Abstract
Objectives. To compare changes in food-purchasing knowledge, self-efficacy, and behavior after viewing nutrition education videos among Los Angeles, California Latinas responsible for household grocery shopping.
Methods. From February to May 2015, a convenience sample of 113 Latinas watched 1 video (El Carrito Saludable) featuring MyPlate guidelines applied to grocery shopping (1-video intervention) and another convenience sample of 105 Latinas watched 2 videos (El Carrito Saludable and Ser Consciente), the latter featuring mindfulness to support attention and overcome distractions while grocery shopping (2-video intervention). We administered questionnaires before and after intervention. A preselected sample in each intervention condition (n = 72) completed questionnaires at 2-months after intervention and provided grocery receipts (before and 2-months after intervention).
Results. Knowledge improved in both intervention groups (P < .001). The 2-video group improved more in self-efficacy and use of a shopping list (both P < .05) and purchased more healthy foods (d = 0.60; P < .05) at 2 months than did the 1-video group.
Conclusions. Culturally tailored videos that model food-purchasing behavior and mindfulness show promise for improving the quality of foods that Latinas bring into the home.
Overweight and obesity are a growing and pervasive threat to public health in the United States, with substantial costs to society and future generations.1–3 Latinas have among the highest rates of overweight and obesity (77%), and Latino children are disproportionately affected by obesity (22%).4 Mexican Americans are particularly at risk for obesity, with overweight or obesity reported in more than three fourths of Mexican American women, and obesity reported in one fourth of Mexican American children 6 to 11 years of age.5
Effective consumption-focused obesity intervention approaches seek to help with weight loss through changes in dietary habits and dietary intake.6 Factors related to household shopping behavior, such as planning ahead and being a conscientious nutritional shopper, can affect dietary intake.7,8 Educating Latinos/as about food-purchasing decisions that occur at the grocery store9–11 can change food planning decisions and in-store shopping practices, resulting in decreases in total mean calories and increases in purchases of fruits and vegetables.9,10,12,13 Improving nutritional knowledge and grocery list planning skills appears to be the main target for promoting healthier eating.14,15 Additional low-cost and effective interventions are needed to facilitate the purchase of healthy foods and subsequent access to a healthy diet at home.
Although efforts have been made to increase access to healthy food items in communities featuring economically disadvantaged populations, offering healthier options does not appear to be sufficient.16 Interventions focused on equipping “food gatekeepers” (i.e., those responsible for purchasing food and cooking family meals) to make decisions about food purchases have the potential to promote healthier eating habits in the home.17 Mindfulness-based interventions18 can support individuals to change their obesity-related eating behaviors.19
Considering previous work, it is unclear whether brief, culturally tailored videos can spur healthy change in grocery shopping behavior among Latinas who serve as food gatekeepers for their households. To address this limitation, we compared 2 interventions featuring culturally tailored videos designed to improve cognitive and behavioral skills and help Latinas prepare a shopping plan of action, acquire knowledge of healthy food choices, and focus attention on their intended grocery list while managing distractions during shopping. The El Carrito Saludable video uses the US Department of Agriculture’s MyPlate icon20 to guide food choices while shopping by translating the icon to food distribution in the grocery cart. The Ser Consciente video demonstrates a mindfulness18 approach (i.e., paying attention, on purpose, in the present moment, nonjudgmentally) while shopping to bolster self-regulation of attention and awareness to overcome distractions while shopping to support intentional decision-making.
We compared the effects of viewing El Carrito Saludable (1-video intervention) alone with those of viewing both El Carrito Saludable and Ser Consciente (2-video intervention). We hypothesized that the 2-video intervention would outperform the 1-video intervention on outcomes related to healthy food purchasing.
METHODS
We conducted a 2-group nonrandomized controlled study (with pretest, posttest, and 2-months posttest measurements) from February to May 2015. We recruited participants at Head Start programs and churches in East and South Los Angeles, California. Participants were Spanish- or English-literate Latinas aged 18 to 55 years who self-identified as the primary person responsible for family grocery shopping.
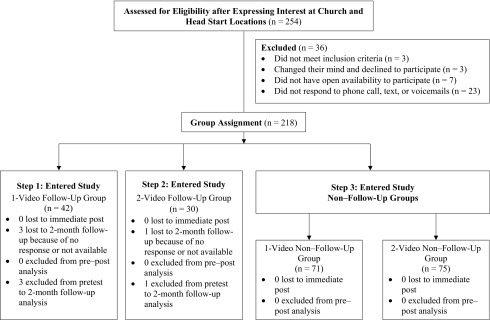
First, we enrolled a cohort for the 1-video condition to be followed for 2 months. Next, we enrolled a cohort for the 2-video condition to be followed for 2 months. Last, we consecutively enrolled a cohort for each intervention condition to complete pre- and posttest assessments only (Figure 1). To reduce potential bias, at enrollment, participants were unaware of which study condition they were assigned. We determined sample size (n = 218, of whom we preselected 72 for 2-month follow-up) on the basis of budget and to test intervention feasibility and promise. All participants completed the postintervention questionnaire. In the preselected 2-month follow-up sample, 94% completed the 2-month assessment (n = 68).
