Abstract
Shigella flexneri is a gram-negative bacterium that causes bacillary dysentery in humans that is characterized by an acute inflammatory response of the colon. The fate of phagocytes that are infected in vitro with virulent Shigella has been the subject of some investigation and debate. In this study we found that virulent Shigella caused a rapid increase in the cell membrane permeability of infected human monocyte-derived macrophages (HMDM) but not in the cell membrane permeability of monocytes, as demonstrated by the uptake of fluorescent vital dyes. Within 2 h of infection, 59% ± 6% of the HMDM and ≤4% of the monocytes were stained with propidium iodide. Treatment of the cells with the inhibitors of caspases YVAD and zVAD, the antioxidants N-acetyl-l-cysteine and butylated hydroxyanisole, or an inhibitor of NADPH oxidase, diphenyleniodonium, did not alter the infection outcome. Importantly, we found that virulent Shigella caused a rapid drop in the ATP level to about 50% in infected HMDM. Furthermore, using a combination of fluorescent vital dyes and mitochondrial membrane potential-sensitive dyes, we observed that cells that exhibited a permeable cell membrane were not stained by the mitochondrion-specific dyes, indicating that the mitochondrial membrane potential was lost in these cells. We also observed infected cells that were not stained with either type of dye, indicating that the loss of the mitochondrial membrane potential preceded the increase in cell membrane permeability. Taken together, our studies showed that virulent Shigella flexneri targets the host cell mitochondria for destruction. This activity may account for the necrotic cell death precipitated by these pathogens.
Shigella flexneri is a gram-negative enteric pathogen that causes dysentery, an acute inflammatory disease of the colon. Worldwide, the number of Shigella cases exceeds 150 million per year (22). Young children and infants are particularly vulnerable to Shigella, and more than 65% of the casualties are in this age group. Despite the fact that Shigella was discovered almost a century ago (35), the mechanisms underlying Shigella-induced disease is still an ongoing area of research.
Shigella enters the intestinal epithelium via specialized epithelial cells, known as M cells, that overlie lymphoid follicles in the colon (18). The M cells selectively bind and deliver pathogens to the resident macrophages, T and B cells that are present in the mucosal lymphoid layer directly beneath them (25, 26). The response of the phagocytes to the bacterial challenge is therefore central to progression of the disease. The fate of phagocytes infected with virulent Shigella has been the subject of some investigation and debate. Rapid changes in the cell membrane permeability were noted within a couple of hours following infection of J774 cells, a murine macrophage cell line (5, 42). However, since the cells also displayed apoptotic features that included nucleus condensation and DNA fragmentation, it was concluded that Shigella triggered apoptosis in J774 cells (42). These findings were recently disputed by Nonaka et al. (30). Infection of human neutrophils (9) or human monocyte-derived macrophages (HMDM) (7) with virulent Shigella caused a rapid disruption of the cell membrane in the absence of other apoptotic features. Based on these data, it was concluded that Shigella-infected human macrophages and neutrophils die by a nonapoptotic-necrotic mechanism (7, 9). A contrary conclusion, that Shigella kills human macrophages by an apoptotic mechanism, has also been reported (11, 16). In a recent report the workers concluded that human monocytes phagocytose and kill virulent Shigella and then die by apoptosis within 6 to 8 h after infection (12).
The cytotoxic effect of virulent Shigella on cultured human monocytes and HMDM resembles, but is not identical to, the cytotoxic effect of Salmonella. Apparently, Salmonella kills macrophages by two distinct mechanisms. The first type of cell death was observed within 2 h of infection and was characterized by necrosis-like features that included an increase in the cell membrane permeability in the absence of either nuclear condensation or caspase-3 activation (3). Furthermore, the mitochondria in bone marrow-derived macrophages infected with wild-type Salmonella had a disrupted morphology characterized by swelling and the disappearance of cistae (13). The second type of cell death attributed to Salmonella was characterized by features more typical of apoptosis, including chromatin condensation and DNA breakage (4, 28). A recent report showed that SipB, a Salmonella protein that is delivered into host cells by the type III secretion system, is localized to the host cell mitochondria and is cytotoxic to cells (13).
Confirming previous reports (7), in this study we demonstrated that virulent Shigella causes rapid, caspase-independent disruption of the cell membrane permeability of infected HMDM but not monocytes. Furthermore, the Shigella infection-induced change in cell membrane permeability correlates with, and is preceded by, an abrupt drop in the ATP level in infected HMDM and a rapid collapse of the mitochondrial membrane potential. These findings place Shigella in a growing group of viruses and bacterial pathogens that target proteins to the host cell mitochondria (2). Loss of mitochondrial functions may lead to the necrosis seen in Shigella-infected macrophages.
MATERIALS AND METHODS
Isolation and culture of human monocytes and HMDM.
Monocytes were isolated from buffy coats derived from peripheral blood of healthy donors. The buffy coats were purchased from the New York Blood Center. The buffy coats were mixed with an equal volume (40 ml) of Hanks' buffered saline solution (HBSS) (Gibco) and layered at a ratio of 2:1 (buffy coat suspension/Ficoll medium) on Ficoll-Hypaque Plus medium (Amersham ICN) in 15-ml centrifuge tubes and spun for 20 min at 2,000 rpm in a Beckman TJ-6 centrifuge. The layer containing the peripheral blood mononuclear cells was collected, resuspended in 20 ml of HBSS, and recentrifuged for 10 min at 1,000 rpm. After two washes in HBSS, the cells were resuspended at a density of 5 × 106 cells/ml in RPMI medium containing 2.5% human type AB serum (Sigma). The cells were plated at a concentration of 100 μl per well in non-tissue-culture-treated, flat-bottom, 96-well Microtest plates (Falcon) or at a concentration of 1 ml per well in non-tissue-culture-treated 35-mm dishes. Nonadherent cells were removed after 4 h, which left a population that was approximately 10% of the original number of cells firmly attached. The cells were subsequently cultured in RPMI medium containing 5% human type AB serum in an atmosphere containing 5% CO2. Cells were termed monocytes if they were used within 24 h after isolation. Monocyte-derived macrophages were cultured for a minimum of 7 days. The cultures were fed every 3 days.
