Abstract
An estimated 10 million Americans age 50 and older have osteoporosis, and many experience associated fractures. Although several interventions have been shown to be effective in preventing osteoporosis, their impact on bone health among older adults was limited. The aim of this study was, therefore, to examine the effects of a theory-based online bone health program (Bone Power program) for a large number of older adults. The 8-week program included learning modules, discussion boards, and other resources. Participants (N = 866; M age = 62.5 years) were recruited online and randomized into a Bone Power or control group. At the end of the intervention, the Bone Power group showed significantly greater improvement over the control group in osteoporosis knowledge, self-efficacy/outcome expectations for calcium intake and exercise, and calcium intake and exercise behaviors. This study's findings suggest that online health programs can be effective in improving older adults’ knowledge, beliefs, and health behaviors.
Keywords: theory-based intervention, online study, bone health, physical activities, diet
Introduction
Low bone density and its associated fractures are a serious health problem among older adults (Rosen, 2014; MacLean et al., 2008; National Osteoporosis Foundation [NOF], 2014a; NOF, n.d.-c). In 2014, 10 million Americans age 50 and older had osteoporosis (8 million women and 2 million men), and 34 million had low bone mass (NOF, 2014a, b). If the current prevalence continues, by 2020, 64.4 million older adults will have osteoporosis or low bone mass. In addition, 2 million Americans experience osteoporotic fractures annually and osteoporosis is a main culprit for 0.3 million hip fractures, with debilitating consequences for older adults (NOF, 2014b).
Bone health research over the past few decades has led to several efficacious interventions that can maintain and improve bone density, including calcium and vitamin D intake, exercise, bone density screening tests, and bone active medications (Bass, Pracht, & Foulis, 2007; Kimber & Grimmer-Somers, 2008; NOF, 2013; NOF, n.d.-a,b,c). National guidelines for those interventions have been developed based on sex, age, and health conditions (see Table 1 for a summary of selected examples). Unfortunately, many older adults do not meet recommended guidelines for maintaining healthy bones (Bailey et al., 2010; Curtis et al., 2008; President's Council on Fitness, 2010). National surveys have indicated that older adults take less than the recommended amount of calcium (Mangano, Walsh, Insogna, Kenny, & Kerstetter, 2011) and that only a small proportion (6%-16%) of individuals undertake bone-strengthening exercises (President's Council on Fitness, 2010). In addition, only 8.4% to 30% (1999-2005) of adults at high risk for osteoporosis have received a bone density test (Curtis et al., 2008). Several factors can influence these low adoption rates, including a lack of knowledge about the protective effects of calcium, vitamin D, and exercise on bone density (Campbell, 2012; Miller, Jarvis, & McBean, 2006; Webb, Joseph, Yardley, & Michie, 2010). Care providers might not discuss the importance of bone density screening tests with older adults (Kleerekoper, 2013). Thus, disseminating information about interventions to optimize bone health is needed to achieve better bone health nationally.
Table 1.
Selected National Guidelines to Optimize Bone Health.
| Bone density screening recommendationsa |
|---|
| Women age 65 or older |
| Men age 70 or older |
| Persons who break a bone after age 50 |
| Women of menopausal age with risk factors |
| Postmenopausal women below age 65 with risk factors |
| Men aged 50-69 with risk factors |
| A bone density test may also be necessary if persons have any of the following: |
| An x-ray showing a break or bone loss of the spine |
| Back pain with a possible break in the spine |
| Height loss of ½ inch or more within 1 year |
| Total height loss of 1½ inches from the original height |
| Calcium and vitamin D intake recommendationsb | ||
|---|---|---|
| Women | Men | |
| Calcium intake | ||
| ≤50 years: 1,000 mg/dayc | ≤70 years: 1,000 mg/dayc | |
| ≥51 years: 1,000 mg/dayc | ≥71 years: 1,200 mg/dayc | |
| Vitamin D intake | ||
| <50 years: 400-800 IU dailyd | ||
| ≥50 years: 800-1,000 IU dailyd | ||
| Physical activity guidelines for Americanse |
|---|
| Guidelines for adults 50-64 |
| For substantial health benefits |
| At least 150 min a week of moderate intensity, or |
| 75 min a week of vigorous-intensity aerobic physical activity, or |
| An equivalent combination of moderate- and vigorous-intensity aerobic activity (aerobic activity: episodes of at least 10 min spreading throughout the week). |
| For additional and more extensive health benefits |
| Increase aerobic physical activity to 300 min a week of moderate intensity, or |
| 150 min a week of vigorous-intensity aerobic physical activity, or |
| An equivalent combination of moderate- and vigorous-intensity activity |
| Include muscle-strengthening activities that are moderate or high intensity and involve all major muscle groups on 2 or more days a week |
| Physical activity guidelines for Americanse |
|---|
| Guidelines for adults 65 and older |
| The key guidelines for adults also apply to older adults. In addition, the following guidelines are specific to older adults: |
| When older adults cannot do 150 min of moderate-intensity aerobic activity a week because of chronic conditions, be as physically active as their abilities and conditions allow. |
| Do exercises that maintain or improve balance if at risk of falling. |
| Determine the level of effort for physical activity relative to the level of fitness. |
| Know whether and how chronic conditions affect the ability to do regular physical activity safely. |
Note. IU = international units.
National Osteoporosis Foundation (http://nof.org/articles/743).
National Osteoporosis Foundation (http://nof.org/calcium#CALCIUM).
Total amount of calcium from food and supplements.
Some people need more vitamin D (both women and men). The safe upper limit is 4,000 IU/day for most adults.
United States Department of Health and Human Services (http://www.health.gov/paguidelines/guidelines/summary.aspx).
Simply having knowledge is insufficient to motivate individuals to change behaviors. Thus, in our study, “dissemination” emphasizes strategic mechanisms that package and deliver health interventions to specific target populations to make positive changes in their health behaviors (Brownson, Colditz, & Proctor, 2012). A growing body of knowledge suggests the effectiveness of behavioral change theory–based interventions in health-promotion studies (American College of Sports Medicine, 2004; Bandura, 1998; Webb et al., 2010). The aim of this study, therefore, was to test the effects of an online theory-based bone health program (Bone Power) on health-related outcomes of older adults. It was hypothesized that at the end of the 8-week intervention period, the Bone Power group would show significantly greater improvement than the control group in knowledge of calcium intake and exercise, self-efficacy, and outcome expectations for calcium intake and exercise, and health behaviors of calcium intake, and amount of exercise.
Research on Online Health Interventions in Older Adults
In the current digital era, the Internet has become an effective vehicle for dissemination efforts (World Health Organization [WHO], 2012). In 2014, 89% of American adults were Internet users (Pew Internet, 2014). Although older adults are late adopters, their rates of Internet use has grown rapidly, reaching 79% of adults aged 55 to 65 and 57% of adults aged 65+ (Aron Smith, 2014). The majority (72%) of Internet users look for health information online (Fox & Duggan, 2013), and the Internet has also been used to deliver health interventions. Prior findings have shown that those interventions have a positive impact on health promotion (Desroches et al., 2013; Murphy et al., 2013; Schweier et al., 2014) and management of health conditions (Murphy et al., 2013; Ramadas, Quek, Chan, & Oldenburg, 2011; Schweier et al., 2014). Upon a review of 85 published articles, Webb et al. (2010) reported significant effects of online interventions on health behavior change and the importance of using theory-based interventions.
Although fewer online studies have focused on older adults than on other age groups, there is growing evidence that using online approaches to reach out to older adults can be effective in promoting healthy behaviors in this population. Irvine and his colleagues conducted a randomized controlled trial (RCT) that assessed the impact of an online physical activity program on sedentary older adults (n = 368; M age = 60.3). The program included 11 consecutive weekly sessions, and the intervention group participants significantly improved physical activity levels compared with the control group (Irvine, Gelatt, Seeley, Macfarlane, & Gau, 2013). In another study (n = 245; M age = 69.3), researchers tested the effects of a 2-week self-efficacy-based online hip fracture prevention program comprised of learning modules and discussion boards. Upon completion of the intervention, participants showed improvement on most selected health outcomes associated with calcium intake and exercise (Nahm et al., 2010). Other investigators also assessed the impact of a social cognitive theory (SCT)–based online health-promotion program among older workers (n = 278; age = 50-59, 69%; Cook, Hersch, Schlossberg, & Leaf, 2015). The program was a media-rich (e.g., videos and pictures) website that included learning content on major health topics, including healthy aging, diet, and physical activity. Findings showed that the intervention group participants performed significantly better than the control group on diet behavioral self-efficacy, healthy eating planning, and exercise at a 3-month follow-up.
