Abstract
Objectives. To quantify the inflation-adjusted costs associated with initial hospitalizations for firearm-related injuries in the United States.
Methods. We used the Healthcare Cost and Utilization Project Nationwide Inpatient Sample to identify patients admitted for firearm-related injuries from 2006 to 2014. We converted charges from hospitalization to costs, which we inflation-adjusted to 2014 dollars. We used survey weights to create national estimates.
Results. Costs for the initial inpatient hospitalization totaled $6.61 billion. The largest proportion was for patients with governmental insurance coverage, totaling $2.70 billion (40.8%) and was divided between Medicaid ($2.30 billion) and Medicare ($0.40 billion). Self-pay individuals accounted for $1.56 billion (23.6%) in costs.
Conclusions. From 2006 to 2014, the cost of initial hospitalizations for firearm-related injuries averaged $734.6 million per year. Medicaid paid one third and self-pay patients one quarter of the financial burden. These figures substantially underestimate true health care costs.
Public health implications. Firearm-related injuries are costly to the US health care system and are particularly burdensome to government insurance and the self-paying poor.
The United States has the highest rate of firearm homicides among developed countries. Although the US homicide rate is 7.0 times higher than that of other developed nations, gun homicide rates are 25.2 times higher.1 Between 2003 and 2010, 82% of all individuals killed by firearms in high-income countries were in the United States.1 In 2014 alone, firearms caused an estimated 33 700 deaths.2 However, that same year there were approximately 81 000 nonfatal firearm injuries, far exceeding the number of deaths.3 The financial burden on patients and the US health care system to care for these injuries is substantial and not frequently discussed.
To our knowledge, the most recent estimation of the medical costs of firearm injuries extends through 1997 and uses hospital data from only 2 states.4 Although estimations of the societal cost of firearm injuries have been made more recently, these values often include a broad range of metrics, such as productivity loss and pain and suffering, that make standardization or comparison of actual hospital costs difficult.5,6 The most recent estimations of these broader costs caused by firearm injuries extend through 2010.7 The frequency of firearm injuries likely generates a substantial financial burden to the health care system and to patients themselves.
We sought to determine the costs associated with the initial hospitalization of individuals with firearm-related injuries and where the burden of payment fell. Our goal was to better understand the financial burden of these injuries and to inform discussions of firearm-related public policy decisions and health care funding.
METHODS
We used the Healthcare Cost and Utilization Project Nationwide Inpatient Sample (NIS) from the Agency for Healthcare Research and Quality for 2006 to 2014. The NIS is the largest inpatient care database in the United States, contains data from about 8 million discharges each year, and is a stratified sample of approximately 20% of nonfederal, short-term, and general specialty hospitals in the United States.8 The NIS provides sample weights that allow national estimates to be derived. Details regarding NIS data have been published, and there are multiple internal validation quality measures.9
We identified admissions caused by firearm-related injuries using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM])10 codes. We included patients if they had an ICD-9-CM diagnosis code of E922.0–0.3, 0.8, 0.9, E955.0–0.4, E965.0–4, E979.4, E985.0–0.4, or E970.10 Because E-codes distinguish emergency conditions, we were able to identify injured patients. However, we could not identify patients being hospitalized subsequent to their initial injury. Thus we focused on initial hospitalization, which we defined as the first hospitalization of a patient injured by a firearm until discharge, as distinguished by the association of admission with an E-code.
We did not include patients treated and released from an emergency department (i.e., not admitted) or subsequent inpatient experiences not associated with an E-code (i.e., readmission). We derived the injury severity score using the ICD Programs for Injury Characteristic, a Stata module that translates diagnosis codes into standard injury categories and scores.11 We reported race/ethnicity according to the NIS classification, which included White, Black, Hispanic, Asian/Pacific Islander, Native American, and other. Because of small sample sizes of Asian/Pacific Islanders, Native Americans, and others, we combined these subgroups and included them in our “other” classification.
The primary outcome of interest was the cost associated with admissions for firearm-related injuries. The NIS contains information regarding the total charges billed for services and cost to charge ratios, allowing us to estimate costs. We inflation-adjusted costs to 2014 dollars using Consumer Price Index rates.
We performed unadjusted and adjusted analyses. We used the Student t test for normally distributed continuous data. We used χ2 analysis and analysis of variance to compare categorical variables. We considered P values of less than .05 to be significant. We used linear regression to determine adjusted costs on the basis of payer status. Regression variables included demographics, length of stay, injury severity scores, and hospital region; we controlled for center.
