Summary
Background
The Global Burden of Diseases, Injuries, and Risk Factors Study 2015 provides an up-to-date synthesis of the evidence for risk factor exposure and the attributable burden of disease. By providing national and subnational assessments spanning the past 25 years, this study can inform debates on the importance of addressing risks in context.
Methods
We used the comparative risk assessment framework developed for previous iterations of the Global Burden of Disease Study to estimate attributable deaths, disability-adjusted life-years (DALYs), and trends in exposure by age group, sex, year, and geography for 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks from 1990 to 2015. This study included 388 risk-outcome pairs that met World Cancer Research Fund-defined criteria for convincing or probable evidence. We extracted relative risk and exposure estimates from randomised controlled trials, cohorts, pooled cohorts, household surveys, census data, satellite data, and other sources. We used statistical models to pool data, adjust for bias, and incorporate covariates. We developed a metric that allows comparisons of exposure across risk factors—the summary exposure value. Using the counterfactual scenario of theoretical minimum risk level, we estimated the portion of deaths and DALYs that could be attributed to a given risk. We decomposed trends in attributable burden into contributions from population growth, population age structure, risk exposure, and risk-deleted cause-specific DALY rates. We characterised risk exposure in relation to a Socio-demographic Index (SDI).
Findings
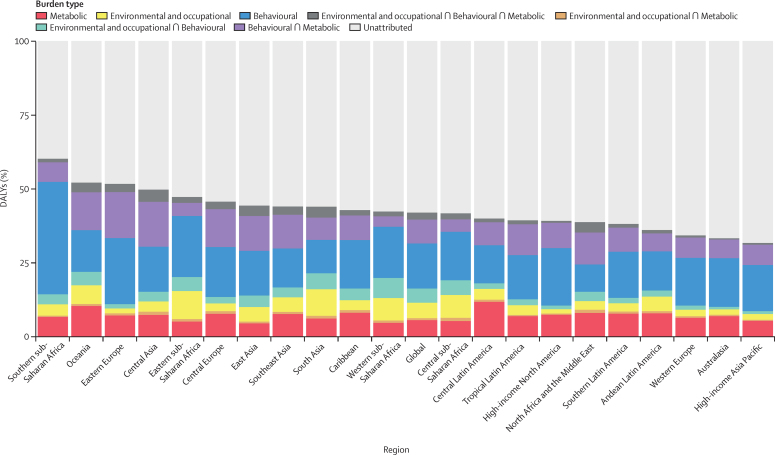
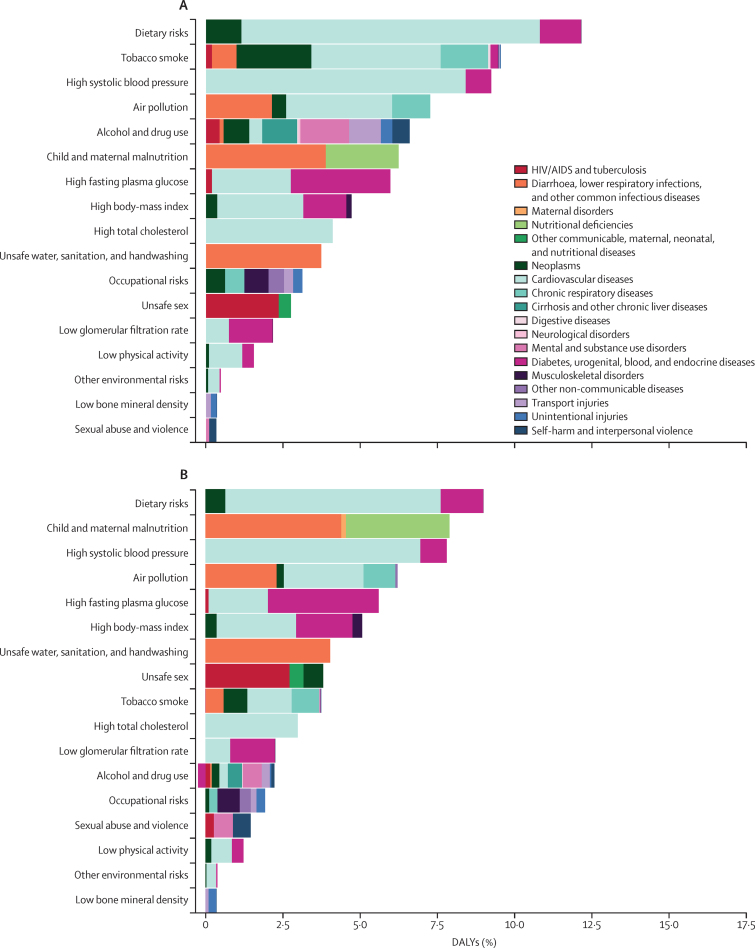
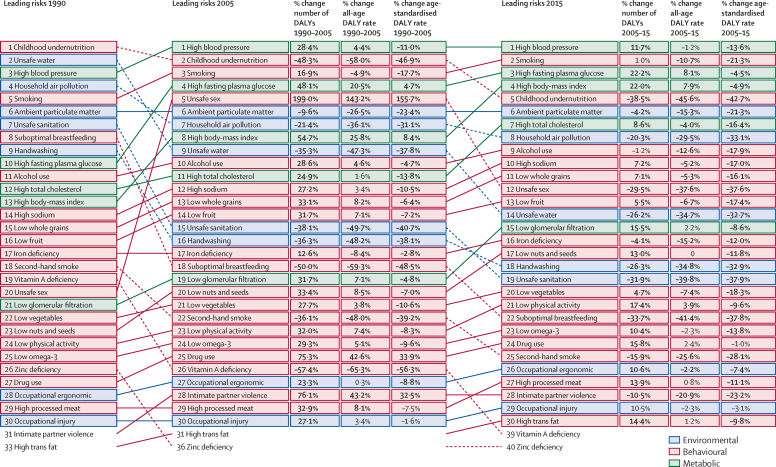
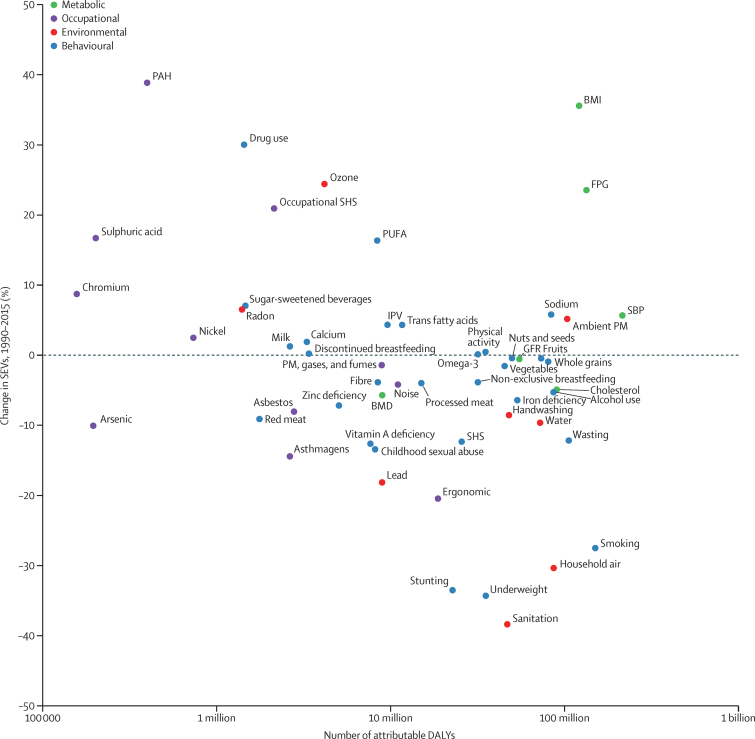
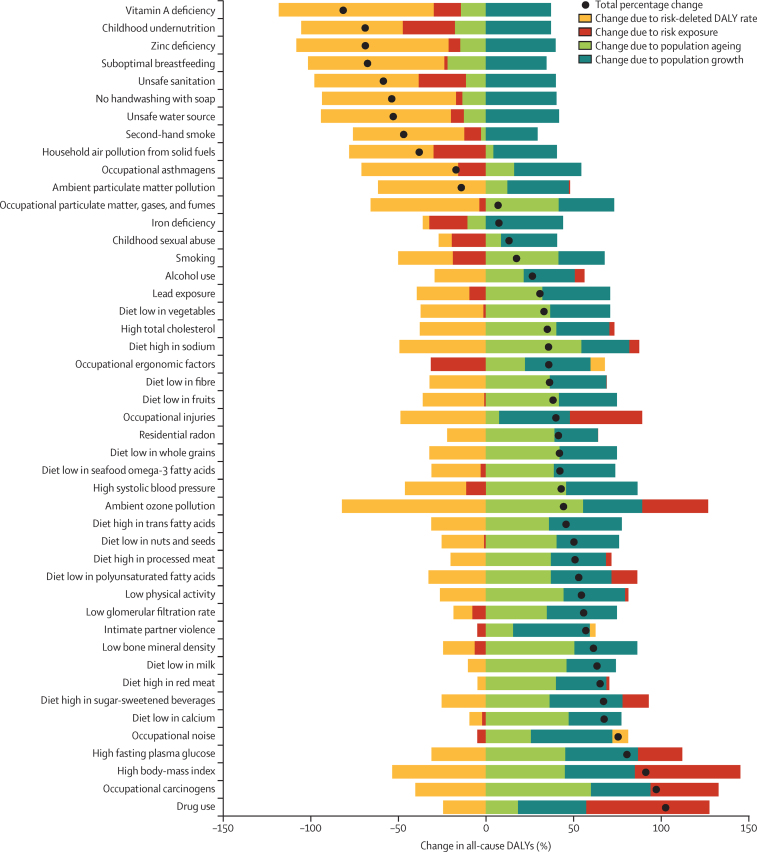
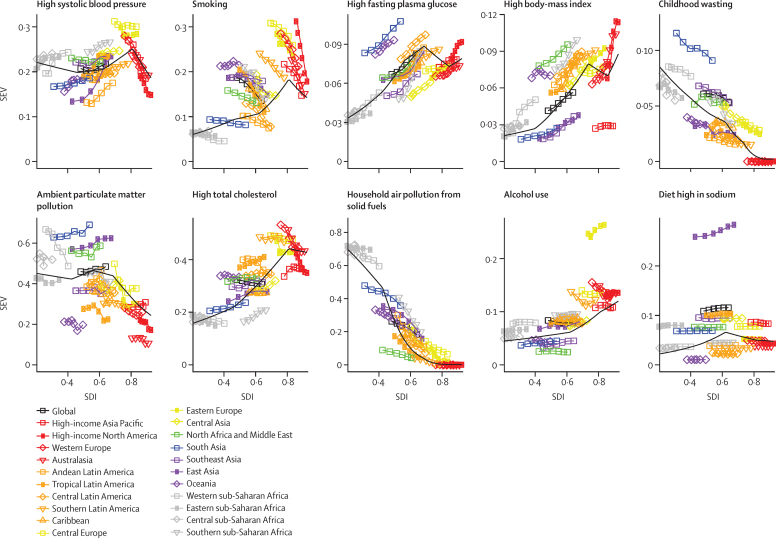
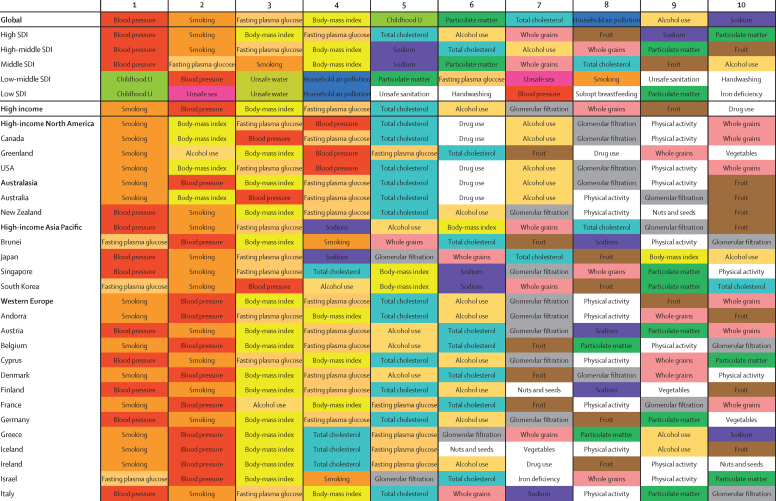
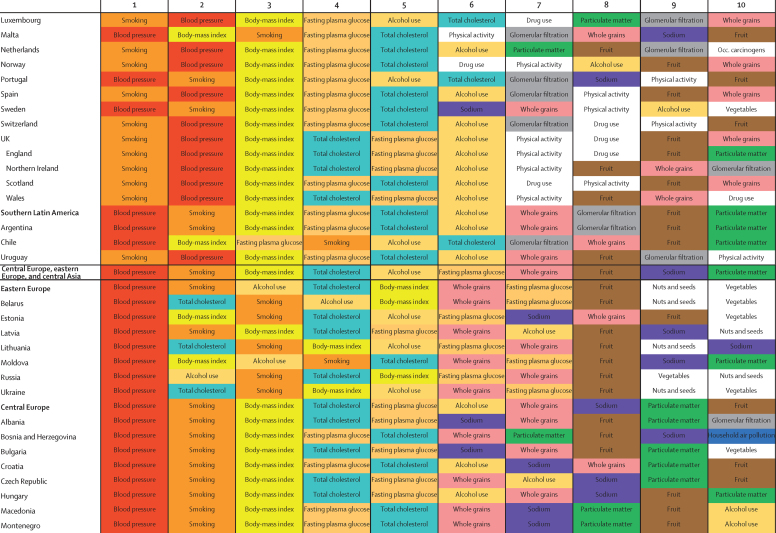
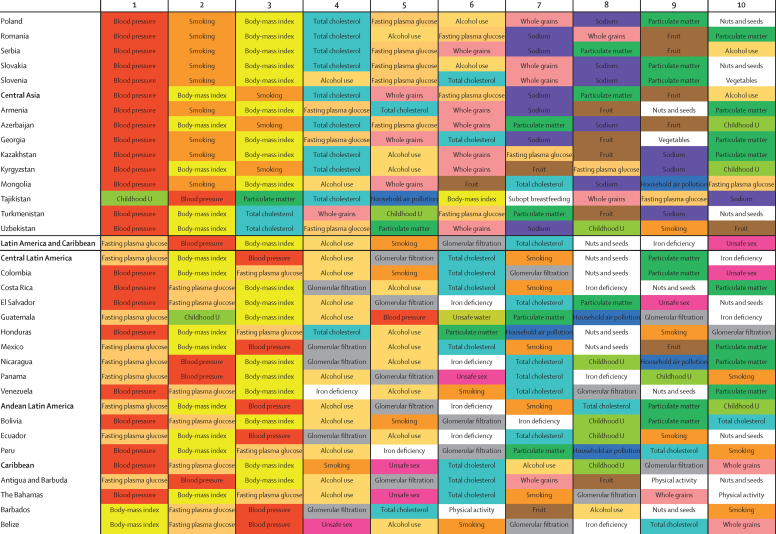
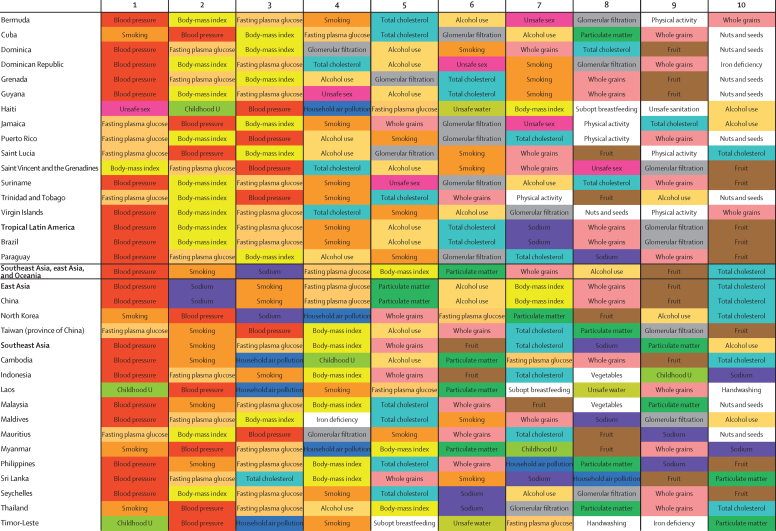
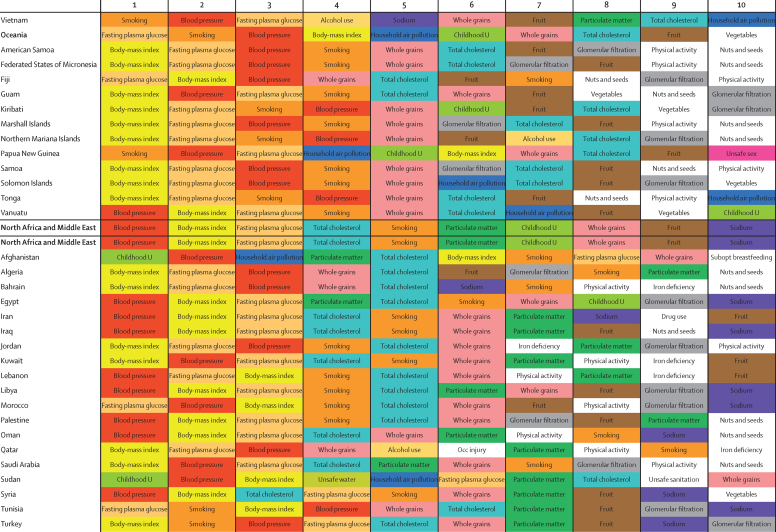
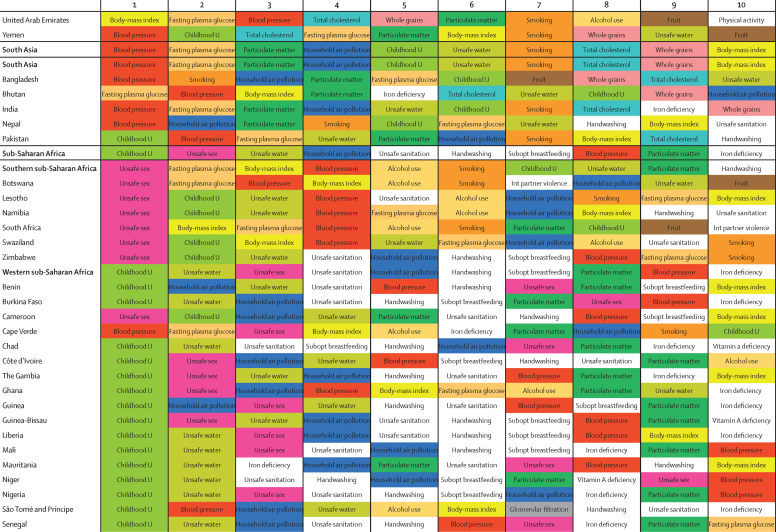
Between 1990 and 2015, global exposure to unsafe sanitation, household air pollution, childhood underweight, childhood stunting, and smoking each decreased by more than 25%. Global exposure for several occupational risks, high body-mass index (BMI), and drug use increased by more than 25% over the same period. All risks jointly evaluated in 2015 accounted for 57·8% (95% CI 56·6–58·8) of global deaths and 41·2% (39·8–42·8) of DALYs. In 2015, the ten largest contributors to global DALYs among Level 3 risks were high systolic blood pressure (211·8 million [192·7 million to 231·1 million] global DALYs), smoking (148·6 million [134·2 million to 163·1 million]), high fasting plasma glucose (143·1 million [125·1 million to 163·5 million]), high BMI (120·1 million [83·8 million to 158·4 million]), childhood undernutrition (113·3 million [103·9 million to 123·4 million]), ambient particulate matter (103·1 million [90·8 million to 115·1 million]), high total cholesterol (88·7 million [74·6 million to 105·7 million]), household air pollution (85·6 million [66·7 million to 106·1 million]), alcohol use (85·0 million [77·2 million to 93·0 million]), and diets high in sodium (83·0 million [49·3 million to 127·5 million]). From 1990 to 2015, attributable DALYs declined for micronutrient deficiencies, childhood undernutrition, unsafe sanitation and water, and household air pollution; reductions in risk-deleted DALY rates rather than reductions in exposure drove these declines. Rising exposure contributed to notable increases in attributable DALYs from high BMI, high fasting plasma glucose, occupational carcinogens, and drug use. Environmental risks and childhood undernutrition declined steadily with SDI; low physical activity, high BMI, and high fasting plasma glucose increased with SDI. In 119 countries, metabolic risks, such as high BMI and fasting plasma glucose, contributed the most attributable DALYs in 2015. Regionally, smoking still ranked among the leading five risk factors for attributable DALYs in 109 countries; childhood underweight and unsafe sex remained primary drivers of early death and disability in much of sub-Saharan Africa.
Interpretation
Declines in some key environmental risks have contributed to declines in critical infectious diseases. Some risks appear to be invariant to SDI. Increasing risks, including high BMI, high fasting plasma glucose, drug use, and some occupational exposures, contribute to rising burden from some conditions, but also provide opportunities for intervention. Some highly preventable risks, such as smoking, remain major causes of attributable DALYs, even as exposure is declining. Public policy makers need to pay attention to the risks that are increasingly major contributors to global burden.
Funding
Bill & Melinda Gates Foundation.
Research in context.
Evidence before this study
The most recent assessment of attributable deaths and disability-adjusted life-years (DALYs) at the global, regional, and national level was the Global Burden of Diseases, Injuries, and Risk Factors Study 2013, which covered 79 risk factors or combinations of risks from 1990 to 2013 in 188 countries.
Added value of this study
This study (the Global Burden of Diseases, Injuries, and Risk Factors Study 2015) incorporates recently published studies, newly acquired data for exposure to relative risks, and new risk-outcome pairs meeting study inclusion criteria. To enhance transparency of the supporting evidence, we provided an assessment of the strength of evidence supporting causality for all 388 risk-outcome pairs. For the first time, we separately assessed trends in risk exposure by computing a summary exposure value, which allows comparisons over time and across place for dichotomous, polytomous, and continuous risks. Quantification of exposure trends allowed decomposition of trends in attributable DALYs into the portion contributed by changes in population growth, population structure, exposure, and risk-deleted DALY rates. We found that reductions in exposure have been key drivers of change for only a small set of environmental risks, including sanitation, household air pollution, and behavioural risks (eg, undernutrition and smoking). For many risks, trends in attributable DALYs have been driven by the interplay between population growth, ageing, and declines in risk-deleted DALY rates. For some risks, including body-mass index, fasting plasma glucose, occupational exposure to carcinogens, and drug use, exposure is increasing and driving up attributable burden. Although an average risk transition has occurred as countries move through the development continuum, many risks initially increase and then decline at the highest development levels. We document leading risks for each country and territory included in the study.
Implications of all the available evidence
Risk assessments allow identification of several groups of risk factors that deserve policy attention. Risks such as smoking, unsafe sanitation, and childhood undernutrition still cause many attributable DALYs, but recent trends show that exposure can be reduced. This assessment of risk also shows many large global risks for which changes in exposure are slow, such as high systolic blood pressure, ambient air pollution, diets high in sodium, high cholesterol, and alcohol intake, highlighting huge opportunities for intervention. Two large risks—high BMI and high fasting plasma glucose—have particularly large and concerning increases in exposure.
Introduction
Analysis of the causes of poor health—specifically, the connections between risk factors and development of poor health—can provide insights into opportunities and priorities for prevention, research, policy, and development. One of the mainstays of modern epidemiology is quantification of elevated risks for particular diseases or injuries from exposure to a given risk factor for groups of individuals. Quantification of elevated risk for exposed groups of individuals from an array of risk-outcome pairs is important to inform decision making on individual health; however, public policy debates require the comprehensive metric of population-level risk, which is a function of elevated risk in the exposed population and the fraction of the population exposed to a given risk. Efforts to measure population risk have combined data for excess risk with the number of individuals exposed to provide comparative quantification of different health risks for populations that have been influential in establishment of policy priorities.1, 2
The comparative risk assessment (CRA) approach developed for the Global Burden of Diseases, Injuries, and Risk Factors (GBD) Study3, 4 provides an overarching conceptual framework for population risk assessment across risks and over time. The scale of the GBD Study required extensive work to develop exposure metrics, assess relationships, and compile health data from different parts of the world with differing levels of metadata and uncertainty, and the unique contribution of this work has been broadly recognised.5, 6, 7 A robust debate on specific risks and results emerged after publication of the Global Burden of Diseases, Injuries, and Risk Factors Study 2013 (GBD 2013).8 Inclusion and exclusion of particular risks and outcomes;3, 4, 9 the optimum targets for indicators such as high systolic blood pressure,10, 11 cholesterol,11, 12 diets high in sodium,13 and air pollution;4, 14 and the certainty of some dietary components of risk8, 15 were challenged, in addition to some details of methods. Underlying many of these discussions were heterogeneities in the strength of causal evidence for different risk-outcome pairs.8
The Global Burden of Diseases, Injuries, and Risk Factors Study 2015 (GBD 2015) CRA, in addition to updating data and methods, adds new transparency about the evidence supporting causal connections for each of the 388 risk-outcome pairs included in the analysis, allows the quantification and reporting of levels and trends in exposure, decomposes changes in attributable burden into population growth, ageing, risk exposure, and risk-deleted disability-adjusted life-year (DALY) rates, and examines how risks change with development. As with all iterations of the GBD Study, GBD 2015 results presented here supersede all previously published GBD CRA estimates.
Methods
Overview
The CRA conceptual framework was developed by Murray and Lopez,16 who established a causal web of hierarchically organised risks or causes that contribute to health outcomes (methods appendix p 161), which allows quantification of risks or causes at any level in the framework. In GBD 2015, as in previous iterations of the GBD Study, we evaluated a set of behavioural, environmental and occupational, and metabolic risks, where risk-outcome pairs were included based on evidence rules (methods appendix p 161). These risks were organised into four hierarchical levels, described in table 1. To date, we have not quantified the contribution of other classes of risk factors (methods appendix p 161); however, using an analysis of the relationship between risk exposures and development, measured with use of the Socio-demographic Index (SDI), we provide some insights into the potential magnitude of distal social, cultural, and economic factors.
Table 1.
Global Burden of Disease 2015 risk factor hierarchy, exposure definitions, theoretical minimum risk exposure level, and data representativeness index for 1985–2015, pre-2005, and 2005–15
| Exposure definition | Theoretical minimum risk exposure level |
Data representativeness index |
||||||
|---|---|---|---|---|---|---|---|---|
| <2005 | 2005–15 | Total | ||||||
| All risk factors | .. | .. | 100·0% | 100·0% | 100·0% | |||
| Environmental and occupational risks | .. | .. | 100·0% | 100·0% | 100·0% | |||
| Unsafe water, sanitation, and handwashing | .. | .. | 73·2% | 60·6% | 78·8% | |||
| Unsafe water source | Proportion of households with access to different water sources (unimproved, improved except piped, piped water supply) and reported use of household water treatment methods (boiling or filtering; chlorinating or solar filtering; no treatment) | All households have access to water from a piped water supply that is also boiled or filtered before drinking | 83·5% | 70·1% | 88·4% | |||
| Unsafe sanitation | Proportion of households with access to different sanitation facilities (unimproved, improved except sewer, sewer connection) | All households have access to toilets with sewer connection | 83·5% | 69·5% | 88·4% | |||
| No handwashing with soap | Proportion of individuals who wash their hands with soap and water after potential faecal contact | All individuals wash hands with soap and water after potential faecal contact | 7·6% | 24·2% | 27·3% | |||
| Air pollution | .. | .. | 100·0% | 100·0% | 100·0% | |||
| Ambient particulate matter pollution | Annual average daily exposure to outdoor air concentrations of PM with an aerodynamic diameter smaller than 2·5 μm, measured in μg/m3 | Uniform distribution between 2·4 μg/m3 and 5·9 μg/m3 | 100·0% | 100·0% | 100·0% | |||
| Household air pollution from solid fuels | Annual average daily exposure to household concentrations of PM with an aerodynamic diameter smaller than 2·5 μm, measured in μg/m3 from solid fuel use (coal, wood, charcoal, dung, and agricultural residues) | No households are exposed to excess indoor concentration of particles from solid fuel use (assuming concentration of particulate matters, aerodynamic diameter smaller than 2·5 μm, measured in μg/m3 in no fuel use is consistent with a theoretical minimum risk level of 2·4–5·9) | 69·7% | 60·6% | 75·8% | |||
| Ambient ozone pollution | Seasonal (3 month) hourly maximum ozone concentrations, measured in ppb | Uniform distribution between 33·3 μg/m3 and 41·9 μg/m3, according to minimum/5th percentile concentrations | 100·0% | 100·0% | 100·0% | |||
| Other environmental risks | .. | .. | 44·9% | 40·9% | 47·0% | |||
| Residential radon | Average daily exposure to indoor air radon levels measured in becquerels (radon disintegrations per s) per cubic metre (Bq/m3) | 10 Bq/m3, corresponding to the outdoor concentration of radon | 36·4% | 36·4% | 36·4% | |||
| Lead exposure | Blood lead levels in μg/dL of blood, bone lead levels in μg/g of bone | 2 μg/dL, corresponding to lead levels in preindustrial humans as natural sources of lead prevent the feasibility of zero exposure | 33·3% | 19·2% | 36·9% | |||
| Occupational risks | .. | .. | 94·4% | 93·4% | 94·4% | |||
| Occupational carcinogens | 94·4% | 93·4% | 94·4% | |||||
| Occupational exposure to asbestos | Proportion of the population with cumulative exposure to asbestos | No occupational exposure to asbestos | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to arsenic | Proportion of the population ever exposed to arsenic at work/through their occupation | No occupational exposure to arsenic | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to benzene | Proportion of the population ever exposed to benzene at work/through their occupation | No occupational exposure to benzene | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to beryllium | Proportion of the population ever exposed to beryllium at work/through their occupation | No occupational exposure to beryllium | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to cadmium | Proportion of the population ever exposed to cadmium at work/through their occupation | No occupational exposure to cadmium | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to chromium | Proportion of the population ever exposed to chromium at work/through their occupation | No occupational exposure to chromium | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to diesel engine exhaust | Proportion of the population ever exposed to diesel engine exhaust at work/through their occupation | No occupational exposure to diesel engine exhaust | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to second-hand smoke | Proportion of the population ever exposed to second-hand smoke at work/through their occupation | No occupational exposure to second-hand smoke | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to formaldehyde | Proportion of the population ever exposed to formaldehyde at work/through their occupation | No occupational exposure to formaldehyde | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to nickel | Proportion of the population ever exposed to nickel at work/through their occupation | No occupational exposure to nickel | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to polycyclic aromatic hydrocarbons | Proportion of the population ever exposed to polycyclic aromatic hydrocarbons at work/through their occupation | No occupational exposure to polycyclic aromatic hydrocarbons | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to silica | Proportion of the population ever exposed to silica at work/through their occupation | No occupational exposure to silica | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to sulphuric acid | Proportion of the population ever exposed to sulphuric acid at work/through their occupation | No occupational exposure to sulphuric acid | 94·4% | 93·4% | 94·4% | |||
| Occupational exposure to trichloroethylene | Proportion of the population ever exposed to trichloroethylene at work/through their occupation | No occupational exposure to trichloroethylene | 94·4% | 93·4% | 94·4% | |||
| Occupational asthmagens | Proportion of the population currently exposed to asthmagens at work/through their occupation | Background asthmagen exposures | 94·4% | 93·4% | 94·4% | |||
| Occupational particulate matter, gases, and fumes | Proportion of the population ever exposed to particulates, gases, or fumes at work/through their occupation | No occupational exposure to particulates, gases, or fumes | 94·4% | 93·4% | 94·4% | |||
| Occupational noise | Proportion of the population ever exposed to noise greater than 85 decibels at work/through their occupation | Background noise exposure | 94·4% | 93·4% | 94·4% | |||
| Occupational injuries | Proportion of the population at risk of injuries related to work/through their occupation | The rate of injury deaths per 100 000 person-years is zero | 24·2% | 32·3% | 35·4% | |||
| Occupational ergonomic factors | Proportion of the population who are exposed to ergonomic risk factors for low back pain at work/through their occupation | All individuals have the ergonomic factors of clerical and related workers | 94·4% | 93·4% | 94·4% | |||
| Behavioural risks | .. | .. | 100·0% | 100·0% | 100·0% | |||
| Child and maternal malnutrition | .. | .. | 93·9% | 91·4% | 93·9% | |||
| Suboptimal breastfeeding | 70·7% | 57·6% | 77·8% | |||||
| Non-exclusive breastfeeding | Proportion of children younger than 6 months who receive predominant, partial, or no breastfeeding | All children are exclusively breastfed for first 6 months of life | 70·7% | 57·6% | 77·8% | |||
| Discontinued breastfeeding | Proportion of children aged 6–23 months who do not receive any breastmilk | All children continue to receive breastmilk until 2 years of age | 68·1% | 65·3% | 79·2% | |||
| Childhood undernutrition | 77·8% | 61·6% | 79·3% | |||||
| Childhood underweight | Proportion of children less than −3 SDs, −3 to −2 SDs, and −2 to −1 SDs of the WHO 2006 standard weight-for-age curve | All children are above −1 SD of the WHO 2006 standard weight-for-age curve | 77·3% | 61·6% | 78·8% | |||
| Childhood wasting | Proportion of children less than −3 SDs, −3 to −2 SDs, and −2 to −1 SDs of the WHO 2006 standard weight-for-length curve | All children are above −1 SD of the WHO 2006 standard weight-for-height curve | 75·8% | 61·1% | 79·3% | |||
| Childhood stunting | Proportion of children less than −3 SDs, −3 to −2 SDs, and −2 to −1 SDs of the WHO 2006 standard height-for-age curve | All children are above −1 SD of the WHO 2006 standard height-for-height curve | 92·3% | 79·6% | 93·7% | |||
| Iron deficiency | Peripheral blood haemoglobin concentration in g/L | Country specific | 66·8% | 30·7% | 68·3% | |||
| Vitamin A deficiency | Proportion of children aged 28 days to 5 years with serum retinol concentration <0·7 μmol/L | No childhood vitamin A deficiency | 38·9% | 5·1% | 40·9% | |||
| Zinc deficiency | Proportion of the population with inadequate zinc intake versus loss | No inadequate zinc intake | 84·3% | 84·3% | 84·3% | |||
| Tobacco smoke | .. | .. | 87·9% | 94·4% | 97·0% | |||
| Smoking | Proportion of the population with cumulative exposure to tobacco smoking; proportion of the population who currently smoke | 100% of population are lifelong non-smokers | 84·8% | 92·4% | 95·5% | |||
| Second-hand smoke | Average daily exposure to indoor air PM from second-hand smoke with an aerodynamic diameter smaller than 2·5 μg, measured in μg/m3 | No second-hand smoke exposure | 58·6% | 79·8% | 86·4% | |||
| Alcohol and drug use | .. | .. | 100·0% | 100·0% | 100·0% | |||
| Alcohol use | Average daily alcohol consumption of pure alcohol (measured in g/day) in current drinkers who had consumed alcohol during the past 12 months; binge drinking: proportion of the population reporting binge consumption of at least 60 g for males and 48 g for females of pure alcohol on a single occasion | No alcohol consumption | 100·0% | 100·0% | 100·0% | |||
| Drug use | Proportion of the population dependent on opioids, cannabis, cocaine, or amphetamines; proportion of the population who have ever injected drugs | No use | 26·3% | 49·0% | 50·0% | |||
| Dietary risks | .. | .. | 90·4% | 92·4% | 92·9% | |||
| Diet low in fruits | Average daily consumption of fruits (fresh, frozen, cooked, canned, or dried, excluding fruit juices and salted or pickled fruits) | Consumption of fruit between 200 g and 300 g per day | 88·9% | 88·9% | 88·9% | |||
| Diet low in vegetables | Average daily consumption of vegetables (fresh, frozen, cooked, canned or dried vegetables including legumes but excluding salted or pickled vegetables, juices, nuts and seeds, and starchy vegetables such as potatoes or corn) | Consumption of vegetables between 340 g and 500 g per day | 88·9% | 88·9% | 88·9% | |||
| Diet low in whole grains | Average daily consumption of whole grains (bran, germ, and endosperm in their natural proportion) from breakfast cereals, bread, rice, pasta, biscuits, muffins, tortillas, pancakes, and other sources | Consumption of whole grains between 100 g and 150 g per day | 10·6% | 9·1% | 16·2% | |||
| Diet low in nuts and seeds | Average daily consumption of nut and seed foods | Consumption of nuts and seeds between 16 g and 25 g per day | 88·9% | 88·9% | 88·9% | |||
| Diet low in milk | Average daily consumption of milk, including non-fat, low-fat, and full-fat milk, excluding soy milk and other plant derivatives | Consumption of milk between 350 g and 520 g per day | 88·9% | 88·9% | 88·9% | |||
| Diet high in red meat | Average daily consumption of red meat (beef, pork, lamb, and goat but excluding poultry, fish, eggs, and all processed meats) | Consumption of red meat between 18 g and 27 g per day | 88·9% | 88·9% | 88·9% | |||
| Diet high in processed meat | Average daily consumption of meat preserved by smoking, curing, salting, or addition of chemical preservatives | Consumption of processed meat between 0 g and 4 g per day | 22·2% | 11·6% | 27·3% | |||
| Diet high in sugar-sweetened beverages | Average daily consumption of beverages with ≥50 kcal per 226·8 g serving, including carbonated beverages, sodas, energy drinks, and fruit drinks, but excluding 100% fruit and vegetable juices | Consumption of sugar-sweetened beverages between 0 g and 5 g per day | 22·2% | 12·6% | 26·8% | |||
| Diet low in fibre | Average daily intake of fibre from all sources, including fruits, vegetables, grains, legumes, and pulses | Consumption of fibre between 19 g and 28 g per day | 88·9% | 88·9% | 88·9% | |||
| Diet low in calcium | Average daily intake of calcium from all sources, including milk, yogurt, and cheese | Consumption of calcium between 1·00 g and 1·50 g per day | 88·9% | 88·9% | 88·9% | |||
| Diet low in seafood omega-3 fatty acids | Average daily intake of eicosapentaenoic acid and docosahexaenoic acid | Consumption of seafood omega-3 fatty acids between 200 mg and 300 mg per day | 88·9% | 88·9% | 88·9% | |||
| Diet low in polyunsaturated fatty acids | Average daily intake of omega-6 fatty acids from all sources, mainly liquid vegetable oils, including soybean oil, corn oil, and safflower oil | Consumption of polyunsaturated fatty acids between 9% and 13% of total daily energy | 88·9% | 88·9% | 88·9% | |||
| Diet high in trans fatty acids | Average daily intake of trans fat from all sources, mainly partially hydrogenated vegetable oils and ruminant products | Consumption of trans fatty acids between 0% and 1% of total daily energy | 39·9% | 39·4% | 39·9% | |||
| Diet high in sodium | 24 h urinary sodium measured in g per day | 24 h urinary sodium between 1 g and 5 g per day | 28·8% | 13·1% | 32·3% | |||
| Sexual abuse and violence | .. | .. | 43·9% | 59·1% | 66·2% | |||
| Childhood sexual abuse | Proportion of the population who have ever experienced one or more acts of childhood sexual abuse, defined as the experience with an older person of unwanted non-contact, contact abuse, or intercourse, when aged 15 years or younger | No childhood sexual abuse | 27·8% | 19·7% | 34·3% | |||
| Intimate partner violence | Proportion of the population who have ever experienced one or more acts of physical or sexual violence by a present or former intimate partner since age 15 years | No intimate partner violence | 41·9% | 56·6% | 63·6% | |||
| Unsafe sex | Proportion of the population with exposure to sexual encounters that convey the risk of disease | No exposure to a disease agent through sex | 17·7% | 48·0% | 48·0% | |||
| Low physical activity | Average weekly physical activity at work, at home, transport related, and recreational measured by MET min per week | Highly active, ≥8000 MET min per week | 45·5% | 50·5% | 66·7% | |||
| Metabolic risks | .. | .. | 83·8% | 88·4% | 93·9% | |||
| High fasting plasma glucose | Serum fasting plasma glucose measured in mmol/L | 4·8–5·4 | 46·0% | 60·1% | 71·2% | |||
| High total cholesterol | Serum total cholesterol, measured in mmol/L | 2·78–3·38 | 49·5% | 48·5% | 69·2% | |||
| High systolic blood pressure | Systolic blood pressure, measured in mm Hg | 110–115 | 55·1% | 66·2% | 79·3% | |||
| High body-mass index | Body-mass index, measured in kg/m2 | 20–25 | 78·3% | 83·3% | 90·9% | |||
| Low bone mineral density | Standardised mean bone mineral density values measured at the femoral neck in g/cm2 | 99th percentile of NHANES 2005–10 by age and sex | 23·7% | 11·1% | 25·8% | |||
| Low glomerular filtration rate | Proportion of the population with a glomerular filtration rate <60 mL/min per 1·73 m2, and excluding end-stage renal disease | >60 mL/min per 1·73 m2 | 9·1% | 17·2% | 20·2% | |||
The percentage of available data is calculated out of a total of 519 subnational Level 2 geographies. PM=particulate matter. ppb=parts per billion. MET=metabolic equivalent. NHANES=National Health and Nutrition Examination Survey.
Two types of risk assessments are possible within the CRA framework: attributable burden and avoidable burden. Attributable burden is the reduction in current disease burden that would have been possible if past population exposure had shifted to an alternative or counterfactual distribution of risk exposure. Avoidable burden is the potential reduction in future disease burden that could be achieved by changing the current distribution of exposure to a counterfactual distribution of exposure. Murray and Lopez16 identified four types of counterfactual exposure distributions: theoretical, plausible, feasible, and cost-effective minimum risk. In GBD studies to date and in this study, we focus on attributable burden using the theoretical minimum risk level (TMREL), which is the level of risk exposure that minimises risk at the population level, or the level of risk that captures the maximum attributable burden.
Overall, this analysis follows the CRA methods used in GBD 2013.4 The methods described in this study provide a high-level overview of the analytical logic, with a focus on areas of notable change from the methods used in GBD 2013, with details provided in the methods appendix. This study complies with the Guidelines for Accurate and Transparent Health Estimates Reporting statement (methods appendix pp 177–79).17
Geographic units of analysis and years for estimation
In the GBD framework, geographies have been arranged as a set of hierarchical categories: seven super-regions, 21 regions nested within the seven super-regions, and 195 countries and territories nested in the 21 regions. Additionally, GBD collaborator interest and availability of data resulted in an expansion of countries for which we disaggregate our estimates at the subnational level. At the first level of subnational division, 256 geographic units are included in GBD 2015. For this study, we present results for the 195 national and territory-level geographies. We produced a complete set of age-specific, sex-specific, cause-specific, and location-specific estimates of risk factor exposure and attributable burden for 1990, 1995, 2000, 2005, 2010, and 2015 for included risk factors. Results presented in this study emphasise results for 1990, 2005, and 2015; online data visualisations provide access to results for all GBD metrics from 1990 to 2015.
Attributable burden formula
Four key components are included in estimation of the burden attributable to a given risk factor: the metric of burden being assessed (number of deaths, years of life lost [YLLs], years lived with disability [YLDs], or DALYs [the sum of YLLs and YLDs]), the exposure levels for a risk factor, the relative risk of a given outcome due to exposure, and the counterfactual level of risk factor exposure. Estimates of attributable DALYs for a risk-outcome pair are equal to DALYs for the outcome multiplied by the population attributable fraction (PAF) for the risk-outcome pair for a given age, sex, location, and year. A similar logic applies for estimation of attributable deaths, YLLs, or YLDs. Risks are categorised on the basis of how exposure was measured: dichotomous, polytomous, and continuous. The PAF represents the proportion of risk that would be reduced in a given year if the exposure to a risk factor in the past were reduced to a counterfactual level of exposure (methods appendix p 27).
Causal evidence for risk-outcome pairs
In this study, as in GBD 2013, we have included risk-outcome pairs that we have assessed as meeting the World Cancer Research Fund grades of convincing or probable evidence (methods appendix pp 12–13 contains definitions of these grades).9 Table 2 provides a summary of the evidence supporting a causal relationship between a risk and an outcome for each pair included in GBD 2015. For each risk-outcome pair, we used recent systematic reviews to identify independent prospective studies (randomised controlled trials, non-randomised interventions, and cohorts) that evaluated the putative relationship. For risk-outcome pairs for which no recent systematic review was available, we either updated reviews developed for GBD 2013 or did a new systematic search of literature (methods appendix pp 44–159). Table 2 summarises the evidence using multiple dimensions, which supports our assessment that each included risk-outcome pair meets the criteria of convincing or probable evidence (methods appendix [pp 12–13] contains a justification of the criteria presented to support causality). In this summary of evidence, we have focused on randomised controlled trials and prospective observational studies, along with supporting evidence, like dose-response relationships and biologically plausible mechanisms. Other evidence supporting causal connections, such as case-control studies, are not summarised in table 2.
Table 2.