FIGURE 1—
Flow Chart of Study Enrollment and Steps in Intervention and Follow-Up Sample Implementation: Los Angeles, CA, 2015
Procedures
We notified participants of intervention location, date, and time. We asked the follow-up sample to bring 2 recent grocery store receipts representative of usual grocery shopping before the pretest and follow-up appointments. A bilingual–bicultural researcher orally administered the paper-and-pencil baseline questionnaire to groups of 15 to 25 participants, collected receipts from the follow-up sample, showed the video or videos in English or Spanish (language groups scheduled separately), and administered the posttest questionnaire.
We scheduled follow-up sample participants to complete the 2-month postintervention questionnaire at the original community sites. Participants received $25 for combined pre–post questionnaire completion. Follow-up sample participants received $25 for 2-month questionnaire completion plus $5 per grocery receipt at pretest and 2-month follow-up.
Interventions
El Carrito Saludable is a 13-minute video that author D. E. C. developed previously.11 It features a Latina nutritional health educator in a Latino supermarket shopping for foods by category while explaining the components of the MyPlate icon (grains, protein, fruits, vegetables, and dairy) and adapting them to the quadrants of the shopping cart. She discusses her choice to purchase culturally relevant options that are cost-efficient and of high nutritional value.
Ser Consciente is an 11-minute video that the study team developed to build on the lessons of El Carrito Saludable. It features a Latina mother and her child shopping in a Latino supermarket and demonstrates her use of mindfulness approaches while confronting challenges to making healthy choices. The video teaches viewers how to self-regulate attention and awareness while shopping to promote intentional decision-making. Consumer behavior and social cognitive theories guided both videos. The role of mindful attention in conscious decision-making also guided Ser Consciente.
Measures
We used questionnaires to collect sociodemographic information, including age; number of people in the household; number of children younger than 18 years in the household; country of birth; language preference derived from the question, “What languages do you speak?” and rated on a scale of 1 (only Spanish), 2 (mostly Spanish), 3 (both English and Spanish), 4 (mostly English), and 5 (only English) then recoded as Spanish monolingual versus other responses; and highest level of education completed (coded as completed less than high school vs completed high school or above). To better understand household composition, we asked participants whether anyone in their household is overweight or obese or has high blood pressure; if children living in the household eat meals at school (breakfast, lunch, and a snack), selecting all that apply (coded as yes or no); whether their family receives food stamps or Women, Infants, and Children benefits; and which family member determines the monthly grocery budget (coded as participant vs someone else).
We collected background information on the participants’ familiarity with nutritional concepts by asking whether they were familiar with the MyPlate icon (yes or no) and whether they considered a well-balanced diet as part of healthy eating (yes or no). We also asked participants, “When you are grocery shopping, how confident are you in your ability to select whole-grain bread?” and “When you are grocery shopping, how confident are you in your ability to select foods that are low in saturated fat?” We measured these items on a scale of 1 to 5 as follows: 1 (not at all confident), 2 (not confident), 3 (neither), 4 (confident), and 5 (very confident).
We quantified food-purchasing knowledge as a sum score of 5 true or false questions that the research team developed using the MyPlate icon and dietary recommendations,21 with higher scores indicating greater knowledge:
“When shopping for grains, it is better to choose whole wheat grains.”
“Frozen vegetables are included in MyPlate Method.”
“Fish, meat, and chicken can be included in the protein section of MyPlate Method.”
“Pasta and bread can be included in the grain section of MyPlate Method.”
“Yogurt, cheese, and butter can be included in the dairy section of MyPlate Method.”
We measured self-efficacy with the validated Self-Efficacy of Eating and Purchasing Healthy Foods Scale,22 which features 16 items rated on a 5-point Likert scale, with higher scores indicating greater self-efficacy. We assessed preparatory grocery shopping behavior with 2 questions (yes or no): “Do you use a shopping list when grocery shopping?” and “Do you eat before you go grocery shopping?” With guidance from a nutritional health consultant, we rated food items on grocery receipts (qualified, unqualified, or not specified) on the basis of nutritional value using federal dietary guidelines and MyPlate recommendations.21
Analysis
We compared the 1- and 2-video groups on demographic and behavior variables at baseline with the independent t test to identify potential differences. We adjusted statistical models for variables showing P < .05 difference by group at baseline, which included
A household member is overweight or obese.
