Abstract
The purpose of this descriptive repeated-measures study was to describe depressive symptom patterns and report changes over time in levels of perceived stress and social support depending on patterns of depressive symptoms in single, low-income, African American, adolescent mothers during the initial, 6-month postpartum period. Thirty-five adolescent subjects between the ages of 16 and 22 years old were recruited at health care clinics in two Midwestern cities. Data collections by advanced practice nurses were completed at 1 week, 6 weeks, 3 months, and 6 months postpartum at mothers’ homes. Established instruments were used to measure depressive symptoms, perceived stress and social support. Results indicated 63% of adolescent mothers’ experienced depressive symptoms sometime during this transition period and 11.4% of these subjects had depressive symptoms at all 4 time points. Depressive symptoms were associated with perceived stress at each time point. Emotional support was inversely associated with depressive symptoms at 2 of the 4 time points. Depressive symptoms and problematic support were significantly related at 3 months and 6 months. Although single, low-income, African American, adolescent mothers are considered a high risk group, some are at even greater risk. This extremely high risk group have depressive symptoms throughout the first 6 months postpartum with the highest level of perceived stress and the most variability in social support relative to groups that were never depressed or were in and out of depression. More studies are needed to understand how to best help these high risk adolescents successfully transition to motherhood.
Keywords: Social support, adolescent, mothers, African American, transition
Introduction
The initial postpartum period is a critical time of transition for all first-time mothers who are undergoing bio-psycho-social changes (Mercer, 2004; Suplee et al., 2014), and particularly for single, low-income, African American adolescent mothers (Keating-Lefler, Hudson, Campbell-Grossman, Fleck, & Westfall, 2004; Logsdon, Birkimer, & Usui, 2000). An indication of difficulties with this transition is depressive symptoms. Approximately half (49%) of African American adolescent mothers report significant depressive symptoms (Ramos-Marcus et al., 2010). Furthermore, researchers have found depressive symptoms linked to less social support (Edwards et al., 2012; Hatcher, Rayens, Peden, & Hall, 2008; Leahy-Warren, McCarthy, & Corcoran, 2011; Logsdon et al., 2000) and more perceived stress (Hammen, 2003; Manuel, Martinson, Bledsoe-Mansori, & Bellamy, 2012). However, the majority of studies examining depressive symptoms, social support, and perceived stress in adolescent mothers have not collected data repeatedly during the first 6 months postpartum. More studies are needed with African American adolescent mothers focusing on this transition period to examine how depressive symptoms change during this time and how such changes are related to the stress and social support.
Regardless of whether the underlying causes of depressive symptoms were physiological and/or psychological, these symptoms commonly include fluctuating mood swings, irritability, crying, decreased concentration, and difficulty sleeping (Bobo & Yawn, 2014). A considerable portion (35% – 67%) of low-income new mothers report depressive symptoms (Beck, 2002; Beeghly et al., 2003; Ramos-Marcus et al., 2010). However, there is some evidence that everyone does not experience depressive symptoms in the same pattern during the postpartum period. For example, Ramos-Marcuse et al. (2010) found three levels/patterns of depressive symptoms in 181 low-income, African American adolescent mothers over the first two years postpartum: low (41%), moderate (45%), and high (14%) symptom levels. In the group with initial moderate levels, a decrease in depressive symptoms was found between 6 and 24 months although the level remained higher than the low symptom group (Ramos-Marcuse et al.). Interestingly, those mothers who were initially low or high in depressive symptoms continued to present with the same symptom levels at 6 months and 24 months. In contrast, Edwards et al. (2012) found depressive symptoms were highest during pregnancy and declined throughout the 24 months postpartum in 248 low-income African American mothers although the percentage of adolescents in the sample were not reported. In yet another study, Mora et al. (2009) found 5 distinct trajectories of depressive symptoms in a multiethnic sample of low-income mothers of all ages that was 70% African American (N=1,735). These groups were categorized as: (a) always, showing chronic depressive symptomatology during both pre and postpartum periods (7%); (b) antepartum, depressive symptoms only during antepartum period (6%); (c) postpartum, showing depressive symptoms during the postpartum period and resolving during the first year postpartum (9%); (d) late, depressive symptoms that increase in the second year postpartum (7%); and (e) never, no depressive symptoms reported (71%). Although the patterns of depressive symptoms were found to vary, many researchers have not examined these patterns during the first 6 months postpartum, a critical time of adapting and intervening (Goodman, 2009; Ramos-Marcuse et al., 2010; Schmidt, Wiemann, Rickert, & Smith, 2006).
New mothers often perceive stress during the transition period after the birth of the baby (Brubaker & Wright, 2006; Campbell-Grossman, Hudson, Keating-Lefler, & Heusinkvelt, 2009; Walker, Timmerman, Kim, & Sterling, 2002). Situations in one’s life appraised as stressful depends on the persons’ perception that the demands of a situation exceed their ability to cope (Cohen, Kamarck, & Mermelstein, 1983). Risk factors associated with the stress a new mother experiences include being under twenty years of age, being unmarried, having a low income, and having inadequate social support (Manuel et al., 2012). The inadequate social support may be particularly important for low-income mothers. Negron, Martin, Almog, Balbierz, and Howell (2012) reported results from four focus groups of ethnically diverse low-income mothers. Stressors identified by a subset of African American mothers at 6–12 months postpartum were difficulty caring for themselves, and difficulty caring for their new infant full time with minimal assistance and inadequate resources. Perceived stressors identified by all 32 mothers were: not knowing what services and resources were available for support, fear of judgment if they asked for help, embarrassment when asking for help, feeling like a burden, having unrealistic expectations of their support networks, and stress from the stigma of being labeled poor and in need of more resources (Negron et al.).
