Abstract
Background
One of the features associated with pre-eclampsia is elevated liver transaminases. The reason this happens has not been fully described. However, the hepatocytes are not known to be spared by free radical injury. This study was conducted to examine the relationship between product of free radical injury (malondialdehyde) and transaminases in pre-eclamptic women.
Patients and Methods
A total of 98 and 115 pre-eclamptic and apparently normal pregnant women were selected from the booking clinic of Ladoke Akintola University of Technology Teaching Hospital, Osogbo. Non-pregnant women were selected from volunteered members of staff. Malondialdehyde (MDA), aspartate transaminase (AST) and alanine transaminase (ALT) analyses were determined on collected venous blood sample. Statistical analyses of variables were done using SPSS 17 taking level of significance to be p<0.05.
Results
Subjects with plasma AST between 10 and 20U/L had mean plasma MDA of 0.92µmol/l whereas those with plasma levels greater than 41U/L had mean plasma MDA of 4.72µmol/l. Similarly, Subjects with plasma ALT between 10 and 20U/L had mean plasma MDA of 0.86µmol/l, and subjects with plasma ALT greater than 51 U/L had mean plasma MDA of 4.71µmol/l. Positive correlation was observed between AST and ALT(r=0.79; p=0.047), between AST and MDA(r=0.690; p=0.061) as well as between ALT and MDA(r=0.571; p=0.049).
Conclusion
The elevated liver enzymes seen in women with pre-eclampsia may be due to free radical injury to the liver. Pre-eclamptic women without free radical injury did not have elevated transaminases
Keywords: Pre-eclempsia, free radical, malondialdehyde, alanine and aspartate aminotransaminases
Introduction
Pregnancy may be complicated with pre-eclampsia (1,2). A study in Nigeria found a prevalence of 6.5%2. The underlying pathogenesis is yet to be ascertained. However, there are suggested pathogeneses (3,4). Oxidative stress injury has been linked with pre-eclampsia (5,6). Despite the unknown pathogenesis, reduced blood flow to the placenta resulting in hypoperfusion and diffuse endothelia cell injury are considered as the central pathologic events (7). Adequate maternal-foetal exchange is a key requirement for a successful pregnancy (8). Early in pregnancy, maternal blood flow is absent from the precursors of the intervillous space (IVS). Therefore, a capillary circulation or simple diffusion performs the exchange of oxygen, nutrients and waste products (8). Around the 10th week of gestation, oxygen tension rises as a result of maternal blood flow into IVS.
With this, there is generation of reactive oxygen spices, free radical (oxidant) (8) which may lead to oxidative stress. Oxidative stress occurs when there is an imbalance in oxidant and antioxidant in excess of oxidant (9,10). Free radicals, because of their nature of attack on cellular organelles behave like oxidants. The attack of free radical on polyunsaturated membrane lipid gives hydroperoxide with subsequent production of malondialdehyde (MDA). This attack on membrane lipid is termed as lipid peroxidation, and malondiadehyde is now measured as the product of free radical injury on membrane lipid (11). The attack of free radical on polyunsaturated membrane lipid results in hydroperoxide with subsequent production of malondialdehyde (MDA).
One of the features associated with pre-eclampsia is elevated liver transaminases. Why this happenes has not been fully described (12,13). However, the hepatocytes are not known to be spared by free radical injury (14). This study, therefore, was designed to determine the association that may exist among plasma levels of aspartate amnino transaminase (AST), alanine amino transaminase (ALT) and malondialdehyde in women with preeclampsia.
Materials and Methods
The study site was Ladoke Akintola University of Technology Teaching Hospital, Osogbo, Nigeria. This study was a cross sectional and prospective cohort type.There were 98 pre-eclamptic and 115 apparently normal pregnant women recruited into the study. All subjects were in their second trimester. All selected subjects at first contact were all above 20 weeks of gestation. Ninety (90) age matching, apparently healthy non-pregnant women were also recruited from the volunteered members of staff as controls. Women previously known to be hypertensive and those with other complications of pregnancy such as gestational diabetes, multiple gestation, jaundice in pregnancy and cancer coexisting with pregnancy were excluded from the study. All recruited subjects were not on any medication other than routine self-prescribed haematinics. None of our pre-eclamptic women was on antihypertensive as they were all recruited from the booking clinic. Ethical clearance for the study was obtained from the Ethical Committee of Ladoke Akintola University of Technology Teaching Hospital, Osogbo in accordance with Helsinki declaration.