A household member has high blood pressure.
The household receives Women, Infants, and Children benefits.
The children eat breakfast at school.
The children eat snacks at school.
The participant agreed that a well-balanced diet is part of healthy eating.
The participant has confidence in her ability to select whole-grain bread when shopping.
The participant has confidence in her ability to select foods with low saturated fat when shopping.
Among these covariates, 1 through 3 are time-invariant variables measured at baseline only, whereas 4 through 8 were measured at baseline and 2-month follow-up.
We tested between-group contrasts in outcomes and differences in changes across the assessment periods using mixed-effect models. By specifying both random and fixed effects, the model accounted for the correlation between repeated measures within individuals. The mixed-effect model included the effect of time, group, and a time by group interaction term while adjusting for covariates. We selected maximum likelihood to address missing data. With an iterative optimization algorithm, this approach yields unbiased parameter estimates by using all available data points under the assumption that data are missing at random.23
We obtained adjusted means and SEs for each time point of the 1- and 2-video conditions. We reported the Cohen effect sizes, d and h (the latter is derived from the arcsine transformation of probabilities), for continuous outcome and binary outcomes, respectively, as standardized measures.24 Guided by intent-to-treat principles, we assessed whether data provided evidence of a null effect or the equivalence in change between the 2 intervention conditions, according to original group assignment regardless of program attendance or missing data. We performed all statistical analyses using SAS version 9.3 (SAS Institute, Cary, NC).
RESULTS
Table 1 lists summary descriptive statistics comparing 1-video and 2-video conditions at baseline and comparing the follow-up sample with the original sample. At baseline, most participants were foreign born (82.1%), and 40.3% were monolingual Spanish speakers. Pretest differences between the 1- and 2-video conditions are noted in Table 1 and controlled in all subsequent analyses. Individuals in the follow-up sample were more likely to be monolingual Spanish speakers, to have completed high school, and to report having a family member who is obese or has high blood pressure.
TABLE 1—
Latina Food Shopper Characteristics at Baseline by Group and Total Sample Compared With Follow-Up Sample: Los Angeles, CA, 2015
| Variable | 1-Video (n = 113), Mean ±SD or No. (%) | 2-Video (n = 105), Mean ±SD or No. (%) | Total (n = 218), Mean ±SD or No. (%) | 2-Mo Follow-Up (n = 68), Mean ±SD or No. (%) |
| Age, y | 39.8 ±10.7 | 38.8 ±9.2 | 39.3 ±10.0 | 39.1 ±9.7 |
| No. people in the household | 4.5 ±2.0 | 4.5 ±1.3 | 4.5 ±1.7 | 4.4 ±1.5 |
| No. children 18 y or younger in household | 1.8 ±1.3 | 2.0 ±1.1 | 1.9 ±1.2 | 1.7 ±1.2 |
| Born in United States | 19 (16.8) | 20 (19.1) | 39 (17.9) | 18 (26.5) |
| Monolingual Spanish speaker | 48 (42.5) | 39 (37.9) | 87 (40.3) | 18 (26.5)b |
| High school education completed or above | 57 (50.4) | 58 (55.2) | 115 (52.8) | 46 (67.7)b |
| Household member is overweight or obese | 51 (51.5) | 28 (30.4)a | 79 (41.4) | 31 (58.5)b |
| Household member has high blood pressure | 49 (47.6) | 33 (34.0) | 82 (41.0) | 40 (67.8)b |
| Children eat breakfast at school | 34 (30.6) | 53 (51.0)a | 87 (40.5) | 30 (44.8) |
| Children eat snack at school | 19 (17.1) | 39 (37.5)a | 58 (27.0) | 21 (31.3) |
| Household receives food stamps | 33 (29.7) | 37 (35.6) | 70 (32.6) | 16 (23.9) |
| Household receives Women, Infants, and Children benefits | 30 (27.3) | 44 (41.9)a | 74 (34.4) | 15 (22.7) |
| Sets monthly household food budget | 67 (63.8) | 66 (64.7) | 133 (64.3) | 41 (63.1) |
| Considers a well-balanced diet part of healthy eating | 45 (39.8) | 64 (61.0)a | 109 (50.0) | 32 (47.1) |
| Familiar with MyPlate icon | 39 (35.5) | 38 (36.2) | 77 (35.8) | 22 (32.4) |
| Confidence in ability to select whole-grain bread when shopping | 3.8 ±1.3 | 4.2 ±1.0a | 4.0 ±1.2 | 4.0 ±1.2 |
| Confidence in ability to select foods with low saturated fat when shopping | 3.4 ±1.4 | 3.9 ±1.1a | 3.6 ±1.3 | 3.5 ±1.2 |
Note. Figures may not sum to 100% because of missing data or rounding error. 1-Video = El Carrito Saludable; 2-Video = El Carrito Saludable and Ser Consciente.