Despite the increasing use of online health interventions among older adults, there is a lack of evidence that shows the impact of online health interventions on improving bone health in this population. Thus, in an effort to fill the gap, we developed a theory-based online Bone Power program specifically designed for older adults to improve their bone health knowledge, belief, and behaviors.
Theoretical Framework
The study was guided by SCT that emphasizes the importance of social and cognitive processes in changing people's behaviors (Bandura, 1997a, 1997b, 1998) (Table 2). Based on SCT, motivation is a key factor for behavior change, and setting goals is the first step. In addition, individuals’ beliefs about their ability to perform (self-efficacy) and the consequences of (outcome expectations) planned behaviors are vital to the process. Specifically, four mechanisms can enhance a person's efficacy expectations: (a) successful performance of the behavior (mastery experience), (b) social (verbal) persuasion, (c) modeling others’ successful performances (vicarious experiences), and (d) relief of physiological and emotional distress (Bandura, 1997a, 1997b, 1998).
Table 2.
Application of SCT in the Trial.
| SCT component | Application |
|---|---|
| Goal setting | Discuss the importance of goal setting; encourage participants to set health goals and provide a mechanism for follow-up (e.g., use of the Goal Attainment Scale [Kloseck, 2007]). |
| Motivation | Use a motivational tone throughout all intervention components (e.g., video clips of peers' successful performance, moderators' encouraging comments, peers' success stories in newsletters). |
| Outcome expectations | Explain and emphasize the expected outcomes of health behaviors. |
| Self-efficacy | |
| Mastery experience | Promote mastery experiences via interactive quizzes (for web learning), discussion forums (e.g., participants were reminded to think about what they have had accomplished and asked to explain those experiences), and tracking health goal progress. |
| Vicarious experiences | Demonstrate social modeling via video clips or animated pictures in learning modules and via discussion boards (e.g., participants, who overcome barriers for their healthy behaviors, can share their stories and inspire others to start healthy behaviors). |
| Social (verbal) persuasion | Provide encouragement via audio/video clips and discussion boards (e.g., “wow, you are doing great!”). |
| Physiological and emotional states | Provide information and facilitate discussions about the affective benefits of health behaviors and methods that relieve the unpleasant sensations associated with behavior change (e.g., potential fatigue or pain related to exercise). |
Note. SCT = social cognitive theory.
Application of SCT to the Bone Power program was achieved by using learning modules and a discussion board (Nahm et al., 2015). The learning modules provided information about evidence-based interventions for bone health, such as calcium and vitamin D intake, exercise, and bone density screening tests. They explained the expected outcomes from those behaviors. Discussion forums focused on health behaviors accompanied the learning modules and were moderated by a nurse. To facilitate mastery experiences, in the modules, participants were encouraged to set goals for their bone health (e.g., exercise, calcium take) and keep track of them. On the accompanying discussion forum, they were asked specific follow-up questions about their health behaviors (e.g., “Let's discuss exercise. Please think about how you kept up with your exercise schedule and explain it to us.”). For vicarious experiences or role modeling, the modules included video clips of people or animated pictures that demonstrated competent behaviors. Discussion forums encouraged participants to share success stories and serve as role models for others. Verbal persuasion was provided by using encouraging words on discussion boards, modules, and video clips. To minimize physiological and emotional stress, the modules and the discussion forum comments included specific techniques to decrease unpleasant sensations associated with behaviors (e.g., possible pain associated with exercise).
Method
Design and Participants
The Bone Power study was a two-arm parallel-group RCT comparing the Bone Power group with the no-intervention control group. This was Phase I of a large online longitudinal trial comparing the impact of the two different online bone health interventions. (In Phase II, the intervention group split into Bone Power and Bone Power Plus [with additional 10-month booster intervention] groups.) The study was approved by the institutional review boards at the University of Maryland, Baltimore and the U.S. Department of Veterans Affairs.
Individuals were eligible if they were aged 50 or older, had access to the Internet/email, could use the Internet/email independently, were able to read and write English, and resided in a community setting the United States. Individuals were excluded if they were participating in any study on falls, osteoporosis, or nutrition. Participants were recruited from two online communities, SeniorNet (seniornet.org), and My HealtheVet (MHV) (myhealth.va.gov; 11/30/2010-7/9/2011). SeniorNet is a leading older adult online community with a large nationwide membership. It provides adults with health education and computer training. MHV is a national health web portal for veterans. The two sites serve a large number of older adults, and our investigators had collaborated with them previously.
A brief description of this study and a hyperlink to the study website were posted on SeniorNet and MHV. The study was also advertised via monthly eNewsletters. Individuals who were interested in the study completed the interactive eligibility criteria form on the study website. Only those who met all inclusion criteria could proceed to the online consent form. At the end of the consent process, the participant filled out the contact information form and the project manager contacted the person within 72 hr via phone to provide more detailed information about the study. The telephone follow-ups also served as a mechanism to validate the demographic information and the cognitive status (e.g., ability to understand the study procedures) of the participant. Upon the follow-up phone call, the participant was placed on a waiting list until approximately 60 participants (a team) were recruited. Once a team was filled, participants completed the baseline survey (1 week) and the participants’ study IDs were provided to the statistician, who performed randomization using a statistical program (SAS Institute Inc., n.d.). Participants were assigned to blocks of two within two recruitment sites, and the members of each block were randomly assigned to one of the three study conditions (Bone Power, Bone Power Plus, or Control). In Phase I, both intervention groups received the 8-week Bone Power program; thus, they were combined into an intervention group.
Bone Power Program
The Bone Power program consisted of learning modules, moderated discussion boards, and additional resources, such as virtual and video lecture libraries, an Ask-the-Experts section, and a health toolkit. A total of 11 learning modules were grouped into the following three categories (Table 3): bone health core modules (Modules 1-5), condition-specific bone health modules (Modules 6-8), and general health behavior modules (Modules 9-11). The third category was included because it can directly impact bone health. Each module contained specific learning objectives, structured learning content along with external links to other websites for further information, and self-assessment quizzes. The program had eight asynchronous discussion forums that accompanied learning modules for the week. The virtual libraries included additional relevant articles, health websites recommended by experts, and video lectures on specific topics. The toolkit contained various online health tools, such as the Fracture Risk Assessment Tool (FRAX®; WHO Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, UK, n.d.) and interactive health trackers (U.S. Department Agriculture, n.d.). The program also had an Ask-the-Experts function that allowed participants to submit their questions. Answers were provided by an expert panel comprised of a nurse practitioner, physician, social worker, and activity expert.
Table 3.