Prior investigators reported higher levels of perceived stress were related to greater depressive symptoms in low-income mothers during the postpartum period. Mora et al. (2009) found perceived stress positively related to depressive symptomatology that began during pregnancy in mothers (70% African American; n = 1,735) and continued up to 2 years postpartum. Manuel et al. (2012) did a secondary analysis of national health data and found that certain types of stressors, particularly economic hardship, parenting stress, and poor physical health, increased the risk of depressive symptoms in low-income mothers up to 5 years postpartum. Ngai and Chan (2012) found higher stress levels in the early postpartum period compared to stress levels during the antepartum period in first-time Chinese mothers. More studies are needed with single, low-income, African American adolescent mothers during the first 6 months postpartum to better understand the relationship of perceived stress and depressive symptoms.
Inadequate social support and problematic support have been identified as two factors associated with both perceived stress and depressive symptoms. Social support was broadly defined as the provision of assistance or comfort to help one cope with a variety of problems. The four types of social support frequently examined were (a) informational, (b) emotional, (c) tangible, and (d) problematic support (House, 1981; Revenson & Majerovitz, 1991). In the current study, social support was conceptualized and measured as the mother’s perceptions of the actual receipt of support compared to the mother’s perception of the availability of social support when it is needed. Receipt of support was examined because social support does not always materialize when it is needed (Campbell-Grossman et al., 2009; Wills & Shinar, 2000).
Informational support was defined as the provision of advice or suggestions about what to do, how to solve problems, or where to get needed information to cope with personal and environmental problems (House, 1981). Informational support, particularly from health care providers, has long been thought to be important to new mothers to link them to broad and diverse information or to community resources. In addition, the provision of informational support, particularly through the educational and hands-on skills training sessions provided by nurses, has been considered an important component of the nurses’ role to facilitate the women’s transition to motherhood (George, 2005). There is some evidence that this type of support is associated with depressive symptoms during this transitional period. Leahy-Warren et al. (2012) found that informational support was a significant dimension of social support in lowering depressive symptoms at 6 weeks, but not at 12 weeks postpartum. Because of the few studies examining informational support in relation to depressive symptoms among new mothers during postpartum, more studies are needed.
Emotional support has been the primary type of support examined and found to be significant in prior studies (Gee & Rhodes, 2003; Israel, Farquhar, Schulz, James, & Parker, 2002; McBride et al., 2004). This type of support is defined as the provision of affection, liking, love, or listening (House, 1981). There is evidence that support has an association with perceived stress. Israel et al. (2002) found that emotional support was a major factor in reducing stress and stress effects in low-income African American mothers of young children. However, the relationship was only significant when stress was at a moderate, but not high level.
Tangible support has been defined as the provision of goods and services (Revenson & Schiaffino, 1990). Examples might include transportation, buying or preparing food, paying the rent, or doing chores around the home that they normally do. Logsdon and Usui (2006) found that the adolescents’ mothers were the most important source of tangible support. Tangible support from the adolescents’ mothers in this study included hands-on assistance with tasks and responsibilities a new mother is expected to assume such as provisions of food and financial support for herself and her baby (Logsdon & Usui). Interestingly, high levels of tangible support from the adolescents’ mothers was not always viewed as positive as high tangible support from the adolescents’ mothers resulted in more depressive symptoms in these young, low-income, African American mothers (Logsdon & Usui). The authors attributed these results to differences in desire for help and role confusion. That is, if too much tangible help was from the adolescents’ mothers, the new adolescent mothers felt inadequate and more prone to depressive symptoms.
Problematic support is the final type of social support and was conceptualized as support perceived as unhelpful even though the provider’s actions may have been well intended (Hudson, Campbell-Grossman, Keating-Lefler et al., 2012; Revenson & Majerovitz, 1991; Revenson, Schiaffino, Majerovitz, & Gibofsky, 1991). Prior researchers reported problematic support may lead to increased stress and depressive symptoms during the transition period for new mothers (Gee & Rhodes, 2003; Logsdon et al., 2000). Problematic support may occur because potential supporters may not understand how certain situations affect people or how to behave positively toward others. The potential supporter may avoid open exchange of feelings, give misleading (but well-meant) advice, or be overly optimistic and minimize the situation. Despite the potential importance of problematic social support, no quantitative studies were found examining problematic support in postpartum African American adolescent mothers.
In summary, little is known about the types of social support received by single, low-income, African American adolescent mothers during the initial postpartum transition period. Few studies were found that examined changes in types of social support over the first 6 months postpartum in a sample of African American adolescent mothers. Further, although some types of social support were found to be associated with depressive symptoms and stress, there is a paucity of research on changes in stress and depressive symptoms in relation to changes in types of support among low income African American new mothers. Thus, the purpose of this study, in a sample of adolescent, single, low-income, first time, African American mothers, was to: (a) describe the pattern of depressive symptoms in adolescent mothers during the first six months postpartum; and (b) describe the changes over time in their levels of stress and social support in relation to the pattern of depressive symptoms found.
Method
This descriptive repeated-measures study was a secondary analysis of existing data collected as part of a randomized controlled trial (RCT) assisting African American, first-time mothers during the first 6-month postpartum period (Hudson, Campbell-Grossman, & Hertzog, 2012). In the parent RCT, the intervention group received the New Mothers Network, a theory-based social support intervention (House, 1981; Revenson & Majerovitz, 1991). This was a 6-month intervention designed to improve the adolescent mothers’ psychological and parenting outcomes. The mothers accessed the intervention through an Internet device provided to them. Because there were no significant differences between the invention and control groups in depressive symptoms, perceived stress, and social support in this study the participants were collapsed into one group for this secondary analysis.
