Abstract
Objectives. To describe secular trends in reported HIV diagnoses in Massachusetts concurrent with treatment access expansion.
Methods. We characterized cases of HIV infection reported to the Massachusetts HIV/AIDS Surveillance Program between 2000 and 2014 by sex, age, race/ethnicity, and exposure mode. We used Poisson regression to test the statistical significance of trends in diagnoses.
Results. Between 2000 and 2014, annual new HIV infections diagnosed in Massachusetts decreased by 47% (P < .001 for trend). We observed significant reductions in diagnoses among women (58% when comparing 2000 with 2014), men (42%), Whites (54%), Blacks (51%), and Hispanics (35%; P < .001 for trend). New diagnoses decreased significantly among men who have sex with men (19%), persons who inject drugs (91%), and heterosexuals (86%; P < .001 for trend). We saw statistically significant downward trends among all men by race/ethnicity, but the trend among Black men who have sex with men was nonsignificant.
Conclusions. Sustained reduction in new HIV diagnoses was concurrent with Massachusetts’s Medicaid expansion, state health care reform, and public health strategies to improve care access. A contributory effect of expanded HIV treatment and population-level viral suppression is hypothesized for future research.
Over the past 2 decades, the estimated annual incidence of HIV infection in the United States has been relatively stable.1 With improvements in clinical care, and the availability of highly active antiretroviral therapy since the mid-1990s, the number of people living with HIV infection has increased by more than 50%, presenting prevention challenges given the larger number of people who could potentially transmit HIV.2 However, recent data suggest decreasing rates of reported HIV cases, particularly among certain populations.3,4
The Obama Administration’s first National HIV/AIDS Strategy set an ambitious goal of reducing new HIV infections by 25% by 2015.5 This goal was partially predicated on recent findings suggesting that suppressing HIV with effective antiretroviral treatment decreases transmission by more than 95%.6 Incidence of HIV in several African countries has decreased in recent years,7 raising optimism that community mobilization to increase rates of HIV testing and earlier uptake of treatment may slow the spread of HIV in affected communities. However, recent data from several European countries8,9 found that local HIV incidence had not declined despite universal access to health care and antiretroviral therapy.
National surveys in the United States have suggested that more than half of Americans with HIV are either unaware of their HIV status or have not been fully engaged in HIV care, limiting the clinical and prevention benefits of effective treatment.10 In this report we discuss the experience of the Commonwealth of Massachusetts, which has seen a steady decrease in new HIV diagnoses over the past 15 years. We will explore several features of the state’s response to the epidemic, including the evolution of health care financing policy, support for rapid access to high-quality medical care, and targeted services to enhance engagement and retention in care as contributing to an apparent statewide treatment-as-prevention effect.
Massachusetts was the one of the first US states to advance novel health care financing mechanisms starting in 2001 with an expansion of the state’s Medicaid program to cover the health care and medication expenses of individuals with HIV infection (with and without an AIDS diagnosis) earning below 200% of the federal poverty level.11 State health care reform legislation beginning in 2006 further expanded treatment access for persons with HIV/AIDS. During this period, Massachusetts increased the number of publicly funded HIV tests performed annually by 43% (from 46 613 in 2000 to 66 422 in 2014; Liisa Randall and Monica Morrison, e-mail communication, March 23, 2016) and expanded funded HIV care linkage and retention services. We assessed trends in HIV diagnoses, HIV clinical indicators, and mortality among persons with HIV/AIDS for the period 2000 to 2014 in the context of the state’s health policy and program interventions.
METHODS
Since 1983, Massachusetts state regulations have required that physicians report all newly diagnosed cases of AIDS directly to the Massachusetts Department of Public Health.12 New diagnoses of HIV infection became a reportable condition in Massachusetts in 1999, initially reportable by unique identifier, then by name starting in 2007.12 All CD4+ T-lymphocyte (CD4+) test values and HIV plasma RNA (viral load) test results became reportable by clinical laboratories in 2012.13 Reporting of positive HIV diagnostic test results has been required of clinical and commercial laboratories by state regulation since 1999.12 Routine data quality assessments of the HIV/AIDS Surveillance Program are performed annually, including estimates of completeness through capture–recapture methods. Intrastate and interstate evaluation of duplication of case reports is conducted on an annual basis, and cases diagnosed and reported initially in another state were excluded from analysis. Routine matches to Massachusetts and out-of-state death reports are performed as an additional cross-check to verify completeness of reporting and to ascertain mortality. State epidemiologists routinely contact clinicians about incomplete case reports to eliminate missing data and clarify inconsistencies.