Learning Modules and Topics.
| Modules | Subtopics | |
|---|---|---|
| Bone health core modules | ||
| Week1 | M1: Osteoporosis: overview | Bone Health: Screening; Diagnosis; Prevention; |
| Week1 | M2: Importance of bone health | Confidence and Adherence to Healthy Bone Behaviors; Barriers |
| Starting an Exercise Program; Resources | ||
| Week2 | M3: Calcium and vitamin D | a. Calcium: General Health (Healthy diet); Calcium; Lactose Intolerance; Recipes for Calcium-Rich Dishes |
| b. Vitamin D: Role of Vitamin D; Physiology of Vitamin D; Recommended daily Vitamin D; Groups as Risk; Vitamin D and Healthy Diets | ||
| Week3 | M4: Falls | Introduction; Fall Outcomes; Fall Prevention; Home Safety; If You Fall; Assistive Devices |
| Week4 | M5: Physical activity and exercise | Importance of Exercise; Exercise and Bone Health; Exercise 101; Goal Setting/Motivation; Getting Started; Resources |
| Condition-specific bone health modules | ||
| Week5 | M6: Osteoporosis management | Who should be Considered for Drug Therapy; Food and Drug Administration (FDA)-Approved Drugs for Osteoporosis; Breast Cancer and Osteoporosis; Medicines and Osteoporosis Risk; Goal of Treatment |
| Week5 | M7: Medicine safety | Introduction to Medicine Safety; Guidelines for Taking Medicines Safely; Buying Prescriptions Online; Drug Disposal; Resources |
| Week6 | M8: Fractures | General Fracture Facts; Hip Fracture; Spinal Fracture; Wrist Fracture; Rib Fracture |
| General health-promotion modules | ||
| Week 7 | M9: Balanced diet | Servings and Portions; Food Groups; Foods to Encourage; Foods to Limit Calories; Nutrition Facts Label; BMI; Healthy Diet Resources |
| Week 8 | M10: Smoking | a. Effects of Smoking (all participants): Introduction; Harmful Effects |
| b. To Quit Smoking (smokers preparing to quit): Preparing to Quit; Quitting; Withdrawal; Self-Management; Resources | ||
| Week 8 | M11: Drinking | a. Effects of Drinking (for all participants); Introduction; Alcohol and Bone Health; Resources |
| b. To Quit Drinking (drinkers preparing to quit): Drinking Cessation/Moderation; Resources | ||
Note. BMI = body mass index.
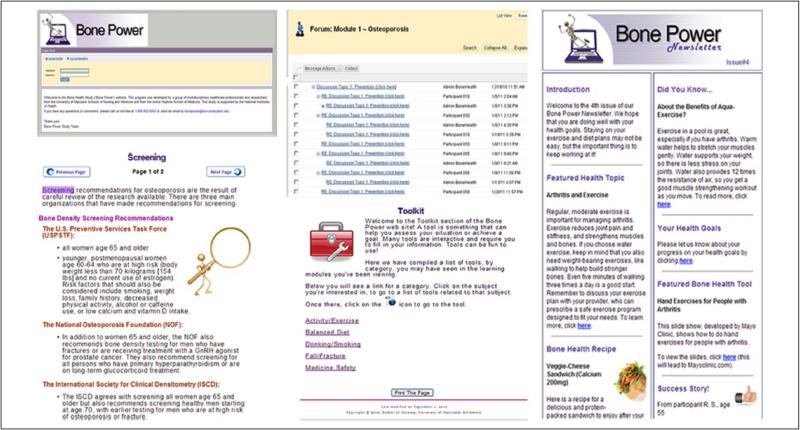
The password-protected intervention website was developed by the University of Maryland School of Nursing Research Web development team (Figure 1). Web pages were developed to be older adult-friendly following the National Institute on Aging web design guidelines (National Institute on Aging, 2009). The Blackboard (BB) program (Blackboard Inc., 2013) was used as an upper layer of the web architecture to help manage the 48 study groups. The original BB web pages were modified to simulate regular web pages. The Bone Power program had a short instructional video about how to use the program, and a help desk was available via phone and email.
Figure 1.
Selected screen shots of the Bone Power Program.
Procedures
A new learning module(s) and an accompanying discussion forum were opened on the Bone Power website weekly for 8 weeks. Participants were to visit the Bone Power website at least weekly for about 15 to 20 min to review the new learning module(s) and share their experiences and thoughts in the moderated discussion boards. The nurse project manager moderated the discussions based on SCT, offering encouraging comments to participants and inviting others’ comments. She also monitored discussion postings daily to identify any untoward postings. Participants could further explore health information by using the Virtual Libraries or the Ask-the-Experts sections as needed.
No specific intervention was provided to the control group. All participants completed an online follow-up survey at the end of 8 weeks. To maintain contact with participants, an email with information about upcoming follow-up surveys was sent to them monthly. In appreciation of participants’ time, an incentive of US $20 (check) was mailed to them upon completion of the 8-week survey.
Measures
The following demographics and descriptive data were collected at baseline: age, sex, education, health conditions (e.g., osteoporosis, chronic and acute illnesses, prior falls, fractures), and Internet experience. The participants’ eHealth literacy was also assessed using the eHealth Literacy Scale (eHEALS), an 8-item measure on a 10-point Likert-type scale (Norman & Skinner, 2006).
Osteoporosis knowledge
Knowledge about osteoporosis was measured using the revised Osteoporosis Knowledge Test (Qi, Resnick, & Nahm, 2014), which includes a total of 26 items focused on knowledge about exercise, calcium, and vitamin D intake. There was sufficient evidence for the internal consistency reliability (α = .81) in the presented study, and the validity of the measure had been supported using Rasch analysis (Qi et al., 2014).
Self-efficacy and outcome expectations
Calcium intake self-efficacy was assessed using the 11-item Self-Efficacy subscale of the Osteoporosis Health Belief Scale (Kim, Horan, Gendler, & Patel, 1991). Prior use of the measure supported its sensitivity to change (Nahm et al., 2010) and criterion-related validity (Wallace, 2002). The calculated alpha in this study was .94. Exercise self-efficacy was assessed using the nine-item Self-Efficacy for Exercise scale on an 11-point scale (0 = “no confidence”; 10 = “very confident”; Resnick & Jenkins, 2000). In this study, the calculated alpha coefficient was .93, and appropriate validity coefficients (≥.81) of the measure were also reported when used with older adults (Resnick & Jenkins, 2000).
The six-item Calcium Benefit subscale (1 = “strongly disagree”; 5 = “strongly agree”) of the Osteoporosis Health Belief Scale (Kim et al., 1991) was used to assess outcome expectations for calcium intake. Internal consistency (α = .82; Nahm et al., 2010) and criterion validity (Kim, Horan, Gendler, & Patel, 2003) of the measure have been reported. Outcome expectations associated with exercise were assessed using the Outcome Expectations for Exercise Scale (Resnick, Zimmerman, Orwig, Furstenberg, & Magaziner, 2001). This nine-item measure focuses on the perceived consequences of exercise. The calculated alpha in this study was .93, and the validity of the measure was evidenced by the confirmatory factor analysis (Resnick et al., 2006).
Calcium intake and exercise
Dietary calcium intake was estimated using a short screening tool developed by Blalock, Norton, Patel, Cabral, and Thomas (2003). It includes 22 items that assess both frequency (9-point scale: “never” to “every day”) and portions (3-point scale: “small,” “medium,” and “large”) of various foods that contain calcium and vitamin D. The amount of dietary calcium and vitamin D intake was calculated using the Diet History Questionnaire database developed by the National Cancer Institute (2008). Evidence of concurrent validity of the measure was reported using estimates of calcium intakes derived from the 7-day food diary (Blalock et al., 2003). The online version of the measure used in our prior study was sufficiently sensitive to detect changes over time (Nahm et al., 2010).
Exercise behavior was assessed using a six-item exercise subscale that is part of the Yale Physical Activity Survey (Dipietro, Caspersen, Ostfeld, & Nadel, 1993). Participants reported the type and amount of time they engaged in specific exercise activities, such as walking briskly or aerobics, and then a weekly energy expenditure (Kcal) and time (minutes) spent for exercise was estimated. The measure has been validated against several physiological variables (Dipietro et al., 1993) and was successfully used in our prior online study (Nahm et al., 2010).
Fidelity Monitoring of the Intervention
Participants’ use of the learning modules and discussion board (the main components of the program) was monitored weekly via the usage reports generated from BB. Monitoring was performed per module and per group because new modules and discussion forums were opened weekly and groups were on different study schedules. Usage of modules and discussion forums was based on the frequency of visits (captured by logins) to each component. The frequency of postings in the discussion forums was assessed separately, as posting responses could be considered a more “active” form of participation than simply reading responses. More frequent usage was expected for the core modules (Weeks 1-4) than for the condition-specific and general modules (Weeks 5-8), as some modules (e.g., Quit Smoking) might not have been applicable to all participants. In addition to the usage, perceived usability of the program was assessed via the Perceived Health Web Site Usability Questionnaire that includes 12 items on a 7-point Likert-type scale (Nahm, Resnick, & Mills, 2006).