We used Stata SE version 14.1 (StataCorp LP, College Station, TX) for analyses. The NIS contains survey strata using US Census division, location, teaching status, ownership, and bed size. We applied survey weights according to Healthcare Cost and Utilization Project recommendations to create national estimates for the entire US population.
RESULTS
A total of 267 265 patients were admitted for firearm-related injuries from 2006 through 2014. Table 1 displays the patient demographics broken down by the primary payer status, including Medicare (6.0%), Medicaid (29.1%), private insurance (21.4%), self-pay (29.4%), and other (14.1%). Other insurance includes individuals who were not charged by the hospital and those with alternative forms of insurance. We found age, gender, race/ethnicity, median household income, injury severity, length of stay, injury intent (self-inflicted, assault, etc.), and discharge disposition to differ significantly (P < .001) between payer groups. Across all payer groups, patients were overwhelmingly male. Medicaid patients were younger, more likely to be non-White, and more likely to fall into a lower income quartile than were privately insured patients. Medicaid-insured individuals stayed in the hospital for an average of 3 days longer and their injuries were more likely to be from assault. Self-pay and privately insured individuals had the shortest average length of stay compared with other insurance groups.
TABLE 1—
Patient Characteristics and Outcomes by Payer Status: Healthcare Cost and Utilization Project Nationwide Inpatient Sample, United States, 2006–2014
| Characteristic | Medicare, No. (%) or Mean (95% CI) | Medicaid, No. (%) or Mean (95% CI) | Private Insurance, No. (%) or Mean (95% CI) | Self-Pay, No. (%) or Mean (95% CI) | Other, No. (%) or Mean (95% CI) |
| Count | 15 864 (6.0) | 77 224 (29.1) | 56 877 (21.4) | 78 020 (29.4) | 37 299 (14.1) |
| Age, y | 57 (55.8, 57.7) | 26 (25.7, 26.2) | 32 (31.2, 32.1) | 29 (29.4, 30.0) | 31 (30.2, 31.0) |
| Gender | |||||
| Male | 13 224 (83.4) | 66 344 (86.5) | 48 783 (86.2) | 72 285 (93.2) | 34 247 (92.5) |
| Female | 2 624 (16.6) | 10 381 (13.5) | 7 797 (13.8) | 5 266 (6.8) | 2 781 (7.5) |
| Race/ethnicity | |||||
| White | 8 732 (64.2) | 11 377 (16.6) | 21 100 (44.1) | 15 480 (22.9) | 8 255 (24.5) |
| Black | 3 634 (26.7) | 40 209 (58.8) | 18 069 (37.8) | 36 490 (53.9) | 15 994 (47.5) |
| Hispanic | 796 (5.9) | 13 230 (19.4) | 6 139 (12.8) | 12 407 (18.3) | 7 288 (21.6) |
| Other | 444 (3.3) | 3 555 (5.2) | 2 505 (5.2) | 3 310 (4.9) | 2 156 (6.4) |
| Median household income | |||||
| 0–25th percentile ($1–$37 999) | 6 989 (45.3) | 42 465 (58.0) | 22 027 (39.7) | 41 563 (55.3) | 18 006 (50.1) |
| 26th–50th percentile ($38 000–$47 999) | 4 256 (27.6) | 16 440 (22.5) | 14 720 (26.5) | 18 696 (24.9) | 8 703 (24.2) |
| 51st–75th percentile ($48 000–$63 999) | 2 750 (17.8) | 10 265 (14.0) | 11 483 (20.7) | 10 498 (14.0) | 6 415 (17.9) |
