Abstract
Objective:
To investigate the speed of action and injection discomfort of 4% articaine and 2% mepivacaine for upper teeth extractions.
Materials and Methods:
Forty-five patients were included in the articaine 4% group, and 45 in the mepivacaine 2% control group. After all injections, soft and hard tissue numbness was objectively gauged by dental probe at intervals of 15 s. Furthermore, the discomfort of the injections were recorded by the patients after each treatment on standard 100 mm visual analog scales, tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm).
Results:
There were significant differences in the meantime of first numbness to associated palatal mucosa and tooth of patients between mepivacaine and articaine buccal infiltration (BI) groups P = 0.01 and 0.01. Patients in the articaine group recorded earlier palatal mucosa and teeth numbness than those in the mepivacaine group. With regards to the discomfort of the needle injections, palatal injection was significantly more painful than BI (t-test: P < 0.001). Articaine buccal injection was significantly more painful than mepivacaine buccal injection (t-test: P <0.001). However, articaine palatal injection was less painful than articaine BI. Clinically, anesthesia onset time was faster in anterior upper teeth than upper middle and posterior teeth.
Conclusions:
BIs with 4% articaine was faster in achieving palate and teeth anesthesia than 2% mepivacaine for extraction of upper maxillary teeth. Patients in mepivacaine BI and articaine palatal injection groups reported less pain with needle injection. Failure of anesthesia was noticeable with maxillary multiple-rooted teeth.
Keywords: Articaine, buccal infiltration, mepivacaine, needle discomfort, teeth extraction
Introduction
Work is still going on by dental clinicians and researchers to find an optimal local anesthetic agent which it has a high potency and rapid onset of action.[1,2,3,4] However, pain-free injection also plays a role in improving the patient perceptions toward the dentist and dental treatments and encouraging patients to attend a regular checkup.[2,5,6] A study by Gazal[3] was carried out to compare the injection pain and speed of local anesthetic effect induced by tissue infiltration of mepivacaine 2% with epinephrine 1:100,000 versus articaine 4% with epinephrine 1:100,000 in securing mandibular first molar pulp anesthesia. The finding of this study showed that the 4% articaine was faster than 2% mepivacaine in anesthetizing the pulps of lower molar teeth after buccal infiltrations (BIs). Earlier lip and teeth numbness were recorded in articaine group. Articaine and mepivacaine BIs were more comfortable than mepivacaine inferior alveolar nerve block (IANB) injections. Plain articaine shows a faster onset of action associated with a shorter time of activity in comparison to plain mepivacaine. In literature, there are many studies reported that the superiority of articaine over other local anesthetic agents.[7,8,9,10,11,12] This statement was explained by the fact that the articaine has great lipid-solubility and potency allowing an increased entry into the neurons.[3,4] An epinephrine-free anesthetic solution of articaine 4% can be used as a possible option in short dental routine treatments instead of using vasoconstrictor-containing local anesthetics.[13] The primary aim of this study is to evaluate the length of time for achieving first numbness to associated soft tissue and teeth following BIs either with 2% mepivacaine or with 4% articaine for achieving maxillary teeth anesthesia. Our null hypothesis stated that the BIs of mepivacaine and articaine have equal length of time for achieving first numbness to associated soft tissue and teeth.
Materials and Methods
This randomized, controlled study was conducted from February 22, 2015, to June 1, 2015. Taibah Dental School Research Ethics Committee had approved the study. Patients who attended the Oral Surgery Department of Taibah University College of Dentistry, scheduled for extraction of teeth under local anesthesia was considered for inclusion in the study. Using convenient sampling pattern, ninety patients were selected to one of the two groups.
Patients who fulfilled the following criteria were eligible for inclusion into the study:
(1) Male aged 16–70 years of age. (2) Scheduled for extraction with upper tooth. (3) American Society of Anesthesiology I or II patients. (4) Where the patient was able to understand and cooperate with the requirements of the protocol and was able and willing to exercise an appropriate written informed consent. Patients were excluded from the study who were allergy to local anesthesia, need multiple upper teeth extraction, and have vomiting reflex.