Data Analysis
Descriptive statistics were computed on each variable to assess normality and to ensure analysis model assumptions were met. Transformations were used for continuous outcome variables to correct skewness. We examined baseline differences between the intervention and control groups in demographic characteristics, health conditions, and baseline outcome scores using t tests for continuous variables and chi-square tests for categorical variables.
In the primary analysis, to compare the Bone Power group with the control group on outcomes, we used linear mixed models (LMMs). LMMs allow inclusion of all data, even if an individual drops out and is not assessed post-treatment, and therefore is an intent-to-treat analysis. Furthermore, outcome assessments were attempted even when an individual did not complete all modules. For each outcome, LMMs included a random intercept to account for baseline heterogeneity and correlation between the baseline and post-treatment outcome measurements. The fixed effects included a time indicator variable (post-treatment vs. baseline) and the group-by-time interaction term. The significance of the group-by-time interaction tests whether the change (baseline to 8 weeks) differs between Bone Power and control conditions. Because of randomization of participants to the groups, the model did not assume outcome differences at baseline between groups, and thus no main effect group indicator was included in the mean model (Fitzmaurice, Laird, & Ware, 2011). We used empirical “sandwich” standard errors (SEs) due to their robustness properties. Within group effect sizes were calculated as the model-based difference of the outcome from baseline to 8 weeks, divided by baseline standard deviation. Between-group effect sizes were calculated as the model-based difference in change divided by the pooled standard deviation of the outcome at baseline (Feingold, 2009).
There was a difference in attrition rates from baseline to the 8-week assessment between the Bone Power and control groups (Bone Power = 23.7%; control = 6.8%). Thus, as a sensitivity analysis, we refit the mixed-effect models using model-based SEs. Under normality, using model-based SEs results in tests that are less likely to be biased to the extent that the “missingness” of outcomes is dependent on observed data (i.e., baseline outcome measurements; Feingold, 2009). Statistical Analysis System (SAS) 9.4 was used for analysis (SAS Institute Inc., n.d.).
Within the intervention group, we also assessed the potential effect of intervention usage on the changes in major outcomes (“dose-effects”) using LMMs. The fixed effects included time, usage (frequencies of module and discussion use), and time-by-usage interaction. A random intercept was included to account for the correlation between repeated measures within each participant. The significance of the interaction term indicated the effects.
Power Calculation
Initially, a sample size of 768 (256 per group) was calculated based on detecting a small effect (Cohen's f = .08) in group-by-time interactions using a repeated-measures analysis of variance with sufficient power (≥.90, α = .5). During the trial, we experienced a dropout rate of approximately 20%, which was higher than we anticipated (10%) based on our prior studies (Nahm et al., 2010; Nahm et al., 2012). Thus, the sample size was increased and a total of 866 participants were recruited.
Results
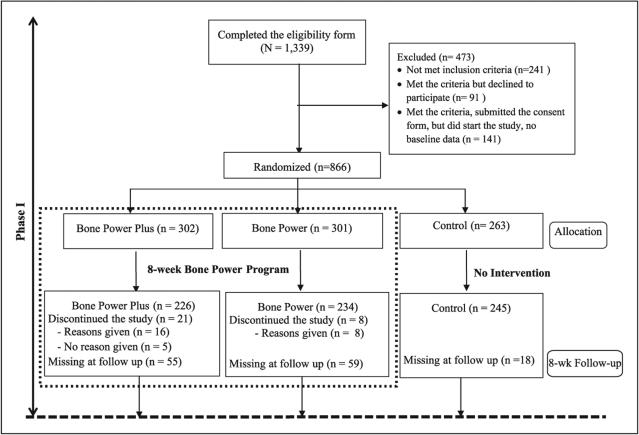
A total of 1,339 individuals who visited the study website completed the online eligibility form. Among those, 241 did not meet the criteria, 91 declined to participate, and 141 submitted the consent form but did not start the study (Figure 2, CONSORT diagram). A total of 866 participants were randomized into either the control (n = 263) or intervention (Bone Power, n = 301; Bone Power Plus, n = 302) group. At the end of the intervention, 705 participants completed the 8-week follow-up survey. Twenty-nine participants dropped out of the study (i.e., expressed the wish to stop participating), and an additional 132 participants did not respond to the 8-week survey. The most frequent reasons for discontinuation were lack of time and illness. Participants who did not complete the survey (n = 161, 18.6%) had frailer health (e.g., more arthritis, depression) than those who completed the survey and were more likely to have seen a physician due to acute illness during the 3 months prior to the baseline survey.
Figure 2.
Consolidated Standards of Reporting Trials (CONSORT)diagram showing the flow of participants through each stage of the Bone Power trial (Phase I).
Table 4 summarizes participant characteristics. More than half (63.4%) of participants were male, with a mean age of 62.8 ± 8.5 years. The majority were White (n = 776, 89.6%), followed by Black (n = 64, 7.4%), and had some college or higher level of education (n = 755, 87.2%). Approximately one in four (n = 202, 23.3%) reported having osteoporosis, and 37.4% (n = 324) reported depression. The average years of web experience was 14.5 ± 6.6, and the mean amount of time spent using the web was 15 ± 13.8 hr per week. The average level of eHealth literacy was 30.9 ± 6.0 (scale range = 8-40). Participant characteristics were comparable between the intervention and control groups at baseline. Only one baseline variable (weekly web use hours) was significantly different between the groups, which could have occurred by chance variation considering the number of participant characteristics that were compared. A total of 705 participants completed the 8-week end-of-intervention survey. For the intervention group, the mean perceived usability of the program was 70.44 ± 12.7 (scale range = 12-84).
Table 4.
Characteristics of Participants at Study Baseline by Intervention and Control Groups.
| Total sample |
Bone power |
Control |
||
|---|---|---|---|---|
| Characteristic | N = 866 | n = 603 | n = 263 | p valuea |
| Age, M ± SD | 62.8 ± 8.5 | 62.6 ± 8.5 | 63.5 ± 8.5 | .138 |
| Gender, n (%) | .419 | |||
| Male | 549 (63.4) | 377 (62.5) | 172 (65.4) | |
| Female | 317 (36.6) | 226 (37.5) | 91 (34.6) | |
| Race, n (%) | .767 | |||
| White | 776 (89.6) | 543 (90.0) | 233 (88.6) | |
| Black | 64 (7.4) | 42 (7.0) | 22 (8.4) | |
| Others | 26 (3.0) | 18 (3.0) | 8 (3.0) | |
| Married, n (%) | .606 | |||
| Married | 456 (52.7) | 321 (53.2) | 135 (51.3) | |
| Nonmarried | 410 (47.3) | 282 (46.8) | 128 (48.7) | |
| Education, n (%) | .705 | |||
| High school or less | 111 (12.8) | 79 (13.1) | 32 (12.2) | |
| Some college or higher | 755 (87.2) | 524 (86.9) | 231 (87.8) | |
| PC knowledge, n (%) | .474 | |||
| Beginner | 28 (3.2) | 22 (3.6) | 6 (2.3) | |
| Advanced beginner | 114 (13.2) | 74 (12.3) | 40 (15.2) | |
| Competent | 356 (41.1) | 246 (40.8) | 110 (41.8) | |
| Proficient | 297 (34.3) | 214 (35.5) | 83 (31.6) | |
| Expert | 71 (8.2) | 47 (7.8) | 24 (9.1) | |
| Web experience in years, M ± SD | 14.5 ± 6.6 | 14.6 ± 6.5 | 14.2 ± 6.8 | .390 |
| Weekly web use hours, M ± SD | 15.4 ± 13.8 | 16.3 ± 14.8 | 13.4 ± 10.7 | .005 |
| eHealth literacyb, M ± SD | 30.9 ± 6.0 | 31.0 ± 6.0 | 30.9 ± 6.1 | .807 |
| Chronic diseases (Yes), n (%) | ||||
| Bronchitis | 122 (14.1) | 91 (15.1) | 31 (11.8) | .199 |
| High BP | 489 (56.5) | 341 (56.6) | 148 (56.3) | .940 |
| Cardiac problem | 184 (21.3) | 123 (20.4) | 61 (23.2) | .355 |
| Diabetes | 214 (24.7) | 142 (23.6) | 72 (27.4) | .230 |
| Depression | 324 (37.4) | 229 (38.0) | 95 (36.1) | .604 |
| Osteoporosis | 202 (23.3) | 144 (23.9) | 58 (22.1) | .559 |
From tests of comparison of means (t test) or proportions (χ2) between the bone power group and control group.
eHealth Literacy Scale, Range: 8-40.
