Abstract
Objectives. To examine population and HIV care outcomes of people living with HIV/AIDS (PLWHA) at their first incarceration of 2014 in 2 county jails in King County, Washington.
Methods. Using HIV surveillance data linked with jail booking data, we examined demographic information, viral loads, CD4 counts, and incarceration details for the period prior to jail booking, during incarceration, and year following jail release.
Results. In 2014, 202 PLWHA were incarcerated, 51% of whom were virally nonsuppressed at booking. This population represented approximately 3% of all HIV-diagnosed persons and 7% of virally nonsuppressed persons in King County. Within a year of release, 62% were virally suppressed, compared with 79% of the general HIV-diagnosed population in King County.
Conclusions. Incarcerated PLWHA are disproportionately virally nonsuppressed compared with nonincarcerated PLWHA up to a year after release from jail.
Public Health Implications. Coordination of health information exchange between the health department and jails could enhance public health efforts to improve the HIV care continuum.
Incarcerated people living with HIV/AIDS (PLWHA) are at risk for poor health outcomes, and national estimates suggest that approximately 14% of PLWHA in the United States will be incarcerated at least once in their lifetime.1 Compared with PLWHA who are not incarcerated, this population has lower rates of antiretroviral therapy (ART) use prior to incarceration2 and higher HIV RNA levels, or viral load (VL), upon entry into correctional facilities.3 The transition between a correctional facility and the community can lead to disruption of ART use,4 and reincarceration compounds this problem.5 Incarceration is a time during which public health interventions can be deployed to diagnose HIV infection, initiate ART, and provide PLWHA with assistance linking or relinking to ongoing HIV medical care and treatment.6–8 However, fewer than 20% of prisons and jails currently provide Centers for Disease Control and Prevention (CDC)-recommended HIV discharge planning.4,9
Many more PLWHA are booked into jails—which are designed for short-term incarceration prior to trial—than into prisons each year.10,11 Because some of the factors associated with incarceration, such as substance use and homelessness, are also associated with disengagement from HIV care, jails could play an important role in public health efforts to reengage out-of-care persons.12,13 However, the rapid turnover of populations in jail systems makes implementation of interventions challenging.14
In King County, Washington, the health department and the largest Ryan White Part C–funded HIV clinic have implemented several programs designed to improve patient engagement in HIV care. These include a surveillance-based data to care program that utilizes HIV surveillance data to help engage PLWHA in care15,16; a clinic-based patient retracing program that uses clinical data to identify out-of-care clients, matches this to surveillance data, and then employs a linkage specialist to try to reengage them in care17; and a low-threshold clinic with intensive outreach assistance for the hardest-to-reach individuals.18 This low-threshold clinic provides HIV care on a walk-in basis, meal vouchers, phones, bus passes, and cash incentives for clients who do not engage in traditional HIV health care.18 At the end of 2014, an estimated 79% of diagnosed PLWHA in King County were virally suppressed.19 Nonetheless, an estimated 11% of HIV-diagnosed persons presumed to be living in King County were not engaged in HIV care in 2014 (defined as ≥ 1 HIV care visits).19 Currently, an HIV case manager located at the jail coordinates care by helping to engage the incarcerated PLWHA in care and scheduling appointments either during incarceration or upon release. However, once patients are released from jail, they can be lost to follow-up because of a lack of structured transitional care to bridge incarceration and release. Reaching these persons with interventions after release to promote engagement in HIV care is challenging and resource intensive. Improved coordination between the health department and local jails could be a way to locate and engage out-of-care individuals.
Our objectives were to determine the number of PLWHA incarcerated in King County jails in a calendar year; assess their key HIV care outcomes prior to booking, during incarceration, and after release; and assess booking and release patterns relevant to a potential intervention to improve postincarceration HIV care outcomes. To address these objectives, we matched county jail booking data with HIV surveillance data.