We characterized newly reported cases by sex, age, race/ethnicity, and exposure mode according to Centers for Disease Control and Prevention criteria.13 We performed calculation of frequencies and tests of significance with SAS version 9.3 (SAS Institute Inc, Cary, NC). Because of the relatively continuous reducing trends in prevalence, diagnosis, and mortality, we employed Poisson regression to test the statistical significance of the observed secular trends. We deemed trends to be significant at the P less than .05 level. We assessed model fit with the Pearson χ2 dispersion statistic. We used negative binomial models to adjust for overdispersion when indicated. All data were current as of March 1, 2016.
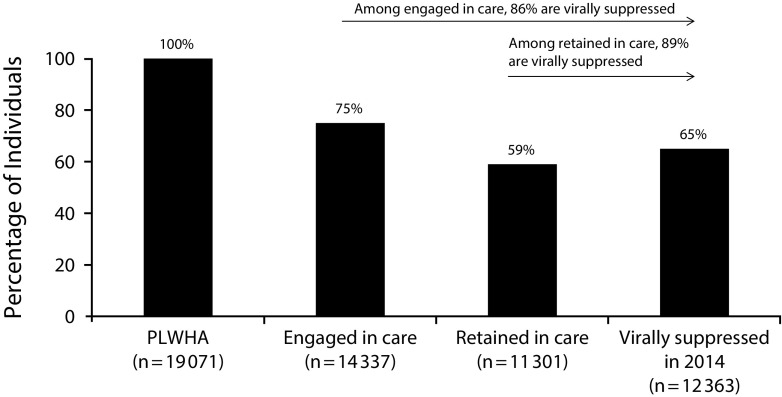
The Massachusetts HIV care cascade for calendar year 2014 is also presented here. The cascade presents evidence of care among individuals residing in and receiving care in Massachusetts diagnosed with HIV infection by the end of 2013 and alive in 2014. Engagement in care is defined as at least 1 CD4+ or HIV viral load laboratory result reported during 2014, with retention in care defined as 2 or more CD4+ or viral load results reported at least 3 months apart in 2014. Viral suppression is defined as fewer than 200 copies per cubic millimeter at the most recent laboratory blood sample drawn in 2014 (all cascade data current as of January 1, 2016).
RESULTS
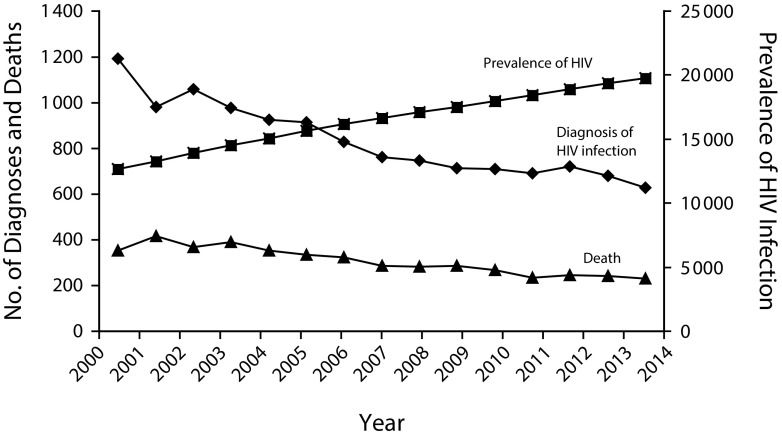
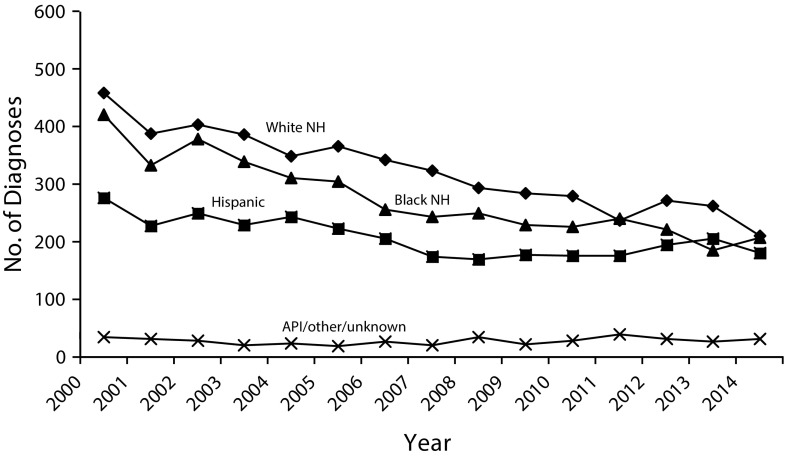
Between 2000 and 2014, annual new HIV infections diagnosed in Massachusetts decreased by 47%, from 1191 cases in 2000 to 629 in 2014 (P < .001 for trend; Figure 1). The statewide case rate, accounting for the increase in the Massachusetts population during this period, decreased by 50% (18.7 per 100 000 in 2000 to 9.3 per 100 000 in 2014). We observed substantial, statistically significant reductions in newly reported diagnoses among women (58%), men (42%), Whites (54%), Blacks (51%), and Hispanics (35%; P < .001; Figure 2). In addition, the numbers of new diagnoses decreased significantly across multiple exposure modes: men who have sex with men (MSM) had 19% fewer cases reported in 2014 compared with 2000; persons who inject drugs and heterosexuals had 91% (from 265 to 24) and 86% (from 205 to 29) fewer cases reported, respectively, during the same time period (P < .001). We saw statistically significant downward trends among all men by race/ethnicity, but the trend among Black MSM was nonsignificant. Trends appear to extend beyond the study period as evidenced by 2015 (624) and preliminary 2016 (465 as of November 1, 2016) case counts.