Outcomes Measures
Table 5 presents the results of primary LMM analyses, including group raw means and standard deviations at baseline and at the end of treatment. Overall, the Bone Power group had greater improvement than the control group in all outcomes. Results of the sensitivity analysis were similar to the main analysis.
Table 5.
Group Means and Standard Deviations at Baseline and Post-Treatment and Liner Mixed Model Results.
| Baseline (N = 866) |
8-weeks (n = 705) |
β estimationa |
Estimated effect sizes |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Bone power |
Control |
Bone power |
Control |
Within bone power group | ||||||
| Outcome | (n = 603) M (SD) | (n = 263) M (SD) | (n = 460) M (SD) | (n = 245) M (SD) | Estimation | 95% CI | p value | Within control group | Between groups | |
| Osteoporosis knowledge (0-27) | 15.3 (5.0) | 15.1 (4.9) | 19.6 (4.0) | 16.6 (4.4) | 2.66 | [2.21, 3.11] | <.001 | .79 | .26 | .54 |
| CA intake self-efficacy (0-110)b | 82.5 (21.6) | 81.9 (20.7) | 90.3 (16.9) | 82.7 (21.2) | 1070.4 | [662.1, 1478.8] | <.001 | .35 | .02 | .33 |
| CA outcome expectation (6-30) | 21.7 (3.5) | 21.8 (3.5) | 23.1 (3.8) | 22.5 (3.7) | 0.70 | [0.18, 1.23] | .009 | .40 | .20 | .20 |
| CA intake (mg)c | 1273.6 (1115.9) | 1187.1 (967.8) | 1526.1 (1326.9) | 1278.1 (1059.6) | 0.17 | [0.08, 0.26] | <.001 | .24 | .03 | .21 |
| Exercise self-efficacy (0-90) | 48.7 (26.0) | 51.1 (25.5) | 51.0 (25.7) | 47.5 (25.5) | 4.76 | [1.73, 7.79] | .002 | .05 | −.14 | .18 |
| Ex. outcome expectation (6-30)b | 37.0 (7.0) | 37.3 (7.2) | 37.5 (7.1) | 36.6 (7.6) | 66.90 | [5.62, 128.17] | .032 | .04 | −.11 | .14 |
| Yale exercise (Kcals)c | 603.5 (994.2) | 582.8 (831.3) | 824.6 (1130.2) | 688.6 (1018.3) | 0.37 | [0.04, 0.70] | .030 | .25 | .13 | .12 |
| Yale exercise (minutes)c | 110.2 (173.2) | 104.2 (149.3) | 149.1 (200.0) | 125.6 (177.9) | 0.27 | [0.01, 0.54] | .042 | .25 | .14 | .11 |
Note. CI = confidence interval; LMM = linear mixed models; CA = Calcium.
Coefficient estimation of the group-by-time interaction term in LMM.
LMM analysis performed after square transformation of outcome variable.
LMM analysis performed after natural log transformation of outcome variable.
Participants in both the Bone Power and control groups improved their knowledge of osteoporosis at the end of the intervention. The Bone Power group, however, showed greater improvement than the control group, t(703) = 11.4, p < .001, effect size (ES) = .54. Both groups also increased their levels of self-efficacy and outcome expectations for calcium intake. Greater improvements by the Bone Power group were observed for both calcium intake self-efficacy, t(703) = 5.15, p < .001, ES = .33; and calcium outcome expectations, t(703) = 2.63, p = .009, ES = .20. Calcium intake also improved relative to the control group, t(703) = 3.69, p < .001, ES = .21. For exercise, the Bone Power group improved for both self-efficacy and outcome expectations after the intervention, whereas the control group declined. The differences in change between the two groups were significant, t(703) = 3.08, p = .002, ES = .18, for exercise self-efficacy; t(703) = 2.14, p = .032, ES = .14, for exercise outcome expectation. In regard to exercise behaviors, both groups increased the amount of and time spent on exercises, with greater improvement observed in the Bone Power group, t(700) = 2.18, p = .030, ES = .12, for exercise Kcals; t(703) = 2.03, p = .042, ES = .11, for exercise minutes.
Fidelity Monitoring of the Intervention
All intervention group participants (100%) logged on to the Bone Power web-site. The majority (74.2%) of participants reviewed five or more modules. On average, 63% of participants in each group reviewed the new learning content weekly during the first 4 weeks (many participants logged on to modules multiple days during the week). A total of 73.6% of participants used the discussion board, reading, and/or posting responses. The mean number of visits to the discussion forums was 43.2 ± 77.1. More than half of participants (51.1%) actively participated in the discussions by posting more than 10 responses, 22.7% responded 1 to 10 times, and 26.2% posted no responses. The degree of module usage (frequency) had positive effects on changes in total knowledge scores, t(458) = 3.58, p < .001; self-efficacy for calcium intake, t(458) = 2.88, p = .004; and outcome expectation for calcium intake, t(458) = 3.0, p = .003. Discussion forum usage (reading and posting) also showed positive effects on changes in self-efficacy on calcium intake, t(457) = 2.25, p = .025, and outcome expectation on calcium intake, t(457) = 1.97, p = .049, but not on the knowledge score. Active participation in discussion (frequency of posting) showed a significant effect only on calcium intake self-efficacy, t(458) = 2.67, p = .008.
Discussion
The overall findings of this study suggest the effectiveness of the online Bone Power program in improving older adults’ bone health–related outcomes. In regard to osteoporosis knowledge, both the intervention and control groups showed increased knowledge at the end of the intervention; however, the intervention group's improvement was significantly greater than that of the control group. The slight improvement in the control group may suggest a potential impact from the online survey and a motivation factor from being enrolled in a bone health study. In fact, considering that participants were online users, the online survey itself might have facilitated participants’ own search of online health information.
For the outcomes associated bone health behaviors, participants who were exposed to the Bone Power program showed significantly greater improvement over the control group for self-efficacy and outcome expectations for both calcium intake and exercise. The group's calcium intake and amount of exercise also increased more than that of the control group. These findings are consistent with other studies that showed the effectiveness of theory-based online programs for older adults (Cook et al., 2015; Irvine et al., 2013). In an RCT conducted by Cook and his colleague (2015), an online SCT-based health-promotion program was effective in improving older adults’ dietary behavioral change self-efficacy, healthy eating planning, and exercise. Irvine et al. (2013) also reported the positive impact of a theory-based online physical activity intervention on knowledge, attitudes, self-efficacy, and behavioral intentions of older adults. Our findings provide support for effectively using online programs to improve bone health among older adults.
Regarding the magnitude of intervention effects, overall, the Bone Power intervention showed a higher effect size for knowledge (.54) compared with other behavior-related health outcomes, such as self-efficacy, outcome expectations, calcium intake, and amount of exercise (.11-.30). Several prior studies also reported similar findings (Lustria et al., 2013; van den Berg et al., 2007; Webb et al., 2010). Based on recent meta-analysis reports (van den Berg et al., 2007; Webb et al., 2010), online interventions were efficacious in changing health behaviors; however, their effect sizes were often small (<.2). Theory-based approaches, additional communication with participants, and just-in-time reminders have been shown to improve effects of online interventions (van den Berg et al., 2007; Webb et al., 2010).