Epidemiological evidence supporting causality for risk-outcome pairs included in the Global Burden of Disease study 2015
| Outcome | RCTs (n) | RCTs with significant effect in the opposite direction (%) | RCTs with null findings (%) | Prospective observational studies (n)* | Prospective observational studies with significant association in the opposite direction (%) | Lower limit of RR >1·5 | Dose-response relationship | Biological plausibility† | Analogy‡ | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Unsafe water, sanitation, and handwashing | |||||||||||
| Unsafe water source: chlorination or solar (point-of-use treatment) | Diarrhoeal diseases | 24 | 0 | 42% | 6 | 0 | Yes | .. | Yes | No | |
| Unsafe water source: filter | Diarrhoeal diseases | 11 | 0 | 45% | 2 | 0 | Yes | .. | Yes | No | |
| Unsafe water source: improved water | Diarrhoeal diseases | 0 | .. | .. | 5 | 0 | Yes | .. | Yes | No | |
| Unsafe water source: improved water | Typhoid fever | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| Unsafe water source: improved water | Paratyphoid fever | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| Unsafe water source: piped | Diarrhoeal diseases | 1 | 0 | 0 | 9 | 11% | Yes | .. | Yes | No | |
| Unsafe water source: piped | Typhoid fever | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| Unsafe water source: piped | Paratyphoid fever | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| Unsafe sanitation: improved sanitation | Diarrhoeal diseases | 0 | .. | .. | 9 | 0 | Yes | .. | Yes | No | |
| Unsafe sanitation: improved sanitation | Typhoid fever | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| Unsafe sanitation: improved sanitation | Paratyphoid fever | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| Unsafe sanitation: piped | Diarrhoeal diseases | 0 | .. | .. | 1 | 0 | Yes | .. | Yes | No | |
| Unsafe sanitation: piped | Typhoid fever | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| Unsafe sanitation: piped | Paratyphoid fever | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| No handwashing with soap | Diarrhoeal diseases | 19 | 0 | 42% | 0 | .. | No | .. | Yes | No | |
| No handwashing with soap | Typhoid fever | 0 | .. | .. | 0 | .. | No | .. | Yes | Yes | |
| No handwashing with soap | Paratyphoid fever | 0 | .. | .. | 0 | .. | No | .. | Yes | Yes | |
| No handwashing with soap | Lower respiratory infections | 1 | 0 | 0 | 6 | 0 | No | .. | Yes | No | |
| Air pollution | |||||||||||
| Ambient particulate matter pollution | Lower respiratory infections | 0 | .. | .. | 13 | 0 | No | Yes | Yes | No | |
| Ambient particulate matter pollution | Ischaemic stroke | 0 | .. | .. | 25 | 0 | No | Yes | Yes | Yes | |
| Ambient particulate matter pollution | Haemorrhagic stroke | 0 | .. | .. | 25 | 0 | No | Yes | Yes | Yes | |
| Ambient particulate matter pollution | Ischaemic heart disease | 0 | .. | .. | 16 | 0 | No | Yes | Yes | Yes | |
| Ambient particulate matter pollution | Chronic obstructive pulmonary disease | 0 | .. | .. | 11 | 0 | No | Yes | Yes | Yes | |
| Ambient particulate matter pollution | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 27 | 0 | No | Yes | Yes | Yes | |
| Household air pollution from solid fuels | Lower respiratory infections | 0 | .. | .. | 0 | .. | No | Yes | Yes | No | |
| Household air pollution from solid fuels | Cataract | 0 | .. | .. | 0 | .. | No | Yes | Yes | No | |
| Household air pollution from solid fuels | Ischaemic stroke | 0 | .. | .. | 25 | 0 | No | Yes | Yes | Yes | |
| Household air pollution from solid fuels | Haemorrhagic stroke | 0 | .. | .. | 25 | 0 | No | Yes | Yes | Yes | |
| Household air pollution from solid fuels | Ischaemic heart disease | 0 | .. | .. | 16 | 0 | No | Yes | Yes | Yes | |
| Household air pollution from solid fuels | Chronic obstructive pulmonary disease | 0 | .. | .. | 0 | .. | No | Yes | Yes | Yes | |
| Household air pollution from solid fuels | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 0 | .. | No | Yes | Yes | Yes | |
| Ambient ozone pollution | Chronic obstructive pulmonary disease | 0 | .. | .. | 4 | 0 | No | Yes | Yes | No | |
| Other environmental risks | |||||||||||
| Residential radon | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 3 | 0 | No | Yes | Yes | No | |
| Lead exposure | Systolic blood pressure | 0 | .. | .. | 3 | 0 | .. | Yes | Yes | .. | |
| Lead exposure | Idiopathic intellectual disability | 0 | .. | .. | 8 | 0 | No | Yes | Yes | No | |
| Occupational risks | |||||||||||
| Occupational exposure to asbestos | Larynx cancer | 0 | .. | .. | 27 | .. | No | .. | Yes | Yes | |
| Occupational exposure to asbestos | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 18 | 0 | Yes | .. | Yes | Yes | |
| Occupational exposure to asbestos | Ovarian cancer | 0 | .. | .. | 15 | 0 | No | .. | Yes | Yes | |
| Occupational exposure to asbestos | Mesothelioma | 0 | .. | .. | 5 | 0 | Yes | .. | Yes | Yes | |
| Occupational exposure to arsenic | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 3 | 0 | No | .. | Yes | No | |
| Occupational exposure to benzene | Leukaemia | 0 | .. | .. | 12 | 0 | Yes | .. | Yes | No | |
| Occupational exposure to beryllium | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 4 | 0 | No | .. | Yes | No | |
| Occupational exposure to cadmium | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 7 | 0 | No | .. | Yes | No | |
| Occupational exposure to chromium | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 26 | 0 | No | .. | Yes | No | |
| Occupational exposure to diesel engine exhaust | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 17 | 0 | No | .. | Yes | No | |
| Occupational exposure to second-hand smoke | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 25 | 0 | No | .. | Yes | No | |
| Occupational exposure to formaldehyde | Nasopharyngeal cancer | 0 | .. | .. | 1 | 0 | No | .. | Yes | Yes | |
| Occupational exposure to formaldehyde | Leukaemia | 0 | .. | .. | 12 | 0 | No | .. | Yes | Yes | |
| Occupational exposure to nickel | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 1 | 0 | No | .. | Yes | No | |
| Occupational exposure to polycyclic aromatic hydrocarbons | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 39 | 0 | No | .. | Yes | No | |
| Occupational exposure to silica | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 17 | 0 | No | .. | Yes | No | |
| Occupational exposure to sulphuric acid | Larynx cancer | 0 | .. | .. | 3 | 0 | Yes | .. | Yes | No | |
| Occupational exposure to trichloroethylene | Kidney cancer | 0 | .. | .. | 20 | 0 | No | .. | Yes | No | |
| Occupational asthmagens | Asthma | 0 | .. | .. | 3 | 0 | No | .. | Yes | No | |
| Occupational particulate matter, gases, and fumes | Chronic obstructive pulmonary disease | 0 | .. | .. | 1 | 0 | No | .. | Yes | No | |
| Occupational noise | Age-related and other hearing loss | 0 | .. | .. | 4 | 0 | Yes | .. | Yes | No | |
| Occupational ergonomic factors | Low back pain | 0 | .. | .. | 10 | 0 | No | .. | Yes | No | |
| Child and maternal malnutrition | |||||||||||
| Non-exclusive breastfeeding | Diarrhoeal diseases | 0 | .. | .. | 5 | 0 | Yes | .. | Yes | No | |
| Non-exclusive breastfeeding | Lower respiratory infections | 0 | .. | .. | 6 | 0 | Yes | .. | Yes | No | |
| Discontinued breastfeeding | Diarrhoeal diseases | 0 | .. | .. | 2 | 0 | No | .. | Yes | No | |
| Childhood underweight | Diarrhoeal diseases | 0 | .. | .. | 7 | .. | Yes | .. | Yes | No | |
| Childhood underweight | Lower respiratory infections | 0 | .. | .. | 7 | .. | Yes | .. | Yes | No | |
| Childhood underweight | Measles | 0 | .. | .. | 7 | .. | Yes | .. | Yes | No | |
| Childhood wasting | Diarrhoeal diseases | 0 | .. | .. | 7 | .. | Yes | .. | Yes | No | |
| Childhood wasting | Lower respiratory infections | 0 | .. | .. | 7 | .. | Yes | .. | Yes | No | |
| Childhood wasting | Measles | 0 | .. | .. | 7 | .. | Yes | .. | Yes | No | |
| Childhood stunting | Diarrhoeal diseases | 0 | .. | .. | 7 | .. | No | .. | Yes | No | |
| Childhood stunting | Lower respiratory infections | 0 | .. | .. | 7 | .. | No | .. | Yes | No | |
| Childhood stunting | Measles | 0 | .. | .. | 7 | .. | No | .. | Yes | No | |
| Iron deficiency | Maternal haemorrhage | 0 | .. | .. | 0 | .. | No | .. | Yes | Yes | |
| Iron deficiency | Maternal sepsis and other pregnancy-related infections | 0 | .. | .. | 0 | .. | No | .. | Yes | Yes | |
| Vitamin A deficiency | Diarrhoeal diseases | 19 | 0 | 63% | 0 | .. | No | .. | Yes | No | |
| Vitamin A deficiency | Measles | 12 | 0 | 83% | 0 | .. | Yes | .. | Yes | No | |
| Zinc deficiency | Diarrhoeal diseases | 14 | 0 | 29% | 0 | .. | No | .. | Yes | No | |
| Zinc deficiency | Lower respiratory infections | 6 | 0 | 17% | 0 | .. | No | .. | Yes | No | |
| Tobacco smoke | |||||||||||
| Smoking | Tuberculosis | 0 | .. | .. | 4 | 0 | No | .. | Yes | Yes | |
| Smoking | Lower respiratory infections | 0 | .. | .. | 0 | .. | No | .. | Yes | Yes | |
| Smoking | Lip and oral cavity cancer | 0 | .. | .. | 3 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Nasopharyngeal cancer | 0 | .. | .. | 3 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Oesophageal cancer | 0 | .. | .. | 5 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Larynx cancer | 0 | .. | .. | 4 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Stomach cancer | 0 | .. | .. | 9 | 0 | No | .. | Yes | Yes | |
| Smoking | Colon and rectum cancer | 0 | .. | .. | 19 | 0 | No | .. | Yes | Yes | |
| Smoking | Liver cancer | 0 | .. | .. | 54 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Pancreatic cancer | 0 | .. | .. | 13 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 38 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Cervical cancer | 0 | .. | .. | 15 | 0 | No | .. | Yes | Yes | |
| Smoking | Kidney cancer | 0 | .. | .. | 8 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Bladder cancer | 0 | .. | .. | 17 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Leukaemia | 0 | .. | .. | 14 | 0 | No | .. | Yes | Yes | |
| Smoking | Ischaemic heart disease | 0 | .. | .. | 86 | .. | No | .. | Yes | Yes | |
| Smoking | Ischemic stroke | 0 | .. | .. | 60 | .. | No | .. | Yes | Yes | |
| Smoking | Haemorrhagic stroke | 0 | .. | .. | 60 | .. | No | .. | Yes | Yes | |
| Smoking | Hypertensive heart disease | 0 | .. | .. | 5 | .. | No | .. | Yes | Yes | |
| Smoking | Atrial fibrillation and flutter | 0 | .. | .. | 16 | 0 | No | .. | Yes | Yes | |
| Smoking | Aortic aneurysm | 0 | .. | .. | 10 | 0 | No | .. | Yes | Yes | |
| Smoking | Peripheral vascular disease | 0 | .. | .. | 10 | 0 | No | .. | Yes | Yes | |
| Smoking | Other cardiovascular and circulatory diseases | 0 | .. | .. | 1 | 0 | No | .. | Yes | Yes | |
| Smoking | Chronic obstructive pulmonary disease | 0 | .. | .. | 42 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Silicosis | 0 | .. | .. | 0 | .. | No | .. | Yes | Yes | |
| Smoking | Asbestosis | 0 | .. | .. | 0 | .. | No | .. | Yes | Yes | |
| Smoking | Coal workers pneumoconiosis | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| Smoking | Other pneumoconiosis | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| Smoking | Asthma | 0 | .. | .. | 6 | 0 | No | .. | Yes | Yes | |
| Smoking | Interstitial lung disease and pulmonary sarcoidosis | 0 | .. | .. | 0 | .. | Yes | .. | Yes | Yes | |
| Smoking | Other chronic respiratory diseases | 0 | .. | .. | 1 | 0 | Yes | .. | Yes | Yes | |
| Smoking | Peptic ulcer disease | 0 | .. | .. | 7 | 0 | No | .. | Yes | No | |
| Smoking | Diabetes mellitus | 0 | .. | .. | 51 | 0 | No | .. | Yes | No | |
| Smoking | Cataract | 0 | .. | .. | 10 | 0 | No | .. | Yes | No | |
| Smoking | Macular degeneration | 0 | .. | .. | 5 | 20% | No | .. | Yes | No | |
| Smoking | Rheumatoid arthritis | 0 | .. | .. | 5 | 0 | No | .. | Yes | No | |
| Smoking | Hip fracture | 0 | .. | .. | 15 | 20% | No | .. | Yes | Yes | |
| Smoking | Non-hip fracture | 0 | .. | .. | 14 | 14% | No | .. | Yes | Yes | |
| Second-hand smoke | Otitis media | 0 | .. | .. | 17 | 0 | No | Yes | Yes | No | |
| Second-hand smoke | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 4 | 0 | No | Yes | Yes | Yes | |
| Second-hand smoke | Ischaemic heart disease | 0 | .. | .. | 4 | 25% | No | Yes | Yes | Yes | |
| Second-hand smoke | Ischaemic stroke | 0 | .. | .. | 10 | 0 | Yes | Yes | Yes | Yes | |
| Second-hand smoke | Haemorrhagic stroke | 0 | .. | .. | 10 | 0 | Yes | Yes | Yes | Yes | |
| Alcohol and drug use | |||||||||||
| Alcohol use | Tuberculosis | 0 | .. | .. | 3 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Lower respiratory infections | 0 | .. | .. | 2 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Lip and oral cavity cancer | 0 | .. | .. | 1 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Nasopharyngeal cancer | 0 | .. | .. | 1 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Other pharyngeal cancer | 0 | .. | .. | 1 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Oesophageal cancer | 0 | .. | .. | 1 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Colon and rectum cancer | 0 | .. | .. | 6 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Liver cancer | 0 | .. | 3 | 0 | No | Yes | Yes | Yes | ||
| Alcohol use | Laryngeal cancer | 0 | .. | .. | 0 | .. | No | Yes | Yes | Yes | |
| Alcohol use | Breast cancer | 0 | .. | .. | 12 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Ischaemic heart disease | 0 | .. | .. | 32 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Ischaemic stroke | 0 | .. | .. | 20 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Haemorrhagic stroke | 0 | .. | .. | 16 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Atrial fibrillation and flutter | 0 | .. | .. | 10 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Hypertensive heart disease | 0 | .. | .. | 2 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Pancreatitis | 0 | .. | .. | 4 | 0 | No | Yes | Yes | No | |
| Alcohol use | Epilepsy | 0 | .. | .. | 0 | .. | No | Yes | Yes | No | |
| Alcohol use | Diabetes mellitus | 0 | .. | .. | 9 | 0 | No | Yes | Yes | No | |
| Alcohol use | Cirrhosis | 0 | .. | .. | 14 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Injuries | 0 | .. | .. | 29 | 0 | No | Yes | Yes | Yes | |
| Alcohol use | Self-harm | 0 | .. | .. | 0 | .. | No | Yes | Yes | Yes | |
| Alcohol use | Interpersonal violence | 0 | .. | .. | 11 | 0 | No | Yes | Yes | Yes | |
| Drug use | Hepatitis B | 0 | .. | .. | 6 | 0 | Yes | .. | Yes | Yes | |
| Drug use | Hepatitis C | 0 | .. | .. | 16 | 0 | Yes | .. | Yes | Yes | |
| Drug use | Self-harm | 0 | .. | .. | 1 | 0 | No | .. | Yes | No | |
| Dietary risks | |||||||||||
| Diet low in fruits | Lip and oral cavity cancer | 0 | .. | .. | 2 | 0 | No | Yes | Yes | Yes | |
| Diet low in fruits | Nasopharyngeal cancer | 0 | .. | .. | 2 | 0 | No | Yes | Yes | Yes | |
| Diet low in fruits | Other pharyngeal cancer | 0 | .. | .. | 2 | 0 | No | Yes | Yes | Yes | |
| Diet low in fruits | Larynx cancer | 0 | .. | .. | 2 | 0 | No | Yes | Yes | Yes | |
| Diet low in fruits | Oesophageal cancer | 0 | .. | .. | 5 | 0 | No | Yes | Yes | Yes | |
| Diet low in fruits | Tracheal, bronchial, and lung cancer | 0 | .. | .. | 22 | 0 | No | Yes | Yes | Yes | |
| Diet low in fruits | Ischaemic heart disease | 0 | .. | .. | 9 | 0 | No | Yes | Yes | Yes | |
| Diet low in fruits | Ischaemic stroke | 0 | .. | .. | 9 | 0 | No | Yes | Yes | Yes | |
| Diet low in fruits | Haemorrhagic stroke | 0 | .. | .. | 5 | 0 | No | Yes | Yes | Yes | |
| Diet low in fruits | Diabetes mellitus | 0 | .. | .. | 9 | 0 | No | Yes | Yes | No | |
| Diet low in vegetables | Oesophageal cancer | 0 | .. | .. | 5 | 0 | No | Yes | Yes | No | |
| Diet low in vegetables | Ischaemic heart disease | 0 | .. | .. | 9 | 0 | No | Yes | Yes | Yes | |
| Diet low in vegetables | Ischaemic stroke | 0 | .. | .. | 8 | 0 | No | Yes | Yes | Yes | |
| Diet low in vegetables | Haemorrhagic stroke | 0 | .. | .. | 5 | 0 | No | Yes | Yes | Yes | |
| Diet low in whole grains | Ischaemic heart disease | 0 | .. | .. | 7 | 0 | No | Yes | Yes | Yes | |
| Diet low in whole grains | Ischaemic stroke | 0 | .. | .. | 6 | 0 | No | Yes | Yes | Yes | |
| Diet low in whole grains | Haemorrhagic stroke | 0 | .. | .. | 6 | 0 | No | Yes | Yes | Yes | |
| Diet low in whole grains | Diabetes mellitus | 0 | .. | .. | 10 | 0 | No | Yes | Yes | No | |
| Diet low in nuts and seeds | Ischaemic heart disease | 1 | 0 | 100% | 6 | 0 | No | Yes | Yes | No | |
| Diet low in nuts and seeds | Diabetes mellitus | 1 | 0 | 100% | 5 | 0 | No | Yes | Yes | No | |
| Diet low in milk | Colon and rectum cancer | 0 | .. | .. | 7 | 0 | No | Yes | Yes | No | |
| Diet high in red meats | Colon and rectum cancer | 0 | .. | .. | 8 | 0 | No | Yes | Yes | No | |
| Diet high in red meats | Diabetes mellitus | 0 | .. | .. | 9 | 11% | No | Yes | Yes | No | |
| Diet high in processed meats | Colon and rectum cancer | 0 | .. | .. | 9 | 11% | No | Yes | Yes | No | |
| Diet high in processed meats | Ischaemic heart disease | 0 | .. | .. | 5 | 0 | No | Yes | Yes | No | |
| Diet high in processed meats | Diabetes mellitus | 0 | .. | .. | 8 | 0 | No | Yes | Yes | No | |
| Diet high in sugar-sweetened beverages | Body-mass index | 10 | 0 | 60% | 22 | 0 | .. | Yes | Yes | .. | |
| Diet low in fibre | Colon and rectum cancer | 0 | .. | .. | 15 | 0 | No | Yes | Yes | No | |
| Diet low in fibre | Ischaemic heart disease | 0 | .. | .. | 12 | 0 | No | Yes | Yes | No | |
| Diet low in calcium | Colon and rectum cancer | 0 | .. | .. | 13 | 0 | No | Yes | Yes | No | |
| Diet low in seafood omega-3 fatty acids | Ischaemic heart disease | 17 | 0 | 88% | 16 | 0 | No | Yes | Yes | No | |
| Diet low in polyunsaturated fatty acids | Ischaemic heart disease | 8 | 0 | 75% | 11 | 0 | No | Yes | Yes | No | |
| Diet high in trans fatty acids | Ischaemic heart disease | 0 | .. | .. | 4 | 0 | No | Yes | Yes | No | |
| Diet high in sodium | Systolic blood pressure | 45 | 0 | 73% | .. | .. | .. | Yes | Yes | .. | |
| Diet high in sodium | Stomach cancer | 0 | .. | .. | 3 | 0 | No | Yes | Yes | No | |
| Sexual abuse and violence | |||||||||||
| Intimate partner violence | HIV/AIDS | 0 | .. | .. | 2 | 0 | No | .. | Yes | No | |
| Intimate partner violence | Maternal abortion, miscarriage, and ectopic pregnancy | 0 | .. | .. | 1 | 0 | Yes | .. | Yes | No | |
| Intimate partner violence | Depressive disorders | 0 | .. | .. | 6 | 0 | No | .. | Yes | Yes | |
| Intimate partner violence | Self-harm | 0 | .. | .. | 2 | 0 | Yes | .. | Yes | Yes | |
| Childhood sexual abuse | Alcohol use disorders | 0 | .. | .. | 4 | 0 | No | .. | Yes | Yes | |
| Childhood sexual abuse | Depressive disorders | 0 | .. | .. | 5 | 0 | No | .. | Yes | Yes | |
| Childhood sexual abuse | Self-harm | 0 | .. | .. | 8 | 0 | No | .. | Yes | Yes | |
| Low physical activity | |||||||||||
| Low physical activity | Colon and rectum cancer | 0 | .. | .. | 20 | 15% | No | Yes | Yes | Yes | |
| Low physical activity | Breast cancer | 0 | .. | .. | 35 | 0 | No | Yes | Yes | Yes | |
| Low physical activity | Ischaemic heart disease | 0 | .. | .. | 45 | 9% | No | Yes | Yes | Yes | |
| Low physical activity | Ischaemic stroke | 0 | .. | .. | 27 | 11% | No | Yes | Yes | Yes | |
| Low physical activity | Diabetes mellitus | 0 | .. | .. | 57 | 7% | No | Yes | Yes | No | |
| Metabolic risks | |||||||||||
| High fasting plasma glucose | Ischaemic heart disease | 8 | 0 | 100% | 150 | .. | Yes | Yes | Yes | Yes | |
| High fasting plasma glucose | Ischaemic stroke | 9 | 0 | 100% | 150 | .. | Yes | Yes | Yes | Yes | |
| High fasting plasma glucose | Haemorrhagic stroke | 9 | 0 | 100% | 150 | .. | Yes | Yes | Yes | Yes | |
| High fasting plasma glucose | Peripheral vascular disease | 14 | .. | .. | 4 | 0 | Yes | Yes | Yes | Yes | |
| High fasting plasma glucose | Tuberculosis | 0 | .. | .. | 17 | 0 | Yes | Yes | Yes | No | |
| High fasting plasma glucose | Chronic kidney disease | 5 | .. | .. | 32 | .. | Yes | Yes | Yes | No | |
| High total cholesterol | Ischaemic heart disease | 21 | 0 | 57% | 88 | .. | Yes | Yes | Yes | Yes | |
| High total cholesterol | Ischaemic stroke | 21 | 0 | 57% | 88 | .. | Yes | Yes | Yes | Yes | |
| High systolic blood pressure | Rheumatic heart disease | 0 | .. | .. | 62 | .. | Yes | Yes | Yes | Yes | |
| High systolic blood pressure | Ischaemic heart disease | 56 | 0 | .. | 88 | .. | Yes | Yes | Yes | Yes | |
| High systolic blood pressure | Ischaemic stroke | 54 | 0 | .. | 150 | .. | Yes | Yes | Yes | Yes | |
| High systolic blood pressure | Haemorrhagic stroke | 54 | 0 | .. | 150 | .. | Yes | Yes | Yes | Yes | |
| High systolic blood pressure | Cardiomyopathy and myocarditis | 0 | .. | .. | 62 | .. | Yes | Yes | Yes | Yes | |
| High systolic blood pressure | Atrial fibrillation and flutter | 20 | 5% | 60% | 88 | .. | Yes | Yes | Yes | Yes | |
| High systolic blood pressure | Aortic aneurysm | 0 | .. | .. | 62 | .. | Yes | Yes | Yes | Yes | |
| High systolic blood pressure | Peripheral vascular disease | 0 | .. | .. | 88 | .. | Yes | Yes | Yes | Yes | |
| High systolic blood pressure | Endocarditis | 0 | .. | .. | 62 | .. | Yes | Yes | Yes | Yes | |
| High systolic blood pressure | Other cardiovascular and circulatory diseases | 0 | .. | .. | 88 | .. | No | Yes | Yes | Yes | |
| High systolic blood pressure | Chronic kidney disease | 8 | .. | .. | 88 | .. | Yes | Yes | Yes | No | |
| High body-mass index | Oesophageal cancer | 0 | .. | .. | 8 | 0 | No | Yes | Yes | Yes | |
| High body-mass index | Colon and rectum cancer | 0 | .. | .. | 38 | 0 | No | Yes | Yes | Yes | |
| High body-mass index | Liver cancer | 0 | .. | .. | 34 | 0 | No | Yes | Yes | Yes | |
| High body-mass index | Gallbladder and biliary tract cancer | 0 | .. | .. | 10 | 0 | No | Yes | Yes | Yes | |
| High body-mass index | Pancreatic cancer | 0 | .. | .. | 20 | 0 | No | Yes | Yes | Yes | |
| High body-mass index | Breast cancer (after menopause) | 0 | .. | .. | 44 | 2% | No | Yes | Yes | Yes | |
| High body-mass index | Breast cancer (before menopause) | 0 | .. | .. | 25 | 8% | No | Yes | Yes | No | |
| High body-mass index | Uterine cancer | 0 | .. | .. | 37 | 0 | No | Yes | Yes | Yes | |
| High body-mass index | Ovarian cancer | 0 | .. | .. | 31 | 3% | No | Yes | Yes | Yes | |
| High body-mass index | Kidney cancer | 0 | .. | .. | 28 | 0 | No | Yes | Yes | Yes | |
| High body-mass index | Thyroid cancer | 0 | .. | .. | 16 | 0 | No | Yes | Yes | Yes | |
| High body-mass index | Leukaemia | 0 | .. | .. | 17 | 0 | No | Yes | Yes | Yes | |
| High body-mass index | Ischaemic heart disease | 0 | .. | .. | 129 | .. | No | Yes | Yes | Yes | |
| High body-mass index | Ischaemic stroke | 0 | .. | .. | 102 | .. | No | Yes | Yes | Yes | |
| High body-mass index | Haemorrhagic stroke | 0 | .. | .. | 129 | .. | No | Yes | Yes | Yes | |
| High body-mass index | Hypertensive heart disease | 0 | .. | .. | 85 | .. | No | Yes | Yes | Yes | |
| High body-mass index | Diabetes mellitus | 0 | .. | .. | 85 | .. | Yes | Yes | Yes | No | |
| High body-mass index | Chronic kidney disease | 0 | .. | .. | 57 | .. | No | Yes | Yes | No | |
| High body-mass index | Osteoarthritis | 0 | .. | .. | 32 | 0 | No | Yes | Yes | Yes | |
| High body-mass index | Low back pain | 0 | .. | .. | 5 | 0 | No | Yes | Yes | Yes | |
| Low bone mineral density | Injuries | 0 | .. | .. | 12 | .. | No | Yes | Yes | Yes | |
| Low glomerular filtration rate | Ischaemic heart disease | 0 | .. | .. | 10 | 0 | Yes | .. | Yes | Yes | |
| Low glomerular filtration rate | Ischaemic stroke | 0 | .. | .. | 12 | 0 | Yes | .. | Yes | Yes | |
| Low glomerular filtration rate | Haemorrhagic stroke | 0 | .. | .. | 12 | 0 | Yes | .. | Yes | Yes | |
| Low glomerular filtration rate | Peripheral vascular disease | 0 | .. | .. | 1 | 0 | Yes | .. | Yes | Yes | |
| Low glomerular filtration rate | Gout | 0 | .. | .. | 3 | 0 | Yes | .. | Yes | No | |
If multiple reports existed from one study, we counted them as one study. We only assessed the dose-response relationship for continuous risks. To evaluate the magnitude of the effect size for continuous risks, we evaluated the RR comparing the 75th percentile with the 25th percentile of the exposure distribution at the global level. Additional information for this table is found in the methods appendix (pp 245–63). RCT=randomised controlled trial. RR=relative risk.
Prospective cohort studies or non-randomised interventions.
Whether or not any biological or mechanistic pathway exists that could potentially explain the relationship of the risk-outcome pair.
Whether or not the risk is associated with another outcome from the same category and whether or not any evidence exists that it can cause the current outcome through the same pathway.
Estimation process
Information about the data sources, estimation methods, computational tools, and statistical analysis used in derivation of our estimates are provided in the methods appendix. The analytical steps for estimation of burden attributable to single or clusters of risk-outcome pairs are summarised in the methods appendix (p 162). Table 1 provides definitions of exposure for each risk factor, the TMREL used, and metrics of data availability. For each risk, we estimated effect size as a function of age and sex and exposure level, mean exposure, the distribution of exposure across individuals, and the TMREL. The approach taken is largely similar to GBD 2013 for each quantity for each risk. Some methodological improvements have been implemented and new data sources incorporated. The methods appendix (pp 44–159) provides details of each step by risk. Citation information for the data sources used for relative risks are provided in searchable form through a web tool. We estimate the joint effects of combinations of risk factors using the same methods as GBD 2013, namely using published studies to estimate the fraction of a risk that was mediated through the other risk (methods appendix pp 28–35). Relative risks by age and sex for each risk factor and outcome pair are provided in the methods appendix (pp 215–44).
All point estimates are reported with 95% uncertainty intervals (UIs). UIs include uncertainty from each relevant component, consisting of exposure, relative risks, TMREL, and burden rates. Where percentage change is reported (with 95% UIs), we computed it on the basis of the point estimates being compared. In this study, we provide further methodological detail on new extensions to the CRA analysis.
Summary exposure value calculation
In previous GBD studies, we did not report comparable exposure metrics for the risk factors included because of the complexity of quantification of polytomous and continuous risks.18 Because of substantial interest in the trends in exposure, we developed a summary measure of exposure for each risk. This measure, called the summary exposure value (SEV), is the relative risk-weighted prevalence of exposure. Formally, it is defined as:
where Pri is prevalence of category i exposure, RRi is relative risk of the category i, and RRmax is the maximum relative risk observed (between categories). This quantity is estimated for each age, sex, location, year, and outcome. For each risk factor, a single SEV is estimated by averaging of the outcome of specific SEV values for each age, sex, location, and year across outcomes. In the case of dichotomous exposure, SEV is equal to prevalence. For continuous risks:
where P(x) is the density of exposure at level x of exposure, RR(x) is relative risk of the level x, and RRmax is the highest relative risk that is supported by data and reflects a level where more than 1% of the global population are exposed to that level or a higher risk.
SEV takes the value zero when no excess risk for a population exists and the value one when the population is at the highest level of risk; we report SEV on a scale from 0% to 100% to emphasise that it is risk-weighted prevalence. We computed as the level for exposure with the highest relative risk supported by cohort or trial data and for which at least 1% or more of the global population is exposed. For comparison purposes, we have also computed age-standardised SEVs for every risk factor from the most detailed level using the GBD population standard.
Decomposition of changes in deaths and DALYs into the contribution of population growth, ageing, risk exposure, and risk-deleted DALY rates
We did two related decomposition analyses of changes in DALYs from 1990 to 2015: decomposing changes in cause-specific DALYs due to changes in population growth, population age structure, exposure to all risks for a disease, and risk-deleted death and DALY rates; and decomposing changes in risk-attributable all-cause DALYs due to changes in population growth, population age structure, risk exposure to the single risk factor, and risk-deleted DALY rates. Risk-deleted rates are the rates after removal of the effect of a risk factor or combination of risk factors; in other words, observed DALY rates multiplied by one minus the PAF for the risk or set of risks. Our decomposition analyses draw from methods developed by Das Gupta19 to provide a computationally tractable solution to estimate the contribution of multiple factors to an outcome (methods appendix pp 36–37). For some risks where the PAF is 100%, such as fasting plasma glucose and diabetes, the methods have had to be further adapted. We were not able to include three outcomes in this analysis: cervical cancer, sexually transmitted diseases, and HIV/AIDS.
Risk transition with development
We examined how changes in risk exposure were related to changes along the development spectrum. Drawing from methods used to construct the Human Development Index,20 we constructed the SDI, a summary measure of overall development based on estimates of lag-dependent income per capita, average educational attainment over the age of 15 years, and total fertility rate. In the SDI, we weighted each component equally and rescaled them from zero (for the lowest value observed during 1980–2015) to one (for the highest value observed) for income per capita and average years of schooling, and the reverse for the total fertility rate. We computed the final SDI score as the geometric mean of each of the components. For each risk, we calculated the average relationship between risk exposure, as measured by SEV, and SDI across all geography years by age and sex using spline regression (methods appendix pp 38–39). We then used this relationship to characterise how exposures to risk vary on the basis of SDI alone.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The authors had full access to all the data in the study and had final responsibility to submit for publication.
Results
Global exposure to risks
The SEV is a single, interpretable measure, which captures risk-weighted exposure for a population, or risk-weighted prevalence of an exposure. The scale for SEV spans 0% to 100%, such that an SEV of 0% reflects no risk exposure in a population and 100% indicates that an entire population has maximum possible risk. A decline in SEV indicates reduced exposure to a given risk factor, whereas an increase in SEV indicates increased exposure. Table 3 provides age-standardised SEVs for 61 risks at the global level, by sex, for 1990, 2005, and 2015 (results appendix pp 3619–4070 contains results for every geography). From 1990 to 2015, SEVs decreased by more than 30% for four risks: unsafe sanitation (38·3% [95% UI 36·1–40·5]), childhood underweight (34·2% [30·9–37·9]), childhood stunting (33·4% [30·3–37·4]), and household air pollution (30·2% [26·9–33·2]). The global SEV for smoking also decreased by 2015, decreasing by 27·5% (23·2–30·9) for men and 28·7% (20·2–34·1) for women; notably, smoking exposure among men still far exceeded that for women in 2015. Significant, although more moderate than for smoking reductions in global SEVs for both sexes occurred for second-hand smoke (12·2% [9·4–15·1]), unsafe water (9·4% [5·3–13·0]), and diet high in red meat (9·0% [7·6–10·3]) from 1990 to 2015. Risk exposure for high total cholesterol significantly declined for both men and women during this time, although this decrease was smaller among men (3·2% [2·2–4·4]) than among women (5·6% [4·6–6·7]). For a subset of occupational risk factors, such as ergonomic factors and asthmagens, global SEVs were reduced from 1990 to 2015.
Table 3.
Global age-standardised summary exposure values for all risk factors for 1990, 2005, and 2015
|
Men |
Women |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1990 (%) | 2005 (%) | 2015 (%) | Percentage change 1990–2005 | Percentage change 2005–15 | Percentage change 1990–2015 | 1990 (%) | 2005 (%) | 2015 (%) | Percentage change 1990–2005 | Percentage change 2005–15 | Percentage change 1990–2015 | |
| Unsafe sanitation | 55·0 (53·8 to 56·5) | 42·6 (41·5 to 43·8) | 33·7 (32·2 to 35·1) | −22·6 (−24·0 to −20·9)* | −26·5 (−23·5 to −18·5)* | −38·8 (−41·0 to −36·6)* | 54·2 (52·8 to 55·7) | 42·3 (41·2 to 43·6) | 33·7 (32·2 to 35·1) | −21·9 (−23·4 to −20·2)* | −25·6 (−23·0 to −18·0)* | −37·8 (−40·0 to −35·6)* |
| Childhood underweight | 13·2 (11·7 to 14·7) | 11·3 (9·9 to 12·6) | 8·7 (7·4 to 10·0) | −14·5 (−16·9 to −12·1)* | −30·0 (−26·5 to −20·1)* | −34·2 (−37·8 to −30·8)* | 13·1 (11·6 to 14·5) | 11·2 (9·8 to 12·5) | 8·6 (7·3 to 9·9) | −14·7 (−17·1 to −12·3)* | −29·9 (−26·5 to −20·1)* | −34·3 (−37·9 to −31·0)* |
| Childhood stunting | 27·0 (18·6 to 29·6) | 22·5 (15·7 to 24·8) | 18·0 (12·6 to 20·2) | −16·7 (−19·1 to −14·6)* | −25·2 (−23·5 to −17·7)* | −33·5 (−37·6 to −30·5)* | 26·3 (18·1 to 28·8) | 21·9 (15·2 to 24·2) | 17·5 (12·2 to 19·8) | −16·6 (−19·0 to −14·5)* | −24·9 (−23·2 to −17·5)* | −33·2 (−37·3 to −30·2)* |
| Household air pollution from solid fuels | 23·2 (15·7 to 32·1) | 19·9 (13·5 to 27·6) | 16·0 (10·8 to 22·2) | −14·1 (−16·1 to −12·1)* | −24·2 (−22·6 to −16·3)* | −30·8 (−33·9 to −27·4)* | 29·3 (20·2 to 39·3) | 25·4 (17·6 to 34·1) | 20·6 (14·1 to 27·6) | −13·3 (−15·4 to −11·2)* | −23·2 (−21·9 to −15·8)* | −29·6 (−32·7 to −26·3)* |
| Smoking | 29·0 (27·0 to 31·6) | 24·7 (22·7 to 27·4) | 21·0 (19·4 to 23·4) | −15·0 (−17·5 to −12·3)* | −17·2 (−17·9 to −11·5)* | −27·5 (−30·9 to −23·2)* | 8·7 (7·7 to 10·6) | 7·6 (6·6 to 9·5) | 6·2 (5·5 to 7·9) | −12·9 (−16·0 to −8·2)* | −22·2 (−24·1 to −11·8)* | −28·7 (−34·1 to −20·2)* |
| Occupational ergonomic factors | 36·5 (35·4 to 37·9) | 30·5 (29·2 to 32·0) | 26·8 (25·3 to 28·6) | −16·5 (−17·6 to −15·3)* | −13·7 (−13·5 to −10·6)* | −26·6 (−28·6 to −24·3)* | 23·9 (23·3 to 24·7) | 22·2 (21·4 to 23·0) | 21·3 (20·4 to 22·4) | −7·4 (−8·5 to −6·3)* | −4·0 (−5·2 to −2·5)* | −11·0 (−12·9 to −9·0)* |
| Lead exposure | 19·4 (7·6 to 36·3) | 18·6 (7·3 to 35·2) | 15·7 (5·7 to 31·5) | −4·1 (−6·3 to −2·6)* | −18·0 (−22·4 to −10·4)* | −18·8 (−26·3 to −13·1)* | 17·5 (6·3 to 34·2) | 17·1 (6·2 to 33·7) | 14·5 (4·8 to 30·2) | −2·5 (−4·7 to −0·9)* | −17·9 (−22·7 to −10·3)* | −17·3 (−25·6 to −11·9)* |
| Occupational asthmagens | 30·2 (23·1 to 38·1) | 26·3 (20·4 to 32·9) | 23·6 (18·7 to 29·2) | −12·9 (−14·7 to −10·6)* | −11·5 (−12·0 to −8·1)* | −21·8 (−24·7 to −18·1)* | 17·3 (13·0 to 22·7) | 16·9 (12·8 to 21·9) | 17·1 (13·3 to 21·7) | −2·6 (−6·0 to 1·2) | 1·4 (−1·1 to 4·2) | −1·3 (−5·8 to 4·9) |
| Childhood sexual abuse | 8·8 (4·6 to 9·4) | 7·9 (4·1 to 8·4) | 7·5 (3·9 to 8·0) | −10·4 (−12·0 to −8·9)* | −4·9 (−6·2 to −3·2)* | −14·6 (−15·9 to −13·3)* | 9·8 (5·1 to 10·4) | 8·9 (4·6 to 9·5) | 8·6 (4·5 to 9·2) | −9·0 (−10·6 to −7·5)* | −3·5 (−5·0 to −1·8)* | −12·1 (−13·5 to −10·6)* |
| Vitamin A deficiency | 32·4 (30·6 to 34·6) | 32·4 (30·4 to 34·7) | 28·4 (26·7 to 30·4) | −0·3 (−3·1 to 2·5) | −13·8 (−14·6 to −9·5)* | −12·4 (−15·0 to −9·8)* | 29·5 (27·8 to 31·7) | 29·2 (27·4 to 31·5) | 25·8 (24·2 to 27·8) | −1·0 (−3·8 to 1·9) | −13·2 (−14·2 to −9·1)* | −12·6 (−15·2 to −9·8)* |
| Second-hand smoke | 21·0 (19·4 to 22·6) | 19·2 (17·8 to 20·8) | 18·5 (17·0 to 20·1) | −8·5 (−10·7 to −6·3)* | −3·5 (−5·1 to −1·6)* | −11·6 (−14·5 to −8·7)* | 31·7 (29·8 to 33·8) | 29·1 (27·6 to 30·7) | 27·8 (26·3 to 29·3) | −8·1 (−10·9 to −5·5)* | −4·8 (−5·8 to −3·4)* | −12·3 (−15·6 to −9·3)* |
| Childhood wasting | 6·2 (5·5 to 6·8) | 6·0 (5·3 to 6·6) | 5·4 (4·8 to 6·0) | −2·1 (−6·6 to 2·6) | −11·4 (−15·0 to −5·7)* | −12·1 (−16·7 to −7·0)* | 6·0 (5·3 to 6·6) | 5·9 (5·1 to 6·4) | 5·3 (4·6 to 5·9) | −2·2 (−6·9 to 2·5) | −11·3 (−14·9 to −5·6)* | −12·1 (−16·7 to −6·9)* |
| Occupational exposure to arsenic | 0·3 (0·3 to 0·3) | 0·3 (0·3 to 0·3) | 0·3 (0·3 to 0·3) | 0·3 (−0·5 to 1·0) | −9·9 (−9·6 to −8·5)* | −8·8 (−9·6 to −7·9)* | 0·1 (0·1 to 0·1) | 0·1 (0·1 to 0·1) | 0·1 (0·1 to 0·1) | 2·5 (1·0 to 4·1)* | −20·5 (−18·1 to −15·8)* | −14·9 (−16·6 to −13·3)* |
| Unsafe water source | 62·1 (57·8 to 66·8) | 58·6 (53·6 to 64·1) | 56·0 (50·4 to 62·1) | −5·7 (−8·2 to −3·2)* | −4·7 (−6·2 to −2·6)* | −10·0 (−13·5 to −5·9)* | 61·1 (56·8 to 65·8) | 58·0 (53·0 to 63·5) | 55·7 (50·2 to 61·8) | −5·1 (−7·6 to −2·4)* | −4·3 (−5·8 to −2·2)* | −8·9 (−12·6 to −4·9)* |
| Diet high in red meat | 10·5 (8·9 to 12·5) | 9·8 (8·2 to 11·7) | 9·7 (8·0 to 11·5) | −6·5 (−7·8 to −5·3)* | −2·0 (−3·3 to −0·8)* | −8·4 (−9·8 to −6·9)* | 9·5 (7·9 to 11·4) | 8·8 (7·3 to 10·6) | 8·6 (7·1 to 10·4) | −7·2 (−8·5 to −5·9)* | −2·7 (−3·8 to −1·4)* | −9·6 (−11·0 to −8·1)* |
| No handwashing with soap | 84·3 (81·3 to 87·2) | 80·7 (76·7 to 84·6) | 77·1 (72·4 to 81·8) | −4·4 (−5·9 to −2·9)* | −4·6 (−5·8 to −3·2)* | −8·6 (−11·3 to −6·0)* | 83·9 (80·8 to 86·8) | 80·3 (76·3 to 84·3) | 76·9 (72·2 to 81·6) | −4·2 (−5·7 to −2·8)* | −4·5 (−5·6 to −3·1)* | −8·4 (−11·0 to −5·8)* |
| Occupational exposure to asbestos | 2·5 (1·7 to 4·2) | 2·3 (1·6 to 3·7) | 2·4 (1·7 to 3·7) | −8·4 (−15·3 to 2·7) | 4·9 (−0·4 to 11·8) | −3·7 (−14·3 to 10·6) | 0·9 (0·7 to 1·5) | 0·7 (0·5 to 1·2) | 0·8 (0·6 to 1·2) | −21·5 (−30·4 to −9·1)* | 3·0 (−3·2 to 10·5) | −19·1 (−27·4 to −8·5)* |
| Zinc deficiency | 16·8 (9·8 to 20·3) | 16·8 (9·8 to 20·2) | 15·6 (9·1 to 18·8) | −0·0 (−2·6 to 2·9) | −7·8 (−9·6 to −4·7)* | −7·2 (−9·6 to −4·4)* | 16·8 (9·8 to 20·2) | 16·8 (9·8 to 20·3) | 15·6 (9·1 to 18·9) | 0·3 (−2·3 to 3·2) | −7·6 (−9·4 to −4·4)* | −6·8 (−9·2 to −4·0)* |
| Iron deficiency | .. | .. | .. | .. | .. | .. | 17·6 (12·4 to 23·7) | 17·5 (12·6 to 23·4) | 16·5 (12·1 to 21·8) | −0·5 (−7·2 to 4·7) | −6·0 (−14·7 to 1·1) | −6·1 (−19·1 to 5·0) |
| Low bone mineral density | 19·0 (15·8 to 22·9) | 18·3 (15·3 to 22·0) | 17·8 (14·4 to 21·6) | −3·8 (−8·4 to 1·6) | −2·8 (−8·3 to 2·8) | −6·4 (−11·5 to −0·9)* | 22·1 (18·8 to 25·8) | 21·5 (18·3 to 24·9) | 21·1 (17·5 to 25·0) | −2·7 (−6·4 to 1·0) | −1·9 (−6·5 to 2·9) | −4·6 (−8·8 to −0·2)* |
| Alcohol use | 10·9 (10·1 to 11·6) | 10·5 (9·8 to 11·3) | 10·7 (9·5 to 11·8) | −2·8 (−3·7 to −1·8)* | 1·7 (−3·0 to 5·1) | −1·1 (−6·0 to 2·3) | 5·9 (5·3 to 6·4) | 5·3 (4·8 to 5·8) | 5·1 (4·5 to 5·7) | −10·1 (−11·0 to −9·3)* | −3·4 (−6·4 to −0·9)* | −13·1 (−16·1 to −10·7)* |
| High total cholesterol | 30·4 (24·2 to 37·2) | 29·8 (23·7 to 36·6) | 29·4 (23·3 to 36·2) | −1·8 (−2·7 to −1·0)* | −1·5 (−2·1 to −0·8)* | −3·2 (−4·4 to −2·2)* | 33·7 (27·5 to 40·6) | 32·4 (26·2 to 39·3) | 31·8 (25·7 to 38·6) | −3·9 (−4·8 to −3·0)* | −1·8 (−2·5 to −1·2)* | −5·6 (−6·7 to −4·6)* |
| Occupational noise | 42·5 (32·4 to 53·5) | 40·6 (30·5 to 52·9) | 40·5 (31·0 to 53·4) | −4·5 (−10·4 to 1·0) | −0·3 (−3·8 to 3·2) | −4·7 (−10·9 to 1·2) | 25·2 (19·4 to 32·9) | 24·1 (18·4 to 32·5) | 24·4 (18·9 to 33·4) | −4·5 (−10·5 to 0·9) | 1·2 (−4·1 to 6·1) | −3·3 (−9·8 to 3·7) |
| Diet high in processed meat | 9·2 (7·3 to 11·3) | 9·0 (7·1 to 11·1) | 8·9 (7·0 to 11·0) | −2·6 (−3·9 to −1·2)* | −0·6 (−1·9 to 0·8) | −3·1 (−4·6 to −1·7)* | 8·4 (6·6 to 10·5) | 8·1 (6·3 to 10·1) | 8·0 (6·3 to 10·0) | −3·6 (−5·0 to −2·3)* | −1·0 (−2·3 to 0·3) | −4·6 (−6·1 to −3·3)* |
| Diet low in fibre | 15·6 (8·0 to 24·3) | 15·2 (7·8 to 23·7) | 15·0 (7·6 to 23·5) | −2·5 (−4·1 to −1·1)* | −1·2 (−3·5 to 0·9) | −3·7 (−5·3 to −2·5)* | 14·4 (7·2 to 22·7) | 14·0 (6·9 to 22·1) | 13·8 (6·8 to 21·8) | −2·8 (−4·7 to −1·3)* | −1·1 (−3·4 to 1·2) | −3·9 (−5·4 to −2·6)* |
| Non-exclusive breastfeeding | 16·5 (8·1 to 40·4) | 15·8 (8·2 to 37·6) | 15·9 (8·4 to 37·1) | −4·6 (−13·0 to 11·9) | 1·2 (−7·9 to 18·6) | −3·5 (−14·2 to 23·2) | 16·5 (8·0 to 40·4) | 15·7 (8·1 to 37·6) | 15·9 (8·3 to 37·1) | −5·0 (−13·0 to 10·5) | 1·0 (−7·4 to 17·7) | −4·0 (−14·0 to 21·4) |
| Occupational exposure to beryllium | 0·1 (0·1 to 0·1) | 0·1 (0·1 to 0·1) | 0·1 (0·1 to 0·1) | 7·8 (6·3 to 9·1)* | −10·3 (−10·3 to −8·5)* | −2·3 (−3·8 to −0·8)* | 0·1 (0·1 to 0·1) | 0·1 (0·1 to 0·1) | 0·0 (0·0 to 0·1) | 12·9 (10·3 to 15·5)* | −20·2 (−18·4 to −15·2)* | −6·1 (−8·8 to −3·4)* |
| Diet low in vegetables | 57·7 (39·1 to 77·0) | 57·6 (39·0 to 77·1) | 56·8 (38·5 to 76·1) | −0·1 (−0·7 to 0·5) | −1·3 (−1·8 to −0·8)* | −1·4 (−2·2 to −0·7)* | 56·2 (37·9 to 75·5) | 55·9 (37·6 to 75·2) | 55·3 (37·2 to 74·4) | −0·4 (−1·0 to 0·2) | −1·1 (−1·8 to −0·6)* | −1·5 (−2·5 to −0·8)* |
| Occupational particulate matter, gases, and fumes | 23·4 (17·7 to 30·5) | 22·8 (17·5 to 29·5) | 23·2 (18·0 to 29·7) | −2·6 (−4·6 to −0·6)* | 1·6 (0·7 to 2·7)* | −1·1 (−3·8 to 2·0) | 13·3 (10·0 to 19·2) | 13·0 (9·9 to 18·4) | 13·0 (9·9 to 18·5) | −2·6 (−5·5 to −0·0)* | 0·2 (−0·7 to 1·1) | −2·4 (−5·3 to 0·2) |
| Diet low in whole grains | 71·8 (52·1 to 89·1) | 71·7 (51·9 to 89·2) | 71·3 (51·5 to 89·1) | −0·1 (−0·5 to 0·2) | −0·5 (−0·9 to −0·1)* | −0·7 (−1·2 to 0·0) | 71·7 (52·0 to 89·0) | 71·5 (51·8 to 89·0) | 71·1 (51·3 to 88·8) | −0·2 (−0·6 to 0·1) | −0·6 (−1·0 to −0·2)* | −0·9 (−1·4 to −0·1)* |
| Low glomerular filtration rate | 3·5 (3·1 to 3·8) | 3·4 (3·1 to 3·7) | 3·5 (3·1 to 3·8) | −1·1 (−2·2 to −0·0)* | 1·6 (0·8 to 2·5)* | 0·5 (−0·5 to 1·4) | 4·9 (4·4 to 5·3) | 4·8 (4·4 to 5·3) | 4·8 (4·4 to 5·3) | −0·7 (−1·9 to 0·3) | 0·6 (−0·3 to 1·5) | −0·2 (−1·3 to 1·0) |
| Diet low in fruits | 58·7 (41·1 to 75·6) | 58·9 (41·3 to 75·8) | 58·6 (40·9 to 75·4) | 0·3 (0·1 to 0·6)* | −0·6 (−1·1 to −0·1)* | −0·3 (−0·7 to 0·1) | 55·3 (38·3 to 71·7) | 55·6 (38·5 to 72·0) | 55·0 (38·0 to 71·5) | 0·6 (0·3 to 0·9)* | −1·0 (−1·7 to −0·5)* | −0·4 (−1·1 to 0·1) |
| Diet low in nuts and seeds | 96·3 (84·3 to 99·8) | 96·1 (84·0 to 99·8) | 96·0 (83·9 to 99·7) | −0·2 (−0·5 to −0·0)* | −0·1 (−0·2 to 0·1) | −0·3 (−0·6 to −0·1)* | 96·1 (83·8 to 99·8) | 95·9 (83·5 to 99·8) | 95·8 (83·4 to 99·7) | −0·2 (−0·5 to −0·0)* | −0·1 (−0·2 to 0·0) | −0·3 (−0·6 to −0·1)* |
| Diet low in seafood omega-3 fatty acids | 77·3 (57·6 to 94·0) | 77·3 (57·6 to 94·0) | 77·4 (57·8 to 94·1) | −0·0 (−0·3 to 0·2) | 0·2 (0·0 to 0·5)* | 0·2 (−0·1 to 0·6) | 77·3 (57·5 to 94·0) | 77·4 (57·7 to 94·1) | 77·6 (57·9 to 94·3) | 0·1 (−0·1 to 0·4) | 0·3 (0·1 to 0·6)* | 0·5 (0·1 to 0·9)* |
| Discontinued breastfeeding | 13·5 (13·3 to 14·0) | 12·9 (12·8 to 13·2) | 13·7 (13·5 to 14·1) | −4·8 (−7·1 to −2·5)* | 5·6 (3·9 to 8·0)* | 0·8 (−1·8 to 3·9) | 13·5 (13·3 to 13·9) | 12·8 (12·7 to 13·1) | 13·5 (13·4 to 13·9) | −5·4 (−7·5 to −3·2)* | 5·4 (3·7 to 7·8)* | 0·0 (−2·5 to 3·0) |
| Low physical activity | 45·3 (40·9 to 49·2) | 45·9 (41·5 to 49·8) | 46·3 (42·0 to 50·3) | 1·3 (0·7 to 2·0)* | 1·0 (0·7 to 1·4)* | 2·4 (1·8 to 2·9)* | 39·9 (35·7 to 43·9) | 39·4 (35·1 to 43·4) | 39·4 (35·0 to 43·4) | −1·3 (−1·8 to −0·8)* | −0·2 (−0·6 to 0·2) | −1·5 (−2·0 to −1·0)* |
| Diet low in milk | 81·0 (63·4 to 95·4) | 81·6 (64·0 to 95·9) | 81·9 (64·2 to 96·2) | 0·8 (0·5 to 1·1)* | 0·4 (0·2 to 0·5)* | 1·2 (0·9 to 1·5)* | 80·0 (62·4 to 94·7) | 80·8 (63·1 to 95·2) | 81·2 (63·5 to 95·7) | 1·0 (0·6 to 1·3)* | 0·5 (0·3 to 0·7)* | 1·5 (1·1 to 1·9)* |
| Diet low in calcium | 63·3 (34·2 to 94·0) | 63·9 (34·6 to 94·8) | 64·3 (35·1 to 95·2) | 0·9 (0·5 to 1·4)* | 0·7 (0·1 to 1·5)* | 1·6 (0·8 to 2·7)* | 60·2 (32·2 to 91·4) | 61·0 (32·6 to 92·6) | 61·7 (33·3 to 93·3) | 1·3 (0·7 to 2·0)* | 1·0 (0·3 to 2·0)* | 2·4 (1·4 to 3·7)* |
| Occupational exposure to nickel | 0·9 (0·9 to 1·0) | 1·1 (1·1 to 1·1) | 1·0 (1·0 to 1·0) | 13·6 (12·1 to 14·9)* | −8·5 (−8·7 to −7·0)* | 4·6 (3·1 to 6·2)* | 0·4 (0·4 to 0·4) | 0·5 (0·5 to 0·5) | 0·4 (0·4 to 0·4) | 14·9 (12·3 to 17·6)* | −19·4 (−17·7 to −14·7)* | −3·8 (−6·4 to −1·1)* |
| Diet high in trans fatty acids | 7·8 (3·5 to 14·2) | 8·0 (3·7 to 14·5) | 8·1 (3·8 to 14·6) | 2·4 (0·5 to 5·3)* | 1·5 (−0·3 to 3·8) | 4·0 (2·5 to 7·0)* | 7·9 (3·6 to 14·3) | 8·1 (3·7 to 14·6) | 8·3 (3·9 to 14·8) | 2·6 (0·9 to 5·4)* | 2·3 (0·6 to 5·2)* | 5·0 (3·2 to 8·8)* |
| Intimate partner violence | .. | .. | .. | .. | .. | .. | 15·6 (13·2 to 17·8) | 15·4 (13·2 to 17·4) | 16·3 (14·0 to 18·5) | −1·4 (−3·7 to 1·1) | 5·7 (4·4 to 7·6)* | 4·5 (2·7 to 6·6)* |
| Ambient particulate matter pollution | 46·4 (39·8 to 53·4) | 47·7 (41·1 to 54·7) | 48·9 (42·2 to 55·8) | 2·8 (2·1 to 3·7)* | 2·3 (1·8 to 3·1)* | 5·3 (4·0 to 6·6)* | 45·5 (39·0 to 52·5) | 46·8 (40·2 to 53·7) | 48·0 (41·4 to 54·9) | 2·7 (2·0 to 3·6)* | 2·6 (2·0 to 3·3)* | 5·4 (4·1 to 6·8)* |
| High systolic blood pressure | 18·2 (15·7 to 21·0) | 18·9 (16·2 to 21·8) | 20·7 (17·9 to 23·8) | 3·3 (2·3 to 4·3)* | 8·8 (8·7 to 10·8)* | 13·3 (12·1 to 14·7)* | 18·2 (15·8 to 20·8) | 17·4 (15·0 to 20·1) | 18·1 (15·6 to 20·8) | −4·6 (−5·9 to −3·3)* | 3·7 (2·8 to 4·9)* | −0·9 (−2·3 to 0·5) |
| Diet high in sodium | 12·2 (5·1 to 23·5) | 12·8 (5·6 to 24·3) | 13·1 (6·0 to 24·9) | 4·9 (2·2 to 10·3)* | 2·1 (−1·8 to 8·4) | 7·2 (0·7 to 19·0)* | 9·0 (3·4 to 19·0) | 9·4 (3·7 to 19·4) | 9·4 (3·7 to 19·4) | 4·0 (1·8 to 8·7)* | −0·0 (−2·6 to 3·8) | 4·0 (−0·3 to 12·1) |
| Residential radon | 14·7 (12·6 to 16·8) | 15·2 (13·0 to 17·4) | 15·6 (13·5 to 17·9) | 3·4 (2·3 to 4·4)* | 3·0 (2·6 to 3·8)* | 6·6 (5·0 to 8·2)* | 14·8 (12·6 to 17·0) | 15·3 (13·1 to 17·5) | 15·8 (13·6 to 18·1) | 3·4 (2·2 to 4·6)* | 3·2 (2·7 to 3·9)* | 6·8 (5·1 to 8·5)* |
| Diet high in sugar-sweetened beverages | 8·3 (7·5 to 9·0) | 8·8 (7·9 to 9·7) | 8·7 (7·8 to 9·7) | 6·6 (1·6 to 11·2)* | −1·0 (−2·9 to 1·0) | 5·6 (−0·4 to 10·9) | 6·4 (5·7 to 7·1) | 7·0 (6·3 to 7·6) | 7·0 (6·2 to 7·7) | 8·8 (3·1 to 14·0)* | 0·4 (−1·9 to 2·5) | 9·2 (1·5 to 15·6)* |
| Occupational exposure to chromium | 1·3 (1·3 to 1·3) | 1·4 (1·4 to 1·5) | 1·4 (1·4 to 1·4) | 12·5 (11·2 to 13·8)* | −4·3 (−5·0 to −3·2)* | 7·9 (6·4 to 9·4)* | 0·6 (0·6 to 0·6) | 0·7 (0·7 to 0·7) | 0·6 (0·6 to 0·6) | 19·7 (17·3 to 22·3)* | −10·3 (−10·7 to −8·0)* | 8·5 (5·8 to 11·2)* |
| Occupational exposure to formaldehyde | 1·1 (1·0 to 1·1) | 1·1 (1·0 to 1·1) | 1·1 (1·1 to 1·2) | 5·9 (4·9 to 6·9)* | 1·7 (0·8 to 2·4)* | 7·7 (6·4 to 9·0)* | 0·6 (0·5 to 0·6) | 0·6 (0·6 to 0·6) | 0·6 (0·6 to 0·6) | 12·7 (11·0 to 14·6)* | −1·8 (−3·0 to −0·6)* | 10·7 (8·6 to 12·8)* |
| Occupational exposure to trichloroethylene | 0·5 (0·5 to 0·5) | 0·5 (0·5 to 0·5) | 0·5 (0·5 to 0·5) | 13·5 (12·3 to 14·6)* | −1·2 (−2·0 to −0·3)* | 12·2 (10·8 to 13·5)* | 0·2 (0·2 to 0·2) | 0·2 (0·2 to 0·2) | 0·2 (0·2 to 0·2) | 20·6 (18·5 to 22·8)* | −5·8 (−6·6 to −4·1)* | 14·0 (11·6 to 16·4)* |
| Diet low in polyunsaturated fatty acids | 34·1 (32·1 to 36·8) | 35·7 (32·4 to 40·0) | 39·8 (34·5 to 46·3) | 4·7 (−1·4 to 11·9) | 10·3 (4·1 to 19·5)* | 16·7 (4·8 to 31·0)* | 35·8 (33·6 to 38·5) | 37·6 (33·8 to 42·1) | 41·7 (35·9 to 48·4) | 5·1 (−1·7 to 12·7) | 9·8 (3·7 to 18·2)* | 16·5 (4·4 to 29·8)* |
| Occupational exposure to sulphuric acid | 1·4 (1·2 to 1·5) | 1·6 (1·4 to 1·8) | 1·6 (1·4 to 1·8) | 16·7 (14·9 to 18·6)* | −0·4 (−2·0 to 0·9) | 16·3 (14·5 to 18·1)* | 0·5 (0·5 to 0·6) | 0·6 (0·6 to 0·7) | 0·6 (0·6 to 0·7) | 22·9 (20·5 to 25·4)* | −6·8 (−8·1 to −4·9)* | 15·1 (12·4 to 17·7)* |
| Occupational exposure to cadmium | 0·3 (0·3 to 0·3) | 0·4 (0·4 to 0·4) | 0·4 (0·4 to 0·4) | 17·1 (15·8 to 18·5)* | 1·3 (0·4 to 2·3)* | 18·7 (17·1 to 20·3)* | 0·1 (0·1 to 0·1) | 0·2 (0·2 to 0·2) | 0·1 (0·1 to 0·2) | 21·3 (18·9 to 23·8)* | −10·0 (−10·4 to −7·7)* | 10·3 (7·6 to 12·9)* |
| Occupational exposure to second-hand smoke | 14·3 (14·2 to 14·3) | 16·2 (16·1 to 16·2) | 16·5 (16·4 to 16·6) | 13·3 (12·7 to 14·0)* | 2·0 (1·5 to 2·7)* | 15·6 (14·8 to 16·4)* | 5·4 (5·3 to 5·4) | 6·5 (6·5 to 6·6) | 7·0 (7·0 to 7·1) | 21·4 (20·8 to 22·1)* | 7·4 (7·5 to 8·6)* | 31·2 (30·3 to 32·0)* |
| High fasting plasma glucose | 6·8 (5·7 to 8·2) | 7·6 (6·4 to 9·1) | 8·5 (7·2 to 10·1) | 11·7 (10·8 to 12·7)* | 10·6 (11·0 to 12·7)* | 25·0 (23·3 to 26·7)* | 6·6 (5·4 to 7·9) | 7·2 (6·0 to 8·6) | 8·0 (6·7 to 9·6) | 9·4 (8·6 to 10·4)* | 10·8 (11·2 to 13·1)* | 22·7 (21·1 to 24·4)* |
| Ambient ozone pollution | 38·5 (13·9 to 67·9) | 42·8 (15·5 to 73·7) | 48·2 (17·6 to 78·3) | 11·2 (8·4 to 13·8)* | 11·2 (6·3 to 16·8)* | 25·2 (15·3 to 32·8)* | 38·2 (13·8 to 67·4) | 42·2 (15·3 to 72·8) | 47·4 (17·2 to 77·4) | 10·3 (7·9 to 12·7)* | 11·0 (6·3 to 16·4)* | 24·0 (14·8 to 31·0)* |
| Drug use | 0·4 (0·2 to 0·7) | 0·4 (0·2 to 0·8) | 0·5 (0·2 to 0·9) | 17·6 (12·7 to 24·4)* | 9·5 (7·7 to 13·7)* | 29·9 (22·4 to 40·3)* | 0·2 (0·1 to 0·3) | 0·2 (0·1 to 0·4) | 0·2 (0·1 to 0·4) | 15·6 (12·5 to 19·3)* | 11·3 (9·9 to 15·6)* | 30·3 (24·3 to 36·7)* |
| High body-mass index | 3·6 (1·6 to 6·1) | 4·4 (2·2 to 7·3) | 5·0 (2·5 to 8·0) | 23·7 (18·5 to 33·9)* | 10·8 (9·6 to 16·5)* | 38·7 (29·9 to 55·6)* | 4·6 (2·5 to 7·3) | 5·7 (3·2 to 8·7) | 6·2 (3·7 to 9·4) | 21·9 (17·8 to 28·8)* | 9·3 (8·1 to 13·9)* | 34·4 (27·7 to 45·7)* |
| Occupational exposure to polycyclic aromatic hydrocarbons | 1·6 (1·6 to 1·6) | 2·0 (2·0 to 2·0) | 2·2 (2·2 to 2·2) | 27·7 (26·4 to 28·9)* | 6·4 (5·9 to 7·8)* | 36·4 (34·9 to 38·0)* | 0·6 (0·5 to 0·6) | 0·8 (0·8 to 0·8) | 0·8 (0·8 to 0·8) | 37·6 (35·3 to 39·8)* | 2·9 (1·7 to 4·2)* | 41·7 (39·0 to 44·4)* |
| Occupational exposure to benzene | 1·3 (1·2 to 1·4) | 1·6 (1·5 to 1·8) | 1·9 (1·7 to 2·1) | 26·3 (24·4 to 28·2)* | 15·0 (16·1 to 19·2)* | 48·5 (46·0 to 51·2)* | 0·6 (0·6 to 0·7) | 0·9 (0·9 to 1·0) | 1·2 (1·1 to 1·3) | 52·6 (50·6 to 54·5)* | 22·7 (28·2 to 30·8)* | 97·5 (94·5 to 100·5)* |
| Occupational exposure to silica | 6·6 (6·5 to 6·7) | 9·6 (9·5 to 9·7) | 11·3 (11·2 to 11·5) | 46·5 (44·4 to 48·7)* | 15·1 (16·3 to 19·3)* | 72·6 (69·6 to 75·4)* | 1·3 (1·2 to 1·3) | 1·8 (1·7 to 1·8) | 1·8 (1·8 to 1·8) | 40·5 (38·6 to 42·4)* | 3·1 (2·0 to 4·5)* | 44·9 (42·6 to 47·4)* |
| Occupational exposure to diesel engine exhaust | 6·7 (6·6 to 6·7) | 9·9 (9·8 to 10·0) | 11·5 (11·4 to 11·6) | 47·9 (46·5 to 49·3)* | 14·0 (15·3 to 17·4)* | 72·1 (69·9 to 74·1)* | 1·5 (1·5 to 1·6) | 2·7 (2·6 to 2·7) | 3·5 (3·5 to 3·6) | 72·9 (70·7 to 75·0)* | 24·7 (30·9 to 35·3)* | 129·8 (125·0 to 134·7)* |
Data in parentheses are 95% uncertainty intervals. Risks are reported in order of percentage change for both sexes combined, 1990–2015.
