann, Bringmann, & Borsboom, 2013; Fried, 2015; McNally et al., 2015; Robinaugh, LeBlanc, Vuletich, & McNally, 2014). However, a smaller number of studies have employed network analysis to study psychopathology at the construct level (i.e., where nodes represent conceptually related symptom/behavior aggregates; Costantini et al., 2015; Costantini & Perugini, 2012; Hoorelbeke, Marchetti, De Schryver, & Koster, 2016; Schlegel, Grandjean, & Scherer, 2013). The construct level and symptom level approaches taken by these investigators demonstrate the flexibility of the network approach in characterizing psychopathology phenomena at various levels of analysis.
Because of our interest in applying network analysis to characterize the vicious cycle model at the level of analysis used in the models development and clinical application, we operationalized elements in the present study using summary scores representing manifest levels of internalizing constructs (e.g., social anxiety, panic attacks, depression) and alcohol use (e.g., alcohol craving and total drinks), along with levels of DTC and other extradiagnostic constructs relevant to the vicious cycle model. The latter included a measure of general subjective stress as this may be distinct from anxiety and depression psychopathology (Cohen, Kamarck, & Mermelstein, 1983), as well as a measure of self-efficacy for coping with negative affect without alcohol use. In addition to being a part of the vicious cycle model, both perceived stress and self-efficacy have been linked to alcohol use generally and DTC specifically in past research (Black et al., 2012; Cooper, Russell, Skinner, Frone, & Mudar, 1992; Goldsmith, Thompson, Black, Tran, & Smith, 2012; Laurent, Catanzaro, & Callan, 1997; Peirce, Frone, Russell, & Cooper, 1994).
The Present Study
The first aim of the present study was to visualize the network structure of unique relationships between elements of the vicious cycle model (described above). Because the various internalizing measures are known to be highly intercorrelated (e.g., Krueger, 1999), we used the GLASSO (graphical least absolute selection and shrinkage operator) procedure (Friedman, Hastie, & Tibshirani, 2014), as this method characterizes the unique variance between nodes in the network. The second aim was to probe changes in the correlational structure when controlling for specific network elements. This allowed us to identify “keystone” network elements; that is, those that, if removed, would maximally disrupt relationships among other elements in the network. Toward this end, we first computed an association network from a zero-order correlation matrix and then computed a series of semipartial correlations that systematically controlled the variance associated with selected individual elements in the model (e.g., DTC, internalizing conditions, perceived stress). It is important to note that while these simulations cannot demonstrate causality (Pearl, 2000), they do provide a means of interrogating the cross-sectional data for clues as to which elements are important for maintaining the network structure. For the third and final aim, we explored potential gender differences in network structure as well as the presence of gender-specific effects on the results of the model simulations. This aim is important as gender is a moderator in the prevalence, development, and treatment of AUD and internalizing disorders (Altemus, Sarvaiya, & Neill Epperson, 2014; Karpyak et al., 2016; Simonds & Whiffen, 2003; Zilberman, Tavares, Blume, & el-Guebaly, 2003).
Method
Participants
Data were obtained at the baseline assessment of a randomized clinical trial (RCT) of a cognitive-behavioral therapy for co-occurring anxiety disorder and alcohol use disorder (Kushner et al., 2013). Unfortunately, data from post treatment follow-ups of the RCT could not be utilized in the present study because several of the variables used in the network analysis were only collected at the baseline assessment. Data were collected from 362 adult AUD treatment patients with a co-occurring anxiety disorder during a single baseline session within the first week of residential treatment before the clinical trial interventions. A more detailed description of the sampling methods is provided by Kushner et al. (2013).
Inclusion/Exclusion Criteria
Participants were selected from a 21-day community-based residential chemical dependency (CD) treatment program. Inclusion criteria were current (past 30 days) DSM–IV diagnosis of alcohol dependence and at least one current diagnosis of the following anxiety disorders: panic (with or without agoraphobia), social anxiety, and/or generalized anxiety. Exclusion criteria were primary diagnosis of major depression or posttraumatic stress disorder, a history of bipolar disorder, psychosis or schizophrenia, ongoing acute suicidality, inability to read or speak English, or the presence of cognitive impairments that were deemed sufficiently severe to impede study participation. Patients with a current diagnosis of drug dependence were not excluded; however, alcohol had to be the primary reason for their treatment. DSM–IV diagnoses of current (past 30 days) major depression and posttraumatic stress disorder were also assessed and recorded. Information on lifetime history of DSM–IV disorders was not obtained from participants. Eligible participants provided written informed consent. The study was approved by the University of Minnesota’s Institutional Review Board and was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) awarded to the last author.
Recruitment
A fuller description of the recruitment methods is reported in Kushner et al. (2013) and is briefly summarized here. Participants were recruited during their first week of the CD treatment program in three screening steps. In Step 1, a screening questionnaire was offered to 100% of the patients entering the CD treatment. In Step 2, responding patients who reported alcohol as the primary problem for which they were receiving treatment and also endorsed significant symptoms of social anxiety, panic, and/or generalized anxiety on the questionnaire were invited to a screening interview where they were asked to elaborate on their endorsements. The clinical team (including a staff psychologist) then evaluated these responses to determine if the candidate was likely to meet the inclusion/exclusion criteria. Qualified candidates proceeded to Step 3 where psychiatric diagnoses were formally established using the Structured Clinical Interview (SCID) for DSM–IV (First, Spitzer, Gibbon, & Wilhams, 1998).
Measures
Internalizing psychopathology measures
Informed by the constructs that characterize internalizing psychopathology (Krueger, 1999), we obtained symptom-level aggregate measures of “distress” (pervasive negative affect and dysphoria associated with generalized anxiety and depression) and “fear” (fear or avoidance of specific stimuli associated with social anxiety, panic, and agoraphobia). Ah internalizing assessments referred to the previous 30 days prior to treatment entry. It is important to note that assessment measures do not represent diagnoses but rather severity levels of different internalizing psychopathologies. We selected the internalizing measures described below because they are psychometrically sound, are in wide use in both clinical and research settings, and produce reasonably well-distributed scores for variables specified in the vicious cycle model. To capture the full range of variance within the sample, internalizing assessments were completed by ah participants regardless of whether they met criteria for the corresponding DSM diagnosis.
Distress measures
Generalized anxiety (labeled GA in models)
The total score on the 16-item Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990) was used to quantify the extent of generalized anxiety experienced by participants. Each item was rated on a 5-point scale that ranged from 1 = not at all typical to 5 = very typical (score range: 16 to 80). The instrument was designed to capture the excessiveness, generality, and uncontrollable dimensions of worry.
Depression (labeled DEP models)
Behavioral manifestations of depression severity were assessed using the total score on the Beck Depression Inventory (BDI; Beck, Steer, & Brown, 1996). Participants were instructed to rate descriptions that correspond to specific symptoms of depression on a 4-point scale (0 = symptom is not present to 3 = symptom is severe; score range: 0 to 63).
Fear measures
Social phobia (labeled SOC in models)
The total score on the 20-item Social Phobia Scale (SPS; Mattick & Clarke, 1998) was used to assess social fears. The scale measures fear of being evaluated/scrutinized during activities such as eating, drinking, and writing. Participants are instructed to rate their level of discomfort engaging in various social activities on a scale from 0 = not at all to 4 = extremely (score range: 0 to 80).
Panic (labeled PAN in models)
The total score from a 13-item version of the Panic Disorder Severity Scale (PDSS-SR) was used as a measure of the frequency and severity of panic symptoms (Houck, Spiegel, Shear, & Rucci, 2002). Items are variously rated in terms of severity, frequency, and consequences of panic attacks (score range: 0 to 28).
Agoraphobia (labeled AGR in models)
Avoidance behaviors that typify agoraphobia were quantified by summing items from the Mobility Inventory for Agoraphobia (MI; Chambless, Caputo, Jasin, Gracely, & Williams, 1985). Participants rated the frequency (from 0 = never avoid to 1 = always avoid; score range: 0 to 100) they avoided situations generally associated with fear and avoidance in individuals with agoraphobia (e.g., crowds, driving, being far away from home, etc.).
Drinking-related measures
We chose two alcohol-related measures to represent cognitive and behavioral aspects of AUD, alcohol craving, and total number of drinks.
Alcohol craving (labeled CRA in models)
The frequency of alcohol craving during the 30 days before treatment was assessed using a single item from the Obsessive Compulsive Drinking Scale (OCDS). The item read, “How much of your time when you’re not drinking is occupied by ideas, thoughts, impulses or images related to drinking?” The five response options included: none, less than 1 hour a day, 1–3 hours a day, 4–8 hours a day, and greater than 8 hours a day (score range: 0 to 4; Anton, Moak, & Latham, 1995).