Within the intervention group, participants who used the modules or discussion forums more frequently showed greater improvement in self-efficacy, outcome expectations, and knowledge, which is consistent with other prior findings (Irvine et al., 2013). These findings indicate the importance of including specific strategies to motivate participants to use the intervention in online trials. In our study, we sent out weekly emails informing participants of the availability of new learning content for the week. In addition, the use of SCT-based interventions, moderated discussion forums, and small-group approaches was also helpful in engaging participants. Based on SCT, a social learning averment is important because social modeling, motivation, and encouragement can occur in this setting (Bandura, 1998). Prior studies have shown the effectiveness of the small-group approach in delivering theory-based health-promotion interventions (Carpenter, Finley, & Barlow, 2004; Cimprich et al., 2005; Nahm et al., 2011). For example, in this study, participants in each group had the opportunity to interact with each other through the discussion board for a prolonged time period as they progressed in the trial. Using a well-prepared moderator for the discussion boards can also be helpful, as he or she can direct the group members’ discussions toward the goals of the study and provide encouraging comments (Cudney & Weinert, 2000). We have used moderated discussion boards successfully in our prior work (Nahm et al., 2011; Nahm, Resnick, Grezia, & Brothemarkle, 2009).
From the recruitment and retention perspective, we were able to recruit 866 participants online within a 7-month period. This suggests a high interest in and demand for bone health interventions in older adults, as well as a great potential for using online formats to deliver health interventions to this group. The total attrition rate at the end of the 8-week intervention was 18.6%. Dropout rates reported in other eHealth intervention trials vary, ranging from 0% to 83% (Donkin et al., 2011; Vandelanotte, Spathonis, Eakin, & Owen, 2007), and high attrition rates have raised concerns in several studies. Only 24 participants in this study provided specific reasons for dropout (e.g., no time, health conditions). When the group of participants that dropped out was compared with the group that stayed in the study, the dropout group had frailer health (e.g., more arthritis, depression, visits to a physician due to acute illnesses). In contrast to other studies where computer competency influenced participation (Irvine et al., 2013), in this study, there were no differences in computer competency or education level among those who did versus did not drop out. This could be because the participants were already online users.
There were more dropouts in the intervention group (23.7%) than in the control group (6.8%) in our study. Higher dropout rates in online intervention studies have been reported. In an online physical activity study, Irvine et al. (2013) reported an overall attrition rate of 17.9% at 12 weeks. However, the attrition rate for the intervention group was 30% compared with 7% for the control group. Cook and his colleagues (2015) also reported differential attrition rates between the intervention and control groups (19.6% vs. 5.7%, respectively) in their study that tested the impact of an online health-promotion program in older adults. Although no specific reasons for differential dropouts were reported, the higher dropout rate in the intervention group could have been associated with the increased burden of using the intervention (e.g., reviewing modules, participating in discussion boards). Further investigation is needed to identify specific reasons for differential dropout.
In addition to our findings relating to this study's main outcomes, participants noted additional benefits from taking part in the study. For example, many commented on experiencing weight loss due to increased physical activity and having healthier diets. Future studies may consider including weight management a health outcome from bone health interventions. Another interesting finding of the study was associated with prevalence of osteoporosis. Osteoporosis is more prevalent in women (~20%) than men (NOF, 2014a); however, in our sample, of which 63.4% (n = 549) were men, 23.3% reported having osteoporosis, suggesting a higher prevalence rate than in the general population. These findings raise a couple of clinically significant issues. First, a higher proportion of males in this sample are from MHV, which suggests that these individuals may require more rigorous bone health screening and preventive measures. Second, high interest in this trial among males suggests increased awareness of bone health in this group. Further research efforts are needed to investigate bone health issues specific to males and to educate them about the importance of bone health.
Limitations
Some of the sample characteristics may limit generalizability of the findings. Participants were recruited from two large online communities, and these individuals may have been more familiar with the technology than the general older adult population. In addition, the majority of the sample was white, with high educational levels. More efforts must be made to disseminate this type of program to underserved older adults who are less technically savvy. Although 183 (21%) older adults were recruited from SeniorNet, the majority of the sample was recruited from MHV, and veterans may have different health needs than non-veteran older adults. The data were collected using self-reported online surveys only. In a future study, collection of objective data may be considered for a subset of the sample. The 8-week follow-up time frame focused only on initial behavior change. Future research also needs to consider the long-term effects of the intervention, as well as the cost-effectiveness of this study.
Conclusion
Despite some limitations, the findings of this study support the effectiveness of online interventions to improve knowledge, beliefs, and behaviors associated with bone health. As the American population gets older, age-related bone health issues will become more prevalent in health care. Certain older adult populations, such as veterans, may be at higher risk for bone health–related illnesses. Online bone health interventions have the advantage of reaching a large number of individuals and widely disseminating evidence-based information. Thus, the use of online health interventions has significant potential for improving the health of older adults. The theory-based online approach used in this study can be replicated for other health conditions and diverse older adult populations. Considering current national efforts to engage patients in their own care using health information technologies, now is an excellent time to make progress in this health care field.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by Grant R01 NR011296 from the National Institute of Nursing Research and P30 AG028747 from the National Institute on Aging. The study was registered with ClinicalTrials.gov (NCT01963169).
Biography
Eun-Shim Nahm, PhD, RN, FAAN, is a professor at the University of Maryland School of Nursing. Her research focuses on the use of technology-based interventions to promote the health of older adults. She has developed and implemented many eHealth interventions for older adults, and her studies were supported by multiple grant awards from the National Institutes of Health.
Barbara Resnick, PhD, CRNP, is a professor in the Department of Organizational Systems and Adult Health at the University of Maryland School of Nursing, co-directs the Adult/Gerontological Nurse Practitioner Program and the Biology and Behavior Across the Lifespan Research Center of Excellence, holds the Sonya Ziporkin Gershowitz chair in gerontology, and does clinical work at Roland Park Place.
Clayton Brown, PhD, is an associate professor in the Department of Epidemiology, University of Maryland School of Medicine. He is also the director of the Biostatistics Core for the VA Capitol Healthcare Network Mental Illness, Research, Education and Clinical Center.
Shijun Zhu, PhD, is an assistant professor at the University of Maryland School of Nursing. His research interests include statistical methods and applications in biomedical, public health, and health care research, as well as joint modeling of longitudinal observations and recurrent events.
Jay Magaziner, PhD, MSHyg, is a professor and chair of the Department of Epidemiology & Public Health. He pursues research on consequences of hip fracture, health and long-term care, and methods for studying older populations. The major focus of this work is to enhance functioning and improving the quality of life for older persons.
Michele Bellantoni, MD, is an associate professor and clinical director of the Johns Hopkins University School of Medicine Division of Geriatric Medicine and Gerontology. Her current research focuses on improving care in skilled nursing facilities and transitions in care for older adults.
Patricia Flatley Brennan, PhD, RN, is the Lillian L. Moehlman Bascom Professor at the School of Nursing and College of Engineering at the University of Wisconsin– Madison. She directs an AHRQ-funded study, vizHOME, to examine contextual influences on personal health information management, and is the director of the Living Environments Laboratory (LEL) at the Wisconsin Institutes for Discovery.
Kathleen Charters, PhD, RN, CPHIMS, is a nurse consultant to the Defense Health Agency. Her research focuses on evaluation of Health IT and the effect it has on patient safety, quality of care delivery, and consumer empowerment. She has integrated quality measure data collection into clinical workflow. She has developed and implemented content for VA and DoD patient portals.
Jeanine Brown, MS, RN, is a research nurse/nurse care manager at the University of Maryland School of Nursing. Her research interests include health promotion, online research, and health literacy. She has managed and participated in numerous research projects and has helped develop interventions related to bone health in older adults, kidney disease, and health literacy.
Mathew Rietschel, MS, is an assistant professor and the assistant dean for information and learning technology at the University of Maryland School of Nursing. He has been involved in multiple research studies focusing on technology centered interventions to improve the health of older adults and the education of nursing workforce.
Minjeong An, PhD, RN, ACNP-BC, is an assistant professor at the Chonnam National University College of Nursing in Korea. Her research interests include health disparity, disease prevention, and health promotion in middle-aged adults. She has been involved in various health promotion studies in the United States and Korea. Dr. An is now at the Chonnam National University, Korea.
