Abstract
Background:
Sexually transmitted infections (STIs) are a global health problem. Trends of STIs vary from place to place depending on various epidemiological factors prevailing in that respective geographic area.
Aims and Objectives:
The present study was conducted to find the pattern and prevalence of different STIs out of total STI clinic attendees, to identify any change in the trend of STIs, various epidemiological factors, and behavior of individual diseases.
Materials and Methods:
Case records of the patients, attending the STI clinic (Suraksha Clinic) attached with Department of Dermatology, Venereology, and Leprosy of a tertiary care medical college and hospital of North India from April 2007 to March 2014, were analyzed. All the patients were thoroughly examined and investigated.
Results:
This study included a total of 5468 STI clinic attendees out of which 3908 were diagnosed to have STIs. Most of the patients were male, married, and in the third decade of their lives. In our study, the highest number of patients had herpes genitalis, i.e., 850 patients (21.75%) followed by 415 patients (10.61%) having genital warts. Molluscum contagiosum was present in 239 patients (6.11%), 106 patients (2.71%) had urethral discharge whereas 81 patients (2.07%) diagnosed to have syphilis. Viral infections accounted for 38.48% of cases. Human immunodeficiency virus (HIV) positivity was seen in 414 patients (10.59%) of total STI cases.
Conclusion:
The trend of STIs is changing from bacterial to viral diseases. This is because of the widespread use of antibacterial, self-medication, and treatment through national program. STIs enhance the susceptibility of an individual to acquire or transmit HIV through sexual contact.
Key words: Clinico-epidemiological profile of sexually transmitted infections, human immunodeficiency virus, National AIDS Control Organization, Suraksha Clinic
INTRODUCTION
Sexually transmitted infections (STIs) are a loosely defined as a constellation of infections and syndromes that are epidemiologically heterogeneous, but all of which are almost always or at least often transmitted sexually.[1] STIs are diseases with tremendous health and economic consequences. As per STI prevalence study conducted in 2003, about 6% of the adult population in the country suffers from STIs.[2] The emergence of human immunodeficiency virus (HIV) as a global pandemic has focused greater attention on the control of these diseases as they play an important role in the acquisition and transmission of HIV. The association between STI and HIV has been well established.[3] Several studies have shown that the clinical manifestation of ulcerative STI facilitates the transmission of HIV.[3] A proper knowledge of the pattern of STIs in different geographical regions is necessary for evolving proper control measures. As per statistics released by the National AIDS Control Organization (NACO) 2008–2009, HIV prevalence rate in the general population in the country is 0.29% and HIV prevalence in STI clinic (Suraksha Clinic) is 2.5%.[3] The present study was conducted to find out the pattern and prevalence of STIs in Amritsar and its nearby areas, to identify any change in the trends of STIs, the epidemiological factors and behavior of individual diseases.
MATERIALS AND METHODS
A retrospective analysis of data collected from the clinical records of 5468 patients over a period of 7 years (April 2007–March 2014) was carried out. The data were collected from individuals attending the STI clinic (Suraksha Clinic) attached with the Department of Dermatology, Venereology, and Leprosy of a tertiary care medical college and hospital of North India. All individuals above the age of 15 years presenting to the STI clinic (Suraksha Clinic) were included in the analysis.
Patients were clinically evaluated by trained physicians for STIs. The diagnosis was based on detailed history, clinical examination, and relevant investigations. Gram's stain was done in urethral discharge cases. Serological tests included HIV antibody testing by enzyme-linked immunosorbent assay and Venereal disease research laboratory (VDRL) by Rapid plasma reagin test which was performed in all patients in the Microbiology Department after due counseling and consent. In cases of genital ulcer, dark ground illumination, smear for multinucleated giant cells, Gram's stain, and Giemsa's staining of tissue smears were done.