Drinking behavior (labeled DRI in models)
The total drinks consumed during the 4 months before residential treatment entry served as a measure of drinking behavior and was assessed with the Timeline Follow-Back (TLFB) interview (Sobell & Sobell, 1992). The 4-month timeframe was selected as we considered it to be a more representative and stable sampling of pretreatment drinking behavior than the 1-month prior to treatment (e.g., due to changes in circumstances and opportunities to drink in the period leading up to treatment; Stasiewicz, Schlauch, Bradizza, Bole, & Coffey, 2013). In the TLFB, an interviewer uses a calendar to document a participant’s estimate of the number of alcoholic drinks they consumed on each day of the assessment period. A standard alcoholic drink was defined as one ounce of alcohol spirits, four ounces of wine, or 12 ounces of beer. The TLFB has been deemed a psychometrically reliable and valid instrument for collecting drinking history in clinical populations (Pedersen & LaBrie, 2006).
Coping- and stress-related measures
DTC in negative affect situations (labeled DTC in models)
The Inventory of Drinking Situations IDS-100 (Annis, 1982) is a psychometrically reliable and valid 100-item self-report questionnaire that assesses the frequency of heavy drinking in relation to Marlatt’s eight high-risk situations/categories (Cannon, Leeka, Patterson, & Baker, 1990; Marlatt, 1979). Index scores for the 20-item unpleasant emotions (IDS-UE) subscale of the IDS served as the primary measure of DTC, as it was designed to capture DTC behavior associated with negative affect situations (e.g., “When I was depressed about things in general,” “When I felt under a lot of pressure;” see supplemental materials for a complete list of items). Participants were instructed to mark a response that most accurately described the extent (1 = never to 4 = almost always) to which they drank heavily in IDS-UE situations during the 30 days leading up to their CD treatment (score range: 20 to 80).
Coping self-efficacy (labeled SEL in models)
Respondents’ confidence they could refrain from drinking heavily to cope with negative affect situations (“self-efficacy”) was assessed using the total score on the eight-item negative emotional states subscale of the Situational Confidence Questionnaire (SCQ-NE; e.g., “If I felt confused about what I should do,” “If I were afraid that things were not going to work out;” Annis, 1988). Values were coded so that low total scores represented high self-efficacy and high total scores represented low self-efficacy (1 = very confident to 5 = not at all confident; score range: 8 to 48).
Perceived stress (labeled as STR in models)
Perceived stress experienced during the 30 days before treatment admission was measured using the total score on the 10-item Perceived Stress Scale (PSS; Cohen et al., 1983). The PSS is a widely used psychometrically reliable measure that assesses subjective stress and perceived ability to cope with this stress on a 4-point scale containing the following response options: 1 = almost never, 2 = sometimes, 3 = fairly often, and 4 = very often (score range: 10 to 40). Sample items include “In the last month, how often have you been upset because something that happened unexpectedly?” and “… how often have you found that you could not cope with all the things you had to do?”
Statistical Analyses
Networks were based on Spearman rank-order correlation matrices using the statistical platform R (R Core Team, 2015) and accompanying package igraph (Csardi & Nepusz, 2006). Spearman’s rank-order correlations were used due to the skewed (i.e., non-normal) distribution of several assessment scores, which likely reflects the severity of psychopathology that characterizes the comorbid study sample. Each network contained two basic components: nodes, representing the observed variables described above, and edges, representing the statistical relationship between the nodes (i.e., correlations and partial correlations).
Aim 1: Network Structure
GLASSO network
To assess the network structure of comorbidity we plotted measures using the GLASSO procedure (contained in the R package GLASSO; Friedman et al., 2014; Borsboom & Cramer, 2013). The GLASSO procedure estimates a network in which edges represent partial correlation coefficients (i.e., each edge represents the relationship between two elements while controlling for all other elements in the network). The least absolute shrinkage and selection operator precludes the need to select an ultimately arbitrary edge weight cut-off, and has been widely used to establish parsimony, avoid spurious correlations within the model, and facilitate objective interpretability of network structures in complex models that contain a limited set of elements (Costantini et al., 2015; Epskamp, Borsboom, & Fried, 2016; Hoorelbeke et al., 2016).
Centrality indices
The following measures were used to index the centrality of specific network elements/nodes within the comorhidity network. “Betweenness” indexes the number of times each node lies on the shortest path between two other nodes. “Closeness” indexes the average distance (via the number of steps/edges) from each node to all other nodes in the network (Wasserman & Faust, 1994). “Strength” is the sum of edge weights (i.e., the strength of the partial correlations represented by edges) that connect directly to each node (Wasserman & Faust, 1994). From a psychopathology network perspective, elements with high centrality across all three indices reflect elements that are strongly interrelated with other elements in the network, and thus may have high clinical relevance (Fried, Epskamp, Nesse, Tuerlinckx, & Borsboom, 2016; Rhemtulla et al., 2016). The R package qgraph was used to calculate and plot centrality for each element of the GLASSO network (Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, 2012).
Stability of GLASSO centrality indices
As noted above, centrality indices are important for making inferences about the “connectivity” of individual elements in networks. To assess centrality measure stability within the GLASSO network we used bootstrap routines available in the R package bootnet (Epskamp, 2015), following the guidelines established by Epskamp et al. (2016). This approach involves comparing centrality measures from a bootstrapped subsample of nodes and cases/subjects as a function of varying subsample sizes. For each subsample size, 1,000 bootstrap samples of the data were obtained and centrality measures were recalculated. Stability of the centrality indices of the GLASSO network was assessed by examining the correlation between the centrality measures derived from the entire sample and the centrality measures derived from bootstrapped subsets of the sample; the higher the correlation, especially with respect to greater diminution in sample and node size, the more stable the centrality measures. Because a primary focus of this article is to examine the specific patterns of relationships among the elements, we also assessed stability of the centrality indices for each GLASSO element/node. We defined poor stability following the guidelines of Epskamp et al. (2016) in terms of a substantial change in the rank order of centrality measures after dropping 10% of the case or nodes.
Aim 2: Models Probing the Contribution of Specific Elements to Network Connectivity
While centrality measures identify which elements maintain network connectivity, they do not provide information about the impact on the network if the effects of key variables were removed. To address this, we first computed a zero-order correlation matrix and plotted it based on the Fruchterman and Reingold algorithm (i.e., a stochastic algorithm, which helps to identify patterns in a network by clustering closely related nodes together). This represented the baseline network from which we compared a series of targeted, theory-driven simulations that statistically controlled for (i.e., regressed out) specific network features (i.e., DTC; perceived stress; and elements related to the fear and distress dimensions of internalizing symptom levels, separately and combined). These probes offer a means of identifying the extent to which specific elements are necessary in maintaining connectivity within the comorbidity network.
To facilitate visual representation of meaningful network relationships in the baseline association network and network probes (i.e., those with targeted elements removed), edges at or below 0.15 were omitted and the magnitude of relationships between network elements were represented by edge width (stronger relationship = thicker width; Robinaugh et al., 2014). Three edge thickness gradients denoted the zero-order correlation strength between nodes according to the following parameters: thinnest width = 0.16 to 0.25, medium width = 0.26 to 0.35, thickest width = > 0.36. Finally, node colors represent the following variable categories: (a) blue: distress-related measures (GA and DEP); (b) red: fear-related measures (SOC, PAN, and AGR); (c) pink: drinking-related measures (CRA and DRI); and (d) yellow: perceived stress (STR) and coping-related measures (DTC and SEL).
Aim 3: Examining Gender Differences
The networks detailed above, were reproduced separately for both men and women to determine whether the network structure (Aim 1), and the impact of network probes (Aim 2) differed as a function of gender.
Results
Participants
Of the 362 participants, the average age was 39.3 (standard deviation [SD] = 10.24) and 38% were female (N = 138). Participants with more than one of the three anxiety disorders required for inclusion in the study were asked to identify their “primary” disorder in terms of its interference in their daily functioning: 41.7% endorsed primary social anxiety disorder (N = 151), 40.3% endorsed primary generalized anxiety disorder (N = 146), 14.9% endorsed primary panic disorder without agoraphobia (N = 54), and an additional 3.0% endorsing primary panic disorder with agoraphobia (N = 11). Secondary and tertiary anxiety and major depression diagnoses were also recorded. More than half of the sample had two or more co-occurring anxiety disorders (56.0%, N = 201), and approximately half of the total sample met diagnostic criteria for major depression (51.4%, N = 186).