Where indicated below, the cultures were treated with an inhibitor of caspase-1, YVAD-cmk (100 μM; Calbiochem), or with the pancaspase inhibitor zVAD(Ome)FMK (Enzyme Systems Products) at a concentration of 25 or 100 μM. An inhibitor of NADPH oxidase, diphenyleniodonium (Sigma), was used at a concentration of 10 μM, and the antioxidant N-acetyl-l-cysteine (Sigma) was used at concentration of 25 mM. Butylated hydroxyanisole (Sigma) was used at a concentration of 100 μM. Cyclosporin A (Sigma) was used at a concentration of 0.5 μM.
Bacterial infection.
The bacterial strains used in this study have been described previously (7). Bacterial stocks were frozen in dimethyl sulfoxide and kept at −70°C. Overnight cultures were inoculated by placing 50 μl of the bacterial stock in 3 ml of Luria-Bertani medium. The cultures were kept on a shaker in a 37°C incubator. Logarithmic cultures were obtained by diluting 50 μl of the overnight culture in 3 ml of fresh Luria-Bertani medium. The cultures were incubated on the shaker for 3 h. The bacterial cultures were then centrifuged for 10 min at 2,000 rpm. Each resulting pellet was resuspended in HBSS. This process was repeated twice. The pellet obtained was resuspended in HBSS, and the absorbance at 450 nm was adjusted to 0.1. Serial dilution and plating on tryptic soy agar with 0.01% Congo red and 0.2% galactose demonstrated that this regimen yielded a concentration of 3 × 107 to 5 × 107 bacteria/ml. Cells were infected at a multiplicity of infection of 100:1. The bacteria were centrifuged onto cells at 950 × g for 5 min. The infected cells were then incubated at 37°C for 25 min. At 30 min postinfection the medium was removed and replaced with RPMI medium containing 5% AB serum supplemented with 50 μg of gentamicin per ml. The plates were analyzed immediately (at 30 min) or were returned to the incubator until they were needed.
Analysis of the cell membrane permeability by fluorescence microscopy.
Time-dependent changes in cell membrane permeability were monitored by fluorescence microscopy by using two DNA binding dyes, the green fluorescent dye Syto 9 and the red fluorescent vital dye propidium iodide (PI) (Molecular Probes), as described previously (29). A stock of the dyes was made by diluting each dye at a ratio of 1:200 in HBSS. Aliquots (5 μl) of the stock containing the two dyes were added to wells at the time indicated below. The cells were incubated with the dyes for 5 min, and the wells were then washed with fresh HBSS. The stained cells were examined by using a Nikon Eclipse TE 200 inverted microscope equipped with ×4 and ×10 objectives; the entire surface of the well was viewed with the ×4 objective. Although dead cells are stained by both PI and Syto 9, PI, which has a greater affinity for DNA than Syto 9, displaces Syto 9 when both dyes are present in the same cell. Dead cells therefore appear red, while the cells with an intact membrane appear green. Green and red fluorescent images were collected by using a Spot imaging system (Diagnostic Instruments Inc.) and were analyzed by using the IP Lab image analysis software (Scanalytic Inc.). Each data point was based on observation of at least three wells, and the data were expressed as means ± standard errors of the means for three or more independent experiments.
Confocal microscopy.
Cells were plated in 35-mm dishes containing non-tissue-culture-treated plastic Thermanox coverslips (Fisher). On the day of the experiment the cells were infected and/or treated as described above. At the time indicated below, the cells were stained with 1 μM Hoechst 33342 (Sigma), 100 nM Mitotracker Orange (Molecular Probes), and the green fluorescent vital dye Sytox (Molecular Probes) at a concentration of 10 nM. In one set of experiments the cells were stained with 100 nM Mitotracker Green (Molecular Probes) and PI. Prior to the analysis, the coverslips were removed from the dye-containing medium, inverted, and placed onto glass bottom culture dishes (MakTek Corporation) for viewing. Confocal images were obtained with a Zeiss LSM 510 laser scanning microscope equipped with the Axiovision Viewer software.
Measurement of superoxide production.
The production of superoxide (O2·−) was determined based on the superoxide dismutase-inhibitable reduction of cytochrome c (32). To measure the release of superoxide, the growth medium was replaced with a solution containing 200 μM cytochrome c (Sigma) in HBSS supplemented or not supplemented with 50 μg of superoxide dismutase (Sigma) per ml. The reaction mixtures were examined at 550 nm. To establish the background for each sample, a reading for each plate was taken immediately prior to infection. The infected cultures were analyzed immediately after centrifugation of the bacteria onto the cells and subsequently at 30-min intervals for a total of 2 h. After the background values were subtracted, the superoxide production was calculated as follows: (absorbance at 550 nm × 100)/6.3 (32).
Analysis of intracellular ATP levels.
The level of ATP was determined by using an ApoGlow kit (Cambrex) according to the manufacturer's protocol.
RESULTS
Wild-type Shigella triggers a rapid change in the cell membrane permeability of HMDM but not in the cell membrane permeability of monocytes.