1-video and 2-video values are significantly different at P < .05 (2-sided).
Full sample and 2-month follow-up sample values are significantly different at P < .05 (2-tailed).
Postintervention Changes in Knowledge and Self-Efficacy
Table 2 provides results of unadjusted and adjusted models controlling for intervention groups’ pretest differences. In the adjusted model, pre–post improvements in food-purchasing knowledge were significant for both the 1-video and 2-video (P < .001) groups, and these changes were statistically equivalent between groups (d = 0.19; P > .05).
TABLE 2—
Video-Based Intervention Effects on Cognitive and Behavioral Measures of Food Purchasing Among Latina Food Shoppers: Los Angeles, CA, 2015
| Pretest (n = 218)a |
Posttest (n = 218) |
2-Mo Follow-Up (n = 68) |
||||||
| Outcomea | 1-Video (n = 113), Mean ±SE or % | 2-Video (n = 105), Mean ±SE or % | 1-Video (n = 113), Mean ±SE or % | 2-Video (n = 105) | Time × Group, Posttest, Cohen d or h | 1-Video (n = 39), Mean ±SE or % | 2-Video (n = 29), Mean ±SE or % | Time × Group, 2-Mo Follow-Up, Cohen d or h |
| Food-purchasing knowledge | ||||||||
| Unadjusted | 3.86 ±0.09 | 3.72 ±0.09 | 4.50 ±0.09*** | 4.56 ±0.09*** | 0.19 | 4.47 ±0.14*** | 4.54 ±0.16*** | 0.19 |
| Adjusted | 3.89 ±0.09 | 3.71 ±0.09 | 4.51 ±0.09*** | 4.54 ±0.09*** | 0.19 | 4.45 ±0.14*** | 4.54 ±0.16*** | 0.24 |
| Self-efficacy | ||||||||
| Unadjusted | 3.44 ±0.06 | 3.55 ±0.06 | 3.55 ±0.06 | 3.76 ±0.06** | 0.14 | 3.71 ±0.10* | 3.86 ±0.11** | 0.06 |
| Adjusted | 3.60 ±0.05 | 3.51 ±0.05 | 3.57 ±0.05 | 3.64 ±0.05** | 0.25* | 3.68 ±0.08 | 3.74 ±0.09* | 0.23 |
| Uses shopping lista | ||||||||
| Unadjusted | 60.0 | 54.7 | . . . | . . . | . . . | 61.4 | 90.5* | 0.70* |
| Adjusted | 56.0 | 61.1 | . . . | . . . | . . . | 59.2 | 92.4* | 0.57 |
| Eats before shoppinga | ||||||||
| Unadjusted | 70.6 | 54.1 | . . . | . . . | . . . | 79.4 | 85.0* | 0.45 |
| Adjusted | 73.5 | 55.7 | . . . | . . . | . . . | 81.5 | 82.9 | 0.39 |
| Percentage of qualified foodsa | ||||||||
| Unadjusted | 72.70 ±0.04 | 68.39 ±0.04 | . . . | . . . | . . . | 75.48 ±0.04 | 84.35 ±0.04** | 0.53 |
| Adjusted | 73.64 ±0.04 | 67.62 ±0.05 | . . . | . . . | . . . | 74.93 ±0.04 | 84.87 ±0.05** | 0.60* |
Note. 1-Video = El Carrito Saludable; 2-Video = El Carrito Saludable and Ser Consciente. Unadjusted and adjusted estimates obtained from mixed models.
n = 68 at baseline and 2-month follow-up for using a shopping list, eating before shopping, and percentage of qualified foods.
P < .05; **P < .01; ***P < .001 (2-tailed significance test values for time, group, and time by group effects).
As shown in the adjusted model, self-efficacy scores of the 2-video group improved by a mean of 0.13 (P < .01), whereas the 1-video group showed a mean reduction of −0.03, indicating relative improvement in the 2-video group (d = 0.25; P < .05).
Changes in Knowledge, Self-Efficacy, and Shopping Behavior
As shown in Table 2 (adjusted model), both groups improved in food-purchasing knowledge at 2-month follow-up. The 2-video group improved by a mean of 0.83 (P < .001), the 1-video group improved by a mean of 0.56 (P < .001), and changes were equivalent between groups (d = 0.24; P > .05). Only the 2-video group showed significant improvement in mean self-efficacy scores (P < .05) in the adjusted model, and this relative improvement over time did not reach statistical significance between groups (d = 0.23; P > .05).