Participants
The sample was 35 first time African American mothers, 34 (97%) were adolescents at baseline. The adolescent age range from 16 to 21 years was appropriate as individuals were working on the same developmental tasks such as Erickson’s classical Identity vs Role Confusion and Intimacy vs. Isolation (Erikson, 1950). These ages are part of the developmental age group of late adolescence and prolonged adolescence as individuals are showing signs of maturing to adulthood and independence, but are often still dependent on others for most types of support (LeTendre, 2000).
The sample of participants was recruited from two health care clinics in two urban Midwestern cities. The inclusion criteria for the RCT were: (a) unmarried, (b) low-income, (c) full-term baby, (d) first-time birth, and (e) planning to keep the infant. The exclusion criteria was complicated birth including cesarean section delivery. Participant consents, or participant assents with parental consents were obtained before data collection began. This RCT was considered a feasibility study with results used to guide further research. The final sample size for this study was determined by logistical and budgetary constraints.
Procedure
Depressive symptoms, perceived stress, and social support were measured at each of the four data collection time points: 1 and 6 weeks, 3 and 6 months after delivery of the baby. Outcome data were collected at each home visit where participants completed the instruments on their own. At the completion of each data collection time point, mothers were given a thank-you gift card for $20 as compensation for their time. The study was approved by the Institutional Review Board at the University and at the clinical sites where the study was conducted.
Measures
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale (CES-D). The CES-D is a 20 item tool quantifying the frequency of affective, behavioral, or somatic symptoms during the preceding week rated on a 0 – 3 score. The total score could range from 0 to 60 with a total score of 16 or higher indicating significant depressive symptoms (Radloff, 1991). As part of the study protocol, mothers with scores of 16 or greater were instructed to notify their primary health care professional and seek assistance for their symptoms. The CES-D has documented validity when compared to other related outcomes and tools. Brage and Meredith (1993) found depressive symptom directly related to both loneliness (r =.414, p < .01) and self-esteem (r = −.396, p < .01) in adolescent subjects. Logsdon and Myers (2010) reported a sensitivity of .70 and specificity of .52 with criterion measures of affective disorders. In the current study, the CES-D instrument had robust reliability with Cronbach alphas ranging from .81 to .87 for the various time points.
Perceived stress was measured using the Perceived Stress Scale (PSS) which assesses the degree to which situations in one’s life were appraised as stressful during the previous month (Cohen et al., 1983; Lee, 2012). Each of 14 items were rated on a 5-point scale ranging from 0 (never) to 4 (very often). Total scores can range from 0 to 56 with higher scores denoting higher levels of perceived stress. Internal consistency of the PSS for a sample of 70 mothers was estimated as .97 (Carro, Grant, Gotlib, & Compass, 1993). The test-retest reliability was .85 (Cohen et al.). The PSS was highly correlated with depressive symptoms, but was found to measure a different and independent construct of general stress (Cohen et al.). Mitchell, Crane, and Kim (2008) reported the PSS had good criterion validity when compared to the Medical Outcome Study-Short Form 36, mental component (r= −.65) and a one-factor solution which accounted for 56.6% of the variance. In the current study, Cronbach alphas were .69–.79 for the various time points.
Social support was measured using Revenson’s and Schiaffino’s (1990) Social Support Measure. This tool measures the participants’ perceptions of received support for the four dimensions; emotional (5 items), informational (5 items), tangible (3 items), and problematic subscale (4 items). Items were measured on a Likert scale that ranged from 1 (never) to 5 (always); higher scores denoted greater levels of received social support. In prior research, internal consistency reliabilities for each subscale were .75 for emotional, .83 for informational, .79 for tangible, and .66 for problematic subscale (Revenson & Schiaffino). In a factor analysis, a four-factor structure emerged with emotional, tangible aid, informational, and problematic support named as factors (Revenson & Schiaffino). In the current study, Cronbach alphas were: emotional (.59 – .88), informational (.78 – .88), tangible (.70 – .93), and problematic (.71 – .94).
Data Analyses
For Aim 1, descriptive statistics were used to describe depressive symptoms in three groups of adolescent mothers during the first 6 months postpartum (i.e., frequencies, spaghetti plots). For Aim 2, Spearman rho correlations were calculated to examine relationships between depressive symptoms and perceived stress and each type of social support. To further assess how depressive symptoms may be related to perceived stress and social support over time, the means of the stress and support variables over time were plotted in relation to patterns of depressive symptoms.
Results
The participants in the sample included 35 single, first-time, African American mothers with a mean age of 18.3 years (SD = 1.7; Range = 16 to 22) at enrollment. Only 50% (n= 17) had completed high school and 85% (23 out of the 27 who reported income) made less than $10,000 annually.
Across the four data collection time points, the proportion of participants with depressive symptoms (scores ≥ 16) ranged from 25% to 38% as seen in Table 1. However, at some point in the first 6 months, 22 out of the 35 participants (63%) had CES-D scores ≥ 16. Across the entire sample (n=35), 13 participants (37%) did not score ≥ 16 at any point in the study, 4 (11%) reported scores ≥ 16 at all of the time points, and the remaining 18 participants (51%) scored ≥ 16 at some, but not all points in the study as seen in Table 2. If mothers had depressive symptoms at one, two, or three time points during the study, they were labeled the In-and-Out Depressive Symptom Group (n = 18; 51%) in subsequent analysis. The other two patterns that emerged were labeled the Never Depressed Group (n=13; 37%) and the Always Depressed Group (n=4; 11%).