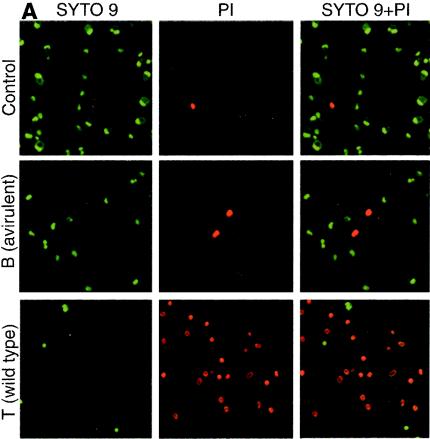
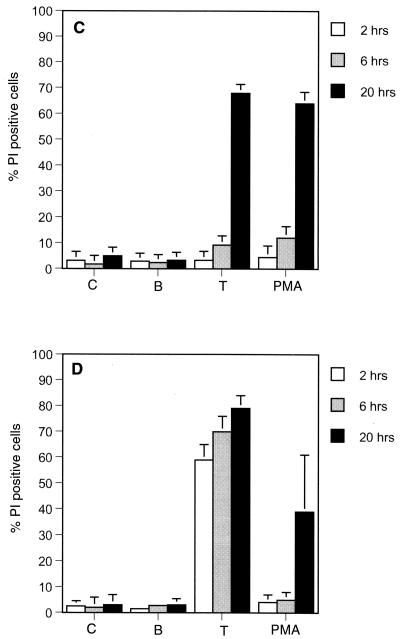
The effect of Shigella infection on cell membrane permeability was determined in previous studies based on the release of intracellular lactate dehydrogenase or loaded 51Cr or by analysis of PI uptake by flow cytometry (7, 30, 42). One objective in this study was to examine the temporal correlation between the change in cell membrane permeability and other intracellular events that take place in the same cell. To this end, the effect of Shigella on cell viability was examined by using a microscopy-based assay with two fluorescent dyes, the red-fluorescing membrane-impermeable dye PI and the green-fluorescing membrane-permeable dye Syto 9 (29). In preliminary studies, cells were stained and analyzed by fluorescence microscopy within 30 min of infection and subsequently at 30-min intervals. Significant numbers of PI-positive cells were seen only at 2 h postinfection. Based on these initial findings, cell viability was examined by using HMDM (Fig. 1A and C) and monocytes (Fig. 1B) at 2, 6, and 20 h postinfection (Fig. 1). Images were acquired and analyzed as described in Materials and Methods. In each case cultures either were not treated (control) or were infected with the avirulent plasmid-cured Shigella flexneri 2a strain BS103 or the wild-type S. flexneri 2a strain 2457-T. HMDM images obtained 2 h postinfection are shown in Fig. 1A. Uninfected monocytes and HMDM excluded PI for the duration of the experiment (Fig. 1), and identical results were observed following infection with either an IpaB deletion mutant strain (S. flexneri 2a strain SF620 [Fig. 1B and C]) or the plasmid-cured strain BS103 (Fig. 1A and Fig. 2). Monocytes infected with 2457-T or SF620 complemented with an IpaB-expressing plasmid (SF620PcB) excluded PI for the first 6 h postinfection (Fig. 1B). Identical results were obtained with opsonized bacteria (data not shown). In contrast, 59% ± 6% and 70% ± 6% of the HMDM were PI positive, respectively, within 2 to 6 h after infection with wild-type Shigella (Fig. 1A and C and 2). Infection with the SF620PcB strain produced identical results (Fig. 1C). By 20 h postinfection with 2457-T and SF620PcB, 68% ± 15% and 64% ± 14% of the monocytes, respectively, and 79% ± 5% and 90% ± 5% of the HMDM, respectively, were PI positive (Fig. 1B and C). The appearance of PI-positive monocytes by 20 h reflected the delayed change in the cell membrane permeability that is seen when cells die by apoptosis. This interpretation is consistent with previously published reports demonstrating that Shigella triggers apoptosis of infected human monocytes (7, 12). In contrast, the rapid loss of cell membrane permeability in approximately 60% of the HMDM within 2 h after infection strongly argues that Shigella killed these cells by a more acute mechanism resembling oncosis or necrosis (7).
FIG. 1.
Wild-type Shigella affects the cell membrane permeability of monocyte-derived macrophages but not the cell membrane permeability of monocytes. (A) Monocyte-derived macrophages that were not treated (control) or were examined 2 h after infection with two Shigella strains, the avirulent plasmid-cured derivative strain BS103 [B (avirulent)] and wild-type strain 2457-T [T (wild type)]. The cells were stained with a combination two fluorescent dyes, Syto 9 and PI, and were analyzed by fluorescence microscopy. Single and dual fluorescence images are shown. (B and C) Monocytes (B) and monocyte-derived macrophages (C) were not treated (control [C]) or were examined 2, 6, or 20 h after infection with the wild-type strain (T), the IpaB deletion mutant strain (SF620), or the IpaB deletion mutant-complemented strain (SF620PcB) of Shigella. The cells were stained with Syto 9 and PI and analyzed by fluorescence microscopy. The data are expressed as percentages of PI-positive cells per field. The bars indicate averages and the error bars indicate standard errors of the means for four independent experiments.
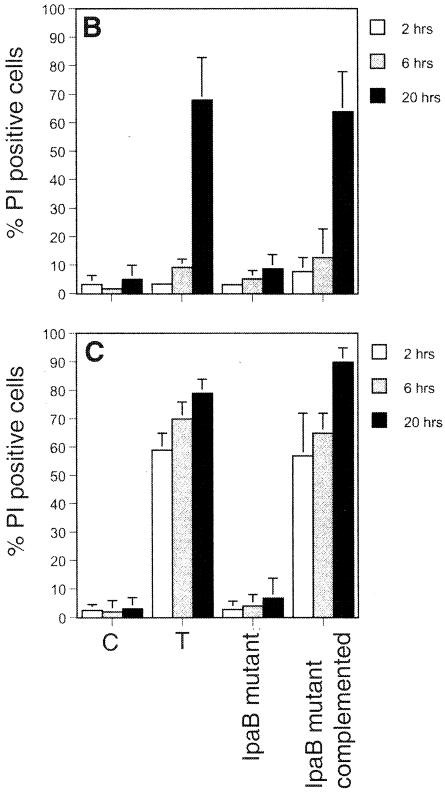
FIG. 2.
Caspase inhibitors YVAD and zVAD do not prevent the increase in cell membrane permeability of monocyte-derived macrophages triggered by wild-type Shigella. Monocytes (A and C) and monocyte-derived macrophages (B and D) were not treated (control [C]) or were examined 2, 6, or 20 h after infection with the avirulent strain (B) or the wild-type strain (T) of Shigella. Some cells were treated for 30 min with 100 μM YVAD (A and B) or with 25 μM zVAD or 100 μM zVAD (C and D) prior to infection with the wild-type strain of Shigella. One group was treated only with 100 μM YVAD (A). The cells were stained with the fluorescent dyes Syto 9 and PI and analyzed as described in the legend to Fig. 1. The bars indicate averages and the error bars indicate standard errors of the means for three independent experiments.
Caspase inhibitors do not prevent a Shigella-induced change in HMDM membrane permeability.