Statistically significant increase or decrease.
For a subset of risks, minimal changes in exposure occurred between 1990 and 2015. This finding was particularly evident among various dietary risks (eg, diet low in fruits) and behaviours related to nutrition (eg, non-exclusive and discontinued breastfeeding). Discordant trends emerged by sex for some risk factors, such as low physical activity, where global SEVs for men increased by 2·4% (95% UI 1·8–2·9), whereas the SEV for women declined by 1·5% (1·0–2·0). Global SEVs significantly increased for 27 risk factors for both sexes combined from 1990 to 2015; significant increases occurred for 24 risks for men alone and 23 risks for women alone. We recorded the most pronounced rises for various occupational exposures, such as diesel engine exhaust, silica, and benzene. Global SEVs for high body-mass index (BMI) increased by 38·7% (29·9–55·6) for men and 34·4% (27·7–45·7) for women. For both sexes, other risks with large increases included drug use (30·2% [23·3–39·1]), ambient ozone pollution (24·6% [15·0–31·9]), and high fasting plasma glucose (23·8% [22·4–25·4]).
Global attributable burden for all risk factors combined and their overlap
The proportion of deaths, YLLs, YLDs, and DALYs that could be jointly attributable to all risk factors combined differed by cause group and measure of health (table 4). Globally, 57·8% (95% UI 56·6–58·8) of deaths, 48·4% (47·4–49·3) of YLLs, 26·1% (25·0–27·1) of YLDs, and 41·2% (39·8–42·8) of DALYs could be attributed to the risk factors currently assessed as part of GBD 2015. Across health outcomes, attributable DALYs were highest for non-communicable diseases (NCDs), although the percentage of attributable burden ranged from 20·9% (19·7–22·0) for YLDs to 64·8% (63·3–66·2) for deaths in 2015. Among NCD cause groups, attributable DALYs were as high as 85·3% (84·0–86·6) for cardiovascular and circulatory diseases compared with low attributable DALYs, even among leading causes of disease burden (ie, 16·0% [13·9–18·2] for musculoskeletal disorders and 22·5% [20·1–25·4] for mental and substance use disorders). In 2015, approximately 40–60% of DALYs due to cancers, cirrhosis, and chronic respiratory diseases could be attributed to risk factors assessed in this study. Except for YLDs, less than 50% of disease burden for Group 1 causes—communicable, maternal, neonatal, and nutritional diseases—could be attributed to analysed risk factors. Risk factors accounted for less than 20% of early death and disability from maternal disorders (eg, 10·2% [4·1–16·8] of DALYs).
Table 4.
Global all-age deaths and DALYs attributable to each risk factor at each level of the risk factor hierarchy and outcome for both sexes combined in 2005 and 2015
| 2005 deaths(in thousands) | 2015 deaths(in thousands) | Percentage change of 2005–15 deaths | Percentage change of 2005–15 age-standardised PAF | 2005 DALYs(in thousands) | 2015 DALYs(in thousands) | Percentage change of 2005–15 DALYs | Percentage change of 2005–15 age-standardised DALYs PAF | |||
|---|---|---|---|---|---|---|---|---|---|---|
| All risk factors: all causes | 30 718 (30 074 to 31 360) | 32 234 (31 456 to 33 035) | 4·9 (3·2 to 6·7)* | −1·1 (−1·7 to −0·4)* | 1 076 067 (1 022 161 to 1 137 872) | 1 015 470 (953 300 to 1 084 249) | −5·6 (−7·5 to −3·8)* | −4·6 (−5·8 to −3·5)* | ||
| Environmental or occupational risks: all causes | 9523 (8704 to 10 321) | 9315 (8523 to 10 145) | −2·2 (−4·8 to 0·6) | −6·7 (−8·3 to −5·1)* | 362 041 (335 616 to 387 712) | 319 569 (295 706 to 344 884) | −11·7 (−14·7 to −8·3)* | −9·2 (−11·8 to −6·5)* | ||
| Unsafe water, sanitation, and handwashing: all causes | 2179 (1993 to 2386) | 1766 (1586 to 1944) | −18·9 (−23·6 to −14·2)* | −16·0 (−20·3 to −11·8)* | 129 221 (116 430 to 142 602) | 95 305 (85 818 to 105 821) | −26·2 (−31·4 to −20·5)* | −18·9 (−24·5 to −12·6)* | ||
| Unsafe water source: all causes | 1587 (1284 to 1812) | 1251 (1008 to 1428) | −21·2 (−26·3 to −16·0)* | −18·0 (−22·9 to −13·0)* | 97 248 (78 516 to 112 113) | 71 745 (57 707 to 83 257) | −26·2 (−31·9 to −19·8)* | −18·8 (−25·0 to −12·1)* | ||
| Diarrhoeal diseases | 1411 (1147 to 1592) | 1101 (887 to 1244) | −22·0 (−27·4 to −16·5)* | −1·4 (−1·9 to −0·9)* | 84 526 (68 642 to 96 429) | 61 104 (49 352 to 69 584) | −27·7 (−33·6 to −21·2)* | −0·6 (−1·0 to −0·4)* | ||
| Typhoid fever | 147 (77 to 245) | 126 (67 to 215) | −14·6 (−21·0 to −8·8)* | −0·7 (−1·5 to −0·3)* | 10 688 (5712 to 17 653) | 8943 (4822 to 15 133) | −16·3 (−23·1 to −10·0)* | −0·7 (−1·5 to −0·3)* | ||
| Paratyphoid fever | 29 (13 to 57) | 25 (11 to 48) | −14·8 (−22·2 to −7·1)* | −0·8 (−1·6 to −0·3)* | 2034 (898 to 4009) | 1699 (757 to 3318) | −16·5 (−24·8 to −8·1)* | −0·7 (−1·6 to −0·3)* | ||
| Unsafe sanitation: all causes | 1114 (1012 to 1230) | 808 (727 to 895) | −27·5 (−32·7 to −22·3)* | −24·7 (−29·7 to −19·9)* | 67 949 (61 085 to 75 899) | 46 275 (41 065 to 51 818) | −31·9 (−37·4 to −25·7)* | −25·1 (−31·1 to −18·1)* | ||
| Diarrhoeal diseases | 997 (914 to 1087) | 720 (657 to 792) | −27·8 (−33·5 to −22·3)* | −8·9 (−10·9 to −7·2)* | 59 454 (53 638 to 65 649) | 40 005 (36 020 to 44 351) | −32·7 (−38·8 to −26·1)* | −7·6 (−9·4 to −5·9)* | ||
| Typhoid fever | 98 (53 to 164) | 74 (40 to 125) | −24·7 (−30·9 to −18·4)* | −12·4 (−15·2 to −10·0)* | 7149 (3893 to 11 816) | 5290 (2877 to 8857) | −26·0 (−32·6 to −19·3)* | −12·2 (−15·0 to −9·8)* | ||
| Paratyphoid fever | 19 (9 to 36) | 14 (7 to 27) | −25·8 (−32·7 to −18·8)* | −13·6 (−16·5 to −10·9)* | 1346 (627 to 2551) | 981 (456 to 1902) | −27·1 (−34·7 to −19·7)* | −13·4 (−16·3 to −10·8)* | ||
| No handwashing with soap: all causes | 1116 (927 to 1296) | 927 (760 to 1082) | −16·9 (−21·3 to −12·6)* | −14·3 (−18·3 to −10·4)* | 64 152 (53 252 to 74 634) | 47 271 (39 034 to 55 164) | −26·3 (−31·0 to −21·0)* | −19·0 (−24·0 to −13·4)* | ||
| Diarrhoeal diseases | 643 (514 to 763) | 502 (402 to 599) | −21·9 (−27·4 to −16·5)* | −1·4 (−2·0 to −0·9)* | 38 311 (30 403 to 45 759) | 27 628 (22 106 to 32 796) | −27·9 (−33·9 to −21·3)* | −0·9 (−1·4 to −0·5)* | ||
| Typhoid fever | 67 (34 to 114) | 56 (29 to 97) | −15·2 (−21·6 to −9·2)* | −1·4 (−2·1 to −0·8)* | 4831 (2568 to 8256) | 4019 (2135 to 6933) | −16·8 (−24·0 to −10·4)* | −1·3 (−2·1 to −0·7)* | ||
| Paratyphoid fever | 13 (6 to 26) | 11 (5 to 22) | −15·2 (−22·7 to −7·5)* | −1·4 (−2·2 to −0·8)* | 918 (422 to 1837) | 763 (355 to 1543) | −16·9 (−25·0 to −8·5)* | −1·3 (−2·1 to −0·7)* | ||
| Air pollution: all causes | 6466 (5675 to 7291) | 6485 (5708 to 7292) | 0·3 (−2·6 to 3·3) | −6·3 (−8·2 to −4·4)* | 186 850 (164 716 to 209 142) | 167 290 (148 167 to 185 780) | −10·5 (−13·6 to −7·3)* | −10·5 (−13·1 to −7·9)* | ||
| Ambient particulate matter pollution: all causes | 3934 (3437 to 4448) | 4241 (3698 to 4777) | 7·8 (5·1 to 10·8)* | 0·3 (−1·5 to 1·9) | 107 582 (94 319 to 121 177) | 103 066 (90 830 to 115 073) | −4·2 (−7·5 to −0·7)* | −4·9 (−7·7 to −2·3)* | ||
| Lower respiratory infections | 736 (549 to 957) | 675 (492 to 889) | −8·3 (−13·2 to −3·6)* | −3·4 (−5·8 to −1·6)* | 38 632 (29 407 to 48 531) | 28 360 (21 142 to 35 797) | −26·6 (−31·4 to −21·5)* | −3·1 (−5·4 to −1·4)* | ||
| Tracheal, bronchial, and lung cancer | 225 (140 to 318) | 283 (178 to 399) | 25·7 (20·8 to 32·0)* | 5·0 (3·2 to 7·7)* | 5171 (3244 to 7263) | 6209 (3935 to 8689) | 20·1 (14·9 to 27·1)* | 5·0 (3·2 to 7·6)* | ||
| Ischaemic heart disease | 1284 (1060 to 1530) | 1521 (1232 to 1821) | 18·5 (14·3 to 22·4)* | 3·1 (1·7 to 4·5)* | 28 484 (24 254 to 32 699) | 32 406 (27 078 to 37 427) | 13·8 (10·0 to 17·5)* | 3·4 (2·4 to 4·7)* | ||
| Ischaemic stroke | 347 (260 to 432) | 381 (283 to 483) | 9·9 (3·9 to 15·2)* | 3·2 (0·9 to 5·5)* | 6271 (5039 to 7454) | 6618 (5328 to 7905) | 5·5 (0·7 to 10·1)* | 3·5 (1·8 to 5·5)* | ||
| Haemorrhagic stroke | 505 (417 to 599) | 517 (425 to 614) | 2·3 (−2·2 to 7·1) | 0·4 (−0·9 to 1·6) | 12 605 (10 552 to 14 743) | 12 625 (10 570 to 14 867) | 0·2 (−3·9 to 4·6) | 1·3 (0·3 to 2·5)* | ||
| Chronic obstructive pulmonary disease | 837 (522 to 1174) | 864 (538 to 1213) | 3·2 (−1·1 to 8·4) | 0·2 (−0·9 to 1·9) | 16 418 (10 295 to 23 033) | 16 848 (10 517 to 23 590) | 2·6 (−1·6 to 7·7) | 1·2 (−0·1 to 3·3) | ||
| Household air pollution from solid fuels: all causes | 3280 (2505 to 4068) | 2854 (2179 to 3587) | −13·0 (−17·0 to −9·3)* | −17·8 (−21·1 to −14·8)* | 107 509 (83 554 to 132 012) | 85 644 (66 659 to 106 136) | −20·3 (−24·5 to −16·6)* | −19·2 (−22·7 to −15·8)* | ||
| Lower respiratory infections | 905 (663 to 1160) | 729 (523 to 949) | −19·5 (−24·2 to −14·5)* | −13·8 (−16·7 to −10·9)* | 52 898 (38 845 to 67 622) | 36 883 (26 631 to 46 916) | −30·3 (−35·1 to −25·0)* | −7·6 (−10·2 to −4·9)* | ||
| Tracheal, bronchial, and lung cancer | 159 (83 to 249) | 149 (76 to 241) | −6·3 (−12·6 to 0·4) | −21·4 (−25·9 to −17·4)* | 3806 (1996 to 5932) | 3439 (1767 to 5534) | −9·6 (−15·8 to −3·2)* | −20·8 (−25·2 to −16·9)* | ||
| Ischaemic heart disease | 778 (621 to 964) | 765 (598 to 965) | −1·6 (−7·0 to 3·7) | −13·8 (−18·0 to −10·1)* | 18 865 (15 180 to 22 902) | 18 200 (14 417 to 22 512) | −3·5 (−9·1 to 1·8) | −11·9 (−16·0 to −8·0)* | ||
| Ischaemic stroke | 245 (177 to 324) | 214 (152 to 290) | −12·6 (−18·2 to −7·0)* | −17·5 (−21·5 to −13·6)* | 4778 (3479 to 6282) | 4104 (2931 to 5426) | −14·1 (−19·6 to −8·6)* | −15·6 (−19·6 to −12·0)* | ||
| Haemorrhagic stroke | 418 (306 to 542) | 340 (252 to 446) | −18·6 (−23·5 to −13·7)* | −20·2 (−24·1 to −16·8)* | 10 857 (8159 to 13 941) | 8902 (6581 to 11 543) | −18·0 (−23·0 to −13·2)* | −17·2 (−21·2 to −13·7)* | ||
| Chronic obstructive pulmonary disease | 776 (422 to 1183) | 657 (360 to 1014) | −15·3 (−21·2 to −9·8)* | −17·5 (−22·0 to −13·4)* | 15 600 (8513 to 23 817) | 13 373 (7246 to 20 608) | −14·3 (−19·9 to −8·8)* | −15·5 (−20·0 to −11·2)* | ||
| Cataract | .. | .. | .. | .. | 705 (484 to 972) | 742 (512 to 1021) | 5·3 (1·7 to 9·1)* | −15·9 (−18·6 to −13·2)* | ||
| Ambient ozone pollution: all causes | 207 (77 to 353) | 254 (97 to 422) | 22·7 (16·6 to 30·3)* | 10·6 (5·5 to 17·0)* | 3472 (1281 to 5913) | 4116 (1577 to 6789) | 18·5 (12·1 to 26·5)* | 9·6 (3·7 to 17·3)* | ||
| Chronic obstructive pulmonary disease | 207 (77 to 353) | 254 (97 to 422) | 22·7 (16·6 to 30·3)* | 19·1 (16·0 to 23·6)* | 3472 (1281 to 5913) | 4116 (1577 to 6789) | 18·5 (12·1 to 26·5)* | 16·6 (12·9 to 21·7)* | ||
| Other environmental risks: all causes | 514 (273 to 804) | 558 (293 to 883) | 8·6 (4·9 to 11·8)* | −2·1 (−5·3 to 0·3) | 10 400 (5470 to 16 412) | 10 673 (5516 to 16 975) | 2·6 (−0·8 to 5·4) | −4·0 (−7·1 to −1·5)* | ||
| Residential radon: all causes | 53 (36 to 71) | 64 (42 to 86) | 19·7 (12·5 to 28·2)* | 10·6 (5·8 to 17·6)* | 1212 (841 to 1638) | 1386 (941 to 1871) | 14·3 (8·3 to 20·6)* | 6·9 (3·1 to 12·0)* | ||
| Tracheal, bronchial, and lung cancer | 53 (36 to 71) | 64 (42 to 86) | 19·7 (12·5 to 28·2)* | −0·0 (−4·1 to 6·0) | 1212 (841 to 1638) | 1386 (941 to 1871) | 14·3 (8·3 to 20·6)* | −0·1 (−3·2 to 4·6) | ||
| Lead exposure: all causes | 461 (227 to 745) | 495 (237 to 815) | 7·3 (2·6 to 10·7)* | −3·4 (−7·8 to −0·7)* | 9188 (4357 to 15 216) | 9287 (4200 to 15 594) | 1·1 (−3·7 to 4·4) | −5·3 (−9·5 to −2·3)* | ||
| Rheumatic heart disease | 4 (1 to 7) | 3 (1 to 6) | −8·2 (−14·7 to −2·0)* | −6·1 (−10·8 to −3·1)* | 97 (31 to 204) | 83 (25 to 175) | −14·9 (−21·6 to −9·3)* | −9·9 (−16·4 to −6·2)* | ||
| Ischaemic heart disease | 220 (107 to 359) | 240 (111 to 396) | 8·8 (3·3 to 12·7)* | −7·0 (−11·4 to −4·3)* | 3984 (1823 to 6675) | 4123 (1807 to 7049) | 3·5 (−1·8 to 7·1) | −7·6 (−11·9 to −5·0)* | ||
| Ischaemic stroke | 67 (32 to 115) | 68 (31 to 118) | 1·1 (−5·3 to 6·9) | −5·7 (−10·5 to −2·6)* | 1092 (485 to 1882) | 1055 (457 to 1828) | −3·4 (−9·3 to 1·0) | −5·9 (−10·5 to −3·3)* | ||
| Haemorrhagic stroke | 89 (38 to 155) | 87 (37 to 154) | −1·4 (−6·7 to 3·6) | −4·7 (−8·7 to −2·1)* | 1901 (750 to 3415) | 1807 (695 to 3293) | −4·9 (−9·4 to −1·2)* | −5·2 (−9·7 to −2·7)* | ||
| Hypertensive heart disease | 40 (12 to 92) | 47 (13 to 112) | 18·1 (7·0 to 26·8)* | −7·9 (−14·2 to −4·0)* | 710 (232 to 1561) | 772 (240 to 1738) | 8·8 (−0·1 to 15·4) | −9·1 (−15·1 to −5·4)* | ||
| Cardiomyopathy and myocarditis | 5 (2 to 8) | 5 (2 to 8) | 1·3 (−4·7 to 7·8) | −8·5 (−13·8 to −4·8)* | 99 (34 to 202) | 91 (31 to 183) | −8·5 (−13·2 to −3·1)* | −9·1 (−13·7 to −5·6)* | ||
| Atrial fibrillation and flutter | 3 (1 to 4) | 3 (1 to 5) | 22·1 (13·1 to 27·9)* | −9·7 (−15·8 to −6·3)* | 65 (30 to 113) | 72 (30 to 130) | 10·1 (0·7 to 15·5)* | −13·3 (−20·5 to −9·2)* | ||
| Aortic aneurysm | 2 (1 to 4) | 2 (1 to 4) | 7·4 (−3·1 to 14·5) | −13·5 (−20·9 to −9·3)* | 38 (16 to 67) | 39 (15 to 73) | 1·8 (−8·9 to 9·0) | −14·8 (−22·9 to −10·1)* | ||
| Peripheral vascular disease | 0 (0 to 1) | 1 (0 to 1) | 17·3 (3·0 to 28·6)* | −14·4 (−24·2 to −9·1)* | 11 (4 to 20) | 12 (4 to 23) | 11·9 (−0·6 to 19·7) | −14·2 (−23·2 to −9·6)* | ||
| Endocarditis | 1 (0 to 2) | 1 (0 to 2) | 11·8 (2·8 to 18·6)* | −11·6 (−18·6 to −7·6)* | 21 (8 to 39) | 21 (8 to 42) | 4·1 (−4·9 to 10·9) | −13·5 (−22·2 to −7·6)* | ||
| Other cardiovascular and circulatory diseases | 8 (4 to 14) | 9 (4 to 15) | 9·0 (2·6 to 14·3)* | −8·5 (−13·7 to −5·5)* | 223 (98 to 388) | 235 (98 to 422) | 5·4 (−2·3 to 10·4) | −10·3 (−16·9 to −6·5)* | ||
| Idiopathic developmental intellectual disability | .. | .. | .. | .. | 471 (214 to 815) | 423 (188 to 739) | −10·3 (−15·7 to −6·1)* | −13·7 (−19·2 to −9·8)* | ||
| Chronic kidney disease due to diabetes mellitus | 7 (3 to 12) | 9 (4 to 17) | 28·9 (20·2 to 34·6)* | −9·0 (−14·7 to −5·9)* | 150 (58 to 293) | 179 (65 to 356) | 19·4 (10·5 to 24·7)* | −10·5 (−17·1 to −6·9)* | ||
| Chronic kidney disease due to hypertension | 11 (5 to 18) | 14 (6 to 23) | 28·0 (20·9 to 33·0)* | −7·2 (−11·5 to −4·7)* | 196 (84 to 353) | 231 (97 to 416) | 17·8 (10·8 to 22·8)* | −8·4 (−13·5 to −5·4)* | ||
| Chronic kidney disease due to glomerulonephritis | 4 (2 to 7) | 5 (2 to 8) | 22·1 (16·9 to 27·8)* | 0·1 (−2·1 to 2·0) | 94 (34 to 180) | 102 (37 to 197) | 8·7 (4·5 to 12·9)* | −3·6 (−6·7 to −1·4)* | ||
| Chronic kidney disease due to other causes | 0 (0 to 1) | 1 (0 to 1) | 33·1 (24·5 to 42·3)* | −2·3 (−8·2 to 1·9) | 36 (14 to 73) | 41 (16 to 86) | 13·7 (7·8 to 17·7)* | −9·4 (−15·1 to −5·6)* | ||
| Occupational risks: all causes | 951 (889 to 1016) | 1086 (1013 to 1165) | 14·2 (10·4 to 18·6)* | 7·2 (4·2 to 10·5)* | 55 835 (47 024 to 65 679) | 63 615 (53 616 to 75 415) | 13·9 (11·0 to 17·3)* | 13·0 (10·2 to 16·2)* | ||
| Occupational carcinogens: all causes | 391 (370 to 410) | 489 (461 to 517) | 25·1 (20·4 to 30·2)* | 15·9 (12·0 to 20·2)* | 8109 (7708 to 8503) | 9832 (9318 to 10 385) | 21·2 (16·5 to 26·7)* | 12·9 (8·6 to 18·0)* | ||
| Occupational exposure to asbestos: all causes | 135 (118 to 154) | 180 (158 to 205) | 33·4 (27·3 to 40·1)* | 21·5 (16·2 to 27·2)* | 2210 (1919 to 2529) | 2769 (2391 to 3185) | 25·3 (19·4 to 31·6)* | 16·1 (10·6 to 21·7)* | ||
| Laryngeal cancer | 1 (1 to 1) | 1 (1 to 2) | 38·5 (25·8 to 56·8)* | 19·4 (9·0 to 35·4)* | 17 (11 to 25) | 22 (14 to 31) | 27·8 (17·9 to 41·3)* | 14·5 (6·5 to 25·6)* | ||
| Tracheal, bronchial, and lung cancer | 117 (101 to 135) | 155 (132 to 179) | 31·6 (25·6 to 38·6)* | 8·3 (4·1 to 12·5)* | 1875 (1590 to 2179) | 2314 (1947 to 2732) | 23·4 (17·3 to 29·9)* | 6·8 (2·7 to 11·0)* | ||
| Ovarian cancer | 1 (1 to 2) | 1 (1 to 2) | 27·3 (18·6 to 37·3)* | 3·7 (−2·6 to 10·4) | 19 (9 to 31) | 23 (11 to 38) | 22·1 (12·3 to 33·8)* | 0·7 (−6·0 to 8·2) | ||
| Mesothelioma | 16 (12 to 18) | 23 (19 to 26) | 47·2 (39·4 to 55·0)* | 3·9 (1·9 to 7·1)* | 298 (226 to 362) | 410 (320 to 488) | 37·3 (30·2 to 44·1)* | 3·9 (1·8 to 6·8)* | ||
| Occupational exposure to arsenic: all causes | 9 (7 to 11) | 9 (7 to 11) | −0·1 (−5·3 to 5·9) | −6·5 (−11·2 to −1·2)* | 196 (152 to 242) | 194 (150 to 242) | −0·9 (−6·2 to 5·4) | −7·6 (−12·4 to −1·7)* | ||
| Tracheal, bronchial, and lung cancer | 9 (7 to 11) | 9 (7 to 11) | −0·1 (−5·3 to 5·9) | −15·5 (−18·6 to −12·2)* | 196 (152 to 242) | 194 (150 to 242) | −0·9 (−6·2 to 5·4) | −13·7 (−16·8 to −10·7)* | ||
| Occupational exposure to benzene: all causes | 4 (4 to 5) | 6 (5 to 7) | 31·6 (26·4 to 36·6)* | 29·0 (24·9 to 33·2)* | 162 (137 to 190) | 211 (178 to 247) | 30·8 (25·4 to 36·0)* | 31·0 (25·9 to 36·5)* | ||
| Leukaemia | 4 (4 to 5) | 6 (5 to 7) | 31·6 (26·4 to 36·6)* | 13·6 (10·7 to 16·4)* | 162 (137 to 190) | 211 (178 to 247) | 30·8 (25·4 to 36·0)* | 17·5 (14·4 to 20·7)* | ||
| Occupational exposure to beryllium: all causes | 1 (0 to 1) | 1 (0 to 1) | −1·2 (−6·7 to 5·4) | −7·5 (−12·3 to −1·7)* | 13 (10 to 15) | 12 (10 to 15) | −2·1 (−7·7 to 4·7) | −8·7 (−14·0 to −2·7)* | ||
| Tracheal, bronchial, and lung cancer | 1 (0 to 1) | 1 (0 to 1) | −1·2 (−6·7 to 5·4) | −16·4 (−19·7 to −12·8)* | 13 (10 to 15) | 12 (10 to 15) | −2·1 (−7·7 to 4·7) | −14·7 (−17·9 to −11·2)* | ||
| Occupational exposure to cadmium: all causes | 2 (2 to 2) | 2 (2 to 3) | 9·5 (3·6 to 16·2)* | 2·4 (−2·6 to 8·2) | 43 (36 to 51) | 47 (38 to 56) | 8·7 (2·8 to 15·5)* | 1·2 (−4·2 to 7·5) | ||
| Tracheal, bronchial, and lung cancer | 2 (2 to 2) | 2 (2 to 3) | 9·5 (3·6 to 16·2)* | −7·4 (−10·8 to −3·7)* | 43 (36 to 51) | 47 (38 to 56) | 8·7 (2·8 to 15·5)* | −5·5 (−8·6 to −2·0)* | ||
| Occupational exposure to chromium: all causes | 7 (6 to 8) | 7 (6 to 8) | 4·4 (−1·1 to 10·8) | −2·2 (−6·8 to 3·6) | 151 (133 to 171) | 157 (137 to 178) | 3·6 (−2·1 to 10·1) | −3·5 (−8·3 to 2·4) | ||
| Tracheal, bronchial, and lung cancer | 7 (6 to 8) | 7 (6 to 8) | 4·4 (−1·1 to 10·8) | −11·7 (−14·6 to −8·5)* | 151 (133 to 171) | 157 (137 to 178) | 3·6 (−2·1 to 10·1) | −9·8 (−12·6 to −6·8)* | ||
| Occupational exposure to diesel engine exhaust: all causes | 91 (81 to 103) | 120 (106 to 136) | 30·8 (24·6 to 37·8)* | 22·2 (17·0 to 28·3)* | 2048 (1815 to 2304) | 2657 (2341 to 2994) | 29·8 (23·6 to 37·1)* | 20·8 (15·3 to 27·6)* | ||
| Tracheal, bronchial, and lung cancer | 91 (81 to 103) | 120 (106 to 136) | 30·8 (24·6 to 37·8)* | 10·4 (7·4 to 13·7)* | 2048 (1815 to 2304) | 2657 (2341 to 2994) | 29·8 (23·6 to 37·1)* | 12·8 (10·0 to 15·7)* | ||
| Occupational exposure to second-hand smoke: all causes | 84 (79 to 89) | 96 (90 to 103) | 14·7 (9·9 to 20·1)* | 7·3 (3·4 to 11·8)* | 1860 (1742 to 1972) | 2113 (1966 to 2262) | 13·6 (8·9 to 18·9)* | 5·7 (1·6 to 10·9)* | ||
| Tracheal, bronchial, and lung cancer | 84 (79 to 89) | 96 (90 to 103) | 14·7 (9·9 to 20·1)* | −3·0 (−5·1 to −0·7)* | 1860 (1742 to 1972) | 2113 (1966 to 2262) | 13·6 (8·9 to 18·9)* | −1·2 (−3·1 to 0·8) | ||
| Occupational exposure to formaldehyde: all causes | 2 (2 to 2) | 2 (2 to 2) | 1·7 (−4·6 to 7·9) | −1·1 (−6·8 to 4·7) | 71 (57 to 87) | 71 (57 to 87) | −0·1 (−6·4 to 6·2) | −1·0 (−7·1 to 5·0) | ||
| Nasopharyngeal cancer | 1 (1 to 1) | 1 (1 to 1) | −6·0 (−16·3 to 4·0) | −15·3 (−20·2 to −9·5)* | 36 (23 to 51) | 33 (21 to 47) | −8·8 (−19·4 to 1·8) | −13·4 (−18·5 to −7·1)* | ||
| Occupational exposure to nickel: all causes | 32 (24 to 42) | 33 (24 to 43) | 2·2 (−3·7 to 9·0) | −4·3 (−10·0 to 2·0) | 720 (535 to 927) | 729 (535 to 956) | 1·3 (−4·9 to 8·5) | −5·6 (−11·3 to 1·2) | ||
| Tracheal, bronchial, and lung cancer | 32 (24 to 42) | 33 (24 to 43) | 2·2 (−3·7 to 9·0) | −13·6 (−17·5 to −9·5)* | 720 (535 to 927) | 729 (535 to 956) | 1·3 (−4·9 to 8·5) | −11·8 (−15·7 to −7·9)* | ||
| Occupational exposure to polycyclic aromatic hydrocarbons: all causes | 15 (13 to 18) | 18 (15 to 21) | 16·9 (11·1 to 23·7)* | 9·3 (4·2 to 15·5)* | 342 (283 to 402) | 397 (327 to 470) | 16·1 (10·1 to 23·1)* | 8·1 (2·6 to 14·4)* | ||
| Tracheal, bronchial, and lung cancer | 15 (13 to 18) | 18 (15 to 21) | 16·9 (11·1 to 23·7)* | −1·2 (−4·5 to 2·3) | 342 (283 to 402) | 397 (327 to 470) | 16·1 (10·1 to 23·1)* | 1·0 (−2·1 to 4·1) | ||
| Occupational exposure to silica: all causes | 65 (59 to 71) | 86 (79 to 95) | 32·9 (25·8 to 40·8)* | 24·6 (18·6 to 31·3)* | 1444 (1308 to 1578) | 1894 (1724 to 2073) | 31·1 (24·2 to 39·3)* | 22·4 (16·2 to 29·8)* | ||
| Tracheal, bronchial, and lung cancer | 65 (59 to 71) | 86 (79 to 95) | 32·9 (25·8 to 40·8)* | 12·6 (8·7 to 17·0)* | 1444 (1308 to 1578) | 1894 (1724 to 2073) | 31·1 (24·2 to 39·3)* | 14·4 (10·6 to 18·4)* | ||
| Occupational exposure to sulphuric acid: all causes | 7 (5 to 9) | 8 (6 to 10) | 13·9 (9·1 to 18·9)* | 5·7 (1·5 to 10·2)* | 175 (134 to 219) | 199 (151 to 253) | 13·8 (9·2 to 18·7)* | 5·3 (1·0 to 10·0)* | ||
| Laryngeal cancer | 7 (5 to 9) | 8 (6 to 10) | 13·9 (9·1 to 18·9)* | 0·7 (−2·4 to 3·7) | 175 (134 to 219) | 199 (151 to 253) | 13·8 (9·2 to 18·7)* | 2·0 (−0·8 to 5·0) | ||
| Occupational exposure to trichloroethylene: all causes | 0 (0 to 0) | 0 (0 to 0) | 25·3 (19·4 to 30·3)* | 16·6 (11·3 to 20·5)* | 3 (1 to 6) | 4 (1 to 8) | 26·3 (20·4 to 31·2)* | 17·2 (11·6 to 21·8)* | ||
| Kidney cancer | 0 (0 to 0) | 0 (0 to 0) | 25·3 (19·4 to 30·3)* | −3·5 (−6·4 to −0·6)* | 3 (1 to 6) | 4 (1 to 8) | 26·3 (20·4 to 31·2)* | −2·7 (−5·5 to 0·7) | ||
| Occupational asthmagens: all causes | 50 (39 to 61) | 42 (35 to 48) | −16·9 (−26·0 to −2·4)* | −21·0 (−29·8 to −7·0)* | 2754 (2190 to 3373) | 2621 (2081 to 3223) | −4·8 (−12·0 to 3·6) | −5·3 (−12·2 to 3·8) | ||
| Asthma | 50 (39 to 61) | 42 (35 to 48) | −16·9 (−26·0 to −2·4)* | −4·6 (−11·0 to 3·0) | 2754 (2190 to 3373) | 2621 (2081 to 3223) | −4·8 (−12·0 to 3·6) | −5·4 (−9·1 to −1·7)* | ||
| Occupational particulate matter, gases, and fumes: all causes | 337 (280 to 392) | 357 (293 to 419) | 5·9 (0·9 to 11·6)* | −3·7 (−7·4 to 0·6) | 8405 (7325 to 9570) | 8787 (7598 to 9987) | 4·5 (0·5 to 9·2)* | −1·8 (−5·2 to 2·4) | ||
| Chronic obstructive pulmonary disease | 334 (278 to 389) | 354 (290 to 417) | 6·0 (1·0 to 11·8)* | 3·8 (1·2 to 6·9)* | 8346 (7264 to 9509) | 8729 (7541 to 9926) | 4·6 (0·6 to 9·3)* | 4·5 (2·5 to 6·8)* | ||
| Occupational noise: all causes | .. | .. | .. | .. | 8659 (5925 to 11 948) | 10 875 (7410 to 15 038) | 25·6 (23·5 to 27·7)* | 26·6 (24·1 to 29·2)* | ||
| Age-related and other hearing loss | .. | .. | .. | .. | 8659 (5925 to 11 948) | 10 875 (7410 to 15 038) | 25·6 (23·5 to 27·7)* | 3·8 (2·8 to 4·8)* | ||
| Occupational injuries: all causes | 189 (168 to 207) | 204 (191 to 232) | 8·0 (−3·4 to 24·3) | 12·4 (0·1 to 29·3)* | 12 212 (10 736 to 13 682) | 13 492 (12 006 to 15 545) | 10·5 (−0·2 to 25·9) | 16·9 (5·7 to 33·3)* | ||
| Pedestrian road injuries | 26 (22 to 30) | 30 (27 to 37) | 16·9 (−0·9 to 42·4) | 23·3 (3·0 to 54·6)* | 1320 (1110 to 1528) | 1510 (1362 to 1842) | 14·4 (−2·9 to 39·0) | 26·8 (6·3 to 58·0)* | ||
| Cyclist road injuries | 3 (3 to 3) | 3 (3 to 4) | 21·9 (8·3 to 35·5)* | 33·3 (18·7 to 50·2)* | 190 (166 to 215) | 243 (211 to 280) | 27·8 (16·1 to 40·6)* | 39·9 (26·6 to 55·3)* | ||
| Motorcyclist road injuries | 19 (17 to 21) | 22 (20 to 26) | 17·7 (3·2 to 36·2)* | 13·3 (1·5 to 28·3)* | 1101 (975 to 1222) | 1287 (1158 to 1469) | 16·9 (3·6 to 33·4)* | 16·5 (4·8 to 31·0)* | ||
| Motor vehicle road injuries | 42 (38 to 47) | 46 (43 to 51) | 9·4 (−0·1 to 21·1) | 15·2 (5·8 to 27·7)* | 2419 (2206 to 2692) | 2668 (2457 to 2977) | 10·3 (1·2 to 21·5)* | 18·2 (8·5 to 30·1)* | ||
| Other road injuries | 2 (1 to 3) | 2 (1 to 3) | −6·0 (−32·1 to 41·6) | −14·8 (−39·3 to 28·1) | 127 (86 to 169) | 127 (95 to 182) | −0·1 (−26·0 to 42·7) | −9·4 (−32·9 to 29·2) | ||
| Other transport injuries | 5 (4 to 6) | 6 (5 to 8) | 23·5 (0·3 to 55·7)* | 21·5 (1·2 to 52·9)* | 275 (229 to 325) | 332 (286 to 408) | 20·8 (−0·6 to 51·1) | 23·6 (3·7 to 53·3)* | ||
| Falls | 19 (17 to 22) | 23 (21 to 26) | 21·2 (7·1 to 39·4)* | 6·2 (−7·0 to 21·7) | 1847 (1520 to 2255) | 2329 (1892 to 2877) | 26·1 (13·2 to 41·2)* | 17·9 (6·0 to 32·0)* | ||
| Drowning | 26 (20 to 31) | 22 (19 to 31) | −15·0 (−33·5 to 15·9) | 3·8 (−19·8 to 42·5) | 1358 (1052 to 1625) | 1137 (967 to 1591) | −16·3 (−33·9 to 14·8) | 10·7 (−13·5 to 50·2) | ||
| Fire, heat, and hot substances | 12 (10 to 14) | 12 (11 to 15) | 7·7 (−6·0 to 25·5) | 21·9 (7·2 to 42·1)* | 815 (704 to 964) | 909 (771 to 1084) | 11·5 (−2·2 to 28·7) | 26·6 (10·7 to 46·4)* | ||
| Poisonings | 4 (3 to 4) | 3 (3 to 4) | −19·5 (−26·2 to −11·5)* | −4·9 (−18·9 to 9·0) | 233 (193 to 262) | 199 (168 to 225) | −14·6 (−22·0 to −6·1)* | 0·2 (−20·3 to 20·8) | ||
| Unintentional firearm injuries | 2 (1 to 2) | 2 (1 to 2) | −1·4 (−11·2 to 8·9) | 3·8 (−6·2 to 14·3) | 100 (71 to 113) | 99 (73 to 112) | −1·5 (−10·9 to 8·4) | 5·0 (−5·8 to 17·0) | ||
| Unintentional suffocation | 0 (0 to 0) | 0 (0 to 0) | 46·8 (7·5 to 75·3)* | 39·4 (12·7 to 68·3)* | 9 (8 to 11) | 13 (10 to 15) | 33·1 (11·7 to 54·0)* | 34·6 (13·0 to 61·0)* | ||
| Other exposure to mechanical forces | 9 (8 to 10) | 10 (8 to 12) | 15·0 (−1·1 to 28·9) | 18·1 (7·8 to 31·2)* | 737 (625 to 859) | 875 (704 to 1055) | 18·7 (6·7 to 31·0)* | 23·2 (11·9 to 35·9)* | ||
| Venomous animal contact | 3 (2 to 4) | 3 (2 to 4) | −8·1 (−23·4 to 15·9) | 2·2 (−12·2 to 18·8) | 210 (152 to 247) | 202 (143 to 247) | −3·8 (−17·2 to 15·6) | 8·9 (−7·1 to 26·2) | ||
| Non-venomous animal contact | 0 (0 to 1) | 0 (0 to 0) | −10·1 (−24·7 to 10·9) | 0·6 (−14·0 to 17·7) | 36 (29 to 45) | 36 (29 to 46) | −0·1 (−14·3 to 16·5) | 11·1 (−6·1 to 30·1) | ||
| Pulmonary aspiration and foreign body in airway | 3 (3 to 4) | 4 (3 to 4) | 28·0 (15·5 to 40·1)* | 20·7 (10·3 to 32·0)* | 192 (163 to 225) | 239 (205 to 274) | 24·4 (14·1 to 34·8)* | 25·3 (11·8 to 40·9)* | ||
| Foreign body in eyes | .. | .. | .. | .. | 3 (1 to 6) | 4 (2 to 8) | 38·6 (28·8 to 49·0)* | 20·1 (11·8 to 29·2)* | ||
| Foreign body in other body part | 2 (1 to 3) | 2 (1 to 2) | 6·1 (−12·7 to 24·0) | 13·5 (−0·2 to 28·2) | 138 (105 to 179) | 157 (124 to 191) | 13·8 (−2·8 to 29·5) | 20·1 (4·4 to 36·1)* | ||
| Other unintentional injuries | 11 (10 to 13) | 11 (9 to 14) | −5·8 (−22·6 to 23·4) | 6·3 (−12·0 to 38·6) | 1101 (882 to 1349) | 1128 (895 to 1490) | 2·4 (−12·1 to 24·5) | 12·5 (−3·4 to 37·4) | ||
| Occupational ergonomic factors: all causes | .. | .. | .. | .. | 16 792 (11 730 to 23 448) | 18 573 (12 979 to 25 759) | 10·6 (9·2 to 12·0)* | 11·7 (9·5 to 14·2)* | ||
| Low back pain | .. | .. | .. | .. | 16 792 (11 730 to 23 448) | 18 573 (12 979 to 25 759) | 10·6 (9·2 to 12·0)* | −4·9 (−5·6 to −4·1)* | ||
| Behavioural risks: all causes | 22 355 (21 183 to 23 567) | 22 744 (21 408 to 24 126) | 1·7 (−0·3 to 3·8) | −3·1 (−4·2 to −2·0)* | 825 546 (781 724 to 872 847) | 745 463 (698273 to 797 964) | −9·7 (−11·8 to −7·7)* | −7·9 (−9·3 to −6·5)* | ||
| Child and maternal malnutrition: all causes | 2280 (2113 to 2453) | 1414 (1308 to 1533) | −38·0 (−41·9 to −33·7)* | −30·4 (−34·9 to −25·6)* | 248 339 (226 327 to 275 262) | 172 120 (151 792 to 196 176) | −30·7 (−34·6 to −26·9)* | −22·2 (−26·4 to −18·3)* | ||
| Suboptimal breastfeeding: all causes | 592 (390 to 843) | 391 (258 to 550) | −33·9 (−39·7 to −27·5)* | −25·3 (−31·8 to −18·1)* | 51 338 (33 863 to 73 062) | 34 030 (22 497 to 47 771) | −33·7 (−39·5 to −27·2)* | −24·9 (−31·2 to −17·6)* | ||
| Non-exclusive breastfeeding: all causes | 551 (347 to 789) | 364 (227 to 520) | −34·0 (−39·5 to −27·6)* | −25·3 (−31·7 to −18·3)* | 47 654 (30 141 to 68 060) | 31 507 (19 669 to 44 929) | −33·9 (−39·4 to −27·5)* | −25·0 (−31·2 to −18·0)* | ||
| Diarrhoeal diseases | 228 (141 to 309) | 156 (98 to 216) | −31·5 (−40·4 to −21·0)* | −5·0 (−15·2 to 7·9) | 19 768 (12 250 to 26 755) | 13 579 (8489 to 18 758) | −31·3 (−40·1 to −20·8)* | −2·2 (−10·7 to 7·6) | ||
| Lower respiratory infections | 323 (137 to 555) | 208 (86 to 355) | −35·7 (−41·6 to −30·2)* | −24·9 (−31·0 to −19·0)* | 27 886 (11 846 to 47 863) | 17 928 (7453 to 30 580) | −35·7 (−41·5 to −30·2)* | −12·4 (−18·2 to −6·2)* | ||
| Discontinued breastfeeding: all causes | 55 (19 to 103) | 37 (13 to 69) | −33·2 (−42·7 to −21·6)* | −25·2 (−35·9 to −12·3)* | 4909 (1745 to 9248) | 3356 (1147 to 6281) | −31·6 (−40·8 to −20·5)* | −23·2 (−33·3 to −10·8)* | ||
| Diarrhoeal diseases | 55 (19 to 103) | 37 (13 to 69) | −33·2 (−42·7 to −21·6)* | −8·3 (−19·9 to 3·9) | 4909 (1745 to 9248) | 3356 (1147 to 6281) | −31·6 (−40·8 to −20·5)* | −3·6 (−12·1 to 5·5) | ||
| Childhood undernutrition: all causes | 2093 (1931 to 2261) | 1265 (1160 to 1383) | −39·6 (−43·6 to −35·1)* | −32·1 (−36·9 to −27·0)* | 184 339 (170 596 to 199 097) | 113 280 (103 941 to 123 401) | −38·5 (−42·5 to −34·2)* | −30·8 (−35·2 to −26·0)* | ||
| Childhood underweight: all causes | 666 (531 to 857) | 373 (304 to 468) | −44·0 (−52·0 to −34·8)* | −37·2 (−46·1 to −27·1)* | 60 146 (48 823 to 76 465) | 34 911 (28 903 to 43 357) | −42·0 (−49·6 to −33·2)* | −34·7 (−43·0 to −25·0)* | ||
| Diarrhoeal diseases | 124 (101 to 157) | 69 (55 to 87) | −44·7 (−51·5 to −36·1)* | −23·8 (−31·6 to −15·2)* | 10 975 (8985 to 13 785) | 6162 (4984 to 7724) | −43·9 (−50·7 to −35·6)* | −20·6 (−26·2 to −14·9)* | ||
| Lower respiratory infections | 209 (139 to 359) | 110 (70 to 197) | −47·5 (−52·7 to −42·3)* | −38·9 (−44·2 to −34·0)* | 17 904 (11 962 to 30 872) | 9416 (5994 to 16 919) | −47·4 (−52·6 to −42·2)* | −28·7 (−33·4 to −24·5)* | ||
| Measles | 100 (21 to 252) | 20 (4 to 56) | −79·9 (−88·1 to −68·7)* | −20·2 (−37·5 to −9·6)* | 8476 (1751 to 21 476) | 1701 (311 to 4763) | −79·9 (−88·1 to −68·7)* | −20·2 (−37·3 to −9·9)* | ||
| Protein-energy malnutrition | 233 (180 to 301) | 174 (131 to 227) | −25·3 (−42·5 to −3·6)* | −5·9 (−16·9 to 6·5) | 22 791 (18 010 to 28 484) | 17 633 (13 635 to 22 230) | −22·6 (−38·0 to −3·6)* | −0·8 (−4·3 to 2·8) | ||
| Childhood wasting: all causes | 1882 (1608 to 2125) | 1169 (982 to 1306) | −37·9 (−42·9 to −32·8)* | −30·2 (−35·7 to −24·3)* | 166 166 (142 764 to 186 926) | 104 945 (88 636 to 117 151) | −36·8 (−41·7 to −32·0)* | −28·8 (−34·2 to −23·4)* | ||
| Diarrhoeal diseases | 663 (543 to 749) | 431 (353 to 490) | −34·9 (−42·9 to −25·2)* | −10·4 (−19·4 to −1·0)* | 58 779 (48 152 to 66 140) | 38 905 (31 778 to 44 310) | −33·8 (−41·7 to −24·5)* | −6·5 (−11·4 to −1·3)* | ||
| Lower respiratory infections | 861 (623 to 1010) | 535 (377 to 639) | −37·9 (−43·3 to −32·4)* | −27·8 (−32·6 to −22·6)* | 73 987 (53 576 to 86 771) | 45 989 (32 457 to 54 877) | −37·8 (−43·2 to −32·4)* | −15·7 (−19·7 to −12·0)* | ||
| Measles | 125 (30 to 374) | 28 (6 to 92) | −77·2 (−86·2 to −63·8)* | −9·3 (−27·5 to −0·8)* | 10 608 (2529 to 31 860) | 2419 (483 to 7851) | −77·2 (−86·2 to −63·8)* | −9·3 (−27·4 to −0·9)* | ||
| Protein-energy malnutrition | 233 (180 to 301) | 174 (131 to 227) | −25·3 (−42·5 to −3·6)* | −5·9 (−16·9 to 6·5) | 22 791 (18 010 to 28 484) | 17 633 (13 635 to 22 230) | −22·6 (−38·0 to −3·6)* | −0·8 (−4·3 to 2·8) | ||
| Childhood stunting: all causes | 508 (248 to 853) | 257 (114 to 454) | −49·4 (−58·0 to −43·2)* | −43·1 (−53·0 to −36·2)* | 43 961 (21 558 to 73 511) | 22 420 (9964 to 39 448) | −49·0 (−57·4 to −42·9)* | −42·5 (−52·3 to −35·6)* | ||
| Diarrhoeal diseases | 154 (59 to 268) | 87 (31 to 156) | −43·6 (−51·1 to −33·4)* | −22·3 (−30·5 to −13·0)* | 13 638 (5210 to 23 658) | 7824 (2807 to 13 947) | −42·6 (−50·1 to −32·8)* | −18·9 (−24·7 to −13·1)* | ||
| Lower respiratory infections | 282 (25 to 615) | 155 (12 to 348) | −45·1 (−50·9 to −36·6)* | −36·1 (−42·0 to −26·4)* | 24 248 (2170 to 52 767) | 13 335 (1014 to 29 932) | −45·0 (−50·8 to −36·5)* | −25·4 (−31·1 to −16·1)* | ||
| Measles | 71 (7 to 202) | 15 (1 to 45) | −79·2 (−87·9 to −61·9)* | −16·9 (−30·7 to −5·4)* | 6074 (612 to 17 171) | 1262 (108 to 3787) | −79·2 (−87·9 to −61·9)* | −16·9 (−30·6 to −5·3)* | ||
| Iron deficiency: all causes | 87 (59 to 116) | 84 (58 to 114) | −3·5 (−14·8 to 10·0) | 1·7 (−9·3 to 14·7) | 55 120 (37 924 to 76 937) | 52 870 (36 518 to 74 437) | −4·1 (−5·8 to −2·4)* | 6·1 (3·9 to 8·5)* | ||
| Maternal haemorrhage | 30 (12 to 48) | 24 (9 to 40) | −20·3 (−32·7 to −7·6)* | −4·4 (−11·2 to 2·2) | 1694 (672 to 2705) | 1338 (509 to 2236) | −21·0 (−32·8 to −8·8)* | −4·5 (−11·1 to 2·1) | ||
| Maternal sepsis and other pregnancy-related infections | 8 (3 to 13) | 5 (2 to 9) | −34·1 (−47·7 to −17·6)* | −8·8 (−14·7 to −3·0)* | 475 (187 to 776) | 315 (118 to 543) | −33·7 (−46·9 to −17·2)* | −8·7 (−14·6 to −2·9)* | ||
| Iron-deficiency anaemia | 48 (32 to 63) | 54 (35 to 73) | 12·1 (−2·1 to 28·0) | .. | 52 951 (36 342 to 74 874) | 51 217 (35 014 to 72 661) | −3·3 (−4·8 to −1·8)* | .. | ||
| Vitamin A deficiency: all causes | 191 (116 to 291) | 83 (50 to 119) | −56·7 (−66·6 to −47·3)* | −51·6 (−62·5 to −41·0)* | 16 864 (10 421 to 25 457) | 7611 (4693 to 10 841) | −54·9 (−64·7 to −45·6)* | −49·4 (−60·2 to −39·1)* | ||
| Diarrhoeal diseases | 107 (60 to 158) | 64 (36 to 93) | −40·2 (−48·1 to −30·7)* | −17·9 (−26·8 to −8·5)* | 9531 (5402 to 14 012) | 5805 (3234 to 8402) | −39·1 (−46·7 to −29·8)* | −14·2 (−20·1 to −8·0)* | ||
| Measles | 84 (31 to 176) | 19 (7 to 41) | −77·9 (−86·0 to −66·3)* | −12·1 (−23·1 to −2·7)* | 7124 (2655 to 14 910) | 1574 (556 to 3469) | −77·9 (−86·0 to −66·3)* | −12·0 (−22·8 to −2·8)* | ||
| Vitamin A deficiency | .. | .. | .. | .. | 209 (131 to 309) | 232 (143 to 346) | 10·9 (7·5 to 14·6)* | .. | ||
| Zinc deficiency: all causes | 93 (5 to 208) | 55 (3 to 125) | −40·5 (−49·1 to −28·8)* | −33·8 (−43·3 to −21·0)* | 8162 (819 to 17 948) | 4967 (600 to 10 853) | −39·1 (−47·3 to −25·0)* | −32·2 (−40·9 to −16·2)* | ||
| Diarrhoeal diseases | 51 (0 to 119) | 31 (0 to 73) | −39·7 (−50·0 to 0·0) | −17·9 (−30·1 to 0·0) | 4663 (301 to 10 330) | 2911 (275 to 6369) | −37·6 (−47·4 to −8·3)* | −12·8 (−22·8 to 29·3) | ||
| Lower respiratory infections | 41 (0 to 143) | 24 (0 to 83) | −41·4 (−49·4 to 0·0) | −32·8 (−40·8 to 0·0) | 3498 (13 to 12 111) | 2056 (11 to 7031) | −41·2 (−48·8 to −11·0)* | −21·4 (−29·4 to 21·5) | ||
| Tobacco smoke: all causes | 6879 (6207 to 7522) | 7165 (6544 to 7775) | 4·2 (0·9 to 7·6)* | −4·0 (−6·4 to −1·5)* | 174 309 (158 980 to 190 805) | 170 889 (156 216 to 185 988) | −2·0 (−5·1 to 1·3) | −6·4 (−9·0 to −3·6)* | ||
| Smoking: all causes | 6113 (5402 to 6780) | 6402 (5749 to 7037) | 4·7 (1·2 to 8·5)* | −3·9 (−6·7 to −0·8)* | 147 153 (131 914 to 161 831) | 148 623 (134 236 to 163 140) | 1·0 (−2·4 to 4·6) | −5·0 (−8·1 to −1·9)* | ||
| Tuberculosis | 114 (57 to 180) | 87 (41 to 140) | −23·9 (−32·0 to −16·9)* | −9·4 (−15·3 to −4·8)* | 3717 (1859 to 5830) | 2836 (1357 to 4514) | −23·7 (−31·0 to −17·4)* | −9·0 (−15·5 to −3·9)* | ||
| Lower respiratory infections | 332 (265 to 405) | 350 (276 to 433) | 5·4 (1·0 to 9·4)* | −1·3 (−4·6 to 2·0) | 7119 (5724 to 8603) | 7044 (5589 to 8640) | −1·1 (−5·4 to 3·3) | 13·3 (7·0 to 19·9)* | ||
| Lip and oral cavity cancer | 48 (41 to 55) | 60 (50 to 71) | 25·8 (18·6 to 32·7)* | −4·9 (−8·8 to −1·6)* | 1288 (1099 to 1487) | 1548 (1284 to 1831) | 20·2 (12·5 to 27·8)* | −6·8 (−10·9 to −3·1)* | ||
| Nasopharyngeal cancer | 21 (15 to 28) | 23 (16 to 30) | 8·3 (−2·0 to 20·0) | −4·5 (−9·9 to 2·3) | 640 (431 to 887) | 643 (451 to 867) | 0·5 (−11·1 to 14·2) | −6·4 (−13·5 to 2·9) | ||
| Oesophageal cancer | 163 (101 to 236) | 157 (104 to 216) | −4·0 (−13·8 to 8·6) | 0·3 (−7·2 to 13·0) | 3736 (2336 to 5384) | 3418 (2286 to 4696) | −8·5 (−18·1 to 4·4) | −1·1 (−8·9 to 11·6) | ||
| Stomach cancer | 88 (51 to 138) | 81 (47 to 126) | −8·0 (−14·7 to −1·5)* | −7·0 (−11·9 to −2·3)* | 2030 (1162 to 3180) | 1706 (958 to 2630) | −16·0 (−23·2 to −8·8)* | −10·0 (−15·9 to −4·6)* | ||
| Colon and rectal cancer | 45 (32 to 60) | 50 (35 to 66) | 10·2 (4·8 to 15·3)* | −10·3 (−13·7 to −7·4)* | 978 (682 to 1293) | 996 (696 to 1314) | 1·9 (−3·4 to 6·8) | −14·0 (−17·5 to −11·1)* | ||
| Liver cancer due to hepatitis B | 37 (17 to 72) | 35 (16 to 64) | −5·0 (−20·0 to 13·1) | −5·1 (−15·4 to 10·9) | 1176 (512 to 2280) | 1022 (467 to 1899) | −13·1 (−29·5 to 7·7) | −8·6 (−21·7 to 11·0) | ||
| Liver cancer due to hepatitis C | 20 (12 to 29) | 24 (14 to 35) | 20·3 (12·8 to 28·6)* | −0·4 (−6·0 to 5·0) | 426 (248 to 634) | 474 (275 to 712) | 11·4 (2·1 to 21·4)* | −2·7 (−8·7 to 4·1) | ||
| Liver cancer due to alcohol use | 34 (17 to 58) | 40 (20 to 69) | 18·2 (6·8 to 31·0)* | −5·9 (−12·1 to −0·1)* | 849 (426 to 1476) | 958 (467 to 1652) | 12·8 (−0·3 to 26·9) | −7·8 (−14·9 to −0·7)* | ||
| Liver cancer due to other causes | 16 (8 to 29) | 16 (9 to 28) | 0·5 (−12·5 to 18·5) | −0·1 (−10·4 to 15·6) | 440 (204 to 817) | 396 (202 to 684) | −9·8 (−24·7 to 11·0) | −4·0 (−16·4 to 15·6) | ||
