Highlights
-
•
Dengue induced Hemophagocytic lymphohistiocytosis (HLH), is a serious entity and can adversely affect the course of the infection.
-
•
HLH is a potentially life threatening disorder and early diagnosis and management is crucial for successful outcome.
-
•
A disproportionately high ferritin level should trigger investigations for HLH.
Keywords: Bicytopenia, Dengue, Hemophagocytic lymphohistiocytosis (HLH), Infection, Intravenous immunoglobulin G
Abstract
Dengue, transmitted by the mosquito Aedes aegypti affects millions of people worldwide every year. Dengue induced hemophagocytic lymphohistiocytosis (HLH) is a serious condition and may prove fatal if not detected early and treated appropriately. Diagnosis of HLH is challenging and usually missed as clinical and laboratory findings are nonspecific. Moreover, the pathophysiology of the systemic inflammatory response syndrome and/or sepsis is remarkably similar to HLH. Secondary HLH following infection by the dengue virus is now being increasingly recognized as a cause of severe form of the disease. We report a case of dengue associated HLH in an otherwise healthy person who deteriorated during the course of hospitalization. A disproportionately high ferritin level and persistent bicytopenia prompted investigations for HLH. Diagnosis of dengue fever with virus-associated hemophagocytic syndrome was established according to the diagnostic criteria laid down by the Histiocyte Society. We discuss the diagnosis and management of this complex case and try to generate awareness about dengue induced HLH as one of the possible causes for severe manifestations of this infection
Introduction
Hemophagocytic lymphohistiocytosis (HLH), a potentially fatal condition that is often under recognised contributing to its high mortality and morbidity. Early recognition is crucial for any efforts at curative therapy. Although HLH is now being increasingly detected in clinical practice due to improved understanding on the part of physicians, pathologists and microbiologists; still much work remains to raise awareness, explore treatment options and improve outcome of this complex condition. We report a case of dengue associated HLH who had a successful outcome following timely diagnosis and appropriate intervention.
Case report
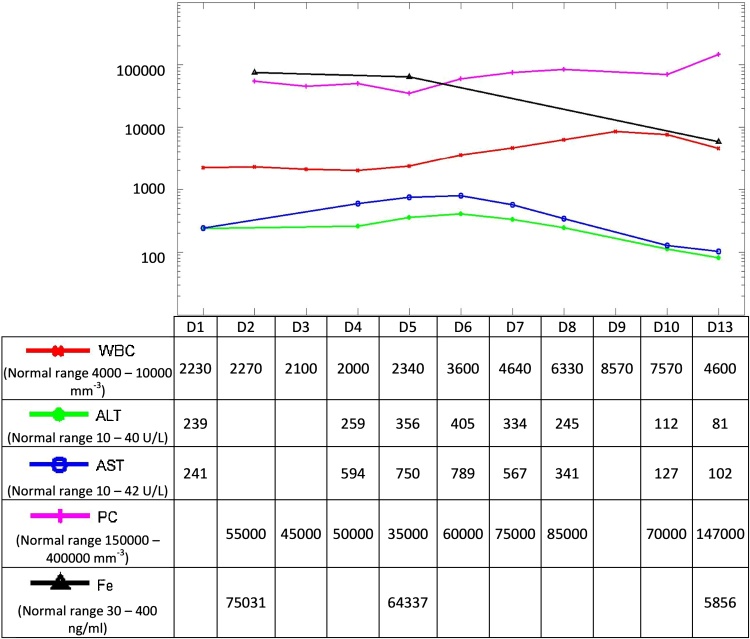
A 65 year old otherwise fit and well gentleman from eastern region of India presented in October 2015 with fever for three days and vomiting and pain abdomen for a day. Significant findings on examination were fever of 38.3 °C, epigastric and right hypochondriac tenderness and dullness over lung bases. Routine laboratory parameters revealed hemoglobin 10.9gm/dl, Leukopenia with presence of reactive Lymphocytes (WBC count 2230 mm−3; reference value [RV]:4000–10000 mm−3) and low platelet count (55000 mm−3; RV: 150000–400000 mm−3).There were significant derangements of the biochemical parameters as well. Liver enzymes were elevated, AST 239 U/L (RV: 10–42 U/L) and ALT 241U/L (RV: 10–40 U/L). Serum amylase and lipase levels were high 305 U/L; (RV: 25–125 U/L) and 465U/L; (RV: 22–51 U/L) respectively. Serum ferritin level done at day 2 of admission was 75031 ng/ml (RV: 30–400 ng/ml) (Fig. 1).Serum procalcitonin level at admission was 2 ng/dl (RV: <0.5 ng/ml) which was indicative of bacterial sepsis. Serum triglyceride and plasma fibrinogen levels were within normal range. The platelet count dropped to 45,000 mm−3on day three of admission with coffee ground vomiting. The patient subsequently received two units of single donor platelet. Ultrasound imaging showed mild splenomegaly (measured length13 cm), minimal free fluid in abdomen and edematous pancreas and bilateral pleural effusion. Chest X-ray showed pneumonitic changes in both lung fields.