FIGURE 1—
HIV Infection, Deaths Among People Reported With HIV/AIDS, and HIV Prevalence by Year: Massachusetts, 2000–2014
Source. Massachusetts Department of Public Health HIV/AIDS Surveillance Program, data as of March 1, 2016.
FIGURE 2—
People Diagnosed With HIV Infection by Race/Ethnicity and Year of Diagnosis: Massachusetts, 2000–2014
Note. API = Asian/Pacific Islander; NH = non-Hispanic.
Source. Massachusetts Department of Public Health HIV/AIDS Surveillance Program, cases reported through January 1, 2016.
Although we observed a statistically significant reduction by age at diagnosis for the group aged 25 to 44 years (P < .001), the annual number of diagnoses among people aged 0 to 19 years and those aged 45 years or older did not change significantly. We observed a small but significant increase from 65 to 80 annual cases in the group aged 20 to 24 years (P < .001). Annual case counts for these populations and Massachusetts overall, as well as all P values for trends, are presented in Table 1.
TABLE 1—
Characteristics of Cases of HIV Infection Reported in Massachusetts: 2000–2014
| Characteristic | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Poisson Regression P for 15-y Trend | % Change 2000 vs 2014 |
| Sex | |||||||||||||||||
| Male | 823 | 667 | 712 | 658 | 648 | 663 | 595 | 544 | 544 | 545 | 502 | 497 | 525 | 510 | 475 | < .001 | −42 |
| Female | 368 | 313 | 347 | 318 | 278 | 250 | 234 | 218 | 202 | 169 | 208 | 195 | 194 | 169 | 154 | < .001 | −58 |
| Race/ethnicity | |||||||||||||||||
| White non-Hispanic | 459 | 388 | 403 | 387 | 349 | 366 | 342 | 323 | 294 | 285 | 280 | 237 | 271 | 263 | 211 | < .001 | −54 |
| Black non-Hispanic | 421 | 333 | 378 | 339 | 311 | 305 | 256 | 244 | 249 | 230 | 226 | 240 | 221 | 185 | 207 | < .001 | −51 |
| Hispanic | 277 | 228 | 249 | 230 | 243 | 223 | 205 | 175 | 169 | 177 | 176 | 176 | 195 | 205 | 180 | < .001 | −35 |
| API/other/unknown | 34 | 31 | 29 | 20 | 23 | 19 | 26 | 20 | 34 | 22 | 28 | 39 | 32 | 26 | 31 | .43 | −9 |
| Exposure category | |||||||||||||||||
| MSM | 355 | 291 | 319 | 321 | 291 | 350 | 346 | 299 | 297 | 321 | 295 | 273 | 323 | 309 | 288 | < .001 | −19 |
| IDU | 265 | 191 | 189 | 151 | 147 | 125 | 98 | 97 | 73 | 53 | 68 | 62 | 46 | 35 | 24 | < .001 | −91 |