| 76th–100th percentile (≥ $64 000) | 1 421 (9.2) | 3 995 (5.5) | 7 296 (13.1) | 4 389 (5.8) | 2 791 (7.8) |
| ISS | |||||
| 0–9 | 9 885 (62.4) | 42 786 (55.4) | 34 474 (60.6) | 46 212 (59.2) | 21 611 (57.9) |
| 10–15 | 2 126 (13.4) | 14 491 (18.8) | 9 743 (17.1) | 15 495 (19.9) | 7 553 (20.3) |
| 16–25 | 3 209 (20.2) | 14 368 (18.6) | 9 982 (17.6) | 13 022 (16.7) | 6 333 (17.0) |
| ≥ 26 | 636 (4.0) | 5 559 (7.2) | 2 679 (4.7) | 3 292 (4.2) | 1 805 (4.8) |
| Average | 10 (9.5, 10.3) | 11 (11.2, 11.5) | 10 (10.0, 10.4) | 10 (10.0, 10.4) | 10 (10.3, 10.7) |
| Length of stay, d | 8 (7.4, 8.3) | 9 (9.4, 9.7) | 6 (6.2, 6.8) | 6 (5.3, 5.8) | 7 (7.0, 7.9) |
| Intent | |||||
| No E-code | 1 559 (9.8) | 6 726 (8.7) | 4 261 (7.5) | 4 525 (5.8) | 3 338 (9.0) |
| Unintentional | 4 757 (30.0) | 13 892 (18.0) | 15 821 (27.8) | 16 158 (20.7) | 6 785 (18.2) |
| Self-inflicted | 4 394 (27.7) | 3 583 (4.6) | 7 299 (12.8) | 4 869 (6.2) | 2 066 (5.5) |
| Assault | 4 144 (26.1) | 48 941 (63.4) | 26 675 (46.9) | 47 390 (60.7) | 23 293 (62.5) |
| Undetermined | 966 (6.1) | 3 961 (5.1) | 2 748 (4.8) | 4 947 (6.3) | 1 768 (4.7) |
| Disposition | |||||
| Routine discharge | 7 211 (45.5) | 53 188 (69.0) | 38 336 (67.4) | 60 833 (78.1) | 29 356 (78.9) |
| Transfer to short-term hospital | 628 (4.0) | 2 052 (2.7) | 2 171 (3.8) | 1 129 (1.5) | 759 (2.0) |
| Transfer to other (SNF, ICF) | 3 707 (23.4) | 8 762 (11.4) | 5 628 (9.9) | 3 295 (4.2) | 2 237 (6.0) |
| Home health care | 1 723 (10.9) | 6 795 (8.8) | 5 559 (9.8) | 3 723 (4.8) | 2 096 (5.6) |
| Left AMA | 143 (0.9) | 1 342 (1.7) | 318 (0.6) | 1 745 (2.2) | 439 (1.2) |
| Died in hospital | 2 415 (15.2) | 4 929 (6.4) | 4 786 (8.4) | 7 135 (9.2) | 2 315 (6.2) |
| Discharged to court, law enforcement | 5 (0.0) | 5 (0.0) | 0 (0.0) | 11 (0.0) | 10 (0.0) |
| Discharged alive, destination unknown | 16 (0.1) | 59 (0.1) | 45 (0.1) | 26 (0.0) | 15 (0.0) |
Note. AMA = against medical advice; CI = confidence interval; ICF = intermediate care facility; ISS = Injury Severity Score; SNF = skilled nursing facility.
Medicare and privately insured patients were more likely to be White and from higher income quartiles. Medicare patients sustained injuries that were significantly more likely to be self-inflicted, whereas privately insured patients comprised the highest proportion of unintentional injuries.
Patients with firearm injuries were overwhelmingly admitted to large urban teaching hospitals. Table 2 shows hospital characteristics by the primary payer status of the patient. We found that 43.0% of all initial hospital admissions for firearm injuries were in the South; the West and Midwest each had 20.0%, and the Northeast had 16%. Hospitals in the South had the highest proportion of self-pay patients and the lowest proportion of Medicaid patients. In fact, 48.3% of all self-pay patients in the study—but only 30.0% of Medicaid patients—were from this region.