Table 1.
Depressive Symptoms (CES-D scores ≥ 16) over the First 6 Months Postpartum
| 1 Week | 6 Weeks | 3 Months | 6 Months | |
|---|---|---|---|---|
| Sample Size | 35 | 32 | 32 | 32 |
| N (%) Depressed: | ||||
| CES-D scores > 16 | 12 (34%) | 8 (25%) | 12 (38%) | 10 (31%) |
CES-D = Center for Epidemiological Studies – Depression Scale
Table 2.
Frequency of Elevated Depressive Symptoms (CES-D scores ≥ 16)
| # of Occasions Depressed | Frequency | Percent |
|---|---|---|
| 0 | 13 | 37.1% |
| 1 | 12 | 34.3% |
| 2 | 4 | 11.4% |
| 3 | 2 | 5.7% |
| 4 (All Time Points) | 4 | 11.4% |
The trajectories of each of these participants in the In-and-Out Depressive Symptoms Group (n=18) are depicted in Figure 1, a spaghetti plot which includes a dashed line as a reference indicating a CES-D score of 16. Figure 1 shows the amount of variability around the cutoff score of 16 in these participants, and how depressive symptoms changed over time for each individual.
Figure 1.
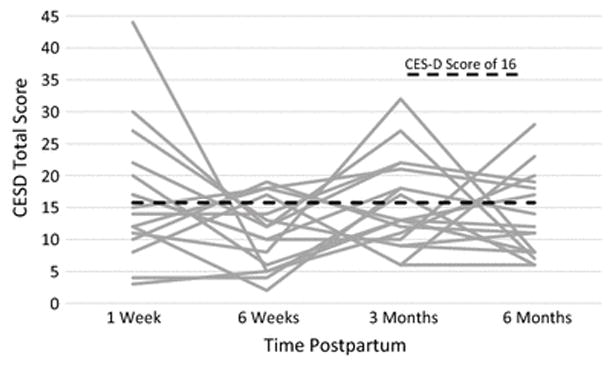
Spaghetti Plot of Participants’ CES-D Scores Over the Course of the Study (In-and-Out of Depressive Symptoms Group, n=18).
The relationships between depressive symptoms and perceived stress and social support during the first six months postpartum are reported in Table 3. Spearman correlations and p-values are presented for the relationships between depressive symptoms and stress and social support at each time point. Depressive symptoms were significantly and positively related to perceived stress at each time point. Depressive symptoms and emotional support were negatively related at the 6 week and 6 month time points. Depressive symptoms and problematic social support had significant positive relationships at months 3 and 6.
Table 3.
Correlations (p-value) between CES-D and Stress and Social Support over Time
| CES-D at the following times: | Perceived Stress | Emotional Support | Informational Support | Tangible Support | Problematic Support |
|---|---|---|---|---|---|
| 1 week (n=35) | 0.663 (<.001) | −0.133 (0.447) | 0.147 (0.399) | 0.147 (0.4) | 0.272 (0.114) |
| 6 weeks (n=32) | 0.719 (<.001) | −0.417 (0.017) | −0.243 (0.181) | −0.274 (0.13) | 0.258 (0.154) |
| 3 months (n=32) | 0.498 (.004) | −0.146 (0.424) | −0.054 (0.77) | −0.272 (0.132) | 0.405 (0.021) |
| 6 months (n=32) | 0.439 (.012) | −0.459 (0.008) | −0.209 (0.25) | −0.222 (0.222) | 0.414 (0.018) |
To further assess how depressive symptoms were related to perceived stress and social support over time, the means of the stress and support variables over time were plotted in relation to patterns of depressive symptoms. Figures 2 and 3 show average perceived stress scores and four types of social support (emotional, educational, tangible, and problematic support) at each time point based on whether mothers were below the clinical depression cutoff throughout the entire study (Never Depressed Group; n=13), if they were at, or above the CES-D cutoff throughout the study (Always Depressed Group; n=4), or if they moved above and below the CES-D cutoff between time points over the course of the study (In-and-Out of Depressive Symptoms Group; n=18). Although differences in change were not found to be significant over time, this was likely due to the small sample sizes of these groups.
Figure 2.
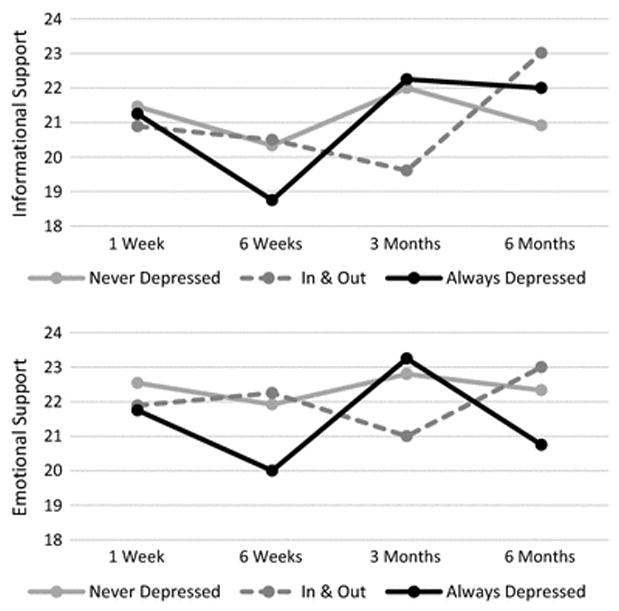
Types of social support (informational and emotional) by depressive symptom patterns.
Figure 3.