We found significant improvements in grocery shopping preparation in the 2-video group. In the 2-video intervention, participants who used a shopping list increased 31.3% (P < .05) and participants who ate before grocery shopping increased 27.2% (P = .05) from baseline, whereas the corresponding change in the 1-video group was 3.2% and 8.0%, respectively. The difference in changes between the 2 groups did not reach statistical significance (P > .05), although the effect sizes were between medium and large, suggesting an artifact of the small sample size.
The percentage of qualified foods purchased on the basis of grocery store receipts in the 2-video group improved by a mean of 17.25 and in the 1-video group by a percentage mean of 1.29, indicating greater improvement in the 2-video group (h = 0.60; P < .05), as shown in the adjusted model.
DISCUSSION
In this community-based trial, we examined the effects of a 1-video health education intervention (focused on grocery shopping) and a 2-video health education intervention (focused on grocery shopping and mindfulness) on food-purchasing knowledge, self-efficacy, and grocery shopping behavior of low-income Latina adult food gatekeepers. Exposure to either nutrition education video condition improved food-purchasing knowledge that lasted through the 2-month assessment. The 2-video intervention extended improvements to self-efficacy, using a shopping list, and percentage of qualified foods purchased that lasted through the 2-month assessment. The 2-video intervention outperformed the 1-video intervention on percentage of healthy foods purchased at 2 months, which suggests a lasting change in food-purchasing behavior. The 2-video intervention was infused with the modeling of mindfulness for self-regulation of attention and awareness.
In 2-month follow-up adjusted models, the relative effect sizes for the 2- versus 1-video intervention were medium to large for several grocery shopping behavioral changes (0.39–0.60). We could not identify previous video-based intervention studies seeking to improve grocery shopping behaviors that provided effect sizes; however, meta-analyses evaluating e-health interventions for dietary behavior change (effect sizes ranged from 0 to 0.29 for fruit and vegetable servings and dietary fat)25 and brief computer-delivered interventions to decrease fat and increase fruit and vegetable consumption (effect sizes on knowledge = 0.36, self-efficacy = 0.16, and nutrition = 0.15)26 reported small to medium effect sizes. Most of these were multiple-session interventions with varying demographic groups and varying follow-up measurement points.
Previous research has shown that although nutrition knowledge is a factor in food choices, it is insufficient to produce behavior change.27,28 For example, previous studies have documented the importance of self-efficacy and specific behavioral skills in behavior change.29–33 Furthermore, mindfulness-related factors such as awareness, attention, and self-regulation elements have been noted as influential in food choice.34–37 Mindfulness-based interventions have documented benefits, including improved food selection, among individuals with eating disorders.38–41 However, these previous studies have been largely limited to clinical populations and counseling interventions. A recent community-based mindfulness intervention achieved stress reduction for general health promotion.42 To our knowledge, no previous studies have targeted mindfulness-related factors through a grocery shopping intervention for Latinos in the community. We advanced these findings by showing that healthy grocery shopping choices can be improved through a brief video-based intervention.
Our findings suggest that the 2-video condition illustrating how to sustain attention to purchasing healthier food options and respond to distractions may have helped curtail impulsive item selection. This finding is aligned with the basic skill of mindfulness, a nonreactive attentional stance to events occurring in the present moment. This stance is thought to bolster self-regulation18,43–45 and might increase an individual’s ability to remain focused on purchasing healthy foods. Previous studies have shown that inducing mindfulness can increase activation of attention networks and executive function, which are prominent cognitive features of conscious decision-making that counter habitual responses.46–48 Thus, integrating mindfulness cues during our education program had the potential to enhance attention and awareness, which can bolster conscious decision-making regarding food purchasing. This extends previous work on the impact of mindfulness on decision-making and health behavior.49 The intervention group that viewed the mindfulness education video demonstrated greater improvement in grocery shopping behaviors than did individuals in the 1-video intervention, and this process of change likely entails improved decision-making processes.
Our findings support earlier findings related to the suitability of the MyPlate method to educate individuals about healthy eating because it does not rely on complex nutritional information, numeracy skills, or measuring devices, which may complicate understanding already complex information.50 Our results also support the feasibility of focusing on grocery shopping education to change grocery shopping behavior to promote healthy eating—an emerging research field—and ameliorate environmental forces such as the grocery store setting, which tends to offer an overwhelming array of distracting alternatives to healthier options that disadvantaged populations with limited nutrition knowledge may not be prepared to decipher.9–11
Strengths and Limitations
Study strengths include combining food-purchasing education with mindfulness-informed educational messages regarding managing challenges faced in a shopping environment, the use of a community sample, and that participants were unaware of their assigned intervention condition at recruitment.