METHODS
In 2014, a total of 24 414 individuals were booked into either of the 2 King County jails included in this analysis: King County Correctional Facility and King County Regional Justice Center.11 We chose these jails for analysis because they house the majority of pretrial inmates in King County and they made data available for analysis. All patients are evaluated in an initial jail intake health screen that includes questions about medical, mental health, and dental problems as well as a focused examination for signs of communicable diseases. Jail Health Services, a division of Public Health—Seattle & King County (PHSKC), does not perform routine HIV testing. If a patient discloses that he or she is HIV infected during the intake screen, the nurse requests a medical clinic appointment for a complete medical assessment. Patients who acknowledge being on ART upon jail entry are continued on their regimens. Patients can initiate ART in jail in coordination with an HIV medical provider at the HIV clinic at Harborview Medical Center through an in-person appointment. However, HIV care appointments are only scheduled for patients who complete a medical assessment in the jail, and some are released from jail prior to completing the HIV clinic visit. The clinic at Harborview Medical Center also provides ongoing HIV care if patients remain incarcerated for an extended period of time, even if their usual community primary HIV provider is at an alternate clinic.
We obtained a data file from the King County Department of Adult and Juvenile Detention for all persons booked into a King County jail in 2014 with a unique jail identifier and information including name, date of birth (DOB), social security number (SSN), and dates of booking and release. We matched these data with public health HIV surveillance data, including the HIV Incidence and Core HIV Surveillance registries. An epidemiologist familiar with both data sources conducted the match. Initial linkages were made by matching full name and DOB, including any alias names and DOBs available in surveillance data. For those that did not match by full name and DOB, we attempted to match by systematically applying each of the following criteria:
full SSN and DOB,
last name and full SSN,
full SSN alone,
last 4 digits of SSN and last name, and
last name and DOB.
When alias names, DOBs, and SSNs were available, we also included them in these match criteria. We manually reviewed and verified all of the linkages resulting from a match on criteria other than full name and date of birth, either by medical record or by Accurint, a LexisNexis database that collates public records. PHSKC surveillance data are deduplicated upon creation of a new case record. This matching process did not identify any PHSKC surveillance data with 2 jail records and different unique jail identifiers. We then de-identified this information by removing names, DOBs, and SSNs.
This analysis focuses on the first incarceration in 2014 among individuals with diagnosed HIV at the time of first booking. Using HIV surveillance data, we compared the following demographic characteristics of incarcerated PLWHA with those of the general population of HIV-diagnosed persons in King County: age, gender, race/ethnicity, and HIV exposure risk category. We were not able to reliably identify patients who were transgender.
To assess HIV care and disease status at the time of jail booking, we identified each person’s most recent HIV RNA viral load prior to booking in the year prior to incarceration and most recent CD4 count result in the 2 years prior to incarceration. We assumed that persons were out of care if they had no CD4 count or VL laboratory test result reported in the year prior to incarceration and that persons were not virally suppressed if they had no VL reported in that time frame. In accordance with the definition used by the CDC and the National HIV/AIDS Strategy to monitor the HIV care continuum, we defined viral suppression as a VL of fewer than 200 copies per milliliter.20,21 We also evaluated CD4 and VL results reported during periods of incarceration to further evaluate HIV immunological and suppression status at the time of incarceration and assess what proportion of incarcerated PLWHA had any laboratory assessment during incarceration. To analyze postrelease outcomes, we examined timing of VL monitoring in the year after release, whether the patient was engaged in continuous care (defined as ≥ 2 HIV-related laboratory tests at least 3 months apart), and time to viral suppression in the year after release. To determine feasibility of and to inform the development of potential interventions, we examined the medical care facility associated with the most recent laboratory report prior to booking, the day of the week when the PLWHA was released from jail, the length of the incarceration, and the total number of incarcerations for each individual PLWHA in King County jails in 2014. We also examined HIV care outcomes by 3 racial/ethnic categories (non-Hispanic White, non-Hispanic Black, and Hispanic) for the proportion that were virally suppressed at booking, proportion virally suppressed within 6 months of jail release, and proportion engaged in continuous care.