| MSM/IDU | 30 | 32 | 35 | 35 | 29 | 24 | 21 | 22 | 29 | 18 | 25 | 20 | 22 | 14 | 15 | .71 | −20 |
| Heterosexual sex | 205 | 183 | 187 | 135 | 139 | 116 | 103 | 82 | 98 | 92 | 86 | 87 | 73 | 49 | 29 | < .001 | −86 |
| Other | 17 | 16 | 7 | 13 | 12 | 5 | 5 | 4 | 6 | 4 | 6 | 4 | 4 | 3 | 4 | .32 | −76 |
| Presumed heterosexuala | 119 | 102 | 123 | 136 | 113 | 99 | 105 | 85 | 80 | 65 | 89 | 78 | 100 | 94 | 82 | < .001 | −31 |
| Unknown | 200 | 165 | 199 | 185 | 195 | 194 | 151 | 173 | 163 | 161 | 141 | 168 | 151 | 175 | 187 | < .001 | −26 |
| Age at HIV diagnosis, y | |||||||||||||||||
| < 13 | 14 | 13 | 4 | 8 | 11 | 5 | 5 | 4 | 6 | 3 | 6 | 4 | 2 | 2 | 3 | .21 | −79 |
| 13–19 | 27 | 15 | 22 | 19 | 21 | 9 | 20 | 13 | 20 | 20 | 12 | 25 | 23 | 16 | 16 | .68 | −41 |
| 20–24 | 65 | 58 | 69 | 63 | 56 | 60 | 66 | 55 | 59 | 63 | 65 | 70 | 80 | 79 | 80 | < .001 | +25 |
| 25–29 | 138 | 101 | 126 | 98 | 95 | 92 | 90 | 85 | 105 | 71 | 70 | 73 | 99 | 101 | 91 | .045 | −34 |
| 30–34 | 204 | 178 | 187 | 165 | 135 | 146 | 102 | 89 | 89 | 97 | 88 | 88 | 98 | 88 | 86 | < .001 | −58 |
| 35–39 | 282 | 225 | 228 | 204 | 183 | 153 | 145 | 136 | 83 | 92 | 111 | 91 | 80 | 53 | 65 | < .001 | −77 |
| 40–44 | 212 | 171 | 183 | 168 | 171 | 191 | 149 | 129 | 124 | 112 | 97 | 112 | 85 | 74 | 68 | < .001 | −55 |
| 45–49 | 112 | 126 | 107 | 122 | 118 | 130 | 121 | 118 | 106 | 116 | 106 | 96 | 103 | 106 | 86 | .35 | −23 |
| ≥ 50 | 137 | 93 | 133 | 129 | 136 | 127 | 131 | 133 | 154 | 140 | 155 | 133 | 149 | 160 | 134 | .30 | −2 |
| Massachusetts total | 1191 | 980 | 1059 | 976 | 926 | 913 | 829 | 762 | 746 | 714 | 710 | 692 | 719 | 679 | 629 | < .001 | −47 |
Notes. API = Asian/Pacific Islander; IDU = injection drug user; MSM = men who have sex with men.
HIV-infected women whose only identified risk is sex with man of unknown HIV infection status or unknown HIV risk.
The annual number of deaths among persons living with HIV infection decreased by 35% (P < .001), from 353 to 231. During this period, the annual mean CD4+ count at first report of HIV infection rose 26% from 353 to 446 cells per cubic millimeter. Mean HIV seropositivity among those tested at state-funded HIV testing sites fell 44% from 0.9% in 2000 to 0.5% in 2014. The proportion of individuals diagnosed concurrently (within 2 months) with HIV infection and AIDS dropped from 35% to 22% during this period, and it is notable that the proportion of individuals diagnosed in Massachusetts who were non–US-born rose from 27% to 36%.