The disparity in previous reports related to the type of cell death triggered by Shigella in monocytes and HMDM could be partially accounted for by multiple experimental variables. These variables include the use of different pharmacological inhibitors of caspases, such as YVAD, an inhibitor of caspase-1, and zVAD, a broad-spectrum inhibitor of caspases, the concentration of the inhibitors used, the origin of the cells studied (J774 versus human cells), and the age of the cultures (monocytes versus monocyte-derived macrophages). To evaluate these variables in more detail, infection of both monocytes and HMDM by Shigella was examined simultaneously in the presence and in the absence of different concentrations of YVAD and zVAD (Fig. 2). Treatment of monocytes with 100 μM YVAD prior to infection resulted in a 50% decrease in the number of PI-positive cells compared to the number of PI-positive cells observed after infection in the absence of the inhibitor (Fig. 2A). In contrast, treatment of HMDM with YVAD or zVAD prior to infection had no effect on cell viability at any of the three times examined (Fig. 2B and D). Unexpectedly, treatment of monocytes with zVAD increased their sensitivity to wild-type Shigella (Fig. 2C). Within 2 h of infection, 48% of the monocytes treated with zVAD were PI positive, compared to 8% of the monocytes not treated with the inhibitor (Fig. 2C); zVAD alone had no effect on cell viability (data not shown). These results confirm and extend previous reports which indicated that Shigella kills HMDM by a caspase-independent mechanism and triggers apoptosis of human monocytes that is partially dependent on caspase-1. These data also indicate that caspases may protect human monocytes against cytotoxicity that could be induced by bacterial infections. This type of protection by caspases against cell death has been described previously in other systems (39, 40).
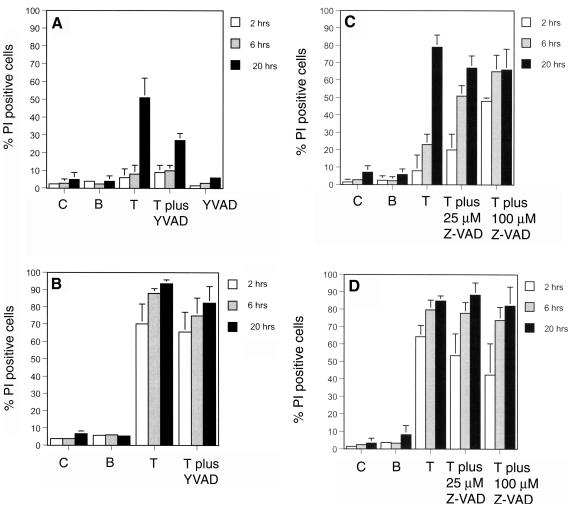
ROI are not the primary cause of the necrotic cell death induced by virulent Shigella.
Reactive oxygen intermediates (ROI) regulate multiple physiological processes, but when there is excess ROI, they can precipitate necrotic cell death due to the damage that they can cause by lipid peroxidation and modification of proteins and nucleic acids (8, 21). Reactive oxygen species can also cause mitochondrial damage, and ultimately cell death, by activating the mitochondrial megachannel, leading to mitochondrial depolarization, uncoupling of oxidative phosphorylation, and ATP depletion (20, 23).
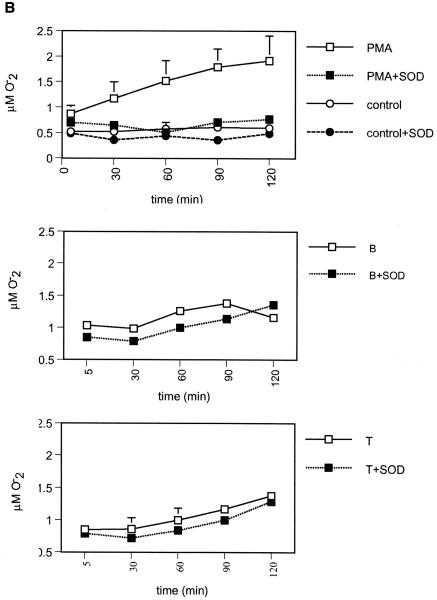
To determine whether cell death due to Shigella is linked to the production of ROI, the production of superoxide was monitored in cells infected with either the avirulent strain (BS103) or the wild-type Shigella strain (2457-T). Superoxide generation was measured as described in Materials and Methods by using the method of Pick and Mizel (32). Specificity in this assay is assumed if the reduction of ferricytochorome C is inhibited by superoxide dismutase (1). As a positive control for these studies, monocytes and HMDM were treated with the phorbol ester 12-myristate-13-acetate, and they were shown to produce large amounts of superoxide, which was inhibited by superoxide dismutase (Fig. 3A and B). However, the cell membrane permeability, as measured by uptake of PI, remained intact for at least 6 h posttreatment (Fig. 3C and 3D). In contrast, no increase in ROI was seen in monocytes (Fig. 3A) or HMDM (Fig. 3B) upon infection with either BS103 or 2457-T, even though PI-positive cells were seen in HMDM preparations within 2 h after infection with 2457-T (Fig. 3D).
FIG. 3.
Shigella does not trigger the release of significant amounts of superoxide by infected cells. (A and B) Monocytes (A) and monocyte-derived macrophages (B) were not treated (control), were treated with 10 μM phorbol 12-myristate 13-acetate (PMA), or were infected with the avirulent strain (B) or the wild-type strain (T) of Shigella. At 30 min after infection the culture medium was replaced with a solution containing 200 μM cytochrome c with or without 50 μg of superoxide dismutase (SOD) per ml. Changes in absorbance at 550 nm were monitored at 30-min intervals for 2 h. The data are the averages and standard errors of the means for three experiments. (C and D) Monocytes (C) and monocyte-derived macrophages (D) were not treated (control [C]), were infected with the avirulent strain (B) or the wild-type strain (T) of Shigella, or were treated with 10 μM phorbol 12-myristate 13-acetate. The cells were stained with Syto 9 and PI at 2, 6, and 20 h after infection or after treatment with phorbol 12-myristate 13-acetate and analyzed by fluorescence microscopy. The data are expressed as percentages of PI-positive cells per field. The bars indicate averages and the error bars indicate standard errors of the means for four independent experiments.