Data were collected at the first visit. The following characteristics were used for analysis: (1) Demographic information – age and marital status, (2) sexual orientation, and (3) clinical information. All the details of disease including chief complaints at the time of presentation, duration of complaints, and any treatment taken for the complaints were duly noted. Syndromic and clinical diagnosis was made on the basis of clinical features and laboratory investigations. Treatment was provided to the patient as per NACOs guidelines.[2]
RESULTS
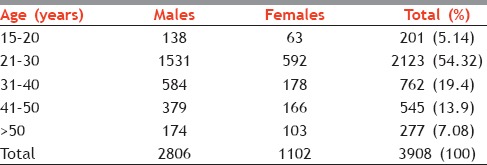
During the study period of 7 years, there were 5468 new clinic attendees. Out of these 5468 new clinic attendees, 3908 were diagnosed to have STIs. The majority of the patients, i.e., 2123 (54.32%) patients were in the third decade of their life (21–30 years) followed by 762 (19.4%) patients were in the 31–40 years of age group [Table 1]; this was true for both males and females. Males outnumbered females, with 2806 (71.8%) males and 1102 (28.19) females, forming a male:female ratio of 2.54:1 [Table 1]. Most of the female attendees, i.e., 986 (89.47%) were married, whereas 1453 (51.78%) male patients were married.
Table 1.
Age and sex distribution (n=3908)
In our study, majority of the attendees, i.e., 586 (20.88%) were a daily wager, 489 (17.42%) were private employees followed by 412 (14.68%) who were farmers. Majority of the female attendees were homemakers. Regarding sexual behavior, 1034 (36.84%) males gave a history of premarital sexual contact, whereas 735 (26.19%) gave a history of extramarital sexual contact. Thirty-six (1.28%) of the male patients were found to be homosexuals. Most of the female attendees, i.e., 904 (82.03%) denied any history of premarital or extramarital contact.
In our study, among the ulcerative group, the majority of the patients had herpes genitalis (HG), i.e., 850 (21.75%), followed by 81 (2.06%) patients with syphilis and 43 (1.10%) patients with chancroid [Table 2]. Lymphogranuloma venereum (LGV) and donovanosis constituted only seven (0.17%) and three (0.07%) cases, respectively [Table 2].
Table 2.
Incidence and distribution of various sexually transmitted infections
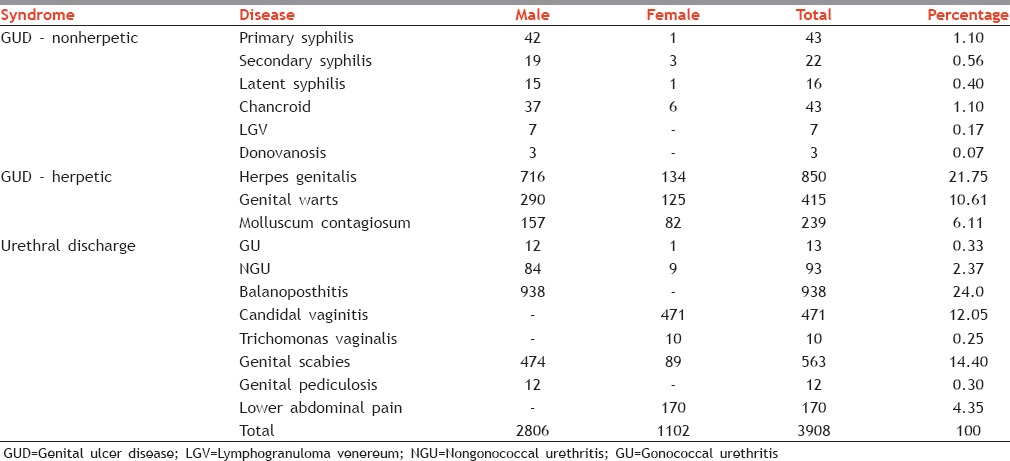
Among the nonulcerative group, genital warts (GW) were present in 415 (10.61%) cases, followed by genital molluscum contagiosum accounting for 239 (6.11%) cases [Table 2 and Figure 1].
Figure 1.
