Abstract
Self-monitoring (SM) of food intake is central to weight loss treatment. Technology makes it possible to reinforce this behavior change strategy by providing real-time feedback (FB) tailored to the diary entry. To test the feasibility of providing 1–4 daily FB messages tailored to dietary recordings via a smartphone, we conducted a 12-week pilot randomized clinical trial in Pittsburgh, PA in US in 2015. We compared 3 groups: SM using the Lose It! smartphone app (Group 1); SM + FB (Group 2); and SM + FB + attending three in-person group sessions (Group 3). The sample (N = 39) was mostly white and female with a mean body mass index of 33.76 kg/m2. Adherence to dietary SM was recorded daily, weight was assessed at baseline and 12 weeks. The mean percentage of days adherent to dietary SM was similar among Groups 1, 2, and 3 (p = 0.66) at 53.50% vs. 55.86% vs. 65.33%, respectively. At 12 weeks, all groups had a significant percent weight loss (p < 0.05), with no differences among groups (− 2.85% vs. − 3.14% vs. − 3.37%) (p = 0.95); 26% of the participants lost ≥ 5% of their baseline weight. Mean retention was 74% with no differences among groups (p = 0.37). All groups adhered to SM at levels comparable to or better than other weight loss studies and lost acceptable amounts of weight, with minimal intervention contact over 12 weeks. These preliminary findings suggest this 3-group approach testing SM alone vs. SM with real-time FB messages alone or supplemented with limited in-person group sessions warrants further testing in a larger, more diverse sample and for a longer intervention period.
Keywords: Self-monitoring, Feedback, Self-efficacy, Weight loss, Standard behavioral treatment, Overweight, Obesity, Mobile technology, mHealth
Highlights
-
•
Preliminary data are provided on testing of novel algorithm-based feedback system.
-
•
Pilot study informed refinement of algorithm and real-time feedback message system.
-
•
Using a smartphone app for self-monitoring diet could enhance adherence.
-
•
Receiving feedback messages with no face-to-face groups could lead to weight loss.
1. Introduction
The evidence supporting the central role of self-monitoring (SM) in weight management has been accumulating for nearly three decades (Acharya et al., 2009, Burke et al., 2008, Burke et al., 2011a, Butryn et al., 2007, Carels et al., 2005, Peterson et al., 2014). A recent review of the weight loss SM literature demonstrated consistent support for a significant association between participant SM and weight loss (Burke et al., 2011b). More recently, consistency and timing of SM in relation to eating were shown to be significantly related to weight outcomes (Sereika et al., 2011).
There is strong theoretical and empirical support for providing feedback (FB) on SM recordings to guide the individual towards better food choices and reinforce behavior changes that lead to weight loss. The technology available today can facilitate personalized FB that can be delivered remotely and in real-time, which translates into the person receiving FB the same day as the recording. Theoretical underpinnings for optimizing the timing of the FB messages are drawn from behavioral theory that provides a wealth of empirical evidence demonstrating that positive reinforcement for an emitted, desired behavior provided immediately following the behavior leads to increases in the occurrences of the desired behavior; the more proximal the reinforcer to the desired behavior, the more likely the desired behavior will be increase (Kanfer and Grimm, 1980). Earlier studies using personal digital assistants (PDA) showed promising results (Burke et al., 2011a, Spring et al., 2012, Burke et al., 2012a). More recently, studies have used mobile phones to deliver messages via text or short message service to participants to promote healthful behaviors (Shapiro et al., 2012, Gerber et al., 2009, Haapala et al., 2009a, Patrick et al., 2009, Carter et al., 2013, Napolitano et al., 2013, Siopis et al., 2014, Martin et al., 2015, Turner-McGrievy and Tate, 2011, Turner-McGrievy et al., 2013). However, these studies did not directly incorporate SM of diet. Thus, the messages were generic in content, rather than focused on the SM data (Gerber et al., 2009, Patrick et al., 2009).
Our SMART Trial provided evidence that FB messages delivered via a PDA are most effective when tailored specifically to the individual's current behaviors (Burke et al., 2012a, Ambeba et al., 2012). The aim of the current study was to test the feasibility of providing 1 to 4 daily FB messages tailored to dietary recordings via a smartphone and compare the effect of SM alone to SM with tailored FB and SM plus tailored FB and face-to-face group sessions. The primary outcomes of the 12-week, pilot, randomized clinical trial (RCT) were recruitment, retention and adherence to SM as well as percent weight loss from baseline to 12 weeks. The secondary outcomes were changes in blood pressure and self-efficacy from baseline to 12 weeks.
2. Subjects and methods
2.1. Study design
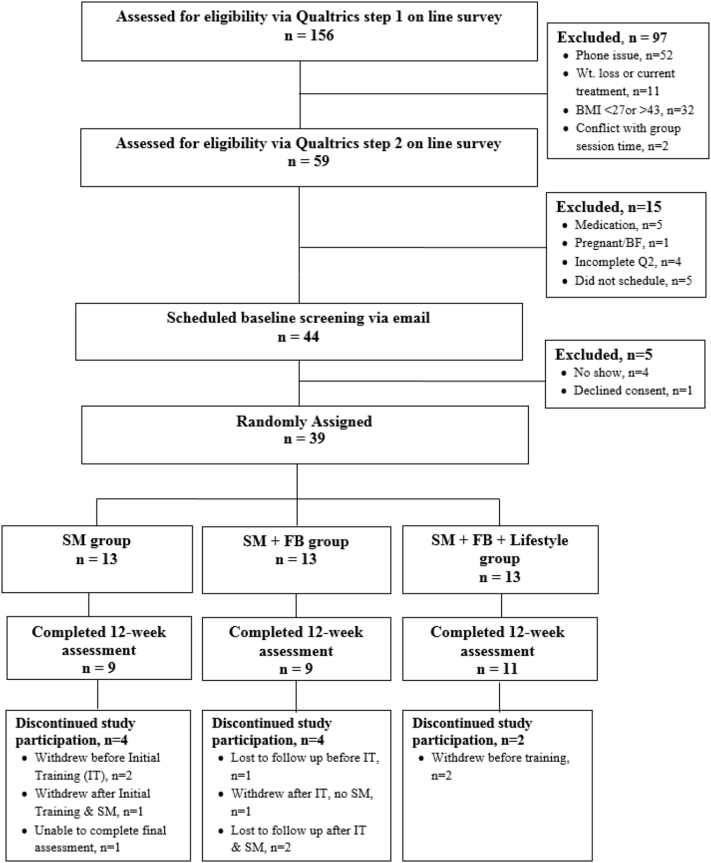
The SMARTER pilot study was a 12-week RCT of behavioral treatment for weight loss with 39 adults randomized to one of 3 groups: Group 1 used the Lose It! app (LoseIt! FitNow, Inc., Boston, MA) on the smartphone for SM of dietary intake; Group 2 used the app for SM and received 1 to 4 tailored FB messages daily; and Group 3 used the app for SM, received 1 to 4 FB messages daily and attended 3 group behavioral weight loss sessions at weeks 2, 4, and 8. Participants were assessed at baseline and 12 weeks and compensated for the final assessment. Written informed consent was obtained from all participants; the study was approved by the University of Pittsburgh Institutional Review Board. The study flow is shown in Fig. 1.