Although lack of randomization may jeopardize our findings, analytic methods controlled for all identified baseline differences between intervention groups. The risk of potential bias of confounding owing to unmeasured between-group differences still exists. Other limitations include small follow-up sample size, possible reporting bias of behavior and receipt selection, and baseline differences in variables in the preselected follow-up sample and total sample. Although generalizability of findings may be limited to populations with a similar demographic profile to study participants, it is important to note that study participants had a similar demographic profile (e.g., education, language spoken, and Hispanic group)51,52 to residents in the study communities.
Our study shows promise, yet further research is needed to test the efficacy of the intervention in a randomized controlled study to address threats to validity and rule out alternative explanations. Such a study should also include a larger follow-up sample, feature diverse samples of Latino populations, and investigate the mechanisms of action that lead to intervention effects.
Public Health Implications
Culturally tailored educational videos about food-purchasing choice and mindfulness delivered to Latina adults can improve the quality of household food, which can modulate the impact of food quality access on overweight and obesity. Videos allow wide dissemination, are not costly, and have low participant burden.
ACKNOWLEDGMENTS
The study and the development of the Ser Consciente video were funded by the USC Community Benefits and Sponsorship Program, Keck Medical Center, University of Southern California ([USC]; grant to H. A., principal investigator). The El Carrito Saludable video was developed with funding from the Hispanic Health Services Research Grant Program, Centers for Medicare and Medicaid Services, US Department of Health and Human Services (grant 1HOCMS331089 to D. E. C., principal investigator).
The following students or staff from USC assisted in data collection or grocery store receipt coding: Maria Alejandra Heman, Edith Jaurequi, Beatriz Sosa-Prado, Lucette Sosa, Connie Valencia, and Ruth Vergara. The following community partners facilitated participant recruitment in their respective locations and provided space for data collection and intervention delivery: Fathers John Moretta and David Matz of the Los Angeles Catholic Archdiocese; Phillipa Johnson, executive director, USC School for Early Childhood Education; and Theda Douglas, vice president, USC Government Partnerships and Programs. Intercultural Productions of Boston, Massachusetts developed the script and produced the Ser Consciente video and produced the English version of the El Carrito Saludable video. Teresa Abdala, mindfulness teacher, provided input during the conceptualization of the Ser Consciente video. Erick Lindberg provided editorial assistance on an early draft of the article.
HUMAN PARTICIPANT PROTECTION
The University of Southern California institutional review board approved the study protocol.
REFERENCES
- 1.Fryar CD, Carroll M, Ogden CL. Prevalence of overweight, obesity, and extreme obesity among adults: United States, 1960–1962 through 2011–2012. 2014. Available at: http://www.cdc.gov/nchs/data/hestat/obesity_adult_11_12/obesity_adult_11_12.pdf. Accessed September 15, 2015.
- 2.Centers for Disease Control and Prevention. Adult obesity causes & consequences. 2015. Available at: http://www.cdc.gov/obesity/adult/causes/index.html. Accessed September 15, 2015.
- 3.Gillman MW, Ludwig DS. How early should obesity prevention start? N Engl J Med. 2013;369(23):2173–2175. doi: 10.1056/NEJMp1310577. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Center for Health Statistics. Health, United States, 2014: with special feature on adults aged 55–64. Available at: http://www.cdc.gov/nchs/data/hus/hus14.pdf. Published 2015. Accessed September 15, 2015.