Prior to the study, a researcher allocated the sequence of patient identity numbers to either the test or control group. Slips of paper with 4% articaine (test group) or 2% mepivacaine (control group) were placed in opaque envelopes and sealed by a secretary who was not associated with the study. These envelopes had been numbered sequentially on their outside with the patient identity number and were attached to the patient's dental hospital treatment record. On dental chair, once the patient signed the consent the attached envelope was opened by the dental assistant who was completely independent of the whole process. If the patient was in mepivacaine or articaine group, the local anesthetic needle was inserted at the depth of the sulcus adjacent to the apical of the tooth listed for extraction and advanced 4–7 mm until an adequate bony contact is achieved then, 1.4 ml mepivacaine 2% or articaine 4% with epinephrine 1:100,000 was delivered slowly over 40 s after aspiration plus a 0.4 ml mepivacaine infiltration in the hard palate 5 mm far from gingival margin over 20 s. No anesthetic solution will be deposited as the needle is advanced to the target site in either regimen.
The discomfort of the injections was recorded by the patients after each treatment on standard 100 mm visual analog scales (VAS), tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm).
After all injections, soft and hard tissue numbness was subjectively gauged by dental probe at intervals of 15 s. After 10 min of injection of local anesthesia, if the anesthetized tooth is still positively sensitized, the second cartridge of LA was administered.
Both patients and the researcher testing anesthetic effectiveness were not aware to which local anesthetic BI regimen was administered. All injections were given by the same operator (GG). Standard aspirating dental cartridge syringes (USA: ATI) fitted with 27-gauge, 21 mm short needles (C-K Ject [27 gauge] 0.4 mm × 21 mm, Korea) were used for buccal and palatal infiltrations.
Data were entered and analyzed in statistical software package SPSS (SPSS 17.0, SPSS, Inc., Chicago, IL, USA).
Results
Ninety-four patients were recruited into this study. Four patients were excluded from this study because they fainted during the administration of local anesthesia and as a consequence, their dental extractions were canceled. In mepivacaine and articaine groups, patients had successful teeth extraction within the study allocated time 10 min. There were four patients in mepivacaine group and only one patient in articaine group who has an anesthetic failure and required additional local anesthetic to carry out the dental extraction.
Time of first numbness to associated buccal, palatal soft tissue, and teeth
The mean time of the first numbness to associated buccal, palatal mucosa, and tooth of the ninety patients who participated in the study was 1.40, 0.71, and 2.66 min (standard deviation [SD] 1.97, 0.72, and 2.64).
The mean time of first numbness to associated buccal, palatal mucosa, and tooth of patients in mepivacaine BI group was 1.74, 0.90, and 3.37 min (SD 2.14, 0.96, and 3.05). Whereas, the mean time of first numbness to associated buccal, palatal mucosa, and tooth of patients in articaine BI group were 1.05, 0.52, and 1.96 min (SD 1.68, 0.20, and 1.93).
There were significant differences in the meantime of first numbness to associated palatal mucosa and tooth of patients between mepivacaine and articaine BI groups P = 0.01 and 0.01 [Table 1 and Figure 1]. In light of this result, patients in articaine group recorded earlier palatal mucosa and teeth numbness than those in mepivacaine group.
Table 1.
Comparisons between mean time of first numbness to associated buccal, palatal mucosa, and tooth of the patients in mepivacaine and articaine infiltration groups
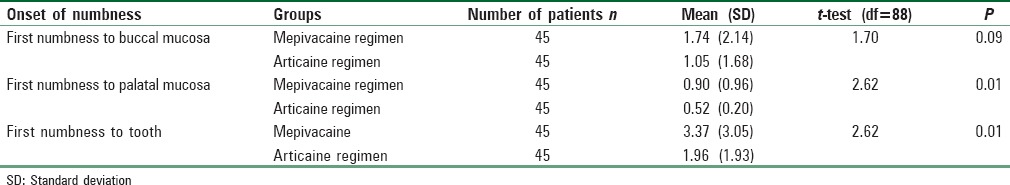
Figure 1.