Fig. 1.
Consort diagram.
2.2. Setting and participants
Individuals were eligible if they were ≥ 18 years of age with a body mass index ≥ 27 and ≤ 43, using an Android smartphone, currently not SM their food intake daily, and no recent intentional 10-pound weight loss. Exclusion criteria included pregnancy; conditions requiring medical supervision of diet or exercise.
2.3. Recruitment, screening, and baseline assessment
Participants were recruited from the community using the University Mailing Services batch email system and screened using a Qualtrics survey (Qualtrics, n.d.). Eligible individuals were notified via a second email message with a link to another survey and consent for providing more in-depth health history, including diagnoses of major medical conditions.
2.4. Randomization
The 39 eligible individuals provided consent and were randomized with equal allocation to 1 of the 3 groups. Randomization was conducted using the minimization method considering the pre-randomization factors of gender and race (White vs. non-White) to ensure group balance with respect to these characteristics.
2.5. Intervention
2.5.1. Training on the use of the Lose It! app for dietary SM
All participants were provided the Lose It! app for dietary SM, a commercially available app for mobile and desktop platforms. Prior to training, they were sent an email with directions on installing the app on their smartphone, creating an account, and responding to an email invitation to join the University of Pittsburgh Lose It! portal. After participants “accepted” the invitation, their account was accessible via the portal to the study interventionist. Participants randomized to Groups 2 and 3 were also sent instructions for downloading and installing the FB message software. Each of the three groups had separate training sessions; each was observed by the research staff to perform several SM tasks, e.g., search and enter foods consumed, find an ethnic food, enter physical activity minutes.
Dietary goals. Participants in all three groups were given a daily calorie and daily fat gram goal using the following as a guideline: < 250 lb, 1200–1800 cal and 40–50 g of fat; ≥ 250 lb, 1800–2200 cal and 50–60 g of fat, with the lower numbers being for females. The interventionist discussed with each participant their recommended calorie and fat goal ranges and emphasized timely recording of dietary intake. The groups were instructed how to distribute the calorie and fat allowance across the full day; and about the different types of fat and limiting the saturated fat to no more than 10%. Limiting added sugar drinks was also addressed as a source of calories that did not add nutrients.
For Groups 2 and 3, the interventionist explained that as they completed dietary SM on the app, the FB app would generate responsive “pop-up” messages related to calories, fat, or total sugar they had consumed; if data suggested the absence of SM, a message on the importance of SM may be sent. These three dietary components, calories, fat and sugar, that are tracked in the Lose It! app are important in the management of energy consumption and thus were the focus of the feedback messages. All participants were given a daily goal for total calories and fat consumption.
2.5.2. Weight loss intervention
Participants were asked to self-monitor their dietary intake as soon as possible after eating as well as to weigh daily and enter the weight on the app. Participants were provided one if they had no home scale. One week after the initiation of the SM period, the interventionist sent a generic reminder email regarding continuing self-monitoring and contacting the interventionist if they had questions or technical issues. All participants received an individualized, generic email message at the start of Week 3, providing encouragement and asking if there were any technology issues that needed troubleshooting. For Group 2 and 3 participants who reported not receiving FB messages, troubleshooting with the software installation followed. Ongoing generic email messages were sent to all participants every two weeks to encourage continued SM or to offer technical support. Sending the message to all participants prevented the creation of bias.
2.5.3. FB messages
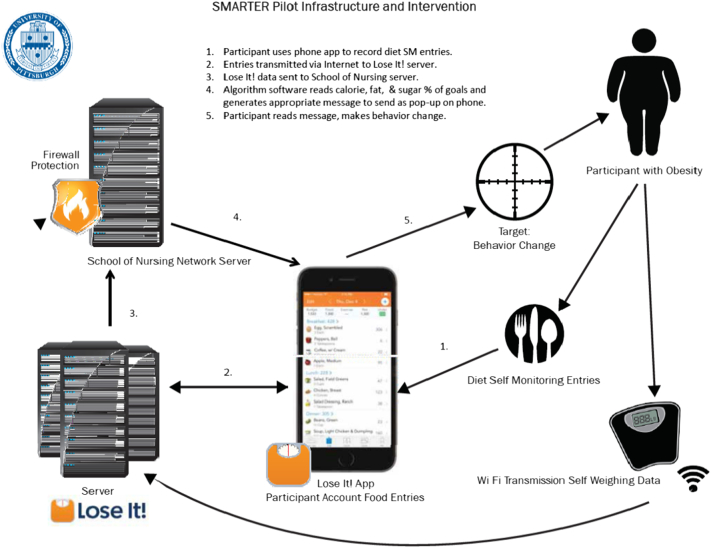
SM data were downloaded hourly between 9 AM and 10 PM from the Lose It! portal to the Oracle database maintained by the School of Nursing housed at the University of Pittsburgh Network Operating Center via the network server (see Fig. 2). The FB message algorithm was programmed to read the most recently recorded calories, fat, and sugar data 1 to 4 times per day from the download and randomly select an appropriate message. Conditions were created using percentages of calories, fat and sugar that approximated various combinations of 1) under-eating, 2) meeting goals, or 3) exceeding goals. See Table 1 for examples of conditions at breakfast. At each time point that a participant was randomly assigned to receive a message, the algorithm performed the following sequential tasks: calculated percentages, matched percentages to a condition, randomly chose a message from the library that was applicable to the condition and delivered the message to the participant's smartphone as a pop-up message. If the participant consumed amounts of calories, fat and sugar for which no condition “matched,” no message would be delivered. The algorithm randomly selected the message from a library of messages. The library contained hundreds of messages, which we continued to develop over the course of the study to keep the messages fresh and prevent desensitization, an issue we experienced in the first study in which we tested an earlier version of the algorithm (Ambeba et al., 2015).