Fig. 1.
Trend of laboratory results. D: Day of illness; WBC: Total white blood count (mm−3); PC: Platelet count (mm−3): AST: aspartate transaminase (IU/L); ALT: alanine transaminase (IU/L); Fe: ferritin (mg/L). All units are converted to Log10scale in the figure.
Work up of locally common infectious causes were done including urine and blood cultures, Epstein Barr Virus (EBV) Viral Capsid Antigen IgM, Cytomegalovirus (CMV) IgM, Malaria smear and antigen detection, Dengue NS1 antigen detection, Leptospira IgM serology, Weil Felix screening test for rickettsial infections. The Dengue NS1 antigen test was positive (Panbio Dengue Early Elisa, Standard Diagnostics, Korea) while all other tests were negative including cultures. A diagnosis of dengue fever complicated by pancreatitis and hepatitis with associated chest infection was made. The patient was managed in high dependency unit.
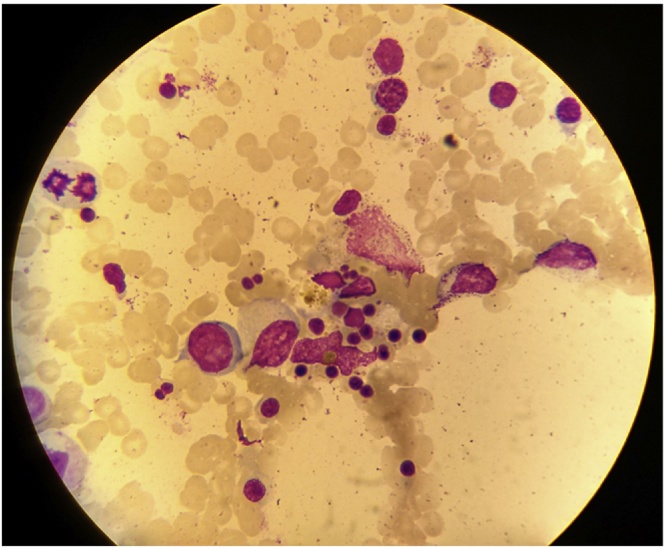
Despite supportive therapy he remained unwell with spikes of temperature, worsening abdominal pain and progressive bi-basal crepitations. Laboratory investigations showed persistent leukopenia, thrombocytopenia and rising aminotransferases. A bone marrow aspiration and trephine biopsy was done for further evaluation on day 4 of admission triggered by high ferritin and bicytopenia. Bone marrow study showed normocellular reactive marrow with evidence of macrophage activation and hemophagocytosis (Fig. 2). A dengue serology on day 6 of fever was positive for IgM antibodies by capture ELISA (Index 5.71, RV: Index < 1.1; Panbio Dengue IgM Capture Elisa, Standard Diagnostics, Korea) but negative for IgG antibodies establishing the diagnosis of primary dengue infection with secondary HLH. Following the diagnosis of HLH, the patient was given intravenous immunoglobulin (400 mg/kg/day for 5 days) starting on day 5 of hospitalisation in view of associated pancreatitis and chest infection. The patient continued to be febrile (T max 38.3 °C) till day 8 of admission. He improved over the next few days, became afebrile and was discharged after 13 days in the hospital. At the time of discharge his blood counts and biochemical parameters had recovered to almost normal levels.