Graph showing diagnosis in the 3908 study cases. GUD-NH = Genital ulcer disease nonherpetic; HG = Herpes genitalis; GW = Genital warts; MC = Molluscum contagiosum; UD = Urethral discharge; BP = Balanoposthitis; CVV = Candidal vulvovaginitis; TV = Trichomonas Vaginalis; GS = Genital scabies; GP = Genital pediculosis; LAP = Lower abdominal pain
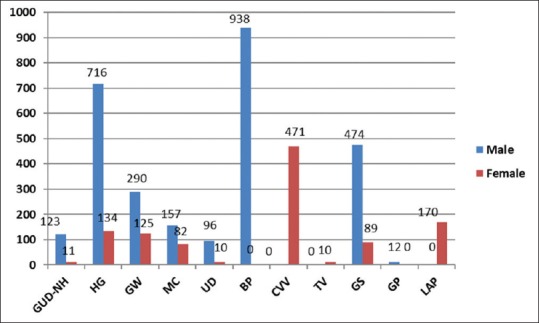
Among the urethritis group, gonococcal urethritis (GU) was present in 13 (0.33%) patients and non-GU (NGU) had higher prevalence present in 93 (2.37%) patients [Table 2]. Viral infections (HG, GW, and molluscum contagiosum) accounted for 1504 (38.48%) patients of all cases [Figure 2].
Figure 2.
The etiological categorization of sexually transmitted infection/reproductive tract infection among the study cases
Out of the protozoal, parasitic, and fungal (PPF) group, majority cases were of fungal diseases, i.e., 1409 (36.05%) patients, followed by parasitic infection seen in 575 (14.71%) patients [Figure 2]. In female, candidal vulvovaginitis in 471 (12.05%) patients whereas 170 patients (4.35%) suffered from lower abdomen pain [Table 2 and Figure 1]. Among male patients, balanoposthitis (BP) was the most common STI seen in 938 patients (24.0%). Genital scabies was observed in 563 (14.40%) patients whereas genital pediculosis was present in 12 (0.30%) patients [Table 2, Figure 1].
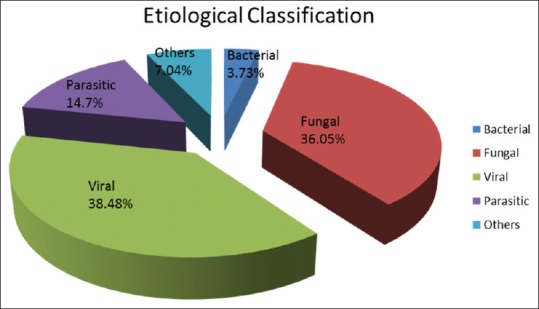
In our study, HIV positivity was seen in 414 patients (10.59%) of total STI cases. Among HIV-positive patients, 142 (34.29%) patients had ulcerative STIs. HG was seen in 134 (32.36%) patients followed by 3 (0.72%) cases of syphilis and 5 (1.20%) cases of chancroid. Nearly 65.70% patients had nonulcerative STI (GW 17.14% and molluscum contagiosum 3.6%) [Figure 3].
Figure 3.
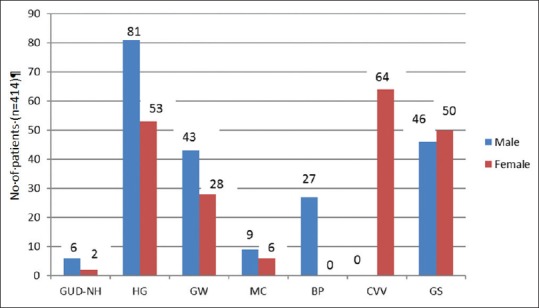
Diagnosis in the 589 study cases in human immunodeficiency virus reactive patients. GUD-NH = Genital ulcer disease-nonherpetic; HG = Herpes genitalis; GW = Genital warts; MC = Molluscum contagiosum; BP = Balanoposthitis; CVV = Candidal vulvovaginitis; GS = Genital scabies
Out of the PPF group, majority cases were suffering from fungal diseases. In females, candidal vulvovaginitis in 64 (15.4%) patients, whereas majority of the male patients, i.e., 27 (6.52%) suffered from BP [Figure 3].