Fig. 2.
SMARTER pilot study infrastructure.
Table 1.
Examples of conditions for percentages of participant goals of calories, fat, and sugar at breakfast to match to FB messages.
| 9 AM–12 noon | Calorie (% of goal) | Fat (% of goal) | Sugar (g) | SM data suggestive of |
|---|---|---|---|---|
| Condition number | ||||
| 1 | > 0–< 25% | Participant not eating or SM | ||
| 2 | 25–30% | 25–30% | ≥ 15–25 | Participant meeting goals |
| 3 | > 30% | > 30% | ≥ 15–25 | Fat and calorie too high; sugar within limits |
| 4 | 25–30% | 25–30% | > 25 | Calorie and fats within limits; sugar too high |
| 5 | 25–30% | < 10% | > 25 | Calorie intake at goal but fat too low, sugar too high |
| 6 | > 30% | 25–30% | > 25 | Calories over goal; fat at goal; sugar too high |
| 7 | > 30% | > 30% | > 25 | Calories, fat, and sugar exceeding goals |
| 8 | 25–30% | > 30% | > 25 | Calories at goal; fat and sugar too high |
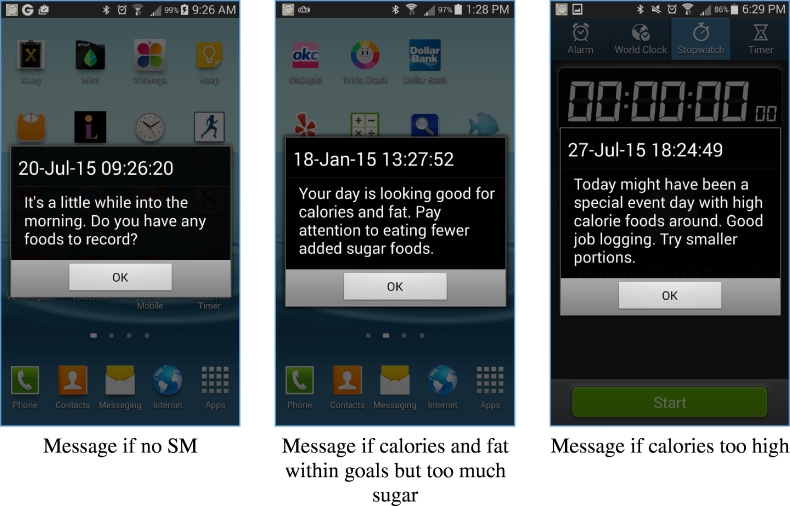
The FB message library contained approximately 6 to 9 messages for each condition; messages were refreshed with additional or alternative verbiage during the pilot study to prevent desensitization (see Fig. 3). Messages were written to provide FB about consumption, and to provide positive reinforcement or a suggestion to guide the participant to a healthier choice. See Table 2 for examples. Messages remained on the phone (see Fig. 3) until the participant tapped the “OK” box, or timed out at 11 PM that day.
Fig. 3.
Screen shots of pop-up messages to participants.
Table 2.
Examples of conditions and samples of possible FB messages.
| Condition ID | Message ID | Message content | Time of download |
|---|---|---|---|
| 6 | 1 | Terrific job so far. Try some healthy fats at next meal. Nuts, oils, avocado. | 12/8/2014 4:36:00 PM |
| 8 | 4 | Food portions have been high in calories and fat grams. Eat smaller portions and you can still make your goals today. | 12/8/2014 4:36:00 PM |
| 10 | 1 | You haven't recorded much today. Have you tried using an entry from “Meals” that matches? | 12/8/2014 4:36:00 PM |
| 22 | 2 | Total calories and sugars are within range. Wonderful choices. Terrific SM. | 12/8/2014 4:36:00 PM |
| 30 | 2 | Nice effort limiting calories and fat. Total sugars are high-added sugars in sweets, soda and goodies are the ones to limit. | 12/8/2014 4:36:00 PM |
2.5.4. Behavioral intervention for weight loss
Group 3 participants attended three group behavioral weight loss sessions. Session topics included: 1) dietary guidelines for a reduced calorie diet; 2) behavior modification and mindfulness strategies for lifestyle change; and 3) increasing physical activity and decreasing sedentary time.
2.6. Measures
All measures were taken at two time points: baseline – prior to randomization, and at 12 weeks – after the completion of the intervention.
Socio-demographic data. At baseline, participants completed the Socio-demographic and Lifestyle Questionnaire that was comprised of 25 questions.
Adherence to dietary SM. Daily adherence to dietary SM was treated as a binary variable, where adherence was defined as recording ≥ 50% of the prescribed daily calorie intake goal, e.g., if the person who was prescribed a 1200/day calorie allowance recorded eating foods that amounted to 900 cal that day, the person would be considered adherent to dietary SM. This definition has been used in several trials (Acharya et al., 2009, Burke et al., 2012a, Turk et al., 2012a, Zheng et al., 2016).
Weight. Weights were measured at baseline and 12 weeks on a digital scale (Tanita Corporation of America, Inc., Arlington Heights, IL, USA). The individual wore light clothing and no shoes for the weight measure.