Table 1 shows the mean (SD) levels of each network element in our sample. Not surprisingly, the severity of each measure (i.e., total scores) in the study sample were well above population norms. Specifically, differences between the various internalizing disorder severity scores in the present study and the normed scores for these measures in healthy participants reported in previous work were as follows: PSWQ (GA): 64.13, SD = 11.59 versus 42.2, SD = 11.5 (Gillis, Haaga, & Ford, 1995); BDI (DEP): 20.40, SD = 9.09 versus 6.6, SD = 8.1 (Gillis et al., 1995); SPS (SOC): 32.43, SD = 17.30 versus 12.5, SD = 11.5 (Heimberg, Mueller, Holt, Hope, & Liebowitz, 1992); and PDSS-SR (PAN): 10.99, SD = 6.34 versus 2.67, SD = 1.16 (Keough et al., 2012). Similarly, the score on the PSS (STR) scale was 28.15 (SD = 5.50) versus 25.0 (SD = 8.00) reported in healthy samples (Cohen et al., 1983).
Table 1.
Mean Total Scores, Element Labels, and the Study Assessments/Measures Used to Create Networks
| Network element (Node label) | Assessment | Mean (SD) |
|---|---|---|
| Internalizing distress measures (Blue) | ||
| Generalized anxiety (GA) | Penn State Worry Questionnaire | 64.13 (11.59) |
| Depression (DEP) | Beck Depression Inventory | 20.40 (9.09) |
| Internalizing fear measures (Red) | ||
| Social phobia (SOC) | Social Phobia Scale | 32.43 (17.30) |
| Panic disorder (PAN) | Panic Disorder Severity Scale | 10.99 (6.34) |
| Agoraphobia (AGR) | Mobility Inventory for Agoraphobia | 31.59 (19.78) |
| Alcohol-related measures (Pink) | ||
| Alcohol craving (CRA) | Obsessive Compulsive Drinking Scale | 2.67 (1.05) |
| Total drinks 4 months before treatment (DRI) | Time Line Follow-Back Interview | 1,608.76 (1271.51) |
| Stress and coping measures (Yellow) | ||
| Perceived stress (STR) | Perceived Stress Scale | 28.15 (5.50) |
| Drinking to cope with negative affect (DTC) | Inventory of Drinking Situations – unpleasant emotions subscale | 62.93 (12.15) |
| Coping self-efficacy (SEL) | Situational Confidence Questionnaire – negative emotions subscale | 32.91 (10.91) |
Note. GA = generalized anxiety; DEP = depression; SOC = social anxiety; PAN = panic; AGR = agoraphobia; STR = perceived stress; DTC = drinking to cope; SEL = coping self-efficacy; CRA = alcohol craving; DRI = drinking behavior.
Aim 1: Network Structure
GLASSO network
The GLASSO network is shown in Figure 1A. Anxiety/depression elements are on one end, separated from the drinking-related elements (alcohol craving and drinking behavior) on the opposite end, and DTC and perceived stress are between the two clusters, with direct links to both. To quantify element importance within the network structure, centrality measures of betweenness, closeness, and strength were calculated for each element and summarized in a centrality plot (Figure 1B, 1C, and 1D). The plot shows that DTC was the most central element in the GLASSO network, indicating that it: (a) lies on the shortest path between other network elements (“betweenness,” Figure 1B); (b) has the highest number of actual connections relative to total number of possible connections (“closeness,” Figure 1C); and (c) has the highest sum of connected edge weights (“strength,” Figure 1D). Taken together, the GLASSO network configuration suggests DTC is an important element of the internalizing-AUD comorbidity network.
Figure 1.
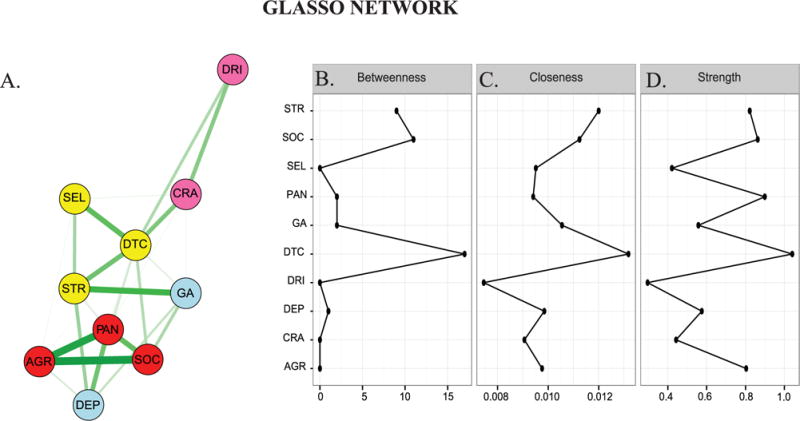
GLASSO network structure (left panel) and corresponding centrality plots (right panels). Nodes/elements represent measures of internalizing disorders, perceived stress, alcohol craving, drinking behavior/total number of drinks consumed, DTC, and coping self-efficacy. Edges represent partial correlations between nodes (controlling for all other nodes) and edge widths represent the strength of element-element relationship according to the GLASSO algorithm. The algorithm removes edges that are at or near zero. See the online article for the color version of this figure.
Stability of GLASSO centrality measures
Figure 2 depicts the stability of the centrality measures in the GLASSO network. Shown are the average correlations between centrality indices of the original GLASSO network and GLASSO networks where varying proportions of nodes (Figure 2A) and cases (Figure 2B) are dropped. The average correlation remained high after 50% of the nodes and cases were dropped, indicating stability in the centrality measure estimates (Epskamp et al., 2016).
Figure 2.
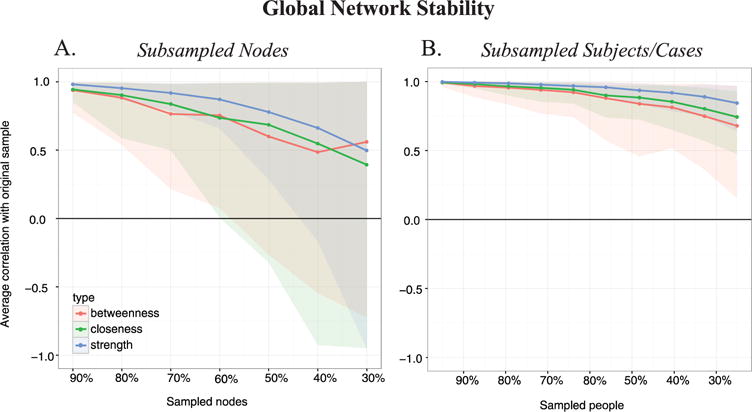
Average correlations between global centrality indices (betweenness, closeness, and strength) of the GLASSO network after dropping varying proportions of nodes/elements (left panel) and cases/subjects (right panel). See the online article for the color version of this figure.
Figure 3 contains estimates of each centrality measure for individual network elements/nodes as a function of different node (upper panels) and case/people (lower panels) sampling levels. The relative rank order for each centrality measure is maintained at the 90% node and case sampling level, indicating stability in the centrality of individual elements (cf. Epskamp et al., 2016). Notably, DTC consistently had the highest centrality, even after dropping large proportions of nodes or cases, reinforcing DTC as the most central network element in the GLASSO network.
Figure 3.
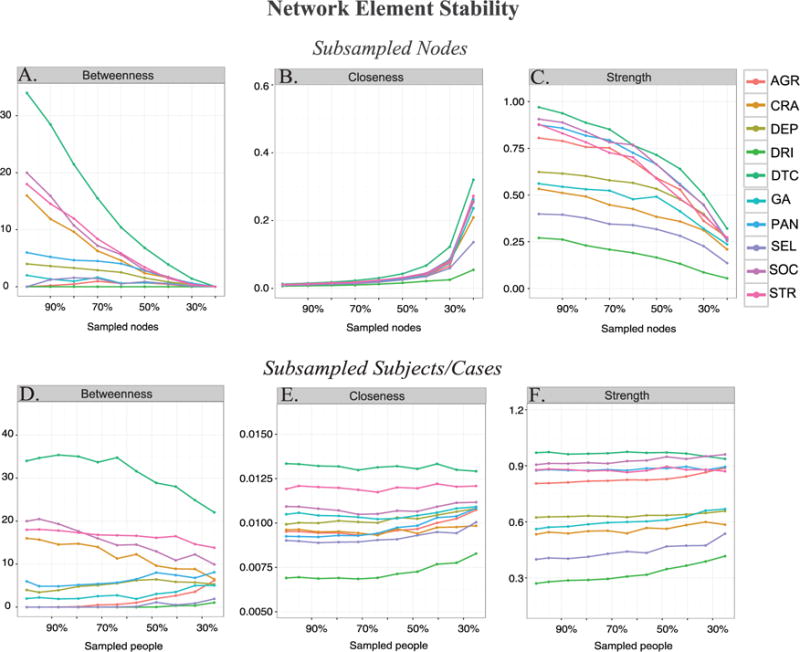
Centrality measure estimates (betweenness, closeness, and strength) for each element of the GLASSO network after dropping varying proportions of nodes/elements (upper panels) and subjects/cases (lower panels). See the online article for the color version of this figure.