The Massachusetts HIV/AIDS Surveillance Program in 2014 documented a rate of viral suppression (65%) among individuals with HIV alive in 2014, higher than the national average, and a suppression rate of 89% among those retained in health care (Figure 3). Viral suppression in 2014 did not vary significantly by sex (63% of females, 66% of males), race/ethnicity (69% for White non-Hispanics, 63% for Black non-Hispanics, and 60% for Hispanics), or exposure category (70% for MSM and from 60% to 66% for other risk categories).14 We observed similar rates of viral suppression in 2014 in a random sample of more than 1400 individuals with HIV whose medical records were reviewed at 22 Massachusetts care sites; 89% of patients with at a least 1 care visit during 2014 had a suppressed viral load at most recent test that year.15
FIGURE 3—
Stages of HIV Care Among People Living With HIV/AIDS in Massachusetts: 2014
Note. PLWHA = people living with HIV/AIDS. Includes individuals diagnosed through 2013 and living in Massachusetts as of December 31, 2014, based on last known address, regardless of state of diagnosis. Viral load data missing on 27.5% of cases; 7.7% of cases have evidence of nonsuppression.
aLaboratory test result received by Massachusetts Department of Public Health.
DISCUSSION
During the past decade and a half, Massachusetts saw a substantial, statistically significant decrease in the annual number of new HIV diagnoses and deaths among persons with HIV/AIDS, as well as reduced HIV seroprevalence among publicly funded HIV tests and a reduced rate of concurrent HIV/AIDS diagnoses. Case rate calculation, accounting for the increase in the Massachusetts population during the study period, yields a 50% reduction when the overall case rates for 2000 and 2014 are compared. Mean CD4+ T-lymphocyte counts at the time of first report of HIV infection rose significantly, suggesting that observed reductions in diagnoses and deaths were not attributable to delays in diagnosing or reporting HIV infection. These reductions were observed across diverse demographic and exposure mode categories, and were of greater magnitude than noted nationally. Of particular note is the significant reduction in diagnoses among MSM, the most at-risk population in the United States, though similar reduction was not observed among Black MSM, the group currently most heavily impacted by the epidemic. The reduction in MSM cases occurred simultaneous to increasing rates of syphilis in this population, indicative of trends in sexual risk behavior parallel to national trends. We observed high rates of viral suppression both via laboratory reporting to the HIV/AIDS Surveillance Program and through systematic chart reviews.
We recognize that new diagnoses, which may reflect past infection, are not a perfect measure of HIV incidence. Recent estimations of diagnosis and reporting delay from multiple US jurisdictions suggest that, in 2011, median estimated time from infection to diagnosis was 3.6 years, compared with 5.4 years in 2003.16 Furthermore, Massachusetts has estimated HIV incidence by using the Centers for Disease Control and Prevention method that relies on the serologic testing algorithm for recent HIV seroconversion (STARHS) assay and analysis of patient testing history and has seen a decline in these estimates for the period 2007 to 2014 (annual values for this period: 816, 699, 405, 462, 528, 689, 674, and 533; B. J. e-mail communication, December 19, 2016) comparable in scale to changes in reported new diagnoses, increasing confidence that diagnoses reflect changes in actual incidence.
The specific reasons Massachusetts has been successful in reducing HIV diagnoses during the past decade and a half are not fully known, but Massachusetts during this period implemented a wide range of progressive health care and public health policies that may have contributed to this success. In 2001 Massachusetts expanded Medicaid coverage for single, childless, nondisabled persons with HIV infection earning less than 200% of the federal poverty level, greatly expanding full health care and medication coverage (all Food and Drug Administration–approved antiretrovirals) for this population. In 2003 to 2004, the state Massachusetts HIV Drug Assistance Program, substantially funded under the federal Ryan White Program and supplemented with state resources, shifted policy from direct medication purchase to health insurance premium and medication copayment coverage to expand health care access for persons with HIV infection. This policy change granted access to full health care coverage (under a range of commercial insurance carriers) and all Food and Drug Administration–approved antiretroviral medications for persons earning up to 500% of the federal poverty level. The effects of both the Medicaid expansion and the HIV Drug Assistance Program policy change were to support entry into and participation in routine medical care for persons with HIV independent of an AIDS diagnosis.
In 2006 Massachusetts became the first state to implement health care reform providing near-universal health insurance coverage (exceeding 96% since 2007).17 State health care reform mandated individual health insurance coverage, required large employers to offer health insurance to their employees, and expanded the commercial insurance coverage by providing subsidies for low-income individuals earning above the level of eligibility for Medicaid.