Blood pressure. After at least a 5-minute rest period, blood pressure was measured with an Omron cuff on the right arm with the individual sitting and with 1-minute rest between readings. The first reading was discarded and the mean of the second and third readings were used.
Self-efficacy was measured by the Weight Efficacy Lifestyle (WEL) (Clark et al., 1996) questionnaire. The individual completed the scale at the research center. This 20-item scale assesses level of confidence to resist eating in varied situations or emotional states. It has established psychometric properties (Clark et al., 1991a) and has demonstrated explanatory value in weight loss behavior in our previous studies (Warziski et al., 2008). The Cronbach's alpha of WEL has been reported at > 0.70 among several samples (Clark et al., 1991b, Hays et al., 2014, Turk et al., 2012b). This scale has been used in several of our studies and is easy to complete.
2.7. Statistical analysis
Data were analyzed using SAS for Windows (version 9.4, SAS Institute, Inc., Cary, NC, USA). For the primary outcomes, analyses were conducted based on the principle of intention-to-treat and per protocol analysis. In the per protocol analysis, we included only the participants who complied with their assigned protocol, i.e., for Group 3, we included only the participants who attended all of the three group sessions and self-monitored their diet. Group differences in attrition were analyzed using binary logistic regression. Continuous variables were assessed for normality using the Shapiro Wilks test, and no significant departures from normality were found. Baseline characteristics were reported as mean and standard deviation (SD) for continuous and count descriptors, and percentages (%) and frequency counts (n) for categorical variables. For baseline group comparisons, we used one-way analysis of variance (ANOVA) for continuous descriptors, Fisher's exact test for categorical variables, and Poisson regression for any count descriptors not normally distributed, i.e., number of people in the household.
Percent days adherent to dietary SM over 12 weeks was computed as the number of days adherent to dietary SM divided by days in the study (84 days of 12 weeks or days until the withdrawal) and expressed as a percentage. One-way ANOVA with post hoc pairwise comparisons with Bonferroni adjustment of p-values was used to compare group differences.
Both absolute change and percent change of weight, systolic blood pressure (SBP), diastolic blood pressure (DBP) and WEL total score from baseline to the 12th week were computed and analyzed. If the 12th week assessment was not completed, we assumed no change from baseline and therefore used the baseline observations to impute the missing values. Independent two-sample t-tests and Fisher's exact tests were used to examine baseline differences between completers and non-completers. Percent changes of weight, DBP, SBP and WEL from baseline to 12 weeks were tested against the null hypothesis of no within-group change using paired t-tests. Omnibus group comparisons of percent change were analyzed using the F-test from one-way ANOVA. Sensitivity analyses were conducted for incomplete data from some participants. When participants with incomplete data were excluded from the analyses, the results did not markedly change suggesting that our findings were robust.
3. Results
The sample (N = 39) was predominantly female (87.18%) and White (84.62%) with a mean BMI of 33.76 kg/m2. The baseline description of the sample is detailed in Table 3. There were no significant differences among the three groups in baseline weight or other participant characteristics. Twenty-nine participants complied with the protocols they were assigned, 11 (84.6%) in Group 1, 11 (84.6%) in Group 2 and 7 (53.8%) in Group 3.
Table 3.
Baseline description of sample (N = 39).
| Characteristic | Overall (N = 39) |
Group 1 SM only (n = 13) |
Group 2 SM + FB (n = 13) |
Group 3 SM + FB + group sessions (n = 13) |
p-Value |
|---|---|---|---|---|---|
| Gender (female), % (n) | 87.18 (34) | 84.62 (11) | 84.62 (11) | 92.31 (12) | 1.00 |
| Race (white), % (n) | 84.62 (33) | 84.62 (11) | 76.92 (10) | 92.31 (12) | 0.85 |
| Marital status, % (n) | 0.73 | ||||
| Never married | 5.13 (2) | 7.69 (1) | 0 (0) | 7.69 (1) | |
| Currently married | 56.41 (22) | 61.54 (8) | 69.23 (9) | 38.46 (5) | |
| Formerly married (divorced/separated/widowed) | 15.38 (6) | 15.38 (2) | 7.69 (1) | 23.08 (3) | |
| Employed full time, % (n) | 92.31 (36) | 84.62 (11) | 92.31 (12) | 100.00 (13) | 0.76 |
| Number of people currently in household, mean ± SD | 2.03 ± 0.78 | 2.23 ± 1.01 | 2.08 ± 0.76 | 1.77 ± 0.44 | 0.70 |
| Family gross incomea, % (n) | 0.92 | ||||
| <$50,000 | 12.12 (4) | 9.09 (1) | 10.00 (1) | 16.67 (2) | |
| $50,000–$99,999 | 39.39 (13) | 45.45 (5) | 30.00 (3) | 41.67 (5) | |
| ≥$100,000 | 48.48 (16) | 45.45 (5) | 60.00 (6) | 41.67 (5) | |
| Formal education (years), mean ± SD | 16.31 ± 2.96 | 15.08 ± 2.53 | 16.69 ± 3.57 | 17.15 ± 2.44 | 0.17 |
| Age (years), mean ± SD | 44.85 ± 12.75 | 49.46 ± 13.04 | 46.38 ± 10.77 | 38.69 ± 12.75 | 0.08 |
| Baseline weight (kg), mean ± SD | 93.15 ± 15.89 | 93.43 ± 16.03 | 92.55 ± 18.09 | 93.47 ± 14.64 | 0.99 |
| Baseline BMI (kg/m2), mean ± SD | 33.76 ± 4.28 | 34.49 ± 4.06 | 33.46 ± 4.49 | 33.32 ± 4.53 | 0.76 |
| Systolic BP (mm Hg), mean ± SD | 123.62 ± 12.74 | 125.87 ± 14.07 | 122.36 ± 12.21 | 122.64 ± 12.61 | 0.75 |
| Diastolic BP (mm Hg), mean ± SD | 82.89 ± 6.94 | 85.13 ± 7.48 | 81.56 ± 7.14 | 81.97 ± 6.09 | 0.37 |
| WEL | 120.41 ± 29.26 | 112.85 ± 30.78 | 126.08 ± 25.89 | 122.31 ± 31.52 | 0.51 |
Note: SM = self-monitoring, SM + FB = self-monitoring + feedback messages, BP = blood pressure, WEL = weight efficacy lifestyle.