To further examine the role of ROI in Shigella-infected cells, monocytes and HMDM were pretreated with the antioxidant N-acetyl-l-cysteine (5 mM) (36), diphenyleniodonium (10 μM), which inhibits the NADPH complex both in phagolysosomes and in the mitochondrion (24), cyclosporin A, an inhibitor of the mitochondrial megachannel (20), or butylated hydroxyanisole (100 μM), an oxygen radical scavenger that protected L929 cells from the necrotic cell death induced by tumor necrosis factor (39). None of these pharmacological agents altered the necrotic outcome seen in HMDM infected with virulent Shigella (data not shown). Based on all the data, we concluded that the ROI produced by infected host cells were not the primary cause of the rapid cell death induced by virulent Shigella.
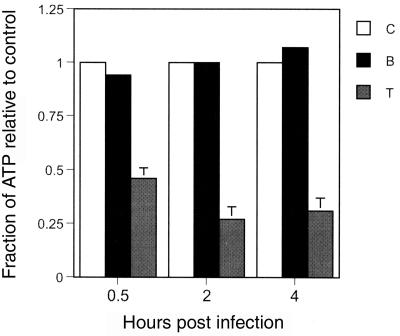
Wild-type Shigella causes depletion of cellular ATP in infected HMDM.
A distinction between necrosis and apoptosis is linked to the rate of depletion of ATP in cells. Necrosis is usually accompanied by a rapid loss of ATP (20). Infection of HMDM with virulent Shigella was accompanied by a >50% decrease in the intracellular ATP levels within 30 min after infection. In contrast, cells infected with the avirulent strain maintained a stable ATP level indistinguishable from that of the control group (Fig. 4).
FIG. 4.
Wild-type Shigella affects the intracellular ATP level in infected monocyte-derived macrophages. Monocyte-derived macrophages were not infected (control [C]) or were infected with the avirulent strain (B) or the wild-type strain (T) of Shigella. At 0.5, 2, and 4 h after infection, they were lysed by using the reagents supplied with the ApoGlow ATP detection kit (Cambrex), and the level of ATP was determined by using the protocol provided by the manufacturer. The bars indicate averages and the error bars indicate standard errors of the means for eight experiments for all groups.
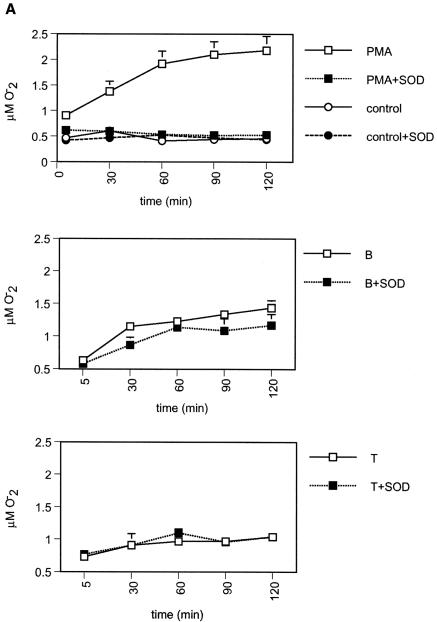
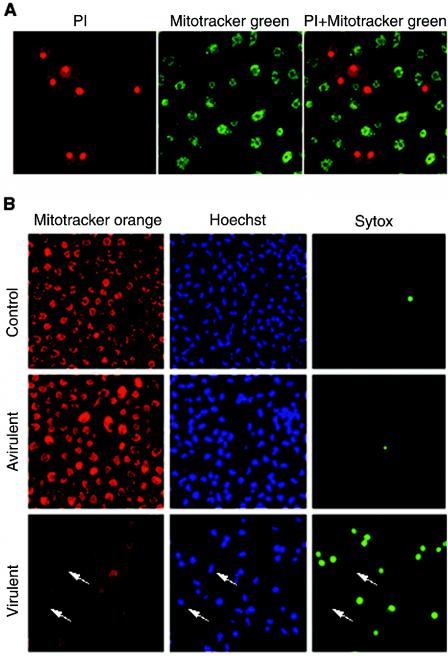
Wild-type Shigella affects the mitochondrial membrane potential of cultured macrophages.
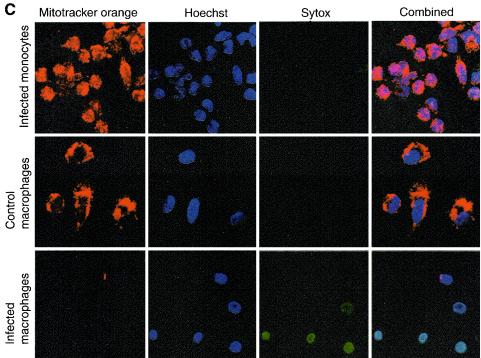
Since mitochondria are the energy-producing organelles inside cells, the rapid loss of ATP from HMDM infected with virulent Shigella suggested that mitochondrial functions were most likely affected. To determine whether infection of HMDM with Shigella affected mitochondrial membrane potential, infected cells were stained by using a combination of PI and the mitochondrial membrane potential-sensitive dye Mitotracker Green (Fig. 5A). Cells that were labeled with PI did not exhibit any Mitotracker Green staining, indicating that in infected HMDM loss of cell membrane permeability was accompanied by a loss of mitochondrial potential; none of the cells observed was stained with both dyes. In subsequent experiments uninfected cells (control) and infected monocyte and HMDM cultures were simultaneously stained with three dyes, Hoechst 33342 (a blue-fluorescing DNA binding dye), Mitotracker Orange (a red-fluorescing mitochondrial membrane potential-sensitive dye), and Sytox (a green-fluorescing vital dye). In preliminary studies we found that Sytox and PI can be used interchangeably (data not shown). In uninfected HMDM and in cells infected with the avirulent strain, brightly stained mitochondria were evident 2 h postinfection (Fig. 5B and C). These cells excluded the green-fluorescing vital dye, indicating that they were alive. A similar pattern of staining was observed with human monocytes infected with virulent Shigella and stained 2 h postinfection (Fig. 5C). In marked contrast, HMDM infected with virulent Shigella for the same period of time showed three staining patterns (Fig. 5C). One group of cells, which we believe represented the live cells, was stained with Mitotracker Orange but not with Sytox. The second group of cells, representing the dead cells, was stained brightly with Sytox but not with Mitotracker Orange. The third group of cells, identified based on staining of the nuclei with Hoechst 33342, was not stained with either Mitotracker Orange or Syto 9 (Fig. 5C). None of the cells exhibited Mitrotracker Orange and Sytox staining simultaneously. At later times following infection, all the cells were Sytox positive (data not shown). These data demonstrate that wild-type Shigella triggers a marked reduction in the mitochondrial membrane potential in HMDM. These data also suggest that disruption of the host cell mitochondria preceded the change in the cell membrane permeability, as monitored by uptake of the vital dyes PI and Sytox.