- 6.Casazza K, Fontaine K, Astrup A et al. Myths, presumptions, and facts about obesity. N Engl J Med. 2013;368(5):446–454. doi: 10.1056/NEJMsa1208051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crawford D, Ball K, Mishra G, Salmon J, Timperio A. Which food-related behaviours are associated with healthier intakes of fruits and vegetables among women? Public Health Nutr. 2007;10(3):256–265. doi: 10.1017/S1368980007246798. [Erratum in: Public Health Nutr. 2007;10(5):536] [DOI] [PubMed] [Google Scholar]
- 8.VanKim NA, Erickson DJ, Laska MN. Food shopping profiles and their association with dietary patterns: a latent class analysis. J Acad Nutr Diet. 2015;115(7):1109–1116. doi: 10.1016/j.jand.2014.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hunt MK, Lefebvre RC, Hixson ML, Banspach SW, Assaf AR, Carleton RA. Pawtucket Heart Health Program point-of-purchase nutrition education program in supermarkets. Am J Public Health. 1990;80(6):730–732. doi: 10.2105/ajph.80.6.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cortés DE, Millán-Ferro A, Schneider K, Vega RR, Caballero AE. Food purchasing selection among low-income, Spanish-speaking Latinos. Am J Prev Med. 2013;44(3 suppl 3):S267–S273. doi: 10.1016/j.amepre.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Cortés DE, Vega R, Domínguez D. Improving food purchasing selection among Spanish-speaking Hispanic families. Poster presented at: 142nd Annual Meeting of the American Public Health Association; November 19, 2014; New Orleans, LA. [Google Scholar]
- 12.Inman JJ, Winer RS. Where the Rubber Meets the Road: A Model of In-Store Consumer Decision Making. Cambridge, MA: Marketing Science Institute; 1998. [Google Scholar]
- 13.Milliron BJ, Woolf K, Appelhans BM. A point-of-purchase intervention featuring in-person supermarket education affects healthful food purchases. J Nutr Educ Behav. 2012;44(3):225–232. doi: 10.1016/j.jneb.2011.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fusillo AE, Beloian AM. Consumer nutrition knowledge and self reported food shopping behavior. Am J Public Health. 1977;67(9):846–850. doi: 10.2105/ajph.67.9.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hersey J, Anliker J, Miller C et al. Food shopping practices are associated with dietary quality in low-income households. J Nutr Educ. 2001;33(suppl 1):S16–S26. doi: 10.1016/s1499-4046(06)60066-3. [DOI] [PubMed] [Google Scholar]
- 16.Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff (Millwood) 2014;33(2):283–291. doi: 10.1377/hlthaff.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reid M, Worsley A, Mavondo F. The obesogenic household: factors influencing dietary gatekeeper satisfaction with family diet. Psychol Mark. 2015;32(5):544–557. [Google Scholar]
- 18.Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract. 2003;10(2):144–156. [Google Scholar]
- 19.O’Reilly GA, Cook L, Spruijt-Metz D, Black DS. Mindfulness-based interventions for obesity-related eating behaviours: a literature review. Obes Rev. 2014;15(6):453–461. doi: 10.1111/obr.12156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.US Department of Agriculture. MyPlate. 2015. Available at: http://www.choosemyplate.gov/about. Accessed September 11, 2015.
- 21.Office of Disease Prevention and Health Promotion. Dietary guidelines for Americans. 2015. Available at: http://health.gov/dietaryguidelines. Accessed September 15, 2015.
- 22.Pawlak R, Colby S. Benefits, barriers, self-efficacy and knowledge regarding healthy food; perception of African Americans living in eastern North Carolina. Nutr Res Pract. 2009;3(1):56–63. doi: 10.4162/nrp.2009.3.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Enders CK. Applied Missing Data Analysis. New York, NY: Guilford Press; 2010. [Google Scholar]
- 24.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 25.Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med. 2007;33(4):336–345. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Portnoy DB, Scott-Sheldon LA, Johnson BT, Carey MP. Computer-delivered interventions for health promotion and behavioral risk reduction: a meta-analysis of 75 randomized controlled trials, 1988–2007. Prev Med. 2008;47(1):3–16. doi: 10.1016/j.ypmed.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Worsley A. Nutrition knowledge and food consumption: can nutrition knowledge change food behaviour? Asia Pac J Clin Nutr. 2002;11(suppl 3):S579–S585. doi: 10.1046/j.1440-6047.11.supp3.7.x. [DOI] [PubMed] [Google Scholar]
- 28.Haack SA, Byker CJ. Recent population adherence to and knowledge of United States federal nutrition guides, 1992–2013: a systematic review. Nutr Rev. 2014;72(10):613–626. doi: 10.1111/nure.12140. [DOI] [PubMed] [Google Scholar]
- 29.Anderson ES, Winett RA, Wojcik JR, Winett SG, Bowden T. A computerized social cognitive intervention for nutrition behavior: direct and mediated effects on fat, fiber, fruits, and vegetables, self-efficacy, and outcome expectations among food shoppers. Ann Behav Med. 2001;23(2):88–100. doi: 10.1207/S15324796ABM2302_3. [DOI] [PubMed] [Google Scholar]