Family gross income has 6 missing values.
Adherence and retention were primary outcomes in this pilot study. The percent days adherent to dietary SM over 12 weeks was 53.50 ± 34.40% in Group 1, 55.86 ± 39.26% in Group 2, and 65.33 ± 26.54% in Group 3 with no significant differences among the three groups (p = 0.67). For the 29 participants who complied with the protocol, the percent days adherent to dietary SM over 12 weeks was 58.37 ± 31.46% in Group 1, 60.60 ± 37.40% in Group 2, and 75.31 ± 21.22% in Group 3 with no significant differences among three groups (p = 0.52). Due to early technical problems, only 30–60% of the messages were delivered initially; this increased to 70–80% in the later part of the trial. Overall, the retention rate at 12 weeks was 74%. As noted in Fig. 1, four participants withdrew from each of the SM and the SM + FB groups, two withdrew from the SM + FB + Lifestyle behavior group. In Group 3, 7 participants (53.85%) attended all three group sessions and 9 participants (69.23%) attended at least two group sessions. The numbers of participants who attended the 1st, 2nd, and 3rd group session were 10 (76.92%), 9 (69.23%) and 8 (61.54%), respectively.
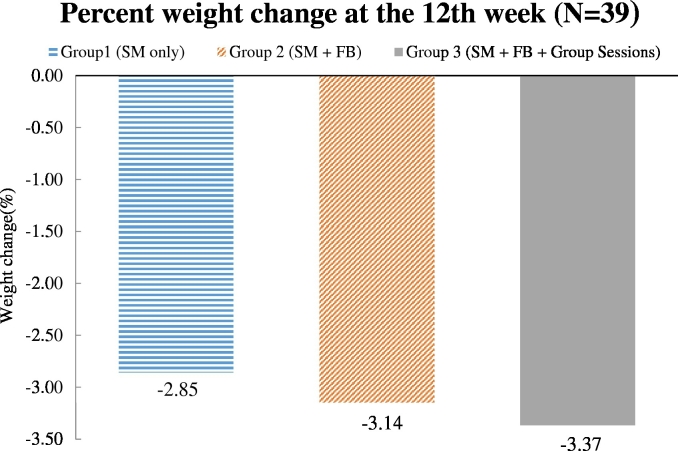
At 12 weeks, the outcome weights were on average 90.86 ± 16.33 kg, 89.67 ± 17.39 kg, and 90.45 ± 15.64 kg and the absolute weight changes were on average − 2.47 ± 4.24 kg, − 2.88 ± 4.54 kg, and − 3.01 ± 3.15 kg in Groups 1, 2, and 3, respectively. Mean percent weight changes from baseline to 12 weeks were − 2.85% (95% CI: [− 5.21%, − 0.50%]), − 3.14% (95% CI:[− 5.50%, − 0.79%]), − 3.37% (95% CI: [− 5.72%, − 1.01%]) for Groups 1, 2 and 3, respectively (Fig. 4). There were no significant differences in the mean percent weight loss among the three groups (p = 0.95); however, there were significant weight losses within each group (p's < 0.05). More specifically, 26% of the participants lost ≥ 5% of their baseline weight, which is clinically significant. When examined by group, 3 in the SM only group, 3 in the SM + FB group, and 4 in the SM + FB + lifestyle group lost 5% or more of their baseline weight. For participants who complied with the protocols, the outcome weights were 87.97 ± 14.40 kg, 89.47 ± 18.87 kg, and 87.23 ± 11.77 kg and the absolute weight loss was − 3.03 ± 4.48 kg, − 3.40 ± 4.77 kg, and − 3.53 ± 3.39 kg in Groups 1, 2, and 3, respectively. Mean percent weight changes from baseline to 12 weeks were − 3.37% (95% CI: [− 6.15%, − 0.59%]), − 3.71% (95% CI: [− 6.49%, − 0.94%]), and − 3.94% (95% CI: [− 7.42, − 0.45%]) for Groups 1, 2 and 3, respectively. There were no significant differences in mean percent weight loss among the three groups (p = 0.96).
Fig. 4.
Percent weight change from baseline to 12 weeks (N = 39).
For Groups 1, 2, and 3, respectively, SBP was reduced by 5.32 ± 6.58%, 5.78 ± 6.36%, and 5.51 ± 6.71% and DBP was reduced by 5.48 ± 7.51%, 2.82 ± 7.67%, and 4.18 ± 5.31%. There were no significant differences among the groups for the mean percent changes in SBP (p = 0.98) and DBP (p = 0.51). Within each group, there was a significant decrease in SBP (p's < 0.05); Group 1 (p = 0.02) and Group 3 (p = 0.02) also experienced a significant decrease in DBP. There were no significant differences among the groups on mean change in the total WEL score (p = 0.54). All three groups reported higher levels of self-efficacy at 12 weeks compared to baseline, with the total WEL score increasing by 13.03% in Group 1, 14.15% in Group 2, and 4.98% in Group 3; only Group 1 (SM Only) demonstrated a significant increase in the WEL score (p = 0.03).
4. Discussion
This pilot study tested the feasibility of providing 1 to 4 daily FB messages tailored to dietary recordings via a smartphone and compared the effect of SM with tailored FB to two other groups: SM without tailored FB and SM plus tailored FB and in-person group sessions. The mean percent of days adherent to dietary SM was similar among the three groups and at 12 weeks, and all three groups had a significant percent weight loss with no differences among groups.