We used the χ2 test to compare the characteristics of PLWHA incarcerated in jail in 2014 with those of the overall HIV-diagnosed population of PLWHA in King County in 2014 presumed not to be incarcerated and to evaluate the association between the number and length of incarcerations and proportion virally suppressed at 12 months. Length of incarceration was a categorical variable grouped into 4 categories (< 48 hours, 2–6 days, 7–13 days, ≥ 14 days). Number of incarcerations was a continuous variable that we dichotomized as 1 incarceration versus more than 1 incarceration. The χ2 test also compared racial/ethnic categories and CD4 count prior to incarceration, laboratory tests prior to incarceration, time to viral suppression following release, length of incarceration, and multiple incarcerations. We conducted these analyses using Stata Statistical Software version 14 (StataCorp LP, College Station, TX).
RESULTS
In 2014, a total of 202 diagnosed and reported PLWHA were booked into one or the other of the 2 largest King County jails. Compared with the overall population of 6788 HIV-diagnosed persons in King County who were not incarcerated, incarcerated persons were younger (15% vs 29% aged < 35 years; P < .001) and more likely to be men who have sex with men who also had injected drugs at the time of HIV diagnosis (8% vs 26%; P < .001; Table 1). The proportion of non-Hispanic Black individuals was lower in the overall population of HIV-diagnosed persons in King County than in the incarcerated population (19% vs 25%, respectively; P = .03). The proportion of persons whose most recently reported CD4 count was less than 200 cells per cubic millimeter was lower in the overall population of HIV-diagnosed persons in King County than in the incarcerated population (7% vs 25%; P < .001).
TABLE 1—
Characteristics of All People Diagnosed With HIV/AIDS Who Were Not Incarcerated in 2014 Compared With Those Known to Have Been Incarcerated at Least Once in 2014: King County, WA
| Characteristic | Not Incarcerated (n = 6778),a No. (%) | ≥ 1 Incarceration (n = 202),b No. (%) | P |
| Age, y | |||
| ≤ 34 | 999c (15) | 59d (29) | < .001 |
| 35–44 | 1535 (23) | 66 (33) | .001 |
| 45–54 | 2481 (37) | 61 (30) | .04 |
| ≥ 55 | 1763 (26) | 16 (8) | < .001 |
| Male gender | 6001 (89) | 178 (88) | .70 |
| Race/ethnicity | |||
| Non-Hispanic White | 4176 (62) | 107 (53) | .01 |
| Non-Hispanic Black | 1255 (19) | 50 (25) | .03 |
| Hispanic | 829 (12) | 22 (11) | .70 |
| Non-Hispanic Asian | 273 (4) | 4 (2) | .20 |
| Non-Hispanic American Indian/Alaska Native | 58 (1) | 4 (2) | .20 |
| Non-Hispanic Native Hawaiian/Pacific Islander | 23 (< 1) | 3 (2) | .004 |
| Multiracial | 164 (2) | 12 (6) | < .001 |
| HIV risk factor | |||
| MSM | 4580 (68) | 84 (42) | < .001 |
| IDU | 275 (4) | 31 (1) | .03 |
| MSM–IDU | 559 (8) | 52 (26) | < .001 |
| Heterosexual | 679 (10) | 11 (6) | .06 |
| Presumed heterosexuale | . . . | 6 (3) | . . . |
| Perinatal | 40 (1) | 3 (2) | .20 |
| Unknown | 625 (9) | 15 (7) | .30 |
| CD4 count in 2 y prior to first incarceration, cells/mm3 | |||
| < 200 | 475 (7) | 51 (25) | < .001 |
| 200–349 | 760 (11) | 31 (15) | .07 |
| 350–499 | 1245 (18) | 33 (16) | .50 |
| ≥ 500 | 3837 (57) | 75 (37) | < .001 |
| Missing | 461 (7) | 12 (6) | . . . |
Note. IDU = injection drug use; MSM = men who have sex with men; MSM–IDU = men who have sex with men and who also inject drugs.
In King County in 2014, there were 6980 people diagnosed with HIV living in King County. This number reflects those not incarcerated in 2014.
Those who were known to have an HIV diagnosis when first incarcerated. An additional 17 individuals were diagnosed with HIV after first booking of 2014.
All people younger than 24 years, including pediatric cases.
Aged 18–24 years, excluding pediatric cases.
Presumed heterosexual HIV risk factor is included in heterosexual risk factor for King County surveillance data although not in jail data.