Aim 2: Models Probing the Contribution of Specific Elements to Network Connectivity
The baseline (zero-order) association network is shown in Figure 4A. The model simulation probes were conducted by regressing out subsets of elements from the network, beginning with DTC. As shown in Figure 4B, controlling for DTC accounted for the majority of the relationships among the other network elements. In particular, after controlling for DTC, CRA and total drinks (DRI) were effectively isolated from the rest of the network elements. This suggests that once DTC is eliminated alcohol craving and total drinks are conditionally independent (in terms of having an edge weight ≤ 0.15) of both perceived stress and the internalizing elements. Removing DTC from the network also weakened or eliminated direct connections between the perceived stress and the internalizing elements, particularly with respect to the fear-related elements of PAN, SOC, and AGR which decreased by 39% (from 0.31 to 0.19), 60% (from 0.25 to 0.1), and 57% (from 0.21 to 0.09), respectively. This suggests relationships between perceived stress and the fear-related elements are attributed, in part, to variance shared with DTC.
Figure 4.
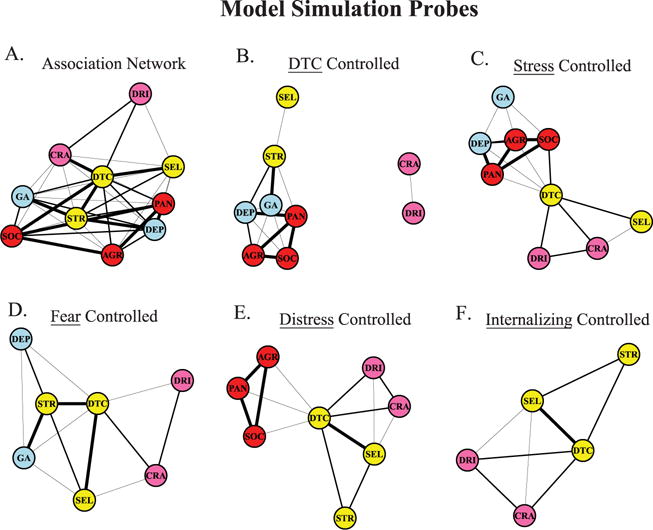
Association network (Figure 4A; edges represent zero-order correlations) and networks after controlling for DTC (Figure 4B), perceived stress (Figure 4C), fear-related elements (Figure 4D), distress-related elements (Figure 4E), and all internalizing elements (Figure 4F). Edges represent semipartial correlations between nodes after controlling for the specified elements. Edge width corresponds to the following correlation values: thinnest width = 0.16 to 0.25, medium width = 0.26 to 0.35, thickest width = 0.36. Edges under 0.15 were omitted from the network. Nodes/elements represent measures of internalizing disorders (red = fear; blue = distress), coping measures (yellow), and drinking-related measures (pink). Edges under 0.15 were omitted from the network to facilitate interpretation of important relationships. See the online article for the color version of this figure.
To determine whether this level of change was unique to the influence of DTC, we examined additional probes that selectively controlled for perceived stress (STR; Figure 4C); as well as domains of fear (Figure 4D; SOC, PAN, and AGR), distress (Figure 4E; GA and DEP), and all internalizing measures (i.e., fear and distress combined; Figure 4F). In contrast to the DTC probe, none of these probes isolated the drinking-related elements from the rest of the network elements.
The central role of perceived stress on the relationship between DTC and the internalizing elements was also revealed. For example, relative to the zero-order association network (Figure 4A), controlling for perceived stress (Figure 4C) resulted in a reduction of the number and strength of edges/relationships connecting DTC to the distress-related internalizing elements. Specifically, the perceived stress probe resulted in a 58% reduction in relationship strength between DTC and GA (0.13 vs. 0.31) and a 42% reduction in relationship strength between DTC and DEP (0.18 vs. 0.31). In contrast, the change in relationship strength between DTC and the fear-related elements after controlling for perceived stress was less robust and ranged from 19% for SOC (0.29 vs. 0.36) and 33% for PAN (0.19 vs. 0.33). Thus, perceived stress accounts for approximately one half of the shared variance between DTC and the distress-related internalizing elements and it accounts for approximately one quarter of the shared variance between DTC and the fear-related elements.
Aim 3: Examining Gender Differences
Networks were also generated separately for men and women to explore possible gender-dependent differences in the aforementioned results. Visual comparison of network elements in the association and GLASSO networks as well as a comparison of each network’s corresponding centrality values indicated marked similarity between men and women. Namely, these results indicated that DTC was a central factor, regardless of gender (see Figure 5). There was also congruence in results between women and men with respect to the model simulation probes such that controlling for DTC accounted for the majority of the relationships among the other network elements, and isolated alcohol craving and total drinks from networks of both men and women (see Figure 6). Together these results suggest DTC accounts for much of the association between internalizing disorders and AUD, regardless of gender.
Figure 5.
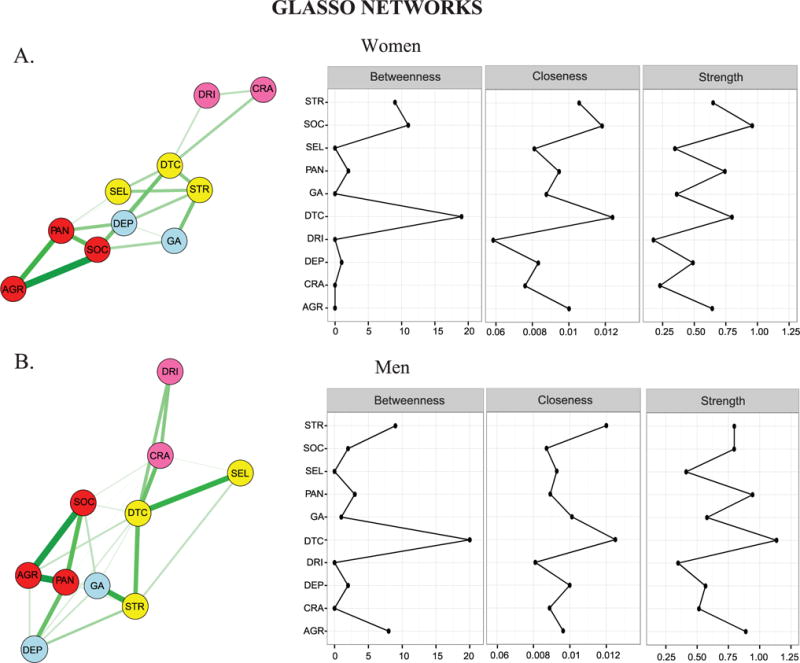
GLASSO networks (left panel) and corresponding centrality plot (right panels) for women (Figure 5A) and men (Figure 5B). Nodes/elements represent measures of anxiety and depression, perceived stress, alcohol craving, drinking behavior/total number of drinks consumed, DTC, and coping self-efficacy. Edges represent partial correlations between nodes (controlling for all other nodes) and edge widths represent the strength of element-element relationship according to the GLASSO algorithm. The algorithm removes edges that are at or near zero. See the online article for the color version of this figure.
Figure 6.
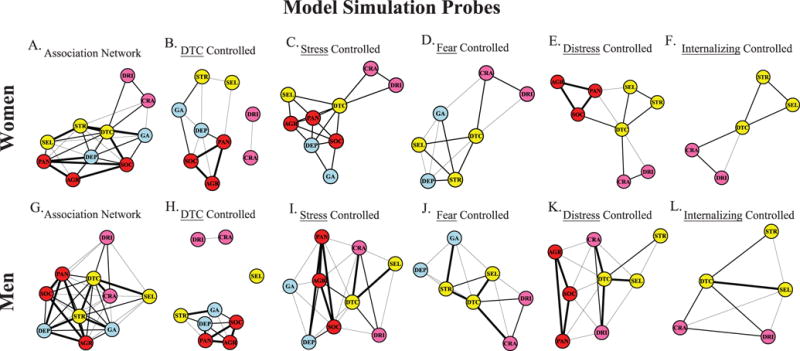
Association networks (edges represent zero-order correlations; Figures 6A and 6G) and networks after controlling for perceived stress (Figures 6A and 6G), fear (Figures 6A and 6G), distress (Figures 6A and 6G), and fear and distress elements combined Figures (6A and 6G) in women (top panels) and men (bottom panels). Nodes/elements represent measures of depression and anxiety measures (red = fear; blue = distress), coping- and stress-related measures (yellow), and drinking-related measures (pink). Edges represent semipartial correlations between nodes, and edge width corresponds to the following correlation values: thinnest width = 0.16 to 0.25, medium width = 0.26 to 0.35, thickest width = 0.36. Edges under 0.15 were omitted from the network. See the online article for the color version of this figure.