After taking an informed consent, about 10ml of venous blood was collected into lithium heparin containing specimen bottle. This was taken from antecubital fossa following aseptic procedure of venepuncture from each subject and control. Each batch of samples was centrifuged at 3000g for 5 min. Carefully, plasma was separated into plain screw cap specimen bottles. The plasma samples were used for MDA, AST and ALT assay. Malondialdehyde (MDA) was estimated using method of Satoh et al (15) because it is a thiobarbituric acid reacting substance. After the initial precipitation by trichloroacetic acid (TCA), the reaction of MDA with thiobarbituric acid gives a red coloured complex that is read spectrophotometrically at 532nm.. Aspartate amino transaminase was measured using the method of Bergeyer et al (16). This method was based on the principle that oxaloacetate is formed from the reaction of α- oxoglutamate and L-aspartate reduces NADH+ by the help of malate dehydrogenase. The reduced NADH+ is measured spectrophotometrically at 340nm. Alanine amino tranaminase was measured also spectrophometrically from reduced NADH+ formed from the reaction of α- oxoglutarate and L-alanine. This reaction is catalyzed by alanine amino transaminase (17). Each of these biochemical parameters was run in a batch of 30 samples. The data were entered and analysed using Statistical Package for the Social Sciences (SPSS) version 17.0 setting level of significance at p< 0.05.
Results
Table 1 shows the mean age distributions of the study groups. There was no statistically significant difference (P>0.05) in age of the study groups. There was no statistically significant difference (p>0.05) also in the mean values of body mass index within the groups. There was no statistically significant difference (p>0.05) in systolic blood pressure (SBP) (mmHg) among the study groups. Similar findings were observed in diastolic blood pressure (DBP) (mmHg).
Table 1.
Comparison of Mean±SD of Clinical Variables/Parameters
| Variables | Comparison | Mean ±SD | p-Values |
| Age (year) | NonP Vs NP NonP Vs PE NP Vs PE |
25.26±5.32 Vs 28.87±6.62 25.26±5.32 Vs 28.87±4.33 28.87±6.62 Vs 28.87±4.33 |
>0.05 >0.05 >0.05 |
| BMI (kg/m2) | NonP Vs NP NonP Vs PE NP Vs PE |
24.32±4.14 Vs 23.46±4.38 24.32±4.14 Vs 24.60±3.50 23.46±4.38 Vs 24.60±3.50 |
>0.05 >0.05 >0.05 |
| GA (week) | NP Vs PE | 24.28±5.81 Vs 24.03±1.73 | >0.05 |
| SBP (mmHg) | NonP Vs NP NonP Vs PE NP Vs PE |
121.60±12.20 Vs 117.83±13.03 121.60±12.20 Vs 166.15±9.40 117.83±13.03 Vs 166.15±9.40 |
>0.05 <0.03 <0.03 |
| DBP (mmHg) | NonP Vs NP NonP Vs PE NP Vs PE |
69.30±8.07 Vs 70.87±9.65 69.30±8.07 Vs 99.80±2.66 70.87±9.65 Vs 99.80±2.66 |
>0.05 <0.05 <0.05 |
NP-Normal pregnant women , PE- Pre-eclamptic women, NonP-Non pregnant women, * Statistically significant (p<0.05)
Table 2 shows comparison of mean of biochemical variables. Higher level, although not statistically significant (p>0.05) of AST(U/L), was observed in the normal pregnancy group compared with non-pregnant women. There was significantly higher value (p<0.03) of AST (U/L) in pre-eclamptic women compared with non-pregnant women. Also, significantly higher value (p<0.05) of AST was observed in pre-eclamptic group than in the normal pregnancy group. Similar findings were observed when ALT was compared among the study groups. Statistically significant higher level of plasma MDA (µmol/l) was observed in normal pregnancy group compared with non-pregnant group. In the same vein, significant (p<0.0001) higher plasma level of MDA (µmol/l) was observed in women with pre-eclampsia (3.00±2.21) compared with non-pregnant women. Furthermore, plasma MDA (µmol/l) was found to be significantly higher (p<0.0001) in pre-eclamptic group than in the normal pregnancy group.