FIG. 5.
Mitochondrial membrane potential is altered in monocyte-derived macrophages infected with wild-type Shigella. (A) Monocyte-derived macrophages infected with the wild-type strain of Shigella. The cells were stained 1 h after infection with a combination of PI and Mitotracker Green, a green-fluorescing mitochondrial membrane potential-sensitive dye. (B) Monocyte-derived macrophages that were not treated (control) or were infected with the avirulent strain or the virulent strain of Shigella. The cells were stained 2 h after infection with Mitotracker Red, a red-fluorescing mitochondrial membrane potential-sensitive dye, Hoechst 33342, a blue-fluorescing DNA binding dye, and Sytox, a green-fluorescing vital dye. The arrows indicate cells that were stained only with Hoechst 33342. (C) Monocytes infected with the wild-type strain of Shigella, control monocyte-derived macrophages that were not infected, and monocyte-derived macrophages infected the wild-type strain of Shigella. The cells were stained 2 h after infection with Mitotracker Orange, Hoechst 123, and Sytox. Individual and triple (combined) fluorescent confocal images are shown.
DISCUSSION
Virulent Shigella kills cultured monocytes and macrophages by a mechanism(s) that is associated with an increase in cell membrane permeability. In this study, a side-by-side analysis carried out with HMDM and monocytes revealed that the change in cell membrane permeability triggered by virulent Shigella takes place in these two cell types on different time scales. Within 2 h after infection, the cell membrane of 59% ± 6% of HMDM was permeable, compared to less than 4% of the monocytes. By 20 h, however, the numbers of PI-positive cells were similar for the two cell populations. We also found that an inhibitor of caspase-1, YVAD, partially inhibited the change in the cell membrane permeability in infected monocytes but not in HMDM. zVAD had no effect on either cell population. These findings are consistent with previous reports which showed that virulent Shigella kills HMDM, but not fresh monocytes, by a mechanism that is more similar to oncosis or necrosis than to apoptosis and that this occurs in the absence of DNA fragmentation or nucleus condensation (6, 7). Significantly, our data demonstrate that the change in cell membrane permeability of HMDM infected with virulent Shigella was preceded by an abrupt decrease in the ATP level and a collapse of the mitochondrial membrane potential, while infected monocytes maintained an intact cell membrane and functional mitochondria.
Mitochondria are the energy-producing organelles within cells and, as such, are central to whether a cell lives or dies and how death occurs. An acute and profound disruption of cellular metabolism occurs by the opening of pores in the inner membrane of the mitochondrial membrane. Opening of the pores enables nonselective diffusion of molecules across the mitochondrial inner membrane, leading to mitochondrial depolarization, uncoupling of oxidative phosphorylation, and swelling, which in turn lead to rapid ATP depletion and cell death (20). Mitochondria also play a key role in the apoptotic process by releasing proapototic proteins, such as cytochrome c, that are normally located in the mitochondrial intermembrane space. The release of these proteins is promoted by the formation of specific release channels in the outer membrane of the mitochondria by proapoptotic Bcl-2 family members (41). Once released, cytochrome c triggers activation of caspases, which in turn regulate the apoptotic process (33). The orderly process of apoptosis is energy dependent, and consequently, damage of the mitochondria to the point that they can no longer produce ATP can easily shift cell death from apoptosis to necrosis (20). In view of the finding that a variable such as ATP can determine whether cells die by apoptosis or necrosis, Kim et al. (20) proposed that these two types of cell death are not distinct and independent but rather represent extremes on a continuum.
To address the possibility that the rapid death of HMDM was due to an overload of reactive oxygen species produced by the infected cells, the production of ROI was monitored, and we found no evidence for differential production of ROI by cells infected with either virulent or avirulent bacteria. In addition, we examined the effect of a wide range of other agents that have been shown to prevent ROI-mediated necrosis (36, 24, 20, 39). These agents included antioxidants (36, 39), an inhibitor of the NADPH oxidase enzyme system (24), cyclosporin A (23), and glycine, which has been shown to prevent the necrotic cell death triggered by Salmonella (3). None of the chemicals tested prevented the Shigella-induced increase in membrane permeability. Cell death was completely inhibited, however, by pretreatment of the cells with cytochalasin D (100 μM for 30 min) (data not shown), an inhibitor of phagocytosis. Similar results were reported by other investigators (30, 42). It is noteworthy that cytochalasin D did not prevent cell death in HMDM induced by Salmonella (4).
All pathogenic strains of Shigella carry a large ∼213-kb plasmid termed the virulence plasmid or the invasion plasmid (38). A 31-kb region within the virulence plasmid, referred to as the spa-mxi-ipa locus, encodes a group of ∼32 genes that are essential for the invasion of nonphagocytes by Shigella and for the escape of effector proteins from phagolysosomes (34, 37). The protein secretion and delivery system known as the type III secretion system, which is encoded by spa and mxi genes, is shared by several gram-negative pathogenic bacteria, including Escherichia coli and Salmonella, and was most likely acquired by horizontal gene transfer among several bacterial strains (10, 31). Shigella invasion plasmid antigens B, C, and D (designated IpaB, IpaC, and IpaD, respectively) orchestrate the escape of bacterial effector proteins from phagosomal vacuoles (15, 27). An interaction between IpaB and caspase-1, a proapoptotic and proinflammatory cysteine protease that cleaves interleukin-1β and interleukin-18 to their biologically active forms, first seen in J744 cells, was viewed as a key to the mechanism by which Shigella kills host cells (11, 16, 17). However, recent studies have shown that an IpaB deletion mutant lacking residues 307 to 316 (IpaBΔ307-316) failed to affect the cell membrane permeability despite the fact that the binding of this mutant to caspase-1 was intact (11). These findings raised the possibility that an activity other than the binding to caspase-1 was essential for the cytotoxic effector function of IpaB. Furthermore, proteins other than IpaB may play a critical role in Shigella-induced macrophage cell death.