Discussion
The present study aimed to characterize the relationships among the elements of the vicious cycle model using network analysis. Overall, the findings highlight that DTC in particular accounts for the connection of anxiety and depression with alcohol-related variables. The GLASSO network provided initial evidence for the centrality of DTC in the comorbidity network. With the network edges restricted to unique (conditionally independent) relationships, the direct associations between internalizing conditions and AUD were negligible, while DTC (and perceived stress) had strong direct relationships with these network elements. Moreover, DTC was the highest ranked network element across all centrality indices (closeness, betweenness, and strength). The reliability of this finding was further confirmed by centrality stability analyses showing that DTC retained its high centrality ranking even after dropping large proportions of nodes or cases. These findings are consistent with the vicious cycle model (Kushner, Abrams, Thuras et al., 2000) and they are also in line with previous results demonstrating that DTC is a predictor of AUD among those with an internalizing disorder and serves as a moderator of AUD treatment response among comorbid individuals (Anker et al., 2016; Armeli, O’Hara, Covault, Scott, & Tennen, 2016; Armeli, Sullivan, & Tennen, 2015; Cooper, Hildebrandt, & Gerlach, 2014; Crum, La Flair et al., 2013; Crum, Mojtabai et al., 2013; Holahan, Moos, Holahan, Cronkite, & Randall, 2003; Menary et al., 2011).
The present results also extend what is known about the vicious cycle model and previous DTC findings in several important respects. First, the findings suggest anxiety and depression are primarily linked to drinking variables indirectly through their mutual connection to DTC. Second, the work shows that removing the influence of DTC, but not other elements of the model, eliminates the connectivity between internalizing and AUD elements. These findings are consistent with our earlier clinical work showing that the incorporation of treatment elements meant to reduce DTC improved AUD outcomes in comorbid patients relative to a treatment that focused exclusively on anxiety reduction (Kushner et al., 2013). This finding also provides a possible explanation as to why reducing distress-related conditions in comorbid AUD patients fails to meaningfully decrease relapse risk (Hobbs et al., 2011); that is, because DTC is left to maintain or reinitiate the vicious cycle.
The findings also showed that subjective stress plays an important role in comorbidity that is partially independent of specific anxiety and depression levels (i.e., stress was more strongly related to alcohol variables than were either anxiety or depression in the GLASSO network). Removal of the effects of stress from the association network substantially reduced the association between the distress-related elements (general anxiety and depression) with DTC. These findings are consistent with previous work suggesting that anxiety and depression are associated with alcohol use indirectly through a cascade of intermediary effects related to high levels of perceived stress and DTC (Armeli et al., 2016, 2015; Cooper et al., 1992; Peirce et al., 1994; Wills & Hirky, 1996). Additionally, these findings portend that significant stress (e.g., from poverty, crime, divorce) not directly associated with anxiety or depressive disorders might well be sufficient to drive the vicious cycle. In other words, DTC may also be an important impetus to pathological drinking among those who experience high chronic stress in the absence of clinical levels of anxiety or depression.
Finally, the stability of network structures for men and women in this study were somewhat surprising given past findings. For example, several studies note the presence of gender differences in the prevalence of comorbidity in AUD and that men and women show differential effects of anxiety/depression on the course and severity of AUD (Schneider et al., 2001). Moreover, previous findings indicate that women are more likely to use alcohol to self-medicate stress (Rice & Van Arsdale, 2010; Timko, Finney, & Moos, 2005) and to drink in response to negative affect states characterized by anxiety and depression (Karpyak et al., 2016). In spite of these gender differences results in the present study indicated a marked level of consistency between men and women in terms of overall network structure and centrality values. Namely, in line with the primary results, DTC was a central element in both the association and GLASSO networks. Furthermore, regardless of gender, DTC was the only network probe that resulted in the isolation of the drinking-related elements. This suggests that while DTC may be more prevalent among women than men, its bivariate and multivariate relationships with comorbid anxiety/depression and AUD is similar for both men and women. This conclusion is consistent with our earlier findings showing both men and women benefited from a treatment specifically targeting DTC tendencies (Kushner et al., 2013) and that gender does not affect the importance of DTC in moderating this treatment effect (Anker et al., 2016).
Limitations
Findings from the present study should be interpreted in the context of its limitations. First, as noted in the Method section, we did not have prospective data on several key variables in the RCT that generated this data set; thus, causal relationships between variables represented in the networks and simulations cannot be inferred (Pearl, 2000; Rubin, 2011). It is important to note that the model simulations were not intended to reveal causal relationships, but rather to quantify the importance of network elements that are commonly targeted in treatment as a means of generating hypotheses about both the nature of comorbidity and the development of real-world targeted therapies for comorbid patients. Future work in this area should seek to test these hypotheses over multiple time points of the recovery process before as well as after treatments to establish whether the present simulation results can be confirmed as causal.
Second, our selection of variables, measures, and level of analysis (i.e., behavioral/symptom aggregates vs. individual symptoms) was guided by our theoretical and clinical conceptualization of the vicious cycle model (Kushner, Abrams, & Borchardt, 2000). Factors such as alcohol use expectancies, measures of impulsivity/sensation seeking, and distress tolerance, to name but a few, have also been found to influence in drinking decisions (Boschloo et al., 2013; Brière, Rohde, Seeley, Klein, & Lewinsohn, 2014; Kushner, Abrams, Thuras et al., 2000; Pacek et al., 2013) but were outside of the scope of the present investigation. Similarly, our approach to measuring DTC using the negative emotion subscale of the Inventory of Drinking Situations may have affected our results. Although this scale was not made with diagnostic comorbidity in mind, a review of the items (see supplemental materials) raises the possibility that they represent more distress-related than fear-related situations. To the extent that this was the case, fear-related internalizing measures (i.e., panic, social fears and agoraphobia) might have been less fully represented in network relations with DTC than were distress-related internalizing measures (i.e., generalized anxiety, depression, and stress). It is, however, important to note that the wording of the DTC scales was sufficiently distinct from wording of the alcohol-related measures, perceived stress scale, and internalizing measures; thus, DTC’s relationships within the network were not likely due purely to shared measurement variance. Future research could more fully mitigate this concern by employing a DTC measurement approach that represents distress and fear internalizing elements more equally. Finally, our decision to represent network elements at the construct/aggregate level as opposed to the symptom level (as is more common in the extant network analysis work in psychopathology to date) reflected our goal of representing the clinical and theoretical constructs of the vicious cycle model at the same theoretical and clinical level used in the model’s development and application. With that said, we have little doubt that symptom-level networks of comorbidity elements would produce unique and potentially important findings.
Third, our sample was restricted to patients being treated primarily for AUD with one or more current anxiety disorders (panic, generalized anxiety, and/or social anxiety). While this characteristic of the sample is representative of a large proportion of the AUD patient population entering treatment (estimated to be as high as 50%; Kushner et al., 2005), it remains unknown whether results would generalize to patients receiving treatment primarily for drug dependence (e.g., opioids or stimulants) or who endorsed different current or lifetime internalizing disorders. Extending findings from the present study to a range of comorbidity types and accounting for lifetime histories of mental health disorders could evaluate whether DTC is important in maintaining not just associations between AUD and anxiety or depression but associations between other substance dependencies and comorbid mental health disorders.
Fourth, the drinking behavior measure (total number of drinks consumed) referenced the 4 months leading to treatment while all other measures referenced the 30 days prior to treatment entry. We chose a 4-month window to assess alcohol use because drinking patterns immediately preceding treatment are typically not representative of the “typical” day-to-day drinking patterns that led to treatment (Stasiewicz et al., 2013). However, this design feature could have introduced ambiguity in the temporal priority between internalizing manifestations and alcohol use. In this regard, it is important to note that our research agenda was not related to establishing temporal order between these variables. The vicious cycle model that inspired the work minimizes the importance of temporal order in comorbid conditions, as the conditions are understood to ultimately reinforce one another in a self-sustaining cycle such that temporal priority of one element over the other is seen as largely arbitrary.
Conclusion
Visual representation of comorbid conditions as interconnected networks of clinical and theory-relevant variables, along with simulations of the network when elements are removed, provides a novel perspective on comorbidity. First, the work showed that DTC was necessary (i.e., served as a “keystone”) to maintaining the correlational connectivity of both internalizing problems and stress with alcohol use. This was shown both through the GLASSO network in which DTC was the most central element and through the model simulations in which controlling for DTC, and only for DTC, eliminated the comorbid associations. A second noteworthy finding was that the importance of perceived stress within the comorbidity network was partially independent of internalizing problems. Because stress-alcohol research has generally proceeded independently of psychiatric comorbidity research (Anthenelli & Grandison, 2012), this work is among the few studies that have examined stress, anxiety, and depression levels in a unified framework. Finally, these findings inform clinical hypotheses for interventions targeting DTC to eliminate the connection between comorbid internalizing and drinking-related elements.