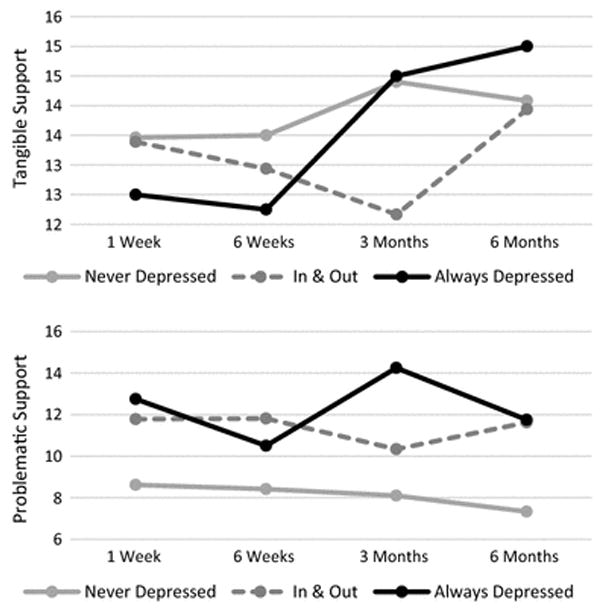
Types of social support (tangible and problematic) by depressive symptom patterns.
Figure 4 shows the group of mothers in the Always Depressed Group had consistently higher levels of perceived stress than the other two groups. In contrast, mothers in the Never Depressed Group consistently reported the lowest level of perceived stress. As seen in Figure 4, the Always Depressed Group reported a much less stable pattern of emotional social support than the other two groups. Similar patterns were seen in the other types of support (informational, tangible, and problematic support) over time in this group. The Always Depressed Group was characterized by variability in their perceived social support. To a lesser extent, the In-and-Out of Depressive Symptoms Group also had patterns of social support that varied more than the Never Depressed Group.
Figure 4.
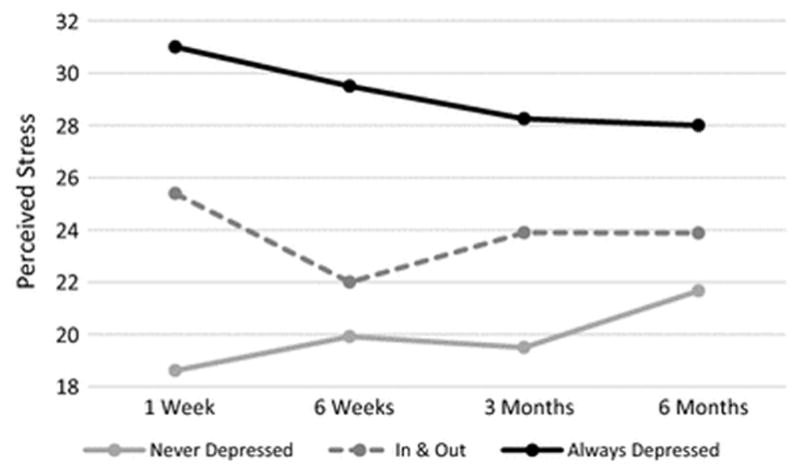
Perceived Stress by Depressive Symptom Patterns.
Discussion
The majority of mothers, almost two-thirds (63%) of the sample, had depressive symptoms (scores on the CES-D ≥ 16) sometime during the first 6 months postpartum, the initial transition to motherhood. This percentage is greater than others have reported (Beeber et al., 2010; Campbell, Matestic, von Stauffenberg, Mohan, & Kirchner, 2007; Edwards et al., 2012; Riola, Nguyen, Greden, & King, 2005) and may be due to more frequent assessments over the initial 6 month postpartum period. This high proportion having depressive symptoms may also indicate that the first 6 months is indeed a critical period of adaptation as others have speculated (Goodman, 2009). Not surprisingly, the sub-group of mothers who reported continuously depressive symptoms over the 6 month period (Always Depressed Group) also had consistently higher levels of perceived stress and a less stable pattern of social support than the other two groups. These results suggest there is a subgroup of mothers who need to be identified early and provided with social support and needed resources. All African American adolescent mothers need to be screened at birth so that depressive symptoms can be identified early and resources can be provided based on their identified needs.
In this study, the proportion of mothers in the Never Depressed Group (37%) was similar to Ramos-Marcus et al. (2010) who found that 41% of their African American single, adolescent subjects were never depressed. However, the percentage of individuals reported by Mora et al. (2009) in their no-depression group was higher (71%), possibly because they did not measure the new mothers during the initial 6 months but rather at birth, 6, 12, and 24 months. Other differences between the study by Mora et al. and this study was that Mora et al. included multiethnic (70% African American), older women (M = 23.9 years, SD= 5.8 years), who were married (26%) – all factors that may account for the lower incidence of depressive symptoms in their study. In this study, the women in the Never Depressed Group were also characterized by the lowest level of perceived stress and the most stability in social support scores over time.
For mothers in the In and Out of Depressive Symptoms Group, the spaghetti plots indicated that they had high variability in depressive symptoms over the first six months. This group also reported more perceived stress at each time point and more variability in social support than the Never Depressed Group. This group received the least amount of all types of social support at 3 months post-birth. Three months may be a vulnerable point in the transition to motherhood because the new mothers are past the initial challenges of the birth circumstances and some routines have been established in the home environment. The new mother may have exhausted their sources of support at this time point or supporters may think that the new mother is no longer in need of as much support and assistance. Future studies need to examine, over the first 6 months post-birth, sources and types of support, what the support needs are at each time point, and what it is about 3 months post-birth that makes the new mothers more vulnerable at this time point.
