Pulmonary arteriovenous malformations (PAVMs) are abnormal blood vessels that connect pulmonary arteries direct to pulmonary veins, thus bypassing the pulmonary capillaries which are essential to filter, process and oxygenate blood [1]. Population-wide screening programmes using thoracic computed tomography scans suggest a prevalence of 1 in 2630 (95% CI 1 in 1315–1 in 5555) [2], although the condition is subject to substantial under-ascertainment [3].
Short abstract
PAVMs pose unique management challenges; publication patterns indicate their importance remains poorly recognised http://ow.ly/7iIT304WYl2
To the Editor:
Pulmonary arteriovenous malformations (PAVMs) are abnormal blood vessels that connect pulmonary arteries direct to pulmonary veins, thus bypassing the pulmonary capillaries which are essential to filter, process and oxygenate blood [1]. Population-wide screening programmes using thoracic computed tomography scans suggest a prevalence of 1 in 2630 (95% CI 1 in 1315–1 in 5555) [2], although the condition is subject to substantial under-ascertainment [3].
As detailed elsewhere [1], treatment of asymptomatic individuals is recommended to prevent paradoxical embolic strokes, and brain abscess that affect high proportions of patients, irrespective of PAVM respiratory symptoms [4]. There are unique recommendations for the management of hypoxaemia and pregnancy, when usual population-based guidance does not suffice or apply [1]. Furthermore, the majority of patients with PAVMs have underlying hereditary haemorrhagic telangiectasia (HHT), necessitating a range of additional screening and management interventions [5]. This is particularly important in pregnancy, for which there is a 1.00% (95% CI 0.13–1.92%) maternal death rate; however, in comparison with having undiagnosed HHT or PAVMs, an existing HHT/PAVM diagnosis is associated with improved survival in women experiencing a life-threatening event (p=0.041) [6].
PAVMs therefore pose unique management challenges. Yet their importance remains poorly recognised: In one recent UK series, the mean delay from diagnosis to referral for treatment was 7.5 years (95% CI 4.3–10.8 years) [4]. We were concerned that the condition still does not appear to be prominent in respiratory medicine training and sought to provide further evidence.
First, training curriculae in the UK and USA were examined. For the UK, PAVMs were not mentioned specifically within the current General Medical Council (GMC) Specialty training curriculum for Respiratory Medicine. In the USA, PAVMs were not mentioned specifically within the current Accreditation Council for Graduate Medical Education (ACGME) Programme Requirements for Graduate Medical Education in Pulmonary Disease (Internal Medicine).
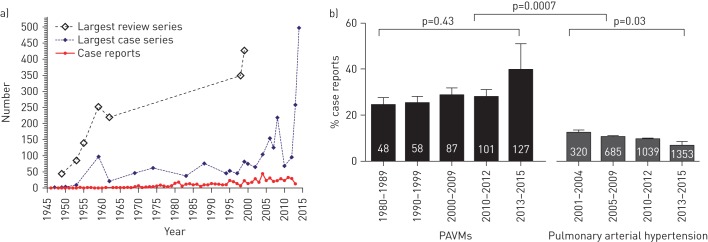
Second, PubMed searches were performed using the search term “pulmonary arteriovenous malformation” with specified date ranges, with and without the filter “case report” applied. 3604 publications were retrieved from PubMed for “pulmonary arteriovenous malformation” between 1946 and 2015. These included an article reviewing 140 cases in 1955, describing serious complications in 30 (21.4%) [7]. The evidence base prior to 1999 was summarised in two large review articles [8, 9] that continue to be highly cited. Since then, multiple individual case series have reported more than 100 cases (figure 1a).
FIGURE 1.
Evolution of pulmonary arteriovenous malformations (PAVMs) evidence base since 1945. a) Types of articles. For case series and review articles, “number” represents the number of cases within an individual paper. For case reports, “number” represents the number of case reports published per calendar year. b) Proportion of published literature per annum that is represented by single case reports, comparing PAVMs with pulmonary arterial hypertension. Mean and standard error indicated for each time period. White figures indicate mean number of publications per annum within the stated decade/time period. Within group p-values were calculated by Kruskal–Wallis, between group by Mann–Whitney.