- 30.Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: social cognitive theory and nutrition behavior. Ann Behav Med. 2007;34(3):304–312. doi: 10.1007/BF02874555. [DOI] [PubMed] [Google Scholar]
- 31.Steptoe A, Perkins-Porras L, Rink E, Hilton S, Cappuccio FP. Psychological and social predictors of changes in fruit and vegetable consumption over 12 months following behavioral and nutrition education counseling. Health Psychol. 2004;23(6):574–581. doi: 10.1037/0278-6133.23.6.574. [DOI] [PubMed] [Google Scholar]
- 32.Shaikh AR, Yaroch AL, Nebeling L, Yeh MC, Resnicow K. Psychosocial predictors of fruit and vegetable consumption in adults: a review of the literature. Am J Prev Med. 2008;34(6):535–543. doi: 10.1016/j.amepre.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 33.Young EM, Fors SW, Hayes DM. Associations between perceived parent behaviors and middle school student fruit and vegetable consumption. J Nutr Educ Behav. 2004;36(1):2–8. doi: 10.1016/s1499-4046(06)60122-x. [DOI] [PubMed] [Google Scholar]
- 34.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007;23(11–12):887–894. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 35.Wardle J, Gibson EL. Impact of stress on diet: processes and implications. In: Stansfeld S, Marmot M, editors. Stress and the Heart: Psychosocial Pathways to Coronary Heart Disease. London, UK: BMJ Books; 2002. pp. 124–149. [Google Scholar]
- 36.Takeda E, Terao J, Nakaya Y et al. Stress control and human nutrition. J Med Invest. 2004;51(3–4):139–145. doi: 10.2152/jmi.51.139. [DOI] [PubMed] [Google Scholar]
- 37.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701. doi: 10.1037/a0016136. [DOI] [PubMed] [Google Scholar]
- 38.Godsey J. The role of mindfulness based interventions in the treatment of obesity and eating disorders: an integrative review. Complement Ther Med. 2013;21(4):430–439. doi: 10.1016/j.ctim.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 39.Daubenmier J, Kristeller J, Hecht FM et al. Mindfulness intervention for stress eating to reduce cortisol and abdominal fat among overweight and obese women: an exploratory randomized controlled study. J Obes. 2011;2011:651936. doi: 10.1155/2011/651936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Field T. Yoga clinical research review. Complement Ther Clin Pract. 2011;17(1):1–8. doi: 10.1016/j.ctcp.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 41.Hepworth NS. A mindful eating group as an adjunct to individual treatment for eating disorders: a pilot study. Eat Disord. 2011;19(1):6–16. doi: 10.1080/10640266.2011.533601. [DOI] [PubMed] [Google Scholar]
- 42.Galla BM, O’Reilly GA, Kitil MJ, Smalley SL, Black DS. Community-based mindfulness program for disease prevention and health promotion: targeting stress reduction. Am J Health Promot. 2015;30(1):36–41. doi: 10.4278/ajhp.131107-QUAN-567. [DOI] [PubMed] [Google Scholar]
- 43.Tang YY, Hölzel BK, Posner MI. The neuroscience of mindful meditation. Nat Rev Neurosci. 2015;16(4):213–225. doi: 10.1038/nrn3916. [DOI] [PubMed] [Google Scholar]
- 44.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 45.Black DS. Mindfulness-based interventions: an antidote to suffering in the context of substance use, misuse, and addiction. Subst Use Misuse. 2014;49(5):487–491. doi: 10.3109/10826084.2014.860749. [DOI] [PubMed] [Google Scholar]
- 46.Chiesa A, Calati R, Serretti A. Does mindfulness training improve cognitive abilities? A systematic review of neuropsychological findings. Clin Psychol Rev. 2011;31(3):449–464. doi: 10.1016/j.cpr.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 47.Stillman CM, Feldman H, Wambach CG, Howard JH, Jr, Howard DV. Dispositional mindfulness is associated with reduced implicit learning. Conscious Cogn. 2014;28(1):141–150. doi: 10.1016/j.concog.2014.07.002. [Corrigendum in: Conscious Cogn. 2015;31:124–125] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Whitmarsh S, Uddén J, Barendregt H, Petersson KM. Mindfulness reduces habitual responding based on implicit knowledge: evidence from artificial grammar learning. Conscious Cogn. 2013;22(3):833–845. doi: 10.1016/j.concog.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 49.Black DS, Sussman S, Johnson CA, Milam J. Trait mindfulness helps shield decision-making from translating into health-risk behavior. J Adolesc Health. 2012;51(6):588–592. doi: 10.1016/j.jadohealth.2012.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Camelon KM, Hådell K, Jämsén PT et al. The plate model: a visual method of teaching meal planning. J Am Diet Assoc. 1998;98(10):1155–1158. doi: 10.1016/s0002-8223(98)00267-3. [DOI] [PubMed] [Google Scholar]
- 51.Los Angeles Department of City Planning. Health atlas for the city of Los Angeles. 2013. Available at: http://planning.lacity.org/cwd/framwk/healthwellness/text/HealthAtlas.pdf. Accessed January 18, 2017.
- 52. Los Angeles Times. Mapping L.A. neighborhoods. 2009. Available at: http://maps.latimes.com/neighborhoods. Accessed January 18, 2017.