Massachusetts has a social and political environment supportive of HIV prevention and care programs, maintains a wide array of HIV/AIDS health and social services, and has partnered with academic institutions, medical providers, and community-based organizations in the development of innovative programs. Massachusetts implemented progressive HIV prevention policies including legal needle exchange (since 1993) and over-the-counter syringe sales (since 2006), school-based and community-based condom availability programs, and sexual health promotion programming. Massachusetts benefits from an extensive health care infrastructure providing HIV medical care, including 73 acute care hospitals and more than 50 community health centers operating in more than 280 sites. The Ryan White Program and state resources have been historically invested in this health care system to ensure access to medical care for persons with HIV/AIDS.
The Commonwealth has long-standing statutory protections of the rights of gay, lesbian, and bisexual persons and, since 2004, legal recognition of same-sex marriage, creating an affirming environment for stable relationships for MSM and other members of the lesbian, gay, bisexual, and transgender community. These protections and ecological factors may have improved health care access for this population and contributed to the observed reductions in HIV diagnoses.18 Modeling studies may be able to estimate the relative contribution of these programs and policies to the observed reductions in the number of persons diagnosed with HIV and deaths among persons with HIV/AIDS.
The limitations of this study are linked to the sources of the reported data. Massachusetts relies primarily on voluntary HIV testing and screening and clinical reporting of diagnosed infections to determine the incidence and prevalence of HIV/AIDS. Untested HIV-infected individuals would not be captured in these data. Case reporting may also be incomplete or delayed. However, the Massachusetts HIV/AIDS Surveillance Program performs at a high level of completeness meeting or exceeding Centers for Disease Control and Prevention standards,13 and is supported by electronic laboratory reporting of all positive HIV tests, all CD4+ T-lymphocyte counts, and all HIV viral load results, as well as matching to death data.12 Mean CD4+ T-lymphocyte counts of newly diagnosed patients have increased during this period, and state-supported testing volumes have increased substantially as well, while seropositivity and concurrent diagnosis rates have fallen. This is consistent with increasingly timely diagnosis and entry into care and suggests that the observed trends are not attributable to reporting bias.
In more recent years, the advent of Food and Drug Administration–approved use of antiretrovirals for the primary prevention of HIV infection, pre-exposure prophylaxis (PrEP), promises to enable individuals at risk to reduce the transmission of HIV, especially for MSM, transwomen, and serodiscordant heterosexual couples. Documented uptake of PrEP before 2014 in Massachusetts was low (for example, only 102 patients attending Fenway Health, the state’s primary care site serving the lesbian, gay, bisexual, and transgender community, were prescribed PrEP in 2013) and not likely to have significantly contributed to the observed reductions in diagnoses, but analysis of the further impact of PrEP on transmission after this period is indicated.
Massachusetts has seen a substantial decrease in new HIV diagnoses during the past 15 years, including reductions among men and women; White, Black, and Hispanic residents; MSM; heterosexuals; and persons who use injection drugs. These positive findings do not lead to complacency, because HIV transmissions continue to occur with the decrease in new diagnoses modest among MSM, the population associated with the largest number of new HIV infections in the state, and a decrease was not seen among Black MSM.
The specific epidemiological, resource, policy, and program factors that underpin these changes are not known, though they may be revealed through future modeling or evaluation studies. However, increased access to health care services, progressive HIV-related policies, and strong partnerships among public health authorities, community organizations, and academic institutions engaged in HIV prevention and care occurred concomitantly with these epidemiological changes. The prevention effect of expanded HIV treatment and population-level viral suppression is hypothesized and should be explored in future research.
ACKNOWLEDGMENTS
The collection of HIV/AIDS surveillance data reported in this article was supported under cooperative agreements between the Massachusetts Department of Public Health and the Centers for Disease Control and Prevention, Division of HIV/AIDS Prevention.
The authors wish to thank Kimberly Harris-McCoy for her analytic work on an earlier version of this article and R. Monina Klevens for her helpful review of and suggestions for improvements to this article.
Note. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
HUMAN PARTICIPANT PROTECTION
Institutional review board review was not required as all data were obtained under routine disease surveillance.