The two types of received social support that were related to depressive symptoms and perceived stress in this sample of African American adolescents were emotional support and problematic support. More emotional support was related to fewer depressive symptoms at 6 weeks and 6 months. In prior studies, it was found that mothers need emotional support postpartum to increase their self-esteem and to facilitate achievement of the maternal role (Suplee et al., 2014). In a study by de la Rosa, Perry and Johnson (2009), new mothers with high levels of emotional support achieved higher adaptation to the maternal role compared to those who reported low levels of support. Logsdon and Usui (2006) found that the African American adolescent’s partner was the most important person providing emotional support. Thus, more research is needed examining not only the type of support but also the source of support in these African American adolescents.
One of the main contributions of this study was the finding that greater problematic support was related to more depressive symptoms at 3 and 6 months postpartum. Few prior studies have examined the effect of problematic support in the postpartum period and how it is related to outcomes of the postpartum period. The potential supporter may not understand how the new mother is feeling or know how to behave positively toward others. Alternatively, this may reflect the effects of advice, although well intended, may be counter to what the adolescent believes needs to be done and subsequently contributed to the adolescent’s worsening feeling about herself. Earlier studies have found that young mothers’ disagreements with their primary support persons were associated with depressive symptoms during the postpartum transition period (Edwards et al., 2012; Kalil, Spencer, Spieker, & Gilchrist, 1998). In the current study, the mothers who never had depressive symptoms over the 6 month period had the lowest level of problematic support. Thus, future studies need to examine sources of problematic support and how to minimize it in African American adolescent mothers.
Another new contribution of this study were the findings from examining changes in social support based on their level of depressive symptoms. The amount of all four types of social support was stable only for the never depressed group. For the remaining mothers who experienced depressive symptoms, which was nearly two-thirds of the sample, the levels of social support were highly variable. These mothers did not appear to receive stable or adequate levels of social support. Thus, interventions need to be tested to provide additional support and/or to supplement the African American adolescent mother’s existing support system to potentially reduce the depressive symptoms and stressors these mothers experience.
We also found that depressive symptoms were related to greater perceived stress levels at each time point. Other researchers have documented similar findings in young mothers (Druss, Rosenheck & Sledge, 2000; Hammen, 2003; Israel et al., 2002; Readings & Reynolds, 2001; Manuel et al., 2012; Mulsow, Caldera, Pursely, Reifman & Huston, 2002; Ostberg & Hagekull, 2000) even though the mothers were not all single, low-income, African American adolescents. In the current study, the correlations between depressive symptoms and perceived stress levels were highest at 1 and 6 weeks compared to 3 and 6 months postpartum. In addition, the majority of mothers had the highest perceived stress scores at 1 and 6 weeks. Taken together, these findings suggest that African American adolescent mothers may be the most vulnerable to stressors during the first 6 weeks.
Limitations
There were some limitations to this secondary analysis. One of the limitations was collapsing the intervention groups into one group for this secondary analysis. There may have been small effects of the intervention that affected the findings in the current study in a unknown way. In addition, the sample size was small and, likewise, the Always Depressed Group had a very small cell size (n=4) which limited our ability to draw conclusions about this group. Another limitation was that convenience sampling was used. This limits the generalizability of the results to adolescents who are similar to the single, low-income, African American adolescent mothers in this study. However, this descriptive work provided important insights into depressive symptoms, perceived stress, and social support in the early transitional period for adolescent, low-income, single mothers. Another limitation of this study was that we measured general perceived stress rather than stress specific to the postpartum period. Measuring specific postpartum stressors may be more useful in understanding the unique stressors they are experiencing and how to best help these adolescents.
Contributor Information
Christie Campbell-Grossman, College of Nursing, University of Nebraska Medical Center, Lincoln, NE.
Diane Brage Hudson, College of Nursing, University of Nebraska Medical Center, Lincoln, NE.
Kevin A. Kupzyk, College of Nursing, University of Nebraska Medical Center, Omaha, NE
Sara E. Brown, College of Nursing, University of Nebraska Medical Center, Omaha, NE
Kathleen M. Hanna, College of Nursing, University of Nebraska Medical Center, Omaha, NE
Bernice C. Yates, College of Nursing, University of Nebraska Medical Center, Omaha, NE
References
- Beck C. Postpartum depression: A metasynthesis. Qualitative Health Research. 2002;12:453–472. doi: 10.1177/104973202129120016. [DOI] [PubMed] [Google Scholar]