TABLE 2—
Hospital Characteristics by Payer Status: Healthcare Cost and Utilization Project Nationwide Inpatient Sample, United States, 2006–2014
| Characteristic | Medicare | Medicaid | Private Insurance | Self-Pay | Other | P |
| Hospital region, no. (%) | < .001 | |||||
| Northeast | 1 997 (4.1) | 22 860 (47.4) | 8 522 (17.7) | 11 469 (23.8) | 3 381 (7.0) | |
| Midwest | 3 535 (6.2) | 15 609 (27.5) | 14 179 (25.0) | 17 237 (30.4) | 6 179 (10.9) | |
| South | 8 599 (7.3) | 24 276 (20.6) | 25 963 (22.0) | 39 564 (33.5) | 19 558 (16.6) | |
| West | 2 524 (4.5) | 18 359 (33.0) | 11 088 (19.9) | 13 678 (24.6) | 10 068 (18.1) | |
| Urban vs rural status of hospital, no. (%) | < .001 | |||||
| Urban | 15 078 (5.7) | 78 686 (29.6) | 56 747 (21.3) | 77 941 (29.3) | 37 468 (14.1) | |
| Rural | 1 381 (15.1) | 1 743 (19.1) | 2 318 (25.4) | 2 921 (32.0) | 757 (8.3) | |
| Teaching status, no. (%) | .73 | |||||
| Nonteaching hospital | 4 508 (9.0) | 11 352 (22.5) | 12 062 (24.0) | 15 975 (31.7) | 6 467 (12.8) | |
| Teaching hospital | 11 953 (5.3) | 69 066 (30.7) | 47 002 (20.9) | 64 887 (28.9) | 31 769 (14.1) | |
| Hospital bed size, no. (%) | .07 | |||||
| Small | 988 (8.4) | 3 581 (30.6) | 2 568 (21.9) | 3 123 (26.7) | 1 443 (12.3) | |
| Medium | 3 367 (6.1) | 15 348 (27.6) | 13 912 (25.0) | 16 300 (29.3) | 6 728 (12.1) | |
| Large | 12 087 (5.8) | 61 497 (29.6) | 42 597 (20.5) | 61 434 (29.6) | 30 053 (14.5) | |
| Hospital ownership, no. (%) | .03 | |||||
| Government or private | 7 984 (5.1) | 46 705 (29.6) | 32 820 (20.8) | 46 974 (29.8) | 23 321 (14.8) | |
| Nonfederal government (public) | 1 703 (6.3) | 7 714 (28.7) | 5 745 (21.4) | 7 803 (29.0) | 3 939 (14.6) | |
| Private not-for-profit (voluntary) | 5 203 (7.1) | 21 811 (29.6) | 16 910 (23.0) | 21 840 (29.7) | 7 830 (10.6) | |
| Private, investor owned (proprietary) | 1 391 (9.0) | 3 979 (25.6) | 3 178 (20.5) | 3 954 (25.5) | 3 023 (19.5) | |
| Private (collapsed) | 169 (13.7) | 213 (17.3) | 423 (34.2) | 306 (24.7) | 124 (10.1) |
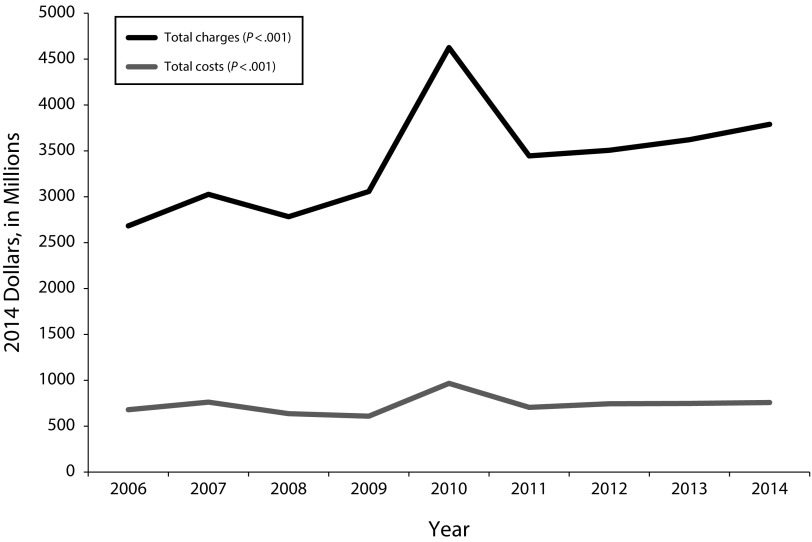
The inflation-adjusted costs of initial inpatient hospitalizations from 2006 through 2014 totaled $6.61 billion (Figure 1). There was a significant increase in both costs and charges over the study period (P = .001 for trend) but no increase in the number of initial hospitalizations. The largest proportion of costs was for patients with governmental insurance coverage, totaling $2.70 billion (40.8%) divided between Medicare (6.0%, $0.40 billion) and Medicaid (34.8%, $2.30 billion). Private insurers were responsible for $1.32 billion (20.0%), and self-pay individuals were in aggregate accountable for $1.56 billion (23.6%) of costs (Table 3).