| Pancreatic cancer | 62 (50 to 75) | 73 (59 to 89) | 18·0 (14·0 to 22·2)* | −9·3 (−11·8 to −6·9)* | 1330 (1068 to 1630) | 1467 (1159 to 1820) | 10·3 (6·2 to 14·7)* | −12·4 (−15·3 to −9·6)* | ||
| Tracheal, bronchial, and lung cancer | 1014 (880 to 1127) | 1175 (1012 to 1324) | 15·8 (11·1 to 21·1)* | −3·6 (−5·3 to −2·1)* | 22 060 (18 918 to 24 709) | 24 140 (20 463 to 27 427) | 9·4 (4·3 to 15·5)* | −4·7 (−6·7 to −2·8)* | ||
| Cervical cancer | 12 (4 to 21) | 12 (4 to 21) | 0·7 (−11·2 to 15·6) | −3·6 (−11·9 to 6·2) | 355 (117 to 647) | 330 (109 to 588) | −7·1 (−21·0 to 9·4) | −8·0 (−17·8 to 3·9) | ||
| Kidney cancer | 20 (13 to 26) | 23 (15 to 31) | 16·6 (10·1 to 22·4)* | −11·1 (−14·6 to −8·1)* | 481 (326 to 625) | 531 (349 to 709) | 10·4 (3·9 to 16·1)* | −14·4 (−18·9 to −10·9)* | ||
| Bladder cancer | 44 (33 to 54) | 51 (38 to 64) | 16·8 (11·2 to 21·9)* | −6·2 (−9·0 to −3·6)* | 835 (629 to 1034) | 907 (674 to 1146) | 8·6 (3·3 to 13·7)* | −8·8 (−11·8 to −6·1)* | ||
| Ischaemic heart disease | 1236 (1020 to 1455) | 1280 (1049 to 1515) | 3·5 (0·1 to 6·9)* | −8·9 (−11·1 to −6·6)* | 32 669 (26 987 to 38 407) | 33 161 (26 987 to 39 130) | 1·5 (−2·1 to 4·9) | −7·4 (−9·4 to −5·4)* | ||
| Ischaemic stroke | 362 (301 to 420) | 352 (293 to 416) | −2·7 (−6·8 to 1·3) | −7·6 (−10·6 to −4·5)* | 7810 (6500 to 9146) | 7520 (6258 to 8897) | −3·7 (−7·8 to 0·2) | −5·4 (−8·2 to −2·6)* | ||
| Haemorrhagic stroke | 609 (510 to 706) | 573 (475 to 673) | −5·9 (−10·3 to −1·1)* | −7·1 (−10·1 to −3·9)* | 16 619 (14 010 to 19 207) | 15 512 (12 884 to 18 266) | −6·7 (−10·9 to −2·2)* | −5·5 (−8·2 to −2·6)* | ||
| Hypertensive heart disease | 99 (77 to 122) | 114 (89 to 138) | 14·9 (8·1 to 21·6)* | −6·8 (−11·2 to −1·4)* | 2527 (1976 to 3091) | 2771 (2168 to 3364) | 9·7 (3·3 to 16·4)* | −5·9 (−9·9 to −1·3)* | ||
| Atrial fibrillation and flutter | 12 (8 to 15) | 14 (10 to 18) | 18·0 (13·9 to 22·2)* | −11·0 (−13·9 to −8·1)* | 537 (379 to 732) | 617 (433 to 846) | 14·9 (12·7 to 16·9)* | −8·1 (−9·5 to −6·7)* | ||
| Aortic aneurysm | 22 (17 to 26) | 23 (18 to 28) | 6·3 (0·1 to 10·8)* | −12·9 (−15·0 to −10·6)* | 542 (426 to 651) | 572 (448 to 693) | 5·6 (−1·1 to 10·4) | −10·3 (−12·4 to −8·1)* | ||
| Peripheral vascular disease | 4 (3 to 5) | 5 (4 to 6) | 15·3 (8·8 to 22·0)* | −13·4 (−17·4 to −9·5)* | 144 (99 to 199) | 167 (114 to 237) | 16·3 (12·0 to 20·6)* | −10·6 (−12·9 to −8·4)* | ||
| Other cardiovascular and circulatory diseases | 58 (45 to 71) | 61 (47 to 75) | 5·9 (1·2 to 10·8)* | −8·8 (−11·7 to −5·5)* | 2187 (1699 to 2688) | 2348 (1816 to 2910) | 7·4 (3·5 to 11·2)* | −6·7 (−9·2 to −4·2)* | ||
| Chronic obstructive pulmonary disease | 1355 (1010 to 1686) | 1427 (1149 to 1699) | 5·3 (−2·5 to 17·1) | 1·8 (−4·5 to 13·4) | 25 834 (20 021 to 31 596) | 26 443 (21 842 to 31 310) | 2·4 (−4·6 to 12·6) | 0·6 (−5·4 to 10·8) | ||
| Silicosis | 2 (1 to 2) | 1 (1 to 2) | −7·1 (−21·0 to 8·8) | −8·7 (−17·1 to −0·8)* | 39 (22 to 66) | 33 (18 to 56) | −15·2 (−29·6 to 1·8) | −14·6 (−24·6 to −4·8)* | ||
| Asbestosis | 1 (0 to 1) | 1 (0 to 1) | 18·5 (6·9 to 30·1)* | −8·5 (−13·2 to −3·3)* | 12 (9 to 15) | 13 (9 to 17) | 7·8 (0·0 to 15·9)* | −12·6 (−16·9 to −7·8)* | ||
| Coal workers pneumoconiosis | 1 (0 to 1) | 0 (0 to 1) | −18·5 (−30·4 to −5·7)* | −12·8 (−21·5 to −5·3)* | 11 (8 to 15) | 9 (6 to 13) | −17·0 (−29·5 to −2·5)* | −14·7 (−22·6 to −6·4)* | ||
| Other pneumoconiosis | 2 (1 to 2) | 2 (2 to 3) | 15·1 (4·9 to 27·8)* | −5·3 (−14·8 to 5·8) | 49 (35 to 67) | 52 (37 to 71) | 6·3 (−2·8 to 15·5) | −13·5 (−20·2 to −6·6)* | ||
| Asthma | 55 (41 to 69) | 45 (35 to 56) | −17·6 (−27·0 to −4·2)* | −8·2 (−17·3 to 2·6) | 2226 (1692 to 2804) | 2024 (1514 to 2579) | −9·0 (−15·9 to −0·7)* | −13·3 (−18·5 to −7·8)* | ||
| Interstitial lung disease and pulmonary sarcoidosis | 12 (9 to 16) | 17 (12 to 21) | 37·2 (26·4 to 45·4)* | −9·7 (−13·2 to −5·2)* | 244 (179 to 302) | 302 (224 to 377) | 24·1 (15·2 to 31·7)* | −13·0 (−16·5 to −8·1)* | ||
| Other chronic respiratory diseases | 3 (2 to 4) | 4 (3 to 6) | 30·6 (16·5 to 49·4)* | 6·3 (−4·5 to 20·5) | 191 (140 to 248) | 211 (150 to 278) | 10·0 (0·6 to 20·1)* | 3·2 (−6·7 to 13·2) | ||
| Diabetes mellitus | 56 (17 to 98) | 68 (19 to 120) | 21·2 (13·4 to 27·9)* | −7·6 (−13·1 to −3·5)* | 2873 (831 to 5122) | 3402 (949 to 6090) | 18·4 (13·6 to 22·4)* | −8·5 (−11·7 to −6·1)* | ||
| Second-hand smoke: all causes | 884 (685 to 1093) | 886 (695 to 1091) | 0·2 (−3·5 to 3·9) | −4·8 (−7·4 to −2·4)* | 29 996 (22 370 to 38 043) | 25 212 (19 297 to 31 653) | −15·9 (−20·0 to −11·2)* | −13·3 (−16·5 to −9·7)* | ||
| Lower respiratory infections | 238 (151 to 330) | 183 (114 to 259) | −23·0 (−27·4 to −19·0)* | −15·0 (−17·5 to −12·5)* | 15 685 (9917 to 21 832) | 10 103 (6305 to 14 390) | −35·6 (−39·9 to −31·4)* | −13·5 (−15·9 to −11·1)* | ||
| Otitis media | 0 (0 to 0) | 0 (0 to 0) | −32·6 (−40·5 to −23·5)* | −11·7 (−25·4 to 2·6) | 266 (149 to 426) | 250 (138 to 406) | −5·8 (−9·4 to −3·0)* | −3·8 (−5·9 to −1·6)* | ||
| Tracheal, bronchial, and lung cancer | 22 (11 to 37) | 29 (15 to 49) | 32·6 (26·5 to 37·2)* | 10·7 (6·1 to 14·9)* | 536 (282 to 928) | 691 (371 to 1189) | 29·0 (21·4 to 35·0)* | 13·5 (7·4 to 19·0)* | ||
| Ischaemic heart disease | 331 (252 to 422) | 386 (291 to 494) | 16·5 (12·1 to 20·5)* | 0·9 (−0·8 to 2·6) | 7187 (5734 to 8847) | 8066 (6409 to 9894) | 12·2 (7·9 to 16·2)* | 1·9 (−0·0 to 3·9) | ||
| Ischaemic stroke | 69 (51 to 90) | 72 (52 to 95) | 5·4 (−0·7 to 10·9) | −1·5 (−4·2 to 0·9) | 1229 (948 to 1561) | 1248 (947 to 1589) | 1·5 (−3·8 to 6·3) | −0·6 (−3·2 to 1·7) | ||
| Haemorrhagic stroke | 104 (81 to 132) | 103 (80 to 132) | −0·6 (−5·2 to 4·7) | −2·5 (−5·1 to 0·1) | 2637 (2076 to 3305) | 2548 (1991 to 3201) | −3·4 (−8·2 to 2·2) | −2·1 (−4·9 to 0·9) | ||
| Alcohol and drug use: all causes | 2595 (2314 to 2866) | 2750 (2424 to 3051) | 6·0 (3·0 to 8·8)* | 3·2 (1·0 to 5·4)* | 108 717 (100 094 to 117 134) | 111 365 (102 247 to 120 352) | 2·4 (0·0 to 4·8)* | 3·4 (1·2 to 5·5)* | ||
| Alcohol use: all causes | 2228 (1943 to 2500) | 2306 (1986 to 2608) | 3·5 (0·0 to 6·8)* | 0·5 (−2·1 to 3·0) | 86 048 (78 266 to 93 716) | 84 990 (77 180 to 93 010) | −1·2 (−3·9 to 1·5) | −0·9 (−3·4 to 1·9) | ||
| Tuberculosis | 147 (117 to 187) | 126 (94 to 169) | −13·9 (−23·0 to −5·2)* | 4·7 (−3·7 to 11·1) | 5498 (4497 to 6911) | 4725 (3591 to 6198) | −14·1 (−22·4 to −6·2)* | 4·7 (−3·3 to 11·0) | ||
| Lower respiratory infections | 93 (83 to 104) | 106 (89 to 121) | 13·6 (6·7 to 20·2)* | 8·7 (2·9 to 14·5)* | 2279 (2036 to 2495) | 2355 (1995 to 2628) | 3·3 (−4·2 to 10·9) | 20·9 (11·7 to 30·3)* | ||
| Lip and oral cavity cancer | 29 (26 to 31) | 38 (33 to 41) | 31·9 (24·7 to 38·9)* | 0·5 (−4·4 to 4·5) | 820 (759 to 874) | 1046 (929 to 1134) | 27·5 (20·5 to 34·4)* | −0·3 (−4·8 to 3·6) | ||
| Nasopharyngeal cancer | 15 (11 to 16) | 18 (13 to 20) | 18·8 (7·8 to 28·3)* | 5·2 (−0·6 to 9·6) | 494 (367 to 538) | 556 (407 to 623) | 12·6 (1·9 to 22·3)* | 5·6 (0·3 to 9·9)* | ||
| Other pharyngeal cancer | 16 (14 to 17) | 20 (17 to 22) | 26·3 (18·9 to 32·8)* | 2·2 (−2·7 to 6·1) | 454 (418 to 486) | 560 (499 to 611) | 23·4 (16·3 to 29·7)* | 2·0 (−2·6 to 5·4) | ||
| Oesophageal cancer | 73 (66 to 80) | 75 (64 to 84) | 2·3 (−6·2 to 10·9) | 7·6 (0·8 to 12·9)* | 1847 (1673 to 2002) | 1826 (1579 to 2027) | −1·1 (−9·3 to 7·3) | 7·1 (0·9 to 11·9)* | ||
| Colon and rectal cancer | 27 (24 to 29) | 32 (28 to 36) | 20·8 (15·8 to 25·4)* | −1·4 (−5·2 to 1·6) | 599 (548 to 650) | 702 (626 to 771) | 17·2 (12·3 to 21·5)* | −1·0 (−4·7 to 2·0) | ||
| Liver cancer due to hepatitis B | 1 (1 to 2) | 1 (1 to 1) | −26·6 (−41·4 to −8·1)* | −17·6 (−33·3 to −2·5)* | 75 (53 to 97) | 56 (38 to 76) | −24·9 (−39·5 to −7·1)* | −12·8 (−28·3 to 1·5) | ||
| Liver cancer due to hepatitis C | 0 (0 to 0) | 0 (0 to 0) | −10·0 (−26·7 to 8·8) | −14·5 (−30·3 to 2·0) | 4 (3 to 6) | 4 (2 to 5) | −12·0 (−27·8 to 5·2) | −12·2 (−27·1 to 3·5) | ||
| Liver cancer due to alcohol use | 195 (169 to 208) | 245 (225 to 267) | 26·1 (18·5 to 37·1)* | .. | 4787 (4075 to 5169) | 5889 (5368 to 6441) | 23·0 (14·8 to 36·1)* | .. | ||
| Liver cancer due to other causes | 0 (0 to 0) | 0 (0 to 0) | −30·2 (−43·3 to −13·8)* | −20·6 (−35·7 to −5·6)* | 19 (13 to 25) | 14 (9 to 19) | −28·7 (−41·6 to −12·5)* | −15·0 (−29·8 to −0·7)* | ||
| Laryngeal cancer | 18 (16 to 19) | 20 (17 to 22) | 9·9 (3·9 to 15·2)* | −3·0 (−7·9 to 0·7) | 486 (443 to 523) | 520 (456 to 572) | 6·9 (1·6 to 11·9)* | −3·2 (−7·8 to 0·2) | ||
| Breast cancer | 27 (24 to 29) | 30 (26 to 34) | 13·8 (7·2 to 20·0)* | −6·1 (−10·7 to −1·7)* | 801 (712 to 889) | 899 (768 to 1023) | 12·3 (5·4 to 18·7)* | −6·0 (−10·8 to −1·3)* | ||
| Ischaemic heart disease | 35 (−110 to 176) | 10 (−130 to 150) | −71·4 (−400·6 to 326·2) | −85·9 (−325·6 to 241·9) | 1760 (−648 to 4072) | 1004 (−1092 to 2983) | −42·9 (−285·7 to 181·1) | −46·7 (−187·7 to 215·6) | ||
| Ischaemic stroke | 13 (−8 to 34) | 8 (−11 to 27) | −38·1 (−206·5 to 204·3) | −31·8 (−162·0 to 138·1) | 517 (210 to 814) | 455 (213 to 691) | −12·0 (−21·3 to 10·0) | −11·9 (−21·3 to 16·5) | ||
| Haemorrhagic stroke | 237 (213 to 261) | 248 (214 to 280) | 4·7 (−2·1 to 11·3) | 2·8 (−3·8 to 8·0) | 5659 (5148 to 6143) | 5754 (5004 to 6385) | 1·7 (−4·8 to 7·3) | 2·7 (−3·2 to 7·1) | ||
| Hypertensive heart disease | 40 (29 to 51) | 51 (34 to 68) | 30·0 (9·7 to 45·7)* | 7·5 (−9·6 to 22·1) | 1023 (840 to 1211) | 1271 (970 to 1538) | 24·3 (12·0 to 33·8)* | 7·2 (−2·9 to 15·6) | ||
| Atrial fibrillation and flutter | 8 (6 to 9) | 10 (8 to 13) | 35·4 (26·8 to 43·1)* | 0·5 (−5·9 to 5·8) | 237 (184 to 303) | 301 (233 to 391) | 26·9 (20·6 to 32·3)* | 0·5 (−4·6 to 4·5) | ||
| Cirrhosis and other chronic liver diseases due to hepatitis B | 82 (69 to 95) | 87 (69 to 105) | 6·9 (−3·0 to 14·9) | −1·5 (−10·2 to 4·4) | 2456 (2076 to 2832) | 2526 (1989 to 3019) | 2·8 (−6·8 to 10·5) | −1·8 (−10·4 to 3·9) | ||
| Cirrhosis and other chronic liver diseases due to hepatitis C | 66 (54 to 77) | 73 (57 to 88) | 10·1 (−0·0 to 17·3) | −2·9 (−12·0 to 3·1) | 1895 (1538 to 2203) | 2017 (1542 to 2419) | 6·4 (−3·5 to 13·4) | −2·6 (−11·8 to 3·3) | ||
| Cirrhosis and other chronic liver diseases due to alcohol use | 310 (289 to 333) | 348 (323 to 375) | 12·2 (8·4 to 16·7)* | .. | 10 093 (9424 to 10 841) | 10 997 (10 197 to 11 875) | 9·0 (5·0 to 13·7)* | .. | ||
| Cirrhosis and other chronic liver diseases due to other causes | 48 (41 to 55) | 52 (42 to 61) | 7·9 (−0·5 to 14·8) | −0·7 (−8·5 to 4·5) | 1399 (1197 to 1587) | 1430 (1157 to 1681) | 2·2 (−6·1 to 8·9) | 1·1 (−7·0 to 6·7) | ||
| Pancreatitis | 16 (15 to 18) | 19 (16 to 21) | 13·3 (4·3 to 22·0)* | −4·4 (−11·1 to 1·5) | 633 (567 to 691) | 695 (600 to 778) | 9·7 (1·4 to 18·1)* | −5·1 (−11·5 to 0·5) | ||
| Epilepsy | 12 (11 to 13) | 14 (12 to 15) | 10·9 (2·9 to 19·7)* | 2·0 (−4·1 to 7·9) | 1038 (866 to 1219) | 1039 (859 to 1239) | 0·1 (−6·5 to 6·5) | −0·7 (−6·4 to 4·1) | ||
| Alcohol use disorders | 157 (147 to 163) | 138 (131 to 144) | −12·6 (−16·7 to −7·0)* | .. | 11 567 (9618 to 13 835) | 11 194 (9136 to 13 871) | −3·2 (−7·0 to 0·6) | .. | ||
| Diabetes mellitus | −58 (−63 to −53) | −64 (−70 to −58) | 10·5 (0·8 to 19·7)* | −18·4 (−25·9 to −10·3)* | −2324 (−2840 to −1866) | −2685 (−3321 to −2142) | 15·5 (10·4 to 20·0)* | −11·7 (−15·4 to −8·2)* | ||
| Pedestrian road injuries | 107 (89 to 127) | 100 (84 to 119) | −6·1 (−13·2 to −0·0)* | −0·4 (−3·1 to 2·1) | 5360 (4475 to 6380) | 4806 (4012 to 5678) | −10·3 (−16·8 to −4·6)* | 0·3 (−2·5 to 2·9) | ||
| Cyclist road injuries | 13 (10 to 15) | 11 (9 to 13) | −11·4 (−19·4 to −3·5)* | −2·4 (−5·7 to 0·7) | 701 (578 to 838) | 607 (511 to 720) | −13·4 (−19·8 to −6·7)* | −3·6 (−6·9 to −0·5)* | ||
| Motorcyclist road injuries | 77 (64 to 88) | 81 (69 to 93) | 4·3 (−5·1 to 16·4) | −0·0 (−3·3 to 3·5) | 4299 (3632 to 4895) | 4324 (3713 to 5003) | 0·6 (−7·4 to 11·6) | −0·0 (−3·2 to 3·3) | ||
| Motor vehicle road injuries | 148 (130 to 167) | 135 (120 to 152) | −8·8 (−14·7 to −2·9)* | −4·6 (−6·6 to −2·4)* | 7917 (7015 to 8956) | 7067 (6301 to 7927) | −10·7 (−15·9 to −5·6)* | −4·5 (−6·6 to −2·3)* | ||
| Falls | 42 (36 to 50) | 50 (41 to 60) | 17·8 (8·7 to 24·6)* | −1·2 (−5·0 to 2·2) | 2416 (1951 to 2968) | 2602 (2097 to 3230) | 7·7 (2·2 to 12·2)* | −3·2 (−5·9 to −0·0)* | ||
| Drowning | 27 (24 to 32) | 24 (21 to 28) | −13·2 (−17·0 to −9·1)* | 3·0 (−2·9 to 8·4) | 1225 (1057 to 1435) | 1001 (871 to 1168) | −18·3 (−22·1 to −14·4)* | 4·9 (−2·9 to 11·9) | ||
| Fire, heat, and hot substances | 14 (12 to 16) | 12 (10 to 15) | −10·1 (−16·6 to −1·9)* | −3·6 (−10·3 to 1·7) | 694 (586 to 832) | 619 (511 to 755) | −10·8 (−16·2 to −4·5)* | −3·1 (−10·2 to 2·2) | ||
| Poisonings | 9 (7 to 11) | 7 (5 to 9) | −15·8 (−21·5 to −8·5)* | −4·9 (−16·2 to 7·1) | 386 (303 to 478) | 319 (246 to 388) | −17·4 (−22·1 to −11·0)* | −7·0 (−23·3 to 11·0) | ||
| Unintentional firearm injuries | 3 (2 to 4) | 3 (2 to 3) | −8·0 (−13·1 to −2·2)* | −6·7 (−9·8 to −3·0)* | 145 (112 to 174) | 129 (99 to 154) | −10·7 (−15·7 to −5·1)* | −6·9 (−10·6 to −2·5)* | ||
| Unintentional suffocation | 1 (1 to 1) | 2 (1 to 2) | 42·5 (16·3 to 57·0)* | 27·3 (9·8 to 43·3)* | 68 (55 to 84) | 88 (68 to 108) | 28·9 (13·2 to 38·9)* | 25·8 (9·5 to 43·3)* | ||
| Other exposure to mechanical forces | 14 (11 to 17) | 15 (10 to 18) | 0·5 (−15·2 to 12·4) | −0·1 (−5·4 to 4·4) | 913 (724 to 1127) | 905 (684 to 1140) | −0·9 (−10·2 to 6·8) | −0·4 (−3·7 to 3·1) | ||
| Self-harm | 110 (95 to 129) | 111 (96 to 130) | 1·4 (−4·3 to 6·2) | 0·6 (−3·6 to 3·8) | 4649 (4032 to 5436) | 4552 (3953 to 5303) | −2·1 (−7·5 to 2·7) | 0·6 (−3·8 to 3·9) | ||
| Assault by firearm | 23 (21 to 26) | 23 (20 to 26) | −0·6 (−4·2 to 4·2) | −5·3 (−6·9 to −3·6)* | 1313 (1158 to 1481) | 1285 (1128 to 1459) | −2·2 (−5·7 to 2·5) | −5·1 (−6·7 to −3·3)* | ||
| Assault by sharp object | 16 (14 to 18) | 12 (11 to 14) | −19·7 (−24·0 to −14·5)* | −5·3 (−8·0 to −2·8)* | 840 (744 to 968) | 668 (590 to 769) | −20·5 (−24·7 to −15·2)* | −4·7 (−7·5 to −2·2)* | ||
| Assault by other means | 18 (16 to 22) | 16 (14 to 19) | −13·9 (−18·4 to −7·3)* | −6·2 (−9·0 to −3·1)* | 1007 (880 to 1181) | 868 (745 to 1022) | −13·7 (−18·2 to −7·0)* | −5·0 (−7·9 to −1·8)* | ||
| Drug use: all causes | 407 (364 to 448) | 489 (439 to 537) | 20·2 (15·9 to 25·0)* | 19·2 (15·2 to 24·2)* | 24 036 (21 317 to 26 732) | 27 831 (24 437 to 31 171) | 15·8 (12·6 to 18·8)* | 19·5 (16·1 to 23·0)* | ||
| HIV/AIDS—tuberculosis | 11 (9 to 14) | 8 (7 to 10) | −25·7 (−33·4 to −15·9)* | 22·1 (10·1 to 36·9)* | 567 (465 to 698) | 413 (333 to 513) | −27·1 (−33·9 to −18·2)* | 19·4 (8·2 to 33·6)* | ||
| HIV/AIDS resulting in other diseases | 53 (46 to 65) | 52 (44 to 63) | −3·6 (−12·0 to 7·2) | 39·5 (28·9 to 51·1)* | 2746 (2380 to 3317) | 2594 (2216 to 3176) | −5·6 (−13·6 to 4·0) | 34·4 (25·3 to 44·9)* | ||
| Hepatitis B | 1 (0 to 1) | 0 (0 to 1) | −27·7 (−35·2 to −18·4)* | −21·3 (−29·3 to −10·3)* | 18 (8 to 30) | 13 (6 to 21) | −28·0 (−35·8 to −18·8)* | −22·3 (−30·6 to −12·2)* | ||
| Hepatitis C | 1 (0 to 2) | 1 (0 to 2) | −12·0 (−30·1 to 11·0) | −1·4 (−13·0 to 11·5) | 37 (9 to 83) | 33 (8 to 72) | −12·3 (−30·1 to 10·0) | −3·8 (−14·3 to 7·5) | ||
| Liver cancer due to hepatitis B | 3 (1 to 5) | 4 (2 to 6) | 15·2 (1·3 to 38·4)* | 15·3 (4·8 to 30·9)* | 104 (43 to 171) | 110 (49 to 179) | 6·2 (−7·1 to 29·1) | 11·7 (1·8 to 26·0)* | ||
| Liver cancer due to hepatitis C | 53 (38 to 68) | 74 (57 to 91) | 39·0 (28·8 to 54·2)* | 16·6 (8·5 to 29·2)* | 1316 (998 to 1627) | 1678 (1329 to 2012) | 27·5 (18·2 to 41·4)* | 12·7 (5·5 to 24·1)* | ||
| Cirrhosis and other chronic liver diseases due to hepatitis B | 3 (1 to 5) | 3 (1 to 5) | 20·9 (10·3 to 35·7)* | 12·6 (3·0 to 26·4)* | 90 (38 to 149) | 101 (43 to 162) | 12·1 (2·3 to 24·9)* | 8·1 (−1·3 to 20·6) | ||
| Cirrhosis and other chronic liver diseases due to hepatitis C | 124 (98 to 147) | 147 (118 to 175) | 19·0 (12·9 to 27·0)* | 7·0 (2·2 to 14·1)* | 4064 (3321 to 4750) | 4556 (3727 to 5374) | 12·1 (6·4 to 19·0)* | 4·3 (0·2 to 10·2)* | ||
| Opioid use disorders | 94 (91 to 100) | 122 (110 to 130) | 29·6 (18·2 to 37·2)* | .. | 9864 (8127 to 11 517) | 12 068 (9878 to 14 145) | 22·3 (17·5 to 26·1)* | .. | ||
| Cocaine use disorders | 7 (5 to 8) | 11 (9 to 12) | 49·7 (33·6 to 75·4)* | .. | 729 (558 to 902) | 999 (773 to 1234) | 37·0 (29·2 to 47·0)* | .. | ||
| Amphetamine use disorders | 7 (4 to 8) | 12 (8 to 14) | 67·5 (25·6 to 118·9)* | .. | 1001 (706 to 1348) | 1403 (1025 to 1847) | 40·1 (26·1 to 55·2)* | .. | ||
| Cannabis use disorders | .. | .. | .. | .. | 548 (352 to 781) | 577 (372 to 818) | 5·3 (3·7 to 7·1)* | .. | ||
| Other drug use disorders | 20 (19 to 23) | 25 (23 to 27) | 23·0 (12·7 to 32·1)* | .. | 1529 (1245 to 1861) | 1862 (1502 to 2274) | 21·8 (15·7 to 27·5)* | .. | ||
| Self-harm | 28 (19 to 41) | 29 (20 to 41) | 2·6 (−3·0 to 8·9) | 5·6 (1·3 to 10·0)* | 1423 (951 to 2030) | 1425 (955 to 2037) | 0·1 (−5·4 to 6·3) | 5·8 (1·4 to 10·3)* | ||
| Dietary risks: all causes | 10 738 (9473 to 12 010) | 12 058 (10 615 to 13 538) | 12·3 (10·0 to 14·5)* | 2·4 (1·1 to 3·6)* | 242 781 (217 378 to 269 659) | 264411 (236 098 to 294 989) | 8·9 (6·3 to 11·3)* | 2·1 (0·0 to 4·1)* | ||
| Diet low in fruits: all causes | 2713 (1806 to 3703) | 2924 (1905 to 4018) | 7·8 (4·3 to 10·9)* | −0·6 (−3·1 to 1·5) | 68 838 (46 616 to 92 835) | 72 590 (48 514 to 98 667) | 5·5 (1·7 to 8·6)* | −0·3 (−3·4 to 2·5) | ||
| Lip and oral cavity cancer | 8 (0 to 17) | 10 (0 to 22) | 32·7 (0·0 to 37·5)* | 0·1 (−0·6 to 0·7) | 208 (0 to 451) | 266 (0 to 583) | 28·1 (0·0 to 33·1)* | −0·1 (−0·8 to 0·5) | ||
| Nasopharyngeal cancer | 4 (0 to 9) | 5 (0 to 10) | 11·3 (0·0 to 18·2)* | −1·7 (−2·7 to 0·0) | 132 (0 to 281) | 138 (0 to 293) | 4·5 (−3·7 to 11·1) | −2·1 (−3·3 to 0·0) | ||
| Other pharyngeal cancer | 4 (0 to 8) | 4 (0 to 10) | 23·4 (0·0 to 29·4)* | −0·6 (−1·4 to 0·1) | 99 (0 to 221) | 119 (0 to 266) | 20·2 (0·0 to 26·2)* | −0·6 (−1·4 to 0·1) | ||
| Oesophageal cancer | 106 (26 to 187) | 99 (24 to 174) | −6·4 (−11·3 to −0·8)* | −2·0 (−3·2 to −1·2)* | 2466 (618 to 4362) | 2221 (542 to 3911) | −9·9 (−15·1 to −4·0)* | −2·5 (−3·9 to −1·6)* | ||
| Laryngeal cancer | 7 (0 to 15) | 7 (0 to 17) | 13·4 (0·0 to 17·4)* | −0·3 (−1·0 to 0·2) | 168 (0 to 374) | 184 (0 to 413) | 9·8 (0·0 to 13·8)* | −0·5 (−1·3 to 0·1) | ||
| Tracheal, bronchial, and lung cancer | 172 (70 to 291) | 207 (84 to 351) | 20·1 (16·5 to 24·4)* | 0·1 (−0·5 to 0·7) | 3858 (1577 to 6495) | 4391 (1780 to 7445) | 13·8 (9·9 to 18·7)* | −0·5 (−1·3 to 0·1) | ||
| Ischaemic heart disease | 947 (340 to 1585) | 1086 (388 to 1818) | 14·7 (12·1 to 17·0)* | −0·3 (−0·9 to 0·3) | 21 685 (7921 to 35 741) | 23 777 (8598 to 39 451) | 9·6 (6·3 to 12·4)* | −0·0 (−0·8 to 0·6) | ||
| Ischaemic stroke | 509 (271 to 776) | 521 (274 to 805) | 2·3 (−1·1 to 5·2) | −2·4 (−3·6 to −1·5)* | 10 961 (5937 to 16 258) | 11 001 (5940 to 16 513) | 0·4 (−3·1 to 3·5) | −0·7 (−1·8 to 0·1) | ||
| Haemorrhagic stroke | 838 (465 to 1239) | 831 (458 to 1241) | −0·9 (−4·5 to 2·9) | −1·7 (−2·8 to −0·8)* | 22 973 (13 194 to 33 252) | 22 476 (12 752 to 32 682) | −2·2 (−5·8 to 1·5) | −0·4 (−1·4 to 0·3) | ||
| Diet low in vegetables: all causes | 1842 (943 to 2869) | 1994 (1024 to 3121) | 8·2 (4·5 to 11·2)* | −1·1 (−3·7 to 0·7) | 42 617 (22 635 to 65 749) | 44 632 (23 572 to 68 817) | 4·7 (1·5 to 7·9)* | −1·3 (−4·2 to 1·3) | ||
| Ischaemic heart disease | 1261 (489 to 2099) | 1418 (548 to 2363) | 12·5 (10·3 to 14·7)* | −2·8 (−3·7 to −2·1)* | 27 791 (11 029 to 45 849) | 30 048 (11 828 to 49 331) | 8·1 (5·2 to 10·9)* | −1·9 (−2·8 to −1·1)* | ||
| Ischaemic stroke | 226 (51 to 412) | 224 (51 to 412) | −0·8 (−3·8 to 2·0) | −5·7 (−7·1 to −4·4)* | 4869 (1120 to 8768) | 4762 (1097 to 8586) | −2·2 (−5·8 to 0·9) | −3·4 (−4·8 to −2·1)* | ||
| Haemorrhagic stroke | 355 (99 to 666) | 352 (99 to 653) | −1·0 (−4·1 to 2·5) | −1·9 (−3·4 to −0·4)* | 9957 (2799 to 18 328) | 9823 (2800 to 18 053) | −1·3 (−4·6 to 2·3) | 0·6 (−0·8 to 2·2) | ||
| Diet low in whole grains: all causes | 2879 (2056 to 3818) | 3142 (2215 to 4189) | 9·1 (6·3 to 11·8)* | 0·4 (−1·5 to 2·0) | 74 523 (54 213 to 96 519) | 79 813 (57 571 to 104 238) | 7·1 (3·7 to 9·8)* | 1·3 (−1·3 to 3·5) | ||
| Ischaemic heart disease | 1497 (888 to 2168) | 1713 (1013 to 2481) | 14·4 (12·0 to 16·6)* | −0·6 (−1·2 to −0·2)* | 33 870 (20 349 to 48 312) | 36 933 (21 938 to 53 267) | 9·0 (5·7 to 11·6)* | −0·7 (−1·4 to −0·2)* | ||
| Ischaemic stroke | 459 (311 to 620) | 463 (311 to 631) | 0·9 (−2·5 to 3·8) | −3·6 (−4·9 to −2·6)* | 10 195 (6993 to 13 536) | 10 143 (6849 to 13 505) | −0·5 (−4·0 to 2·7) | −1·5 (−2·6 to −0·6)* | ||
| Haemorrhagic stroke | 729 (515 to 982) | 716 (497 to 962) | −1·8 (−5·4 to 2·2) | −2·6 (−3·7 to −1·6)* | 20 024 (14 326 to 26 601) | 19 443 (13 708 to 25 849) | −2·9 (−6·5 to 0·9) | −1·1 (−2·1 to −0·4)* | ||
| Diabetes mellitus | 195 (105 to 301) | 250 (135 to 387) | 28·5 (23·6 to 33·3)* | −1·5 (−2·4 to −0·7)* | 10 434 (5659 to 16 438) | 13 295 (7183 to 21 043) | 27·4 (24·4 to 30·3)* | −0·8 (−1·4 to −0·3)* | ||
| Diet low in nuts and seeds: all causes | 1830 (1160 to 2583) | 2131 (1354 to 3011) | 16·4 (14·2 to 18·6)* | 6·0 (4·5 to 7·5)* | 43 725 (29 136 to 60 125) | 49 411 (32 716 to 68 196) | 13·0 (9·8 to 15·9)* | 6·5 (3·9 to 9·0)* | ||
| Ischaemic heart disease | 1706 (1062 to 2438) | 1970 (1226 to 2810) | 15·5 (13·2 to 17·6)* | −0·0 (−0·4 to 0·3) | 37 340 (23 613 to 52 283) | 41 199 (26 175 to 57 706) | 10·3 (7·3 to 12·9)* | 0·3 (−0·2 to 0·8) | ||
| Diabetes mellitus | 123 (64 to 193) | 160 (83 to 253) | 29·9 (25·2 to 34·6)* | −0·5 (−1·1 to 0·1) | 6384 (3038 to 10 211) | 8212 (3923 to 13 200) | 28·6 (25·6 to 31·5)* | 0·1 (−0·2 to 0·5) | ||
| Diet low in milk: all causes | 101 (35 to 171) | 126 (44 to 212) | 24·7 (22·0 to 27·7)* | 13·8 (11·6 to 15·9)* | 2177 (750 to 3688) | 2603 (897 to 4382) | 19·6 (16·8 to 22·6)* | 11·9 (9·3 to 14·7)* | ||
| Colon and rectal cancer | 101 (35 to 171) | 126 (44 to 212) | 24·7 (22·0 to 27·7)* | 1·3 (0·9 to 1·8)* | 2177 (750 to 3688) | 2603 (897 to 4382) | 19·6 (16·8 to 22·6)* | 1·1 (0·7 to 1·6)* | ||
| Diet high in red meat: all causes | 37 (16 to 60) | 43 (19 to 69) | 14·8 (11·8 to 18·0)* | 5·8 (3·4 to 8·3)* | 1476 (549 to 2473) | 1752 (638 to 2957) | 18·7 (14·8 to 21·7)* | 12·2 (8·2 to 15·1)* | ||
| Colon and rectal cancer | 20 (4 to 36) | 24 (5 to 42) | 17·1 (13·8 to 20·2)* | −4·5 (−6·2 to −2·7)* | 442 (93 to 778) | 504 (108 to 904) | 14·2 (10·8 to 17·5)* | −3·8 (−5·5 to −1·9)* | ||
| Diabetes mellitus | 17 (2 to 31) | 19 (2 to 35) | 12·2 (9·0 to 15·2)* | −14·1 (−16·5 to −11·7)* | 1034 (120 to 1958) | 1247 (146 to 2359) | 20·6 (17·2 to 23·5)* | −6·4 (−8·4 to −4·5)* | ||
| Diet high in processed meat: all causes | 476 (132 to 809) | 541 (156 to 914) | 13·8 (11·1 to 21·8)* | 3·7 (1·4 to 11·6)* | 13 088 (5240 to 20 672) | 14 907 (6450 to 23 452) | 13·9 (9·3 to 24·4)* | 7·2 (3·2 to 18·2)* | ||
| Colon and rectal cancer | 31 (17 to 46) | 37 (20 to 56) | 20·7 (17·6 to 23·6)* | −2·5 (−3·8 to −1·3)* | 644 (350 to 964) | 745 (399 to 1123) | 15·8 (12·8 to 18·7)* | −2·7 (−4·0 to −1·4)* | ||
| Ischaemic heart disease | 363 (16 to 680) | 402 (17 to 759) | 10·7 (7·5 to 12·8)* | −4·0 (−5·3 to −2·7)* | 7931 (340 to 14 939) | 8401 (357 to 15 858) | 5·9 (1·8 to 8·5)* | −3·9 (−5·5 to −2·1)* | ||
| Diabetes mellitus | 82 (40 to 122) | 102 (50 to 153) | 24·8 (20·5 to 29·1)* | −4·9 (−6·5 to −3·5)* | 4513 (2121 to 7031) | 5761 (2708 to 8961) | 27·6 (24·3 to 30·7)* | −0·9 (−2·1 to 0·3) | ||
| Diet high in sugar-sweetened beverages: all causes | 34 (23 to 47) | 39 (27 to 55) | 15·3 (12·5 to 18·0)* | 7·3 (5·1 to 9·2)* | 1234 (852 to 1748) | 1449 (1004 to 2059) | 17·4 (14·3 to 20·3)* | 12·3 (9·9 to 14·7)* | ||
| Oesophageal cancer | 1 (0 to 1) | 1 (0 to 1) | 16·0 (9·5 to 21·3)* | 21·7 (13·7 to 28·3)* | 13 (4 to 24) | 15 (4 to 27) | 13·0 (6·3 to 18·6)* | 22·7 (14·8 to 29·5)* | ||
| Colon and rectum cancer | 1 (0 to 1) | 1 (0 to 1) | 19·9 (16·4 to 23·5)* | −1·8 (−4·4 to 0·7) | 14 (9 to 21) | 17 (11 to 24) | 17·8 (14·1 to 21·3)* | −0·1 (−3·0 to 2·8) | ||
| Liver cancer due to hepatitis B | 0 (0 to 0) | 0 (0 to 0) | 21·7 (13·0 to 30·4)* | 21·8 (12·2 to 30·7)* | 5 (2 to 9) | 6 (3 to 10) | 17·7 (8·5 to 27·3)* | 24·4 (13·5 to 33·8)* | ||
| Liver cancer due to hepatitis C | 0 (0 to 0) | 0 (0 to 0) | 28·9 (23·8 to 33·9)* | 6·7 (3·1 to 10·5)* | 4 (2 to 6) | 5 (2 to 8) | 25·3 (19·8 to 31·0)* | 9·2 (4·9 to 13·7)* | ||
| Liver cancer due to alcohol use | 0 (0 to 0) | 0 (0 to 0) | 30·5 (24·2 to 36·6)* | 3·5 (−4·2 to 9·1) | 5 (2 to 9) | 7 (3 to 12) | 28·1 (21·0 to 35·2)* | 4·2 (−4·7 to 10·6) | ||
| Liver cancer due to other causes | 0 (0 to 0) | 0 (0 to 0) | 26·6 (19·3 to 33·4)* | 25·0 (16·3 to 33·2)* | 3 (1 to 5) | 3 (2 to 5) | 21·3 (13·4 to 28·3)* | 28·3 (18·4 to 37·2)* | ||
| Gallbladder and biliary tract cancer | 0 (0 to 0) | 0 (0 to 0) | 8·2 (−0·3 to 14·6) | −3·4 (−7·5 to −0·3)* | 4 (2 to 6) | 4 (2 to 6) | 4·9 (−2·7 to 11·0) | −1·5 (−6·1 to 2·0) | ||
| Pancreatic cancer | 0 (0 to 0) | 0 (0 to 0) | 25·2 (22·0 to 28·8)* | −3·7 (−6·1 to −1·5)* | 4 (2 to 8) | 5 (2 to 10) | 22·0 (18·7 to 25·9)* | −3·0 (−5·4 to −0·4)* | ||
| Breast cancer | 0 (0 to 0) | 0 (0 to 0) | 25·6 (18·1 to 33·7)* | 2·1 (−2·2 to 7·3) | 8 (5 to 11) | 10 (6 to 14) | 26·6 (17·5 to 36·1)* | 3·5 (−1·6 to 9·1) | ||
| Uterine cancer | 0 (0 to 0) | 0 (0 to 0) | 18·5 (11·9 to 25·7)* | 7·7 (3·6 to 11·9)* | 6 (4 to 9) | 8 (5 to 11) | 19·1 (11·7 to 26·8)* | 10·5 (5·7 to 15·3)* | ||
| Ovarian cancer | 0 (0 to 0) | 0 (0 to 0) | 18·5 (0·0 to 22·9)* | −1·3 (−4·0 to 1·4) | 1 (0 to 2) | 1 (0 to 3) | 17·9 (0·0 to 22·7)* | −0·4 (−3·4 to 2·5) | ||
| Kidney cancer | 0 (0 to 0) | 0 (0 to 0) | 25·6 (21·4 to 29·9)* | −4·1 (−6·6 to −1·7)* | 6 (4 to 9) | 7 (5 to 11) | 23·2 (18·9 to 27·5)* | −3·9 (−7·4 to −0·5)* | ||
| Thyroid cancer | 0 (0 to 0) | 0 (0 to 0) | 25·9 (20·9 to 30·9)* | 1·7 (−2·4 to 7·3) | 1 (0 to 1) | 1 (1 to 2) | 46·0 (35·5 to 55·2)* | 12·7 (5·5 to 20·1)* | ||
| Ischaemic heart disease | 12 (8 to 17) | 13 (9 to 18) | 8·4 (5·6 to 11·0)* | −4·4 (−6·4 to −2·5)* | 326 (224 to 462) | 348 (236 to 494) | 6·7 (3·8 to 9·3)* | −1·9 (−4·1 to 0·2) | ||
| Ischaemic stroke | 2 (1 to 3) | 2 (1 to 3) | 2·7 (−1·5 to 6·7) | −1·1 (−4·0 to 1·9) | 53 (37 to 75) | 55 (39 to 78) | 3·8 (0·3 to 7·2)* | 3·5 (0·8 to 6·5)* | ||
| Haemorrhagic stroke | 5 (4 to 8) | 6 (4 to 8) | 7·5 (3·2 to 11·7)* | 9·0 (5·1 to 12·2)* | 186 (130 to 263) | 198 (137 to 280) | 6·6 (2·3 to 10·8)* | 10·9 (7·3 to 14·2)* | ||
| Hypertensive heart disease | 2 (1 to 3) | 3 (2 to 4) | 20·9 (14·5 to 26·9)* | −2·4 (−6·8 to 3·2) | 59 (39 to 86) | 68 (45 to 100) | 16·0 (10·8 to 21·0)* | 0·2 (−3·6 to 4·5) | ||
| Cardiomyopathy and myocarditis | .. | .. | .. | .. | .. | .. | .. | .. | ||
| Atrial fibrillation and flutter | .. | .. | .. | .. | .. | .. | .. | .. | ||
| Peripheral vascular disease | .. | .. | .. | .. | .. | .. | .. | .. | ||
| Endocarditis | .. | .. | .. | .. | .. | .. | .. | .. | ||
| Other cardiovascular and circulatory diseases | .. | .. | .. | .. | .. | .. | .. | .. | ||
| Diabetes mellitus | 6 (4 to 8) | 7 (5 to 11) | 23·2 (19·3 to 27·0)* | −5·1 (−7·7 to −2·3)* | 378 (248 to 559) | 488 (315 to 731) | 28·9 (25·3 to 32·3)* | 0·9 (−1·4 to 3·1) | ||
| Chronic kidney disease due to diabetes mellitus | 1 (1 to 2) | 2 (1 to 4) | 51·5 (44·8 to 58·8)* | 8·7 (5·0 to 12·2)* | 43 (19 to 75) | 62 (28 to 107) | 43·8 (37·8 to 51·5)* | 8·5 (5·3 to 11·7)* | ||
| Chronic kidney disease due to hypertension | 1 (1 to 2) | 2 (1 to 3) | 28·4 (19·6 to 38·6)* | −4·5 (−8·4 to −0·5)* | 33 (15 to 58) | 42 (19 to 73) | 24·7 (19·9 to 30·8)* | −1·4 (−4·9 to 1·8) | ||
| Chronic kidney disease due to glomerulonephritis | 0 (0 to 0) | 0 (0 to 1) | 27·5 (18·3 to 38·1)* | 7·3 (2·5 to 12·1)* | 12 (4 to 24) | 15 (5 to 29) | 24·6 (19·7 to 33·5)* | 12·8 (8·9 to 16·9)* | ||
| Chronic kidney disease due to other causes | 0 (0 to 0) | 0 (0 to 0) | 36·1 (21·8 to 49·1)* | 5·6 (−0·1 to 11·3) | 8 (3 to 15) | 10 (4 to 18) | 28·3 (22·9 to 36·4)* | 5·0 (2·0 to 8·0)* | ||
| Diet low in fibre: all causes | 334 (158 to 578) | 387 (183 to 670) | 15·8 (12·4 to 19·6)* | 4·3 (1·6 to 7·1)* | 7666 (3534 to 13 299) | 8393 (3908 to 14 657) | 9·5 (5·6 to 13·8)* | 3·6 (0·1 to 7·1)* | ||
| Colon and rectal cancer | 38 (17 to 66) | 47 (21 to 83) | 24·4 (20·6 to 28·9)* | −0·5 (−2·8 to 2·1) | 741 (327 to 1318) | 870 (385 to 1545) | 17·4 (13·5 to 21·5)* | −1·4 (−4·1 to 1·4) | ||
| Ischaemic heart disease | 297 (136 to 531) | 340 (156 to 610) | 14·7 (11·5 to 18·5)* | −1·6 (−4·0 to 0·7) | 6925 (3137 to 12 333) | 7523 (3410 to 13 333) | 8·6 (4·7 to 12·9)* | −0·5 (−3·3 to 2·2) | ||
| Diet low in calcium: all causes | 127 (74 to 185) | 160 (95 to 232) | 26·1 (23·3 to 29·7)* | 14·9 (12·4 to 17·6)* | 2721 (1608 to 3966) | 3284 (1966 to 4755) | 20·7 (17·6 to 24·3)* | 13·0 (10·1 to 16·2)* | ||
| Colon and rectal cancer | 127 (74 to 185) | 160 (95 to 232) | 26·1 (23·3 to 29·7)* | 2·3 (1·3 to 3·9)* | 2721 (1608 to 3966) | 3284 (1966 to 4755) | 20·7 (17·6 to 24·3)* | 2·0 (1·0 to 3·5)* | ||
| Diet low in seafood omega-3 fatty acids: all causes | 1279 (537 to 2079) | 1472 (616 to 2378) | 15·0 (12·5 to 17·5)* | 5·3 (3·7 to 6·8)* | 28 350 (11 995 to 45 414) | 31 310 (13 272 to 49 823) | 10·4 (7·2 to 13·3)* | 4·1 (1·2 to 6·8)* | ||
| Ischaemic heart disease | 1279 (537 to 2079) | 1472 (616 to 2378) | 15·0 (12·5 to 17·5)* | 0·3 (−0·3 to 0·9) | 28 350 (11 995 to 45 414) | 31 310 (13 272 to 49 823) | 10·4 (7·2 to 13·3)* | 0·6 (−0·1 to 1·4) | ||
| Diet low in polyunsaturated fatty acids: all causes | 348 (145 to 548) | 388 (158 to 610) | 11·5 (3·6 to 20·8)* | 1·2 (−6·1 to 10·3) | 7535 (3243 to 11 727) | 8270 (3534 to 12 996) | 9·7 (2·0 to 18·7)* | 2·9 (−4·4 to 11·3) | ||
| Ischaemic heart disease | 348 (145 to 548) | 388 (158 to 610) | 11·5 (3·6 to 20·8)* | −3·6 (−10·5 to 4·7) | 7535 (3243 to 11 727) | 8270 (3534 to 12 996) | 9·7 (2·0 to 18·7)* | −0·6 (−7·3 to 6·7) | ||
| Diet high in trans fatty acids: all causes | 384 (158 to 713) | 448 (190 to 827) | 16·7 (13·1 to 22·8)* | 7·8 (4·8 to 13·4)* | 10 121 (4348 to 18 081) | 11 578 (5138 to 20 322) | 14·4 (9·9 to 21·4)* | 8·9 (4·6 to 15·6)* | ||
| Ischaemic heart disease | 384 (158 to 713) | 448 (190 to 827) | 16·7 (13·1 to 22·8)* | 2·7 (0·4 to 7·6)* | 10 121 (4348 to 18 081) | 11 578 (5138 to 20 322) | 14·4 (9·9 to 21·4)* | 5·2 (2·4 to 11·0)* | ||
| Diet high in sodium: all causes | 3668 (2145 to 5680) | 4130 (2446 to 6419) | 12·6 (8·3 to 16·9)* | 2·8 (−0·1 to 6·3) | 77 456 (45 739 to 118 672) | 83 008 (49 326 to 127 452) | 7·2 (2·7 to 11·3)* | 0·2 (−3·4 to 3·8) | ||
| Stomach cancer | 413 (271 to 567) | 397 (246 to 553) | −3·9 (−11·9 to 3·0) | −2·9 (−7·7 to 0·6) | 9470 (6286 to 12 765) | 8540 (5502 to 11 691) | −9·8 (−17·2 to −3·7)* | −3·4 (−7·8 to −0·4)* | ||
| Rheumatic heart disease | 30 (14 to 53) | 28 (13 to 51) | −7·6 (−15·4 to −1·3)* | −4·9 (−11·3 to −0·1)* | 873 (420 to 1603) | 772 (359 to 1428) | −11·6 (−19·0 to −6·1)* | −6·6 (−13·1 to −2·1)* | ||
| Ischaemic heart disease | 1348 (682 to 2306) | 1632 (852 to 2754) | 21·1 (16·7 to 27·8)* | 4·7 (2·0 to 9·7)* | 26 945 (13 814 to 45 258) | 31 088 (16 524 to 51 139) | 15·4 (11·2 to 21·3)* | 3·8 (1·6 to 8·1)* | ||
| Ischaemic stroke | 513 (278 to 848) | 562 (308 to 916) | 9·5 (3·7 to 17·1)* | 3·4 (0·1 to 9·1)* | 9239 (5141 to 14731) | 9756 (5537 to 15 527) | 5·6 (0·6 to 11·8)* | 3·6 (0·6 to 8·6)* | ||
| Haemorrhagic stroke | 876 (516 to 1340) | 875 (514 to 1347) | −0·0 (−6·1 to 6·0) | −2·7 (−7·0 to 1·4) | 19 630 (11 721 to 29 698) | 19 052 (11 138 to 28 916) | −2·9 (−9·2 to 2·6) | −3·1 (−7·5 to 0·8) | ||
| Hypertensive heart disease | 246 (88 to 484) | 325 (116 to 634) | 32·2 (18·7 to 45·3)* | 4·3 (−0·6 to 11·9) | 4756 (2134 to 8876) | 5810 (2603 to 10 709) | 22·2 (13·2 to 30·9)* | 2·8 (−0·5 to 8·4) | ||
| Cardiomyopathy and myocarditis | 28 (12 to 51) | 31 (14 to 57) | 12·0 (5·8 to 20·4)* | 3·5 (0·3 to 9·3)* | 737 (312 to 1377) | 764 (342 to 1396) | 3·6 (−2·0 to 11·1) | 4·3 (0·9 to 10·6)* | ||
| Atrial fibrillation and flutter | 14 (6 to 25) | 19 (9 to 35) | 39·1 (34·0 to 46·2)* | 4·0 (1·6 to 9·2)* | 449 (221 to 790) | 592 (297 to 1033) | 31·9 (28·8 to 37·4)* | 4·8 (2·6 to 9·3)* | ||
| Aortic aneurysm | 13 (6 to 24) | 16 (8 to 30) | 25·9 (19·0 to 32·8)* | 2·5 (0·3 to 6·2)* | 262 (124 to 460) | 319 (153 to 559) | 21·8 (14·4 to 28·2)* | 2·5 (0·4 to 5·9)* | ||
| Peripheral vascular disease | 2 (1 to 4) | 3 (1 to 6) | 38·4 (30·2 to 49·6)* | 2·9 (−0·4 to 10·0) | 70 (28 to 140) | 97 (40 to 192) | 37·7 (32·4 to 45·6)* | 6·4 (3·3 to 12·7)* | ||
| Endocarditis | 6 (2 to 10) | 7 (3 to 13) | 28·6 (22·6 to 35·9)* | 3·4 (0·3 to 8·1)* | 133 (59 to 248) | 163 (73 to 299) | 22·6 (15·9 to 29·9)* | 3·2 (−0·8 to 7·7) | ||
| Other cardiovascular and circulatory diseases | 50 (25 to 85) | 59 (29 to 100) | 18·1 (11·9 to 24·4)* | 0·4 (−3·1 to 5·0) | 1584 (804 to 2703) | 1920 (993 to 3246) | 21·3 (16·3 to 27·4)* | 3·7 (1·0 to 8·2)* | ||
| Chronic kidney disease due to diabetes mellitus | 41 (18 to 74) | 57 (25 to 103) | 39·3 (33·0 to 44·8)* | −0·6 (−3·6 to 2·0) | 1048 (467 to 1909) | 1391 (635 to 2500) | 32·7 (27·2 to 37·9)* | 0·2 (−2·6 to 3·1) | ||
| Chronic kidney disease due to hypertension | 52 (22 to 99) | 75 (32 to 139) | 42·1 (36·0 to 49·9)* | 4·4 (1·8 to 9·1)* | 1107 (479 to 2079) | 1467 (639 to 2717) | 32·5 (27·3 to 38·8)* | 4·1 (1·5 to 8·6)* | ||
| Chronic kidney disease due to glomerulonephritis | 35 (18 to 57) | 40 (21 to 67) | 15·1 (6·5 to 22·8)* | −2·9 (−8·9 to 2·1) | 918 (471 to 1516) | 971 (496 to 1648) | 5·8 (−2·3 to 13·0) | −4·6 (−11·2 to 0·3) | ||
| Chronic kidney disease due to other causes | 2 (1 to 4) | 3 (1 to 6) | 43·8 (34·1 to 54·4)* | 7·5 (3·0 to 12·7)* | 236 (98 to 449) | 306 (131 to 576) | 29·9 (26·2 to 34·6)* | 4·8 (2·6 to 8·4)* | ||
| Sexual abuse and violence: all causes | 338 (244 to 444) | 281 (199 to 378) | −16·9 (−23·6 to −9·4)* | −15·2 (−21·9 to −8·3)* | 22 527 (17 002 to 28 715) | 20 801 (15 633 to 26 810) | −7·7 (−14·0 to −1·5)* | −4·0 (−9·8 to 2·2) | ||
| Childhood sexual abuse: all causes | 118 (34 to 229) | 113 (31 to 221) | −4·9 (−11·8 to 1·1) | −3·1 (−10·2 to 2·6) | 8200 (3468 to 14 180) | 8107 (3472 to 14 062) | −1·1 (−8·5 to 5·8) | 3·7 (−3·3 to 10·6) | ||
| Alcohol use disorders | 7 (0 to 16) | 6 (0 to 13) | −22·0 (−26·6 to 0·0) | −10·1 (−12·5 to 0·0) | 568 (0 to 1299) | 512 (0 to 1183) | −9·9 (−14·6 to 0·0) | −6·3 (−8·3 to 0·0) | ||
| Major depressive disorder | .. | .. | .. | .. | 2062 (231 to 4518) | 2321 (257 to 5097) | 12·5 (10·7 to 14·0)* | −3·7 (−5·0 to −2·6)* | ||
| Dysthymia | .. | .. | .. | .. | 426 (46 to 943) | 484 (53 to 1074) | 13·8 (11·3 to 15·9)* | −4·1 (−5·4 to −2·8)* | ||
| Self-harm | 111 (27 to 222) | 107 (27 to 213) | −3·8 (−10·5 to 2·1) | −2·5 (−4·5 to −0·7)* | 5145 (1265 to 10 175) | 4791 (1194 to 9542) | −6·9 (−13·6 to −0·9)* | −1·8 (−3·8 to 0·0) | ||
| Intimate partner violence: all causes | 237 (180 to 293) | 186 (148 to 224) | −21·8 (−28·1 to −12·9)* | −20·1 (−26·5 to −11·9)* | 15 431 (12 234 to 19 068) | 13 803 (11 078 to 16 954) | −10·5 (−17·8 to −2·8)* | −7·4 (−14·0 to 0·1) | ||
| HIV/AIDS—tuberculosis | 20 (11 to 31) | 10 (5 to 16) | −49·0 (−52·8 to −44·1)* | −18·0 (−23·3 to −13·0)* | 937 (490 to 1432) | 496 (251 to 775) | −47·1 (−50·6 to −42·5)* | −15·3 (−20·0 to −10·5)* | ||
| HIV/AIDS resulting in other diseases | 86 (45 to 128) | 49 (25 to 72) | −43·5 (−47·8 to −38·9)* | −18·7 (−23·9 to −13·3)* | 4301 (2252 to 6424) | 2520 (1287 to 3716) | −41·4 (−45·9 to −36·8)* | −17·4 (−22·4 to −12·0)* | ||
| Maternal abortion, miscarriage, and ectopic pregnancy | 0 (0 to 0) | 0 (0 to 0) | −22·8 (−36·5 to −5·4)* | 0·2 (−11·4 to 12·9) | 0 (0 to 0) | 0 (0 to 0) | −23·2 (−36·6 to −6·0)* | 0·1 (−10·5 to 13·3) | ||
| Major depressive disorder | .. | .. | .. | .. | 3562 (2279 to 5110) | 4405 (2825 to 6361) | 23·7 (21·3 to 26·0)* | 2·8 (1·1 to 4·6)* | ||
| Dysthymia | .. | .. | .. | .. | 775 (496 to 1148) | 980 (623 to 1438) | 26·4 (23·3 to 29·8)* | 4·0 (2·3 to 6·0)* | ||
| Self-harm | 104 (72 to 126) | 103 (74 to 126) | −1·1 (−11·1 to 13·2) | −2·2 (−9·6 to 6·6) | 4367 (2950 to 5417) | 4107 (2944 to 5117) | −5·9 (−16·3 to 9·1) | −3·1 (−10·7 to 6·9) | ||