Bu Kyung Park, PhD, RN, is an assistant professor at the Red-Cross College of Nursing, Chung-Ang University in Korea. Her research interests include use of social media for children and health promotion. Dr. Park is now at the Red-Cross College of Nursing, Chung-Ang University, Korea.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American College of Sports Medicine Physical activity programs and behavior counseling in older adult populations. Medicine & Science in Sports & Exercise. 2004;36:1997–2003. doi: 10.1249/01.mss.0000145451.08166.97. [DOI] [PubMed] [Google Scholar]
- Bailey RL, Dodd KW, Goldman JA, Gahche JJ, Dwyer JT, Moshfegh AJ, Picciano MS. Estimation of total usual calcium and vitamin D intakes in the United States. The Journal of Nutrition. 2010;140:817–822. doi: 10.3945/jn.109.118539. doi:10.3945/jn.109.118539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. Freeman; New York, NY: 1997a. [Google Scholar]
- Bandura A. Self-efficacy in changing societies. Cambridge University Press; New York, NY: 1997b. [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology and Health. 1998;13:623–649. doi:10.1080/08870449808407422. [Google Scholar]
- Bass E, Pracht E, Foulis P. Bone mineral density scans in veterans. Clinical Interventions in Aging. 2007;2:255–261. [PMC free article] [PubMed] [Google Scholar]
- Blackboard Inc. Blackboard platforms. 2013 Available from http://www.blackboard.com.
- Blalock SJ, Norton LL, Patel RA, Cabral K, Thomas CL. Development and assessment of a short instrument for assessing dietary intakes of calcium and vitamin D. Journal of the American Pharmacists Association. 2003;43:685–693. doi: 10.1331/154434503322642615. doi:10.1331/154434503322642615. [DOI] [PubMed] [Google Scholar]
- Brownson RC, Colditz GA, Proctor EK. Dissemination and implementation research in health: Translating science to practice. Oxford University Press; Oxford, UK: 2012. [Google Scholar]
- Campbell BJ. Exercise and bone health. 2012 Retrieved from http://orthoinfo.aaos.org/topic.cfm?topic=A00674.
- Carpenter RA, Finley C, Barlow CE. Pilot test of a behavioral skill building intervention to improve overall diet quality. Journal of Nutrition Education & Behavior. 2004;36:20–26. doi: 10.1016/s1499-4046(06)60124-3. [DOI] [PubMed] [Google Scholar]
- Cimprich B, Janz NK, Northouse L, Wren PA, Given B, Given CW. Taking charge: A self-management program for women following breast cancer treatment. Psycho-Oncology. 2005;14:704–717. doi: 10.1002/pon.891. doi:10.1002/pon.891. [DOI] [PubMed] [Google Scholar]
- Cook RF, Hersch RK, Schlossberg D, Leaf SL. A Web-based health promotion program for older workers: Randomized controlled trial. Journal of Medical Internet Research. 2015;17(3):e82. doi: 10.2196/jmir.3399. doi:10.2196/jmir.3399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cudney SA, Weinert C. Computer-based support groups: Nursing in cyberspace. Computers in Nursing. 2000;18:35–43. [PubMed] [Google Scholar]
- Curtis JR, Carbone L, Cheng H, Hayes B, Laster A, Matthews R, Delzell E. Longitudinal trends in use of bone mass measurement among older Americans, 1999-2005. Journal of Bone and Mineral Research. 2008;23:1061–1067. doi: 10.1359/JBMR.080232. doi:10.1359/jbmr.080232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desroches S, Lapointe A, Ratte S, Gravel K, Legare F, Turcotte S. Interventions to enhance adherence to dietary advice for preventing and managing chronic diseases in adults. Cochrane Database of Systematic Reviews. 2013;2:CD008722. doi: 10.1002/14651858.CD008722.pub2. doi:10.1002/14651858.CD008722.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dipietro L, Caspersen CJ, Ostfeld AM, Nadel ER. A survey for assessing physical activity among older adults. Medicine & Science in Sports & Exercise. 1993;25:628–642. doi:10.1249/00005768-199305000-00016. [PubMed] [Google Scholar]
- Donkin L, Christensen H, Naismith SL, Neal B, Hickie IB, Glozier N. A systematic review of the impact of adherence on the effectiveness of e-therapies. Journal of Medical Internet Research. 2011;13(3):e52. doi: 10.2196/jmir.1772. doi:10.2196/jmir.1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14:43–53. doi: 10.1037/a0014699. doi:10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. John Wiley; Hoboken, NJ: 2011. [Google Scholar]
- Fox S, Duggan M. Health Online 2013. 2013 Retrieved from http://www.pewinternet.org/files/old-media//Files/Reports/PIP_HealthOnline.pdf.
- Irvine AB, Gelatt VA, Seeley JR, Macfarlane P, Gau JM. Web-based intervention to promote physical activity by sedentary older adults: Randomized controlled trial. Journal of Medical Internet Research. 2013;15(2):e19. doi: 10.2196/jmir.2158. doi:10.2196/jmir.2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim KK, Horan M, Gendler P, Patel M. Osteoporosis health belief, self-efficacy, and knowledge test. In: Redman BK, editor. Measurement tools in patient education. 2nd ed. Springer; New York, NY: 2003. pp. 364–377. [Google Scholar]
- Kim KK, Horan ML, Gendler P, Patel MK. Development and evaluation of the Osteoporosis Health Belief Scale. Research in Nursing & Health. 1991;14:155–163. doi: 10.1002/nur.4770140210. doi:10.1002/nur.4770140210. [DOI] [PubMed] [Google Scholar]
- Kimber CM, Grimmer-Somers KA. Evaluation of current practice: Compliance with osteoporosis clinical guidelines in an outpatient fracture clinic. Australian Health Review. 2008;32:34–43. doi: 10.1071/ah080034. doi:10.1071/AH080034. [DOI] [PubMed] [Google Scholar]
- Kleerekoper M. UpToDate: Patient information: Bone density testing (Beyond the basics) 2013 Retrieved from http://www.uptodate.com/contents/bone-density-testing-beyond-the-basics.