Supplementary Material
General Scientific Summary.
In the present study, we use an innovative statistical approach (network analysis) to identify drinking to cope with negative affect as a keystone feature of co-occurring internalizing (anxiety and/or depression) and alcohol use disorders.
Acknowledgments
This work was supported by grant, R01-AA015069 awarded by NIAAA to the Matt G. Kushner and training Grant T32-DA037183 awarded by NIDA to support the work of the Justin J. Anker and Miriam K. Forbes.
Footnotes
Supplemental materials: http://dx.doi.org/10.1037/abn0000257.supp
Contributor Information
Justin J. Anker, Department of Psychiatry, University of Minnesota
Miriam K. Forbes, Department of Psychiatry, University of Minnesota
Zack W. Almquist, Department of Sociology and School of Statistics, University of Minnesota
Jeremiah S. Menk, Biostatistical Design and Analysis Center, Clinical and Translational Science Institute, University of Minnesota
Paul Thuras, Medical Center, University of Minnesota.
Amanda S. Unruh, Department of Psychiatry, University of Minnesota
Matt G. Kushner, Department of Psychiatry, University of Minnesota
References
- Altemus M, Sarvaiya N, Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Frontiers in Neuroendocrinology. 2014;35:320–330. doi: 10.1016/j.yfrne.2014.05.004. http://dx.doi.org/10.1016/j.yfrne.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anker JJ, Kushner MG, Thuras P, Menk J, Unruh AS. Drinking to cope with negative emotions moderates alcohol use disorder treatment response in patients with co-occurring anxiety disorder. Drug and Alcohol Dependence. 2016;159:93–100. doi: 10.1016/j.drugalcdep.2015.11.031. http://dx.doi.org/10.1016/j.drugalcdep.2015.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annis H. Inventory of drinking situations. Toronto, Ontario, Canada: Addiction Research Foundation; 1982. [Google Scholar]
- Annis H. Situational Confidence Questionnaire. Toronto, Ontario, Canada: Addiction Research Foundation; 1988. [Google Scholar]
- Anthenelli R, Grandison L. Effects of stress on alcohol consumption. Alcohol Research: Current Reviews. 2012;34:381–382. [PMC free article] [PubMed] [Google Scholar]
- Anton RF, Moak DH, Latham P. The Obsessive Compulsive Drinking Scale: A self-rated instrument for the quantification of thoughts about alcohol and drinking behavior. Alcoholism, Clinical and Experimental Research. 1995;19:92–99. doi: 10.1111/j.1530-0277.1995.tb01475.x. http://dx.doi.org/10.llll/j.15300277.1995.tb01475.x. [DOI] [PubMed] [Google Scholar]
- Armeli S, O’Hara RE, Covault J, Scott DM, Tennen H. Episode-specific drinking-to-cope motivation and next-day stress-reactivity. Anxiety, Stress, and Coping. 2016;29:673–684. doi: 10.1080/10615806.2015.1134787. http://dx.doi.org/10.1080/10615806.2015.1134787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armeli S, Sullivan TP, Tennen H. Drinking to cope motivation as a prospective predictor of negative affect. Journal of Studies on Alcohol and Drugs. 2015;76:578–584. doi: 10.15288/jsad.2015.76.578. http://dx.doi.org/10.15288/jsad.2015.76.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF. The classification of alcoholics: Typology theories from the 19th century to the present. Alcohol Research & Health. 1996;20:1. [PMC free article] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Bhadeshia H. Neural networks in materials science. ISIJ International. 1999;39:966–979. http://dx.doi.org/10.2355/isijintemational.39.966. [Google Scholar]
- Black JJ, Tran GQ, Goldsmith AA, Thompson RD, Smith JP, Welge JA. Alcohol expectancies and social self-efficacy as mediators of differential intervention outcomes for college hazardous drinkers with social anxiety. Addictive Behaviors. 2012;37:248–255. doi: 10.1016/j.addbeh.2011.10.004. http://dx.doi.org/10.1016/j.addbeh.2011.10.004. [DOI] [PubMed] [Google Scholar]
- Book SW, Thomas SE, Randall PK, Randall CL. Paroxetine reduces social anxiety in individuals with a co-occurring alcohol use disorder. Journal of Anxiety Disorders. 2008;22:310–318. doi: 10.1016/j.janxdis.2007.03.001. http://dx.doi.org/10.1016/j.janxdis.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borgatti SP, Mehra A, Brass DJ, Labianca G. Network analysis in the social sciences. Science. 2009;323:892–895. doi: 10.1126/science.1165821. http://dx.doi.org/10.1126/science.1165821. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AO. Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. http://dx.doi.org/10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Boschloo L, Vogelzangs N, van den Brink W, Smit JH, Beekman AT, Penninx BW. The role of negative emotionality and impulsivity in depressive/anxiety disorders and alcohol dependence. Psychological Medicine. 2013;43:1241–1253. doi: 10.1017/S0033291712002152. http://dx.doi.org/10.1017/S0033291712002152. [DOI] [PubMed] [Google Scholar]
- Brière FN, Rohde P, Seeley JR, Klein D, Lewinsohn PM. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Comprehensive Psychiatry. 2014;55:526–533. doi: 10.1016/j.comppsych.2013.10.007. http://dx.doi.org/10.1016/j.comppsych.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cannon DS, Leeka JK, Patterson ET, Baker TB. Principal components analysis of the inventory of drinking situations: Empirical categories of drinking by alcoholics. Addictive Behaviors. 1990;15:265–269. doi: 10.1016/0306-4603(90)90069-a. http://dx.doi.org/10.1016/0306-4603(90)90069-A. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Caputo GC, Jasin SE, Gracely EJ, Williams C. The mobility inventory for agoraphobia. Behaviour Research and Therapy. 1985;23:35–44. doi: 10.1016/0005-7967(85)90140-8. http://dx.doi.org/10.1016/0005-7967(85)90140-8. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. http://dx.doi.org/10.2307/2136404. [PubMed] [Google Scholar]
- Conger JJ. Alcoholism: Theory, problem and challenge. II. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, Mudar P. Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology. 1992;101:139–152. doi: 10.1037//0021-843x.101.1.139. http://dx.doi.org/10.1037/0021-843X.101.1.139. [DOI] [PubMed] [Google Scholar]
- Cooper R, Hildebrandt S, Gerlach AL. Drinking motives in alcohol use disorder patients with and without social anxiety disorder. Anxiety, Stress, and Coping. 2014;27:113–122. doi: 10.1080/10615806.2013.823482. http://dx.doi.org/10.1080/10615806.2013.823482. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Salloum IM, Ehler JG, Jarrett PJ, Cornelius MD, Perei JM, Black A. Fluoxetine in depressed alcoholics. A double-blind, placebo-controlled trial. Archives of General Psychiatry. 1997;54:700–705. doi: 10.1001/archpsyc.1997.01830200024004. http://dx.doi.org/10.1001/archpsyc.1997.01830200024004. [DOI] [PubMed] [Google Scholar]
- Costantini G, Epskamp S, Borsboom D, Perugini M, Mottus R, Waldorp L, Cramer A. State of the art personality research: A tutorial on network analysis of personality data in R. Journal of Research in Personality. 2015;54:13–29. http://dx.doi.org/10.1016/jjrp.2014.07.003. [Google Scholar]
- Costantini G, Perugini M. The definition of components and the use of formal indexes are key steps for a successful application of network analysis in personality psychology. European Journal of Personality. 2012;26:434–435. http://dx.doi.org/10.1002/per.1869. [Google Scholar]
- Cramer AO, Waldorp LJ, van der Maas HL, Borsboom D. Comorbidity: A network perspective. Behavioral and Brain Sciences. 2010;33:137–150. doi: 10.1017/S0140525X09991567. http://dx.doi.org/10.1017/S0140525X09991567. [DOI] [PubMed] [Google Scholar]
- Crum RM, La Flair L, Storr CL, Green KM, Stuart EA, Alvanzo AA, Mojtabai R. Reports of drinking to self-medicate anxiety symptoms: Longitudinal assessment for subgroups of individuals with alcohol dependence. Depression and Anxiety. 2013;30:174–183. doi: 10.1002/da.22024. http://dx.doi.org/10.1002/da.22024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum RM, Mojtabai R, Lazareck S, Bolton JM, Robinson J, Sareen J, Storr CL. A prospective assessment of reports of drinking to self-medicate mood symptoms with the incidence and persistence of alcohol dependence. Journal of the American Medical Association Psychiatry. 2013;70:718–726. doi: 10.1001/jamapsychiatry.2013.1098. http://dx.doi.org/10.1001/jamapsychiatry.2013.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csardi G, Nepusz T. The igraph software package for complex network research. Interjournal, Complex Systems. 2006;1695 [Google Scholar]
- De Schryver M, Vindevogel S, Rasmussen AE, Cramer AO. Unpacking constructs: A network approach for studying war exposure, daily stressors and post-traumatic stress disorder. Frontiers in Psychology. 2015;6:1896. doi: 10.3389/fpsyg.2015.01896. http://dx.doi.org/10.3389/fpsyg.2015.01896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S. Bootnet: Bootstrap methods for various network estimation routines (R package version 0.2) [Computer software] 2015 Retrived from http://CRAN.R-project.org/package=bootnet.