Of the 202 PLWHA incarcerated, the majority (95%) had at least 1 HIV-related laboratory test (≥ 1 VL in the prior year or CD4 count in the prior 2 years) before their first booking, which by definition categorizes them as being in care (Table 2) and 54% of these laboratory tests were within 3 months of their booking (data not shown). One hundred and seventy-three (86%) had a VL reported to HIV surveillance in the year prior to incarceration. Viral suppression was lower among incarcerated persons (49%) at booking than among all King County diagnosed PLWHA not incarcerated (79%; P < .001). Forty individuals (20%) had a CD4 or VL at least once during incarceration, including 33 with viral load testing, 12 (37%) of whom were virally suppressed (Table 2). Of the 29 persons who did not have a VL reported in the year prior to booking, 9 (31%) had a VL during incarceration, and none of these 9 were virally suppressed. In the year after release, 170 (84%) had at least 1 VL and 126 (62%) were engaged in continuous HIV care in the year following release. Of the 202 PLWHA jailed, 98 (48%) and 126 (62%) achieved viral suppression within 6 and 12 months, respectively.
TABLE 2—
Linkage to Care and Viral Status Among People Living With HIV/AIDS and Incarcerated: King County, WA, 2014
| Variable | People Living With HIV/AIDS and Incarcerated (n = 202), No. (%) |
| Prior to First 2014 incarceration | |
| ≥ 1 VL test in prior year or CD4 in 2 y prior to first booking | |
| Yes | 191 (95) |
| No (defined as “out of care”) | 11 (6) |
| ≥ 1 VL in year prior | 173 (86) |
| Virally suppressed (VL < 200 copies/mL) in year prior to booking | |
| Yes | 99 (49) |
| No | 74 (37) |
| No VL reported (presumed not suppressed) | 29 (14) |
| During First 2014 incarceration | |
| VL or CD4 tested while incarcerated | |
| Yes | 40 (20) |
| No | 162 (80) |
| Virally suppressed (n = 33) | 12 (37) |
| After First 2014 incarceration | |
| ≥ 1 VL test in the year after release | |
| Yes | 170 (84) |
| Within 1 mo | 31 (18) |
| > 1 mo to ≤ 3 mo | 64 (38) |
| > 3 mo to ≤ 6 mo | 44 (26) |
| Within 12 mo | 31 (18) |
| No | 32 (16) |
| Engaged in continuous care in year following incarcerationa | |
| Yes | 126 (62) |
| No | 76 (38) |
| Viral suppression in year following release | |
| Virally suppressed (VL < 200 copies/mL) in year following releaseb | 126 (62) |
| Within 1 mo | 16 (8) |
| > 1 mo to ≤ 3 mo | 46 (23) |
| > 3 mo to ≤ 6 mo | 36 (18) |
| Within 12 mo | 28 (14) |
| No VL test in the year following release | 32 (16) |
| Virally nonsuppressed (VL > 200 copies/mL) in year following release | 44 (22) |
Note. VL = viral load.
Defined as ≥ 2 care visits or HIV-related laboratory tests ≥ 3 months apart in year.
Proportions by time periods are out of total (n = 202).
An estimated 6980 HIV-diagnosed persons were residing in King County in the same year, and 1466 (21%) were virally nonsuppressed19; thus, the population transiting through jail represented approximately 3% (202 of 6980) of all HIV-diagnosed adults in King County and, based on preincarceration VLs, 7% (103 of 1466) of virally nonsuppressed PLWHA in King County.
Of the 173 PLWHA who had a VL in the year prior to booking, the last VL was reported from one of the Ryan White Part C–funded clinics (50%), from a private medical provider (16%), or from jail (4%), but 19% were missing provider data. The majority of incarcerations (n = 125 [62%]) lasted less than 7 days and 76 (38%) lasted less than 48 hours. The majority of both bookings (n = 127 [63%]) and releases (n = 145 [72%]) occurred Monday through Thursday. Seventy-four PLWHA (37%) were reincarcerated at least once in the same calendar year.