- Beeber LS, Holditch-Davis D, Perreira K, Schwartz TA, Lewis V, Blanchard H, et al. Short-term in-home intervention reduces depressive symptoms in early head start Latino mother of infants and toddlers. Research in Nursing Health. 2010;33:60–76. doi: 10.1002/nur.20363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeghly M, Olson KL, Weinberg MK, Pierre SC, Downey N, Tronick EZ. Prevalence, stability, and socio-demographic correlates of depressive symptoms in Black mothers during the first 18 months postpartum. Maternal and Child Health Journal. 2003;7:157–168. doi: 10.1023/a:1025132320321. [DOI] [PubMed] [Google Scholar]
- Bobo WV, Yawn BP. Concise review for physicians and other clinicians: Postpartum depression. Mayo Clinic Proceedings. 2014;89:835–844. doi: 10.1016/j.mayocp.2014.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brage D, Meredith W. A casual model of adolescent depression. The Journal of Psychology. 1993;128:455–468. doi: 10.1080/00223980.1994.9712752. [DOI] [PubMed] [Google Scholar]
- Brubaker SJ, Wright C. Identify transformation and family caregiving: Narrative of African American teen mothers. Journal of Marriage and Family. 2006;68:1214–1228. [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Developmental Psychology. 2007;43:1202–1215. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- Campbell-Grossman C, Hudson DB, Keating-Lefler R, Heusinkvelt S. New mothers network: The provision of social support to single, low-income, African American mothers via e-mail messages. Journal of Family Nursing. 2009;15:220–236. doi: 10.1177/1074840708323048. [DOI] [PubMed] [Google Scholar]
- Carro M, Grant K, Gotlib I, Compass B. Postpartum depression and child development: An investigation of mothers and fathers as source of risk and resilience. Development and Psychopathology. 1993;5:567–578. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- de la Rosa IA, Perry J, Johnson V. Benefits of increased home-visitation services: Exploring a case management model. Family & Community Health. 2009;32:58–75. doi: 10.1097/01.FCH.0000342817.95390.7e. [DOI] [PubMed] [Google Scholar]
- Druss BG, Rosenheck RA, Sledge WHO. Health and disability costs of depressive illness in a major U.S. corporation. The American Journal of Psychiatry. 2000;157:1274–1278. doi: 10.1176/appi.ajp.157.8.1274. [DOI] [PubMed] [Google Scholar]
- Edwards RC, Thullen MJ, Isarowong N, Shiu C, Henson L, Hans SL. Supportive relationships and the trajectory of depressive symptoms among young African American mothers. Journal of Family Psychology. 2012;26:585–594. doi: 10.1037/a0029053. [DOI] [PubMed] [Google Scholar]
- Gee CB, Rhodes JE. Adolescent mothers’ relationship with their children’s biological fathers: Social support, social strain, and relationship continuity. Journal of Family Psychology. 2003;17:370–383. doi: 10.1037/0893-3200.17.3.370. [DOI] [PubMed] [Google Scholar]
- George L. Lack of preparedness: Experiences of first-time mothers. MCN, American Journal of Maternal Child Nursing. 2005;30:251–255. doi: 10.1097/00005721-200507000-00009. [DOI] [PubMed] [Google Scholar]
- Hammen C. Interpersonal stress and depression in women. Journal of Affective Disorders. 2003;74:49–57. doi: 10.1016/s0165-0327(02)00430-5. [DOI] [PubMed] [Google Scholar]
- Hatcher J, Rayens MK, Peden AR, Hall LA. Predictors of depression for low-income, African American, single mothers. Journal of Health Disparities Research and Practice. 2008;2:89–110. [Google Scholar]
- House J. Work, stress and social support. Menlo Park, CA: Addison-Wesley; 1981. [Google Scholar]
- Hudson DB, Campbell-Grossman C, Hertzog M. Effects of an internet intervention on mothers’ psychological, parenting, and health care utilization outcomes. Issues in Comprehensive Pediatric Nursing. 2012;35:176–193. doi: 10.3109/01460862.2012.734211. [DOI] [PubMed] [Google Scholar]
- Hudson DB, Campbell-Grossman C, Keating-Lefler R, Carraher S, Gehle J, Heusinkvelt S. On-line support for single, low-income, African American mothers. MCN: American Journal of Maternal Child Nursing. 2012;34:350–355. doi: 10.1097/01.NMC.0000363683.35562.56. [DOI] [PubMed] [Google Scholar]
- Israel BA, Farquhar SA, Schulz AJ, James SA, Parker EA. The relationship between social support, stress, and health among women on Detroit’s east side. Health Education & Behavior. 2002;29:342–360. doi: 10.1177/109019810202900306. [DOI] [PubMed] [Google Scholar]
- Kalil A, Spencer MS, Spieker SJ, Gilchrist LD. Effects of grandmother co-residence and quality of family relationships on depressive symptoms in adolescent mothers. Family Relations. 1998;47:433–441. [Google Scholar]
- Keating-Lefler R, Hudson DB, Campbell-Grossman C, Fleck M, Westfall J. Needs, concerns, and social support of single, low-income mothers. Issues in Mental Health Nursing. 2004;25:381–401. doi: 10.1080/01612840490432916. [DOI] [PubMed] [Google Scholar]
- Lee E. Review of psychometric evidence of the perceived stress scale. Asian Nursing Research. 2012;6:121–127. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Leahy-Warren P. First time mothers: Social Support and confidence in infant care. Journal of Perinatal Education. 2005;7:17–25. doi: 10.1111/j.1365-2648.2005.03425.x. [DOI] [PubMed] [Google Scholar]
- Leahy-Warren P, McCarthy G, Corcoran P. First-time mothers: Social support, maternal parental self-efficacy and postnatal depression. Journal of Clinical Nursing. 2012;21:388–397. doi: 10.1111/j.1365-2702.2011.03701.x. [DOI] [PubMed] [Google Scholar]
- LeTendre GK. Learning to be adolescent: Growing up in US and Japanese middle schools. New Haven, CT: Yale University Press; 2000. [Google Scholar]