DISCUSSION
Overall, there is a decline in the number of new STI cases, a common observation in various government health facilities[4,5] which could be attributed to the better diagnostic and management facilities by active NACO intervention. A number of epidemiological studies have been done on the pattern and changing trends of STIs.[6,7,8] In our study, the majority of the patients, i.e., 2123 (54.32%) patients were in the age group of 21–30 years as has been seen in other studies also.[6,7,8] This clustering of patients in the above age group is mainly due to the high sexual activity at this age being behaviorally more vulnerable to STI acquisition, as they generally have a higher number of sexual partners and more concurrent partnerships and change in partners more often than older age groups.[7,9,10,11,12] Majority of the patients were male, married, and in the third decade of their life, which is consistent with the studies.[13,14]
The attendance of female was less, which might be due to social and cultural restrictions, the asymptomatic nature of the disease in females, nonavailability of female venereologists, and the fact that female patients prefer to attend the gynecology department for treatment of such problems. Of the affected males, 36.84% gave a history of premarital sexual contact. Married females outnumbered unmarried female patients, which is consistent with other studies.[4,15,16] In the present study, only 51.78% of male patients were married, almost similar findings were observed, i.e., 46.3%,[10] 50%,[11] and 47%[12] in various studies. In our study, heterosexual contact was the most common type of sexual contact accounting for 98.72% which was slightly more than 95.9%[4] and 89.6%[4] in other studies The incidence of homosexual contact was 1.28% in our study as compared with 1.2% in a study by Devi et al.[9]
Out of the various categories of diseases, there was a significant variation in the prevalence of bacterial and viral STIs, with viral STIs dominating. There was a gradual increase in prevalence of viral STIs over a period of 7 years which was 29.8% in the year 2007–2008, 31.3% in the year 2008–2009, 32% in the year 2009–2010, 39.7% in the year 2010–2011, 38.6% in the year 2011–2012, 46.5% in the year 2012–2013, and 47% in the year 2013–2014 [Figure 4]. This dissimilitude in bacterial and viral STIs in the current study the period of 7 years [Figure 2], can be attributed to interplay of various factors such as free availability of antibiotics, self-medications, and syndromic approach adopted by private practitioners as well as government health centers. Furthermore, the trend of STIs is changing from bacterial to viral diseases as suggested by other studies.[8] This is because all the bacterial diseases are almost curable with either one or the other antibiotic or through national control program. On the contrary, the viral diseases are known to persist because of the latency and recur in spite of treatment and are widely spreading in the community.[8] In the present study, HG was the most common STI, with the incidence of 21.75% which was at par with other studies,[7,13] but lesser than that other studies done at Ahmedabad (27.90%)[14] and Kottayam (24.40%)[4] [Table 3].
Figure 4.
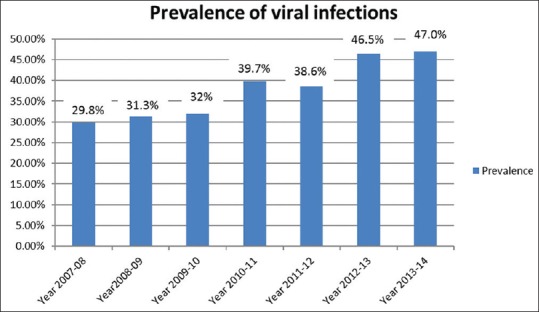
Increase in the prevalence of viral sexually transmitted infections over a period of 7 years
Table 3.