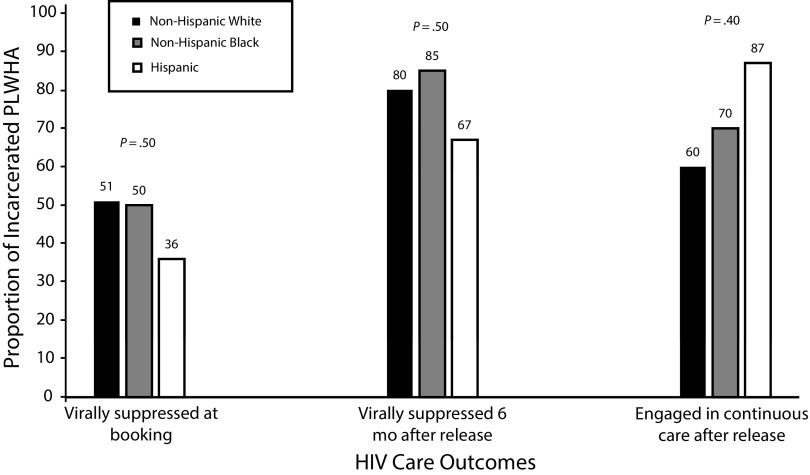
There was no significant association between number of incarcerations or length of incarceration and the likelihood of viral suppression 12 months after release (data not shown). Additionally, there were no significant associations between different races/ethnicities and CD4 counts prior to incarcerations, HIV-related laboratory tests prior to incarceration, time to viral suppression following release, length of incarceration, and multiple incarcerations (data not shown). Similar proportions of non-Hispanic Whites, non-Hispanic Blacks, and Hispanics were virally suppressed at booking and 6 months after release, and were engaged in continuous care after release (Figure 1).
FIGURE 1—
Specific HIV Care Outcomes Among People Living With HIV/AIDS (PLWHA) and Incarcerated, by Race/Ethnicity: King County, WA, 2014
Note. Viral suppression is defined as a viral load of < 200 copies/mL. Engaged in continuous care is defined as ≥ 2 care visits or HIV-related laboratory tests at least 3 months apart.
DISCUSSION
We found that approximately 3% of HIV-diagnosed persons in King County were booked into one of the 2 county jails included in this analysis in 2014, including approximately 7% of all virally nonsuppressed PLWHA in the area. Although almost 80% of diagnosed PLWHA in King County were virally suppressed, only about half of jailed PLWHA were suppressed in the period prior to their incarceration and only 62% achieved viral suppression within the year after their release. These data highlight the fact that, even in an area with very high levels of viral suppression, incarcerated PLWHA were disproportionately likely to be virally nonsuppressed.
Our findings confirm those of previous studies demonstrating poor pre- and postincarceration HIV outcomes among PLWHA,22 and add to the literature by quantifying the proportion of the virally nonsuppressed population of PLWHA in 1 geographic area that passes through jail each year. Another study has found a much larger percentage (14%) of the population being released from the jail system each year.1 Our finding of a lower proportion incarcerated in 1 year likely reflects, at least in part, the lower level of HIV morbidity in the Northwest region of the United States. Our study could have underestimated the number of PLWHA who are incarcerated, but a previous report also demonstrated that the numbers of PLWHA incarcerated tend to be lower in the Northwest than in other regions of the United States.23 Importantly, our study was limited to a single calendar year, and a larger percentage of PLWHA would be incarcerated with more years of observation. Despite the relatively small number of PLWHA incarcerated in King County jails, it is of public health significance because of the disproportionate number of virally nonsuppressed PLWHA.
Although the percentage of incarcerated individuals who were virally suppressed after incarceration (62%) was lower than the percentage of the general King County PLWHA population that was virally suppressed, it was higher than the preincarceration percentage among those later incarcerated (49%). It is possible that contact with the jail system linked some individuals who were previously out of care, although not at the same rate as those who were not incarcerated. A recent study by Schneider et al. demonstrated that criminal justice involvement was associated with improved HIV care outcomes in a cohort of young Black MSM, although repeated incarceration was associated with worse HIV care outcomes.24
Strengths and Limitations
Our study had important strengths and limitations. The population-based approach of linking jail booking data with HIV surveillance data is a major strength of this study. However, we were unable to identify on an individual level the reasons why particular individuals were not virally suppressed or engaged in continuous care, including the existence of comorbidities such as substance use disorders or mental health conditions, as these data are not included in surveillance data. This analysis was limited to 2 county jails in King County, which could lead to an underestimation of the proportion of PLWHA who lived in King County and were incarcerated in a calendar year. Because our study was focused on a single county, the generalizability is unknown. Lastly, our analysis could have been limited by incomplete matching between surveillance and jail data, and it did not include HIV-infected persons not yet diagnosed.