- Kloseck M. The use of Goal Attainment Scaling in a community health promotion initiative with seniors. BMC Geriatrics. 2007;7(1):16. doi: 10.1186/1471-2318-7-16. doi:10.1186/1471-2318-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustria ML, Noar SM, Cortese J, Van Stee SK, Glueckauf RL, Lee J. A meta-analysis of web-delivered tailored health behavior change interventions. Journal of Health Communication. 2013;18:1039–1069. doi: 10.1080/10810730.2013.768727. doi:10.1080/10810 730.2013.768727. [DOI] [PubMed] [Google Scholar]
- MacLean C, Newberry S, Maglione M, McMahon M, Ranganath V, Suttorp M, Grossman J. Systematic review: Comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Annals of Internal Medicine. 2008;148:197–213. doi: 10.7326/0003-4819-148-3-200802050-00198. doi:10.7326/0003-4819-148-3-200802050-00198. [DOI] [PubMed] [Google Scholar]
- Mangano KM, Walsh SJ, Insogna KL, Kenny AM, Kerstetter JE. Calcium intake in the United States from dietary and supplemental sources across adult age groups: New estimates from the National Health and Nutrition Examination Survey 2003-2006. Journal of the American Dietetic Association. 2011;111:687–695. doi: 10.1016/j.jada.2011.02.014. doi:10.1016/j.jada.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GD, Jarvis JK, McBean LD. Handbook of dairy foods and nutrition. 3rd ed. CRC Press; Boca Raton, FL: 2006. [Google Scholar]
- Murphy BM, Worcester MU, Higgins RO, Elliott PC, Le Grande MR, Mitchell F, Globe AJ. Reduction in 2-year recurrent risk score and improved behavioral outcomes after participation in the “Beating Heart Problems” self-management program: Results of a randomized controlled trial. Journal of Cardiopulmonary Rehabilitation and Prevention. 2013;33:220–228. doi: 10.1097/HCR.0b013e31828c7812. doi:10.1097/HCR.0b013e31828c7812. [DOI] [PubMed] [Google Scholar]
- Nahm E-S, Barker B, Resnick B, Covington B, Magaziner J, Brennan PF. Effects of a social cognitive theory-based hip fracture prevention web site for older adults. CIN: Computers, Informatics, Nursing. 2010;28:371–379. doi: 10.1097/NCN.0b013e3181f69d73. doi:10.1097/NCN.0b013e3181f69d73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahm E-S, Bausell B, Resnick B, Covington B, Brennan PF, Mathews R, Park JH. Online research in older adults: Lessons learned from conducting an online randomized controlled trial. Applied Nursing Research. 2011;24:269–275. doi: 10.1016/j.apnr.2009.09.004. doi:10.1016/j.apnr.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahm E-S, Resnick B, Bausell B, Orwig D, Magaziner J, Bellantoni M, Brennan PF. A social cognitive theory-based online hip fracture resource center for caregivers: Effects on dyads. Nursing Research. 2012;61:413–422. doi: 10.1097/NNR.0b013e318270712a. doi:10.1097/NNR.0b013e318270712a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahm E-S, Resnick B, Bellantoni M, Zhu S, Brown C, Brennan PF, Plummer L. Dissemination of theory-based online bone health programs: Two intervention approaches. Health Informatics Journal. 2015;21:120–136. doi: 10.1177/1460458213505573. doi:10.1177/1460458213505573. [DOI] [PubMed] [Google Scholar]
- Nahm E-S, Resnick B, Grezia M, Brothemarkle B. Use of discussion boards in a theory-based health web site for older adults. Nursing Research. 2009;58:419–426. doi: 10.1097/NNR.0b013e3181bee6c4. doi:10.1097/NNR.0b013e3181bee6c4. [DOI] [PubMed] [Google Scholar]
- Nahm E-S, Resnick B, Mills ME. Development and pilot-testing of the perceived health Web site usability questionnaire (PHWSUQ) for older adults. Studies in Health Technology and Informatics. 2006;122:38–43. [PubMed] [Google Scholar]
- National Cancer Institute Diet History Questionnaire: Current database file. 2008 Retrieved from http://riskfactor.cancer.gov/DHQ/database/current.html.
- National Institute on Aging Making your web site senior friendly. 2009 Retrieved from https://www.nia.nih.gov/sites/default/files/making_your_website_senior_friendly.pdf.
- National Osteoporosis Foundation Clinician's guide to prevention and treatment of osteoporosis. 2013 Retrieved from http://www.nof.org/files/nof/public/content/file/344/upload/159.pdf.
- National Osteoporosis Foundation 54 million Americans affected by osteoporosis and low bone mass. 2014a Retrieved from http://nof.org/news/2948.
- National Osteoporosis Foundation Osteoporosis clinical updates: Rehabilitation of patients with fragility-related fractures. 2014b Retrieved from https://my.nof.org/file/bonesource/cme-articles/2014-Rehabilitation-of-Fragility-Fx.pdf.
- National Osteoporosis Foundation Calcium and vitamin D: What you need to know. n.d.-a Retrieved from http://nof.org/calcium#CALCIUM.
- National Osteoporosis Foundation Having a bone density test. n.d.-b Retrieved from http://nof.org/articles/743.
- National Osteoporosis Foundation Learn about osteoporosis. n.d.-c Retrieved from http://www.nof.org/learn/prevention.
- National Osteoporosis Foundation What is osteoporosis? n.d.-d Retrieved from http://www.nof.org/articles/7.
- Norman CD, Skinner HA. eHEALS: The eHealth Literacy Scale. Journal of Medical Internet Research. 2006;8(4):e27. doi: 10.2196/jmir.8.4.e27. doi:10.2196/jmir.8.4.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Internet Demographics of Internet users. 2014 Retrieved from http://www.pewinternet.org/data-trend/internet-use/latest-stats/
- President's Council on Fitness, Sports & Nutrition Exercise comes of age as medicine for older adults. 2010 Retrieved from https://www.presidentschallenge.org/informed/digest/docs/june2010digest.pdf.
- Qi BB, Resnick B, Nahm ES. Reliability and validity of the revised Osteoporosis Knowledge Test (OKT). Journal of Nursing Measurement. 2014;22:342–356. doi: 10.1891/1061-3749.22.2.342. doi:10.1891/1061-3749.22.2.342. [DOI] [PubMed] [Google Scholar]
- Ramadas A, Quek KF, Chan CK, Oldenburg B. Web-based interventions for the management of type 2 diabetes mellitus: A systematic review of recent evidence. International Journal of Medical Informatics. 2011;80:389–405. doi: 10.1016/j.ijmedinf.2011.02.002. doi:10.1016/j.ijmedinf.2011.02.002. [DOI] [PubMed] [Google Scholar]
- Resnick B, Jenkins LS. Testing the reliability and validity of the Self-Efficacy for Exercise Scale. Nursing Research. 2000;49:154–159. doi: 10.1097/00006199-200005000-00007. doi:10.1097/00006199-200005000-00007. [DOI] [PubMed] [Google Scholar]
- Resnick B, Orwig D, Zimmerman S, Hawkes W, Golden J, Werner-Bronzert M, Magaziner J. Testing of the SEE and OEE post-hip fracture. Western Journal of Nursing Research. 2006;28:586–601. doi: 10.1177/0193945906287218. doi:10.1177/0193945906287218. [DOI] [PubMed] [Google Scholar]
- Resnick B, Zimmerman S, Orwig D, Furstenberg AL, Magaziner J. Model testing for reliability and validity of the Outcome Expectations for Exercise Scale. Nursing Research. 2001;50:293–299. doi: 10.1097/00006199-200109000-00007. doi:10.1097/00006199-200109000-00007. [DOI] [PubMed] [Google Scholar]
- Rosen CJ. The epidemiology and pathogenesis of osteoporosis. In: De Groot LJ, et al., editors. Endotext. MDText.com.; South Dartmouth, MA: 2014. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK279134/ [Google Scholar]
- SAS Institute Inc. SAS 9.4. n.d. Retrieved from http://www.sas.com/software/sas9/
- Schweier R, Romppel M, Richter C, Hoberg E, Hahmann H, Scherwinski I, Grande G. A web-based peer-modeling intervention aimed at lifestyle changes in patients with coronary heart disease and chronic back pain: Sequential controlled trial. Journal of Medical Internet Research. 2014;16(7):e177. doi: 10.2196/jmir.3434. doi:10.2196/jmir.3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A. Older adults and technology use. 2014 Retrieved from http://www.pewinternet.org/2014/04/03/older-adults-and-technology-use/
- U.S. Department Agriculture SuperTracker. n.d. Retrieved from https://www.supertracker.usda.gov/default.aspx (accessed 2 June 2015)
- Vandelanotte C, Spathonis KM, Eakin EG, Owen N. Website-delivered physical activity interventions a review of the literature. American Journal of Preventive Medicine. 2007;33:54–64. doi: 10.1016/j.amepre.2007.02.041. doi:10.1016/j.amepre.2007.02.041. [DOI] [PubMed] [Google Scholar]
- van den Berg MH, Schoones JW, Vliet Vlieland TP. Internet-based physical activity interventions: A systematic review of the literature. Journal of Medical Internet Research. 2007;9(3):e26. doi: 10.2196/jmir.9.3.e26. doi:10.2196/jmir.9.3.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace LS. Osteoporosis prevention in college women: Application of the expanded health belief model. American Journal of Health Behavior. 2002;26:163–172. doi: 10.5993/ajhb.26.3.1. doi:10.5993/AJHB.26.3.1. [DOI] [PubMed] [Google Scholar]
- Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research. 2010;12(1):e4. doi: 10.2196/jmir.1376. doi:10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization eHealth. 2012 Retrieved from http://www.who.int/topics/ehealth/en/
- World Health Organization Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, UK. Welcome to FRAX®. n.d. Retrieved from http://www.shef.ac.uk/FRAX/