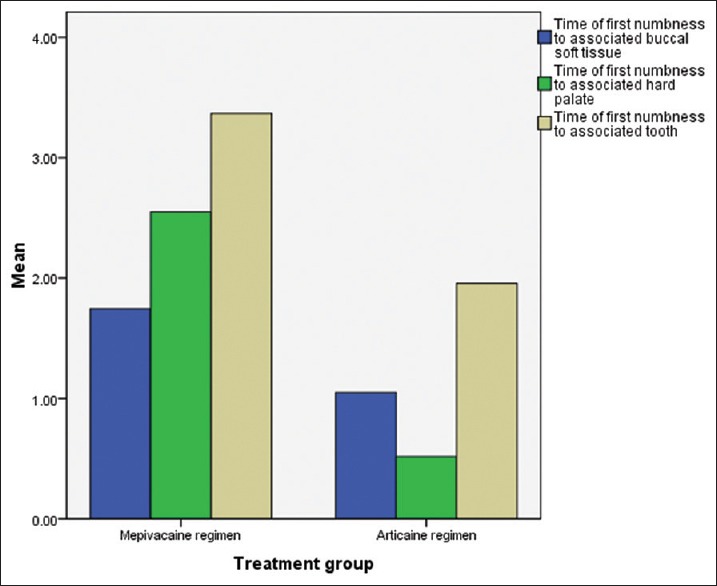
Clustered Bar charts showing the mean time of first numbness to buccal, palatal mucosa, and tooth of patients in the mepivacaine and articaine buccal infiltration groups
There were no significant differences in the meantime of first numbness to associated buccal mucosa of patients between the two BI groups (P > 0.05). However, clinically buccal mucosa numbness was faster in articaine group than patients in the mepivacaine group.
Injection discomfort
The discomfort of the injections was recorded by the patients after each treatment on standard 100 mm VAS, tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm). The range pain injection score of patients in the study was from 0 to 100. The mean pain scores for postbuccal and palatal injections were 43.7 and 48.3 mm, respectively (SD 21 and 20). There were significant differences between the mean pain scores for patients in the postbuccal and postpalatal injection groups (t-test: P < 0.001). Palatal injection was significantly more painful than BI. Articaine buccal injection was significantly more painful than mepivacaine buccal injection [t-test: P < 0.001, Table 2].
Table 2.
Comparisons between mean pain injection scores for patients in the mepivacaine and articaine groups flowing buccal infiltration and palatal injection
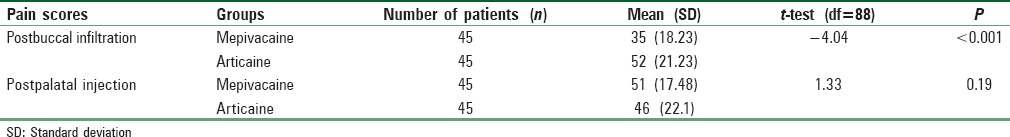
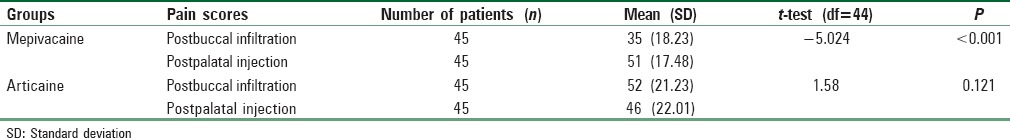
For both mepivacaine and articaine groups, changes in pain injection scores from postbuccal injection score to postpalatal score were made using the paired sample t-test. There was a significant difference for mepivacaine group when comparing the postbuccal scores with the postpalatal injection scores [P < 0.001, Table 3]. Mepivacaine buccal injection was significantly more comfortable than mepivacaine palatal injection. Articaine palatal injection was less painful than articaine BI.