In our previous long-term studies, we typically engaged in a phone-based screening, followed by an orientation visit and 5-day run-in period of dietary SM, with excellent retention results. (Burke et al., 2012b, Burke et al., 2006a) Relying only on online screening and excluding the 5-day run-in period of self-monitoring may have contributed to our uncharacteristically low retention rate of 74%. The faster-paced screening and recruitment may not have permitted the individuals adequate processing time to think about and test what they were committing to, and not experiencing a run-in period with self-monitoring may not have prepared them for the effort that self-monitoring requires when asked to do on a daily basis. Most of our participants' withdrawals were in the early days of the study, seemingly confirming this. To address this, we think it is essential to resume including in the screening phase a 5-day SM period similar to what we have done with our larger trials where we have had excellent retention over 12 to 24 months (Burke et al., 2009, Burke et al., 2006b). We are aware that others have experienced low retention rates in pilot studies but it is not clear why (Helsel et al., 2007, Cavallo et al., 2016). It is possible that investigators may have limited time and resources in the pilot phase and limit some procedures that they would not do in larger scale trials.
Adherence to the dietary SM protocol also was an indicator of the study's feasibility. Compared to a previous 24-month trial testing 3 approaches to SM and considering the infrequent contact with the individuals in this pilot study, the adherence to SM was excellent with Groups 1 and 2 having similar rates of adherence as those who used an electronic diary in a previous trial, and Group 3's adherence at 65% exceeded what we observed previously (Wang et al., 2012).
While there were no significant differences in the percent weight loss among the three groups, each group lost a significant amount of weight over the 12 weeks. The literature does not include studies that used pop-up messages delivered in real time with the message tailored to the diary entries; however, studies have been conducted that sent text messages. Turner-McGrievy et al. (2009) reported a 2.9 kg weight loss in their podcast intervention group at 3 months in a study that compared a podcast and mobile phone app to podcast only, a weight loss very similar to what we observed. In a later study, Turner-McGrievy and Tate compared a podcast + mobile phone app for SM to a group that used the mobile phone app only and observed a − 2.6% loss in both groups at 3 months and − 2.7% at 6 months (Turner-McGrievy and Tate, 2011). These are similar to the losses we observed at 12 weeks in our pilot study (Turner-McGrievy and Tate, 2011, Turner-McGrievy et al., 2009). Haapala et al. (2009b) and Patrick et al. (2009) reported on longer studies in which participants sent their weight via text messaging. Haapala et al. (2009b) compared this approach plus a study website to a wait-list control group and found a 3.1 kg weight loss in the intervention group and 0.7 kg loss in the wait-list control group. Patrick et al. (2009) used text messaging daily as well as multimedia messaging and found a 2.10 kg loss at 4 months in the experimental group compared to 0.40 kg in the attention control group. Compared to these reported studies, our pilot study participants received fewer contacts during the 12 weeks of follow-up yet had similar weight losses (Patrick et al., 2009).
Secondary outcomes included blood pressure and self-efficacy for weight loss. We observed a significant mean decrease in SBP in each of the three groups but not a significant group difference. For DBP there were significant reductions in Groups 1 and 3. Increases in perceived self-efficacy were observed in all groups but these changes were significant only in Group 1, the group that did not receive FB messages. The experience of success without assistance from a professional may have instilled the greater increase in self-efficacy.
4.1. FB messages: lessons learned
During weeks 1–8, data from the server indicated participants in Groups 2 and 3 were receiving between 30 and 60% of the scheduled messages, with a few consistently not receiving any messages. There are several reasons why they did not receive the full dose of intended FB messages. First, as was noted earlier, there were combinations of intake in which the algorithm would find a “no match”, resulting in no message being delivered at some time points. The full implementation of the system involved both the timing of SM and the message delivery programming. Participants were receiving a large proportion of messages for conditions of not eating or not SM when in reality they were SM outside of the “windows” set within the program (i.e. breakfast, 9–12 AM, lunch, 12:01–5 PM, dinner, 5:01–7:30 PM). Thus, they received frequent messages to self-monitor and fewer messages pertaining to suggestions for better food choices. Some participants seemed to view the messages as a reminder system and reported finding that to be helpful. Others found them repetitive or annoying when activities of daily living required that they delay SM, despite intentions to be more adherent. Thus, motivating and enabling participants to self-monitor in a timely fashion as well as tweaking the hours of random message generation may enhance delivery of all modes of message delivery in future studies.
Second, there were difficulties in downloading and installing the FB message software on the user end. For example, non-delivery could be caused by participants upgrading their phone without reinstalling the message software, periods of weak or no connectivity to Wi-Fi or cellular towers, or phones being turned off. Ongoing attempts to reach some of the participants and troubleshoot any software installation or connectivity issues were partially successful. One software glitch was that when a participant lost connectivity or turned his/her phone off, re-connection could take an hour. Messages cued in that hour would have been missed. Some participants routinely turned their phones off and were not amenable to leaving them on continuously. Participants also would turn their phones off when needing to silence the FB message alarm, such as during a meeting, since the software allowed silencing of the alarm only within the app, not by silencing the phone. Participants also informed us that if a pop-up message arrived while they were engaged in another smartphone function (e.g. phone call, GPS), they would have to tap “OK” indicating that the message had been read to resume what they were doing. In that moment, the full impact and intent of the message for the user was likely lessened due to its being a distraction. Because messages were not stored, participants could not re-access them later; thus, a substantial software improvement is needed to modify this.
Third, on the software programming side, issues could be addressed with technical support. A consultant programmer familiar with our system was brought in to review the program data to identify any problems that could be fixed and that could increase message reception. Changes in the software related to missed messages were necessary. Issuance of updates to participants' smartphones resulted in improved message reception rates of 70–85% in the final weeks of the protocol. An especially important correction addressed programming in the FB loop and allowed message delivery to be resumed more quickly after a phone had been turned off or after a period of non-connectivity. The programmer also found via bug reports from staff test phones that the widget (code or portions of code in the Android system) in the app had crashed and would attempt to load a previous version of the software. We found participants were not able to generate bug reports very easily. The correction for widget crashes was for participants to uninstall and then reinstall the most recent software version. Some participants found this to be tedious and would not attend to it for several days, resulting in no messages being delivered.