- Epskamp S, Borsboom D, Fried E. Estimating psychological networks and their stability: A tutorial paper. 2016 doi: 10.3758/s13428-017-0862-1. Retrieved from https://www.researchgate.net/publication/301818323_Estimating_Psychological_Networks_and_their_Accuracy_a_Tutorial_Paper. [DOI] [PMC free article] [PubMed]
- Epskamp S, Cramer A, Waldorp L, Schmittmann V, Borsboom D. qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software. 2012;48:1–18. http://dx.doi.org/10.18637/jss.v048.i04. [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM–IV Axis I Disorders—Patient Edition (SCID-I/P, Version 2.0, 8/98 revision) New York, NY: Biometric Research Department; 1998. [Google Scholar]
- Frewen PA, Schmittmann VD, Bringmann LF, Borsboom D. Perceived causal relations between anxiety, posttraumatic stress and depression: Extension to moderation, mediation, and network analysis. European Journal of Psychotraumatology. 2013 doi: 10.3402/ejpt.v4i0.20656. Advance online publication. http://dx.doi.org/10.3402/ejpt.v4i0.20656. [DOI] [PMC free article] [PubMed]
- Fried EI. Problematic assumptions have slowed down depression research: Why symptoms, not syndromes are the way forward. Frontiers in Psychology. 2015;6:309. doi: 10.3389/fpsyg.2015.00309. http://dx.doi.org/10.3389/fpsyg.2015.00309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, Epskamp S, Nesse RM, Tuerlinckx F, Borsboom D. What are ‘good’ depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. Journal of Affective Disorders. 2016;189:314–320. doi: 10.1016/j.jad.2015.09.005. http://dx.doi.org/10.1016/j.jad.2015.09.005. [DOI] [PubMed] [Google Scholar]
- Friedman J, Hastie T, Tibshirani R. glasso: Graphical lasso-estimation of Gaussian graphical models (R package version 1.8) [Computer software] 2014 Retrivied from http://CRAN.R-project.org/package=glasso.
- Gillis MM, Haaga DA, Ford GT. Normative values for the Beck Anxiety Inventory, Fear Questionnaire, Penn State Worry Questionnaire, and Social Phobia and Anxiety Inventory. Psychological Assessment. 1995;7:450–455. http://dx.doi.org/10.1037/1040-3590.7.4.450. [Google Scholar]
- Goldsmith AA, Thompson RD, Black JJ, Tran GQ, Smith JP. Drinking refusal self-efficacy and tension-reduction alcohol expectancies moderating the relationship between generalized anxiety and drinking behaviors in young adult drinkers. Psychology of Addictive Behaviors. 2012;26:59–67. doi: 10.1037/a0024766. http://dx.doi.org/10.1037/a0024766. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, Michael J. The effect of depression on return to drinking: A prospective study. Archives of General Psychiatry. 1998;55:259–265. doi: 10.1001/archpsyc.55.3.259. http://dx.doi.org/10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Haver B. Comorbid psychiatric disorders predict and influence treatment outcome in female alcoholics. European Addiction Research. 2003;9:39–44. doi: 10.1159/000067735. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Mueller G, Holt CS, Hope DA, Liebowitz MR. Assessment of anxiety in social interaction and being observed by others: The Social Interaction Anxiety Scale and the Social Phobia Scale. Behavior Therapy. 1992;23:53–73. http://dx.doi.org/10.1016/S0005-7894(05)80308-9. [Google Scholar]
- Heizer JE, Pryzbeck TR. The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment. Journal of Studies on Alcohol and Drugs. 1988;49:219–224. doi: 10.15288/jsa.1988.49.219. http://dx.doi.org/10.15288/jsa.1988.49.219. [DOI] [PubMed] [Google Scholar]
- Hobbs JD, Kushner MG, Lee SS, Reardon SM, Maurer EW. Meta-analysis of supplemental treatment for depressive and anxiety disorders in patients being treated for alcohol dependence. The American Journal on Addictions. 2011;20:319–329. doi: 10.1111/j.1521-0391.2011.00140.x. http://dx.doi.org/10.1111/j.l521-0391.2011.00140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Drinking to cope and alcohol use and abuse in unipolar depression: A 10-year model. Journal of Abnormal Psychology. 2003;112:159–165. http://dx.doi.org/10.1037/0021-843X.112.L159. [PubMed] [Google Scholar]
- Hoorelbeke K, Marchetti I, De Schryver M, Koster EH. The interplay between cognitive risk and resilience factors in remitted depression: A network analysis. Journal of Affective Disorders. 2016;195:96–104. doi: 10.1016/j.jad.2016.02.001. http://dx.doi.org/10.1016/j.jad.2016.02.001. [DOI] [PubMed] [Google Scholar]
- Houck PR, Spiegel DA, Shear MK, Rucci P. Reliability of the self-report version of the Panic Disorder Severity Scale. Depression and Anxiety. 2002;15:183–185. doi: 10.1002/da.10049. http://dx.doi.org/10.1002/da.10049. [DOI] [PubMed] [Google Scholar]
- Karpyak VM, Biernacka JM, Geske JR, Abulseoud OA, Brunner MD, Chauhan M, Mrazek DA. Gender-specific effects of comorbid depression and anxiety on the propensity to drink in negative emotional states. Addiction. 2016;111:1366–1375. doi: 10.1111/add.13386. http://dx.doi.org/10.1111/add.13386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keough ME, Porter E, Kredlow MA, Worthington JJ, Hoge EA, Pollack MH, Simon NM. Anchoring the Panic Disorder Severity Scale. Assessment. 2012;19:257–259. doi: 10.1177/1073191112436668. http://dx.doi.org/10.1177/1073191112436668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. The American Journal of Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. http://dx.doi.org/10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology. 2001;24:97–129. doi: 10.1016/S0893-133X(00)00195-0. http://dx.doi.org/10.1016/S0893-133X(00)00195-0. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. http://dx.doi.org/10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Kushner MG. Seventy-five years of comorbidity research. Journal of Studies on Alcohol and Drugs. 2014;75:50–58. doi: 10.15288/jsads.2014.s17.8. http://dx.doi.org/10.15288/jsads.2014.75.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: A review of major perspectives and findings. Clinical Psychology Review. 2000;20:149–171. doi: 10.1016/s0272-7358(99)00027-6. http://dx.doi.org/10.1016/S0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Thuras P, Hanson KL, Brekke M, Sletten S. Follow-up study of anxiety disorder and alcohol dependence in comorbid alcoholism treatment patients. Alcoholism: Clinical and Experimental Research. 2005;29:1432–1443. doi: 10.1097/01.alc.0000175072.17623.f8. http://dx.doi.org/10.1097/01.alc.0000175072.17623.f8. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Thuras P, Hanson KL. Individual differences predictive of drinking to manage anxiety among non-problem drinkers with panic disorder. Alcoholism, Clinical and Experimental Research. 2000;24:448–458. http://dx.doi.org/10.1111/j.1530-0277.2000.tb02011.x. [PubMed] [Google Scholar]
- Kushner MG, Donahue C, Sletten S, Thuras P, Abrams K, Peterson J, Frye B. Cognitive behavioral treatment of comorbid anxiety disorder in alcoholism treatment patients: Presentation of a prototype program and future directions. Journal of Mental Health. 2006;15:697–707. http://dx.doi.org/10.1080/09638230600998946. [Google Scholar]
- Kushner MG, Krueger R, Frye B, Peterson J. Epidemiological perspectives on co-occurring anxiety disorder and substance use disorder. In: Stewart SH, Conrod PJ, editors. Anxiety and substance use disorders. New York, NY: Springer; 2008. pp. 3–17. [Google Scholar]
- Kushner MG, Maurer EW, Thuras P, Donahue C, Frye B, Menary KR, Van Demark J. Hybrid cognitive behavioral therapy versus relaxation training for co-occurring anxiety and alcohol disorder: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2013;81:429–442. doi: 10.1037/a0031301. http://dx.doi.org/10.1037/a0031301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Wall MM, Krueger RF, Sher KJ, Maurer E, Thuras P, Lee S. Alcohol dependence is related to overall internalizing psychopathology load rather than to particular internalizing disorders: Evidence from a national sample. Alcoholism: Clinical and Experimental Research. 2012;36:325–331. doi: 10.1111/j.1530-0277.2011.01604.x. http://dx.doi.org/10.1111/j.1530-0277.2011.01604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, Callan MK. Stress, alcohol-related expectancies and coping preferences: A replication with adolescents of the Cooper et al. (1992) model. Journal of Studies on Alcohol. 1997;58:644–651. doi: 10.15288/jsa.1997.58.644. http://dx.doi.org/10.15288/jsa.1997.58.644. [DOI] [PubMed] [Google Scholar]