Table 2.
Comparison of Mean±SD of Biochemical Parameters.
| Variables | Comparison | Mean ±SD | p-Values |
| AST (U/L) | NonP Vs NP NonP Vs PE NP Vs PE |
12.32±6.45 Vs 19.15±8.69 12.32±6.45 Vs 34.75±24.75 19.15±8.69 Vs 34.75±24.75 |
>0.05 <0.03 <0.05 |
| ALT (U/L) | NonP Vs NP NonP Vs PE NP Vs PE |
8.05±4.19 Vs 15.97±5.41 8.05±4.19 Vs 37.51±23.89 15.97±5.41 Vs 37.51±23.89 |
>0.05 <0.03 <0.05 |
| MDA(µmol/l) | NonP Vs NP NonP Vs PE NP Vs PE |
0.96±0.68 Vs 1.65±0.62 0.96±0.68 Vs 3.00±2.21 1.65±0.62 Vs 3.00±2.21 |
<0.05 <0.0001 <0.0001 |
NP-Normal pregnant women, PE- Pre-eclamptic women, NonP-Non pregnant women, * statistically significant (p<0.05)
Plasma AST and ALT in pre-eclamptic subjects were divided into different ranges with their corresponding mean MDA values (Table 3). There was corresponding increase in MDA with the increase in AST and ALT.
Table 3.
Different Ranges of AST and ALT with their Corresponding Mean Plasma MDA Values in Pre-eclamptic Subjects.
| Range | Category | Mean MDA(µmol/l) | |
| AST (U/L) | 10–44.75 | 10–20 | 0.92 |
| 21–30 | 1.89 | ||
| 31–40 | 3.61 | ||
| >41 | 4.72 | ||
| ALT(U/L) | 13.62–71.40 | 10–20 | 0.86 |
| 21–30 | 1.12 | ||
| 31–40 | 3.20 | ||
| 41–50 | 4.61 | ||
| >51 | 4.71 |
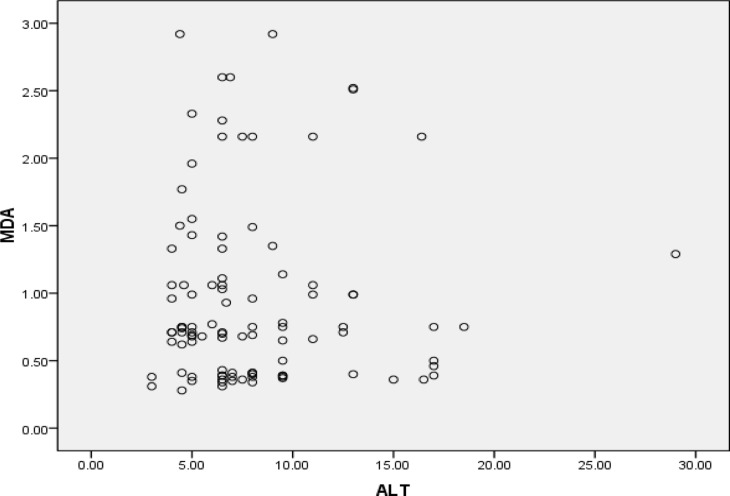
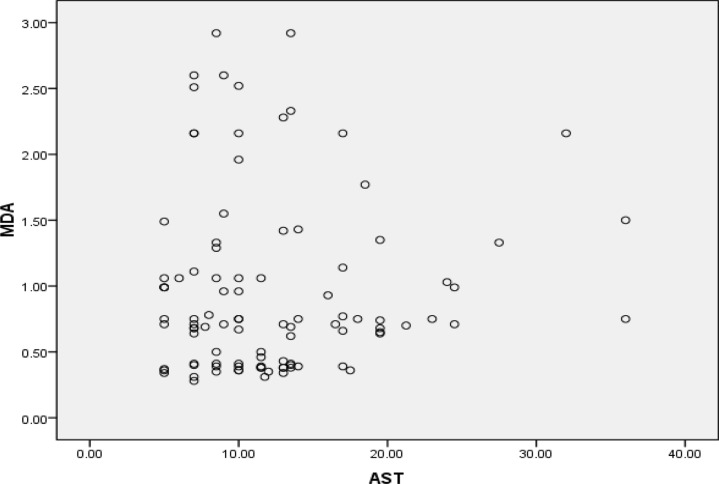
Table 4 shows correlation of biochemical parameters in pre-eclamptic subjects. There was a positive correlation between gestational age (GA/wk) and AST between GA and ALT and between GA and MDA. Positive correlation were observed also between AST and ALT between AST and MDA as well as between ALT and MDA. Correlations of MDA and AST as well as with ALT are represented also in Figures 1 and 2.