| Assault by firearm | 6 (5 to 7) | 6 (5 to 7) | 2·2 (−5·9 to 13·8) | −4·8 (−12·2 to 4·9) | 315 (252 to 356) | 312 (256 to 366) | −1·0 (−9·4 to 11·1) | −4·7 (−12·7 to 5·8) | ||
| Assault by sharp object | 7 (6 to 7) | 5 (5 to 6) | −18·4 (−25·1 to −10·6)* | −4·8 (−12·0 to 2·4) | 340 (305 to 379) | 269 (238 to 302) | −21·0 (−28·1 to −12·6)* | −5·5 (−13·2 to 2·3) | ||
| Assault by other means | 14 (13 to 15) | 12 (11 to 14) | −12·3 (−19·6 to −4·2)* | −3·8 (−10·7 to 3·3) | 835 (760 to 913) | 715 (624 to 805) | −14·3 (−21·5 to −6·0)* | −4·6 (−11·4 to 2·7) | ||
| Unsafe sex: all causes | 2051 (1957 to 2156) | 1452 (1381 to 1541) | −29·2 (−31·6 to −26·1)* | −26·2 (−28·9 to −23·1)* | 112 703 (106 333 to 120 086) | 79 451 (74 248 to 85 532) | −29·5 (−32·0 to −26·8)* | −24·7 (−27·4 to −21·8)* | ||
| HIV/AIDS—tuberculosis | 334 (267 to 379) | 199 (152 to 231) | −40·3 (−44·9 to −34·8)* | −0·8 (−1·4 to −0·4)* | 18 403 (14 762 to 20 870) | 10 990 (8439 to 12 703) | −40·3 (−44·7 to −34·7)* | −0·7 (−1·1 to −0·3)* | ||
| HIV/AIDS resulting in other diseases | 1356 (1271 to 1455) | 906 (844 to 981) | −33·2 (−36·6 to −29·1)* | −1·8 (−2·5 to −1·4)* | 75 102 (70 586 to 80 394) | 51 167 (47 789 to 55 057) | −31·9 (−35·1 to −28·3)* | −1·5 (−2·1 to −1·1)* | ||
| Syphilis | 134 (80 to 206) | 107 (63 to 165) | −20·3 (−28·5 to −12·4)* | .. | 11 190 (6607 to 17 281) | 8957 (5273 to 13 970) | −20·0 (−28·4 to −11·8)* | .. | ||
| Chlamydial infection | 0 (0 to 0) | 0 (0 to 0) | −5·3 (−17·0 to 10·6) | .. | 337 (194 to 538) | 370 (214 to 595) | 9·7 (6·5 to 13·0)* | .. | ||
| Gonococcal infection | 1 (1 to 1) | 1 (1 to 1) | −15·7 (−26·7 to −4·7)* | .. | 383 (239 to 573) | 470 (283 to 717) | 22·7 (15·9 to 28·1)* | .. | ||
| Trichomoniasis | .. | .. | .. | .. | 167 (67 to 355) | 194 (78 to 412) | 16·1 (15·0 to 17·2)* | .. | ||
| Genital herpes | .. | .. | .. | .. | 198 (61 to 468) | 236 (74 to 556) | 19·5 (17·4 to 23·0)* | .. | ||
| Other sexually transmitted diseases | 0 (0 to 0) | 0 (0 to 0) | −16·8 (−27·6 to −6·1)* | .. | 103 (75 to 139) | 104 (74 to 141) | 0·3 (−3·1 to 3·2) | .. | ||
| Cervical cancer | 225 (214 to 238) | 239 (225 to 252) | 5·8 (−0·5 to 13·8) | .. | 6819 (6393 to 7236) | 6963 (6526 to 7408) | 2·1 (−4·5 to 10·5) | .. | ||
| Low physical activity: all causes | 1351 (1047 to 1661) | 1605 (1265 to 1956) | 18·9 (16·5 to 21·6)* | 7·0 (5·3 to 9·1)* | 29 467 (22 694 to 36 268) | 34 603 (26 905 to 42 282) | 17·4 (14·4 to 20·5)* | 9·1 (6·8 to 11·8)* | ||
| Colon and rectal cancer | 95 (66 to 124) | 119 (84 to 156) | 25·2 (22·5 to 28·1)* | 0·8 (0·2 to 1·6)* | 1838 (1263 to 2441) | 2209 (1529 to 2916) | 20·2 (17·7 to 22·9)* | 0·8 (0·1 to 1·8)* | ||
| Breast cancer | 39 (28 to 50) | 48 (35 to 61) | 22·1 (16·9 to 27·0)* | −0·3 (−1·5 to 1·3) | 1064 (765 to 1369) | 1276 (926 to 1644) | 20·0 (14·2 to 25·5)* | −0·1 (−1·6 to 1·7) | ||
| Ischaemic heart disease | 727 (476 to 992) | 859 (572 to 1161) | 18·1 (15·8 to 20·8)* | 1·3 (0·5 to 2·5)* | 14 621 (9264 to 20 247) | 16 673 (10 684 to 22 821) | 14·0 (11·2 to 17·2)* | 2·5 (1·6 to 4·1)* | ||
| Ischaemic stroke | 305 (169 to 449) | 333 (188 to 485) | 9·2 (6·1 to 12·8)* | 1·3 (0·4 to 3·0)* | 5049 (2688 to 7537) | 5291 (2875 to 7911) | 4·8 (1·4 to 8·4)* | 2·1 (1·1 to 3·8)* | ||
| Diabetes mellitus | 184 (142 to 229) | 247 (192 to 306) | 34·2 (30·1 to 38·2)* | 0·6 (−0·3 to 1·5) | 6896 (4991 to 9242) | 9154 (6647 to 12 251) | 32·7 (29·8 to 35·5)* | 1·4 (0·8 to 2·1)* | ||
| Metabolic risks: all causes | 14 403 (13 691 to 15 063) | 16 860 (16 021 to 17 697) | 17·1 (15·1 to 19·2)* | 6·0 (5·1 to 7·0)* | 335 227 (315 739 to 357 389) | 381 845 (357 846 to 409 436) | 13·9 (11·5 to 16·0)* | 6·9 (5·2 to 8·4)* | ||
| High fasting plasma glucose: all causes | 4212 (3647 to 5047) | 5240 (4547 to 6217) | 24·4 (21·5 to 27·4)* | 13·3 (11·5 to 15·3)* | 117 101 (102 561 to 133 960) | 143 076 (125 125 to 163 477) | 22·2 (19·5 to 24·8)* | 15·3 (13·1 to 17·5)* | ||
| Tuberculosis | 133 (83 to 189) | 118 (73 to 169) | −11·1 (−19·7 to −3·5)* | 5·4 (2·1 to 8·3)* | 4313 (2737 to 5960) | 3802 (2430 to 5304) | −11·9 (−19·5 to −5·2)* | 4·2 (−0·6 to 8·1) | ||
| Ischaemic heart disease | 1415 (946 to 2016) | 1761 (1175 to 2528) | 24·4 (19·9 to 29·1)* | 6·8 (5·3 to 8·4)* | 27 891 (19 565 to 37 687) | 33 535 (23 674 to 45 228) | 20·2 (17·1 to 23·4)* | 8·1 (6·9 to 9·5)* | ||
| Ischaemic stroke | 454 (257 to 803) | 514 (291 to 913) | 13·2 (7·9 to 20·3)* | 6·0 (4·0 to 8·6)* | 7750 (4771 to 12 343) | 8524 (5350 to 13 291) | 10·0 (6·0 to 14·3)* | 7·6 (6·1 to 9·6)* | ||
| Haemorrhagic stroke | 529 (366 to 728) | 585 (408 to 802) | 10·5 (6·4 to 15·6)* | 8·3 (6·8 to 10·2)* | 12 434 (8510 to 17 327) | 13 556 (9361 to 18 929) | 9·0 (5·3 to 13·1)* | 9·7 (8·3 to 11·5)* | ||
| Diabetes mellitus | 1150 (1121 to 1177) | 1519 (1470 to 1576) | 32·1 (27·7 to 36·3)* | .. | 49 725 (41 868 to 58 982) | 64 135 (53 490 to 76 113) | 29·0 (26·2 to 31·7)* | .. | ||
| Chronic kidney disease due to diabetes mellitus | 299 (279 to 314) | 418 (389 to 441) | 39·5 (35·4 to 43·5)* | .. | 8713 (7991 to 9466) | 11 258 (10 303 to 12 225) | 29·2 (25·9 to 32·5)* | .. | ||
| Chronic kidney disease due to hypertension | 149 (105 to 192) | 216 (153 to 278) | 44·9 (39·7 to 50·1)* | 6·2 (5·1 to 7·4)* | 3260 (2284 to 4222) | 4467 (3172 to 5743) | 37·0 (32·0 to 42·4)* | 8·0 (6·6 to 9·4)* | ||
| Chronic kidney disease due to glomerulonephritis | 68 (48 to 89) | 89 (63 to 114) | 30·0 (24·2 to 36·0)* | 9·2 (7·6 to 11·0)* | 2106 (1466 to 2770) | 2570 (1805 to 3358) | 22·1 (17·1 to 27·1)* | 10·5 (8·5 to 12·6)* | ||
| Chronic kidney disease due to other causes | 6 (4 to 8) | 9 (6 to 12) | 47·2 (39·6 to 55·6)* | 10·3 (7·8 to 13·1)* | 695 (453 to 983) | 936 (615 to 1313) | 34·6 (31·8 to 37·5)* | 9·3 (7·6 to 11·2)* | ||
| High total cholesterol: all causes | 3816 (2973 to 4849) | 4313 (3324 to 5512) | 13·0 (9·5 to 16·2)* | 1·4 (−0·6 to 3·2) | 81 691 (68 219 to 96 877) | 88 687 (74 558 to 105 681) | 8·6 (5·8 to 11·0)* | 0·9 (−1·5 to 3·1) | ||
| Ischaemic heart disease | 3279 (2594 to 4016) | 3743 (2906 to 4650) | 14·1 (10·2 to 17·7)* | −2·2 (−3·5 to −1·0)* | 71 723 (60 172 to 84 381) | 78 590 (65 999 to 92 772) | 9·6 (6·6 to 12·1)* | −1·3 (−2·0 to −0·6)* | ||
| Ischaemic stroke | 537 (220 to 1058) | 569 (221 to 1127) | 6·0 (−1·8 to 11·5) | −2·7 (−6·2 to −0·5)* | 9968 (5939 to 16 618) | 10 098 (5961 to 16 912) | 1·3 (−2·7 to 4·9) | −2·0 (−3·5 to −0·5)* | ||
| High systolic blood pressure: all causes | 9212 (8326 to 10 101) | 10 704 (9601 to 11 787) | 16·2 (13·9 to 18·6)* | 5·2 (4·0 to 6·4)* | 18 9579 (172 703 to 206 696) | 211 816 (192 712 to 231 114) | 11·7 (9·2 to 14·1)* | 4·4 (2·2 to 6·4)* | ||
| Rheumatic heart disease | 79 (54 to 117) | 80 (56 to 121) | 1·7 (−3·2 to 7·0) | 4·4 (2·9 to 6·3)* | 2377 (1588 to 3481) | 2363 (1615 to 3402) | −0·6 (−4·9 to 3·9) | 5·4 (3·6 to 7·3)* | ||
| Ischaemic heart disease | 4135 (3408 to 4840) | 4862 (3955 to 5740) | 17·6 (14·7 to 20·2)* | 0·9 (−0·0 to 1·7) | 79 828 (68 710 to 90 328) | 90 298 (77 837 to 102 138) | 13·1 (10·4 to 15·6)* | 1·4 (0·8 to 2·0)* | ||
| Ischaemic stroke | 1367 (1083 to 1656) | 1489 (1167 to 1821) | 8·9 (4·7 to 13·5)* | 1·8 (0·4 to 3·4)* | 22 995 (18 429 to 26 872) | 24 198 (19 500 to 28 264) | 5·2 (1·8 to 8·7)* | 2·6 (1·8 to 3·7)* | ||
| Haemorrhagic stroke | 1819 (1486 to 2144) | 1953 (1588 to 2313) | 7·4 (3·6 to 12·1)* | 4·4 (3·2 to 5·8)* | 41 530 (34 162 to 47 708) | 43 412 (36 092 to 49 999) | 4·5 (1·0 to 8·7)* | 4·7 (3·7 to 6·0)* | ||
| Hypertensive heart disease | 761 (712 to 824) | 962 (874 to 1025) | 26·5 (17·5 to 32·3)* | .. | 14 852 (13 919 to 16 053) | 17 485 (16 287 to 18 594) | 17·7 (11·6 to 22·9)* | .. | ||
| Cardiomyopathy and myocarditis | 121 (98 to 145) | 129 (104 to 157) | 7·3 (1·6 to 13·0)* | −1·1 (−3·3 to 1·2) | 3233 (2594 to 3859) | 3188 (2570 to 3795) | −1·4 (−6·3 to 4·0) | −0·4 (−2·9 to 2·3) | ||
| Atrial fibrillation and flutter | 50 (38 to 65) | 68 (50 to 90) | 35·2 (31·4 to 39·1)* | 0·0 (−1·2 to 1·3) | 1409 (1087 to 1820) | 1810 (1398 to 2347) | 28·5 (26·8 to 30·2)* | 1·2 (0·6 to 1·9)* | ||
| Aortic aneurysm | 49 (39 to 58) | 60 (47 to 71) | 22·7 (17·3 to 27·2)* | −1·1 (−2·0 to −0·2)* | 928 (771 to 1080) | 1110 (925 to 1291) | 19·7 (13·6 to 23·7)* | 0·3 (−0·4 to 1·1) | ||
| Peripheral vascular disease | 11 (8 to 14) | 14 (10 to 19) | 33·0 (25·1 to 42·0)* | −2·4 (−4·3 to −0·5)* | 265 (184 to 386) | 346 (235 to 505) | 30·4 (26·2 to 34·9)* | 0·0 (−1·2 to 1·1) | ||
| Endocarditis | 22 (17 to 28) | 28 (22 to 36) | 26·7 (21·8 to 31·6)* | 0·8 (−0·5 to 2·0) | 518 (403 to 644) | 640 (496 to 792) | 23·5 (18·0 to 29·1)* | 3·7 (1·0 to 6·3)* | ||
| Other cardiovascular and circulatory diseases | 176 (154 to 199) | 211 (182 to 240) | 19·8 (15·0 to 24·4)* | 0·8 (−0·2 to 1·7) | 5165 (4411 to 6058) | 6267 (5304 to 7424) | 21·3 (17·6 to 25·1)* | 3·5 (2·4 to 4·7)* | ||
| Chronic kidney disease due to diabetes mellitus | 132 (95 to 167) | 190 (135 to 240) | 43·5 (39·5 to 47·5)* | 1·6 (0·9 to 2·4)* | 3186 (2231 to 4120) | 4365 (3085 to 5671) | 37·0 (33·5 to 40·5)* | 3·0 (2·3 to 3·8)* | ||
| Chronic kidney disease due to hypertension | 409 (377 to 428) | 550 (502 to 576) | 34·5 (30·0 to 38·7)* | .. | 10 366 (9401 to 10 985) | 12 737 (11 489 to 13 554) | 22·9 (18·6 to 27·4)* | .. | ||
| Chronic kidney disease due to glomerulonephritis | 76 (54 to 97) | 98 (71 to 125) | 28·8 (23·9 to 34·0)* | 7·1 (5·5 to 8·8)* | 2151 (1481 to 2852) | 2584 (1808 to 3384) | 20·1 (15·9 to 24·5)* | 7·5 (5·5 to 9·6)* | ||
| Chronic kidney disease due to other causes | 8 (6 to 11) | 12 (8 to 15) | 42·2 (34·0 to 50·6)* | 5·3 (2·7 to 8·1)* | 777 (513 to 1063) | 1013 (668 to 1386) | 30·4 (28·1 to 33·1)* | 4·6 (3·2 to 6·2)* | ||
| High body-mass index: all causes | 3314 (2241 to 4504) | 3960 (2728 to 5332) | 19·5 (15·8 to 23·6)* | 10·0 (7·2 to 13·5)* | 98 478 (67 219 to 131 972) | 120 132 (83 829 to 158 409) | 22·0 (18·1 to 26·8)* | 14·8 (11·7 to 19·0)* | ||
| Oesophageal cancer | 67 (20 to 123) | 71 (22 to 130) | 6·2 (−3·4 to 16·8) | 10·7 (1·3 to 20·5)* | 1573 (459 to 2901) | 1644 (516 to 3015) | 4·5 (−5·3 to 15·8) | 12·3 (2·8 to 22·9)* | ||
| Colon and rectal cancer | 48 (29 to 70) | 62 (38 to 91) | 28·9 (25·5 to 32·9)* | 4·7 (2·5 to 7·3)* | 1050 (632 to 1527) | 1329 (809 to 1924) | 26·6 (23·3 to 30·6)* | 6·2 (4·0 to 8·8)* | ||
| Liver cancer due to hepatitis B | 24 (9 to 48) | 28 (11 to 54) | 17·9 (8·3 to 35·0)* | 16·0 (9·9 to 25·7)* | 762 (268 to 1511) | 870 (326 to 1678) | 14·2 (3·9 to 33·3)* | 18·5 (11·5 to 29·7)* | ||
| Liver cancer due to hepatitis C | 15 (6 to 26) | 20 (9 to 35) | 32·8 (25·8 to 40·8)* | 9·2 (4·0 to 14·4)* | 325 (141 to 574) | 421 (186 to 733) | 29·5 (21·7 to 38·8)* | 12·0 (6·2 to 18·4)* | ||
| Liver cancer due to alcohol use | 21 (8 to 41) | 30 (11 to 56) | 38·0 (28·8 to 50·1)* | 8·9 (3·6 to 13·9)* | 529 (202 to 1034) | 729 (282 to 1393) | 37·7 (27·3 to 52·3)* | 11·2 (5·8 to 17·3)* | ||
| Liver cancer due to other causes | 12 (5 to 22) | 14 (6 to 25) | 18·4 (9·2 to 31·4)* | 16·3 (8·8 to 26·6)* | 317 (127 to 583) | 360 (150 to 646) | 13·3 (3·6 to 28·1)* | 18·7 (10·2 to 30·1)* | ||
| Gallbladder and biliary tract cancer | 18 (10 to 27) | 21 (12 to 31) | 14·5 (6·3 to 22·5)* | 1·2 (−3·1 to 5·2) | 362 (209 to 547) | 402 (233 to 596) | 11·0 (3·6 to 18·6)* | 3·1 (−1·0 to 7·3) | ||
| Pancreatic cancer | 17 (6 to 29) | 23 (8 to 40) | 35·4 (31·6 to 39·5)* | 3·3 (0·6 to 5·7)* | 350 (122 to 614) | 463 (163 to 812) | 32·5 (28·8 to 36·7)* | 4·4 (2·0 to 6·8)* | ||
| Breast cancer | 25 (14 to 39) | 34 (20 to 52) | 36·5 (25·1 to 48·0)* | 7·9 (3·1 to 13·9)* | 551 (299 to 887) | 774 (439 to 1214) | 40·4 (24·5 to 57·5)* | 8·9 (1·7 to 17·3)* | ||
| Uterine cancer | 26 (17 to 35) | 31 (21 to 41) | 19·6 (11·4 to 28·9)* | 8·3 (5·1 to 13·1)* | 654 (441 to 891) | 780 (538 to 1041) | 19·2 (10·1 to 29·8)* | 10·0 (6·2 to 15·5)* | ||
| Ovarian cancer | 4 (0 to 9) | 5 (0 to 11) | 26·3 (22·1 to 31·7)* | 4·3 (2·3 to 7·5)* | 98 (−3 to 221) | 124 (−4 to 275) | 26·0 (21·5 to 31·7)* | 5·0 (2·8 to 8·6)* | ||
| Kidney cancer | 18 (12 to 24) | 24 (16 to 33) | 34·2 (29·8 to 38·8)* | 1·5 (−0·6 to 3·7) | 410 (272 to 565) | 541 (364 to 741) | 31·9 (27·7 to 36·3)* | 1·8 (−0·8 to 4·9) | ||
| Thyroid cancer | 2 (1 to 4) | 3 (2 to 5) | 32·5 (22·6 to 41·1)* | 5·9 (0·4 to 11·3)* | 62 (35 to 96) | 90 (50 to 141) | 45·6 (32·8 to 57·8)* | 10·6 (3·8 to 16·8)* | ||
| Ischaemic heart disease | 1228 (824 to 1687) | 1436 (960 to 1965) | 16·9 (13·2 to 20·9)* | 1·9 (−0·5 to 4·5) | 28 614 (19 490 to 38 838) | 33 038 (22 659 to 44 539) | 15·5 (12·1 to 19·1)* | 4·4 (2·3 to 6·9)* | ||
| Ischaemic stroke | 313 (203 to 449) | 320 (204 to 470) | 2·3 (−4·1 to 8·1) | −1·9 (−6·4 to 2·5) | 7020 (4693 to 9683) | 7318 (4859 to 10 062) | 4·2 (−0·1 to 8·9) | 2·7 (−0·6 to 6·4) | ||
| Haemorrhagic stroke | 606 (390 to 850) | 651 (431 to 894) | 7·3 (1·9 to 13·9)* | 6·9 (2·9 to 11·7)* | 18 122 (11 921 to 24 775) | 19 636 (13 414 to 26 434) | 8·4 (3·3 to 15·0)* | 10·3 (6·6 to 15·6)* | ||
| Hypertensive heart disease | 234 (144 to 341) | 308 (182 to 455) | 32·0 (20·8 to 42·0)* | 4·9 (−0·5 to 10·3) | 5010 (3364 to 6854) | 6313 (4255 to 8539) | 26·0 (19·4 to 33·6)* | 6·8 (3·3 to 11·2)* | ||
| Diabetes mellitus | 408 (293 to 532) | 555 (404 to 718) | 36·0 (30·5 to 42·2)* | 3·6 (0·9 to 6·8)* | 21 809 (15 245 to 29 011) | 30 396 (21 544 to 39 884) | 39·4 (34·7 to 44·8)* | 7·7 (5·3 to 11·4)* | ||
| Chronic kidney disease due to diabetes mellitus | 78 (40 to 124) | 119 (62 to 187) | 51·5 (41·5 to 62·0)* | 8·0 (4·0 to 12·4)* | 2205 (1075 to 3430) | 3231 (1645 to 4932) | 46·5 (40·2 to 55·0)* | 10·0 (7·0 to 14·1)* | ||
| Chronic kidney disease due to hypertension | 94 (45 to 151) | 134 (61 to 217) | 42·5 (25·6 to 53·4)* | 5·3 (−1·1 to 9·3) | 2315 (1159 to 3656) | 3193 (1634 to 4945) | 37·9 (31·6 to 45·0)* | 8·1 (5·1 to 11·7)* | ||
| Chronic kidney disease due to glomerulonephritis | 36 (15 to 61) | 46 (19 to 78) | 27·4 (11·2 to 42·7)* | 7·0 (−2·9 to 14·7) | 1275 (473 to 2206) | 1583 (612 to 2662) | 24·1 (16·8 to 35·7)* | 10·9 (6·6 to 17·1)* | ||
| Chronic kidney disease due to other causes | 3 (1 to 6) | 5 (1 to 9) | 53·8 (10·0 to 69·1)* | 16·2 (4·2 to 24·5)* | 510 (223 to 850) | 696 (308 to 1140) | 36·3 (31·0 to 43·2)* | 9·7 (6·8 to 13·5)* | ||
| Osteoarthritis | .. | .. | .. | .. | 1648 (949 to 2565) | 2393 (1391 to 3716) | 45·2 (42·1 to 49·6)* | 7·4 (5·4 to 10·4)* | ||
| Low back pain | .. | .. | .. | .. | 2501 (1415 to 4001) | 3299 (1896 to 5222) | 31·9 (29·4 to 35·6)* | 8·6 (6·8 to 11·4)* | ||
| Low bone mineral density: all causes | 283 (261 to 295) | 361 (325 to 381) | 27·7 (22·8 to 32·9)* | 12·6 (8·4 to 17·2)* | 7499 (6494 to 8674) | 8810 (7565 to 10 270) | 17·5 (13·9 to 21·1)* | 7·8 (4·6 to 11·0)* | ||
| Pedestrian road injuries | 44 (41 to 48) | 50 (46 to 56) | 14·4 (6·5 to 21·6)* | 5·5 (2·7 to 8·4)* | 974 (882 to 1071) | 1072 (948 to 1199) | 10·0 (2·2 to 17·2)* | 7·0 (3·7 to 10·7)* | ||
| Cyclist road injuries | 4 (4 to 5) | 5 (4 to 5) | 10·5 (1·0 to 20·0)* | 8·0 (3·9 to 12·4)* | 240 (193 to 298) | 273 (215 to 343) | 13·5 (7·3 to 19·1)* | 10·9 (6·1 to 15·4)* | ||
| Motorcyclist road injuries | 11 (9 to 12) | 14 (12 to 16) | 31·4 (16·4 to 48·5)* | 10·9 (4·3 to 17·5)* | 439 (366 to 517) | 559 (461 to 655) | 27·2 (18·2 to 37·3)* | 11·4 (5·2 to 16·5)* | ||
| Motor vehicle road injuries | 29 (26 to 32) | 33 (29 to 37) | 13·6 (6·1 to 21·7)* | 4·8 (1·5 to 7·5)* | 1029 (882 to 1196) | 1163 (982 to 1357) | 13·0 (7·1 to 18·6)* | 6·4 (3·2 to 9·3)* | ||
| Other road injuries | 1 (1 to 2) | 2 (1 to 2) | 28·3 (12·6 to 47·9)* | 0·6 (−10·6 to 11·8) | 51 (40 to 64) | 70 (54 to 88) | 35·6 (26·3 to 45·0)* | 7·2 (−5·5 to 19·7) | ||
| Other transport injuries | 8 (7 to 10) | 10 (8 to 12) | 19·6 (8·1 to 32·9)* | 4·1 (0·4 to 7·4)* | 219 (192 to 252) | 247 (208 to 306) | 13·0 (2·9 to 25·1)* | 2·4 (−1·6 to 5·9) | ||
| Falls | 170 (151 to 179) | 230 (199 to 245) | 35·3 (29·0 to 42·3)* | 2·3 (−1·2 to 6·1) | 3987 (3362 to 4758) | 4816 (4020 to 5788) | 20·8 (17·2 to 24·7)* | −0·9 (−4·3 to 3·1) | ||
| Other exposure to mechanical forces | 8 (7 to 9) | 10 (7 to 11) | 21·1 (5·5 to 29·8)* | 7·7 (0·0 to 13·4)* | 316 (255 to 390) | 361 (280 to 454) | 14·2 (5·7 to 19·1)* | 4·4 (−0·5 to 8·2) | ||
| Non-venomous animal contact | 1 (1 to 1) | 1 (1 to 1) | 6·4 (−2·5 to 24·9) | 3·7 (−4·8 to 10·7) | 20 (17 to 24) | 20 (17 to 25) | 1·1 (−5·9 to 15·2) | −1·1 (−9·2 to 5·5) | ||
| Assault by other means | 5 (5 to 6) | 6 (5 to 6) | 7·5 (1·4 to 14·1)* | 2·4 (−2·8 to 7·3) | 183 (154 to 215) | 187 (156 to 222) | 2·1 (−2·8 to 7·7) | −1·2 (−6·2 to 3·8) | ||
| Exposure to forces of nature | .. | .. | .. | .. | 40 (24 to 58) | 42 (26 to 62) | 6·3 (−21·5 to 40·4) | 274·6 (178·4 to 423·0)* | ||
| Low glomerular filtration rate: all causes | 1991 (1881 to 2107) | 2426 (2290 to 2559) | 21·9 (19·2 to 24·5)* | 10·7 (8·7 to 12·6)* | 47 131 (44 090 to 50 123) | 54 433 (50 890 to 57 912) | 15·5 (12·7 to 18·2)* | 10·4 (8·0 to 12·9)* | ||
| Ischaemic heart disease | 589 (526 to 656) | 691 (618 to 770) | 17·3 (14·7 to 20·1)* | 0·0 (−1·8 to 2·0) | 9659 (8602 to 10 739) | 10 901 (9711 to 12 188) | 12·9 (10·0 to 15·8)* | 0·7 (−1·1 to 2·7) | ||
| Ischaemic stroke | 230 (197 to 267) | 250 (215 to 288) | 8·6 (5·0 to 12·6)* | 0·4 (−1·9 to 3·0) | 3323 (2845 to 3822) | 3427 (2934 to 3932) | 3·1 (−0·5 to 6·9) | 0·2 (−2·3 to 3·0) | ||
| Haemorrhagic stroke | 228 (192 to 271) | 242 (206 to 282) | 6·1 (1·8 to 11·0)* | 2·5 (−0·3 to 5·8) | 4391 (3699 to 5126) | 4492 (3791 to 5191) | 2·3 (−2·0 to 7·1) | 1·9 (−1·1 to 5·3) | ||
| Peripheral vascular disease | 6 (5 to 7) | 8 (6 to 9) | 36·1 (27·3 to 46·4)* | −0·4 (−3·8 to 3·2) | 131 (96 to 187) | 172 (125 to 244) | 30·6 (26·4 to 35·7)* | 0·2 (−1·7 to 2·4) | ||
| Chronic kidney disease due to diabetes mellitus | 299 (279 to 314) | 418 (389 to 441) | 39·5 (35·4 to 43·5)* | .. | 8713 (7991 to 9466) | 11 258 (10 303 to 12 225) | 29·2 (25·9 to 32·5)* | .. | ||
| Chronic kidney disease due to hypertension | 409 (377 to 428) | 550 (502 to 576) | 34·5 (30·0 to 38·7)* | .. | 10 366 (9401 to 10 985) | 12 737 (11 489 to 13 554) | 22·9 (18·6 to 27·4)* | .. | ||
| Chronic kidney disease due to glomerulonephritis | 206 (185 to 218) | 238 (213 to 256) | 15·6 (10·9 to 20·2)* | .. | 7720 (6930 to 8332) | 8136 (7294 to 8861) | 5·4 (1·3 to 9·3)* | .. | ||
| Chronic kidney disease due to other causes | 24 (20 to 29) | 30 (25 to 35) | 23·9 (17·8 to 30·2)* | .. | 2689 (2209 to 3238) | 3128 (2518 to 3803) | 16·3 (13·1 to 19·2)* | .. | ||
| Gout | .. | .. | .. | .. | 138 (91 to 191) | 181 (120 to 250) | 31·2 (29·3 to 33·1)* | 0·9 (−0·0 to 1·8) | ||
Data in parentheses are 95% uncertainty intervals. DALYs=disability-adjusted life-years. PAF=population attributable fraction.
Statistically significant increase or decrease.
Categories of risk factors—metabolic, environmental or occupational, and behavioural risks—often jointly contribute to disease burden. In 2015, 41·2% (95% UI 39·8–42·8) of global DALYs could be attributed to analysed risk factors, whereas 58·8% (57·2–60·2) of global disease burden could not be explicitly attributed to specific risk factors. In terms of individual risk categories, behavioural risk factors accounted for 30·3% (28·6–32·0) of attributable DALYs in 2015, followed by metabolic (15·5% [14·7–16·3]) and environmental or occupational risk factors (13·0 [11·9–14·0]). Regionally, total risk-attributable burden ranged from 59·0% (57·0–60·9) in southern sub-Saharan Africa to 33·5% (32·1–35·1) in north Africa and the Middle East; furthermore, ten regions had less than 40% of total DALYs attributable to risks being analysed (figure 1).
Figure 1.
Global proportion of all-cause DALYs attributable to behavioural, environmental and occupational, and metabolic risk factors and their overlaps by region for both sexes combined in 2015
Locations are reported in order of total all-cause DALYs population attributable fraction. DALYs=disability-adjusted life-years. ∩=interaction.
Levels and trends in the burden attributable to risk factors
Table 4 reports all-cause deaths and DALYs attributable to all risk factors from 2005 to 2015, including detail on attributable deaths and DALYs by risk-outcome pair (results appendix pp 3–2488 contains results for every geography). Globally, 32·2 million (95% UI 31·5 million to 33·0 million) deaths were attributable to all risk factors in 2015, a 4·9% (3·2–6·7) increase since 2005; however, age-standardised attributable deaths declined from 2005 to 2015 (a 17·9% decrease [16·6–19·2] to 497·5 deaths per 100 000 [485·2–510·0]). By contrast, total DALYs attributable to all risks decreased since 2005 by 5·6% (3·8–7·5) to 1·0 billion DALYs (0·96–1·09 billion) in 2015 and age-standardised DALYs attributable to all risks decreased since 2005 by 20·9% (19·5–22·5) to 14 412·9 DALYs per 100 000 (13 553·0–15 360·1) in 2015. Deaths and burden attributable to environmental and occupational risks significantly fell across measures, with age-standardised deaths falling by 22·5% (20·6–24·4) to 142·6 deaths per 100 000 (130·1–155·6) in 2015 and age-standardised DALYs decreasing by 24·8% (22·1–27·1) to 4500 DALYs per 100 000 (4164·6–4853·9) in 2015.
Progress in environmental risks was mainly driven by sizeable reductions in mortality and disease burden attributable to unsafe water, sanitation, and hygiene, as well as to household air pollution. From 2005 to 2015, global deaths attributable to unsafe water and no handwashing with soap fell by more than 12%, whereas DALYs decreased by more than 20%. More rapid declines than in the above-mentioned risks in attributable deaths (27·5% [95% UI 22·3–32·7]) and burden (31·9% [25·7–37·4]) occurred for unsafe sanitation since 2005, to 807 904·2 deaths (727 439·6–895 462·5) in 2015 and to 46·3 million DALYs (41·1 million to 51·8 million) in 2015. Reductions in attributable mortality and DALYs due to diarrhoeal diseases (associated with unsafe water, sanitation, and hygiene) were particularly prominent. Attributable deaths due to household air pollution decreased by 13·0% (9·3–17·0) to 2·9 million deaths (2·2 million to 3·6 million) in 2015 and disease burden decreased by 20·3% (16·6–24·5) to 85·6 million DALYs (66·7 million to 106·1 million) in 2015; large declines also occurred in age-standardised rates of attributable mortality and DALYs. Occupational risk factors generally accounted for a smaller proportion of global deaths and disease burden than did environmental risk factors; nonetheless, attributable mortality and DALYS due to various occupational risk factors substantially increased from 2005 to 2015.
Behavioural risks can be grouped into four main categories: generally large reductions for risk-attributable mortality and disease burden for risk factors associated with child and maternal malnutrition, mixed results for risk factors pertaining to alcohol and drug use, rising attributable deaths and DALYs due to dietary risk factors, and considerably varied trends for other behavioural risks, which span from sexual abuse and intimate partner violence to low physical activity. Attributable deaths and disease burden due to metabolic risks have increased since 2005, particularly for high fasting plasma glucose, for which all measures of attributable mortality and DALYs increased by more than 15% from 2005 to 2015. These increases in attributable burden from high fasting plasma glucose were led by increased deaths and DALYs from ischaemic heart disease, haemorrhagic stroke, chronic kidney disease, and diabetes. Attributable deaths and DALYs for high BMI also increased substantially, with 645 244 (95% UI 457 647–862 412) more attributable deaths in 2015 than in 2005. Attributable mortality and DALYs due to low glomerular filtration rates also significantly increased from 2005 to 2015, with these increases primarily associated with rises in attributable deaths and burden due to cardiovascular and circulatory diseases and chronic kidney disease.
Global risk patterns by sex
In 2015, the relative ranks and attributable burden due to Level 2 risk factors varied between men and women (figure 2). As the leading risk factor for both sexes, dietary risks accounted for 12·2% (95% UI 10·8–13·6) of total DALYs for men and 9·0% (7·8–10·3%) of total DALYs for women. These risks, which include diet high in sodium and diet low in fruit, contributed most to DALYs associated with three cause groups: cardiovascular and circulatory diseases, cancers, and diabetes and urogenital, blood, and endocrine diseases. In 2015, high systolic blood pressure also ranked among the leading risks for both sexes, contributing to 9·2% (8·3–10·2) of DALYs for men and 7·8% (6·9–8·7) of DALYs for women. Air pollution was the fifth-leading risk for both sexes, largely contributing to DALYs associated with cardiovascular and circulatory diseases, as well as lower respiratory infections, diarrhoeal diseases, and other common infectious diseases. Child and maternal malnutrition, the leading global risk factor in 1990, was the second-leading risk for women and the sixth-leading risk for men in 2015.
Figure 2.
Global DALYs attributable to Level 2 risk factors for (A) men and (B) women in 2015
DALYs=disability-adjusted life-years.
Smoking was the second-leading risk factor for men in 2015, contributing to 9·6% (95% UI 8·5–10·7) of DALYs and a large proportion of male disease burden from cardiovascular and circulatory diseases, cancers, and chronic respiratory conditions. As the fifth-leading risk for men, alcohol and drug use was associated with 6·6% (6·1–7·1) of disease burden in 2015, primarily due to mental and substance use disorders, as well as cirrhosis and other chronic liver diseases; the burden attributable to these risk factors was far less for women (2·0% [1·8–2·2]) than for men. In 2015, high fasting plasma glucose was associated with 6·0% (5·4–6·6) of DALYs for men and 5·6% (5·1–6·2) for women. For women, 3·8% (3·4–4·3) of burden was attributable to unsafe sex, largely from HIV/AIDS and cervical cancer, whereas for men, 2·8% (2·5–3·0) was attributable to unsafe sex.
Changes in leading risk factors in 1990, 2005, and 2015
Rising total attributable DALYs amid declines from 1990 to 2015 for age-standardised DALY rates were evident for various metabolic and behavioural risks, emphasising the need to parse out the effects of demographic and epidemiological factors on global risk profiles (figure 3). In 1990, childhood undernutrition, unsafe water, and high systolic blood pressure were the leading three risk factors for attributable DALYs. Of these risks, only high systolic blood pressure ranked among the leading three risks in 2015. Large reductions in both total attributable DALYs and age-standardised DALY rates from 1990 resulted in childhood undernutrition being ranked as the fifth-leading risk factor in 2015 and unsafe water being ranked as the 14th-leading risk factor.
Figure 3.
Leading 30 Level 3 global risk factors for DALYs for both sexes combined, 1990, 2005, and 2015, with percentage change in number of DALYs, and all-age, and age-standardised rates
Risks are connected by lines between time periods. For the time period of 1990 to 2005 and for 2005 to 2015, three measures of change are shown: percent change in the number of DALYs, percent change in the all-age DALY rate, and percent change in the age-standardised DALY rate. Changes that are statistically significant are shown in bold. DALYs=disability-adjusted life-years.
Environmental risk factors, including household air pollution and unsafe sanitation, decreased in terms of total attributable DALYs, age-standardised DALY rates, and relative ranks from 1990 to 2015. Over the period 1990–2005, attributable total DALYs for occupational risk factors, such as ergonomic factors, rose by more than 20% from 1990 to 2005, although age-standardised rates decreased by 9·5% (95% UI 7·3–11·7) over the same time period. Similar patterns occurred for most behavioural risk factors from 1990 to 2005, with significant increases in total attributable DALYs occurring for many of these risks; at the same time, age-standardised DALY rates significantly fell (eg, smoking, low physical activity, and most dietary risks, including diet high in sodium). Unsafe sex and drug use were exceptions, with each measure of attributable burden significantly increasing since from 1990 to 2005. For unsafe sex and drug use in particular, this rapid rise corresponded with the global HIV/AIDS epidemic. For most risk factors, the time period of 2005–15 resulted in an extension of earlier trends, with continued gains in reductions of attributable DALYs due to various environmental risk factors and more varied patterns for many metabolic and behavioural risks than for environmental risks. Yet, some important changes occurred between 2005 and 2015, including large reductions in attributable total DALYs (29·5% [26·8–32·0]) and age-standardised DALY rates (37·6% [35·2–39·8]) for unsafe sex and in attributable total DALYs (10·5% [2·8–17·8]) and age-standardised DALY rates (23·2% [16·8–29·1]) for intimate partner violence.
Contrasting global changes in risk exposure and attributable burden
A comparison of percentage change in risk exposure from 1990 to 2015 with the level of attributable DALYs in 2015 helps to identify large risks for which a long-term increase in global exposure has occurred (figure 4). Although disease burden attributable to unsafe sanitation, household air pollution, stunting, and underweight caused more than 10 million DALYs in 2015, exposure to these risks decreased for both sexes from 1990 to 2015 by more than 30%. Conversely, two risks caused more than 100 million DALYs and increased by more than 20%: high fasting plasma glucose and high BMI. Other risks with large increases in exposure but which caused less than 10 million DALYs include various occupational exposures, drug use, ambient ozone pollution, second-hand smoke, and diets low in polyunsaturated fatty acids (PUFAs). For a large group of risks at the global scale, exposure increased or decreased by less than 10% from 1990 to 2015. These included many components of diet, high systolic blood pressure, ambient particulate matter pollution, and alcohol use.
Figure 4.
Global attributable DALYs in 2015 for each Level 3 risk factor versus percentage change in SEV from 1990 to 2015 for both sexes combined
Risks with 100 000 DALYs or more are presented. DALYs are represented on a logarithmic scale. We have excluded occupational exposure to benzene, diesel engine exhaust, and occupational exposure to silica, which all had SEV increases of greater than 50%. Ambient PM=ambient particulate matter pollution. Arsenic=occupational exposure to arsenic. Asbestos=occupational exposure to asbestos. Asthmagens=occupational asthmagens. Beryllium=occupational exposure to beryllium. BMD=low bone mineral density. BMI=high body-mass index. Cadmium=occupational exposure to cadmium. Calcium=diet low in calcium. Cholesterol=high total cholesterol. Chromium=occupational exposure to chromium. DALYs=disability-adjusted life-years. Ergonomic=occupational ergonomic factors. Fibre=diet low in fibre. Formaldehyde=occupational exposure to formaldehyde. FPG=high fasting plasma glucose. Fruits=diet low in fruits. GFR=low glomerular filtration rate. Handwashing=no handwashing with soap. Household air=household air pollution. IPV=intimate partner violence. Lead=lead exposure. Milk=diet low in milk. Nickel=occupational exposure to nickel. Noise=occupational noise. Nuts and seeds=diet low in nuts and seeds. Occupational SHS=occupational exposure to second-hand smoke. Omega-3=diet low in seafood omega-3 fatty acids. Ozone=ambient ozone pollution. PAH=occupational exposure to polycyclic aromatic hydrocarbons. Physical activity=low physical activity. PM, gases, and fumes=occupational particulate matter, gases, and fumes. Processed meat=diet high in processed meat. PUFA=diet low in polyunsaturated fatty acids. Radon=residential radon. Red meat=diet high in red meat. Sanitation=unsafe sanitation. SBP=high systolic blood pressure. SEV=summary exposure value. SHS=second-hand smoke. Sodium=diet high in sodium. Sugar-sweetened beverages=diet high in sugar-sweetened beverages. Sulphuric acid=occupational exposure to sulphuric acid. Stunting=childhood stunting. Trans fatty acids=diet high in trans fatty acids. Trichloroethylene=occupational exposure to trichloroethylene. Underweight=childhood underweight. Vegetables=diet low in vegetables. Wasting=childhood wasting. Water=unsafe water. Whole grains=diet low in whole grains.
Decomposition of changes in risk-attributable DALYs to population growth, ageing, risk exposure, and risk-deleted DALY rates
Drivers of global changes in overall DALYs attributable to risk factors varied (figure 5). Across Level 3 risk factors, overall changes in all-cause attributable DALYs ranged from declines exceeding 50% for seven risk factors, including childhood undernutrition, suboptimal breastfeeding, and unsafe sanitation, to increases near to or exceeding 100% (ie, high BMI, occupational carcinogens, and drug use). Of these 46 Level 3 risk factors, attributable all-cause DALYs decreased significantly for ten from 1990 to 2015, whereas 34 increased significantly; two did not significantly change. Population ageing led to increased attributable all-cause DALYs for most risk factors, with a relative contribution that spanned from lower than 10% (for household air pollution from solid fuels and occupational injuries) to greater than 60% (for occupational carcinogens). Population ageing contributed to reductions in all-cause DALYs attributable to eight risk factors, namely environmental risks (eg, a 13·5% [95% UI 6·0–19·9] decrease for no handwashing with soap), those associated with nutritional deficiencies (eg, a 17·6% [12·6–24·0] decline for childhood undernutrition), and behavioural risks (eg, a 22·0% [10·9–31·4] decline for suboptimal breastfeeding). Changes in risk-deleted DALY rates since 1990 were primary drivers of reductions in all-cause, risk-attributable burden, with decreases in underlying DALY rates exceeding 50% for 13 risks by 2015. By contrast, changes in risk exposure varied markedly, contributing to declines in all-cause DALYs for ten risks (eg, 30·0% [29·0–38·0] due to declines in risk exposure for household air pollution and 21·7% [17·5–30·4] due to declines in risk exposure for iron deficiency); at the same time, change attributable to risk exposure increased for 16 risk factors to more than 25%, including high fasting blood glucose (25·1% [19·7–27·9]), ambient ozone pollution (37·5% [31·5–42·7]), occupational carcinogens (40·1% [28·5–50·8]), occupational injuries (41·1% [37·0–48·1]), high BMI (60·0% [54·9–69·2]), and drug use (70·0% [65·5–73·6]).
Figure 5.
Global decomposition of changes in all-cause DALYs attributable to Level 3 risk factors from 1990 to 2015
Risks are reported in order of percentage change in the number of attributable DALYs from 1990 to 2015. We excluded DALYs attributable to unsafe sex because this risk factor is not estimated on the basis of exposure and relative risk. Changes due to population growth, population ageing, risk exposure, and the risk-deleted DALY rate are shown. DALYs=disability-adjusted life-years.
Decreases in underlying cause-specific DALY rates—as opposed to other factors—were generally the main drivers of overarching reductions in cause-specific burden attributable to all risk factors (methods appendix pp 164–65). From 1990 to 2015, 36 causes decreased in terms of associated risk exposure, including a number of communicable causes, nutritional deficiencies, and chronic obstructive pulmonary disease. Notably, risk exposure was the only factor that improved from 1990 to 2015 for a subset of causes, with changes in population growth, ageing, and underlying cause-specific DALY rates all contributing to rising cause-specific disease burden; this finding was most evident for tracheal, bronchial, and lung cancer, as well as for cirrhosis and other chronic liver diseases due to alcohol use.
