Abstract
Quinolone resistance of Chlamydia pneumoniae has not been described previously. Serial subcultures of C. pneumoniae under increasing moxifloxacin concentrations (0.0125 to 6.4 mg/liter) resulted in a 256-fold MIC increase compared to moxifloxacin-naive strains. GyrA gene sequencing revealed a novel point mutation with a Ser→Asn substitution. Subcultures under rifalazil and macrolides did not alter the respective MICs.
The 8-methoxy-fluoroquinolone moxifloxacin (BAY 12-8039) has been proved as an efficient drug against all kinds of respiratory pathogens, including Streptococcus pneumoniae, Haemophilus sp., and Moraxella catarrhalis, but also atypical pathogens like Mycoplasma pneumoniae and Chlamydia (Chlamydophila) pneumoniae (12). Emergence of resistance to the newer class of fluoroquinolones in the above-mentioned pathogens is relatively uncommon, currently occurring in approximately 1% of clinical isolates in North America (6). However, C. pneumoniae resistance mutations against quinolones, namely in the gyrA quinolone-resistance-determining region, have not been described in vivo or in vitro so far (5).
We wanted to know whether serial passages of C. pneumoniae in subinhibitory concentrations of moxifloxacin would induce chlamydial resistance to quinolones. Thus, we chose the C. pneumoniae coronary artery isolate CV-6, which was made available to the Centers for Disease Control and Prevention Chlamydia strain collection in 2000, recovered from a chronically infected atheromatous lesion of a 68-year-old male from Northern Germany in 1996 during routine restenosis surgery (7). Susceptibility testing of C. pneumoniae was carried out as shown previously in cell culture with HEp-2 cells (ATCC CCL-23) grown in six-well plates with glass coverslips. After a centrifugation step (1,700 × g for 1 h, 37°C) with 105 inclusion-forming units per ml, the medium was replaced by minimal essential medium containing cycloheximide (1 μg/ml) and moxifloxacin (Bayer Vital GmbH, Leverkusen, Germany) in serial twofold dilutions, starting with the 0.5-fold and 1-fold MIC. Visualization of chlamydial inclusions was performed after incubation at 37°C for 72 h with a fluorescein-conjugated monoclonal anti-Chlamydia lipopolysaccharide antibody (Dako, Hamburg, Germany). Moxifloxacin proved to be highly active against the coronary artery isolate CV-6, showing a MIC of 0.025 mg/liter in a previously described assay (4). Previous studies have shown potent effects of moxifloxacin against standard reference and wild-type C. pneumoniae strains, with MICs ranging from 0.031 to 1.0 mg/liter (8, 10, 13). To induce quinolone resistance, chlamydiae were cultured in six-well plates under increasing doses of moxifloxacin (0.0125 to 6.4 mg/liter; initial inoculum, 106 inclusion-forming units/well) over a total of 40 passages (at 37°C and 5% CO2 for 72 h), splitting the chlamydial inoculum in one culture at the same concentration and one at the twofold moxifloxacin concentration whenever more than 50% of the cell monolayer was infected. Within this prolonged culture period the MIC increased 256-fold (0.025 to 6.4 mg/liter) compared to that for the moxifloxacin-naive CV-6 strain (Fig. 1), which is in contrast to a recent study which found rapid development of fluoroquinolone resistance in subinhibitory concentrations of ofloxacin or ciprofloxacin in Chlamydia trachomatis but not in C. pneumoniae with McCoy cells (11). The propensity of C. pneumoniae to develop drug resistance was investigated in the same manner for rifalazil (ActivBiotics, Lexington, Mass.; MIC, 0.00025 mg/liter), a novel rifamycin, and the macrolides azithromycin (Pfizer, Groton, Conn.; MIC, 0.04 mg/liter) and clarithromycin (Abbot, Wiesbaden, Germany; MIC, 0.04 mg/liter). These drugs did not evoke an increase of their respective MICs.
FIG. 1.