IpaB is a homologue of the Salmonella protein SipB (41% identity) (19). Like IpaB, SipB also binds to and activates caspase-1 (14). J744 cells infected with Salmonella undergo rapid cell death with necrosis-like features referred to as programmed necrosis (3). Salmonella strains carrying a loss-of-function mutation in SipB failed to induce cell death (4). Hernandez et al. have recently demonstrated that SipB is localized to the mitochondria and that, when expressed in cultured cells, induces the formation of structures resembling autophagosomes derived from both mitochondria and endoplasmic reticulum membranes (13). SipB also triggered rapid killing of bone marrow-derived macrophages derived from either wild-type mice or, importantly, caspase-1-deficient mice (caspase-1−/−), indicating that cell death can be induced without caspase-1 (13). These findings also raise the possibility that like SipB, Shigella proteins involved in cell death may also target the host cell mitochondria for destruction. Studies are under way to address this possibility.
Acknowledgments
This work was supported by grant R03-AI 53202 from the National Institutes of Health.
We thank Noriko Kane-Goldsmith from the Neuroscience Imaging Facility, W. M. Keck Center for Collaborative Neuroscience, Rutgers University, for her assistance with the imaging aspects of this work.
Editor: V. J. DiRita
REFERENCES
- 1.Arthure, M. J. P., P. Kowalski-Saunders, S. Gurney, R. Tolcher, F. G. Bull, and R. Wright. 1987. Reduction of ferricytochrome C may underestimate superoxide production by monocytes. J. Immunol. Methods 98:63-69. [DOI] [PubMed] [Google Scholar]
- 2.Boya, P., B. Roques, and G. Kroemer. 2001. New EMBO members' review: viral and bacterial proteins regulating apoptosis at the mitochondrial level. EMBO J. 20:4325-4331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brennan, M. A., and B. T. Cookson. 2000. Salmonella induces macrophage death by caspase-1-dependent necrosis. Mol. Microbiol. 38:31-40. [DOI] [PubMed] [Google Scholar]
- 4.Chen, L. M., K. Kaniga, and J. E. Galan. 1996. Salmonella spp. are cytotoxic for cultured macrophages. Mol. Microbiol. 21:1101-1115. [DOI] [PubMed] [Google Scholar]
- 5.Clerc, P. L., A. Ryter, J. Mounier, and P. J. Sansonetti. 1987. Plasmid-mediated early killing of eucaryotic cells by Shigella flexneri as studied by infection of J774 macrophages. Infect. Immun. 55:521-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fernandez-Prada, C. M., D. L. Hoover, B. D. Tall, A. B. Hartman, J. Kopelowitz, and M. M. Venkatesan. 2000. Shigella flexneri IpaH(7.8) facilitates escape of virulent bacteria from the endocytic vacuoles of mouse and human macrophages. Infect. Immun. 68:3608-3619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernandez-Prada, C. M., D. L. Hoover, B. D. Tall, and M. M. Venkatesan. 1997. Human monocyte-derived macrophages infected with virulent Shigella flexneri in vitro undergo a rapid cytolytic event similar to oncosis but not apoptosis. Infect. Immun. 65:1486-1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fleury, C., B. Mignotte, and J. L. Vayssiere. 2002. Mitochondrial reactive oxygen species in cell death signaling. Biochimie 84:131-141. [DOI] [PubMed] [Google Scholar]
- 9.Francois, M., V. Le Cabec, M. A. Dupont, P. J. Sansonetti, and I. Maridonneau-Parini. 2000. Induction of necrosis in human neutrophils by Shigella flexneri requires type III secretion, IpaB and IpaC invasins, and actin polymerization. Infect. Immun. 68:1289-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galan, J. E., and A. Collmer. 1999. Type III secretion machines: bacterial devices for protein delivery into host cells. Science 284:1322-1328. [DOI] [PubMed] [Google Scholar]
- 11.Guichon, A., D. Hersh, M. R. Smith, and A. Zychlinsky. 2001. Structure-function analysis of the Shigella virulence factor IpaB. J. Bacteriol. 183:1269-1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hathaway, L. J., G. E. Griffin, P. J. Sansonetti, and J. D. Edgeworth. 2002. Human monocytes kill Shigella flexneri but then die by apoptosis associated with suppression of proinflammatory cytokine production. Infect. Immun. 70:3833-3842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hernandez, L. D., M. Pypaert, R. A. Flavell, and J. E. Galan. 2003. A Salmonella protein causes macrophage cell death by inducing autophagy. J. Cell Biol. 163:1123-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hersh, D., D. M. Monack, M. R. Smith, N. Ghori, S. Falkow, and A. Zychlinsky. 1999. The Salmonella invasin SipB induces macrophage apoptosis by binding to caspase-1. Proc. Natl. Acad. Sci. USA 96:2396-2401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.High, N., J. Mounier, M. C. Prevost, and P. J. Sansonetti. 1992. IpaB of Shigella flexneri causes entry into epithelial cells and escape from the phagocytic vacuole. EMBO J. 11:1991-1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hilbi, H., Y. Chen, K. Thirumalai, and A. Zychlinsky. 1997. The interleukin 1beta-converting enzyme, caspase 1, is activated during Shigella flexneri-induced apoptosis in human monocyte-derived macrophages. Infect. Immun. 65:5165-5170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hilbi, H., J. E. Moss, D. Hersh, Y. Chen, J. Arondel, S. Banerjee, R. A. Flavell, J. Yuan, P. J. Sansonetti, and A. Zychlinsky. 1998. Shigella-induced apoptosis is dependent on caspase-1 which binds to IpaB. J. Biol. Chem. 273:32895-32900. [DOI] [PubMed] [Google Scholar]
- 18.Jensen, V. B., J. T. Harty, and B. D. Jones. 1998. Interactions of the invasive pathogens Salmonella typhimurium, Listeria monocytogenes, and Shigella flexneri with M cells and murine Peyer's patches. Infect. Immun. 66:3758-3766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaniga, K., S. Tucker, D. Trollinger, and J. E. Galan. 1995. Homologs of the Shigella IpaB and IpaC invasins are required for Salmonella typhimurium entry into cultured epithelial cells. J. Bacteriol. 177:3965-3971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim, J. S., L. He, and J. J. Lemasters. 2003. Mitochondrial permeability transition: a common pathway to necrosis and apoptosis. Biochem. Biophys. Res. Commun. 304:463-470. [DOI] [PubMed] [Google Scholar]
- 21.Klebanoff, S. J. 1992. Oxygen metabolites from phagocytes, p. 541-588. In J. I. Gallin, I. M. Goldstein, and R. Snyderman (ed.), Inflammation: basic principles and clinical correlates, 2nd ed. Raven Press, New York, N.Y.