The risk transition and development
Figure 6 shows the evolution of SEV by region for the ten leading global risk factors in terms of attributable DALYs as SDI changes and also provides the expected SEV level on the basis of SDI alone. Two main trends emerged: increasing and then levelling of SEVs for most metabolic and dietary risks and reductions in SEVs for environmental risks and those associated with childhood undernutrition as SDI approached mid-levels. For metabolic and dietary risks, above an SDI of approximately 0·8, expected levels of risk exposure either moderately dropped or remained fairly constant. An exception was alcohol use, for which SEVs increased with each increment of SDI. By contrast, SEVs for ambient particulate matter pollution did not substantially decline until above an SDI of 0·60, and the pace of SEV reductions for household air pollution accelerated above an SDI of about 0·40. These patterns reflect the complex shifts in risk exposure that accompany changes in development, which are further emphasised by regional SEV trends by risk factor.
Figure 6.
Coevolution of SEV and SDI for the top ten global risks in terms of attributable disability-adjusted life-years in 2015
Coloured points show SEVs for Global Burden of Disease regions. Each point represents 1 year in 5 year intervals from 1990 to 2015. The solid black line represents the expected SEV on the basis of SDI alone. SDI=Socio-demographic Index. SEV=summary exposure values.
Two risk factors related to nutrition or diet—childhood wasting and diet high in sodium—reflected the nuances of changing risk exposure and levels of development. Particularly among regions with an SDI below 0·8, SEVs for childhood wasting decreased over time and with increasing SDI; nonetheless, a subset of regions, including south Asia and western sub-Saharan Africa, had consistently higher than expected SEVs for childhood wasting on the basis of SDI. For diet high in sodium, most regions saw minimal changes in exposure over time, even amid increases in SDI. In east Asia, SEVs for diet high in sodium were consistently above expected levels of exposure given SDI, whereas the opposite trend was found for Oceania and central Latin America. Across the development spectrum—including high-income Asia Pacific, southeast Asia, and eastern sub-Saharan Africa—exposure for diet high in sodium was at least moderately higher than expected on the basis of the SDI for a given region. Heterogeneous risk patterns occurred for two leading environmental risks—household air pollution and ambient particulate matter pollution—particularly in terms of the relationship between SEVs and increasing SDI. For smoking and alcohol use, strikingly different trends for SEV and SDI occurred. Although nearly every region recorded declines in SEVs for smoking, the rate at which these reductions took place alongside changes in SDI varied.
Regional and national risk profiles
Leading risk factors for early death and disability, as measured by attributable DALYs, varied by region, level of SDI, and sex in 2015 (figure 7). In high-income North America and the UK, smoking was the leading risk for attributable DALYs among both men and women, but for most of western Europe, smoking was the leading risk factor only for men, whereas high systolic blood pressure was the leading risk factor for women. A similar pattern emerged in east and southeast Asia, with smoking ranked as the leading risk factors for men in China, Thailand, Vietnam, and the Philippines, whereas metabolic risk factors—namely high systolic blood pressure—was the leading risk factor for attributable DALYs for women in these countries. Childhood undernutrition ranked as the leading risk factor for early death and disability for both sexes throughout western and central sub-Saharan Africa, as well as in a few countries outside of sub-Saharan Africa (eg, Laos and Tajikistan).
Figure 7.
Leading ten Level 3 risk factors in terms of disability-adjusted life-years for both sexes combined in 2015, by location
The 15 leading risk factors are coloured. Bone mineral density=low bone mineral density. Handwashing=no handwashing with soap. Int partner violence=intimate partner violence. Nuts and seeds=diet low in nuts and seeds. Occ=occupational. Particulate matter=ambient particulate matter pollution. Physical activity=low physical activity. Processed meat=diet high in processed meat. SDI=Socio-demographic Index. Subopt=suboptimal. Sweetened beverages=diet high in sugar-sweetened beverages. Vegetables=diet low in vegetables.
In terms of the leading ten risk factors for both sexes, regional and country risk profiles showed both distinct patterns and heterogeneity. High systolic blood pressure was the leading risk for DALYs for 13 high-income countries and territories in 2015, high fasting plasma glucose was the leading risk for three, and smoking was the leading risk for 21. For a subset of geographies, including the USA, Canada, Australia, and the UK, drug use was a major risk for early death and disability in 2015. In 2015, high systolic blood pressure, high BMI, and high fasting plasma glucose were the leading risk factors for almost all geographies in Latin America and the Caribbean; Haiti was the primary exception, with unsafe sex as its leading risk for attributable DALYs in 2015. Across southeast Asia, east Asia, and Oceania, high systolic blood pressure was the leading risk factor for disease burden in nine countries and territories, ranging from China to Vanuatu. High BMI was the leading risk for DALYs in nine geographies, and high fasting plasma glucose ranked as the leading risk factor for three geographies, including Taiwan.
High systolic blood pressure was among the leading two risk factors for all geographies in south Asia and, except for Pakistan and Bhutan, household air pollution remained among the leading four risk factors for attributable DALYs across geographies in this region. Ambient particulate matter pollution ranked as the third-leading risk factor in India and Nepal, whereas smoking was the second-leading risk factor for attributable burden in Bangladesh. In central Europe, eastern Europe, and central Asia, 28 of 29 countries had high systolic blood pressure as their leading risk factor for attributable DALYs in 2015; Tajikistan, where childhood undernutrition was the leading risk factor, was the only exception. Across central Europe, smoking was the second-leading risk factor for early death and disability, whereas alcohol use was among the leading four risk factors for attributable DALYs in geographies including Belarus, Moldova, and Russia.
Throughout north Africa and the Middle East, except for Tunisia, high systolic blood pressure was among the three leading risk factors for disease burden in 2015, with nine geographies, including Egypt and Iran, recording this risk as the leading driver of early death and disability in that year. High BMI accounted for the highest attributable DALYs in eight countries, including Jordan and Saudi Arabia, and was also among the leading six risks for all countries in the region. For Afghanistan and Sudan, childhood undernutrition was the leading risk for DALYs in 2015, whereas it was the second-leading risk for DALYs in Yemen and the eighth-leading risk in Egypt. Unlike most of sub-Saharan Africa, several metabolic risks also emerged as leading drivers of attributable DALYs in southern sub-Saharan Africa by 2015; high BMI ranked as the second-leading risk factor in South Africa, and high systolic blood pressure was among the leading three risk factors for attributable DALYs in Botswana. In central sub-Saharan Africa, childhood undernutrition and unsafe sex were ranked first and second for attributable disease burden in all geographies except for Gabon. High systolic blood pressure ranked among the leading risk factors for attributable DALYs in most geographies in the region (eg, second in Gabon and third in the Congo).
Discussion
Overview
Drawing from 25 500 data sources, we estimated exposure to 79 metabolic, environmental and occupational, and behavioural risk factors or clusters of risks from 1990 to 2015 in 195 countries and territories and attributed deaths and overall disease burden to these risks. In 2015, all risks combined contributed to 57·8% (95% UI 56·6–58·8) of deaths and 41·2% (39·8–42·8) of DALYs worldwide. Since 1990, global risk exposure for both sexes combined increased significantly for 27 risks, did not significantly change for seven risks, and declined significantly for 27 risks. At the same time, that risk exposure increased for various leading risks, particularly metabolic risk factors associated with NCDs, and age-standardised risk-attributable deaths and DALYs declined for most risks. Globally, pronounced reductions in risk-deleted or underlying cause-specific DALY rates offset minimal changes in, or increased, risk exposure. These gains in risk-deleted DALY rates might not be large enough in the future to compensate for rising levels of risk exposure, such as high BMI or high fasting plasma glucose.
Rethinking the risk transition
Societal processes of urbanisation, the so-called westernisation of diets and lifestyles, and changes in employment activities, have all been viewed as primary drivers of changes in human health.21, 22, 23, 24 Such shifts have been thought to lead to deteriorating diets, rising obesity, decreased physical activity, and, ultimately, to worsening levels of metabolic risks, with associated higher rates of cardiovascular diseases and cancers.25, 26 Results from the this study point to an ongoing risk transition, but with a trajectory complex and nuanced. The relationship between SEVs for most risks and SDI identified that poor water, poor sanitation, household air pollution, and micronutrient deficiencies and undernutrition decline steadily as countries develop. By contrast, some risks become worse as development proceeds, at least up to levels of SDI of about 0·8; these risks include low physical activity, high BMI, high total cholesterol, low PUFAs, partial breastfeeding, alcohol use, diet high in red meat, smoking, and diet high in sugar-sweetened beverages. Some risks that appear to worsen through early phases of development improved at the highest levels of SDI, such as smoking. As improvements in SDI continue and behavioural risks grow in dominance, an understanding of how to change behaviours effectively at both the individual level and for populations becomes increasingly relevant. Many other components of diet, occupational exposures, and some environmental risks do not show a marked relationship with development.
The effects of the risk transition, at least globally, are often mitigated by trends in risk-deleted death or DALY rates. In this study, we identify likely candidates for specific drivers of improvements. Unmeasured risk factors could be driving these trends. Unlike cardiovascular diseases and some neoplasms, for other causes such as mental disorders or neurological disorders, the set of risks included in this study account for comparatively little of the observed burden; these causes make up an increasing share of the burden for geographies at high SDI. To date, we have not identified risk factors that meet our criteria of convincing or probable evidence, suggesting that research into unquantified risks is needed. In accompanying GBD 2015 analyses,27, 28, 29 we documented widespread improvements in overall development as measured by SDI. Gains in SDI are likely to operate through many pathways, including improved access to health care, public health programmes, and social and welfare policy. Advances in treatment are well documented for various causes, including HIV/AIDS,30, 31, 32 ischaemic heart disease,33, 34, 35, 36, 37 and various cancers,38, 39, 40 including breast,41, 42, 43 testicular,44 and Hodgkin's,45 yet for other causes, such as oesophageal cancer and interpersonal violence, the policies, programmes, and interventions responsible for declining risk-deleted death and DALY rates are less clear than for the aforementioned causes. Improvement of understanding of the risk-deleted rates in cause-specific mortality and disease burden will strengthen the evidence base for intervention effectiveness, the role of medical care access in addressing disease burden, and the importance of other social and welfare policies.
A global risk typology
We used our decomposition of drivers of attributable burden to identify four distinct groups of risks at the global level. First, for ten risks, attributable burden is declining, as is the exposure to the risk factor. This set of risks is dominated by the environmental risks, which are particularly common at low levels of SDI, and consist of vitamin A deficiency, undernutrition, zinc deficiency, suboptimal breastfeeding, poor sanitation, no handwashing, poor water, second-hand smoke, household air pollution, and occupational asthmagens. For these risks as a group, not only has exposure been declining, but risk-deleted DALY rates also declined, such as for diarrhoeal diseases. Furthermore, global shifts in population age structure contributed to decreases in both cause-specific and attributable burdens for risks that predominantly affect children. A second group of risks was characterised by declines in exposure exceeding 10% from 1990 to 2015, but increasing attributable burden, due in most cases to large increases driven by population growth and ageing. This group includes smoking, high systolic blood pressure, occupational ergonomic factors, childhood sexual abuse, and iron deficiency; for iron deficiency, the increase in attributable burden was quite small over the period 1990–2015. For a third group, attributable burden is increasing, and trends in exposure account for a less than 10% increase or decrease in attributable burden. This larger group of risks than the first two groups includes all components of diet except for low PUFA intake and diet high in sugar-sweetened beverages, some occupational exposures, residential radon, low glomerular filtration rate, alcohol use, high total cholesterol, intimate partner violence, lead exposure, low bone mineral density, and low physical activity. For these risks, attributable burden is increasing because of population growth and ageing. The degree of increase is driven by the extent to which declines in risk-deleted DALY rates compensate for the increases due to population growth and ageing. The final category is the risks that are perhaps the most concerning: those with increasing attributable burden and exposure contributing to an increase of at least 10% since 1990. This list includes occupational injuries, ambient ozone pollution, occupational carcinogens, diet low in PUFAs, diet high in sugar-sweetened beverages, drug use, high fasting plasma glucose, and high BMI. For these risks, declines in underlying rates were probably responsible for prevention of additional increases in attributable burden. Any risk for which attributable deaths and DALYs are increasing is a threat to both health systems and societies, but the risks that fall within the fourth group—risk factors with rising exposure and associated health loss—require immediate attention from policy makers and other stakeholders.
Unsafe water, sanitation, and handwashing
The conventional approach to assessment of the contribution of unsafe water to health is to assess access to improved water sources as defined in the Millennium Development Goals.46, 47 WHO estimated that, in 2015, 91% of populations living in low-income and middle-income countries had access to improved water and 68% had access to improved sanitation since 1990.48, 49 Implicit in the focus on improved is the idea that the most important reductions in diarrhoea come from movement from an unimproved to an improved source of water or sanitation. However, findings from meta-analyses of intervention studies and retrospective cohorts show a wide variation of relative risks of diarrhoea within the category of improved water and improved sanitation. We found that the SEV for poor water was only 56·0% (95% UI 50·4–62·1) for men and 55·7% (50·2–61·8) for women in 2015, a small improvement of just 9·4% (5·3–13·0) since 1990. By contrast, for unsafe sanitation, the SEV decreased substantially, from 55·0% (53·8–56·5) in 1990 for men and 54·2% (52·8–55·7) for women to 33·7% (32·2–35·1) for both men and women in 2015. Our assessment of SEV for water showed that a substantial agenda is still needed across the world to achieve the overall goal of safe water and sanitation. The sixth Sustainable Development Goal includes targets for achievement of both universal and equitable access to safe drinking water and adequate and equitable sanitation for all by 2030.50, 51 Given SEVs in many of these areas of the world, a large gap remains between current levels of safe water and sanitation and universal access. Moreover, our analyses show that progress in provision of safe water lags behind that of safe sanitation. This shift in focus to the lowest risk categories raises the bar considerably for what is needed for investment to reduce the risk of diarrhoea in all regions of the world.
Tobacco
The SEV for smoking has decreased in many countries as well as globally. Global tobacco-attributable deaths and DALYs, however, have continued to rise because of increases in population numbers and ageing, which overwhelm declines in both exposure and risk-deleted rates of related disease burden. Given a known highly effective set of intervention strategies to reduce tobacco consumption,52, 53, 54, 55, 56, 57, 58 the challenge for tobacco is one of political priority for tobacco control. Despite the important developments of the Framework Convention on Tobacco Control, in many countries, progress has been slow or consumption has even increased. Continued close monitoring of tobacco consumption and the deaths and DALYs attributable to tobacco remains an essential aid to promotion of policies to reduce tobacco consumption.
In GBD 2015, for long-term effects of smoking on lung cancer and chronic obstructive pulmonary disease, we used the Peto-Lopez method,59 which estimates the lifetime cumulative effect of cigarette smoking using a transformation of the observed lung cancer death rate. Although this method provides robust estimates of the burden of cancers related to tobacco, it is not fully consistent with the GBD approach of estimation of exposure independently of the outcomes affected by exposure. With a growing body of evidence for the association between smoking and other cancers and a good estimate of distribution of smoking, direct estimation of attributable burden is possible. Modelling of the direct relationship between smoking exposure in the past and present to cancers will also allow for exploration of counterfactual scenarios and other forms of CRA, such as estimation of avoidable burden. The set of outcomes that have been related to tobacco in pooled cohort studies60 includes many outcomes not quantified in this study, such as road traffic accidents, renal failure, and infectious diseases; careful assessment of which of these new outcomes meet the criteria of convincing or probable evidence is needed. Quantification of the full effects of tobacco will also require inclusion in future GBD studies of smokeless tobacco consumption. Regardless of the estimation method used or the scope of outcomes evaluated, tobacco remains a major global risk factor, despite more than 50 years of antitobacco efforts.
Dietary assessment
Many aspects of dietary assessment remain controversial. Evidence for the effect of diet on NCDs mostly comes from prospective cohort studies using food frequency questionnaires (FFQs) with 1 year recall to establish diet at baseline. Findings from 24 h recalls or multiple-day diary records show a poor correlation with annual FFQs.61, 62 Proponents of FFQs argue that the rank order of levels of intake across individuals in the annual FFQ is robust.62 Some authors have argued that measurement error for each diet component in the statistical analysis of the cohort data will tend to bias the findings towards the null and thus underestimate the effects of a diet component.63 However, the direction of bias in settings with measurement error in multiple independent variables is unknown in the presence of correlation between different variables.64, 65 At the population level, single 24 h recall has been used in many nutrition surveys. 24 h recall probably underestimates, as shown in doubly labelled water66 and urinary sodium studies.67
Correlation between diet components is a crucial aspect of diet. Intake of beneficial dietary factors are generally, but not always, positively correlated with each other and inversely correlated with harmful dietary factors. This correlation could overestimate the relative risk of each dietary factor in cohorts as well as the total effect of dietary risks at the population level. Use of dietary pattern as the main exposure could potentially address this problem; however, several challenges exist in adoption of this approach for GBD. Concerns remain about the magnitude of the effect size of individual dietary risk factors on chronic diseases. Although many prospective cohorts have collected dietary data,68 published meta-analyses for most diet-disease pairs have included reports from only a fraction of these cohorts, indicating the potential for publication bias. Furthermore, most cohorts assessing the effect of diet on disease endpoints have adjusted for total energy intake in their statistical models. This practice emerged to address measurement error in dietary assessment tools and remove the effect of energy as a potential confounder. The adjustment for total energy intake means that diet components are defined as risks in terms of the share of diet and not as absolute levels of exposure. Because diet shares are analysed, increases in any component imply reductions in some other component, leading to the notion of replacement. Diet components are often analysed as pairs in which one component replaces another, further complicating analysis of cohort data. Given that many cohorts do not include the same dietary components in their analyses, the relative risks of dietary factors across cohorts might not be strictly comparable. This issue has been one of the main reasons for inconsistent findings in dietary meta-analyses.69, 70 Future work to encourage more pooled analyses than at present of diet components for all the major cohorts would be beneficial; release of more data than available from the present major cohorts would stimulate various alternative analyses of diet, which would help strengthen the evidence for diet and attributable burden.
Sodium intake
Age-standardised DALYs attributable to diets high in sodium and exposure (as measured by SEV) for diets high in sodium increased slightly at the global level (7·2% [95% UI 0·7–19·0] for men and 4·0% [–0·3 to 12·1] for women) from 1990 to 2015. Reduction in sodium intake at the population level is one of WHO's nine global targets for NCDs.71 Many countries (eg, the UK, Finland, Japan, and Brazil) have already implemented or are considering implementing (eg, the USA) policies to reduce sodium intake.71, 72, 73, 74, 75 Reports from countries with high levels of sodium intake (eg, Japan) that have successfully implemented sodium reduction policies have argued for the beneficial effects of a lowering of sodium intake in these populations.76 Although multiple lines of epidemiological evidence support the harmful effects of very high levels of sodium intake, no scientific consensus has been reached on the optimal level of sodium intake. In GBD 2013, on the basis of findings of the Prospective Urban Rural Epidemiology (PURE) collaboration on sodium and cardiovascular mortality13, 77 and to incorporate the absence of scientific consensus on the optimal intake of sodium, we expanded the uncertainty for the TMREL for sodium to 1–5 g per day.78, 79, 80 PURE collaborators subsequently published a further analysis,13 which raised the possibility that, for those without hypertension, an inverse relationship might exist between sodium intake, all-cause mortality, and cardiovascular events. These findings challenge longstanding beliefs in the public health community with regard to the importance of modulation of sodium intake at the population level. Current policy is grounded in the evidence that links sodium intake and systolic blood pressure, which shows increases in systolic blood pressure with increases in sodium above 1 g per day.81, 82 However, we have identified no prospective cohort studies that directly link sodium to disease endpoints that support reductions in the risk of outcomes at levels of intake below 3 g per day. Proponents of a low TMREL for sodium have argued that the cohort studies that generally show rising mortality at levels below 3–5 g per day might have the issue of reverse causation because ill individuals reduce sodium consumption.83, 84 Given this continued debate, we chose not to change the uncertainty range of the TMREL from the current 1–5 g per day. If the findings from PURE and the pooled analysis are correct, an increased risk might exist for individuals without hypertension who consume less than 5 g per day. We have not included this potential increased risk in our quantification of uncertainty. Many studies have been completed or are underway examining the effects of sodium reduction in population groups or whole communities on systolic blood pressure, but none to date have been done that report the effects of sodium reduction on disease endpoints. Such studies, when and if they are done, could contribute to a resolution of outstanding questions about the TMREL for sodium. Regardless of the debate on the TMREL, we found that sodium accounted for at least 2·0% of global DALYs in 2015. The risk profile of increasing attributable numbers of DALYs, and no global progress in a reduction of exposure to diets high in sodium, places this risk among those of great concern for the management of health systems.
Diet and policies
Much of the diet policy debate has focused on the importance of reductions of sodium, sugar, and fat.85, 86 Our assessment of the burden from diseases attributable to 14 dietary factors showed that, at the global scale, six factors each accounted for more than 1% of global DALYs, in order of importance: diets high in sodium, low in vegetables, low in fruit, low in whole grains, low in nuts and seeds, and low in seafood omega-3. Our findings suggest that, in addition to a policy focus on sodium, sugar, and fat, many other important components of diet should be minimised and promoted through education, subsidies, and other evidence-based programmes.87 If our findings are correct, a policy focus on the sugar and fat components of diets might have a comparatively smaller effect than that of promotion of increased uptake of vegetables, fruit, whole grains, nuts and seeds, and seafood omega-3. The disconnect between the diet policy debate and the evidence of which diet factors are most important globally can also be seen for red meat, where the harm of increased diabetes and colorectal cancer is smaller than that for all of the other 13 diet components considered under the GBD framework. Consideration of diet policy is made more complicated when cost-effectiveness, political feasibility, intensity of implementation, reactions of various stakeholders (eg, consumers and the food industry), and environmental effects, including climate change, are factored into national diet policy discussions. For example, promotion of some components of a healthy diet (eg, milk and dairy products) might have deleterious effects on environmental sustainability. These dimensions of diet policy should be added to the debates on how to transform national diets to be lower risk than at present.
Cholesterol
On the basis of findings from studies12 that showed the benefits from the reduction of LDL and total cholesterol to very low values, for GBD 2015, we revised the TMREL for total cholesterol downwards from 3·80–4·00 mmol/L to 2·78–3·38 mmol/L. This revision increased our estimate of the burden of total cholesterol for the year 2010 from 2·7 million (95% UI 1·9 million to 3·8 million) deaths in GBD 2013 to 4·0 million (3·1 million to 5·1 million) deaths in GBD 2015 and shifted our placement of cholesterol among leading risks from tenth (GBD 2013 ranking for the year 2010) to fourth (GBD 2015 ranking for the year 2010). Effective intervention options to influence population total cholesterol are available, including efforts to increase physical activity and diet and pharmacological interventions. Although consumption of dietary cholesterol is not linked to serum cholesterol,88 dietary interventions, such as increased consumption of fruits, vegetables, and fibre, and increased physical activity can influence LDL and total cholesterol89 and should be encouraged.90, 91 Statins are highly effective, with few side-effects, justifying their use in many individuals, either alone or in combination with other medicines. In general, given the existence of proven and effective intervention strategies, the increase in the importance of cholesterol highlights a major opportunity for intervention.
Systolic blood pressure
In this assessment, as in GBD 2013, we found that the most important Level 3 risk factor globally is elevated systolic blood pressure. The TMREL for this estimation, a systolic blood pressure of between 110 mm Hg and 115 mm Hg, is based on evidence from the pooling of prospective cohort studies that showed that individuals with a baseline blood pressure at this level have the lowest risk of future cardiovascular death.92, 93 In addition to this observational evidence, two randomised clinical trials of blood pressure lowering have added substantially to the evidence in this area. Findings from the SPRINT trial10 showed that adults in the USA with elevated vascular risk and pre-existing hypertension (mean systolic blood pressure at baseline 139·7 mm Hg and on a mean of 1·8 medications) benefited from antihypertensive therapy that targeted a systolic blood pressure of 120 mm Hg. Findings from the HOPE-3 trial,77 a multinational study, showed that older adults (aged ≥55 years) with elevated vascular risk but without susbtantially elevated systolic blood pressure (mean systolic blood pressure at baseline 138·2 mm Hg) did not have any benefit when they received hydrochlorothiazide 12·5 mg plus candesartan 16 mg daily. However, neither study directly addresses selection of the GBD TMREL of 110–115 mm Hg since observational studies necessarily reflect the benefits accrued through maintenance of a healthy blood pressure throughout life rather than through use of blood pressure-lowering medications. The GBD estimate necessarily represents the effect of primary prevention and lifestyle modification, as well as the possibility of pharmacotherapy for achievement of the TMREL. The large potential gain in global health that we estimate if an optimal blood pressure was to be achieved suggests that further studies of blood pressure in people younger than 60 years of age remains an important area for investigation. A wide array of clinical and population strategies are available to reduce systolic blood pressure, including lowering population salt intake, increasing physical activity, reducing or slowing the rise of high BMI, and providing access to effective antihypertensives, which merit considerable attention in many countries.
Alcohol use
We report that the global SEV for alcohol decreased by 1·1% (95% UI −6·0 to 2·3) for men and 13·1% (−16·1 to −10·7) for women. Of note, however, because of the geographical distributions of alcohol consumption and background disease rates, alcohol consumption contributed to an increase in alcohol attributable DALYs over the same period. Assessment of the burden attributable to alcohol is complicated by potentially elevated risks in former drinkers compared with abstainers, potential protective effects of mild-to-moderate use of alcohol, and use of a TMREL of zero consumption for this study. Findings from meta-analyses have shown considerably elevated relative risks in former drinkers, equivalent to 30 g of pure alcohol per day or more for some outcomes,94, 95 although this finding could occur as a result of confounding by misclassification of former drinkers as lifetime abstainers.96, 97, 98, 99 Future GBD studies should carefully re-evaluate whether or not the excess risk in former drinkers is overestimated. If the relative risks for former drinkers have been overestimated, this overestimation will also affect our assessment of the alcohol SEV and the global trend in the SEV. The protective effect of mild-to-moderate alcohol use reported for ischaemic heart disease, diabetes in women, and reduced all-cause mortality is controversial;100, 101, 102, 103, 104, 105 some authors argue that this consistent finding is due to confounding.106, 107 However, investigators of studies108 of all-cause mortality with certain types of quality exclusions find no overall mortality benefit of mild-to-moderate use. Various mendelian randomisation studies have contradicted previously claimed benefits of moderate alcohol consumption for several outcomes.109, 110, 111 Marked differences in male and female patterns of relative risk, such as for diabetes,104, 105 raise many questions about the biological pathways through which these effects might act. Finally, our alcohol analysis uses a TMREL of zero consumption; use of a higher TMREL than zero for alcohol use would increase our estimate of the global burden attributed to alcohol. Given the large burden of alcohol and the availability of effective options to reduce consumption at the population level, such as increased alcohol taxes, controls on outlet location and density, establishment or maintenance of limits on days or hours of sale, and screening and advice from health-care givers,112, 113, 114, 115 narrowing of the uncertainty in the alcohol assessment is important.
High BMI and fasting plasma glucose
Among the top five Level 3 risk factors, DALYs attributable to high BMI increased the most from 1990 to 2015 while SEV also increased. High BMI is mediated through increases in systolic blood pressure, cholesterol, and fasting plasma glucose (methods appendix pp 28–35). Our decomposition analysis suggests that the increase in risk-attributable burden due to high BMI is considerably smaller than it could have been if underlying rates, particularly for cardiovascular diseases, had not declined as much as they did over the past decade. The decline in the underlying rates is likely due to expanded access to preventive treatment and increased quality of care.116, 117, 118, 119, 120 If obesity continues to increase in the future, the consequences for health trends might be greater if the trend in underlying rates attenuates than if it continues to decrease. Although closely linked, we also estimate that the rate of increase in high fasting plasma glucose is slightly higher than that for obesity. The combined effect of rising obesity and rising fasting plasma glucose has consequences for various health outcomes and health-care delivery costs. For obesity, various policy options have been proposed,121, 122, 123 but few, if any, strategies have been proven to work at the population level. Analysis of obesity options needs to be closely linked to consideration of diet and physical activity. Although for most diet components we have reported on the effect of diet composition on health outcomes, a strong argument exists to explore the relationship of specific diet components with overall BMI.
Methods strengths and challenges: uncertainty in causality
To move the GBD and CRA fields forward, we have reported, for the first time, details of the evidence that is available to support the causal relationship of each risk-outcome pair. The strength of the evidence of causality varies widely across risk factors. For the risk-outcome pairs where evidence from randomised controlled trials or high-quality prospective observational studies was not available, we considered the possibility of using other types of evidence, including mendelian randomisation, to establish causality.124 Although we have not used this approach in GBD 2015, this body of evidence seems to provide useful information that deserves a more detailed evaluation in future iterations of GBD than in this study. Likewise, the appropriate use of case-control data to support causality needs to be more clearly defined than in this study.
Being explicit about the supporting evidence also shows that some risks have a similar body of evidence supporting them, even though, in some debates, the strength of evidence is thought to be very different. For this study, we focused on evidence mainly from prospective studies of exposure and disease endpoints. In select cases, we had to use prospective studies of intermediate outcomes, including trials of the effect of sodium on systolic blood pressure, prospective cohort studies of the effect of lead on systolic blood pressure, and trials and cohort studies of sugar-sweetened beverages' effect on BMI.125, 126, 127, 128 We did not include the strength of evidence uncertainty in our estimation of attributable burden, which requires more consensus than we had available on how different types of evidence can be combined to support a causal connection.
Integrated exposure response curve for particulates less than 2·5 μg
In this study, as for GBD 2013, we have estimated the relative risk of exposure to particulate matter with an aerodynamic diameter smaller than 2·5 μm (PM2·5) over a broad range of daily doses by integrating relative risks from diverse sources of PM2·5, consisting of ambient air pollution, household air pollution, second-hand smoke, and tobacco smoking, using a single integrated exposure response (IER) curve.129, 130 The premise behind this approach is that PM2·5 daily dose is a common indicator of risk from diverse sources of particulate pollution. Although assessments support an assumption of the equitoxicity of particulate matter mass from different sources for the purposes of burden estimation,131, 132 this issue remains an area of active research. We expect that the IER will continue to evolve in response to the latest evidence in the field of air pollution dose response; in keeping with the iterative nature of the GBD estimates, inclusion of additional cohort studies at lower levels of exposure to PM2·5 than those previously identified and included led to a revision of the TMREL distribution that is less than half of the level used in GBD 2013. Inclusion of new high-quality studies and the non-linear nature of the IER curve have increased our estimate of global burden. Methodological improvements to the curve-fitting algorithm that better capture the heterogeneity of component studies than do those in GBD 2013 produce UIs that are considerably wider than are those estimated in GBD 2013.
Future directions for GBD CRA
To date, attributable burden has been the primary metric that was methodologically and computationally feasible for GBD risk assessments. As burden forecasts become routinely available, quantification of avoidable burden within the GBD analytic framework will become more tractable than at present. Development of avoidable burden estimates will require resolution of various important issues, such as the degree of reversibility for some risks and the type of counterfactual distribution most relevant to avoidable burden calculation. Arguably, feasible or cost-effective counterfactual distributions of exposure might be more relevant than is minimum risk.
In the next iterations of the GBD CRA, we plan to incorporate new risks into two areas: distal socioeconomic factors, such as educational attainment, and the absence of effective health interventions, such as vaccination or seat belts. We will assess the evidence supporting new risk factors for inclusion and expand the scope of the analysis on the basis of both the evidence for causality and the availability of evidence for estimation of exposure levels. For behavioural, environmental and occupational, and metabolic risks, other candidate risks have been proposed for inclusion in GBD, including climate change, smokeless tobacco, added sugar, and access to health care. For existing risks, we will also carefully assess inclusion of new risk-outcome pairs. Continued close examination of evidence supporting causality might lead to modifications of the criteria for inclusion. For many distal factors, such as educational attainment, highly consistent evidence exists from prospective cohorts for all-cause mortality, but the relationships for cause-specific mortality might vary by context; for example, where access to treatment might modulate the effects of education on an outcome. For GBD 2015, we have made progress clarifying the evidence base for each risk-outcome pair. This type of in-depth examination will, we hope, lead to a simpler and more transparent approach than has been used before to define which risk-outcome pairs at any level of the causal web should be considered convincing or probable.
Limitations
Since estimation of the attributable burden of disease includes estimates of deaths, YLLs, YLDs, or DALYs, the limitations described elsewhere for those also apply to this analysis.133, 134 We have developed our modelling strategies to quantify uncertainty given the available data. New data—particularly from countries where we currently lack data—might reveal levels of exposure that are outside the UIs that we have estimated. We assume that the joint effect for risk factors where we do not correct for mediation can be estimated with the multiplicative risk model. Although plausible, this model might not accurately capture how all risks interact.135 Analyses of the National Health and Nutrition Examination Survey III cohort suggest submultiplicative effects for some risks.136 A shift from a multiplicative model to a submultiplicative model has profound implications for all aspects of risk factor epidemiology, beginning at the estimation of relative risks and extending to use of relative risks as a generalisable construct.
As a consequence of the absence of sufficient studies across all risk-outcome pairs, we did not systematically correct relative risks for publication bias. We did not correct relative risks for non-masking in studies; however, not all risks can be studied in a masked fashion (eg, tobacco smoking). Comparability would be compromised if we corrected some risks but not others. We generally assumed that relative risks were uniform across countries for a given age-sex group.137, 138 Differences in relative risks with geography might exist, as has been found for the BMI relative risk curve and TMREL, but with the exception of breast cancer, we find that insufficient evidence exists to date to identify statistically significant differences.
Development of robust models to estimate variation in SD is more difficult than for estimations of the mean. Because measurement error is necessarily included in SD from studies, they are an overestimate of the true SD. We did not correct SD for measurement error, with the exception of correction of observed systolic blood pressure to usual blood pressure. Measurement error also affects estimation of relative risks through regression dilution bias—the attenuation of the association between the level of risk and the incidence of disease outcomes. Because of the absence of detailed data for key cohorts, we have not corrected cholesterol or fasting plasma glucose relative risks for regression dilution bias. Our approach of estimation of the maximum relative risk on the basis of the reported cohorts and trials might underestimate burden if risk continues to rise at the highest levels of exposure beyond those reported. Although a log-linear function for relative risks and levels of exposure is adequate for the observed range of exposure, available data on the most extreme values are few. Given that a very small fraction of the population in any country is in these extreme exposure levels, the potential bias in our estimates is minimal. Additionally, estimation of burden for risks divided into polytomous risks might underestimate their burden compared with estimation of burden with a continuous risk variable.
Although use of a log-normal distribution is the best of the parametric distributions that we have assessed for fasting plasma glucose, important deviations from the log-normal exist in survey data such as from the National Health and Nutrition Examination Survey. We have explored different mixtures of distributions, including two log-normal or a normal and log-normal, some of which provided better overall fit than the one that we used. However, we have so far not been able to solve the optimisation problem of estimation of two distributions given only a mean and SD reported from particular studies.
We did not use the relative risk and exposure PAF calculation for unsafe sex, HIV risk from injecting drug use, and occupational injuries; we used direct evidence of the attributable fraction. Comparability of the results derived from these direct or categorical approaches to the risks estimated with the relative risk and exposure model is not certain.
Too few studies exist to allow estimation of the contribution of household air pollution to ambient air pollution or vice versa.139 As a consequence, we might have underestimated the burden of household air pollution as a single risk factor; we might also have overestimated the burden of air pollution combined. Furthermore, our analysis of ambient air pollution has focused on PM2·5; other pollutants, including larger particulates than PM2·5 and nitrogen dioxide, might also be important to quantify. For cholesterol, we established our estimates of burden using total cholesterol; however, increasing evidence supporting the effects of LDL cholesterol—and improvements in data availability for serum LDL in different populations—suggest future estimations of risk from high cholesterol should use LDL cholesterol as the unit of estimation.
Proxies for exposure to some risk factors are coarse, which is particularly the case for zinc deficiency, for which we estimated the balance between theoretical intake and physiological requirements from Food and Agriculture Organization food balance sheets for absorbable zinc. Although zinc deficiency can be estimated from the proportion of people estimated to have inadequate zinc intake, individual-level measurement of exposure truly needed to estimate the number of people at risk is not available. In a similar fashion, we used the proportion of the population in coarse occupational categories as a proxy for exposure to specific carcinogens and used fuel type as a proxy for household air pollution. Our ability to capture geographical variation and uncertainty in conversion of household solid fuel use to PM2·5 exposure improved the validity of our findings and UIs. Use of direct PM2·5 exposure measurement in households would be preferable to calibrate the widely available data for fuel use; however, such data have rarely been collected. As with all previous studies, we assessed the burden attributable to the availability of water and sanitation infrastructure, not the use of the infrastructure. Exposure for these risks has been defined in terms of availability and not use because that is what household surveys have collected. Our estimates are not biased, however, by this limitation because we derived relative risks from similar exposure definitions. Finally, we have not estimated intimate partner violence for men because of a scarcity of evidence of the health effects among men.
Conclusion
Quantification of the health effects of a diverse set of largely avoidable risks is an important input into any national or global strategy to improve population health and make progress towards the Sustainable Development Goals. For the first time, we have been able to separately assess and report trends in risk exposure and decompose trends in attributable burden into the contribution of demographic change, risk exposure, and risk-deleted rates. Reductions in some risks strongly associated with low levels of development, such as poor water, poor sanitation, household air pollution, and undernutrition, have been important contributors to global progress. Some crucial risks for NCDs, particularly obesity, high fasting plasma glucose, and alcohol, are increasing. Deleterious trends have had a smaller effect than expected because of favourable declines in risk-deleted DALY rates for many causes, a component of which might be due to access to effective health care. In an era of rapid transition in societies and levels of health, tracking of and response to key risks will require constant monitoring at the local level. As the set of risk factors expands to encompass access to specific health-care interventions in future iterations of GBD, the GBD CRA will provide an even more comprehensive understanding than in this study of the drivers of health improvement and how they relate to the operation and priorities of health systems.
Correspondence to: Prof Christopher J L Murray, Institute for Health Metrics and Evaluation, Seattle, WA 98121, USA cjlm@uw.edu
This online publication has been corrected. The corrected version first appeared at thelancet.com on January 5, 2017
Acknowledgments
Acknowledgments
We would like to thank the countless individuals who have contributed to the Global Burden of Disease Study 2015 in various capacities. The data used in this paper come from the 2009–10 Ghana Socioeconomic Panel Study Survey which is a nationally representative survey of over 5000 households in Ghana. The survey is a joint effort undertaken by the Institute of Statistical, Social and Economic Research (ISSER) at the University of Ghana, and the Economic Growth Centre (EGC) at Yale University. It was funded by the Economic Growth Center. At the same time, ISSER and the EGC are not responsible for the estimations reported by the analyst(s). HBSC is an international study carried out in collaboration with WHO/EURO. A list of principal investigators in each country can be found at http://www.hbsc.org. This analysis uses data or information from the LASI Pilot micro data and documentation. The development and release of the LASI Pilot Study was funded by the National Institute on Ageing / National Institute of Health (R21AG032572, R03AG043052, and R01 AG030153). The Palestinian Central Bureau of Statistics granted the researchers access to relevant data in accordance with license no SLN2014-3-170, after subjecting data to processing aiming to preserve the confidentiality of individual data in accordance with the General Statistics Law—2000. The researchers are solely responsible for the conclusions and inferences drawn upon available data. Persons interested in obtaining data files from Add Health should contact Add Health, Carolina Population Center, 123 W Franklin Street, Chapel Hill, NC 27516-2524 (addhealth@unc.edu). No direct support was received from grant P01-HD31921 for this analysis. This research used data from the National Health Survey 2009–2010, and the authors would like to gratefully acknowledge the Ministry of Health, Survey copyright owner, for use of the database. All results of the study are those of the authors and in no way committed to the Ministry. We thank the Russia Longitudinal Monitoring Survey, RLMS-HSE, conducted by the National Research University Higher School of Economics and ZAO “Demoscope” together with Carolina Population Center, University of North Carolina at Chapel Hill and the Institute of Sociology RAS for making these data available. The Panel Study of Income Dynamics is primarily sponsored by the National Science Foundation, the National Institute of Aging, and the National Institute of Child Health and Human Development and is conducted by the University of Michigan. The following individuals would like to acknowledge various forms of institutional support: Amanda G Thrift is supported by a fellowship from the National Health and Medical Research Council (GNT1042600). Boris Bikbov, Monica Cortinovis, Giuseppe Remuzzi, and Norberto Perico would like to acknowledge that their contribution to this paper has been on behalf of the International Society of Nephrology (ISN) as a follow-up of the activities of the GBD 2010 Genitourinary Diseases Expert Group. José das Neves was supported in his contribution to this work by a Fellowship from Fundação para a Ciência e a Tecnologia, Portugal (SFRH/BPD/92934/2013). Louisa Degenhardt is supported by an Australian National Health and Medical Research Council Principal Research fellowship. Miriam Levi would like to acknowledge the institutional support received from CeRIMP, Regional Centre for Occupational Diseases and Injuries, Tuscany Region, Florence, Italy. Nicholas Steel received funding from Public Health England as a Visiting Scholar in the Institute for Health Metrics and Evaluation in 2016. No individuals acknowledged received additional compensation for their efforts.
GBD 2015 Risk Factors Collaborators
Mohammad H Forouzanfar, Ashkan Afshin, Lily T Alexander, H Ross Anderson, Zulfiqar A Bhutta, Stan Biryukov, Michael Brauer, Richard Burnett, Kelly Cercy, Fiona J Charlson, Aaron J Cohen, Lalit Dandona, Kara Estep, Alize J Ferrari, Joseph J Frostad, Nancy Fullman, Peter W Gething, William W Godwin, Max Griswold, Simon I Hay, Yohannes Kinfu, Hmwe H Kyu, Heidi J Larson, Xiaofeng Liang, Stephen S Lim, Patrick Y Liu, Alan D Lopez, Rafael Lozano, Laurie Marczak, George A Mensah, Ali H Mokdad, Maziar Moradi-Lakeh, Mohsen Naghavi, Bruce Neal, Marissa B Reitsma, Gregory A Roth, Joshua A Salomon, Patrick J Sur, Theo Vos, Joseph A Wagner, Haidong Wang, Yi Zhao, Maigeng Zhou, Gunn Marit Aasvang*, Amanuel Alemu Abajobir*, Kalkidan Hassen Abate*, Cristiana Abbafati*, Kaja M Abbas*, Foad Abd-Allah*, Abdishakur M Abdulle*, Semaw Ferede Abera*, Biju Abraham*, Laith J Abu-Raddad*, Gebre Yitayih Abyu*, Akindele Olupelumi Adebiyi*, Isaac Akinkunmi Adedeji*, Zanfina Ademi*, Arsène Kouablan Adou*, José C Adsuar*, Emilie Elisabet Agardh*, Arnav Agarwal*, Anurag Agrawal*, Aliasghar Ahmad Kiadaliri*, Oluremi N Ajala*, Tomi F Akinyemiju*, Ziyad Al-Aly*, Khurshid Alam*, Noore K M Alam*, Saleh Fahed Aldhahri*, Robert William Aldridge*, Zewdie Aderaw Alemu*, Raghib Ali*, Ala'a Alkerwi*, François Alla*, Peter Allebeck*, Ubai Alsharif*, Khalid A Altirkawi*, Elena Alvarez Martin*, Nelson Alvis-Guzman*, Azmeraw T Amare*, Alemayehu Amberbir*, Adeladza Kofi Amegah*, Heresh Amini*, Walid Ammar*, Stephen Marc Amrock*, Hjalte H Andersen*, Benjamin O Anderson*, Carl Abelardo T Antonio*, Palwasha Anwari*, Johan Ärnlöv*, Al Artaman*, Hamid Asayesh*, Rana Jawad Asghar*, Reza Assadi*, Suleman Atique*, Euripide Frinel G Arthur Avokpaho*, Ashish Awasthi*, Beatriz Paulina Ayala Quintanilla*, Peter Azzopardi*, Umar Bacha*, Alaa Badawi*, Maria C Bahit*, Kalpana Balakrishnan*, Aleksandra Barac*, Ryan M Barber*, Suzanne L Barker-Collo*, Till Bärnighausen*, Simon Barquera*, Lars Barregard*, Lope H Barrero*, Sanjay Basu*, Carolina Batis*, Shahrzad Bazargan-Hejazi*, Justin Beardsley*, Neeraj Bedi*, Ettore Beghi*, Brent Bell*, Michelle L Bell*, Aminu K Bello*, Derrick A Bennett*, Isabela M Bensenor*, Adugnaw Berhane*, Eduardo Bernabé*, Balem Demtsu Betsu*, Addisu Shunu Beyene*, Neeraj Bhala*, Anil Bhansali*, Samir Bhatt*, Sibhatu Biadgilign*, Boris Bikbov*, Donal Bisanzio*, Espen Bjertness*, Jed D Blore*, Rohan Borschmann*, Soufiane Boufous*, Rupert R A Bourne*, Michael Brainin*, Alexandra Brazinova*, Nicholas J K Breitborde*, Hermann Brenner*, David M Broday*, Traolach S Brugha*, Bert Brunekreef*, Zahid A Butt*, Leah E Cahill*, Bianca Calabria*, Ismael Ricardo Campos-Nonato*, Rosario Cárdenas*, David O Carpenter*, Juan Jesus Carrero*, Daniel C Casey*, Carlos A Castañeda-Orjuela*, Jacqueline Castillo Rivas*, Ruben Estanislao Castro*, Ferrán Catalá-López*, Jung-Chen Chang*, Peggy Pei-Chia Chiang*, Mirriam Chibalabala*, Odgerel Chimed-Ochir*, Vesper Hichilombwe Chisumpa*, Abdulaal A Chitheer*, Jee-Young Jasmine Choi*, Hanne Christensen*, Devasahayam Jesudas Christopher*, Liliana G Ciobanu*, Matthew M Coates*, Samantha M Colquhoun*, Alejandra G Contreras Manzano*, Leslie Trumbull Cooper*, Kimberly Cooperrider*, Leslie Cornaby*, Monica Cortinovis*, John A Crump*, Lucia Cuevas-Nasu*, Albertino Damasceno*, Rakhi Dandona*, Sarah C Darby*, Paul I Dargan*, José das Neves*, Adrian C Davis*, Kairat Davletov*, E Filipa de Castro*, Vanessa De la Cruz-Góngora*, Diego De Leo*, Louisa Degenhardt*, Liana C Del Gobbo*, Borja del Pozo-Cruz*, Robert P Dellavalle*, Amare Deribew*, Don C Des Jarlais*, Samath D Dharmaratne*, Preet K Dhillon*, Cesar Diaz-Torné*, Daniel Dicker*, Eric L Ding*, E Ray Dorsey*, Kerrie E Doyle*, Tim R Driscoll*, Leilei Duan*, Manisha Dubey*, Bruce Bartholow Duncan*, Iqbal Elyazar*, Aman Yesuf Endries*, Sergey Petrovich Ermakov*, Holly E Erskine*, Babak Eshrati*, Alireza Esteghamati*, Saman Fahimi*, Emerito Jose Aquino Faraon*, Talha A Farid*, Carla Sofia e Sa Farinha*, André Faro*, Maryam S Farvid*, Farshad Farzadfar*, Valery L Feigin*, Seyed-Mohammad Fereshtehnejad*, Jefferson G Fernandes*, Florian Fischer*, Joseph R A Fitchett*, Tom Fleming*, Nataliya Foigt*, Kyle Foreman*, F Gerry R Fowkes*, Richard C Franklin*, Thomas Fürst*, Neal D Futran*, Emmanuela Gakidou*, Alberto L Garcia-Basteiro*, Tsegaye Tewelde Gebrehiwot*, Amanuel Tesfay Gebremedhin*, Johanna M Geleijnse*, Bradford D Gessner*, Ababi Zergaw Giref*, Maurice Giroud*, Melkamu Dedefo Gishu*, Giorgia Giussani*, Shifalika Goenka*, Mari Carmen Gomez-Cabrera*, Hector Gomez-Dantes*, Philimon Gona*, Amador Goodridge*, Sameer Vali Gopalani*, Carolyn C Gotay*, Atsushi Goto*, Hebe N Gouda*, Harish Chander Gugnani*, Francis Guillemin*, Yuming Guo*, Rahul Gupta*, Rajeev Gupta*, Reyna A Gutiérrez*, Juanita A Haagsma*, Nima Hafezi-Nejad*, Demewoz Haile*, Gessessew Bugssa Hailu*, Yara A Halasa*, Randah Ribhi Hamadeh*, Samer Hamidi*, Alexis J Handal*, Graeme J Hankey*, Yuantao Hao*, Hilda L Harb*, Sivadasanpillai Harikrishnan*, Josep Maria Haro*, Mohammad Sadegh Hassanvand*, Tahir Ahmed Hassen*, Rasmus Havmoeller*, Ileana Beatriz Heredia-Pi*, Norberto Francisco Hernández-Llanes*, Pouria Heydarpour*, Hans W Hoek*, Howard J Hoffman*, Masako Horino*, Nobuyuki Horita*, H Dean Hosgood*, Damian G Hoy*, Mohamed Hsairi*, Aung Soe Htet*, Guoqing Hu*, John J Huang*, Abdullatif Husseini*, Sally J Hutchings*, Inge Huybrechts*, Kim Moesgaard Iburg*, Bulat T Idrisov*, Bogdan Vasile Ileanu*, Manami Inoue*, Troy A Jacobs*, Kathryn H Jacobsen*, Nader Jahanmehr*, Mihajlo B Jakovljevic*, Henrica A F M Jansen*, Simerjot K Jassal*, Mehdi Javanbakht*, Sudha P Jayaraman*, Achala Upendra Jayatilleke*, Sun Ha Jee*, Panniyammakal Jeemon*, Vivekanand Jha*, Ying Jiang*, Tariku Jibat*, Ye Jin*, Catherine O Johnson*, Jost B Jonas*, Zubair Kabir*, Yogeshwar Kalkonde*, Ritul Kamal*, Haidong Kan*, André Karch*, Corine Kakizi Karema*, Chante Karimkhani*, Amir Kasaeian*, Anil Kaul*, Norito Kawakami*, Dhruv S Kazi*, Peter Njenga Keiyoro*, Laura Kemmer*, Andrew Haddon Kemp*, Andre Pascal Kengne*, Andre Keren*, Chandrasekharan Nair Kesavachandran*, Yousef Saleh Khader*, Abdur Rahman Khan*, Ejaz Ahmad Khan*, Gulfaraz Khan*, Young-Ho Khang*, Shahab Khatibzadeh*, Sahil Khera*, Tawfik Ahmed Muthafer Khoja*, Jagdish Khubchandani*, Christian Kieling*, Cho-il Kim*, Daniel Kim*, Ruth W Kimokoti*, Niranjan Kissoon*, Miia Kivipelto*, Luke D Knibbs*, Yoshihiro Kokubo*, Jacek A Kopec*, Parvaiz A Koul*, Ai Koyanagi*, Michael Kravchenko*, Hans Kromhout*, Hans Krueger*, Tiffany Ku*, Barthelemy Kuate Defo*, Ricardo S Kuchenbecker*, Burcu Kucuk Bicer*, Ernst J Kuipers*, G Anil Kumar*, Gene F Kwan*, Dharmesh Kumar Lal*, Ratilal Lalloo*, Tea Lallukka*, Qing Lan*, Anders Larsson*, Asma Abdul Latif*, Alicia Elena Beatriz Lawrynowicz*, Janet L Leasher*, James Leigh*, Janni Leung*, Miriam Levi*, Xiaohong Li*, Yichong Li*, Juan Liang*, Shiwei Liu*, Belinda K Lloyd*, Giancarlo Logroscino*, Paulo A Lotufo*, Raimundas Lunevicius*, Michael MacIntyre*, Mahdi Mahdavi*, Marek Majdan*, Azeem Majeed*, Reza Malekzadeh*, Deborah Carvalho Malta*, Wondimu Ayele Ayele Manamo*, Chabila C Mapoma*, Wagner Marcenes*, Randall V Martin*, Jose Martinez-Raga*, Felix Masiye*, Kunihiro Matsushita*, Richard Matzopoulos*, Bongani M Mayosi*, John J McGrath*, Martin McKee*, Peter A Meaney*, Catalina Medina*, Alem Mehari*, Fabiola Mejia-Rodriguez*, Alemayehu B Mekonnen*, Yohannes Adama Melaku*, Ziad A Memish*, Walter Mendoza*, Gert B M Mensink*, Atte Meretoja*, Tuomo J Meretoja*, Yonatan Moges Mesfin*, Francis Apolinary Mhimbira*, Anoushka Millear*, Ted R Miller*, Edward J Mills*, Mojde Mirarefin*, Awoke Misganaw*, Charles N Mock*, Alireza Mohammadi*, Shafiu Mohammed*, Glen Liddell D Mola*, Lorenzo Monasta*, Julio Cesar Montañez Hernandez*, Marcella Montico*, Lidia Morawska*, Rintaro Mori*, Dariush Mozaffarian*, Ulrich O Mueller*, Erin Mullany*, John Everett Mumford*, Gudlavalleti Venkata Satyanarayana Murthy*, Jean B Nachega*, Aliya Naheed*, Vinay Nangia*, Nariman Nassiri*, John N Newton*, Marie Ng*, Quyen Le Nguyen*, Muhammad Imran Nisar*, Patrick Martial Nkamedjie Pete*, Ole F Norheim*, Rosana E Norman*, Bo Norrving*, Luke Nyakarahuka*, Carla Makhlouf Obermeyer*, Felix Akpojene Ogbo*, In-Hwan Oh*, Olanrewaju Oladimeji*, Pedro R Olivares*, Helen Olsen*, Bolajoko Olubukunola Olusanya*, Jacob Olusegun Olusanya*, John Nelson Opio*, Eyal Oren*, Ricardo Orozco*, Alberto Ortiz*, Erika Ota*, Mahesh PA*, Adrian Pana*, Eun-Kee Park*, Charles D Parry*, Mahboubeh Parsaeian*, Tejas Patel*, Angel J Paternina Caicedo*, Snehal T Patil*, Scott B Patten*, George C Patton*, Neil Pearce*, David M Pereira*, Norberto Perico*, Konrad Pesudovs*, Max Petzold*, Michael Robert Phillips*, Frédéric B Piel*, Julian David Pillay*, Dietrich Plass*, Suzanne Polinder*, Constance D Pond*, C Arden Pope*, Daniel Pope*, Svetlana Popova*, Richie G Poulton*, Farshad Pourmalek*, Noela M Prasad*, Mostafa Qorbani*, Rynaz H S Rabiee*, Amir Radfar*, Anwar Rafay*, Vafa Rahimi-Movaghar*, Mahfuzar Rahman*, Mohammad Hifz Ur Rahman*, Sajjad Ur Rahman*, Rajesh Kumar Rai*, Sasa Rajsic*, Murugesan Raju*, Usha Ram*, Saleem M Rana*, Kavitha Ranganathan*, Puja Rao*, Christian Aspacia Razo García*, Amany H Refaat*, Colin D Rehm*, Jürgen Rehm*, Nikolas Reinig*, Giuseppe Remuzzi*, Serge Resnikoff*, Antonio L Ribeiro*, Juan A Rivera*, Hirbo Shore Roba*, Alina Rodriguez*, Sonia Rodriguez-Ramirez*, David Rojas-Rueda*, Yesenia Roman*, Luca Ronfani*, Gholamreza Roshandel*, Dietrich Rothenbacher*, Ambuj Roy*, Muhammad Muhammad Saleh*, Juan R Sanabria*, Lidia Sanchez-Riera*, Maria Dolores Sanchez-Niño*, Tania G Sánchez-Pimienta*, Logan Sandar*, Damian F Santomauro*, Itamar S Santos*, Rodrigo Sarmiento-Suarez*, Benn Sartorius*, Maheswar Satpathy*, Miloje Savic*, Monika Sawhney*, Josef Schmidhuber*, Maria Inês Schmidt*, Ione J C Schneider*, Ben Schöttker*, Aletta E Schutte*, David C Schwebel*, James G Scott*, Soraya Seedat*, Sadaf G Sepanlou*, Edson E Servan-Mori*, Gavin Shaddick*, Amira Shaheen*, Saeid Shahraz*, Masood Ali Shaikh*, Teresa Shamah Levy*, Rajesh Sharma*, Jun She*, Sara Sheikhbahaei*, Jiabin Shen*, Kevin N Sheth*, Peilin Shi*, Kenji Shibuya*, Mika Shigematsu*, Min-Jeong Shin*, Rahman Shiri*, Kawkab Shishani*, Ivy Shiue*, Mark G Shrime*, Inga Dora Sigfusdottir*, Diego Augusto Santos Silva*, Dayane Gabriele Alves Silveira*, Jonathan I Silverberg*, Edgar P Simard*, Shireen Sindi*, Abhishek Singh*, Jasvinder A Singh*, Prashant Kumar Singh*, Erica Leigh Slepak*, Michael Soljak*, Samir Soneji*, Reed J D Sorensen*, Luciano A Sposato*, Chandrashekhar T Sreeramareddy*, Vasiliki Stathopoulou*, Nadine Steckling*, Nicholas Steel*, Dan J Stein*, Murray B Stein*, Heidi Stöckl*, Saverio Stranges*, Konstantinos Stroumpoulis*, Bruno F Sunguya*, Soumya Swaminathan*, Bryan L Sykes*, Cassandra E I Szoeke*, Rafael Tabarés-Seisdedos*, Ken Takahashi*, Roberto Tchio Talongwa*, Nikhil Tandon*, David Tanne*, Mohammad Tavakkoli*, Belaynew Wasie Taye*, Hugh R Taylor*, Bemnet Amare Tedla*, Worku Mekonnen Tefera*, Teketo Kassaw Tegegne*, Dejen Yemane Tekle*, Abdullah Sulieman Terkawi*, J S Thakur*, Bernadette A Thomas*, Matthew Lloyd Thomas*, Alan J Thomson*, Andrew L Thorne-Lyman*, Amanda G Thrift*, George D Thurston*, Taavi Tillmann*, Ruoyan Tobe-Gai*, Myriam Tobollik*, Roman Topor-Madry*, Fotis Topouzis*, Jeffrey Allen Towbin*, Bach Xuan Tran*, Zacharie Tsala Dimbuene*, Nikolaos Tsilimparis*, Abera Kenay Tura*, Emin Murat Tuzcu*, Stefanos Tyrovolas*, Kingsley N Ukwaja*, Eduardo A Undurraga*, Chigozie Jesse Uneke*, Olalekan A Uthman*, Aaron van Donkelaar*, Jim van Os*, Yuri Y Varakin*, Tommi Vasankari*, J Lennert Veerman*, Narayanaswamy Venketasubramanian*, Francesco S Violante*, Stein Emil Vollset*, Gregory R Wagner*, Stephen G Waller*, JianLi Wang*, Linhong Wang*, Yanping Wang*, Scott Weichenthal*, Elisabete Weiderpass*, Robert G Weintraub*, Andrea Werdecker*, Ronny Westerman*, Harvey A Whiteford*, Tissa Wijeratne*, Charles Shey Wiysonge*, Charles D A Wolfe*, Sungho Won*, Anthony D Woolf*, Mamo Wubshet*, Denis Xavier*, Gelin Xu*, Ajit Kumar Yadav*, Bereket Yakob*, Ayalnesh Zemene Yalew*, Yuichiro Yano*, Mehdi Yaseri*, Pengpeng Ye*, Paul Yip*, Naohiro Yonemoto*, Seok-Jun Yoon*, Mustafa Z Younis*, Chuanhua Yu*, Zoubida Zaidi*, Maysaa El Sayed Zaki*, Jun Zhu*, Ben Zipkin*, Sanjay Zodpey*, Liesl Joanna Zuhlke*, Christopher J L Murray†.