Table 3.
Comparisons between mean postbuccal infiltration and postpalatal injection pain scores for patients in the mepivacaine and articaine groups
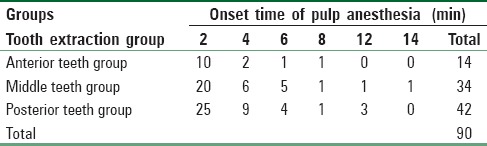
Comparison of speed of action of local anesthesia with extracted teeth morphology
In this study, there were 14 patients who had anterior teeth extraction, 34 had upper premolars extraction, and 42 had molars extraction. Clinically, anesthesia onset time was faster in anterior upper teeth than upper middle and posterior teeth [Table 4]. Five patients with failure anesthesia were found in middle and posterior teeth groups. Teeth with multiple roots might need more local anesthetic than single-rooted teeth.
Table 4.
Description of onset of pulp anesthesia according to tooth pattern
Discussion
The results of this study showed that the patients in articaine group recorded earlier palatal mucosa and teeth numbness than those in mepivacaine group. These differences were statistically significant (P < 0.05). This outcome could be considered as good evidence to conclude that the use of articaine BI was faster in action than mepivacaine for securing pulp anesthesia in maxillary teeth. This result is similar to the findings from the study by Gazal, 2015 who reported that the clinical advantages for using articaine infiltration are including rapid onset, longer duration of action, and greater diffusing property over mepivacaine.[3] These results can be explained by the fact that articaine is amide local anesthesia with a thiophene ring. This aromatic ring has greater fat solubility than a benzene ring found in mepivacaine. However, articaine has a dissociation constant (pKa) of 7.8 and highly protein bound (94%), while mepivacaine has pKa of 7.6 and protein binding of 84%.[14] In light of these facts, mepivacaine has lower pKa which is closer to physiological pH (7.4). This means more uncharged base local anesthetic molecules are present to diffuse through the nerve sheath and as a consequently faster onset time must be achieved.[4,15,16] On the other hand, this study revealed that articaine has slightly faster onset time than mepivacaine. Although the tissue diffusion characteristics of articaine are not well-understood,[1] there is one possible account for the superiority of articaine over mepivacaine in terms of onset time of action. The great lipid solubility of articaine in additional to its high concentration formula as a 4% solution could be the reason for increasing the number of uncharged local anesthetic molecules crossing the nerve membrane.[3,4,17,18] The result of this study is in consistence with the findings of several studies[16,19,20,21] that reported the success of articaine infiltration in achieving faster onset time and more profound level of anesthesia.