FIGURE 1—
Total Costs and Charges Inflation-Adjusted to 2014 Dollars for Initial Inpatient Hospitalizations for Firearm-Related Injuries by Year: United States, 2006–2014
TABLE 3—
Costs and Charges Inflation-Adjusted to 2014 Dollars by Payer Status: Healthcare Cost and Utilization Project Nationwide Inpatient Sample, United States, 2006–2014
| Payer Status | Total Costs, $ | Average Cost per Incident (95% CI), $ | Total Charges, $ | Average Charges per Incident (95% CI), $ |
| Government | 2 696 252 699.68 | 29 911.63 (28 215, 31 607) | 10 219 841 009.15 | 106 630.30 (100 139, 113 121) |
| Medicaid | 2 298 583 423.09 | 30 951.92 (28 975, 32 928) | 8 822 077 248.95 | 110 970.60 (103 746, 118 195) |
| Medicare | 397 669 276.59 | 25 045.96 (23 000, 27 091) | 1 397 763 760.20 | 85 519.05 (78 587, 92 451) |
| Private | 1 324 518 448.60 | 23 150.88 (22 073, 24 228) | 4 668 398 519.47 | 79 630.85 (75 624, 83 636) |
| Self-Pay | 1 563 305 481.06 | 19 642.32 (18 779, 20 504) | 5 436 554 513.37 | 67 210.58 (63 298, 71 122) |
| Other | 997 236 040.59 | 25 802.52 (24 154, 27 450) | 3 505 339 038.58 | 89 818.38 (83 757, 95 879) |
| All | 6 611 291 019.46 | 24 746.10 (23 815, 25 676) | 23 927 812 262.96 | 86 700.16 (82 616, 90 784) |
Note. CI = confidence interval.
Average unadjusted costs per admission ranged from $19 642 for self-pay patients to $30 952 for Medicaid patients. This large difference in unadjusted costs was striking, considering the seemingly similar demographics between Medicaid and self-pay patients. We thus compared these 2 groups to determine whether there were alternative factors that may have accounted for the difference in hospital costs. However, after controlling for length of stay, injury severity score, age, region, race/ethnicity, and center, there was no significant difference in costs (P = .27).
DISCUSSION
From 2006 through 2014, the costs of initial hospitalizations for firearm-related injuries totaled almost $7 billion and averaged $730 million per year. Patients with no form of insurance accounted for approximately a quarter of these costs. In aggregate, the government was responsible for 41% of the total costs of initial hospitalizations for firearm injuries, amounting to almost $2.7 billion. The bulk of government costs was from Medicaid, which accounted for one third of the total financial burden. Medicaid patients also had the highest per incident costs, averaging more than $30 000 per initial hospitalization. Privately insured patients accounted for 20% of the total costs with an average incident cost of approximately $23 000.
The demographic distribution between different payer statuses was noteworthy, with the intent of firearm injury varying significantly between payer groups. Firearm injury with intent of assault ranged from 26.1% among Medicare patients to 63.4% among Medicaid patients, whereas self-inflicted injuries ranged from 4.6% among Medicaid patients to 27.7% among Medicare patients. This is consistent with previous epidemiological research of the intent of firearm injuries considering the racial and age compositions of payer groups.12
Our regression analysis demonstrated that there was no significant difference between Medicaid and uninsured individuals’ costs after controlling for variables that independently alter costs, such as injury severity and region. In fact, we found no significant difference in costs when only controlling for length of stay and center, suggesting that firearm-related cost burden is high for all injured patients and not affected by social or other factors.
These results indicate that firearm-related injuries place a particular burden on governmental payers and the poor. Just more than 80% of self-pay patients fell below the 50th income percentile; this group is unlikely to be able to absorb health care costs. In addition, without a third-party negotiator, these patients are often faced with full hospital charges when billed.
Furthermore, the government covers an enormous share of firearm injury costs. Hospitals that experience high volumes of these injuries, such as urban safety net hospitals, frequently provide unreimbursed care. In addition to uninsured individuals, patients who were not charged by hospitals incurred costs of just more than $200 million over the study period. These costs are often written off as losses to hospitals. As a result, government funding through county tax levies or block grant mechanisms is likely required to keep these hospitals solvent.
These values are a lower bounds estimate of the burden because they identify only costs associated with the initial inpatient hospitalization. These costs do not include the costs of readmissions, rehabilitation, long-term care, or disability. They also exclude the costs of those who were treated and released or died before admission. Finally, these health care costs do not include the broader social cost of firearm injuries such as quality-adjusted life-years or health-related productivity loss, which provide a broader but more abstract estimation.
It is important to note the inherent population differences between individuals killed by firearms and patients hospitalized for firearm injuries. Although suicide is the biggest cause of mortality from firearms, accounting for 60.7% of all firearm deaths in 2015, they accounted for only 8.4% of patients initially hospitalized for firearm injuries.3 Suicide patients typically do not survive long enough to be admitted and, thus, do not incur as many hospital costs. Furthermore, assault victims that survive long enough to be admitted typically survive; many assault victims die before hospitalization. Assault injuries accounted for 56.5% of initial hospitalizations and thus are associated with the highest costs.