4.2. Strengths and limitations
As a pilot feasibility study, there were some familiar limitations, e.g., a small, homogenous sample; however, it also had important strengths. First, it provided preliminary data on the testing of a novel algorithm-based FB system that provided tailored messages retrieved from an investigator-developed library in real time. Second, within this brief 12-week period it demonstrated that participants who used only a mobile phone app for SM diet could lose weight that was comparable to those who received FB messages and those who received the same FB message system and attended three face-to-face group sessions. The testing of the FB system taught us a great deal about the challenges of implementing the system from several perspectives, including the technical aspects of pushing the messages to the participants' phones, timing related to SM and having messages be reinforcing of participant behavior.
In conclusion, all three groups using the same SM program alone or with varying supplemental intervention components (FB, group sessions) achieved comparable weight loss and improvements in blood pressure and self-efficacy. These preliminary findings suggest that this 3-group approach to testing dietary SM alone vs. dietary SM with tailored FB messages alone or supplemented with group sessions warrants further testing in a larger, more diverse sample and for a longer intervention period.
Funding: This work was supported by the National Institutes of Health (NIH) grant R01-HL1073702.
Clinicaltrials.gov registration: NCT02829632.
Conflict of interest: The authors have no conflict of interest to disclose. Please see the Conflict of Interest documentation in the Editorial Policy section for details.
Transparency document
Transparency document
Acknowledgments
NIH grant R01-HL1073702 and the participants of the pilot study.
Footnotes
The Transparency document associated with this article can be found, in the online version.
References
- Acharya S.D., Elci O.U., Sereika S.M. Adherence to a behavioral weight loss treatment program enhances weight loss and improvements in biomarkers. Patient Prefer Adherence. 2009;3:151–160. doi: 10.2147/ppa.s5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambeba E.J., Sereika S.M., Styn M.A. The effect of tailored feedback messages, delivered remotely and daily, on changes in dietary intake and measures of adiposity. Journal of Patient Education and Counseling. 2012 [Google Scholar]
- Ambeba E.J., Ye L., Sereika S.M. The use of mHealth to deliver tailored messages reduces reported energy and fat intake. J Cardiovasc Nurs. 2015;30(1):35–43. doi: 10.1097/JCN.0000000000000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L.E., Styn M.A., Steenkiste A.R., Music E., Warziski M., Choo J. A randomized clinical trial testing treatment preference and two dietary options in behavioral weight management: preliminary results of the impact of diet at 6 months—PREFER study. Obesity (Silver Spring) 2006;14(11):2007–2017. doi: 10.1038/oby.2006.235. [DOI] [PubMed] [Google Scholar]
- Burke L.E., Warziski M., Acharya S. PREFER trial: a randomized clinical trial testing treatment preference and two dietary options combined with behavioral weight management. Obesity. 2006;14(Suppl):A32. doi: 10.1038/oby.2006.235. [DOI] [PubMed] [Google Scholar]
- Burke L.E., Sereika S.M., Music E., Warziski M., Styn M.A., Stone A. Using instrumented paper diaries to document self-monitoring patterns in weight loss. Contemp. Clin. Trials. 2008;29(2):182–193. doi: 10.1016/j.cct.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L.E., Styn M.A., Glanz K. SMART trial: a randomized clinical trial of self-monitoring in behavioral weight management-design and baseline findings. Contemp Clin Trials. 2009;30(6):540–551. doi: 10.1016/j.cct.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L.E., Conroy M.B., Sereika S.M. The effect of electronic self-monitoring on weight loss and dietary intake: a randomized behavioral weight loss trial. Obesity (Silver Spring) 2011;19(2):338–344. doi: 10.1038/oby.2010.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L.E., Wang J., Sevick M.A. Self-monitoring in weight loss: a systematic review of the literature. J. Am. Diet. Assoc. 2011;111(1):92–102. doi: 10.1016/j.jada.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L.E., Styn M.A., Sereika S.M. Using mHealth technology to enhance self-monitoring for weight loss: a randomized trial. Am. J. Prev. Med. 2012;43(1):20–26. doi: 10.1016/j.amepre.2012.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L.E., Styn M.A., Sereika S.M. Using mHealth technology to enhance self-monitoring for weight loss: a randomized trial. Am. J. Prev. Med. 2012;43(1):20–26. doi: 10.1016/j.amepre.2012.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butryn M.L., Phelan S., Hill J.O., Wing R.R. Consistent self-monitoring of weight: a key component of successful weight loss maintenance. Obesity. 2007;15(12):3091–3096. doi: 10.1038/oby.2007.368. [DOI] [PubMed] [Google Scholar]
- Carels R.A., Darby L.A., Rydin S., Douglass O.M., Cacciapaglia H.M., O'Brien W.H. The relationship between self-monitoring, outcome expectancies, difficulties with eating and exercise, and physical activity and weight loss treatment outcomes. Ann. Behav. Med. 2005;30(3):182–190. doi: 10.1207/s15324796abm3003_2. [DOI] [PubMed] [Google Scholar]
- Carter M.C., Burley V.J., Nykjaer C., Cade J.E. Adherence to a smartphone application for weight loss compared to website and paper diary: pilot randomized controlled trial. J. Med. Internet Res. 2013;15(4):e32. doi: 10.2196/jmir.2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavallo D.N., Sisneros J.A., Ronay A.A. Assessing the feasibility of a web-based weight loss intervention for low-income women of reproductive age: a pilot study. JMIR Res Protoc. 2016;5(1) doi: 10.2196/resprot.4865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark M.M., Abrams D.B., Niaura R.S., Eaton C.A., Rossi J.S. Self-efficacy in weight management. J. Consult. Clin. Psychol. 1991;59:739–744. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- Clark M.M., Abrams D.B., Niaura R.S., Eaton C.A., Rossi J.S. Self-efficacy in weight management. J. Consult. Clin. Psychol. 1991;59(5):739–744. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- Clark M.M., Cargill B.R., Medeiros M.L., Pera V. Changes in self-efficacy following obesity treatment. Obes. Res. 1996;4(2):179–181. doi: 10.1002/j.1550-8528.1996.tb00531.x. [DOI] [PubMed] [Google Scholar]