Table 4.
Correlation of Variables in Pre-Eclamptic Women.
| Age | BMI | GA | AST | ALT | MDA | |
| Age | 1 | r=−0.489 p=0.070 |
r=−0.930 p=0.009 |
r=0.451 p=0.076 |
r=0.152 p=0.128 |
r=0.950 p=0.006 |
| BMI | r=−0.489 p=0.070 |
1 | r=0.788 p=0.06 |
r=0.713 p=0.037 |
r=0.571 p=0.057 |
r=0.689 p=0.045 |
| GA | r=−0.930 p=0.009 |
r=0.788 p=0.06 |
1 | r=0.654 p=0.057 |
r=0.843 p=0.020 |
r=0.659 p=0.09 |
| AST | r=0.451 p=0.076 |
r=0.713 p=0.037 |
r=0.654 p=0.057 |
1 | r=0.790 p=0.047 |
r=0.690 p=0.061 |
| ALT | r=0.152 p=0.128 |
r=0.571 p=0.057 |
r=0.843 p=0.020 |
r=0.790 p=0.047 |
1 | r=0.571 p=0.049 |
| MDA | r=0.950 p=0.006 |
r=0.689 p=0.045 |
r=0.659 p=0.09 |
r=0.690 p=0.061 |
r=0.571 p=0.049 |
1 |
Figure 1.
Correlation of Plasma MDA and ALT
Figure 2.
Correlation of Plasma MDA and AST
Discussion
The age differences among our subjects and controls were not significant. This resulted in good unbiased comparison of our biochemical parameters because of the influence of advancing age on plasma MDA. Malondialdehyde has been observed to be increasing with age (18). Influence of body weight on MDA (19) was also eliminated since body mass indexes of our subjects and controls were similar. The addictive contributions of body weight on these selected parameters was eliminated. As pregnancy advances, there are many metabolic changes that accompany it, and these occur in both normal and complicated pregnancies. Gestational ages of recruited normal and pre-eclamptic women were similar. There was no statistically significant difference. This has also helped to eliminate the influence of pregnancy advancement on our analyzed biochemical parameters. Aspartate16, alanine transaminases (20) and malondialdehyde (21) have been found to increase as pregnancy advances. One of the criteria in diagnosing pre-eclampsia is elevated blood pressure (22). Our study found significantly higher values of systolic and diastolic blood pressure in pre-eclamptic group compared with normal pregnant group and non-pregnant controls. This has given us a fair basis for truly recruiting these subjects as clinical cases of pre-eclampsia.
In our study, the observed increase in plasma malondialdehyde levels in pre-eclamptic women compared with normal pregnant and non-pregnant women is in agreement with a similar study which reported significantly elevated levels of malondialdehyde in both normal and pre-eclamptic pregnant women (23). This may be due to overwhelming free radical injury or insufficient antioxidant status in this group of people. Free radical injury can affect many organs in the body irrespective of its origin. It can attack cellular membrane of organs with production of MDA as an intermediate product. This was measured based on an unstable nature of free radical itself in the body system (24). The damage to cellular membrane allows cell contents to be released in the blood, degree which depends on the severity of membrane damage. There is no study so far in the literature to show specificity of damage to a particular organ by free radical. Therefore, its effect on hepatocytes may be accessed through plasma liver enzymes (transaminases). The transaminases (AST, ALT) are markers of hepatocellular injury. It should be born in mind that aspartate amino transaminase is present in other tissues like cardiac muscle, skeletal muscle and red cells. Therefore, the study was also designed to measured Alanine amino transaminase, a cytosolic enzyme which is found in its highest concentrations in the liver and is more speci.c to the liver.