Public Health Implications
The results of our study have particular relevance for health departments, HIV clinics, and community-based organizations working to improve patient engagement in HIV care. Health departments and clinics from multiple regions of the United States have reported substantial challenges to locating out-of-care individuals.22–26 Our results suggest that jails could play an important role in a comprehensive data to care strategy. This would require jails and health departments or other agencies providing HIV care coordination services to work together to identify PLWHA at the time of jail booking and direct transitional care coordination. Because roughly two thirds of King County jail incarcerations are less than 7 days in length, a system is needed to identify and intervene as soon as possible after booking. Health information exchanges have shown promise in identifying out-of-care persons who present to emergency departments.27 An analogous information exchange between jail booking data and HIV surveillance data could be created to alert HIV care relinkage staff (i.e., case managers, disease intervention specialists, or patient navigators) to the presence of an out-of-care individual in jail, which could, in turn, guide an intervention. Additionally, performing HIV opt-out testing at jail booking may facilitate identification of PLWHA to increase the number of HIV-diagnosed individuals, particularly if these individuals do not otherwise engage with the medical system for HIV testing elsewhere.
The relatively high postincarceration levels of viral suppression among PLWHA in our study compared with other studies of incarcerated PLWHA reflect the population-level viral suppression in King County, which is higher than in most other US cities. This is likely attributable to a combination of high-quality HIV care and support system, an engaged community, health department programs, the significant efforts that have gone into improving the accuracy of surveillance data, and other factors specific to the Seattle area.25,26 Increasing collaboration between the health department and jails is a key next step in improving data to care programs in King County. Interventions such as EnhanceLink,27 that includes the COMPASS Program,14 and Project Bridge28 provide models for improving HIV care engagement among incarcerated populations. EnhanceLink’s package of services at 10 sites across the United States provides HIV testing and transitional linkage services, including provision of ART to clients while incarcerated, facilitating ART prescriptions upon release, and connecting PLWHA with community services upon release.29 In the COMPASS Program, operating in Rhode Island, community outreach workers are notified when someone with HIV is booked into jail and meet with that individual as soon as possible after intake. They provide case management while the client is in jail and following release to help link to HIV care, mental health care, and substance use disorder care in the community.14 A qualitative assessment of this program suggested that it enhanced previously available services in the community.14 The experience reported by the COMPASS Program and another demonstration project in Rhode Island, Project Bridge, illustrates that significant contact is required between the recently incarcerated and linkage services for positive results.
This analysis highlights the disparities evident in the incarcerated population, particularly for those who are younger and non-Hispanic Black. Although race/ethnicity was not associated with HIV care outcomes in this analysis, higher proportions of these vulnerable populations are incarcerated compared with other demographic groups. It is crucial that the public health system target interventions at populations who are disproportionately incarcerated by addressing comorbidities, such as mental illness or substance use disorders, that could have precipitated incarceration initially.
In conclusion, incarcerated PLWHA in King County are a vulnerable population, as evidenced by their poorer HIV health outcomes both pre- and postincarceration compared with the overall population of PLWHA in King County. Our future work is to identify mechanisms to facilitate real-time sharing of data and public health resources to facilitate transitional HIV care coordination for incarcerated PLWHA in King County.
ACKNOWLEDGMENTS
This work was supported by the University of Washington Center for AIDS Research (CFAR), a National Institutes of Health (NIH)-funded program (award no. P30AI027757) that is supported by the following NIH institutes and centers: the National Institute of Allergy and Infectious Diseases, the National Cancer Institute, the National Institute of Mental Health, the National Institute on Drug Abuse, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Heart, Lung and Blood Institute, the National Institute on Aging, the National Institute on General Medical Sciences, and the National Institute of Diabetes and Digestive and Kidney Diseases. M. C. Eastment was supported by the NIH STD & AIDS Research Training Program (T32AI07140).