Recent evidence has shown that BI with either articaine or lidocaine alone for extraction of primary maxillary molars in children did not achieve palatal anesthesia. Hence, palatal infiltration was needed to complete the whole process of tooth extraction without pain.[22]
Two techniques for local anesthetic injection were investigated in 52 patients who needed simple extractions of bilateral lower first molars teeth by administration of 4% articaine with 1:100,000 epinephrine.[20] One side extraction was done after administration of buccal and lingual infiltrations, while the other side extraction was carried out after giving conventional IANB technique. Pain assessments were recorded after the injections and teeth extractions by both VAS and verbal rating scale. The finding of this study revealed that there were no significant differences in the level of pain between the two techniques either during the administration of local anesthetic or carrying out the teeth extraction. Hence, the extraction of lower mandibular teeth can be done without the administration of IANB.[20] On the other hand, a review study was carried out by Bartlett and Mansoor[23] to determine whether the articaine BIs is equal or more effective than lidocaine IANBs for securing mandibular molars pulpal anesthesia. A full literature search was done by the MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials databases. The result of this review revealed that the studies present a number of weaknesses in their design, so the level of evidence they provide is inconclusive. The effectiveness of articaine BIs was not stronger than lidocaine IANBs.[23] Moreover, a retrospective study was conducted to determine the anesthetic success of the IANB, and supplemental articaine BI for molars and premolars teeth in patients with symptomatic irreversible pulpitis.[24] Two percent lidocaine with 1:100,000 epinephrine was administrated to 375 patients presenting with symptomatic irreversible pulpitis by the IANB techniques. Endodontic treatment which includes endodontic access and instrumentation were started once the patient felt profound lip numbness. During the endodontic treatments, there were 204 patients felt moderate to severe pain and an additional BIs of 4% articaine with 1:100,000 epinephrine was administered to continue the treatment. The findings of this study reported that the success rates for the IAN block and supplemental BI of articaine were not high enough to guarantee deep anesthesia for mandibular teeth with symptomatic irreversible pulpitis.[24]
However, the controversy mentioned above regarding the effectiveness of articaine does not affect the results and conclusion of this study because mepivacaine and articaine BIs were similarly successful in achieving upper teeth anesthesia and extraction. However, articaine was slightly faster than mepivacaine.
Mepivacaine buccal and articaine palatal injections were more comfortable than articaine buccal and mepivacaine palatal injections. Upper simple extraction was successful with a single buccal injection of 4% articaine.[25] The presence of thiophene ring in articaine could be the reason for increase its ability to diffuse through the bone and producing palatal anesthesia after maxillary BI.[3]
Increased discomfort of injection following 2% mepivacaine palatal injection and 4% articaine buccal injection might be as a result of speed of injection or patient with needle phobia.[26,27,28] Meechan reported that the clinical impact of articaine's higher postinjection pain scores than lignocaine is negligible.[29]
Finally, one of the interesting findings in this study was the failure of anesthesia and, extraction was only reported with multiple rooted teeth. Local anesthetic failure is an unavoidable aspect of dental practice. Local anesthetic failure is an unavoidable aspect of dental practice.[30] A number of factors contribute to this, which may be related to either the patient or the operator. Patient-dependent factors may be anatomical, pathological, or psychological.[1,31,32,33]
Conclusions
