Abstract
Airways management in thoracic surgery is usually more difficult than in other surgery. We reported a case of a patient who underwent surgery of evacuation of empyema where after a correct insertion of a left double-lumen tube 37 Fr (DLT), one-lung ventilation was not permitted by the high airways pressure. In fact, the hole of bronchial tip was just against the left bronchial wall retracted probably from inflammatory process. We introduced blindly an Arndt blocker 9 Fr inside the tracheal lumen of DLT until the orifice of the right upper lobe bronchus, the distance was checked before. After the positioning of the blocker, the DLT was pulled up to above the carina, and the single-lung ventilation was permitted. Sometimes, an unusual use of different devices permits to manage complications. In fact, in this case, the Arndt bronchial blocker helps us to solve an important ventilatory problem.
Keywords: Arndt bronchial blocker, double-lumen tube, One-lung ventilation
Introduction
Correct airways management in thoracic surgery is so complicated that it requires extensive skills even for expert anesthesiologists.[1,2]
In fact, one-lung ventilation in thoracic surgery is assured usually with one or the other device, but in this case, we used the two devices simultaneously to resolve an important ventilatory problem.
Case Report
The patient was a 68-year-old male with a previous history of pleuritis from tuberculosis etiology. The patient was hospitalized due to a fever, night sweats, fatigue, and dyspnea for about 1 month. The chest–abdomen computed tomography examination showed a “loculated right pleural effusion characterized by thickened walls with enhancement and the presence of air bubbles, fibrothorax with reduced volume of the hemithorax, apical pleural thickening, extensive and diffuse pleural calcified plaques, fibrotic shoots fragmented with areas of consolidation in the lower lobe of the left lung.”
After improvement of his clinical conditions, due to a placement of pleural drainage, the patient underwent surgery of evacuation of the loculated empyema.
The patient was intubated with a left-sided double-lumen endotracheal tube 37 Fr. The intubation appeared smooth and proper placement of the double-lumen tube (DLT) was evaluated by bronchoscope.
The patient was positioned on his left side, and the correct positioning of the DLT was Re-evaluated. Before opening, the pleural, left one-lung ventilation was set as controlled pressure ventilation with positive end-expiratory pressure of 5 cm H2O and initially paw of 15 cm H2O, increased to a pressure of 25 cm H2O due to a failure to reach an adequate tidal volume.
The high airway resistance was detected by manual ventilation of the left lung.
The ventilation was changed to controlled volume ventilation; however, a tidal volume of 150–200 ml determined the achievement of peak paw exceeding 38–40 cm H2O.
A further control was carried out with the bronchoscope, and it showed the correct placement of the DLT. The bronchial cuff was seen at the level of the carina while the hole of the bronchial lumen was positioned against the lateral wall of the left main stem bronchus.
At the first time, the surgery begun because it did not involve resection of parenchyma, but only cleaning the pleural cavity and during this step, we alternated phases of double-lung ventilation with phases of apnea.
During maneuvers on the airways, oxygen saturation (SpO2) was maintained >95% with a fraction of inspired oxygen of 0.5 and simultaneously hypercapnia was established with end-tidal CO2 values between 50 and 60 mmHg.
After 30 minutes from beginning of surgery the surgeon requested one-lung ventilation to continue the surgery, in the presence of a swollen parenchyma, a fibrous thickening of the pleura, and numerous nonremovable tacks.
Therefore, we introduced the bronchoscope in the tracheal lumen of the DLT to the orifice of the right upper lobe bronchus, and this distance was recorded. The bronchoscope was extracted, and we introduced an Arndt blocker (Cook Ltd. - 9 Fr) through the same tracheal lumen to the depth previously recorded.
The dimension of the tracheal lumen did not permit us to introduce the two devices simultaneously. Subsequently, the cuff of the blocker was inflated and the surgeon checked if the lung was ventilated or not. After the DLT was pulled up to above the carina and the patient was ventilated as if the DLT was a single tube. Adequate ventilation permitted to raise the PaCO2 values to 38–40 mmHg while the SpO2 was always above 95%. The patient was extubated without complications in the surgery room and after an appropriate observation, he was transferred to the ward.
Discussion
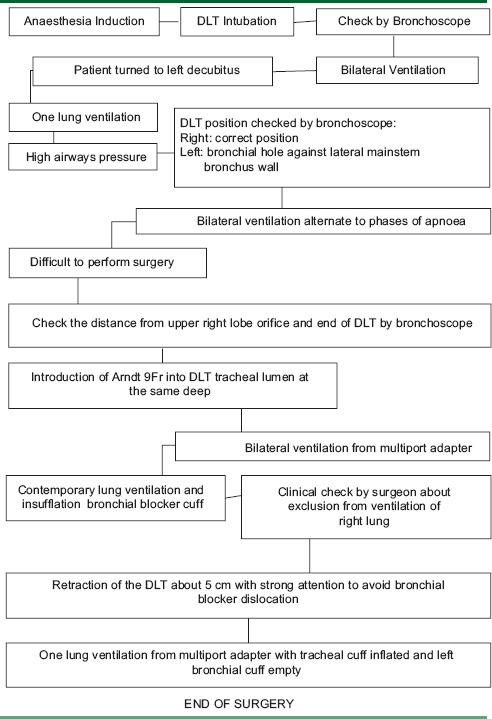
This very challenging experience, as the diagram summarizes [Table 1], allows us to emphasize some points.