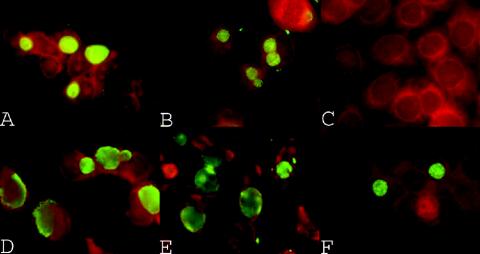
Immunofluorescence staining with monoclonal anti-Chlamydia lipopolysaccharide antibody of HEp-2 cells infected with the C. pneumoniae coronary artery isolate CV-6 (A-C) and the gyrA mutant CV-6 strain (D-F). Growth of untreated chlamydiae is observed without moxifloxacin and at 0.5-fold MIC (A/B) but not at the MIC (0.025 mg/liter) (C). In the gyrA mutant CV-6 strain growth of chlamydiae can still be observed with moxifloxacin concentrations at 64-fold (1.6 mg/liter) and 256-fold (6.4 mg/liter) MIC (E/F).
To assess the underlying resistance mechanism for moxifloxacin, we sequenced the gyrA gene of moxifloxacin-naive and mutant CV-6 strains as described previously (1). A point mutation (G→A) was found leading to a serine-to-asparagine substitution at position 83 (Escherichia coli numbering) in the corresponding gyrase protein. This mutation introduced the recognition site 5′-A▾CGT-3′ (the inverted triangle indicates the cutting site of the enzyme) for the restriction endonuclease HpyCH4IV (New England Biolabs, Frankfurt, Germany), which was used to confirm the sequence data by demonstrating digestion of a 500-bp PCR amplicon (forward, GAT ATC CGG GAT GGA CTC AA; reverse, TGT GGA TTT GCA AGC AGA AG) of the gyrA gene of the mutant but not of the moxifloxacin-naive CV-6 strain.
To analyze the stability of this mutation, the moxifloxacin-resistant CV-6 strain was cultured for more than 10 passages without moxifloxacin. Subsequent gyrA sequencing, restriction enzyme digestion, and MIC determination showed the mutant genotype and phenotype to persist. C. pneumoniae carrying the Ser→Asn substitution showed an eightfold increased MIC for levofloxacin (Aventis Pharma, Bad Soden, Germany) and ciprofloxacin (Bayer Vital GmbH), whereas MICs for rifalazil, azithromycin, clarithromycin, and doxycycline (Sigma-Aldrich, Munich, Germany) remained unchanged (Table 1).
TABLE 1.
Activities of different antibiotics against the vascular C. pneumoniae strain CV-6 and the gyrA mutant straina
| Antimicrobial agent | MIC90 (mg/liter)b for:
|
|
|---|---|---|
| C. pneumoniae | gyrA mutant C. pneumoniae strain | |
| Moxifloxacin | 0.025 | 6.4 |
| Rifalazil | 0.00025 | 0.00025 |
| Azithromycin | 0.04 | 0.04 |
| Clarithromycin | 0.04 | 0.04 |
| Doxycycline | 0.03 | 0.03 |
| Levofloxacin | 0.4 | 3.2 |
| Ciprofloxacin | 1.0 | 8.0 |
After 40 passages in subinhibitory concentrations of moxifloxacin.
MIC90, MIC at which 90% of the strains are inhibited.
Previously, high-level resistance to fluoroquinolones was observed in C. trachomatis L2 reference strains exposed to subinhibitory concentrations of ofloxacin (0.5 mg/liter) and sparfloxacin (0.015 mg/liter) within four rounds of selection. In these quinolone-resistant strains, a point mutation was found in the gyrA quinolone-resistance-determining region leading to a Ser→Ile substitution at position 83 (2), the amino acid also most commonly mutated in quinolone-resistant Enterobacteriaceae (3). Regarding emergence of antibiotic resistance in vitro as a multidimensional event, discrepancies in the mutation rate of C. pneumoniae and C. trachomatis (11) may be based on host-specific (antibiotic-cell interactions) and pathogen-specific (adaptive mutation, bacterial fitness) differences (9). Augmented use of fluoroquinolones as first-line drugs in community-acquired pneumonia and the necessity for recurrent antibiotic treatment in respiratory infections of patients with underlying lung diseases (chronic obstructive pulmonary disease, lung fibrosis, etc.) may promote the development of quinolone-resistant strains of C. pneumoniae in vivo. Further studies are needed to evaluate differences in the disposition of vascular (CV-6) and respiratory (CWL029) chlamydial strains to acquire quinolone resistance mutations, with respect to current clinical studies investigating antibiotic treatment in coronary artery disease patients. The data observed here report for the first time the induction of quinolone resistance in a vascular strain of C. pneumoniae due to a stable point mutation in the gyrA gene featuring a target for endonuclease digestion.