This study observed a higher level of AST and ALT in pre-eclamptic women compared with normal pregnant and non-pregnant women. This is already an established fact; HELLP (haemolysis, elevated liver enzymes and low platelet) syndrome is a known feature of pre-eclampsia (11). However, its pathogenesis has not been fully explained (13). Yet, haemolysis may be responsible for the elevation of AST due to its presence in red blood cells. It can also be suggested that the effect of free radical injury on red blood cell membrane has led to haemolysis. Elevated AST may also be due to an insult from free radical injury to the hepatocytes. This is evidenced by the accompany elevation of ALT which has been said to be more liver-specific. This free radical injury in our study was evidenced by corresponding increase in plasma malondialdehyde, a product of free radical injury. Free radical injury to the liver has been established from the finding of a previous study (14). However, hepatic insult could occur without free radical injury. It should also be noted that this free radicals could also affect other tissues where these enzymes are also present (25). Nevertheless, this study was able to ascertain that the free radical injury could be initiated by pre-eclampsia.
This study demonstrated that the higher the AST and ALT, the higher the plasma malondialdehyde. The severity of free radical injury could be measured by plasma MDA, and also the severity of hepatic involvement could be assessed by plasma AST and ALT. We observed that the higher the plasma MDA, the higher the plasma liver enzymes. One can deduce from the findings of this study that pregnant women with pre-eclampsia without free radical injury (oxidative stress) may not have elevated liver enzymes.
We therefore conclude that there was an increased production of MDA correlating with elevated liver enzymes. The elevated liver enzymes seen in women with pre-eclampsia may be due to free radical injury to the liver. Pre-eclamptic women without free radical injury did not have elevated liver enzymes in this study.
References
- 1.Lydakis C, Beevers M, Beevers DG, et al. The prevalence of pre-eclampsia and obstetric outcome in pregnancies of normotensive and hypertensive women attending a hospital specialist clinic. Int J Clin Pract. 2001;55(6):361–367. [PubMed] [Google Scholar]
- 2.Alphonsus NO, Angela AO. Perinatal Outcome in Patients With Pre-Eclampsia in Benin City, Nigeria. Trop J Obstet Gynaecol. 2004;21:148–152. [Google Scholar]
- 3.Lelia D. Aspirin for preventing and treating pre-eclampsia. BMJ. 1999;318(7186):751–752. doi: 10.1136/bmj.318.7186.751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laura ST, Lisa PS, Branda E. Changes in Paternity: A Risk factor for Preeclampsia in Multipara. Epidemiology. 1996;7(3):240–244. doi: 10.1097/00001648-199605000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Jonathan MM, Nitin KG, Marit JR, et al. Circulating marker of oxidative stress is raised in normal pregnancy and preeclampsia. Briti J Obs Gyn. 1998;105:1195–1199. doi: 10.1111/j.1471-0528.1998.tb09974.x. [DOI] [PubMed] [Google Scholar]
- 6.Ogunro PS, Balogun WO, Fadero FF, et al. Palsma lipid peroxidation and total antioxidant status amonf Dyslinpodaemia and Hypertensive Nigerians with Risk of Coronary Heart Disease. West African J of Med. 2009 Mar;28:87–91. doi: 10.4314/wajm.v28i2.48430. [DOI] [PubMed] [Google Scholar]
- 7.Tsukatani E. Etiology of EPH-gastosis from the view of dynamics of vasoactive prostanoids. Lipid peroxides and vitamin E. Acta Obstet Gynaecol. 1983;35:713–720. [PubMed] [Google Scholar]