However, in the PAVM literature, high proportions of all publications were single case reports, often reflecting common presentation patterns such as asymptomatic hypoxaemia, pregnancy complications, and paradoxical embolic stroke or brain abscess. In the decades after 1980, while the total number of publications per annum rose three-fold (figure 1b), the proportion of single case reports also rose steadily. Since 2010, single case reports have represented more than one-third of the published literature each year (figure 1b).
Furthermore, when the study methodology was repeated for a comparator pulmonary vascular disease, there were striking differences (figure 1b). Pulmonary arterial hypertension (estimated prevalence between 1 in 20 000 and 1 in 66 000 [10]) is a major component of training programmes in the UK and USA. In contrast to PAVMs, PAH has been cited 15 635 times since the term was introduced in 2001 and displays lower and falling proportions of case reports in the published literature (figure 1b).
Taken together with the lack of a formalised training programme, the publication patterns for PAVMs are a matter of concern. First, the case-report biased literature makes it difficult for the reader to ascertain usual clinical presentations. Second, their acceptance suggests continued under-recognition of PAVMs, whereby common patterns described in large review articles more than 60 years ago are deemed, by authors and editors, worthy of publication as single case reports. Third, the pattern appears to be deteriorating further, whereas no such deterioration was observed for pulmonary arterial hypertension which has been the subject of structured training programmes.
In conclusion, we suggest that the relatively common condition of PAVMs should be given greater prominence within Respiratory Medicine training curriculae.
Footnotes
Conflict of interest: None declared.
References
- 1.Shovlin CL. Pulmonary arteriovenous malformations. Am J Respir Crit Care Med 2014; 190: 1217–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakayama M, Nawa T, Chonan T, et al. Prevalence of pulmonary arteriovenous malformations as estimated by low-dose thoracic CT screening. Intern Med 2012; 51: 1677–1681. [DOI] [PubMed] [Google Scholar]
- 3.Donaldson JW, McKeever TM, Hall IP, et al. The UK prevalence of hereditary haemorrhagic telangiectasia and its association with sex, socioeconomic status and region of residence: a population-based study. Thorax 2014; 69: 161–167. [DOI] [PubMed] [Google Scholar]
- 4.Shovlin CL, Jackson JE, Bamford KB, et al. Primary determinants of ischaemic stroke/brain abscess risks are independent of severity of pulmonary arteriovenous malformations in hereditary haemorrhagic telangiectasia. Thorax 2008; 63: 259–266. [DOI] [PubMed] [Google Scholar]
- 5.NHS Choices: hereditary haemorrhagic telangiectasia (HHT): available from www.nhs.uk/conditions/hereditary-hemorrhagic-telangiectasia/Pages/Introduction.aspx Date last accessed: November 30, 2016. Date last updated: February 2, 2015.
- 6.Shovlin CL, Sodhi V, McCarthy A, et al. Estimates of maternal risks of pregnancy for women with hereditary haemorrhagic telangiectasia (Osler–Weber–Rendu syndrome): suggested approach for obstetric services. BJOG 2008; 115: 1108–1115. [DOI] [PubMed] [Google Scholar]
- 7.Stringer CJ, Stanley AL, Bates RC, et al. Pulmonary arteriovenous fistula. Am J Surg. 1955; 89: 1054–1080. [DOI] [PubMed] [Google Scholar]
- 8.Gossage JR, Kanj G. Pulmonary arteriovenous malformations. A state of the art review. Am J Respir Crit Care Med 1998; 158: 643–661. [DOI] [PubMed] [Google Scholar]
- 9.Shovlin CL, Letarte M. Hereditary haemorrhagic telangiectasia and pulmonary arteriovenous malformations: issues in clinical management and review of pathogenic mechanisms. Thorax 1999; 54: 714–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peacock AJ, Murphy NF, McMurray JJV, et al. An epidemiological study of pulmonary arterial hypertension. Eur Respir J 2007; 30: 4–9. [DOI] [PubMed] [Google Scholar]