Fig. 2.
Bone marrow aspirate showing macrophage with marked hemophagocytic activity.
Discussion
HLH is a disease with major therapeutic and diagnostic difficulties. The diagnosis HLH was based on five criteria (fever, splenomegaly, bicytopenia, hypertriglyceridemia and/or hypofibrinogenemia, and hemophagocytosis) [1]. In 2004 three additional criteria were introduced by the Histiocyte Society; low or absent NK-cell-activity, hyperferritinemia, and high-soluble interleukin-2-receptor levels [2]. Five of these eight criteria must be fulfilled for a diagnosis of HLH. The NK cell activity and soluble IL2 receptor quantitation tests are not done in routine clinical practice since they require sending samples out to specialized centers and hence usefulness of these tests in day to day practice is limited. This patient fulfilled five of the eight criteria — splenomegaly, bicytopenia (decr fever, splenomegaly, bicytopenia (decrease in platelets and leucocytes) hyperferritinemia and presence of haemophagocytes in the bone marrow and accordingly was diagnosed as a case of secondary HLH.
HLH may be primary (familial) and secondary. In recent years there is an increased incidence of this disease probably because of better diagnostic abilities of clinicians. Secondary HLH develop due over activation of immune system. Secondary HLH has been associated with a variety of viral, bacterial, fungal and parasitic infections as well as collagen vascular diseases and malignancies particularly T-cell lymphomas [3]. The term reactive HLH has been suggested when HLH is associated with an identifiable infectious or non-infectious etiology to distinguish it from the familial form. Infection has been found to be associated with HLH in half of all reported cases [4].
Phagocytosis of blood cells and their precursors is a hallmark of hemophagocytic syndromes. Hemophagocytosis is achieved mostly by monocytes and macrophages. Excessive activation of monocytes in HLH is due to stimulation by high levels of activating cytokines. It has been recognized that high levels of cytokines like interferon-γ, soluble interleukin-2 receptor, tumor necrosis factor (TNF-α), interleukin-1 and Interleukin-6 by T helper cells result in stimulation of macrophages leading to the cascade of events [3].
About one third of secondary HLH are triggered by viral infections. Several viral infections have been reported to trigger HLH, EBV infection being the most notorious.EBV triggered HLH has been widely reported and studied.Other viruses which are known to trigger HLH include Herpesviridae, Poxviridae, Flaviviridae, Orthomyxoviridae, Paramyxoviridae and Retroviridae [5].
Dengue is endemic in more than 100 countries in Southeast Asia, Latin America, Western Pacific, Africa and Eastern Mediterranean regions.It is estimated that 390 million people suffer from dengue infections every year of which 96 million have clinical manifestation [6]. Dengue outbreaks occur in Eastern India every 3 to 4 years [7]. Given the fact that large numbers of people are affected by dengue every year, it is likely that number of dengue triggered HLH are also high and the spate of recent reports describing dengue induced HLH are testimony to this fact [8], [9], [10], [11], [12]. A mild disease in majority of cases, less than 2% of dengue patients present with severe manifestations, dengue haemorrhagic fever (DHF) and dengue shock syndrome (DSS), both conditions are associated with considerable mortality and morbidity. Though dengue associated HLH was first reported in 1966 and until this writing only 45 cases have been reported in literature [13]. It is likely that the diagnosis of dengue induced HLH is missed as clinicians tend to focus on the underlying infection rather than the overwhelming cytokine production. HLH is a potentially life threatening disorder and several cases reports show dengue induced HLH can be fatal [11], [13], [14]. The pathophysiology of severe dengue (DHF, DSS) is not always well understood and it is now being increasingly believed that macrophage activation may play a role in some cases of severe dengue. It is fairly well established that cross protection among the four dengue serotypes is limited and secondary infection by a different serotype may predispose to DHF and DSS. However DHF and DSS occur in first episode dengue infections also and we believe HLH may have a role in these cases. A literature review of existing cases of dengue associated HLH showed that dengue induced HLH have been reported more often in first episode infections and only a few cases of second episode dengue triggered HLH have been documented [12].