- 8.Germain SJ, Sacks GP, Sooranna SR. Systemic inflammatory priming in normal pregnancy and preeclampsia: the role of circulating syncytiotrophoblast microparticles. J Imunol. 2007;178(9):5949. doi: 10.4049/jimmunol.178.9.5949. [DOI] [PubMed] [Google Scholar]
- 9.Sies H. Oxidative stress: oxidants and antioxidants. Exp Physiol. 1997;82(2):291–295. doi: 10.1113/expphysiol.1997.sp004024. [DOI] [PubMed] [Google Scholar]
- 10.Idogun ES, Odiegwu ME, Momoh SM, Okonofua FE. Effect of Pregnancy on total antioxidant capacity in Nigerian women. Park J Med Sci. 2008 Apr-Jun;24:2292–2295. [Google Scholar]
- 11.Niedernhofer LJ, Daniels JS, Rouzer CA, et al. Malondialdehyde, a product of lipid peroxidation, is mutagenic in human cells. J Biol Chem. 2003;278(33):31426–31433. doi: 10.1074/jbc.M212549200. 15. [DOI] [PubMed] [Google Scholar]
- 12.William MC, Louis WA. Review of HELLP Syndrome. J Perinatol. 1999;19(2):138–143. doi: 10.1038/sj.jp.7200165. [DOI] [PubMed] [Google Scholar]
- 13.Maureen OP. HELLP Syndrome: Recognition and Perinatal Management. Am Fam Physician. 1999;60(3):829–836. [PubMed] [Google Scholar]
- 14.Pablo M. Role of free radicals in liver diseases. Hepatol Int. 2009;3(4):526–536. doi: 10.1007/s12072-009-9158-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Satoh K. Serum lipid peroxide in cardiovascular disorders determined by a new colourimetric method. Clin Chem Acta. 1978;90:37–42. doi: 10.1016/0009-8981(78)90081-5. [DOI] [PubMed] [Google Scholar]
- 16.Bergeyer HU, Herder M. Plasma AST estimation: International Federation of Clinical Chemistry, Scientific Committee. J Clin Chem. 1986;18:521, 534. [Google Scholar]
- 17.Bergmeyer HU, Herder M, Raj R. Approved recommendation on International Federation of Clinical Chemistry method for the measurement of Alanine aminotransferase. J Clin Chem. 1986;24:481–489. [PubMed] [Google Scholar]
- 18.Paolisso G, Tagliamonte MR, Rizzo MR, Manzella D, Gambardella A, Varricchio M. Oxidative stress and advancing age: results in healthy centenarians. J Am Geriatr Soc. 1998;46(7):833–838. doi: 10.1111/j.1532-5415.1998.tb02716.x. [DOI] [PubMed] [Google Scholar]
- 19.Robinson D, Whitehead TP. Effect of body mass and other factors on serum liver enzyme levels in men attending for well population screening. Ann Clin Biochem. 1989 Sep;26(Pt 5):393–400. doi: 10.1177/000456328902600503. [DOI] [PubMed] [Google Scholar]
- 20.John RB, Baha MS. Diagnosis and management of hemolysis, elevated liver enzymes, and low platelets syndrome. Clin Perinatol. 2004;31:807–833. doi: 10.1016/j.clp.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 21.Ahmed HA, Salam S, Hazim HE, Jasim A. Evaluattion of Serum malondialdehyde in relation to other clinical considerations in premature neonate. Tikrit Medical Jour. 2009;15(2):42–51. [Google Scholar]
- 22.Acworth IN, Bailey B. The handbook of oxidative metabolism. Massachusetts: ESU Inc; 1997. Reactive Oxygen Speicies; pp. 1–4. [Google Scholar]
- 23.Zusterzeel PL, Rutten H, Peters WH, et al. Protein carbonyls in deciduas and placenta of preeclampsia women as markers for oxidative stress. Placenta. 2001;22:213–219. doi: 10.1053/plac.2000.0606. [DOI] [PubMed] [Google Scholar]
- 24.Guptal S, Agarwal A, Sharma RK. The role of placental oxidative stress and lipid peroxidation in preeclampsia. Obstet Gynecol Surv. 2005;60(12):807–816. doi: 10.1097/01.ogx.0000193879.79268.59. [DOI] [PubMed] [Google Scholar]
- 25.Mylonas C, Kouretas D. Lipid peroxidation and tissue damage. in Vivo. 1999;13(3):295–309. [PubMed] [Google Scholar]