Limitations
The limitations of this research are rooted in the information available at the NIS, which does not include information about the subsequent health care costs of firearm patients. Because we used ICD-9-CM codes, including E-codes, specifically related to firearm injuries to identify patients, it is possible that this excluded patients with firearm injuries who were classified with different codes. Although we correlated our numerical output with other sources, such as the Web-Based Injury Statistics Query and Reporting System and the Bureau of Justice, it is possible that such exclusions further underestimate the initial hospital costs for these patients.
In addition, the sensitive and unpredictable payment methods between hospitals, individuals, insurance companies, and the government make determining specific values of reimbursed and unreimbursed care very difficult. There is likely an additional burden placed on Medicaid because uninsured patients may be enrolled during their initial hospitalization; thus, subsequent care for their injuries end up being covered by governmental payers. However, we were not able to explore this with our data set because the NIS does not provide readmission information. Finally, the charge to cost conversion, although standardized and an accepted method of assessing cost, does not necessarily reflect actual costs, reimbursements, or capital outlays for patient care.
Public Health Implications
The financial burden of initial hospitalizations for firearm injuries is more than $700 million per year, and likely much greater. The responsibility for payment falls primarily on government payers and the uninsured. This information can be used both to inform public policy recommendations and to track the progress of implemented public policy measures.
Further research should evaluate the burden of costs beyond the initial hospitalization to include rehabilitation, long-term health care costs, and costs associated with time lost from work. In addition, understanding specific state and federal funding of hospitals dedicated to trauma and firearm injury treatment would allow a more realistic estimation of how governments may allocate expenditures for treating firearm injuries.
ACKNOWLEDGMENTS
The Stanford Medical Scholars Fellowship Program funded S. A Spitzer. We thank Daniel Vail for his assistance with data analysis.
HUMAN PARTICIPANT PROTECTION
No protocol approval was necessary because no human participants were involved in this study.
Footnotes
See also Kalesan, p. 638.
REFERENCES
- 1.Grinshteyn E, Hemenway D. Violent death rates: the US compared with other high-income OECD countries, 2010. Am J Med. 2016;129(3):266–273. doi: 10.1016/j.amjmed.2015.10.025. [DOI] [PubMed] [Google Scholar]
- 2.Kochanek KD, Murphy SL, Xu J, Tejada-Vera B. Deaths: final data for 2014. Natl Vital Stat Rep. 2016;65(4):1–122. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS). 2017. Available at: http://www.cdc.gov/injury/wisqars. Accessed January 12, 2017.
- 4.Cook PJ, Lawrence BA, Ludwig J, Miller TR. The medical costs of gunshot injuries in the United States. JAMA. 1999;282(5):447–454. doi: 10.1001/jama.282.5.447. [DOI] [PubMed] [Google Scholar]
- 5.Corso PS, Mercy JA, Simon TR, Finkelstein EA, Miller TR. Medical costs and productivity losses due to interpersonal and self-directed violence in the United States. Am J Prev Med. 2007;32(6):474–482. doi: 10.1016/j.amepre.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 6.Tasigiorgos S, Economopoulos KP, Winfield RD, Sakran JV. Firearm injury in the United States: an overview of an evolving public health problem. J Am Coll Surg. 2015;221(6):1005–1014. doi: 10.1016/j.jamcollsurg.2015.08.430. [DOI] [PubMed] [Google Scholar]
- 7.Lee J, Quraishi SA, Bhatnagar S, Zafonte RD, Masiakos PT. The economic cost of firearm-related injuries in the United States from 2006 to 2010. Surgery. 2014;155(5):894–898. doi: 10.1016/j.surg.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 8.Healthcare Cost and Utilization Project. NIS overview. Available at: https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed January 18, 2017.
- 9.Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract. 2002;5(3):143–151. [PubMed] [Google Scholar]
- 10.International Classification of Diseases, 9th Revision, Clinical Modification. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 11.Clark DE, Osler TM, Hahn DR. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. Available at: https://ideas.repec.org/c/boc/bocode/s457028.html. Accessed October 28, 2016.
- 12.Fowler KA, Dahlberg LL, Haileyesus T, Annest JL. Firearm injuries in the United States. Prev Med. 2015;79:5–14. doi: 10.1016/j.ypmed.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]