*Authors listed alphabetically. †Corresponding author.
Affiliations
Institute for Health Metrics and Evaluation (M H Forouzanfar PhD, A Afshin MD, L T Alexander BA, S Biryukov BS, Prof M Brauer ScD, K Cercy BS, F J Charlson PhD, A J Cohen DSc, Prof L Dandona MD, K Estep MPA, A J Ferrari PhD, J J Frostad MPH, N Fullman MPH, W W Godwin BS, M Griswold MS, Prof S I Hay DSc, H H Kyu PhD, H J Larson PhD, Prof S S Lim PhD, P Y Liu BA, Prof A D Lopez PhD, Prof R Lozano MD, L Marczak PhD, Prof A H Mokdad PhD, M Moradi-Lakeh MD, Prof M Naghavi PhD, M B Reitsma BS, G A Roth MD, P J Sur BA, Prof T Vos PhD, J A Wagner BS, H Wang PhD, Y Zhao BS, Prof M Zhou PhD, R M Barber BS, B Bell MLIS, J D Blore PhD, D C Casey BA, M M Coates MPH, K Cooperrider BA, L Cornaby BS, D Dicker BS, H E Erskine PhD, T Fleming BS, K Foreman PhD, E Gakidou PhD, J A Haagsma PhD, C O Johnson PhD, L Kemmer PhD, T Ku BA, J Leung PhD, F Masiye PhD, A Millear BA, M Mirarefin MPH, A Misganaw PhD, M Moradi-Lakeh MD, E Mullany BA, J E Mumford BA, M Ng PhD, H Olsen MA, P Rao MPH, N Reinig BS, Y Roman MLIS, L Sandar BS, D F Santomauro PhD, E L Slepak MLIS, R J D Sorensen MPH, B A Thomas MD, Prof S E Vollset DrPH, Prof H A Whiteford PhD, B Zipkin BS, Prof C J L Murray DPhil), Harborview Injury Prevention and Research Center (C N Mock PhD), University of Washington, Seattle, WA, USA (Prof B O Anderson MD, N D Futran MD); Population Health Research Institute, St George's, University of London, London, UK (H R Anderson MD); Centre of Excellence in Women and Child Health (Prof Z A Bhutta PhD), Aga Khan University, Karachi, Pakistan (M I Nisar MSc); Centre for Global Child Health, The Hospital for Sick Children, Toronto, ON, Canada (Prof Z A Bhutta PhD, N Akseer MSc); School of Population and Public Health (H Krueger PhD), University of British Columbia, Vancouver, BC, Canada (Prof M Brauer ScD, C C Gotay PhD, Prof N Kissoon MD, J A Kopec PhD, F Pourmalek PhD); Health Canada, Ottawa, ON, Canada (R Burnett PhD); School of Public Health (F J Charlson PhD, A J Ferrari PhD, A A Abajobir MPH, H E Erskine PhD, L D Knibbs PhD, J Leung PhD, D F Santomauro PhD, J L Veerman PhD, Prof H A Whiteford PhD), School of Dentistry (Prof R Lalloo PhD), Centre for Clinical Research (J G Scott PhD), University of Queensland, Brisbane, QLD, Australia (N K M Alam MPH, H N Gouda PhD, Y Guo PhD, Prof J J McGrath MD); Queensland Centre for Mental Health Research, Brisbane, QLD, Australia (F J Charlson PhD, A J Ferrari PhD, H E Erskine PhD, J Leung PhD, D F Santomauro PhD, Prof H A Whiteford PhD); Health Effects Institute, Boston, MA, USA (A J Cohen DSc); Centre for Control of Chronic Conditions (P Jeemon PhD), Public Health Foundation of India, New Delhi, India (Prof L Dandona MD, R Dandona PhD, S Goenka PhD, G A Kumar PhD); Oxford Big Data Institute, Li Ka Shing Centre for Health Information and Discovery (Prof S I Hay DSc); Department of Zoology (P W Gething PhD), Nuffield Department of Medicine (D Bisanzio PhD, A Deribew PhD), Clinical Trial Service Unit (S C Darby PhD), University of Oxford, Oxford, UK (R Ali FRCP, D A Bennett PhD, Prof V Jha DM); Centre for Research & Action in Public Health, Faculty of Health, University of Canberra, Canberra, ACT, Australia (Y Kinfu PhD); Department of Infectious Disease Epidemiology (H J Larson PhD), London School of Hygiene & Tropical Medicine, London, UK (Prof M McKee DSc, Prof G V S Murthy MD, Prof N Pearce PhD, H Stöckl DPhil); National Center for Chronic and Noncommunicable Disease Control and Prevention (Prof M Zhou PhD, L Duan MD, Y Jin MS, Y Li MPH, S Liu PhD, Prof L Wang MD, P Ye MPH), Chinese Center for Disease Control and Prevention, Beijing, China (Prof X Liang MD); Melbourne School of Population and Global Health (Prof A D Lopez PhD), Department of Paediatrics (P Azzopardi MEpi, Prof G C Patton MD), Department of Medicine (A Meretoja PhD), Murdoch Childrens Research Institute (K Alam PhD, P Azzopardi MEpi, R Borschmann PhD, S M Colquhoun PhD, Prof G C Patton MD, R G Weintraub MBBS), Institute of Health and Ageing (Prof C E I Szoeke PhD), The University of Melbourne, Melbourne, VIC, Australia (Z Ademi PhD, K Alam PhD, R Borschmann PhD, S M Colquhoun PhD, Prof H R Taylor AC, R G Weintraub MBBS, Prof T Wijeratne MD); National Council for Science and Technology (C Batis PhD), National Institute of Public Health, Cuernavaca, Mexico (R Lozano MD, S Barquera PhD, I R Campos-Nonato PhD, A G Contreras Manzano MSc, L Cuevas-Nasu MSc, V De la Cruz-Góngora MSc, H Gomez-Dantes MSc, I B Heredia-Pi PhD, C Medina MS, F Mejia-Rodriguez MD, J C Montañez Hernandez MSc, C A Razo-García MSc, Prof J A Rivera PhD, S Rodríguez-Ramírez DSc, T G Sánchez-Pimienta MSc, Prof E E Servan-Mori MSc, T Shamah Levy PhD); Center for Translation Research and Implementation Science, National Heart, Lung, and Blood Institute (G A Mensah MD), Epidemiology and Statistics Program, National Institute on Deafness and Other Communication Disorders (H J Hoffman MA), National Institutes of Health, Bethesda, MD, USA; The George Institute for Global Health, Sydney, NSW, Australia (Prof B Neal PhD); Sydney School of Public Health (Prof T R Driscoll PhD), The University of Sydney, Sydney, NSW, Australia (Prof B Neal PhD, K Alam PhD, Prof A H Kemp PhD, J Leigh PhD, A B Mekonnen MS); Royal Prince Alfred Hospital, Sydney, NSW, Australia (Prof B Neal PhD); Department of Infectious Disease Epidemiology (S Bhatt DPhil, T Fürst PhD), Department of Epidemiology and Biostatistics, School of Public Health (F B Piel PhD, Prof A Rodriguez PhD), Imperial College London, London, UK (S J Hutchings BSc, Prof A Majeed MD, Prof B Neal PhD, M Soljak PhD); Department of Global Health and Population, (Prof J A Salomon PhD), Department of Nutrition, (A L Thorne-Lyman ScD), Harvard T H Chan School of Public Health (O N Ajala MD, Prof T Bärnighausen MD, L E Cahill PhD, I R Campos-Nonato PhD, E L Ding ScD, M S Farvid PhD, S Khatibzadeh MD, G R Wagner MD), Harvard Medical School (M G Shrime MD), Harvard University, Boston, MA, USA (J R A Fitchett MD); Centre for Disease Burden (Prof S E Vollset DrPH), Norwegian Institute of Public Health, Oslo, Norway (G M Aasvang PhD, M Savic PhD); Jimma University, Jimma, Ethiopia (K H Abate MS, T T Gebrehiwot MPH, A T Gebremedhin MPH); La Sapienza, University of Rome, Rome, Italy (C Abbafati PhD); Virginia Tech, Blacksburg, VA, USA (Prof K M Abbas PhD); Department of Neurology, Cairo University, Cairo, Egypt (Prof F Abd-Allah MD); New York University Abu Dhabi, Abu Dhabi, United Arab Emirates (A M Abdulle PhD); School of Public Health, College of Health Sciences (S F Abera MSc), School of Public Health (Y A Melaku MPH), Mekelle University, Mekelle, Ethiopia (Prof G Y Abyu MS, B D Betsu MS, G B Hailu MSc, D Y Tekle MS, A Z Yalew MS); Kilte Awlaelo-Health and Demographic Surveillance Site, Mekelle, Ethiopia (S F Abera MSc); Food Security and Institute for Biological Chemistry and Nutrition, University of Hohenheim, Stuttgart, Germany (S F Abera MSc); NMSM Government College Kalpetta, Kerala, India (Prof B Abraham MPhil); Infectious Disease Epidemiology Group, Weill Cornell Medical College in Qatar, Doha, Qatar (L J Abu-Raddad PhD); College of Medicine, University of Ibadan, Ibadan, Nigeria (A O Adebiyi MD); University College Hospital, Ibadan, Nigeria (A O Adebiyi MD); Olabisi Onabanjo University, Ago-Iwoye, Nigeria (I A Adedeji MS); University of Basel, Basel, Switzerland (Z Ademi PhD, T Fürst PhD); Association Ivoirienne pour le Bien-Être Familial, Abidjan, Côte d'Ivoire (A K Adou MD); University of Extremadura, Cáceres, Spain (Prof J C Adsuar PhD); Institution of Public Health Sciences, Stockholm, Sweden (E E Agardh PhD); Dalla Lana School of Public Health (N Akseer MSc, Prof J Rehm PhD), Department of Nutritional Sciences, Faculty of Medicine (A Badawi PhD), Centre for Addiction and Mental Health (S Popova PhD), University of Toronto, Toronto, ON, Canada (A Agarwal BHSc); McMaster University, Hamilton, ON, Canada (A Agarwal BHSc); CSIR Institute of Genomics and Integrative Biology, Delhi, India (A Agrawal PhD); Department of Internal Medicine, Baylor College of Medicine, Houston, TX, USA (A Agrawal PhD); Department of Clinical Sciences Lund, Orthopedics, Clinical Epidemiology Unit, Lund University, Lund, Sweden (A Ahmad Kiadaliri PhD); Health Services Management Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran (A Ahmad Kiadaliri PhD); University of Pittsburgh Medical Center, McKeesport, PA, USA (O N Ajala MD); Department of Epidemiology (T F Akinyemiju PhD), University of Alabama at Birmingham, Birmingham, AL, USA (D C Schwebel PhD, J A Singh MD); Washington University in Saint Louis, St Louis, MO, USA (Z Al-Aly MD); Queensland Health, Herston, QLD, Australia (N K M Alam MPH); King Saud University, Riyadh, Saudi Arabia (S F Aldhahri MD, K A Altirkawi MD); Department of Anesthesiology (A S Terkawi MD), King Fahad Medical City, Riyadh, Saudi Arabia (S F Aldhahri MD); Centre for Public Health Data Science, Institute of Health Informatics (R W Aldridge PhD), Department of Epidemiology and Public Health (T Tillmann MSc), University College London, London, UK; Debre Markos University, Debre Markos, Ethiopia (Z A Alemu MPH, T K Tegegne MPH); Luxembourg Institute of Health (LIH), Strassen, Luxembourg (A Alkerwi PhD); School of Public Health, University of Lorraine, Nancy, France (Prof F Alla PhD, F Guillemin PhD); Department of Public Health Sciences (P Allebeck PhD, R H S Rabiee MPH), Department of Neurobiology, Care Sciences and Society (NVS) (S M Fereshtehnejad PhD), Aging Research Center (Prof M Kivipelto PhD), Department of Medical Epidemiology and Biostatistics (Prof J J Carrero PhD, E Weiderpass PhD), Karolinska Institutet, Stockholm, Sweden (R Havmoeller PhD, S Sindi PhD); Charité Universitätsmedizin, Berlin, Germany (U Alsharif MPH); Spanish Observatory on Drugs, Government Delegation for the National Plan on Drugs, Ministry of Health, Social Policy and Equality, Madrid, Spain (E Alvarez Martin PhD); Universidad de Cartagena, Cartagena de Indias, Colombia (Prof N Alvis-Guzman PhD); School of Medicine (A T Amare MPH, Y A Melaku MPH), University of Adelaide, Adelaide, SA, Australia (L G Ciobanu MS); College of Medicine and Health Sciences (A T Amare MPH), Bahir Dar University, Bahir Dar, Ethiopia (B W Taye MD); Dignitas International, Zomba, Malawi (A Amberbir PhD); University of Cape Coast, Cape Coast, Ghana (A K Amegah PhD); Environmental Health Research Center, Kurdistan University of Medical Sciences, Sanandaj, Iran (H Amini MSPH); Department of Epidemiology and Public Health (H Amini MSPH, T Fürst PhD), Swiss Tropical and Public Health Institute, Basel, Switzerland (C K Karema MSc); Ministry of Public Health, Beirut, Lebanon (W Ammar PhD, H L Harb MPH); Oregon Health & Science University, Portland, OR, USA (S M Amrock MD); Center for Sensory-Motor Interaction, Department of Health Science and Technology, Faculty of Medicine, Aalborg University, Aalborg, Denmark (H H Andersen MSc); Department of Health Policy and Administration, College of Public Health (C A T Antonio MD), College of Public Health (E J A Faraon MD), University of the Philippines Manila, Manila, Philippines; Self-employed, Kabul, Afghanistan (P Anwari MD); Department of Medical Sciences, Uppsala University, Uppsala, Sweden (Prof J Ärnlöv PhD, Prof A Larsson PhD); Dalarna University, Falun, Sweden (Prof J Ärnlöv PhD); University of Manitoba, Winnipeg, MB, Canada (A Artaman PhD); Department of Medical Emergency, School of Paramedic, Qom University of Medical Sciences, Qom, Iran (H Asayesh PhD); South Asian Public Health Forum, Islamabad, Pakistan (R J Asghar MD); Mashhad University of Medical Sciences, Mashhad, Iran (R Assadi PhD); Graduate Institute of Biomedical Informatics, Taipei Medical University, Taipei, Taiwan (S Atique MS); Institut de Recherche Clinique du Bénin, Cotonou, Benin Republic (E F G A Avokpaho MPH); Laboratoire d'Etudes et de Recherche-Action en Santé (LERAS Afrique), Parakou, Benin Republic (E F G A Avokpaho MPH); Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India (A Awasthi MSc); The Judith Lumley Centre for Mother, Infant and Family Health Research, La Trobe University, Melbourne, VIC, Australia (B P Ayala Quintanilla PhD); Peruvian National Institute of Health, Lima, Peru (B P Ayala Quintanilla PhD); Wardliparingga Aboriginal Research Unit, South Australian Health and Medical Research Institute, Adelaide, SA, Australia (P Azzopardi MEpi); School of Health Sciences, University of Management and Technology, Lahore, Pakistan (U Bacha PhD); Public Health Agency of Canada, Toronto, ON, Canada (A Badawi PhD); INECO Neurociencias, Rosario, Argentina (M C Bahit MD); Department of Environmental Health Engineering, Sri Ramachandra University, Chennai, India (K Balakrishnan PhD); Faculty of Medicine, University of Belgrade, Belgrade, Serbia (A Barac PhD); School of Psychology (S L Barker-Collo PhD), University of Auckland, Auckland, New Zealand (B del Pozo-Cruz PhD); Africa Health Research Institute, Mtubatuba, South Africa (Prof T Bärnighausen MD); Institute of Public Health, Heidelberg University, Heidelberg, Germany (Prof T Bärnighausen MD, S Mohammed PhD); Department of Occupational and Environmental Health (Prof L Barregard MD), Health Metrics Unit (Prof M Petzold PhD), University of Gothenburg, Gothenburg, Sweden; Department of Industrial Engineering, School of Engineering, Pontificia Universidad Javeriana, Bogotá, Colombia (L H Barrero ScD); Stanford University, Stanford, CA, USA (S Basu PhD, L C Del Gobbo PhD); College of Medicine, Charles R Drew University of Medicine and Science, Los Angeles, CA, USA (Prof S Bazargan-Hejazi PhD); David Geffen School of Medicine, University of California, Los Angeles, Los Angeles, CA, USA (Prof S Bazargan-Hejazi PhD); Kermanshah University of Medical Science, Kermanshah, Iran (Prof S Bazargan-Hejazi PhD); Oxford University, Ho Chi Minh City, Vietnam (J Beardsley MBChB); College of Public Health and Tropical Medicine, Jazan, Saudi Arabia (N Bedi MD); IRCCS - Istituto di Ricerche Farmacologiche Mario Negri, Milan, Italy (E Beghi MD); School of Medicine (K N Sheth MD), Yale University, New Haven, CT, USA (Prof M L Bell PhD, J J Huang MD); University of Alberta, Edmonton, AB, Canada (A K Bello PhD); Internal Medicine Department (Prof I S Santos PhD), University of São Paulo, São Paulo, Brazil (I M Bensenor PhD, Prof P A Lotufo DrPH); Debre Berhane University, Debre Berhan, Ethiopia (A Berhane PhD); Division of Health and Social Care Research (Prof C D Wolfe MD), King's College London, London, UK (E Bernabé PhD); College of Health and Medical Sciences (H S Roba MPH), Haramaya University, Harar, Ethiopia (A S Beyene MPH, T A Hassen MS, Y M Mesfin MPH); Queen Elizabeth Hospital Birmingham, Birmingham, UK (N Bhala DPhil); University of Otago Medical School, Wellington, New Zealand (N Bhala DPhil); Postgraduate Institute of Medical Education and Research, Chandigarh, India (A Bhansali DM); Independent Public Health Consultants, Addis Ababa, Ethiopia (S Biadgilign MPH); Department of Nephrology Issues of Transplanted Kidney, Academician V I Shumakov Federal Research Center of Transplantology and Artificial Organs, Moscow, Russia (B Bikbov MD); Department of Community Medicine (Prof E Bjertness PhD), University of Oslo, Oslo, Norway (A S Htet MPhil); Transport and Road Safety (TARS) Research (S Boufous PhD), National Drug and Alcohol Research Centre (Prof L Degenhardt PhD), Brien Holden Vision Institute (Prof S Resnikoff MD), University of New South Wales, Kensington, NSW, Australia (B Calabria PhD); Vision & Eye Research Unit, Anglia Ruskin University, Cambridge, UK (Prof R R A Bourne FRCOphth); Danube-University Krems, Krems, Austria (Prof M Brainin PhD); Faculty of Health Sciences and Social Work, Department of Public Health, Trnava University, Trnava, Slovakia (A Brazinova PhD, M Majdan PhD); International Neurotrauma Research Organization, Vienna, Austria (A Brazinova PhD); College of Medicine (J Shen PhD), The Ohio State University, Columbus, OH, USA (Prof N J K Breitborde PhD); German Cancer Research Center, Heidelberg, Germany (Prof H Brenner MD, B Schöttker MPH); Technion, Haifa, Israel (Prof D M Broday DSc); University of Leicester, Leicester, UK (Prof T S Brugha MD); Institute for Risk Assessment Sciences, Utrecht University, Utrecht, Netherlands (Prof B Brunekreef PhD, Prof H Kromhout PhD); Al Shifa Trust Eye Hospital, Rawalpindi, Pakistan (Z A Butt PhD); Department of Physics and Atmospheric Science (A van Donkelaar PhD), Dalhousie University, Halifax, NS, Canada (L E Cahill PhD, Prof R V Martin PhD); National Centre for Epidemiology and Population Health, Australian National University, Canberra, ACT, Australia (B Calabria PhD); Metropolitan Autonomous University, Mexico City, Mexico (R Cárdenas ScD); University at Albany, Rensselaer, NY, USA (Prof D O Carpenter MD); Colombian National Health Observatory, Instituto Nacional de Salud, Bogotá, Colombia (C A Castañeda-Orjuela MSc); Epidemiology and Public Health Evaluation Group, Public Health Department, Universidad Nacional de Colombia, Bogotá, Colombia (C A Castañeda-Orjuela MSc); Caja Costarricense de Seguro Social, San Jose, Costa Rica (Prof J Castillo Rivas MPH); Universidad de Costa Rica, San Pedro, Montes de Oca, Costa Rica (Prof J Castillo Rivas MPH); Universidad Diego Portales, Santiago, Chile (R E Castro PhD); Department of Medicine, University of Valencia/INCLIVA Health Research Institute and CIBERSAM, Valencia, Spain (F Catalá-López PhD); Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, ON, Canada (F Catalá-López PhD); School of Nursing, College of Medicine, National Taiwan University, Taipei, Taiwan (Prof J Chang PhD); Clinical Governance Unit, Gold Coast Health, Southport, QLD, Australia (P P Chiang PhD); Crowd Watch Africa, Lusaka, Zambia (M Chibalabala BS); Department of Environmental Epidemiology (O Chimed-Ochir MPH), Department of Health Development, Institute of Industrial Ecological Sciences (Y Jiang PhD), Institute of Industrial Ecological Sciences, Department of Environmental Epidemiology (Prof K Takahashi MD), University of Occupational and Environmental Health, Kitakyushu, Japan; University of Zambia, Lusaka, Zambia (V H Chisumpa MPhil, C C Mapoma PhD, F Masiye PhD); University of Witwatersrand, Johannesburg, South Africa (V H Chisumpa MPhil); Ministry of Health, Baghdad, Iraq (A A Chitheer FETP); Seoul National University Medical Library, Seoul, South Korea (J J Choi PhD); Bispebjerg University Hospital, Copenhagen, Denmark (Prof H Christensen DMSCi); Christian Medical College, Vellore, India (Prof D J Christopher MD); Mayo Clinic, Jacksonville, FL, USA (L T Cooper MD); Centre for International Health, Dunedin School of Medicine (Prof J A Crump MD), University of Otago, Dunedin, New Zealand (Prof R G Poulton PhD); Faculty of Medicine, Eduardo Mondlane University, Maputo, Mozambique (Prof A Damasceno PhD); Guy's and St Thomas' NHS Foundation Trust, London, UK (Prof P I Dargan FRCP); i3S - Instituto de Investigação e Inovação em Saúde and INEB - Instituto de Engenharia Biomédica, University of Porto, Porto, Portugal (J das Neves PhD); Public Health England, London, UK (Prof A C Davis PhD, Prof J N Newton FRCP, Prof N Steel PhD); School of Public Health, Kazakh National Medical University, Almaty, Kazakhstan (K Davletov PhD); National Council for Science and Technology (C Batis PhD), National Institute of Public Health, Mexico City, Mexico (E F de Castro PhD); Griffith University, Brisbane, QLD, Australia (Prof D De Leo DSc); University of Colorado School of Medicine and the Colorado School of Public Health, Aurora, CO, USA (R P Dellavalle MD); KEMRI-Wellcome Trust Research Programme, Kilifi, Kenya (A Deribew PhD); Mount Sinai Beth Israel, New York, NY, USA (Prof D C Des Jarlais PhD); Icahn School of Medicine at Mount Sinai, New York, NY, USA (Prof D C Des Jarlais PhD); Department of Community Medicine, Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka (S D Dharmaratne MD); Centre for Control of Chronic Conditions (P Jeemon PhD), Public Health Foundation of India, Gurgaon, India (P K Dhillon PhD, D K Lal MD, Prof S Zodpey PhD); Hospital de la Santa Creu i Sant Pau, Barcelona, Spain (C Diaz-Torné MD); University of Rochester Medical Center, Rochester, NY, USA (E R Dorsey MD); RMIT University, Bundoora, VIC, Australia (Prof K E Doyle PhD); International Institute for Population Sciences, Mumbai, India (M Dubey MPhil, M H U Rahman MPhil, Prof U Ram PhD, A Singh PhD, A K Yadav MPhil); Federal University of Rio Grande do Sul, Porto Alegre, Brazil (B B Duncan PhD, C Kieling MD, Prof M I Schmidt MD); University of North Carolina, Chapel Hill, NC, USA (B B Duncan PhD); Eijkman-Oxford Clinical Research Unit, Jakarta, Indonesia (I Elyazar PhD); Arba Minch University, Arba Minch, Ethiopia (A Y Endries MPH); The Institute of Social and Economic Studies of Population, Russian Academy of Sciences, Moscow, Russia (Prof S P Ermakov DSc); Federal Research Institute for Health Organization and Informatics, Ministry of Health of the Russian Federation, Moscow, Russia (Prof S P Ermakov DSc); Ministry of Health and Medical Education, Tehran, Iran (B Eshrati PhD); Arak University of Medical Sciences, Arak, Iran (B Eshrati PhD); Non-Communicable Diseases Research Center (F Farzadfar MD, A Kasaeian PhD, M Parsaeian PhD), Endocrinology and Metabolism Population Sciences Institute (Prof A Esteghamati MD, N Hafezi-Nejad MD, S Sheikhbahaei MD), Digestive Diseases Research Institute (S Fahimi PhD, Prof R Malekzadeh MD, G Roshandel PhD, S G Sepanlou PhD), Center for Air Pollution Research, Institute for Environmental Research (M S Hassanvand PhD), Multiple Sclerosis Research Center, Neuroscience Institute (P Heydarpour MD), Hematology-Oncology and Stem Cell Transplantation Research Center (A Kasaeian PhD), Department of Epidemiology and Biostatistics, School of Public Health (M Parsaeian PhD), Sina Trauma and Surgery Research Center (Prof V Rahimi-Movaghar MD), Tehran University of Medical Sciences, Tehran, Iran (M Yaseri PhD); Department of Health, Manila, Philippines (E J A Faraon MD); University of Louisville, Louisville, KY, USA (T A Farid MD, A R Khan MD); DGS Directorate General of Health, Lisboa, Portugal (C S E S Farinha MSc); Universidade Aberta, Lisboa, Portugal (C S E S Farinha MSc); Federal University of Sergipe, Aracaju, Brazil (Prof A Faro PhD); Harvard/MGH Center on Genomics, Vulnerable Populations, and Health Disparities, Mongan Institute for Health Policy, Massachusetts General Hospital, Boston, MA, USA (M S Farvid PhD); National Institute for Stroke and Applied Neurosciences, Auckland University of Technology, Auckland, New Zealand (V L Feigin PhD); Institute of Education and Sciences, German Hospital Oswaldo Cruz, São Paulo, Brazil (Prof J G Fernandes PhD); Bielefeld University, Bielefeld, Germany (F Fischer MPH); Institute of Gerontology, Academy of Medical Science, Kyiv, Ukraine (N Foigt PhD); Alzheimer Scotland Dementia Research Centre (I Shiue PhD), University of Edinburgh, Edinburgh, UK (Prof F G R Fowkes PhD); James Cook University, Townsville, QLD, Australia (R C Franklin PhD); Manhiça Health Research Center, Manhiça, Mozambique (A L Garcia-Basteiro MSc); Barcelona Institute for Global Health, Barcelona, Spain (A L Garcia-Basteiro MSc); Ludwig Maximilians University, Munich, Germany (A T Gebremedhin MPH); Division of Human Nutrition (J M Geleijnse PhD), Wageningen University, Wageningen, Netherlands (T Jibat MS); Agence de Médecine Préventive, Paris, France (B D Gessner MD); College of Health Sciences, School of Public Health (W Tefera MPH), Addis Ababa University, Addis Ababa, Ethiopia (A Z Giref PhD, D Haile MPH, T Jibat MS, W A A Manamo MS); University Hospital of Dijon, Dijon, France (Prof M Giroud MD); College of Health and Medical Sciences (H S Roba MPH), Haramaya University, Dire Dawa, Ethiopia (M D Gishu MS A K Tura MPH); Kersa Health and Demographic Surveillance System, Harar, Ethiopia (M D Gishu MS); University Hospital Doctor Peset (J Martinez-Raga PhD), University of Valencia, Valencia, Spain (M C Gomez-Cabrera PhD); INCLIVA Biomedical Research Institute, Valencia, Spain (M C Gomez-Cabrera PhD); University of Massachusetts Boston, Boston, MA, USA (Prof P Gona PhD); Instituto de Investigaciones Cientificas y Servicios de Alta Tecnologia - INDICASAT-AIP, Ciudad del Saber, Panamá (A Goodridge PhD); Department of Health and Social Affairs, Government of the Federated States of Micronesia, Palikir, Federated States of Micronesia (S V Gopalani MPH); Division of Epidemiology, Center for Public Health Sciences (A Goto PhD), National Cancer Center, Tokyo, Japan (M Inoue MD); Departments of Microbiology and Epidemiology & Biostatistics, Saint James School of Medicine, The Quarter, Anguilla (Prof H C Gugnani PhD); West Virginia Bureau for Public Health, Charleston, WV, USA (R Gupta MD); Eternal Heart Care Centre and Research Institute, Jaipur, India (R Gupta PhD); National Institute of Psychiatry Ramon de la Fuente, Mexico City, Mexico (R A Gutiérrez PhD, Prof R Orozco MSc); Department of Public Health, Erasmus MC, University Medical Center, Rotterdam, Netherlands (J A Haagsma PhD); Kilte Awlaelo Health and Demographic Surveillance System, Mekelle, Ethiopia (G B Hailu MSc); Brandeis University, Waltham, MA, USA (Y A Halasa MS, E A Undurraga PhD); Arabian Gulf University, Manama, Bahrain (Prof R R Hamadeh DPhil); Hamdan Bin Mohammed Smart University, Dubai, United Arab Emirates (S Hamidi PhD); University of New Mexico, Albuquerque, NM, USA (A J Handal PhD); School of Medicine and Pharmacology, University of Western Australia, Perth, WA, Australia (Prof G J Hankey MD); Harry Perkins Institute of Medical Research, Nedlands, WA, Australia (Prof G J Hankey MD); Western Australian Neuroscience Research Institute, Nedlands, WA, Australia (Prof G J Hankey MD); School of Public Health, Sun Yat-sen University, Guangzhou, China (Prof Y Hao PhD); Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, India (S Harikrishnan DM); Parc Sanitari Sant Joan de Déu - CIBERSAM, Sant Boi de Llobregat (Barcelona), Spain (J M Haro MD); Universitat de Barcelona, Barcelona, Spain (J M Haro MD); Comisión Nacional contra las Adicciones, Mexico City, Mexico (Prof N F Hernández-Llanes BA); Department of Psychiatry, University Medical Center Groningen (Prof H W Hoek MD), University of Groningen, Groningen, Netherlands (A K Tura MPH); Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY, USA (Prof H W Hoek MD); Nevada Division of Public and Behavioral Health, Department of Health and Human Services, Carson City, NV, USA (M Horino MPH); Department of Pulmonology, Yokohama City University Graduate School of Medicine, Yokohama, Japan (N Horita MD); Albert Einstein College of Medicine, Bronx, NY, USA (Prof H D Hosgood PhD); Public Health Division, The Pacific Community, Noumea, New Caledonia (D G Hoy PhD); Department of Epidemiology, Salah Azaiz Institute, Tunis, Tunisia (Prof M Hsairi MD); International Relations Division, Ministry of Health, Nay Pyi Taw, Myanmar (A S Htet MPhil); Department of Epidemiology and Health Statistics, School of Public Health, Central South University, Changsha, China (G Hu PhD); Birzeit University, Birzeit, Palestine (A Husseini PhD); International Agency for Research on Cancer (IARC), Lyon, France (I Huybrechts PhD); Ghent University, Ghent, Belgium (I Huybrechts PhD); Aarhus University, Aarhus, Denmark (K M Iburg PhD); Boston Medical Center (B T Idrisov MD), School of Medicine (G F Kwan MD), Boston University, Boston, MA, USA; Bucharest University of Economic Studies, Bucharest, Romania (B V Ileanu MPH, A Pana MPH); Graduate School of Medicine (M Inoue MD), School of Public Health (Prof N Kawakami MD), University of Tokyo, Tokyo, Japan (K Shibuya MD); MCH Division, USAID - Global Health Bureau, HIDN, Washington, DC, USA (T A Jacobs MD); Department of Global and Community Health, George Mason University, Fairfax, VA, USA (K H Jacobsen PhD); School of Public Health (N Jahanmehr PhD), Ophthalmic Research Center (M Yaseri PhD), Shahid Beheshti University of Medical Sciences, Tehran, Iran; Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia (Prof M B Jakovljevic PhD); UNFPA Asia and the Pacific Regional Office, Bangkok, Thailand (H A F Jansen Drs); VA San Diego (S K Jassal MD), University of California, San Diego, La Jolla, CA, USA (M B Stein MD); University of Aberdeen, Aberdeen, UK (M Javanbakht PhD); Department of Surgery, Virginia Commonwealth University, Richmond, VA, USA (S P Jayaraman MD); Postgraduate Institute of Medicine, Colombo, Sri Lanka (A U Jayatilleke PhD); Institute of Violence and Injury Prevention, Colombo, Sri Lanka (A U Jayatilleke PhD); Graduate School of Public Health, Yonsei University, Seoul, South Korea (Prof S H Jee PhD); Centre for Chronic Disease Control, New Delhi, India (P Jeemon PhD); Addis Ababa University, Debre Zeit, Ethiopia (T Jibat MS); George Institute for Global Health India, New Delhi, India (Prof V Jha DM); Department of Ophthalmology, Medical Faculty Mannheim, Ruprecht-Karls-University Heidelberg, Mannheim, Germany (Prof J B Jonas MD); University College Cork, Cork, Ireland (Z Kabir PhD); Society for Education, Action and Research in Community Health, Gadchiroli, India (Y Kalkonde MD); CSIR - Indian Institute of Toxicology Research, Lucknow, India (R Kamal MSc, C N Kesavachandran PhD); Department of Pulmonary Medicine, Zhongshan Hospital (J She MD), Fudan University, Shanghai, China (H Kan MD); Epidemiological and Statistical Methods Research Group, Helmholtz Centre for Infection Research, Braunschweig, Germany (A Karch MD); Hannover-Braunschweig Site, German Center for Infection Research, Braunschweig, Germany (A Karch MD); Quality and Equity Health Care, Kigali, Rwanda (C K Karema MSc); Case Western University Hospitals, Cleveland, OH, USA (C Karimkhani MD); Oklahoma State University, Tulsa, OK, USA (A Kaul MD); University of California San Francisco, San Francisco, CA, USA (D S Kazi MD); Institute of Tropical and Infectious Diseases, Nairobi, Kenya (P N Keiyoro PhD); School of Continuing and Distance Education, Nairobi, Kenya (P N Keiyoro PhD); Swansea University, Swansea, UK (Prof A H Kemp PhD); Alcohol, Tobacco & Other Drug Research Unit (Prof C D Parry PhD), South African Medical Researcil, Cape Town, South Africa (A P Kengne PhD, R Matzopoulos PhD, Prof C S Wiysonge PhD); School of Public Health and Family Medicine (R Matzopoulos PhD), Department of Psychiatry (Prof D J Stein PhD), University of Cape Town, Cape Town, South Africa (A P Kengne PhD, Prof B M Mayosi DPhil); Assuta Hospitals, Assuta Hashalom, Tel Aviv, Israel (Prof A Keren MD); Jordan University of Science and Technology, Irbid, Jordan (Prof Y S Khader ScD); Health Services Academy, Islamabad, Pakistan (E A Khan MPH); Department of Microbiology and Immunology, College of Medicine & Health Sciences, United Arab Emirates University, Al Ain, United Arab Emirates (G Khan PhD); College of Medicine (Prof Y H Khang MD), Graduate School of Public Health (Prof S Won PhD), Seoul National University, Seoul, South Korea; New York Medical College, Valhalla, NY, USA (S Khera MD, M Tavakkoli MD); Executive Board of the Health Ministers' Council for Cooperation Council States, Riyadh, Saudi Arabia (Prof T A M Khoja FRCP); Ball State University, Muncie, IN, USA (J Khubchandani PhD); Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil (C Kieling MD); Korea Health Industry Development Institute, Cheongju-si, South Korea (C Kim PhD); Department of Health Sciences, Northeastern University, Boston, MA, USA (Prof D Kim DrPH); Simmons College, Boston, MA, USA (R W Kimokoti MD); Department of Preventive Cardiology, National Cerebral and Cardiovascular Center, Suita, Japan (Y Kokubo PhD); Sher-i-Kashmir Institute of Medical Sciences, Srinagar, India (Prof P A Koul MD); Research and Development Unit, Parc Sanitari Sant Joan de Deu (CIBERSAM), Barcelona, Spain (A Koyanagi MD); Research Center of Neurology, Moscow, Russia (M Kravchenko PhD, Prof Y Y Varakin MD); Department of Demography and Public Health Research Institute (Prof B Kuate Defo PhD), Department of Social and Preventive Medicine, School of Public Health (Prof B Kuate Defo PhD), University of Montreal, Montreal, QC, Canada; Graduation Studies in Epidemiology Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil (Prof R S Kuchenbecker PhD); Institute of Public Health, Hacettepe University, Ankara, Turkey (B Kucuk Bicer PhD); Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands (Prof E J Kuipers PhD); Work Organizations, Work Disability Prevention, The Finnish Institute of Occupational Health, Helsinki, Finland (T Lallukka PhD, R Shiri PhD); Department of Public Health, Faculty of Medicine (T Lallukka PhD), University of Helsinki, Helsinki, Finland (T J Meretoja PhD); National Cancer Institute, Rockville, MD, USA (Q Lan PhD); Department of Zoology, Lahore College for Women University, Lahore, Pakistan (A A Latif PhD); Instituto Nacional de Epidemiología “Dr Juan H Jara”, Mar del Plata, Argentina (A E B Lawrynowicz MPH); College of Optometry, Nova Southeastern University, Fort Lauderdale, FL, USA (J L Leasher OD); Tuscany Regional Centre for Occupational Injuries and Diseases, Florence, Italy (M Levi PhD); National Center of Birth Defects Monitoring of China, Chengdu, China (X Li MD); National Office for Maternal and Child Health Surveillance, West China Second University Hospital, Sichuan University, Chengdu, China (Prof J Liang MD); Eastern Health Clinical School (B K Lloyd PhD), Monash University, Fitzroy, VIC, Australia; Turning Point, Eastern Health, Melbourne, VIC, Australia (B K Lloyd PhD); University of Bari, Bari, Italy (Prof G Logroscino PhD); Aintree University Hospital National Health Service Foundation Trust, Liverpool, UK (Prof R Lunevicius PhD); School of Medicine (Prof R Lunevicius PhD), Department of Public Health and Policy (D Pope PhD), University of Liverpool, Liverpool, UK; Social Security Organization Research Institute, Tehran, Iran (M Mahdavi PhD); Institute of Health Policy and Management, Erasmus University Rotterdam, Rotterdam, Netherlands (M Mahdavi PhD); Universidade Federal de Minas Gerais, Belo Horizonte, Brazil (Prof D C Malta PhD); Division of Population and Patient Health, King's College London Dental Institute, London, UK (Prof W Marcenes PhD); CEU Cardenal Herrera University, Moncada (Valencia), Spain (J Martinez-Raga PhD); Bloomberg School of Public Health (K Matsushita PhD, Prof J B Nachega PhD), Johns Hopkins University, Baltimore, MD, USA (B X Tran PhD); Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA (P A Meaney MD); Children's Hospital of Philadelphia, Philadelphia, PA, USA (P A Meaney MD); College of Medicine, Howard University, Washington, DC, USA (A Mehari MD); University of Gondar, Gondar, Ethiopia (A B Mekonnen MS, B A Tedla BS); Saudi Ministry of Health, Riyadh, Saudi Arabia (Prof Z A Memish MD); College of Medicine, Alfaisal University, Riyadh, Saudi Arabia (Prof Z A Memish MD); United Nations Population Fund, Lima, Peru (W Mendoza MD); Robert Koch Institute, Berlin, Germany (G B M Mensink PhD); Department of Neurology, Helsinki University Hospital, Helsinki, Finland (A Meretoja PhD); Helsinki University Hospital, Comprehensive Cancer Center, Breast Surgery Unit, Helsinki, Finland (T J Meretoja PhD); Ifakara Health Institute, Bagamoyo, Tanzania (F A Mhimbira MS); Pacific Institute for Research & Evaluation, Calverton, MD, USA (T R Miller PhD); Centre for Population Health, Curtin University, Perth, WA, Australia (T R Miller PhD); University of Ottawa, Ottawa, ON, Canada (E J Mills PhD); Neuroscience Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran (A Mohammadi PhD); Health Systems and Policy Research Unit, Ahmadu Bello University, Zaria, Nigeria (S Mohammed PhD); University of Papua New Guinea, Boroko, Papua New Guinea (Prof G L D Mola DPH FRANCOG); Institute for Maternal and Child Health, IRCCS “Burlo Garofolo,” Trieste, Italy (L Monasta DSc, M Montico MSc, L Ronfani PhD); Department of Community Medicine, Gastrointestinal and Liver Disease Research Center, Preventive Medicine and Public Health Research Center, Iran University of Medical Sciences, Tehran, Iran (M Moradi-Lakeh MD); International Laboratory for Air Quality and Health (L Morawska PhD), Institute of Health and Biomedical Innovation (R E Norman PhD), Queensland University of Technology, Brisbane, QLD, Australia; National Center for Child Health and Development, Setagaya, Japan (R Mori PhD); Friedman School of Nutrition Science and Policy (D Mozaffarian MD), Tufts University, Boston, MA, USA (P Shi PhD); Competence Center Mortality-Follow-Up of the German National Cohort (A Werdecker PhD), Federal Institute for Population Research, Wiesbaden, Germany (Prof U O Mueller PhD, R Westerman PhD); Indian Institute of Public Health (Prof G V S Murthy MD), Public Health Foundation of India, Gurgaon, India (P K Dhillon PhD, D K Lal MD, Prof S Zodpey PhD); Graduate School of Public Health (Prof J B Nachega PhD), Public Health Dynamics Laboratory (A J Paternina Caicedo MD), University of Pittsburgh, Pittsburgh, PA, USA; Department of Psychiatry (Prof C D Parry PhD), Stellenbosch University, Cape Town, South Africa (Prof J B Nachega PhD, Prof S Seedat PhD, Prof C S Wiysonge PhD); International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b), Dhaka, Bangladesh (A Naheed PhD); Suraj Eye Institute, Nagpur, India (V Nangia MD); School of Medicine, Wayne State University, Detroit, MI, USA (N Nassiri MD); Institute for Global Health Innovations, Duy Tan University, Da Nang, Vietnam (Q L Nguyen MD); Institute For Research, Socio-Economic Development and Communication, Yaoundé, Cameroon (P M Nkamedjie Pete MS); Department of Global Public Health and Primary Care (Prof S E Vollset DrPH), University of Bergen, Bergen, Norway (Prof O F Norheim PhD); Department of Clinical Sciences, Skane University Hospital, Department of Clinical Sciences Lund, Lund, Sweden (Prof B Norrving PhD); Makerere University, Kampala, Uganda (L Nyakarahuka MPH); Center for Research on Population and Health, Faculty of Health Sciences, American University of Beirut, Beirut, Lebanon (Prof C M Obermeyer DSc); Centre for Health Research, Western Sydney University, Sydney, NSW, Australia (F A Ogbo MPH); Department of Preventive Medicine, School of Medicine, Kyung Hee University, Seoul, South Korea (Prof I Oh PhD); Human Sciences Research Council, Durban, South Africa (O Oladimeji MD); University of KwaZulu-Natal, Durban, South Africa (O Oladimeji MD, Prof B Sartorius PhD); Universidad Autonoma de Chile, Talca, Chile (Prof P R Olivares PhD); Center for Healthy Start Initiative, Lagos, Nigeria (B O Olusanya PhD, J O Olusanya MBA); Lira District Local Government, Lira Municipal Council, Uganda (J N Opio MPH); University of Arizona, Tucson, AZ, USA (Prof E Oren PhD); IIS-Fundacion Jimenez Diaz-UAM, Madrid, Spain (Prof A Ortiz PhD); St Luke's International University, Tokyo, Japan (E Ota PhD); JSS Medical College, JSS University, Mysore, India (Prof Mahesh PA DNB); Department of Medical Humanities and Social Medicine, College of Medicine, Kosin University, Busan, South Korea (E Park PhD); Mount Sinai Health System, New York, NY, USA (T Patel MD); Universidad de Cartagena, Cartagena, Colombia (A J Paternina Caicedo MD); Krishan Institute of Medical Sciences, Deemed University, School of Dental Sciences, Karad, India (S T Patil MDS); Department of Community Health Sciences (Prof S B Patten PhD), University of Calgary, Calgary, AB, Canada (J Wang PhD); REQUIMTE/LAQV, Laboratório de Farmacognosia, Departamento de Química, Faculdade de Farmácia, Universidade do Porto, Porto, Portugal (Prof D M Pereira PhD); IRCCS - Istituto di Ricerche Farmacologiche Mario Negri, Bergamo, Italy (M Cortinovis Biotech D, G Giussani Biol D, N Perico MD, Prof G Remuzzi MD); Flinders University, Adelaide, SA, Australia (Prof K Pesudovs PhD); University of the Witwatersrand, Johannesburg, South Africa (Prof M Petzold PhD); Shanghai Jiao Tong University School of Medicine, Shanghai, China (Prof M R Phillips MD); Rollins School of Public Health (E P Simard PhD), Emory University, Atlanta, GA, USA (Prof M R Phillips MD); Durban University of Technology, Durban, South Africa (J D Pillay PhD); Exposure Assessment and Environmental Health Indicators (D Plass DrPH), German Environment Agency, Berlin, Germany (M Tobollik MPH); Department of Public Health, Erasmus University Medical Center, Rotterdam, Netherlands (S Polinder PhD); University of Newcastle, Callaghan, NSW, Australia (Prof C D Pond PhD); Brigham Young University, Provo, UT, USA (Prof C A Pope PhD); The Fred Hollows Foundation, Sydney, NSW, Australia (N M Prasad DO); Centre for Eye Research Australia, Melbourne, VIC, Australia (N M Prasad DO); Department of Community Medicine, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran (M Qorbani PhD); A T Still University, Kirksville, MO, USA (A Radfar MD); Contech School of Public Health, Lahore, Pakistan (A Rafay MS, Prof S M Rana PhD); Research and Evaluation Division, BRAC, Dhaka, Bangladesh (M Rahman PhD); Hamad Medical Corporation, Doha, Qatar (S U Rahman FCPS); Society for Health and Demographic Surveillance, Suri, India (R K Rai MPH); ERAWEB Program, University for Health Sciences, Medical Informatics and Technology, Hall in Tirol, Austria (S Rajsic MD); University of Missouri, Columbia, MO, USA (M Raju PhD); Contech International Health Consultants, Lahore, Pakistan (Prof S M Rana PhD); University of Michigan Health Systems, Ann Arbor, MI, USA (K Ranganathan MD); Walden University, Minneapolis, MN, USA (Prof A H Refaat PhD); Suez Canal University, Ismailia, Egypt (Prof A H Refaat PhD); Montefiore Medical Center, Bronx, NY, USA (C D Rehm PhD); Centre for Addiction and Mental Health, Toronto, ON, Canada (Prof J Rehm PhD); Azienda Ospedaliera Papa Giovanni XXIII, Bergamo, Italy (Prof G Remuzzi MD); Department of Biomedical and Clinical Sciences L Sacco, University of Milan, Milan, Italy (Prof G Remuzzi MD); Hospital das Clinicas da Universidade Federal de Minas Gerais, Belo Horizonte, Brazil (Prof A L Ribeiro MD); School of Psychology, University of Lincoln, Lincoln, UK (Prof A Rodriguez PhD); (ISGlobal) Instituto de Salud Global de Barcelona, Barcelona, Spain (D Rojas-Rueda PhD); Golestan Research Center of Gastroenterology and Hepatology, Golestan University of Medical Sciences, Gorgan, Iran (G Roshandel PhD); Institute of Epidemiology and Medical Biometry, Ulm University, Ulm, Germany (Prof D Rothenbacher MD); All India Institute of Medical Sciences, New Delhi, India (A Roy DM, M Satpathy PhD, Prof N Tandon PhD); Development Research and Projects Center, Abuja, Nigeria (M M Saleh MPH); Marshall University J Edwards School of Medicine, Huntington, WV, USA (J R Sanabria MD); Institut d'Investigacio Biomedica de Bellvitge (IDIBELL), L’Hospitalet de Llebregat, Spain (L Sanchez-Riera PhD); Case Western Reserve University, Cleveland, OH, USA (J R Sanabria MD); IIS-Fundacion Jimenez Diaz, Madrid, Spain (M D Sanchez-Niño PhD); Universidad Ciencias Aplicadas y Ambientales, Bogotá, Colombia (R Sarmiento-Suarez MPH); Marshall University, Huntington, WV, USA (M Sawhney PhD); Global Perspective Studies Unit, Food and Agriculture Organization, Rome, Italy (J Schmidhuber PhD); Federal University of Santa Catarina, Florianópolis, Brazil (I J C Schneider PhD, D A S Silva PhD); Institute of Health Care and Social Sciences, FOM University, Essen, Germany (B Schöttker MPH); Hypertension in Africa Research Team (HART), North-West University, Potchefstroom, South Africa (Prof A E Schutte PhD); Alcohol, Tobacco & Other Drug Research Unit (Prof C D Parry PhD), South African Medical Research Council, Potchefstroom, South Africa (Prof A E Schutte PhD); Department of Public Health, An-Najah University, Nablus, Palestine (A Shaheen PhD); Tufts Medical Center, Boston, MA, USA (S Shahraz PhD); Independent Consultant, Karachi, Pakistan (M A Shaikh MD); Indian Institute of Technology Ropar, Rupnagar, India (R Sharma MA); Research Institute at Nationwide Children's Hospital, Columbus, OH, USA (J Shen PhD); National Institute of Infectious Diseases, Tokyo, Japan (M Shigematsu PhD); Sandia National Laboratories, Albuquerque, NM, USA (M Shigematsu PhD); Department of Public Health Science, Graduate School (Prof M Shin PhD), Department of Preventive Medicine, College of Medicine (S Yoon PhD), Korea University, Seoul, South Korea; Washington State University, Spokane, WA, USA (K Shishani PhD); Faculty of Health and Life Sciences, Northumbria University, Newcastle upon Tyne, UK (I Shiue PhD); Reykjavik University, Reykjavik, Iceland (I D Sigfusdottir PhD); Brasília University, Brasília, Brazil (D G A Silveira MD); Feinberg School of Medicine (J I Silverberg MD), Department of Preventive Medicine (Y Yano MD), Northwestern University, Chicago, IL, USA; Institute for Human Development, New Delhi, India (P K Singh PhD); Dartmouth College, Hanover, NH, USA (S Soneji PhD); Department of Clinical Neurological Sciences, Western University, London, ON, Canada (L A Sposato MD); Department of Community Medicine, International Medical University, Kuala Lumpur, Malaysia (C T Sreeramareddy MD); Attikon University Hospital, Athens, Greece (V Stathopoulou PhD); Institute and Outpatient Clinic for Occupational, Social and Environmental Medicine, University Hospital Munich, Munich, Germany (N Steckling MSc); University of East Anglia, Norwich, UK (Prof N Steel PhD); South African Medical Research Council Unit on Anxiety & Stress Disorders, Cape Town, South Africa (Prof D J Stein PhD); Luxembourg Institute of Health, Strassen, Luxembourg (S Stranges PhD); Alexandra General Hospital of Athens, Athens, Greece (K Stroumpoulis PhD); Centre Hospitalier Public du Cotentin, Cherbourg, France (K Stroumpoulis PhD); Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania (B F Sunguya PhD); Indian Council of Medical Research, New Delhi, India (S Swaminathan MD); Departments of Criminology, Law & Society, Sociology, and Public Health, University of California, Irvine, Irvine, CA, USA (Prof B L Sykes PhD); Department of Medicine, University of Valencia, INCLIVA Health Research Institute and CIBERSAM, Valencia, Spain (Prof R Tabarés-Seisdedos PhD); Ministry of Health, MINSANTE, Yaoundé, Cameroon (R T Talongwa MD); Chaim Sheba Medical Center, Tel Hashomer, Israel (Prof D Tanne MD); Tel Aviv University, Tel Aviv, Israel (Prof D Tanne MD); James Cook University, Cairns, QLD, Australia (B A Tedla BS); Department of Anesthesiology, University of Virginia, Charlottesville, VA, USA (A S Terkawi MD); Outcomes Research Consortium (A S Terkawi MD), Cleveland Clinic, Cleveland, OH, USA (Prof E M Tuzcu MD); School of Public Health, Post Graduate Institute of Medical Education and Research, Chandigarh, India (Prof J Thakur MD); University of Bath, Bath, UK (G Shaddick PhD, M L Thomas MRes); Adaptive Knowledge Management, Victoria, BC, Canada (A J Thomson PhD); WorldFish, Penang, Malaysia (A L Thorne-Lyman ScD); Department of Medicine, School of Clinical Sciences at Monash Health (Prof A G Thrift PhD), Monash University, Melbourne, VIC, Australia; Nelson Institute of Environmental Medicine, School of Medicine, New York University, Tuxedo, NY, USA (Prof G D Thurston ScD); National Center for Child Health and Development, Tokyo, Japan (R Tobe-Gai PhD); Institute of Public Health, Faculty of Health Sciences, Jagiellonian University Medical College, Kraków, Poland (R Topor-Madry PhD); Faculty of Health Sciences, Wroclaw Medical University, Wroclaw, Poland (R Topor-Madry PhD); Aristotle University of Thessaloniki, Thessaloniki, Greece (Prof F Topouzis PhD); Le Bonheur Children's Hospital, Memphis, TN, USA (Prof J A Towbin MD); University of Tennessee Health Science Center, Memphis, TN, USA (Prof J A Towbin MD); St Jude Children's Research Hospital, Memphis, TN, USA (Prof J A Towbin MD); Hanoi Medical University, Hanoi, Vietnam (B X Tran PhD); Department of Population Sciences and Development, Faculty of Economics and Management, University of Kinshasa, Kinshasa, Democratic Republic of the Congo (Z Tsala Dimbuene PhD); African Population and Health Research Center, Nairobi, Kenya (Z Tsala Dimbuene PhD); University Heart Center of Hamburg, Hamburg, Germany (N Tsilimparis PhD); Parc Sanitari Sant Joan de Déu, Fundació Sant Joan de Déu, Universitat de Barcelona, CIBERSAM, Barcelona, Spain (S Tyrovolas PhD); Department of Internal Medicine, Federal Teaching Hospital, Abakaliki, Nigeria (K N Ukwaja MD); Ebonyi State University, Abakaliki, Nigeria (C J Uneke PhD); Warwick Medical School, University of Warwick, Coventry, UK (O A Uthman PhD); Maastricht University Medical Centre, Maastricht, Netherlands (Prof J van Os PhD); UKK Institute for Health Promotion Research, Tampere, Finland (Prof T Vasankari PhD); Raffles Neuroscience Centre, Raffles Hospital, Singapore, Singapore (N Venketasubramanian FRCP); University of Bologna, Bologna, Italy (Prof F S Violante MD); National Institute for Occupational Safety and Health, Washington, DC, USA (G R Wagner MD); Uniformed Services University of Health Sciences, Bethesda, MD, USA (Prof S G Waller MD); National Office for Maternal and Child Health Surveillance, Chengdu, China (Prof Y Wang BS); McGill University, Montreal, QC, Canada (S Weichenthal PhD); Department of Research, Cancer Registry of Norway, Institute of Population-Based Cancer Research, Oslo, Norway (E Weiderpass PhD); Department of Community Medicine, Faculty of Health Sciences, University of Tromsø, The Arctic University of Norway, Tromsø, Norway (E Weiderpass PhD); Genetic Epidemiology Group, Folkhälsan Research Center, Helsinki, Finland (E Weiderpass PhD); Royal Children's Hospital, Melbourne, VIC, Australia (R G Weintraub MBBS); German National Cohort Consortium, Heidelberg, Germany (R Westerman PhD); Western Health, Footscray, VIC, Australia (Prof T Wijeratne MD); National Institute for Health Research Comprehensive Biomedical Research Centre, Guy's & St Thomas' NHS Foundation Trust and King's College London, London, UK (Prof C D Wolfe MD); Royal Cornwall Hospital, Truro, UK (Prof A D Woolf FRCP); St Paul's Hospital, Millennium Medical College, Addis Ababa, Ethiopia (M Wubshet PhD); St John's Medical College and Research Institute, Bangalore, India (Prof D Xavier MD); Department of Neurology, Jinling Hospital, Nanjing University School of Medicine, Nanjing, China (Prof G Xu PhD); Discipline of Public Health Medicine, School of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa (B Yakob PhD); Social Work and Social Administration Department and The Hong Kong Jockey Club Centre for Suicide Research and Prevention, University of Hong Kong, Hong Kong, China (Prof P Yip PhD); Department of Biostatistics, School of Public Health, Kyoto University, Kyoto, Japan (N Yonemoto MPH); Jackson State University, Jackson, MS, USA (Prof M Z Younis DrPH); Department of Epidemiology and Biostatistics, School of Public Health (Prof C Yu PhD), Global Health Institute (Prof C Yu PhD), Wuhan University, Wuhan, China; University Hospital, Setif, Algeria (Prof Z Zaidi PhD); Faculty of Medicine, Mansoura University, Mansoura, Egypt (Prof M E Zaki PhD); National Office of MCH Surveillance of China, Chengdu, China (Prof J Zhu MD); Red Cross War Memorial Children's Hospital, Cape Town, South Africa (L J Zuhlke PhD).