We thank Ben Sanders, MD, MPH, for reviewing an earlier draft of the article, Amy Bennet, MPH, for her initial surveillance work and for reviewing an earlier draft of the article, and Mike West, MBA, for data management assistance.
HUMAN PARTICIPANT PROTECTION
This analysis, which was conducted to inform a public health program, used de-identified data and therefore was not classified as human participant research and was not subject to institutional review board review.
Footnotes
REFERENCES
- 1.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clements-Nolle K, Marx R, Pendo M, Loughran E, Estes M, Katz M. Highly active antiretroviral therapy use and HIV transmission risk behaviors among individuals who are HIV infected and were recently released from jail. Am J Public Health. 2008;98(4):661–666. doi: 10.2105/AJPH.2007.112656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan SY, Marsh K, Lau R, Pakianathan M, Hughes G. An audit of HIV care in English prisons. Int J STD AIDS. 2015;26(7):504–508. doi: 10.1177/0956462414545118. [DOI] [PubMed] [Google Scholar]
- 4.Iroh PA, Mayo H, Nijhawan AE. The HIV care cascade before, during, and after incarceration: a systematic review and data synthesis. Am J Public Health. 2015;105(7):e5–e16. doi: 10.2105/AJPH.2015.302635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meyer JP, Cepeda J, Springer SA, Wu J, Trestman RL, Altice FL. HIV in people reincarcerated in Connecticut prisons and jails: an observational cohort study. Lancet HIV. 2014;1(2):e77–e84. doi: 10.1016/S2352-3018(14)70022-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Avery AK, Ciomcia RW, Lincoln T et al. Jails as an opportunity to increase engagement in HIV care: findings from an observational cross-sectional study. AIDS Behav. 2013;17(suppl 2):S137–S144. doi: 10.1007/s10461-012-0320-0. [DOI] [PubMed] [Google Scholar]
- 7.Haley DF, Golin CE, Farel CE et al. Multilevel challenges to engagement in HIV care after prison release: a theory-informed qualitative study comparing prisoners’ perspectives before and after community reentry. BMC Public Health. 2014;14:1253. doi: 10.1186/1471-2458-14-1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lichtenstein B, Barber BW West Alabama AIDS Outreach Partnership Group. A partnership approach to providing on-site HIV services for probationers and parolees: a pilot study from Alabama, USA. J Int AIDS Soc. 2016;19(4 suppl 3):20868. doi: 10.7448/IAS.19.4.20868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Solomon L, Montague BT, Beckwith CG et al. Survey finds that many prisons and jails have room to improve HIV testing and coordination of postrelease treatment. Health Aff (Millwood) 2014;33(3):434–442. doi: 10.1377/hlthaff.2013.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.State of Washington Office of Financial Management-Criminal Justice. CrimeStats online: prison admissions for new admission. Access Washington: Statistical Analysis Center Washington State. 2014. Available at: http://wa-state-ofm.us/CrimeStatsOnline. Accessed February 9, 2017.
- 11.King County Dept of Adult and Juvenile Detention. Detention and alternatives scorecard. 2014. Available at: http://www.kingcounty.gov/∼/media/courts/detention/documents/KC_DAR_Scorecard_12_2014.ashx?la=en. Accessed February 9, 2017.