The aim of management of infection associated HLH is to treat the underlying infection that triggered it. Most cases of HLH also need to be treated upfront with standard protocols. Regarding treatment of dengue associated HLH, review of the existing literature showed that few cases have recovered spontaneously with supportive treatment only [11], [15], [16]. However, in majority of the cases pulse dosage of methylprednisolone or dexamethasone have been used to suppress the hyperinflammatory state. Intravenous immunoglobulin G has been used in few cases either alone or with dexamethasone or methylprednisolone. Raju et al. reported successful use of intravenous immunoglobulin G in nineteen children suffering from dengue related HLH [16]. Srichaikul et al. [13], Tan et al. [9] and Wan et al. [11] have reported treating three adult patients successfully with combination of intravenous immunoglobulin G and dexamethasone or methylprednisolone. In the present case high dose steroids was not considered because of associated pancreatitis and concurrent sepsis as the patient had high procalcitonin at presentation and evidence of chest infection in X ray. Our patient of severe dengue with evidence of plasma leak had an uneventful recovery following prompt diagnosis of HLH (on day 7 of fever and 4 of hospitalization) and early institution of specific therapy. The treatment of dengue induced HLH by intravenous immunoglobulin G seems to be associated with a favorable outcome as this case report and similar other cases reported in the literature seem to suggest [8], [16]. Secondary HLH and severe sepsis, systemic inflammatory response syndrome (SIRS), multiple organ dysfunction syndrome (MODS) share clinical and laboratory inflammatory phenotypes and therefore it is important to distinguish these conditions as therapeutic options are radically different. Progressive pancytopenia along with presence of hemophagocytes in the bone marrow helped in establishing the diagnosis of HLH in this patient.
This case report aims to generate awareness about dengue induced HLH and the importance of a high clinical suspicion for early detection thereby facilitating successful treatment. Dengue affects thousands of people worldwide every year and hence may be life saving to detect HLH in patients suffering from dengue. In dengue patients with persistent low counts and multi-organ dysfunction, the possibility of HLH should be kept in mind particularly in first episode dengue infections. The diagnosis is usually challenging, as it can be easily mistaken with other clinical situations, such as sepsis or other systemic inflammatory response syndromes (SIRS). Elevated ferritin levels > 10,000 μg/L has been demonstrated to be 90% sensitive and 96% specific for HLH and should be used as screening tool for early detection of HLH, triggering further investigations [5]. This report adds to the limited adult cases of dengue-associated hemophagocytic syndrome described in the literature and stresses the need to work up patients with severe dengue for possibility of HLH.
Conflict of interest
Nil.
Author contributions
All authors saw the index case, did research on the topic, and contributed to the writing of the report. Syamasis was the clinician primarily responsible for the patient. All the authors helped to proof read and revise the report.
Contributor Information
Ujjwayini Ray, Email: dr_uray@rediffmail.com.
Soma Dutta, Email: dr.somadutta@gmail.com.
Susovan Mondal, Email: drsuso@yahoo.co.in.
Syamasis Bandyopadhyay, Email: sambando@yahoo.co.uk.