Comparison with other studies
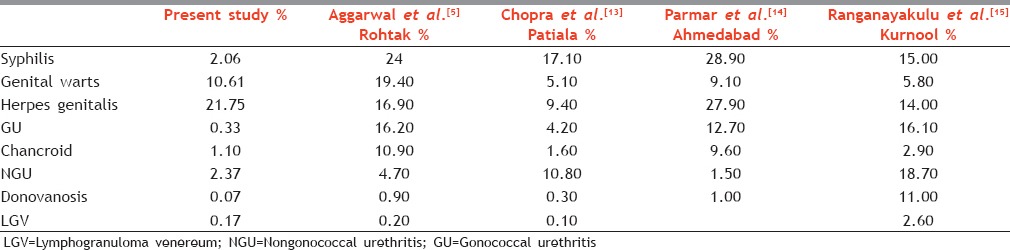
The second most common STI was GW. It was seen in 415 patients (10.61%), which was almost equal to the incidence seen in the studies[7,14] done in the recent past but lesser than Kottayam (17.5%)[4] [Table 3]. Among the urethritis group, GU account for 13 patients (0.33%) which was very less as compared with 7% and 12% by Saikia et al.[10] and Jain et al.,[11] respectively. NGU was seen in 93 patients (2.37%) and was slightly higher than a study done in Ahmedabad (1.50%) [Table 3].[14]
In the present study, VDRL reactivity (confirmed by modified treponema pallidum hemagglutination assay) was seen in 5.4% of total ulcerative STI patients which was much lower than as compared with 14.29%,[14] 15.95%,[7] 42.1%,[4] and 53.3%[17] in other studies. This could be attributed to the widespread use of antibacterials by self-medication as well as prescribed antibiotics for other nonvenereological indications. The incidence of chancroid was found to 1.10% in the present study. Other STIs seen in decreasing order of frequency were LGV (0.17%) and donovanosis (0.07%).
Similar studies at different levels should be conducted to detect the changing trends as they assist in the formulation of the national STD and AIDS control program. The number of new STI cases show a gradual decline overall, a common observation in various government health facilities[3,4] which could be attributed to the better diagnostic and management facilities by active NACO intervention.
In our study, most common STI associated with HIV was HG with the incidence of 32.36% [Figure 3], consistent with Devi et al.[9] study and Kavina et al.[6] study. In the present study, HIV seropositivity among STI patients was 10.59% which was much higher than the national average (2.5%) as per the recent NACO estimates.[3] However, there was a wide variation in HIV seropositivity among STI patients in other studies, i.e., 8.21%,[18] 9.62%, and 17.2%.[10] This could be attributed to the recurrence of the HG which make the patients more prone to acquire HIV and the sociodemographic variations in HIV-infected population. This difference can also attribute to the high prevalence of HIV infection and intravenous drug abuse in the Northeastern part of India.[19,20]
CONCLUSION
The persistent and recurrent nature of viral infections is responsible for their increasing trend in the current STI scenario. HIV and STIs are perfect examples of epidemiologic synergy as they are core transmitters of each other. STI being higher in married individuals further underlines the importance of contact tracing, counseling, and prompt management of the partners. More frequent screening may be appropriate depending on individual risk behaviors, the local epidemiology of STIs, and whether incident STIs are detected by screening or by the presence of symptoms. Hence, more education and counseling are needed with regard to availing the Suraksha Clinic facilities provided by the NACO to decrease the load of STIs and in the HIV in our society.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Marfatia YS, Sharma A, Joshipura SP. Overview of sexually transmitted diseases. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3rd ed. Vol. 59. Mumbai: Bhalani Publishing House; 2008. pp. 1766–78. [Google Scholar]
- 2.National Guideline on Prevention, Management and Control of Reproductive Tract Infections Including Sexually Transmitted Infections. New Delhi: Ministry of Health and Family Welfare, Government of India; 2007. Government of India. [Google Scholar]
- 3.NACO. Department of AIDS Control – Ministry of Health and Family Welfare. Current Epidemiological Situations of HIV/AIDS. Annual Report 2009–2010. [Last Updated on 2017 Feb 15 Cited on 2017 Mar 23]. Available from: http://naco.gov.in/documents/annual-reports .