- 12.Khan MR, Golin CE, Friedman SR et al. STI/HIV sexual risk behavior and prevalent STI among incarcerated African American men in committed partnerships: the significance of poverty, mood disorders, and substance use. AIDS Behav. 2015;19(8):1478–1490. doi: 10.1007/s10461-015-1062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zelenev A, Marcus R, Kopelev A et al. Patterns of homelessness and implications for HIV health after release from jail. AIDS Behav. 2013;17(suppl 2):S181–S194. doi: 10.1007/s10461-013-0472-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nunn A, Cornwall A, Fu J, Bazerman L, Loewenthal H, Beckwith C. Linking HIV-positive jail inmates to treatment, care, and social services after release: results from a qualitative assessment of the COMPASS Program. J Urban Health. 2010;87(6):954–968. doi: 10.1007/s11524-010-9496-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dombrowski JC, Carey JW, Pitts N et al. HIV provider and patient perspectives on the development of a health department “data to care” program: a qualitative study. BMC Public Health. 2016;16(1):491. doi: 10.1186/s12889-016-3152-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dombrowski JC, Simoni JM, Katz DA, Golden MR. Barriers to HIV care and treatment among participants in a public health HIV care relinkage program. AIDS Patient Care STDS. 2015;29(5):279–287. doi: 10.1089/apc.2014.0346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bove JM, Golden MR, Dhanireddy S, Harrington RD, Dombrowski JC. Outcomes of a clinic-based surveillance-informed intervention to relink patients to HIV care. J Acquir Immune Defic Syndr. 2015;70(3):262–268. doi: 10.1097/QAI.0000000000000707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dombrowski JC, Ramchandani M, Moore A The MAX Clinic: a structural healthcare systems intervention designed to engage the hardest-to-reach persons living with HIV. Paper presented at: 11th International Conference on HIV Treatment and Prevention Adherence; May 9–11, 2016; Fort Lauderdale, FL.
- 19.HIV/AIDS Epidemiology Unit. Public Health–Seattle & King County, and the Infectious Disease Assessment Unit, Washington State Department of Health. HIV/AIDS Epidemiology Report 2015. Available at: http://www.kingcounty.gov/depts/health/communicable-diseases/hiv-std/patients/∼/media/depts/health/communicable-diseases/documents/hivstd/2015-hiv-aids-epidemiology-annual-report.ashx. Accessed February 10, 2017.
- 20.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas. 2014. HIV Surveillance Supplemental Report 2016, vol. 21 (no. 4). Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-21-4.pdf. Accessed February 10, 2017.
- 21.Office of National AIDS Policy. National HIV/AIDS Strategy for the United States: Updated to 2020. 2015. Available at: https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf. Accessed August 17, 2016.
- 22.Meyer JP, Cepeda J, Wu J, Trestman RL, Altice FL, Springer SA. Optimization of human immunodeficiency virus treatment during incarceration: viral suppression at the prison gate. JAMA Intern Med. 2014;174(5):721–729. doi: 10.1001/jamainternmed.2014.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maruschak LM. HIV in Prisons, 2001–2010. Washington, DC: US Dept of Justice, Office of Justice Programs; 2012. [Google Scholar]
- 24.Schneider J, Kozloski M, Michaels S et al. Criminal justice involvement history is associated with better HIV care continuum metrics among a population-based sample of young black MSM. AIDS. 2017;31(1):159–165. doi: 10.1097/QAD.0000000000001269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dombrowski JC, Buskin SE, Bennett A, Thiede H, Golden MR. Use of multiple data sources and individual case investigation to refine surveillance-based estimates of the HIV care continuum. J Acquir Immune Defic Syndr. 2014;67(3):323–330. doi: 10.1097/QAI.0000000000000302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buskin SE, Kent JB, Dombrowski JC, Golden MR. Migration distorts surveillance estimates of engagement in care: results of public health investigations of persons who appear to be out of HIV care. Sex Transm Dis. 2014;41(1):35–40. doi: 10.1097/OLQ.0000000000000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Booker CA, Flygare CT, Solomon L et al. Linkage to HIV care for jail detainees: findings from detention to the first 30 days after release. AIDS Behav. 2013;17(suppl 2):S128–S136. doi: 10.1007/s10461-012-0354-3. [DOI] [PubMed] [Google Scholar]
- 28.Zaller ND, Holmes L, Dyl AC et al. Linkage to treatment and supportive services among HIV-positive ex-offenders in Project Bridge. J Health Care Poor Underserved. 2008;19(2):522–531. doi: 10.1353/hpu.0.0030. [DOI] [PubMed] [Google Scholar]
- 29.Spaulding AC, Booker CA, Freeman SH et al. Jails, HIV testing, and linkage to care services: an overview of the EnhanceLink initiative. AIDS Behav. 2013;17(suppl 2):S100–S107. doi: 10.1007/s10461-012-0339-2. [DOI] [PubMed] [Google Scholar]