References
- 1.Henter J.I., Horne A., Aricó M., Egeler M., Filipovich A., Imashuku S. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–131. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 2.Henter J.I., Elinder G., Ost A. Diagnostic guidelines for hemophagocytic lymphohistiocytosis. the FHL study group of the histiocyte society. Semin Oncol. 1991;18(1):29–33. [PubMed] [Google Scholar]
- 3.Fishman D.N. Hemophagocytic syndromes and infection. Emerg Infect Dis. 2000;6:601–608. doi: 10.3201/eid0606.000608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reiner A.P., Spivak J.L. Hematophagic histiocytosis. A report of 23 new patients and a review of the literature. Medicine (Baltimore) 1988;67(6):369–388. [PubMed] [Google Scholar]
- 5.George M.R. Hemophagocytic lymphohistiocytosis: review of etiologies and management. J Blood Med. 2014;5:69–86. doi: 10.2147/JBM.S46255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhatt S., Gething P.W., Brady O.J., Messina J.P., Farlow A.W., Moyes C.L. The global distribution and burden of dengue. Nature. 2013;496:504–507. doi: 10.1038/nature12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bandyopadhyay B., Bhattacharyya I., Adhikary S., Konar J., Dawar N., Sarkar J. A comprehensive study on the 2012 dengue fever outbreak in Kolkata, India. ISRN Virol. 2013;7:5. [Google Scholar]
- 8.De Koninck A.S., Dierick J., Steyaert S., Taelman P. Hemophagocytic lymphohistiocytosis and dengue infection: rare case report. Acta Clin Belg. 2014;69(3):210–213. doi: 10.1179/2295333714Y.0000000019. [DOI] [PubMed] [Google Scholar]
- 9.Tan L.H., Lum L.C.S., Omar S.F.S., Kan F.K. Hemophagocytosis in dengue: comprehensive report of six cases. J Clin Virol. 2012;55(1):79–82. doi: 10.1016/j.jcv.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 10.Mitra S., Bhattacharyya R. Hemophagocytic syndrome in severe dengue fever: a rare presentation. Indian J Hematol Blood Transfus. 2014;30(1):97–100. doi: 10.1007/s12288-013-0273-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wan Jamaludin W.F., Periyasamy P., Wan Mat W.R., Abdul Wahid S.F. Dengue infection associated hemophagocytic syndrome: therapeutic interventions and outcome. J Clin Virol. 2015;69:91–95. doi: 10.1016/j.jcv.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 12.Sharp T.M., Gaul L., Muehlenbachs A., Hunsperger E., Bhatnagar J., Lueptow R. Fatal hemophagocytic lymphohistiocytosis associated with locally acquired dengue virus infection – New Mexico and Texas, 2012. MMWR Morb Mortal Wkly Rep. 2014;63(3):49–54. [PMC free article] [PubMed] [Google Scholar]
- 13.Srichaikul T., Punyagupta S., Kanchanapoom T., Chanokovat C., Likittanasombat K., Leelasiri A. Hemophagocytic syndrome in Dengue hemorrhagic fever with severe multiorgan complications. J Med Assoc Thai. 2008;91(1):104–109. [PubMed] [Google Scholar]
- 14.Jain D., Singh T. Dengue virus related hemophagocytosis: a rare case report. Hematology. 2013;13:286–288. doi: 10.1179/102453308X316095. [DOI] [PubMed] [Google Scholar]
- 15.Lu P.L., Hsiao H.H., Tsai J.J., Chen T.C., Feng M.C., Chen T.P. Dengue virus-associated hemophagocytic syndrome and dyserythropoiesis: a case report. Kaohsiung J Med Sci. 2005;21:34–39. doi: 10.1016/S1607-551X(09)70274-8. [DOI] [PubMed] [Google Scholar]
- 16.Raju S., Kalyanaraman S., Swaminathan K., Nisha A., Praisid S. Hemophagocytic lymphohistiocytosis syndrome in Dengue hemorrhagic fever. Indian J Pediatr. 2014;81(12):1381–1383. doi: 10.1007/s12098-014-1425-4. [DOI] [PubMed] [Google Scholar]