This investigation has demonstrated that the BI with 4% articaine has rapid onset of action, earlier hard palate, and teeth numbness. Articaine palatal injection was significantly more comfortable than mepivacaine palatal injection. Failure of anesthesia was noticeable with maxillary multiple-rooted teeth.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge all the dentists, dental assistants, receptionists, and oral and maxillofacial unit staff involved with local anesthetic extraction service in the Taibah College of Dentistry for their help and advice.
References
- 1.Gazal G, Fareed WM, Zafar MS. Role of intraseptal anesthesia for pain-free dental treatment. Saudi J Anaesth. 2016;10:81–6. doi: 10.4103/1658-354X.169482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Samadani KH, Gazal G. Effectiveness of benzocaine in reducing deep cavity restoration and post-extraction stress in dental patients. Saudi Med J. 2015;36:1342–7. doi: 10.15537/smj.2015.11.12274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gazal G. Comparison of speed of action and injection discomfort of 4% articaine and 2% mepivacaine for pulpal anesthesia in mandibular teeth: A randomized, double-blind cross-over trial. Eur J Dent. 2015;9:201–6. doi: 10.4103/1305-7456.156811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gazal G, Alharbi AM, Al-Samadani KH, Kanaa MD. Articaine and mepivacaine buccal infiltration in securing mandibular first molar pulp anesthesia following mepivacaine inferior alveolar nerve block: A randomized, double-blind crossover study. Saudi J Anaesth. 2015;9:397–403. doi: 10.4103/1658-354X.159463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stenebrand A, Hakeberg M, Helkimo AN, Koch G, Boman UW. Dental anxiety and oral health in 15-year-olds: A repeated cross-sectional study over 30 years. Community Dent Health. 2015;32:221–5. [PubMed] [Google Scholar]
- 6.Gazal G, Fareed WM, Zafar MS, Al-Samadani KH. Pain and anxiety management for pediatric dental procedures using various combinations of sedative drugs: A review. Saudi Pharm J. 2016;24:379–85. doi: 10.1016/j.jsps.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Somuri AV, Rai AB, Pillai M. Extraction of permanent maxillary teeth by only buccal infiltration of articaine. J Maxillofac Oral Surg. 2013;12:130–2. doi: 10.1007/s12663-012-0396-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kandasamya S, Elangovanb R, Johnb RR, Kumar CN. Removal of maxillary teeth with buccal 4% articaine without using palatal anesthesia – A comparative double blind study. J Oral Maxillofac Surg Med Pathol. 2015;27:154–8. [Google Scholar]
- 9.Darawade DA, Kumar S, Budhiraja S, Mittal M, Mehta TN. A clinical study of efficacy of 4% articaine hydrochloride versus 2% lignocaine hydrochloride in dentistry. J Int Oral Health. 2014;6:81–3. [PMC free article] [PubMed] [Google Scholar]
- 10.Fan S, Chen WL, Yang ZH, Huang ZQ. Comparison of the efficiencies of permanent maxillary tooth removal performed with single buccal infiltration versus routine buccal and palatal injection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:359–63. doi: 10.1016/j.tripleo.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 11.Kakroudi SH, Mehta S, Millar BJ. Articaine hydrochloride: Is it the solution? (92-3).Dent Update. 2015;42:88–90. doi: 10.12968/denu.2015.42.1.88. [DOI] [PubMed] [Google Scholar]
- 12.Shurtz R, Nusstein J, Reader A, Drum M, Fowler S, Beck M. Buffered 4% articaine as a primary buccal infiltration of the mandibular first molar: A prospective, randomized, double-blind study. J Endod. 2015;41:1403–7. doi: 10.1016/j.joen.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 13.Said Yekta-Michael S, Stein JM, Marioth-Wirtz E. Evaluation of the anesthetic effect of epinephrine-free articaine and mepivacaine through quantitative sensory testing. Head Face Med. 2015;11:2. doi: 10.1186/s13005-015-0061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malamed SF. Handbook of Local Anesthesia. 6th Edition. Mosby, USA: 2012. pp. 45–50. [Google Scholar]
- 15.Malamed SF. Articaine versus lidocaine: The author responds. J Calif Dent Assoc. 2007;35:383–5. [PubMed] [Google Scholar]