REFERENCES
- 1.Hall HI, Song R, Rhodes P, et al. HIV Incidence Surveillance Group. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prejean J, Song R, Hernandez A, et al. HIV Incidence Surveillance Group. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frieden TR, Foti K, Mermin J. Applying public health principles to the HIV epidemic—how are we doing? N Engl J Med. 2015;373(23):2281–2287. doi: 10.1056/NEJMms1513641. [DOI] [PubMed] [Google Scholar]
- 4.Des Jarlais DC, Arasteh K, McKnight C, et al. Consistent estimates of very low HIV incidence among people who inject drugs: New York City, 2005–2014. Am J Public Health. 2016;106(3):503–508. doi: 10.2105/AJPH.2015.303019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The White House Office of National AIDS Policy. National HIV/AIDS Strategy for the United States. 2010. Available at: https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas.pdf. Accessed March 17, 2017.
- 6.Cohen MS, Chen YQ, McCauley M, et al. HPTN 052 Study Team. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joint United Nations Programme on HIV/AIDS. Global AIDS Update 2016. Available at: http://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf. Accessed March 17, 2017. [PubMed]
- 8.Birrell P, Gill O, Delpech V, et al. HIV incidence in men who have sex with men in England and Wales 2001–10: a nationwide population study. Lancet Inf Dis. 2013;13(4):313–318. doi: 10.1016/S1473-3099(12)70341-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Le Vu S, LeStrat Y, Barin F, et al. Population-based HIV-1 incidence in France, 2003–08: a modelling analysis. Lancet Inf Dis. 2010;10(10):682–687. doi: 10.1016/S1473-3099(10)70167-5. [DOI] [PubMed] [Google Scholar]
- 10.Gardner EM, McLees M, Steiner J, del Rio C, Burman W. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaiser Commission on Medicaid and the Uninsured. Issue Brief: Section 1115 Waivers in Medicaid and the State Children’s Health Insurance Program: an overview, July 10, 2001. Available at: http://kaiserfamilyfoundation.files.wordpress.com/2001/07/section-1115-wiavers-in-medicaid-and-the-state-children-s-health-insurance-program-an-overview.pdf. Accessed November 28, 2014.
- 12. Summary of 105 CMR 300.000: Reportable diseases, surveillance, and isolation and quarantine requirements. Available at: http://www.mass.gov/eohhs/gov/departments/dph/programs/id/epidemiology/rdiq/reporting-diseases-and-surveillance-information.html. Accessed December 14, 2013.
- 13.Schneider E, Whitmore S, Glynn KM, Dominguez K, Mitsch A, McKenna MT Centers for Disease Control and Prevention. Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years—United States, 2008. MMWR Recomm Rep. 2008;57(RR-10):1–12. [PubMed] [Google Scholar]
- 14.Massachusetts Department of Public Health HIV/AIDS Surveillance Program. HIV care continuum fact sheet. 2016. Available at: http://www.mass.gov/eohhs/docs/dph/aids/2016-profiles/hiv-care-continuum-factsheet.pdf. Accessed March 23, 2016.
- 15.Day J, Reinhalter N, Musolino J, et al. Evaluating HIV clinical care quality in Massachusetts sites supported through the medical care management system: results from 2014 medical record review. JSI Research and Training Institute Inc. 2016. Available at: http://www.slideshare.net/jsi/evaluating-hiv-clinical-care-quality-in-massachusetts-sites-supported-through-the-medical-case-management-system-results-from-2014-medical-record-review. Accessed March 1, 2016.
- 16.Hall HI, Song R, Szwarcwald C, Green T. Time from infection with the human immunodeficiency virus to diagnosis, United States. J Acquir Immune Defic Syndr. 2015;69(2):248–251. doi: 10.1097/QAI.0000000000000589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Massachusetts General Laws Chapter 58 of the Acts of 2006. An Act Providing Access to Affordable, Quality, Accountable Health Care. Available at: https://malegislature.gov/Laws/SessionLaws/Acts/2006/Chapter58. Accessed November 28, 2014.
- 18.Hatzenbuehler ML, O’Cleirigh C, Grasso C, Mayer K, Safren S, Bradford J. Effect of same-sex marriage laws on health care use and expenditures in sexual minority men: a quasi-natural experiment. Am J Public Health. 2012;102(2):285–291. doi: 10.2105/AJPH.2011.300382. [DOI] [PMC free article] [PubMed] [Google Scholar]