- Luke DA, Harris JK. Network analysis in public health: History, methods, and applications. Annual Review of Public Health. 2007;28:69–93. doi: 10.1146/annurev.publhealth.28.021406.144132. http://dx.doi.org/10.l146/annurev.publhealth.28.021406.144132. [DOI] [PubMed] [Google Scholar]
- Marlatt GA. A cognitive-behavioral model of the relapse process. NIDA Research Monograph. 1979;25:191–200. doi: 10.1037/e497382006-015. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behaviour Research and Therapy. 1998;36:455–470. doi: 10.1016/s0005-7967(97)10031-6. http://dx.doi.org/10.1016/S0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- McNally R, Robinaugh D, Wu G, Wang L, Desemo M, Borsboom D. Mental disorders as causal systems a network approach to posttraumatic stress disorder. Clinical Psychological Science. 2015;3:836–849. http://dx.doi.org/10.1177/2167702614553230. [Google Scholar]
- Menary KR, Kushner MG, Maurer E, Thuras P. The prevalence and clinical implications of self-medication among individuals with anxiety disorders. Journal of Anxiety Disorders. 2011;25:335–339. doi: 10.1016/j.janxdis.2010.10.006. http://dx.doi.org/10.1016/j.janxdis.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. http://dx.doi.org/10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Newman M. Networks: An introduction. Oxford, UK: Oxford University Press; 2010. [Google Scholar]
- Otte E, Rousseau R. Social network analysis: A powerful strategy, also for the information sciences. Journal of Information Science. 2002;28:441–453. http://dx.doi.org/10.1177/016555150202800601. [Google Scholar]
- Pacek LR, Storr CL, Mojtabai R, Green KLA, Flair LN, Alvanzo AA, Crum RM. Comorbid Alcohol Dependence and Anxiety Disorders: A National Survey. Journal of Dual Diagnosis. 2013;9:271–280. doi: 10.1080/15504263.2013.835164. http://dx.doi.org/10.1080/15504263.2013.835164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl J. The art and science of cause and effect. Causality: Models, reasoning and inference. Cambridge, UK: University of Cambridge; 2000. [Google Scholar]
- Pedersen ER, LaBrie JW. A within-subjects validation of a group-administered timeline followback for alcohol use. Journal of Studies on Alcohol. 2006;67:332–335. doi: 10.15288/jsa.2006.67.332. http://dx.doi.org/10.15288/jsa.2006.67.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirce RS, Frone MR, Russell M, Cooper ML. Relationship of financial strain and psychosocial resources to alcohol use and abuse: The mediating role of negative affect and drinking motives. Journal of Health and Social Behavior. 1994;35:291–308. http://dx.doi.org/10.2307/2137211. [PubMed] [Google Scholar]
- Quitkin FM, Rifkin A, Kaplan J, Klein DF. Phobic anxiety syndrome complicated by drug dependence and addiction. A treatable form of drug abuse. Archives of General Psychiatry. 1972;27:159–162. doi: 10.1001/archpsyc.1972.01750260013002. http://dx.doi.org/10.1001/archpsyc.1972.01750260013002. [DOI] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2015. Retrive from https://www.R-project.org/ [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. Journal of the American Medical Association. 1990;264:2511–2518. http://dx.doi.org/10.1001/jama.1990.03450190043026. [PubMed] [Google Scholar]
- Rhemtulla M, Fried EI, Aggen SH, Tuerlinckx F, Kendler KS, Borsboom D. Network analysis of substance abuse and dependence symptoms. Drug and Alcohol Dependence. 2016;161:230–237. doi: 10.1016/j.drugalcdep.2016.02.005. http://dx.doi.org/10.1016/j.drugalcdep.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice K, Van Arsdale A. Perfectionism, perceived stress, drinking to cope, and alcohol-related problems among college students. Journal of Counseling Psychology. 2010;57:439–450. http://dx.doi.org/10.1037/a0020221. [Google Scholar]
- Robinaugh DJ, LeBlanc NJ, Vuletich HA, McNally RJ. Network analysis of persistent complex bereavement disorder in conjugally bereaved adults. Journal of Abnormal Psychology. 2014;123:510–522. doi: 10.1037/abn0000002. http://dx.doi.org/10.1037/abn0000002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Causal inference using potential outcomes. Journal of the American Statistical Association. 2011;100:322–331. http://dx.doi.org/10.1198/016214504000001880. [Google Scholar]
- Schlegel K, Grandjean D, Scherer KR. Constructs of social and emotional effectiveness: Different labels, same content? Journal of Research in Personality. 2013;47:249. http://dx.doi.org/10.1016/j.jrp.2013.02.005. [Google Scholar]
- Schneider U, Altmann A, Baumann M, Bernzen J, Bertz B, Bimber U, Wittfoot J. Comorbid anxiety and affective disorder in alcohol-dependent patients seeking treatment: The first Multicentre Study in Germany. Alcohol and Alcoholism. 2001;36:219–223. doi: 10.1093/alcalc/36.3.219. http://dx.doi.org/10.1093/alcalc/36.3.219. [DOI] [PubMed] [Google Scholar]
- Sepilicre J, Sabuncu MR, Johnson KA. Network assemblies in the functional brain. Current Opinion in Neurology. 2012;25:384–391. doi: 10.1097/WCO.0b013e328355a8e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ. Stress response dampening. In: Blanc HT, Leonard KE, editors. Psychological theories of drinking and alcoholism. New York, NY: Guilford Press; 1987. pp. 227–271. [Google Scholar]
- Sher KJ, Levenson RW. Risk for alcoholism and individual differences in the stress-response-dampening effect of alcohol. Journal of Abnormal Psychology. 1982;91:350–367. doi: 10.1037//0021-843x.91.5.350. http://dx.doi.org/10.1037/0021-843X.91.5.350. [DOI] [PubMed] [Google Scholar]
- Simonds VM, Whiffen VE. Are gender differences in depression explained by gender differences in co-morbid anxiety? Journal of Affective Disorders. 2003;77:197–202. doi: 10.1016/s0165-0327(02)00113-1. http://dx.doi.org/10.1016/S0165-0327(02)00113-l. [DOI] [PubMed] [Google Scholar]
- Sobell L, Sobell M. Timeline followback: A technique for assessing self-reported ethanol consumption. In: Allen RZLJ, editor. Measuring alcohol consumption: Psychological and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. http://dx.doi.org/10.1007/978-1-4612-0357-5_3. [Google Scholar]
- Stasiewicz PR, Schlauch RC, Bradizza CM, Bole CW, Coffey SF. Pretreatment changes in drinking: Relationship to treatment outcomes. Psychology of Addictive Behaviors. 2013;27:1159–1166. doi: 10.1037/a0031368. http://dx.doi.org/10.1037/a0031368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timko C, Finney JW, Moos RH. The 8-year course of alcohol abuse: Gender differences in social context and coping. Alcoholism: Clinical and Experimental Research. 2005;29:612–621. doi: 10.1097/01.alc.0000158832.07705.22. http://dx.doi.org/10.1097/01.ALC.0000158832.07705.22. [DOI] [PubMed] [Google Scholar]
- Tómasson K, Vaglum P. A nationwide representative sample of treatment-seeking alcoholics: A study of psychiatric comorbidity. Acta Psychiatrica Scandinavica. 1995;92:378–385. doi: 10.1111/j.1600-0447.1995.tb09600.x. http://dx.doi.org/10.1111/j.1600-0447.1995.tb09600.x. [DOI] [PubMed] [Google Scholar]
- Wasserman S, Faust K. Social network analysis: Methods and applications. Vol. 8. New York, NY: Cambridge University Press; 1994. http://dx.doi.org/10.1017/CBO9780511815478. [Google Scholar]
- Wellman B. Computer networks as social networks. Science. 2001;293:2031–2034. doi: 10.1126/science.1065547. http://dx.doi.org/10.1126/science.1065547. [DOI] [PubMed] [Google Scholar]
- Wills TA, Hirky AE. Coping and substance abuse: A theoretical model and review of the evidence 1996 [Google Scholar]
- Zilberman ML, Tavares H, Blume SB, el-Guebaly N. Substance use disorders: Sex differences and psychiatric comorbidities. Canadian Journal of Psychiatry. 2003;48:5–13. doi: 10.1177/070674370304800103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