- Gerber B.S., Stolley M.R., Thompson A.L., Sharp L.K., Fitzgibbon M.L. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: a feasibility study. Health Informatics J. 2009;15(1):17–25. doi: 10.1177/1460458208099865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haapala I., Barengo N.C., Biggs S., Surakka L., Manninen P. Weight loss by mobile phone: a 1-year effectiveness study. Public Health Nutr. 2009;12(12):2382–2391. doi: 10.1017/S1368980009005230. [DOI] [PubMed] [Google Scholar]
- Haapala I., Barengo N.C., Biggs S., Surakka L., Manninen P. Weight loss by mobile phone: a 1-year effectiveness study. Public Health Nutr. 2009;12(12):2382–2391. doi: 10.1017/S1368980009005230. [DOI] [PubMed] [Google Scholar]
- Hays L.M., Finch E.A., Saha C., Marrero D.G., Ackermann R.T. Effect of self-efficacy on weight loss: a psychosocial analysis of a community-based adaptation of the diabetes prevention program lifestyle intervention. Diabetes Spectr. 2014;27(4):270–275. doi: 10.2337/diaspect.27.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helsel D.L., Jakicic J.M., Otto A.D. Comparison of techniques for self-monitoring eating and exercise behaviors on weight loss in a correspondence-based intervention. J. Am. Diet. Assoc. 2007;107(10):1807–1810. doi: 10.1016/j.jada.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Kanfer F.H., Grimm L.G. Managing clinical change: a process model of therapy. Behav. Modif. 1980;4(4):419–444. [Google Scholar]
- Martin C.K., Miller A.C., Thomas D.M., Champagne C.M., Han H., Church T. Efficacy of SmartLoss (SM), a smartphone-based weight loss intervention: results from a randomized controlled trial. Obesity (Silver Spring) 2015;23(5):935–942. doi: 10.1002/oby.21063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napolitano M.A., Hayes S., Bennett G.G., Ives A.K., Foster G.D. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity (Silver Spring) 2013;21(1):25–31. doi: 10.1002/oby.20232. [DOI] [PubMed] [Google Scholar]
- Patrick K., Raab F., Adams M.A. A text message-based intervention for weight loss: randomized controlled trial. J. Med. Internet Res. 2009;11(1) doi: 10.2196/jmir.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson N.D., Middleton K.R., Nackers L.M., Medina K.E., Milsom V.A., Perri M.G. Dietary self-monitoring and long-term success with weight management. Obesity (Silver Spring) 2014;22(9):1962–1967. doi: 10.1002/oby.20807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qualtrics www.qualtrics.com/research-suite/
- Sereika S.M., Styn M.A., Music M., Wang J., Acharya S.D., Burke L.E. AHA EPI/NPAM 2011 Scientific Sessions, March 22–25, 2011, Atlanta, GA. 2011. Weight loss is associated with timing and frequency of dietary self-monitoring in overweight and obese adults in a behavioral weight-loss trial; p. 103. [Google Scholar]
- Shapiro J.R., Koro T., Neal Doran N. Text4Diet: a randomized controlled study using text messaging for weight loss behaviors. Prev. Med. 2012;55:412–417. doi: 10.1016/j.ypmed.2012.08.011. [DOI] [PubMed] [Google Scholar]
- Siopis G., Chey T., Allman-Farinelli M. A systematic review and meta-analysis of interventions for weight management using text messaging. J. Hum. Nutr. Diet. 2014 doi: 10.1111/jhn.12207. [DOI] [PubMed] [Google Scholar]
- Spring B., Schneider K., McFadden H.G. Multiple behavior changes in diet and activity: a randomized controlled trial using mobile technology behavior changes in diet and activity. Arch. Intern. Med. 2012;172(10):789–796. doi: 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turk M.W., Elci O.U., Wang J. Self-monitoring as a mediator of weight loss in the SMART randomized clinical trial. International Journal of Behavioral Medicine. 2012 doi: 10.1007/s12529-012-9259-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turk M.W., Sereika S.M., Yang K., Ewing L.J., Hravnak M., Burke L.E. Psychosocial correlates of weight maintenance among Black & White adults. Am. J. Health Behav. 2012;36(3):395–407. doi: 10.5993/AJHB.36.3.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner-McGrievy G., Tate D. Tweets, apps, and pods: results of the 6-month Mobile Pounds Off Digitally (Mobile POD) randomized weight-loss intervention among adults. J. Med. Internet Res. 2011;13(4) doi: 10.2196/jmir.1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner-McGrievy G.M., Campbell M.K., Tate D.F., Truesdale K.P., Bowling J.M., Crosby L. Pounds Off Digitally study: a randomized podcasting weight-loss intervention. Am. J. Prev. Med. 2009;37(4):263–269. doi: 10.1016/j.amepre.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner-McGrievy G.M., Beets M.W., Moore J.B., Kaczynski A.T., Barr-Anderson D.J., Tate D.F. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J. Am. Med. Inform. Assoc. 2013;20(3):513–518. doi: 10.1136/amiajnl-2012-001510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Sereika S.M., Chasens E.R., Ewing L.J., Matthews J.T., Burke L.E. Effect of adherence to self-monitoring of diet and physical activity on weight loss in a technology-supported behavioral intervention. Patient Prefer Adherence. 2012;6:221–226. doi: 10.2147/PPA.S28889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warziski M.T., Sereika S.M., Styn M.A., Music E., Burke L.E. Changes in self-efficacy and dietary adherence: the impact on weight loss in the PREFER study. J. Behav. Med. 2008;31(1):81–92. doi: 10.1007/s10865-007-9135-2. [DOI] [PubMed] [Google Scholar]
- Zheng Y., Burke L.E., Danford C.A., Ewing L.J., Terry M.A., Sereika S.M. Patterns of self-weighing behavior and weight change in a weight loss trial. Int. J. Obes. 2016 doi: 10.1038/ijo.2016.68. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transparency document