Table 1.
Diagram step by step of procedures
Probably, the difficulty ventilation, clinically evident after placing the patient on the left side lateral decubitus position, is related to the previous fibrosis and inflammatory status of the contralateral lung, which could have led to an anomalous traction of the left main stem bronchus.
We never thought that the high airway pressures were caused by a bronchospasm because the lung auscultation did not present the typical expiratory noise of an airway constriction, and the SpO2 was always more than 95%.
There was certainly an underestimation on our part of by the status of lung fibrosis and the presence of a chronic inflammation. We could not, however, imagine that this status of the lungs could alter the anatomical arrangement of the main left bronchus also because the ventilator impairment was manifested after the lateral decubitus.
The preintubation bronchoscopy although it is useful for identifying anatomical abnormality is not routinely performed by us because it is time consuming.[3,4]
Furthermore, in this clinical case, the difficulty was not to insert the left DLT, but it was to ventilate a cause of the conflict between the tip of the tube and the bronchus wall.
When the difficult ventilation occurred, we thought about a dislocation of DLT and its position has been repeatedly checked with the bronchoscope, so we reasoned that the only other thing to do was to reposition the patient in the supine position and replace the DLT with a bronchial blocker (BB).[5,6]
This possibility was not considered for several reasons: to replace an endotracheal tube always has a risk of losing control of the airways, the repeated intubations increase the trauma of the upper airways, and we thought that the surgery would been simpler, less complicated, and short term.[7]
The use of the BB in an unusual way seemed to be the only possible alternative avoiding tube replacement.[8]
The blindly procedure was necessary because it is difficult to introduce into a tracheal lumen a bronchoscope size 3.5 coupled with an Arndt BB 9 Fr.
We usually prefer the EZ-blocker in cases of difficult intubation or prolonged postoperative ventilation, but in this case, Arndt blocker was the right device.[9,10]
We reiterate that in thoracic surgery, in front of anatomical variables, it is necessary to know the different devices for airway management as well as to be able to use the bronchoscope to solve all the situations that may occur in this type of surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Purohit A, Bhargava S, Mangal V, Parashar VK. Lung isolation, one-lung ventilation and hypoxaemia during lung isolation. Indian J Anaesth. 2015;59:606–17. doi: 10.4103/0019-5049.165855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campos JH, Hallam EA, Van Natta T, Kernstine KH. Devices for lung isolation used by anesthesiologists with limited thoracic experience: Comparison of double-lumen endotracheal tube, Univent torque control blocker, and Arndt wire-guided endobronchial blocker. Anesthesiology. 2006;104:261–6. doi: 10.1097/00000542-200602000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Watson CB. Fibreoptic bronchoscopy in thoracic anesthesia. In: Cohen ED, editor. Textbook of Thoracic Anesthesia. Philadelphia, PA: Springer-Verlog; 2004. p. 1. [Google Scholar]
- 4.Moon YJ, Kim SH, Park SW, Lee YM. The implications of a tracheal bronchus on one-lung ventilation and fibreoptic bronchoscopy in a patient undergoing thoracic surgery: A case report. Can J Anaesth. 2015;62:399–402. doi: 10.1007/s12630-014-0293-8. [DOI] [PubMed] [Google Scholar]
- 5.Clayton-Smith A, Bennett K, Alston RP, Adams G, Brown G, Hawthorne T, et al. A Comparison of the efficacy and adverse effects of double-lumen endobronchial tubes and bronchial blockers in thoracic surgery: A systematic review and meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth. 2015;29:955–66. doi: 10.1053/j.jvca.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 6.Bauer C, Winter C, Hentz JG, Ducrocq X, Steib A, Dupeyron JP. Bronchial blocker compared to double-lumen tube for one-lung ventilation during thoracoscopy. Acta Anaesthesiol Scand. 2001;45:250–4. [PubMed] [Google Scholar]
- 7.Narayanaswamy M, McRae K, Slinger P, Dugas G, Kanellakos GW, Roscoe A, et al. Choosing a lung isolation device for thoracic surgery: A randomized trial of three bronchial blockers versus double-lumen tubes. Anesth Analg. 2009;108:1097–101. doi: 10.1213/ane.0b013e3181999339. [DOI] [PubMed] [Google Scholar]
- 8.Matsunami S, Komasawa N, Minami T. Combination of a double-lumen tracheal tube and bronchial blocker for a patient with continuous bleeding due to invasive lung infection. J Clin Anesth. 2015;27:430–1. doi: 10.1016/j.jclinane.2015.03.033. [DOI] [PubMed] [Google Scholar]
- 9.Campos JH. Which device should be considered the best for lung isolation: Double-lumen endotracheal tube versus bronchial blockers. Curr Opin Anaesthesiol. 2007;20:27–31. doi: 10.1097/ACO.0b013e3280111e2a. [DOI] [PubMed] [Google Scholar]
- 10.Campos JH. Lung isolation techniques for patients with difficult airway. Curr Opin Anaesthesiol. 2010;23:12–7. doi: 10.1097/ACO.0b013e328331e8a7. [DOI] [PubMed] [Google Scholar]