- 4.Narayanan B. A retrospective study of the pattern of sexually transmitted diseases during a ten-year period. Indian J Dermatol Venereol Leprol. 2005;71:333–7. doi: 10.4103/0378-6323.16784. [DOI] [PubMed] [Google Scholar]
- 5.Aggarwal K, Jain VK, Brahma D. Trends of STDs at Rohtak. Indian J Sex Trans Dis. 2002;23:19–21. [Google Scholar]
- 6.Kavina BK, Billimoria FE, Rao MV. The pattern of STDs and HIV seropositivity in young adult attending STD clinic of Civil Hospital Ahmedabad. Indian J Sex Trans Dis. 2005;26:603. [Google Scholar]
- 7.Murugesh SB, Reddy S, Raghunath S. Pattern of sexually transmitted diseases at Davangere. Indian J Sex Trans Dis. 2004;25:9–12. [Google Scholar]
- 8.Chandra Gupta TS, Badri SR, Murty SV, Swarnakumari G, Prakash B. Changing trends of sexually transmitted diseases at Kakinda. Indian J Sex Trans Dis. 2007;28:6–9. [Google Scholar]
- 9.Devi SA, Vetrichevvel TP, Pise GA, Thappa DM. Pattern of sexually transmitted infections in a tertiary care centre at Puducherry. Indian J Dermatol. 2009;54:347–9. doi: 10.4103/0019-5154.57611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saikia L, Nath R, Deuori T, Mahanta J. Sexually transmitted diseases in Assam: An experience in a tertiary care referral hospital. Indian J Dermatol Venereol Leprol. 2009;75:329. doi: 10.4103/0378-6323.51245. [DOI] [PubMed] [Google Scholar]
- 11.Jain VK, Dayal S, Aggarwal K, Jain S. Changing trends of sexually transmitted diseases at Rohtak. Indian J Sex Transm Dis. 2008;29:23–5. [Google Scholar]
- 12.Kumarasamy N, Balakrishnan P, Venkatesh KK, Srikrishnan AK, Cecelia AJ, Thamburaj E, et al. Prevalence and incidence of sexually transmitted infections among South Indians at increased risk of HIV infection. AIDS Patient Care STDS. 2008;22:677–82. doi: 10.1089/apc.2007.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chopra A, Dhaliwal RS, Chopra D. Pattern of changing trend of STDs at Patiala. Indian J Sex Transm Dis. 1999;20:22–5. [Google Scholar]
- 14.Parmar J, Raval RC, Bilimoria FE. Clinic profile of STDs at Civil Hospital, Ahmedabad. Indian J Sex Transm Dis. 2001;22:14–6. [Google Scholar]
- 15.Ranganayakulu B, Ravikumar GP, Bhaskar GV. Pattern of STDs at Kurnool. Indian J Sex Transm Dis. 1998;19:117–21. [Google Scholar]
- 16.Sharma VK, Khandpur S. Epidemiology of sexually transmitted infections. In: Sharma VK, editor. Sexually Transmitted Diseases and HIV/AIDS. 2nd ed. Vol. 1. New Delhi: Viva Books; 2009. pp. 16–7. [Google Scholar]
- 17.Mewada B, Kotia N, Marfatia YS. Role of VDRL in syndromic management of sexually transmitted diseases. Indian J Sex Trans Dis. 2000;21:38–40. [Google Scholar]
- 18.Zamzachin G, Singh NB, Devi TB. STD trends in regional institute of medical sciences, Manipur. Indian J Dermatol Venereol Leprol. 2003;69:151–3. [PubMed] [Google Scholar]
- 19.NACO. Department of AIDS Control – Ministry of Health and Family Welfare. Current Epidemiological Situations of HIV/AIDS. Annual Report 2012–2013. [Last Updated on 2017 Feb 15 Cited on 2017 Mar 23]. Available from: http://naco.gov.in/documents/annual-reports .
- 20.UNODC. Feature-Drug Users Raise Risk of HIV in India's Heartland. 2013 [Google Scholar]