- 22.Kotloff, K. L., J. P. Winickoff, B. Ivanoff, J. D. Clemens, D. L. Swerdlow, P. J. Sansonetti, G. K. Adak, and M. M. Levine. 1999. Global burden of Shigella infections: implications for vaccine development and implementation of control strategies. Bull. W. H. O. 77:651-666. [PMC free article] [PubMed] [Google Scholar]
- 23.Lemasters, J. J., A.-L. Nieminen, T. Qian, L. C. Trost, and B. Herman. 1997. The mitochondrial permeability transition in toxic, hypoxic and reperfusion injury. Mol. Cell. Biochem. 174:159-165. [PubMed] [Google Scholar]
- 24.Li, Y., and M. A. Trush. 1998. Diphenyleneiodonium, an NAD(P)H oxidase inhibitor, also potently inhibits mitochondrial reactive oxygen species production. Biochem. Biophys. Res. Commun. 253:295-299. [DOI] [PubMed] [Google Scholar]
- 25.Mandell. 2000. Principles and practice of infectious diseases. Churchill Livingstone Inc., London, United Kingdom.
- 26.Mathan, M. M., and V. I. Mathan. 1986. Ultrastructural pathology of the rectal mucosa in Shigella dysentery. Am. J. Pathol. 123:25-38. [PMC free article] [PubMed] [Google Scholar]
- 27.Menard, R., M. C. Prevost, P. Gounon, P. Sansonetti, and C. Dehio. 1996. The secreted Ipa complex of Shigella flexneri promotes entry into mammalian cells. Proc. Natl. Acad. Sci. USA 93:1254-1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Monack, D. M., B. Raupach, A. E. Hromockyj, and S. Falkow. 1996. Salmonella typhimurium invasion induces apoptosis in infected macrophages. Proc. Natl. Acad. Sci. USA 93:9833-9838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nadzam, G. S., C. De La Cruz, R. S. Greco, and B. Haimovich. 2000. Neutrophil adhesion to vascular prosthetic surfaces triggers nonapoptotic cell death. Ann. Surg. 231:587-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nonaka, T., T. Kuwabara, H. Mimuro, A. Kuwae, and S. Imajoh-Ohmi. 2003. Shigella-induced necrosis and apoptosis of U937 cells and J774 macrophages. Microbiology 149:2513-2527. [DOI] [PubMed] [Google Scholar]
- 31.Ochman, H., J. G. Lawrence, and E. A. Groisman. 2000. Lateral gene transfer and the nature of bacterial innovation. Nature 405:299-304. [DOI] [PubMed] [Google Scholar]
- 32.Pick, E., and D. Mizel. 1981. Rapid microassays for the measurement of superoxide and hydrogen peroxide production by macrophages in culture using an automatic enzyme immunoassay reader. J. Immunol. Methods 46:211-226. [DOI] [PubMed] [Google Scholar]
- 33.Ravagnan, L., T. Roumier, and G. Kroemer. 2002. Mitochondria, the killer organelles and their weapons. J. Cell. Physiol. 192:131-137. [DOI] [PubMed] [Google Scholar]
- 34.Schuch, R., R. C. Sandlin, and A. T. Maurelli. 1999. A system for identifying post-invasion functions of invasion genes: requirements for the Mxi-Spa type III secretion pathway of Shigella flexneri in intercellular dissemination. Mol. Microbiol. 34:675-689. [DOI] [PubMed] [Google Scholar]
- 35.Shiga, K. 1906. Observations on the epidemiology of dysentery in Japan. Philipp. J. Sci. 1:485. [Google Scholar]
- 36.Takei, H., A. Araki, H. Watanabe, A. Ichinose, and F. Sendo. 1996. Rapid killing of human neutrophils by the potent activator phorbol 12-myristate 13-acetate (PMA) accompanied by changes different from typical apoptosis or necrosis. J. Leukoc. Biol. 59:229-240. [DOI] [PubMed] [Google Scholar]
- 37.Tamano, K., S. Aizawa, E. Katayama, T. Nonaka, S. Imajoh-Ohmi, A. Kuwae, S. Nagai, and C. Sasakawa. 2000. Supramolecular structure of the Shigella type III secretion machinery: the needle part is changeable in length and essential for delivery of effectors. EMBO J. 19:3876-3887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Venkatesan, M. M., M. B. Goldberg, D. J. Rose, E. J. Grotbeck, V. Burland, and F. R. Blattner. 2001. Complete DNA sequence and analysis of the large virulence plasmid of Shigella flexneri. Infect. Immun. 69:3271-3285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vercammen, D., R. Beyaert, G. Denecker, V. Goossens, G. Van Loo, W. Declercq, J. Grooten, W. Fiers, and P. Vandenabeele. 1998. Inhibition of caspases increases the sensitivity of L929 cells to necrosis mediated by tumor necrosis factor. J. Exp. Med. 187:1477-1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vercammen, D., P. Vandenabeele, R. Beyaert, W. Declercq, and W. Fiers. 1997. Tumour necrosis factor-induced necrosis versus anti-Fas-induced apoptosis in L929 cells. Cytokine 9:801-808. [DOI] [PubMed] [Google Scholar]
- 41.Wei, M. C., W. X. Zong, E. H. Cheng, T. Lindsten, V. Panoutsakopoulou, A. J. Ross, K. A. Roth, G. R. MacGregor, C. B. Thompson, and S. J. Korsmeyer. 2001. Proapoptotic BAX and BAK: a requisite gateway to mitochondrial dysfunction and death. Science 292:727-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zychlinsky, A., M. C. Prevost, and P. J. Sansonetti. 1992. Shigella flexneri induces apoptosis in infected macrophages. Nature 358:167-169. [DOI] [PubMed] [Google Scholar]