Contributors
Christopher J L Murray, Mohammad H Forouzanfar, and Alan D Lopez prepared the first draft. Christopher J L Murray and Alan D Lopez conceived the study and provided overall guidance. All other authors did one or more of the following: provided data, developed models, reviewed results, initiated modelling infrastructure, or reviewed and contributed to the report.
Declaration of interests
Bruce Bartholow Duncan and Maria Inês Schmidt have received additional funding from the Brazilian Ministry of Health (Process No 25000192049/2014-14). Benjamin O Anderson is supported by the Susan G Komen Leadership Grant Research Project, award number SAC160001. Itamar S Santos reports grants from FAPESP (Brazilian public agency), outside the submitted work. Carl Abelardo T Antonio reports grants, personal fees and non-financial support from Johnson & Johnson (Philippines), Inc, outside the submitted work. Kunihiro Matsushita reports personal fees from Mitsubishi Tanabe Pharma, Kyowa Hakko Kirin, and MSD outside of the submitted work. Rafael Tabarés-Seisdedos and Ferrán Catalá-López are supported in part by grant PROMETEOII/2015/021 from Generalitat Valenciana, and Rafael Tabarés-Seisdedos is supported by the national grant PI14/00894 from ISCIII-FEDER. Walter Mendoza is currently employed by the Peru Country Office of the United Nations Population Fund, an institution which does not necessarily endorse this study. Bradford D Gessner reports grants from Crucell, GSK, Hilleman Labs, Novartis, Pfizer, Merck, and Sanofi Pasteur, outside the submitted work. Ai Koyanagi's work is supported by the Miguel Servet contract financed by the CP13/00150 and PI15/00862 projects, integrated into the National R + D + I and funded by the ISCIII—General Branch Evaluation and Promotion of Health Research—and the European Regional Development Fund (ERDF-FEDER). Aletta E Schutte is funded by the Medical Research Council of South Africa, and the South African Research Chair Initiative by the National Research Foundation. Dariush Mozaffarian reports ad-hoc honoraria or consulting from Boston Heart Diagnostics, Haas Avocado Board, AstraZeneca, GOED, DSM, and Life Sciences Research Organization; and chapter royalties from UpToDate. Amador Goodridge would like to acknowledge funding for me from Sistema Nacional de Investigadores de Panamá-SNI. Donal Bisanzio is supported by Bill & Melinda Gates Foundation (#OPP1068048). Jost B Jonas reports personal fees from Consultant for Mundipharma Co (Cambridge, UK); from patent holder with Biocompatibles UK Ltd (Franham, Surrey, UK) (Title: Treatment of eye diseases using encapsulated cells encoding and secreting neuroprotective factor and / or anti-angiogenic factor; patent number: 20120263794), from patent application with University of Heidelberg (Heidelberg, Germany) (Title: Agents for use in the therapeutic or prophylactic treatment of myopia or hyperopia; Europäische Patentanmeldung 15 000 771.4), outside the submitted work. Rodrigo Sarmiento-Suarez receives institutional support from Universidad de Ciencias Aplicadas y Ambientales, UDCA, Bogotá Colombia. Juan A Rivera reports personal fees from Tres Montes Lucchetti, outside the submitted work. Stefanos Tyrovolas's work is supported by the Foundation for Education and European Culture (IPEP), the Sara Borrell postdoctoral programme (reference no CD15/00019 from the Instituto de Salud Carlos III (ISCIII - Spain) and the Fondos Europeo de Desarrollo Regional (FEDER). Beatriz Paulina Ayala Quintanilla would like to acknowledge the institutional support of PRONABEC (National Program of Scholarship and Educational Loan), provided by the Peruvian Government, while studying for her doctoral course at the Judith Lumley Centre of La Trobe University funded by PRONABEC. Manami Inoue is the beneficiary of a financial contribution from the AXA Research fund as chair holder of the AXA Department of Health and Human Security, Graduate School of Medicine, The University of Tokyo from Nov 1, 2012; the AXA Research Fund has no role in this work. Sarah C Darby would like to acknowledge Cancer Research UK (grant no C8225/A21133). Yogeshwar Kalkonde is a Wellcome Trust/ DBT India Alliance Intermediate Fellow in Public Health. Heidi Stöckl is funded by a British Academy Postdoctoral Fellowship. Tea Lallukka reports funding from The Academy of Finland, grant #287488. Charles D A Wolfe's research was funded/supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy's and St Thomas' NHS Foundation Trust and King's College London. Simon I Hay is funded by a Senior Research Fellowship from the Wellcome Trust (#095066), and grants from the Bill & Melinda Gates Foundation (OPP1119467, OPP1093011, OPP1106023, and OPP1132415).
The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, or the Department of Health. The other authors declare no competing interests.
Contributor Information
GBD 2015 Risk Factors Collaborators:
Mohammad H Forouzanfar, Ashkan Afshin, Lily T Alexander, H Ross Anderson, Zulfiqar A Bhutta, Stan Biryukov, Michael Brauer, Richard Burnett, Kelly Cercy, Fiona J Charlson, Aaron J Cohen, Lalit Dandona, Kara Estep, Alize J Ferrari, Joseph J Frostad, Nancy Fullman, Peter W Gething, William W Godwin, Max Griswold, Simon I Hay, Yohannes Kinfu, Hmwe H Kyu, Heidi J Larson, Xiaofeng Liang, Stephen S Lim, Patrick Y Liu, Alan D Lopez, Rafael Lozano, Laurie Marczak, George A Mensah, Ali H Mokdad, Maziar Moradi-Lakeh, Mohsen Naghavi, Bruce Neal, Marissa B Reitsma, Gregory A Roth, Joshua A Salomon, Patrick J Sur, Theo Vos, Joseph A Wagner, Haidong Wang, Yi Zhao, Maigeng Zhou, Gunn Marit Aasvang, Amanuel Alemu Abajobir, Kalkidan Hassen Abate, Cristiana Abbafati, Kaja M Abbas, Foad Abd-Allah, Abdishakur M Abdulle, Semaw Ferede Abera, Biju Abraham, Laith J Abu-Raddad, Gebre Yitayih Abyu, Akindele Olupelumi Adebiyi, Isaac Akinkunmi Adedeji, Zanfina Ademi, Arsène Kouablan Adou, José C Adsuar, Emilie Elisabet Agardh, Arnav Agarwal, Anurag Agrawal, Aliasghar Ahmad Kiadaliri, Oluremi N Ajala, Tomi F Akinyemiju, Ziyad Al-Aly, Khurshid Alam, Noore K M Alam, Saleh Fahed Aldhahri, Robert William Aldridge, Zewdie Aderaw Alemu, Raghib Ali, Ala'a Alkerwi, François Alla, Peter Allebeck, Ubai Alsharif, Khalid A Altirkawi, Elena Alvarez Martin, Nelson Alvis-Guzman, Azmeraw T Amare, Alemayehu Amberbir, Adeladza Kofi Amegah, Heresh Amini, Walid Ammar, Stephen Marc Amrock, Hjalte H Andersen, Benjamin O Anderson, Carl Abelardo T Antonio, Palwasha Anwari, Johan Ärnlöv, Al Artaman, Hamid Asayesh, Rana Jawad Asghar, Reza Assadi, Suleman Atique, Euripide Frinel G Arthur Avokpaho, Ashish Awasthi, Beatriz Paulina Ayala Quintanilla, Peter Azzopardi, Umar Bacha, Alaa Badawi, Maria C Bahit, Kalpana Balakrishnan, Aleksandra Barac, Ryan M Barber, Suzanne L Barker-Collo, Till Bärnighausen, Simon Barquera, Lars Barregard, Lope H Barrero, Sanjay Basu, Carolina Batis, Shahrzad Bazargan-Hejazi, Justin Beardsley, Neeraj Bedi, Ettore Beghi, Brent Bell, Michelle L Bell, Aminu K Bello, Derrick A Bennett, Isabela M Bensenor, Adugnaw Berhane, Eduardo Bernabé, Balem Demtsu Betsu, Addisu Shunu Beyene, Neeraj Bhala, Anil Bhansali, Samir Bhatt, Sibhatu Biadgilign, Boris Bikbov, Donal Bisanzio, Espen Bjertness, Jed D Blore, Rohan Borschmann, Soufiane Boufous, Rupert R A Bourne, Michael Brainin, Alexandra Brazinova, Nicholas J K Breitborde, Hermann Brenner, David M Broday, Traolach S Brugha, Bert Brunekreef, Zahid A Butt, Leah E Cahill, Bianca Calabria, Ismael Ricardo Campos-Nonato, Rosario Cárdenas, David O Carpenter, Juan Jesus Carrero, Daniel C Casey, Carlos A Castañeda-Orjuela, Jacqueline Castillo Rivas, Ruben Estanislao Castro, Ferrán Catalá-López, Jung-Chen Chang, Peggy Pei-Chia Chiang, Mirriam Chibalabala, Odgerel Chimed-Ochir, Vesper Hichilombwe Chisumpa, Abdulaal A Chitheer, Jee-Young Jasmine Choi, Hanne Christensen, Devasahayam Jesudas Christopher, Liliana G Ciobanu, Matthew M Coates, Samantha M Colquhoun, Alejandra G Contreras Manzano, Leslie Trumbull Cooper, Kimberly Cooperrider, Leslie Cornaby, Monica Cortinovis, John A Crump, Lucia Cuevas-Nasu, Albertino Damasceno, Rakhi Dandona, Sarah C Darby, Paul I Dargan, José das Neves, Adrian C Davis, Kairat Davletov, E Filipa de Castro, Vanessa De la Cruz-Góngora, Diego De Leo, Louisa Degenhardt, Liana C Del Gobbo, Borja del Pozo-Cruz, Robert P Dellavalle, Amare Deribew, Don C Des Jarlais, Samath D Dharmaratne, Preet K Dhillon, Cesar Diaz-Torné, Daniel Dicker, Eric L Ding, E Ray Dorsey, Kerrie E Doyle, Tim R Driscoll, Leilei Duan, Manisha Dubey, Bruce Bartholow Duncan, Iqbal Elyazar, Aman Yesuf Endries, Sergey Petrovich Ermakov, Holly E Erskine, Babak Eshrati, Alireza Esteghamati, Saman Fahimi, Emerito Jose Aquino Faraon, Talha A Farid, Carla Sofia e Sa Farinha, André Faro, Maryam S Farvid, Farshad Farzadfar, Valery L Feigin, Seyed-Mohammad Fereshtehnejad, Jefferson G Fernandes, Florian Fischer, Joseph R A Fitchett, Tom Fleming, Nataliya Foigt, Kyle Foreman, F Gerry R Fowkes, Richard C Franklin, Thomas Fürst, Neal D Futran, Emmanuela Gakidou, Alberto L Garcia-Basteiro, Tsegaye Tewelde Gebrehiwot, Amanuel Tesfay Gebremedhin, Johanna M Geleijnse, Bradford D Gessner, Ababi Zergaw Giref, Maurice Giroud, Melkamu Dedefo Gishu, Giorgia Giussani, Shifalika Goenka, Mari Carmen Gomez-Cabrera, Hector Gomez-Dantes, Philimon Gona, Amador Goodridge, Sameer Vali Gopalani, Carolyn C Gotay, Atsushi Goto, Hebe N Gouda, Harish Chander Gugnani, Francis Guillemin, Yuming Guo, Rahul Gupta, Rajeev Gupta, Reyna A Gutiérrez, Juanita A Haagsma, Nima Hafezi-Nejad, Demewoz Haile, Gessessew Bugssa Hailu, Yara A Halasa, Randah Ribhi Hamadeh, Samer Hamidi, Alexis J Handal, Graeme J Hankey, Yuantao Hao, Hilda L Harb, Sivadasanpillai Harikrishnan, Josep Maria Haro, Mohammad Sadegh Hassanvand, Tahir Ahmed Hassen, Rasmus Havmoeller, Ileana Beatriz Heredia-Pi, Norberto Francisco Hernández-Llanes, Pouria Heydarpour, Hans W Hoek, Howard J Hoffman, Masako Horino, Nobuyuki Horita, H Dean Hosgood, Damian G Hoy, Mohamed Hsairi, Aung Soe Htet, Guoqing Hu, John J Huang, Abdullatif Husseini, Sally J Hutchings, Inge Huybrechts, Kim Moesgaard Iburg, Bulat T Idrisov, Bogdan Vasile Ileanu, Manami Inoue, Troy A Jacobs, Kathryn H Jacobsen, Nader Jahanmehr, Mihajlo B Jakovljevic, Henrica A F M Jansen, Simerjot K Jassal, Mehdi Javanbakht, Sudha P Jayaraman, Achala Upendra Jayatilleke, Sun Ha Jee, Panniyammakal Jeemon, Vivekanand Jha, Ying Jiang, Tariku Jibat, Ye Jin, Catherine O Johnson, Jost B Jonas, Zubair Kabir, Yogeshwar Kalkonde, Ritul Kamal, Haidong Kan, André Karch, Corine Kakizi Karema, Chante Karimkhani, Amir Kasaeian, Anil Kaul, Norito Kawakami, Dhruv S Kazi, Peter Njenga Keiyoro, Laura Kemmer, Andrew Haddon Kemp, Andre Pascal Kengne, Andre Keren, Chandrasekharan Nair Kesavachandran, Yousef Saleh Khader, Abdur Rahman Khan, Ejaz Ahmad Khan, Gulfaraz Khan, Young-Ho Khang, Shahab Khatibzadeh, Sahil Khera, Tawfik Ahmed Muthafer Khoja, Jagdish Khubchandani, Christian Kieling, Cho-il Kim, Daniel Kim, Ruth W Kimokoti, Niranjan Kissoon, Miia Kivipelto, Luke D Knibbs, Yoshihiro Kokubo, Jacek A Kopec, Parvaiz A Koul, Ai Koyanagi, Michael Kravchenko, Hans Kromhout, Hans Krueger, Tiffany Ku, Barthelemy Kuate Defo, Ricardo S Kuchenbecker, Burcu Kucuk Bicer, Ernst J Kuipers, G Anil Kumar, Gene F Kwan, Dharmesh Kumar Lal, Ratilal Lalloo, Tea Lallukka, Qing Lan, Anders Larsson, Asma Abdul Latif, Alicia Elena Beatriz Lawrynowicz, Janet L Leasher, James Leigh, Janni Leung, Miriam Levi, Xiaohong Li, Yichong Li, Juan Liang, Shiwei Liu, Belinda K Lloyd, Giancarlo Logroscino, Paulo A Lotufo, Raimundas Lunevicius, Michael MacIntyre, Mahdi Mahdavi, Marek Majdan, Azeem Majeed, Reza Malekzadeh, Deborah Carvalho Malta, Wondimu Ayele Ayele Manamo, Chabila C Mapoma, Wagner Marcenes, Randall V Martin, Jose Martinez-Raga, Felix Masiye, Kunihiro Matsushita, Richard Matzopoulos, Bongani M Mayosi, John J McGrath, Martin McKee, Peter A Meaney, Catalina Medina, Alem Mehari, Fabiola Mejia-Rodriguez, Alemayehu B Mekonnen, Yohannes Adama Melaku, Ziad A Memish, Walter Mendoza, Gert B M Mensink, Atte Meretoja, Tuomo J Meretoja, Yonatan Moges Mesfin, Francis Apolinary Mhimbira, Anoushka Millear, Ted R Miller, Edward J Mills, Mojde Mirarefin, Awoke Misganaw, Charles N Mock, Alireza Mohammadi, Shafiu Mohammed, Glen Liddell D Mola, Lorenzo Monasta, Julio Cesar Montañez Hernandez, Marcella Montico, Lidia Morawska, Rintaro Mori, Dariush Mozaffarian, Ulrich O Mueller, Erin Mullany, John Everett Mumford, Gudlavalleti Venkata Satyanarayana Murthy, Jean B Nachega, Aliya Naheed, Vinay Nangia, Nariman Nassiri, John N Newton, Marie Ng, Quyen Le Nguyen, Muhammad Imran Nisar, Patrick Martial Nkamedjie Pete, Ole F Norheim, Rosana E Norman, Bo Norrving, Luke Nyakarahuka, Carla Makhlouf Obermeyer, Felix Akpojene Ogbo, In-Hwan Oh, Olanrewaju Oladimeji, Pedro R Olivares, Helen Olsen, Bolajoko Olubukunola Olusanya, Jacob Olusegun Olusanya, John Nelson Opio, Eyal Oren, Ricardo Orozco, Alberto Ortiz, Erika Ota, Mahesh PA, Adrian Pana, Eun-Kee Park, Charles D Parry, Mahboubeh Parsaeian, Tejas Patel, Angel J Paternina Caicedo, Snehal T Patil, Scott B Patten, George C Patton, Neil Pearce, David M Pereira, Norberto Perico, Konrad Pesudovs, Max Petzold, Michael Robert Phillips, Frédéric B Piel, Julian David Pillay, Dietrich Plass, Suzanne Polinder, Constance D Pond, C Arden Pope, Daniel Pope, Svetlana Popova, Richie G Poulton, Farshad Pourmalek, Noela M Prasad, Mostafa Qorbani, Rynaz H S Rabiee, Amir Radfar, Anwar Rafay, Vafa Rahimi-Movaghar, Mahfuzar Rahman, Mohammad Hifz Ur Rahman, Sajjad Ur Rahman, Rajesh Kumar Rai, Sasa Rajsic, Murugesan Raju, Usha Ram, Saleem M Rana, Kavitha Ranganathan, Puja Rao, Christian Aspacia Razo García, Amany H Refaat, Colin D Rehm, Jürgen Rehm, Nikolas Reinig, Giuseppe Remuzzi, Serge Resnikoff, Antonio L Ribeiro, Juan A Rivera, Hirbo Shore Roba, Alina Rodriguez, Sonia Rodriguez-Ramirez, David Rojas-Rueda, Yesenia Roman, Luca Ronfani, Gholamreza Roshandel, Dietrich Rothenbacher, Ambuj Roy, Muhammad Muhammad Saleh, Juan R Sanabria, Lidia Sanchez-Riera, Maria Dolores Sanchez-Niño, Tania G Sánchez-Pimienta, Logan Sandar, Damian F Santomauro, Itamar S Santos, Rodrigo Sarmiento-Suarez, Benn Sartorius, Maheswar Satpathy, Miloje Savic, Monika Sawhney, Josef Schmidhuber, Maria Inês Schmidt, Ione J C Schneider, Ben Schöttker, Aletta E Schutte, David C Schwebel, James G Scott, Soraya Seedat, Sadaf G Sepanlou, Edson E Servan-Mori, Gavin Shaddick, Amira Shaheen, Saeid Shahraz, Masood Ali Shaikh, Teresa Shamah Levy, Rajesh Sharma, Jun She, Sara Sheikhbahaei, Jiabin Shen, Kevin N Sheth, Peilin Shi, Kenji Shibuya, Mika Shigematsu, Min-Jeong Shin, Rahman Shiri, Kawkab Shishani, Ivy Shiue, Mark G Shrime, Inga Dora Sigfusdottir, Diego Augusto Santos Silva, Dayane Gabriele Alves Silveira, Jonathan I Silverberg, Edgar P Simard, Shireen Sindi, Abhishek Singh, Jasvinder A Singh, Prashant Kumar Singh, Erica Leigh Slepak, Michael Soljak, Samir Soneji, Reed J D Sorensen, Luciano A Sposato, Chandrashekhar T Sreeramareddy, Vasiliki Stathopoulou, Nadine Steckling, Nicholas Steel, Dan J Stein, Murray B Stein, Heidi Stöckl, Saverio Stranges, Konstantinos Stroumpoulis, Bruno F Sunguya, Soumya Swaminathan, Bryan L Sykes, Cassandra E I Szoeke, Rafael Tabarés-Seisdedos, Ken Takahashi, Roberto Tchio Talongwa, Nikhil Tandon, David Tanne, Mohammad Tavakkoli, Belaynew Wasie Taye, Hugh R Taylor, Bemnet Amare Tedla, Worku Mekonnen Tefera, Teketo Kassaw Tegegne, Dejen Yemane Tekle, Abdullah Sulieman Terkawi, J S Thakur, Bernadette A Thomas, Matthew Lloyd Thomas, Alan J Thomson, Andrew L Thorne-Lyman, Amanda G Thrift, George D Thurston, Taavi Tillmann, Ruoyan Tobe-Gai, Myriam Tobollik, Roman Topor-Madry, Fotis Topouzis, Jeffrey Allen Towbin, Bach Xuan Tran, Zacharie Tsala Dimbuene, Nikolaos Tsilimparis, Abera Kenay Tura, Emin Murat Tuzcu, Stefanos Tyrovolas, Kingsley N Ukwaja, Eduardo A Undurraga, Chigozie Jesse Uneke, Olalekan A Uthman, Aaron van Donkelaar, Jim van Os, Yuri Y Varakin, Tommi Vasankari, J Lennert Veerman, Narayanaswamy Venketasubramanian, Francesco S Violante, Stein Emil Vollset, Gregory R Wagner, Stephen G Waller, Jian Li Wang, Linhong Wang, Yanping Wang, Scott Weichenthal, Elisabete Weiderpass, Robert G Weintraub, Andrea Werdecker, Ronny Westerman, Harvey A Whiteford, Tissa Wijeratne, Charles Shey Wiysonge, Charles D A Wolfe, Sungho Won, Anthony D Woolf, Mamo Wubshet, Denis Xavier, Gelin Xu, Ajit Kumar Yadav, Bereket Yakob, Ayalnesh Zemene Yalew, Yuichiro Yano, Mehdi Yaseri, Pengpeng Ye, Paul Yip, Naohiro Yonemoto, Seok-Jun Yoon, Mustafa Z Younis, Chuanhua Yu, Zoubida Zaidi, Maysaa El Sayed Zaki, Jun Zhu, Ben Zipkin, Sanjay Zodpey, Liesl Joanna Zuhlke, and Christopher J L Murray
Supplementary Material
References
- 1.Public Health England . From evidence into action: opportunities to protect and improve the nation's health. Public Health England; London: 2014. [Google Scholar]
- 2.Institute for Health Metrics and Evaluation President Ian Khama: emboldened by evidence to reduce harms of alcohol use in Botswana. http://www.healthdata.org/acting-data/president-ian-khama-emboldened-evidence-reduce-harms-alcohol-use-botswana (accessed July 24, 2016).
- 3.Lim SS, Vos T, Flaxman AD. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.GBD 2013 Risk Factors Collaborators. Forouzanfar MH, Alexander L. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–2323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kellerborg K, Danielsson AK, Allebeck P, Coates MM, Agardh E. Disease burden attributed to alcohol: how methodological advances in the Global Burden of Disease 2013 Study have changed the estimates in Sweden. Scand J Public Health. 2016;44:604–610. doi: 10.1177/1403494816653512. [DOI] [PubMed] [Google Scholar]
- 6.Murray CJ, Richards MA, Newton JN. UK health performance: findings of the Global Burden of Disease Study 2010. Lancet. 2013;381:997–1020. doi: 10.1016/S0140-6736(13)60355-4. [DOI] [PubMed] [Google Scholar]
- 7.Yang G, Wang Y, Zeng Y. Rapid health transition in China, 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987–2015. doi: 10.1016/S0140-6736(13)61097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kivimäki M, Vineis P, Brunner EJ. How can we reduce the global burden of disease? Lancet. 2015;386:2235–2237. doi: 10.1016/S0140-6736(15)00129-4. [DOI] [PubMed] [Google Scholar]
- 9.American Institute for Cancer Research . Food, nutrition, physical activity, and the prevention of cancer: a global perspective. American Institute for Cancer Research; Washington, DC: 2007. [Google Scholar]
- 10.SPRINT Research Group. Wright JT, Williamson JD. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yusuf S, Lonn E, Pais P. Blood-pressure and cholesterol lowering in persons without cardiovascular disease. N Engl J Med. 2016;374:2032–2043. doi: 10.1056/NEJMoa1600177. [DOI] [PubMed] [Google Scholar]
- 12.Boekholdt SM, Hovingh GK, Mora S. Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: a meta-analysis of statin trials. J Am Coll Cardiol. 2014;64:485–494. doi: 10.1016/j.jacc.2014.02.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mente A, O'Donnell M, Rangarajan S. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet. 2016;388:465–475. doi: 10.1016/S0140-6736(16)30467-6. [DOI] [PubMed] [Google Scholar]
- 14.Burnett RT, Pope CA, Ezzati M. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ Health Perspect. 2014;122:397–403. doi: 10.1289/ehp.1307049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ioannidis JP. Implausible results in human nutrition research. BMJ. 2013;347:f6698. doi: 10.1136/bmj.f6698. [DOI] [PubMed] [Google Scholar]
- 16.Murray CJ, Lopez AD. On the comparable quantification of health risks: lessons from the Global Burden of Disease Study. Epidemiol. 1999;10:594–605. [PubMed] [Google Scholar]
- 17.Stevens GA, Alkema L, Black RE. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet. 2016 doi: 10.1016/S0140-6736(16)30388-9. http://dx.doi.org/10.1016/S0140-6736(16)30388-9 published online June 28. [DOI] [PubMed] [Google Scholar]
- 18.Ng M, Freeman MK, Fleming TD. Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. JAMA. 2014;311:183–192. doi: 10.1001/jama.2013.284692. [DOI] [PubMed] [Google Scholar]
- 19.Das Gupta P. Standardization and decomposition of rates: a user's manual. US Bureau of the Census; Washington, DC: 1993. [Google Scholar]
- 20.UNDP . Human Development Report 2015. United Nations Development Programme; New York: 2015. [Google Scholar]
- 21.Popkin BM. The nutrition transition in low-income countries: an emerging crisis. Nutr Rev. 1994;52:285–298. doi: 10.1111/j.1753-4887.1994.tb01460.x. [DOI] [PubMed] [Google Scholar]
- 22.Omran AR. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Mem Fund Q. 1971;49:509–538. [PubMed] [Google Scholar]
- 23.Preston SH. The changing relation between mortality and level of economic development. Popul Stud. 1975;29:231–248. [PubMed] [Google Scholar]
- 24.Vallin J, Meslé F. Convergences and divergences in mortality: a new approach of health transition. Demogr Res. 2004;2:11–44. [Google Scholar]
- 25.Goryakin Y, Suhrcke M. Economic development, urbanization, technological change and overweight: what do we learn from 244 Demographic and Health Surveys? Econ Hum Biol. 2014;14:109–127. doi: 10.1016/j.ehb.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. 2006;84:289–298. doi: 10.1093/ajcn/84.1.289. [DOI] [PubMed] [Google Scholar]
- 27.GBD 2015 Mortality and Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.GBD 2015 Diseases and Injury Incidence and prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1604. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.GBD 2015 Child Mortality Collaborators Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1605–1660. doi: 10.1016/S0140-6736(16)31575-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Granich R, Gupta S, Hersh B. Trends in AIDS deaths, new infections and ART coverage in the top 30 countries with the highest AIDS mortality burden; 1990–2013. PLoS One. 2015;10:e0131353. doi: 10.1371/journal.pone.0131353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.UN Programme on HIV/AIDS . The Gap Report. United Nations programme on HIV/AIDS; Geneva: 2014. [Google Scholar]
- 32.UNDP World AIDS Day: record drop in cost of HIV treatment. Nov 30, 2015. http://www.undp.org/content/undp/en/home/presscenter/articles/2015/11/30/world-aids-day-record-drop-in-cost-of-hiv-treatment.html (accessed July 24, 2016).
- 33.Scandinavian Simvastatin Survival Study Group Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 34.Fihn SD, Gardin JM, Abrams J. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60:e44–164. doi: 10.1016/j.jacc.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 35.Augoustides JG, Ramakrishna H. Recent advances in the management of coronary artery disease: highlights from the literature. J Cardiothorac Vasc Anesth. 2009;23:259–265. doi: 10.1053/j.jvca.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 36.Writing Committee Members. Drozda JP, Ferguson TB. 2015 ACC/AHA Focused Update of Secondary Prevention Lipid Performance Measures: a Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes. 2016;9:68–95. doi: 10.1161/HCQ.0000000000000014. [DOI] [PubMed] [Google Scholar]
- 37.Yancy CW, Jessup M, Bozkurt B. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: an update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2016 doi: 10.1161/CIR.0000000000000435. published online May 20. [DOI] [PubMed] [Google Scholar]
- 38.National Cancer Institute Progress & trends: decreased mortality, increased survival rates. http://www.cancer.gov/about-nci/budget/plan/progress (accessed July 24, 2016).
- 39.Nolte E, McKee M. Measuring the health of nations: analysis of mortality amenable to health care. BMJ. 2003;327:1129. doi: 10.1136/bmj.327.7424.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65:5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 41.Forouzanfar MH, Foreman KJ, Delossantos AM. Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet. 2011;378:1461–1484. doi: 10.1016/S0140-6736(11)61351-2. [DOI] [PubMed] [Google Scholar]
- 42.Anderson BO, Senie RT, Vetto JT, Wong GY, McCormick B, Borgen PI. Improved survival in young women with breast cancer. Ann Surg Oncol. 1995;2:407–415. doi: 10.1007/BF02306373. [DOI] [PubMed] [Google Scholar]
- 43.Murawa P, Murawa D, Adamczyk B, Połom K. Breast cancer: actual methods of treatment and future trends. Rep Pract Oncol Radiother. 2014;19:165–172. doi: 10.1016/j.rpor.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kopp HG, Kuczyk M, Classen J. Advances in the treatment of testicular cancer. Drugs. 2006;66:641–659. doi: 10.2165/00003495-200666050-00005. [DOI] [PubMed] [Google Scholar]
- 45.Arulogun S, Hertzberg M, Gandhi MK. Recent treatment advances in Hodgkin lymphoma: a concise review. Intern Med J. 2016 doi: 10.1111/imj.13051. published online March 1. [DOI] [PubMed] [Google Scholar]
- 46.UNICEF . Progress on sanitation and drinking water. United Nations International Children's Emergency Fund; New York: 2015. [Google Scholar]
- 47.Millennium Project Goals, targets and indicators. http://www.unmillenniumproject.org/goals/gti.htm (accessed July 24, 2016).
- 48.UN . The Millennium Development Goals report 2015. United Nations; Geneva: 2015. [Google Scholar]
- 49.WHO Sanitation. June, 2015. http://www.who.int/mediacentre/factsheets/fs392/en/ (accessed July 24, 2016).
- 50.UN Goal 6: ensure access to water and sanitation for all. http://www.un.org/sustainabledevelopment/water-and-sanitation/ (accessed July 24, 2016).
- 51.International Council for Science . Review of the Sustainable Development Goals: the science perspective. International Council for Science; Paris: 2015. [Google Scholar]
- 52.WHO MPOWER: a policy package to reverse the tobacco epidemic. 2008. http://apps.who.int/iris/handle/10665/43888 (accessed July 24, 2016).
- 53.International Agency for Research on Cancer . Evaluating the effectiveness of smoke-free policies. International Agency for Research on Cancer; Lyon: 2009. [Google Scholar]
- 54.US Department of Health and Human Services . The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General. US Department of Health and Human Services; Atlanta: 2006. [Google Scholar]
- 55.Hopkins DP, Razi S, Leeks KD. Smokefree policies to reduce tobacco use. A systematic review. Am J Prev Med. 2010;38:S275–S289. doi: 10.1016/j.amepre.2009.10.029. [DOI] [PubMed] [Google Scholar]
- 56.Callinan JE, Clarke A, Doherty K, Kelleher C. Legislative smoking bans for reducing secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst Rev. 2010;14 doi: 10.1002/14651858.CD005992.pub2. CD005992. [DOI] [PubMed] [Google Scholar]
- 57.WHO Turkey marks progress in fight against noncommunicable diseases. September, 2012. http://www.who.int/features/2012/ncd_turkey/en/ (accessed July 24, 2016).
- 58.WHO . Global status report on noncommunicable diseases 2010. World Health Organization; Geneva: 2011. [Google Scholar]
- 59.Peto R, Lopez AD, Boreham J, Thun M, Heath C. Mortality from tobacco in developed countries: indirect estimation from national vital statistics. Lancet. 1992;339:1268–1278. doi: 10.1016/0140-6736(92)91600-d. [DOI] [PubMed] [Google Scholar]
- 60.Carter BD, Abnet CC, Feskanich D. Smoking and mortality—beyond established causes. N Engl J Med. 2015;372:631–640. doi: 10.1056/NEJMsa1407211. [DOI] [PubMed] [Google Scholar]
- 61.Subar AF, Thompson FE, Kipnis V. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America's Table Study. Am J Epidemiol. 2001;154:1089–1099. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 62.Willett W. Nutritional epidemiology. Oxford University Press USA; New York: 2013. [Google Scholar]
- 63.National Cancer Institute Effects of measurement error. https://dietassessmentprimer.cancer.gov/concepts/error/error-effects.html (accessed July 24, 2016).
- 64.Blackwell M, Honaker J, King G. A unified approach to measurement error and missing data: overview and applications. Sociol Methods Res. 2015 published online June 30. [Google Scholar]
- 65.Brenner H, Loomis D. Varied forms of bias due to nondifferential error in measuring exposure. Epidemiol. 1994;5:510–517. [PubMed] [Google Scholar]
- 66.Hill RJ, Davies PS. The validity of self-reported energy intake as determined using the doubly labelled water technique. Br J Nutr. 2001;85:415–430. doi: 10.1079/bjn2000281. [DOI] [PubMed] [Google Scholar]
- 67.McLean RM. Measuring population sodium intake: a review of methods. Nutrients. 2014;6:4651–4662. doi: 10.3390/nu6114651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Harvard T.H. Chan School of Public Health. Pooling project of prospective studies of diet and cancer: cohort study participants. https://www.hsph.harvard.edu/pooling-project/cohort-study-participants/ (accessed July 24, 2016).
- 69.Chowdhury R, Warnakula S, Kunutsor S. Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med. 2014;160:398–406. doi: 10.7326/M13-1788. [DOI] [PubMed] [Google Scholar]
- 70.Pimpin L, Wu JH, Haskelberg H, Del Gobbo L, Mozaffarian D. Is butter back? A systematic review and meta-analysis of butter consumption and risk of cardiovascular disease, diabetes, and total mortality. PLoS One. 2016;11:e0158118. doi: 10.1371/journal.pone.0158118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.WHO About 9 voluntary global targets—global monitoring framework for NCDs. http://www.who.int/nmh/ncd-tools/definition-targets/en/ (accessed July 24, 2016).
- 72.US Food and Drug Administration FDA issues draft guidance to food industry for voluntarily reducing sodium in processed and commercially prepared food. June 1, 2016. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm503874.htm (accessed July 24, 2016).
- 73.Lachat C, Otchere S, Roberfroid D. Diet and physical activity for the prevention of noncommunicable diseases in low- and middle-income countries: a systematic policy review. PLoS Med. 2013;10:e1001465. doi: 10.1371/journal.pmed.1001465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Trieu K, Neal B, Hawkes C. Salt reduction initiatives around the world—a systematic review of progress towards the global target. PLoS One. 2015;10:e0130247. doi: 10.1371/journal.pone.0130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bonita R, Magnusson R, Bovet P. Country actions to meet UN commitments on non-communicable diseases: a stepwise approach. Lancet. 2013;381:575–584. doi: 10.1016/S0140-6736(12)61993-X. [DOI] [PubMed] [Google Scholar]
- 76.He FJ, MacGregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis. 2010;52:363–382. doi: 10.1016/j.pcad.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 77.Lonn EM, Bosch J, López-Jaramillo P. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374:2009–2020. doi: 10.1056/NEJMoa1600175. [DOI] [PubMed] [Google Scholar]
- 78.O'Donnell M, Mente A, Rangarajan S. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371:612–623. doi: 10.1056/NEJMoa1311889. [DOI] [PubMed] [Google Scholar]
- 79.Institute of Medicine . Sodium intake in populations: assessment of evidence. The National Academies Press; Washington, DC: 2013. [PubMed] [Google Scholar]
- 80.Trinquart L, Johns DM, Galea S. Why do we think we know what we know? A metaknowledge analysis of the salt controversy. Int J Epidemiol. 2016;45:251–260. doi: 10.1093/ije/dyv184. [DOI] [PubMed] [Google Scholar]
- 81.Cogswell ME, Mugavero K, Bowman BA, Frieden TR. Dietary sodium and cardiovascular disease risk—measurement matters. N Engl J Med. 2016;375:580–586. doi: 10.1056/NEJMsb1607161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Frieden TR. Sodium reduction-saving lives by putting choice into consumers' hands. JAMA. 2016;316:579–580. doi: 10.1001/jama.2016.7992. [DOI] [PubMed] [Google Scholar]
- 83.He FJ, MacGregor GA. Hypertension: salt: flawed research should not divert actions to reduce intake. Nat Rev Nephrol. 2016;12:514–515. doi: 10.1038/nrneph.2016.97. [DOI] [PubMed] [Google Scholar]
- 84.Cook NR, Appel LJ, Whelton PK. Lower levels of sodium intake and reduced cardiovascular risk. Circulation. 2014;129:981–989. doi: 10.1161/CIRCULATIONAHA.113.006032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.WHO . Global action plan for the prevention and control of noncommunicable diseases 2013–2020. World Health Organization; Geneva: 2013. [Google Scholar]
- 86.UN General Assembly Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. http://www.who.int/nmh/events/un_ncd_summit2011/political_declaration_en.pdf (accessed July 24, 2016).
- 87.Afshin A, Penalvo J, Del Gobbo L. CVD prevention through policy: a review of mass media, food/menu labeling, taxation/subsidies, built environment, school procurement, worksite wellness, and marketing standards to improve diet. Curr Cardiol Rep. 2015;17:98. doi: 10.1007/s11886-015-0658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.US Department of Agriculture . Scientific report of the 2015 Dietary Guidelines Advisory Committee. US Department of Agriculture; 2015. [Google Scholar]
- 89.Mann S, Beedie C, Jimenez A. Differential effects of aerobic exercise, resistance training and combined exercise modalities on cholesterol and the lipid profile: review, synthesis and recommendations. Sports Med Auckl Nz. 2014;44:211–221. doi: 10.1007/s40279-013-0110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dowse GK, Gareeboo H, Alberti KG. Changes in population cholesterol concentrations and other cardiovascular risk factor levels after five years of the non-communicable disease intervention programme in Mauritius. Mauritius Non-communicable Disease Study Group. BMJ. 1995;311:1255–1259. doi: 10.1136/bmj.311.7015.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vartiainen E, Laatikainen T, Tapanainen H, Puska P. Changes in Serum cholesterol and diet in North Karelia and all Finland. Glob Heart. 2016;11:179–184. doi: 10.1016/j.gheart.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 92.Singh GM, Danaei G, Farzadfar F. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS One. 2013;8:e65174. doi: 10.1371/journal.pone.0065174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lawes CM, Rodgers A, Bennett DA. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens. 2003;21:707–716. doi: 10.1097/00004872-200304000-00013. [DOI] [PubMed] [Google Scholar]
- 94.Roerecke M, Rehm J. Ischemic heart disease mortality and morbidity rates in former drinkers: a meta-analysis. Am J Epidemiol. 2011;173:245–258. doi: 10.1093/aje/kwq364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Roerecke M, Rehm J. Alcohol consumption, drinking patterns, and ischemic heart disease: a narrative review of meta-analyses and a systematic review and meta-analysis of the impact of heavy drinking occasions on risk for moderate drinkers. BMC Med. 2014;12:182. doi: 10.1186/s12916-014-0182-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fillmore KM, Stockwell T, Chikritzhs T, Bostrom A, Kerr W. Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses. Ann Epidemiol. 2007;17:S16–S23. doi: 10.1016/j.annepidem.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 97.Bergmann MM, Rehm J, Klipstein-Grobusch K. The association of pattern of lifetime alcohol use and cause of death in the European prospective investigation into cancer and nutrition (EPIC) study. Int J Epidemiol. 2013;42:1772–1790. doi: 10.1093/ije/dyt154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Holmes MV, Dale CE, Zuccolo L. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ. 2014;349:g4164. doi: 10.1136/bmj.g4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Stockwell T, Greer A, Fillmore K, Chikritzhs T, Zeisser C. How good is the science? BMJ. 2012;344:e2276. doi: 10.1136/bmj.e2276. [DOI] [PubMed] [Google Scholar]
- 100.Dam MK, Hvidtfeldt UA, Tjønneland A, Overvad K, Grønbæk M, Tolstrup JS. Five year change in alcohol intake and risk of breast cancer and coronary heart disease among postmenopausal women: prospective cohort study. BMJ. 2016;353:i2314. doi: 10.1136/bmj.i2314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Koloverou E, Panagiotakos DB, Pitsavos C. Effects of alcohol consumption and the metabolic syndrome on 10-year incidence of diabetes: the ATTICA study. Diabetes Metab. 2015;41:152–159. doi: 10.1016/j.diabet.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 102.Hange D, Sigurdsson JA, Björkelund C, Sundh V, Bengtsson C. A 32-year longitudinal study of alcohol consumption in Swedish women: reduced risk of myocardial infarction but increased risk of cancer. Scand J Prim Health Care. 2015;33:153–162. doi: 10.3109/02813432.2015.1067515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Li XH, Yu FF, Zhou YH, He J. Association between alcohol consumption and the risk of incident type 2 diabetes: a systematic review and dose-response meta-analysis. Am J Clin Nutr. 2016;103:818–829. doi: 10.3945/ajcn.115.114389. [DOI] [PubMed] [Google Scholar]
- 104.Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006;166:2437–2445. doi: 10.1001/archinte.166.22.2437. [DOI] [PubMed] [Google Scholar]
- 105.Knott C, Bell S, Britton A. Alcohol consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of more than 1·9 million individuals from 38 observational studies. Diabetes Care. 2015;38:1804–1812. doi: 10.2337/dc15-0710. [DOI] [PubMed] [Google Scholar]
- 106.Naimi TS, Stockwell T, Zhao J. Selection biases in observational studies affect associations between ‘moderate’ alcohol consumption and mortality. Addict. 2016 doi: 10.1111/add.13451. published online June 17. [DOI] [PubMed] [Google Scholar]
- 107.Naimi TS, Brown DW, Brewer RD. Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults. Am J Prev Med. 2005;28:369–373. doi: 10.1016/j.amepre.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 108.Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do ‘moderate’ drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality. J Stud Alcohol Drugs. 2016;77:185–198. doi: 10.15288/jsad.2016.77.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Au Yeung SL, Jiang CQ, Cheng KK. Evaluation of moderate alcohol use and cognitive function among men using a Mendelian randomization design in the Guangzhou biobank cohort study. Am J Epidemiol. 2012;175:1021–1028. doi: 10.1093/aje/kwr462. [DOI] [PubMed] [Google Scholar]
- 110.von Hinke Kessler Scholder S, Wehby GL, Lewis S, Zuccolo L. Alcohol exposure in utero and child academic achievement. Econ J. 2014;124:634–667. doi: 10.1111/ecoj.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chen L, Smith GD, Harbord RM, Lewis SJ. Alcohol intake and blood pressure: a systematic review implementing a Mendelian randomization approach. PLoS Med. 2008;5:e52. doi: 10.1371/journal.pmed.0050052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Cobiac L, Vos T, Doran C, Wallace A. Cost-effectiveness of interventions to prevent alcohol-related disease and injury in Australia. Addict. 2009;104:1646–1655. doi: 10.1111/j.1360-0443.2009.02708.x. [DOI] [PubMed] [Google Scholar]
- 113.Elder RW, Lawrence B, Ferguson A. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. Am J Prev Med. 2010;38:217–229. doi: 10.1016/j.amepre.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.O'Donnell A, Anderson P, Newbury-Birch D. The impact of brief alcohol interventions in primary healthcare: a systematic review of reviews. Alcohol Alcohol. 2014;49:66–78. doi: 10.1093/alcalc/agt170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chisholm D, Rehm J, Van Ommeren M, Monteiro M. Reducing the global burden of hazardous alcohol use: a comparative cost-effectiveness analysis. J Stud Alcohol. 2004;65:782–793. doi: 10.15288/jsa.2004.65.782. [DOI] [PubMed] [Google Scholar]
- 116.De Oliveira LH, Giglio N, Ciapponi A. Temporal trends in diarrhea-related hospitalizations and deaths in children under age 5 before and after the introduction of the rotavirus vaccine in four Latin American countries. Vaccine. 2013;31(suppl 3):C99–108. doi: 10.1016/j.vaccine.2013.05.065. [DOI] [PubMed] [Google Scholar]
- 117.Sriplung H, Singkham P, Iamsirithaworn S, Jiraphongsa C, Bilheem S. Success of a cervical cancer screening program: trends in incidence in Songkhla, southern Thailand, 1989–2010, and prediction of future incidences to 2030. Asian Pac J Cancer Prev. 2014;15:10003–10008. doi: 10.7314/apjcp.2014.15.22.10003. [DOI] [PubMed] [Google Scholar]
- 118.Berg J, Björck L, Lappas G, O'Flaherty M, Capewell S, Rosengren A. Continuing decrease in coronary heart disease mortality in Sweden. BMC Cardiovasc Disord. 2014;14:9. doi: 10.1186/1471-2261-14-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kreatsoulas C, Anand SS. The impact of social determinants on cardiovascular disease. Can J Cardiol. 2010;26(suppl C):8C–13C. doi: 10.1016/s0828-282x(10)71075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gakidou E, Cowling K, Lozano R, Murray CJ. Increased educational attainment and its effect on child mortality in 175 countries between 1970 and 2009: a systematic analysis. Lancet. 2010;376:959–974. doi: 10.1016/S0140-6736(10)61257-3. [DOI] [PubMed] [Google Scholar]
- 121.Sassi F, Belloni A, Capobianco C. The role of fiscal policies in health promotion. OECD Working Papers. 2013;66:1–50. [Google Scholar]
- 122.Sassi F. Obesity and the economics of prevention. Organisation for Economic Co-operation and Development Publishing; Paris: 2010. [Google Scholar]
- 123.Dobbs R, Sawers C, Thompson F. Overcoming obesity: an initial economic analysis. McKinsey Global Institute; London: 2014. [Google Scholar]
- 124.Sheehan NA, Didelez V, Burton PR, Tobin MD. Mendelian randomisation and causal inference in observational epidemiology. PLoS Med. 2008;5:e177. doi: 10.1371/journal.pmed.0050177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr. 2013;98:1084–1902. doi: 10.3945/ajcn.113.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2013;346:e7492. doi: 10.1136/bmj.e7492. [DOI] [PubMed] [Google Scholar]
- 127.Mozaffarian D, Fahimi S, Singh GM. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–634. doi: 10.1056/NEJMoa1304127. [DOI] [PubMed] [Google Scholar]
- 128.Navas-Acien A, Schwartz BS, Rothenberg SJ, Hu H, Silbergeld EK, Guallar E. Bone lead levels and blood pressure endpoints: a meta-analysis. Epidemiol. 2008;19:496–504. doi: 10.1097/EDE.0b013e31816a2400. [DOI] [PubMed] [Google Scholar]
- 129.Pope CA, Burnett RT, Turner MC. Lung cancer and cardiovascular disease mortality associated with ambient air pollution and cigarette smoke: shape of the exposure-response relationships. Environ Health Perspect. 2011;119:1616–1621. doi: 10.1289/ehp.1103639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Pope CA, Burnett RT, Krewski D. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: shape of the exposure-response relationship. Circulation. 2009;120:941–948. doi: 10.1161/CIRCULATIONAHA.109.857888. [DOI] [PubMed] [Google Scholar]
- 131.Lippmann M, Chen LC, Gordon T, Ito K, Thurston GD. National Particle Component Toxicity (NPACT) Initiative: integrated epidemiologic and toxicologic studies of the health effects of particulate matter components. Res Rep Health Eff Inst. 2013;177:5–13. [PubMed] [Google Scholar]
- 132.Stanek LW, Sacks JD, Dutton SJ, Dubois JJ. Attributing health effects to apportioned components and sources of particulate matter: an evaluation of collective results. Atmos Environ. 2011;45:5655–5663. [Google Scholar]
- 133.GBD 2013 Mortality and Causes of Death Collaborators Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Global Burden of Disease Study 2013 Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mehta N, Preston S. Are major behavioral and sociodemographic risk factors for mortality additive or multiplicative in their effects? Soc Sci Med. 2016;154:93–99. doi: 10.1016/j.socscimed.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lim SS, Carnahan E, Nelson EC. Validation of a new predictive risk model: measuring the impact of the major modifiable risks of death for patients and populations. Popul Health Metr. 2015;13:27. doi: 10.1186/s12963-015-0059-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Bhaskaran K, Douglas I, Forbes H, dos-Santos-Silva I, Leon DA, Smeeth L. Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5·24 million UK adults. Lancet. 2014;384:755–765. doi: 10.1016/S0140-6736(14)60892-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–578. doi: 10.1016/S0140-6736(08)60269-X. [DOI] [PubMed] [Google Scholar]
- 139.Chafe ZA, Brauer M, Klimont Z. Household cooking with solid fuels contributes to ambient PM2·5 air pollution and the burden of disease. Environ Health Perspect. 2014;122:1314–1320. doi: 10.1289/ehp.1206340. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.