Acknowledgments
We gratefully thank Bayer Vital GmbH, Leverkusen, Germany, and ActivBiotics, Lexington, Mass., for their financial support. This study was partially supported by a grant from the Deutsche Forschungsgemeinschaft (SPP1130 Ma 2070/4-1).
We are grateful to A. Hellberg, A. Gravenhorst, and T. Luedemann (University of Luebeck) for excellent technical assistance.
REFERENCES
- 1.Ameyama, S., Y. Shinmura, and M. Takahata. 2003. Inhibitory activities of quinolones against DNA gyrase of Chlamydia pneumoniae. Antibmicrob. Agents Chemother. 47:2327-2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dessus-Babus, S., C. M. Bébéar, A. Charron, C. Bébéar, and B. de Barbeyrac. 1998. Sequencing of gyrase and topoisomerase IV quinolone-resistance-determining regions of Chlamydia trachomatis and characterization of quinolone-resistant mutants obtained in vitro. Antimicrob. Agents Chemother. 42:2474-2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Everett, M. J., Y. F. Jin, V. Ricci, and L. J. Piddock. 1996. Contributions of individual mechanisms to fluoroquinolone resistance in 36 Escherichia coli strains isolated from humans and animals. Antimicrob. Agents Chemother. 40:2380-2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gieffers, J., W. Solbach, and M. Maass. 1998. In vitro susceptibility of Chlamydia pneumoniae strains recovered from atherosclerotic coronary arteries. Antimicrob. Agents Chemother. 42:2762-2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hammerschlag, M. R., and P. M. Roblin. 2000. Microbiologic efficacy of moxifloxacin for the treatment of community-acquired pneumonia due to Chlamydia pneumoniae. Int. J. Antimicrob. Agents 15:149-152. [DOI] [PubMed] [Google Scholar]
- 6.Jones, R. N. 2002. Microbiology of newer fluoroquinolones: focus on respiratory pathogens. Diagn. Microbiol. Infect. Dis. 44:213-220. [DOI] [PubMed] [Google Scholar]
- 7.Maass, M., C. Bartels, P. M. Engel, U. Mamat, and H. H. Sievers. 1998. Endovascular presence of viable Chlamydia pneumoniae is a common phenomenon in coronary artery disease. J. Am. Coll. Cardiol. 31:823-827. [DOI] [PubMed] [Google Scholar]
- 8.Malay, S., P. M. Roblin, T. Reznik, A. Kutlin, and M. R. Hammerschlag. 2002. In vitro activities of BMS-284756 against Chlamydia trachomatis and recent clinical isolates of Chlamydia pneumoniae. Antimicrob. Agents Chemother. 46:517-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martinez, J. L., and F. Baquero. 2000. Mutation frequencies and antibiotic resistance. Antimicrob. Agents Chemother. 44:1771-1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miyashita, N., H. Fukano, K. Yoshida, Y. Niki, and T. Matsushima. 2002. In-vitro activity of moxifloxacin and other fluoroquinolones against Chlamydia species. J. Infect. Chemother. 8:115-117. [DOI] [PubMed] [Google Scholar]
- 11.Morrissey, I., H. Salman, D. Bakker, D. Farrell, C. M. Bébéar, and G. Ridgway. 2002. Serial passage of Chlamydia spp. in sub-inhibitory fluoroquinolone concentrations. J. Antimicrob. Chemother. 49:757-761. [DOI] [PubMed] [Google Scholar]
- 12.Nightingale, C. H. 2000. Moxifloxacin, a new antibiotic designed to treat community-acquired respiratory tract infections: a review of microbiologic and pharmacokinetic-pharmacodynamic characteristics. Pharmacotherapy 20:245-256. [DOI] [PubMed] [Google Scholar]
- 13.Woodcock, J. M., J. M. Andrews, F. J. Boswell, N. P. Brenwald, and R. Wise. 1997. In vitro activity of BAY 12-8039, a new fluoroquinolone. Antimicrob. Agents Chemother. 41:101-106. [DOI] [PMC free article] [PubMed] [Google Scholar]