- Logsdon MC, Birkimer JC, Usui WM. The link of social support and postpartum depressive symptoms in African American women with low incomes. MCM, American Journal of Maternal Child Nursing. 2000;25:262–266. doi: 10.1097/00005721-200009000-00009. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Myers JA. Comparative performance of two depression screening instruments in adolescent mothers. Journal of Women’s Health. 2010;19:1123–1128. doi: 10.1089/jwh.2009.1511. [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Usui WM. The Postpartum Support Questionnaire: Psychometric properties in adolescents. Journal of Child and Adolescent Psychiatric Nursing. 2006;19:145–156. doi: 10.1111/j.1744-6171.2006.00062.x. [DOI] [PubMed] [Google Scholar]
- Manuel JI, Martinson ML, Bledsoe-Mansori SE, Bellamy JL. The influence of stress and social support on depressive symptoms in mothers with young children. Social Science & Medicine. 2012;75:2013–2020. doi: 10.1016/j.socscimed.2012.07.034. [DOI] [PubMed] [Google Scholar]
- McBride CM, Baucom DH, Peterson BL, Pollak KI, Palmer C, Westman E, et al. Prenatal and postpartum smoking abstinence: A partner-assisted approach. American Journal of Preventative Medicine. 2004;27:232–238. doi: 10.1016/j.amepre.2004.06.005. [DOI] [PubMed] [Google Scholar]
- Mercer RT. Becoming a mother versus maternal role attainment. Journal of Nursing Scholarship. 2004;36(3):226–232. doi: 10.1111/j.1547-5069.2004.04042.x. [DOI] [PubMed] [Google Scholar]
- Mitchell MA, Crane P, Kim Y. Perceived stress in survivors of suicide: Psychometric properties of the perceived stress scale. Research in Nursing and Health. 2008;31:576–585. doi: 10.1002/nur.20284. [DOI] [PubMed] [Google Scholar]
- Mora PA, Bennett IM, Elo IT, Mathew L, Coyne JC, Culhane JF. Distinct trajectories of perinatal depressive symptomatology: Evidence from growth mixture modeling. American Journal of Epidemiology. 2009;169:24–32. doi: 10.1093/aje/kwn283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulsow M, Caldera YM, Pursely M, Reifman A, Huston AC. Multi-level factors influencing maternal stress during the first three years. Journal of Marriage and Family. 2002;64:944–956. [Google Scholar]
- Negron R, Martin A, Almog M, Balbierz A, Howell EA. Social support during the postpartum period: Mothers’ views on needs expectations and mobilization of support. Maternal and Child Health Journal. 2013;17:616–623. doi: 10.1007/s10995-012-1037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngai F, Chan SW. Stress, maternal role, competence, and satisfaction among Chinese women in the perinatal period. Research in Nursing & Health. 2012;35:30–39. doi: 10.1002/nur.20464. [DOI] [PubMed] [Google Scholar]
- Ostberg M, Hagekull B. A structural modeling approach to the understanding of parenting stress. Journal of Clinical Child Psychology. 2000;29:615–629. doi: 10.1207/S15374424JCCP2904_13. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The use of the center for epidemiologic studies depression scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20:149–165. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Ramos-Marcuse F, Oberlander SE, Papas MA, McNary SW, Hurley KM, Black MM. Stability of maternal depressive symptoms among urban, low-income, African American adolescent mothers. Journal of Affective Disorders. 2010;122:68–75. doi: 10.1016/j.jad.2009.06.018. [DOI] [PubMed] [Google Scholar]
- Reading R, Reynolds S. Debt, social disadvantage and maternal depression. Social Science & Medicine. 2001;53:441–453. doi: 10.1016/s0277-9536(00)00347-6. [DOI] [PubMed] [Google Scholar]
- Revenson T, Majerovitz S. The effects of chronic illness on the spouse: Social resources as stress buffers. Arthritis Care & Research. 1991;4:63–72. doi: 10.1002/art.1790040203. [DOI] [PubMed] [Google Scholar]
- Revenson T, Schiaffino K. Development of a contextual social support measure for use with arthritis populations. Proceeding of the Arthritis Health Professionals Association.1990. [Google Scholar]
- Revenson T, Schiaffino K, Majerovitz S, Gibofsky A. Social support as a double edged sward: The relation of positive and problematic support to depression among rheumatoid arthritis patients. Social Science Medicine. 1991;33:807–813. doi: 10.1016/0277-9536(91)90385-p. [DOI] [PubMed] [Google Scholar]
- Riola SA, Nguyen TA, Greden JF, King CA. Prevalence of depression by race/ethnicity: Findings from the national health and nutrition examination survey III. American Journal of Public Health. 2005;95:998–1000. doi: 10.2105/AJPH.2004.047225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt RM, Wiemann CM, Rickert VI, Smith EO. Moderate to severe depressive symptoms among adolescent mothers following four year post-partum. Journal of Adolescent Health. 2006;38:712–718. doi: 10.1016/j.jadohealth.2005.05.023. [DOI] [PubMed] [Google Scholar]
- Suplee PD, Bloch JR, McKeever A, Borucki LC, Dawley K, Kaufman M. Focusing on maternal health beyond breastfeeding and depression during the first year postpartum. JOGNN: Journal of Obstetric, Gynecologic & Neonatal Nursing. 2014;43:782–791. doi: 10.1111/1552-6909.12513. [DOI] [PubMed] [Google Scholar]
- Walker L, Timmerman GM, Kim M, Sterling B. Relationships between body image and depressive symptoms during postpartum in ethnically diverse, low income women. Women & Health. 2002;36(3):101–121. doi: 10.1300/J013v36n03_07. [DOI] [PubMed] [Google Scholar]
- Wade TD, Kendler KS. The relationship between social support and major depression: Cross-sectional, longitudinal, and generic perspectives. The Journal of Nervous and Mental Disease. 2000;188:251–258. doi: 10.1097/00005053-200005000-00001. [DOI] [PubMed] [Google Scholar]
- Wills TA, Shinar O. Measuring perceived and received social support. In: Cohen S, Underwood LG, Gottlieb BH, editors. Social support measurement and intervention: A guide for health and social scientists. New York, NY: Oxford University Press; 2000. pp. 86–132. [Google Scholar]