- 16.Silva CB, Groppo FC, Santos CP, Serpe L, Franz-Montan M, Paula Ed, et al. Anaesthetic efficacy of unilamellar and multilamellar liposomal formulations of articaine in inflamed and uninflamed tissue. Br J Oral Maxillofac Surg. 2016;54:295–300. doi: 10.1016/j.bjoms.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 17.Zain M, Rehman Khattak SU, Sikandar H, Shah SA, Fayyaz R. Comparison of anaesthetic efficacy of 4% articaine primary buccal infiltration versus 2% lidocaine inferior alveolar nerve block in symptomatic mandibular first molar teeth. J Coll Physicians Surg Pak. 2016;26:4–8. [PubMed] [Google Scholar]
- 18.Flanagan DF. The effectiveness of articaine in mandibular facial infiltrations. Local Reg Anesth. 2015;9:1–6. doi: 10.2147/LRA.S94647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Senes AM, Calvo AM, Colombini-Ishikiriama BL, Gonçalves PZ, Dionísio TJ, Sant’ana E, et al. Efficacy and safety of 2% and 4% articaine for lower third molar surgery. J Dent Res. 2015;94(9 Suppl):166S–73S. doi: 10.1177/0022034515596313. [DOI] [PubMed] [Google Scholar]
- 20.Bataineh AB, Alwarafi MA. Patient's pain perception during mandibular molar extraction with articaine: A comparison study between infiltration and inferior alveolar nerve block. Clin Oral Investig. 2016 doi: 10.1007/s00784-016-1712-8. doi:10.1007/s00784-016-1712-8 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Maruthingal S, Mohan D, Maroli RK, Alahmari A, Alqahtani A, Alsadoon M. A comparative evaluation of 4% articaine and 2% lidocaine in mandibular buccal infiltration anesthesia: A clinical study. J Int Soc Prev Community Dent. 2015;5:463–9. doi: 10.4103/2231-0762.167717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mittal M, Sharma S, Kumar A, Chopra R, Srivastava D. Comparison of anesthetic efficacy of articaine and lidocaine during primary maxillary molar extractions in children. Pediatr Dent. 2015;37:520–4. [PubMed] [Google Scholar]
- 23.Bartlett G, Mansoor J. Articaine buccal infiltration vs. lidocaine inferior dental block – A review of the literature. Br Dent J. 2016;220:117–20. doi: 10.1038/sj.bdj.2016.93. [DOI] [PubMed] [Google Scholar]
- 24.Fowler S, Drum M, Reader A, Beck M. Anesthetic success of an inferior alveolar nerve block and supplemental articaine buccal infiltration for molars and premolars in patients with symptomatic irreversible pulpitis. J Endod. 2016;42:390–2. doi: 10.1016/j.joen.2015.12.025. [DOI] [PubMed] [Google Scholar]
- 25.Luqman U, Majeed Janjua OS, Ashfaq M, Irfan H, Mushtaq S, Bilal A. Comparison of articaine and lignocaine for uncomplicated maxillary exodontia. J Coll Physicians Surg Pak. 2015;25:181–4. [PubMed] [Google Scholar]
- 26.Kanaa MD, Whitworth JM, Meechan JG. A prospective randomized trial of different supplementary local anesthetic techniques after failure of inferior alveolar nerve block in patients with irreversible pulpitis in mandibular teeth. J Endod. 2012;38:421–5. doi: 10.1016/j.joen.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 27.Beena JP. Dental subscale of children's fear survey schedule and dental caries prevalence. Eur J Dent. 2013;7:181–5. doi: 10.4103/1305-7456.110166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alsarheed M. Children's perception of their dentists. Eur J Dent. 2011;5:186–90. [PMC free article] [PubMed] [Google Scholar]
- 29.Meechan JG. The use of the mandibular infiltration anesthetic technique in adults. J Am Dent Assoc. 2011;142(Suppl 3):19S–24S. doi: 10.14219/jada.archive.2011.0343. [DOI] [PubMed] [Google Scholar]
- 30.Meechan JG. How to overcome failed local anaesthesia. Br Dent J. 1999;186:15–20. doi: 10.1038/sj.bdj.4800006. [DOI] [PubMed] [Google Scholar]
- 31.Gazal G, Tola AW, Fareed WM, Alnazzawi AA, Zafar MS. A randomized control trial comparing the visual and verbal communication methods for reducing fear and anxiety during tooth extraction. Saudi Dent J. 2016;28:80–5. doi: 10.1016/j.sdentj.2015.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matthews R, Ball R, Goodley A, Lenton J, Riley C, Sanderson S, et al. The efficacy of local anaesthetics administered by general dental practitioners. Br Dent J. 1997;182:175–8. doi: 10.1038/sj.bdj.4809337. [DOI] [PubMed] [Google Scholar]
- 33.Kwon H, Shin Y, Cho SY, Park SH, Jung IY. Factors affecting the success rate of buccal infiltration anaesthesia in the mandibular molar region. Int Endod J. 2014;47:1117–22. doi: 10.1111/iej.12259. [DOI] [PubMed] [Google Scholar]


