Abstract
Using survey data from participants in a public housing relocation program in Atlanta, Georgia, we examine post-relocation changes in healthcare access (having a usual source of care, having an unmet need) and utilization (receiving a medical exam). Although participants moved to safer, less impoverished neighborhoods, some participants experienced improvements in access and utilization whereas others experienced declines. The supply of healthcare providers in the new neighborhood and having health insurance were associated with improvements in access for this population. Future relocation efforts may seek to assist individuals with choosing a new neighborhood that has accessible healthcare resources for low-income populations.
Keywords: Public housing relocation, neighborhood poverty, healthcare access, health insurance
Introduction
Individuals living in more impoverished areas have worse healthcare access (Kirby and Kaneda 2005) and health outcomes (Gaskin et al. 2013; Henry, Sherman, and McDonald 2014; Wight et al. 2010) than those in less impoverished areas. Poor health outcomes are particularly evident among residents of public housing complexes, which spatially concentrate poverty (Culhane-Pera, Ellmore, and Wessel 2007; Krieger and Higgins 2002). Public housing relocation programs allow residents of large public housing complexes to move to less impoverished neighborhoods, often through private market rental vouchers (U.S. Department of Housing and Urban Development 2014). A modest body of research has examined changes in health outcomes post-relocation, with mixed results (Cooper et al. 2013; Cooper et al. 2014; Fauth, Leventhal, and Brooks-Gunn 2004; Kling et al. 2006; Ludwig et al. 2011).
However, no study has examined changes in individual-level healthcare access or utilization post-relocation, which may be relevant to health outcome changes. Contextual- and individual-level enabling resources, in particular, may be associated with changes in healthcare access and utilization for program participants (Andersen 1995). On the one hand, access and utilization may increase if the new communities have more enabling healthcare resources (e.g., more physicians) or offer safer, more convenient routes (e.g., lower crime and/or better public transit) to accessing care (Jiang and Begun 2002; Kirby and Kaneda 2005). On the other hand, access could decline if participants move to neighborhoods with fewer healthcare resources for the poor (Cooper et al. 2012; May, Cunningham, and Hadley 2004). In either case, changes in access and utilization may depend on individual enabling resources, such as insurance coverage -- rates of which are known to be lower among public housing residents (Digenis-Bury et al. 2008).
As part of an ongoing, longitudinal public housing relocation study, this short report provides the first examination of how healthcare access and utilization change for participants in a public housing relocation program. We also examine the associations between key enabling factors and changes in access to and utilization of healthcare for participants.
Materials and Methods
Study Setting
Atlanta, Georgia has been particularly active in its public housing relocation efforts, which have been described in detail elsewhere (Cooper et al. 2012). In short, Atlanta relocated its public housing residents under the Section 18 amendment to the 1937 Housing Act, which shifted public housing residents into the private market using rental vouchers. These data come from a larger study that examined the effects of relocation on substance use, HIV risk, and other health outcomes among people who use drugs. Participants were recruited from seven public housing complexes targeted for demolition, and met the following criteria: lived in the complex for at least one year prior to the study screening; self-identified as non-Hispanic African-American; were at least 18 years of age; had been sexually active in the past year; and did not live with an individual already enrolled in the study. Nonprobability-based quota sampling methods were used to oversample individuals who misused or were dependent on alcohol or others drugs.
Data Collection
We analyzed survey data from the baseline interview (median date June 30, 2009) and follow up. Baseline data captured information about the time period just before relocations began in an individual’s complex. Follow-up data used for this study (median interview date May 16, 2011) were obtained nearly two years post-relocation. This study period was chosen so that participants would have had sufficient time to establish relationships with healthcare providers in their new community.
Census tract-level data were obtained from the 2012 American Community Survey (U.S. Census Bureau 2015) and the 2010 Health Resources and Services Administration (Health Resources and Services Administration 2014). Study protocols were approved by Emory University’s Institutional Review Board, and a federal certificate of confidentiality was obtained for participant protection.
Sample
Of the 172 individuals recruited into the study, 160 completed interviews at baseline and follow-up. After limiting the analytic samples to those with complete data on the study variables, sample sizes ranged from 134 to 139 across the three outcomes.
Measures
Dependent variables
We analyzed three dichotomous outcomes of healthcare access and utilization that were ascertained at each wave. Consistent with Institute of Medicine guidelines, we conceptualized healthcare access as the timely use of personal health services to achieve the best possible outcomes (Millman 1993). First, we created an indicator of whether an individual reported having a usual source of care (USOC) where he/she usually went to for medical care in the 6 months prior to the interview (other than the emergency room), a common measure of access because it provides an entry point into the healthcare system if timely services are needed (Agency for Healthcare Research and Quality 2014). Second, we created a dichotomous indicator for whether a respondent had wanted medical care in the six months prior to the interview, but was unable to receive it (i.e., unmet need). This measure assesses an individual’s perception of their inability to receive timely services (Agency for Healthcare Research and Quality 2014). Finally, we created an indicator for healthcare utilization that assesses whether a respondent had an examination by a physician in the past 12 months.
We also created three categorical variables to capture changes in each measure for individual participants across time. For example, we created a categorical measure of USOC for those who: (1) had a USOC at baseline and follow-up (i.e., access in both waves); (2) gained a USOC between baseline and follow-up (i.e., access improved); (3) lost USOC between baseline and follow-up (i.e., access declined); and (4) never had a USOC in either wave. We created similar measures for unmet need and having a physical in the past 12 months.
Enabling characteristics
We used Anderson’s Behavioral Model of Healthcare Utilization framework to identify enabling characteristics during the follow-up period at the neighborhood and individual levels that may be associated with access and utilization changes (Andersen 1995). At the neighborhood level, we examined the: (1) percentage of census tract residents living in poverty; and (2) number of physicians per 1,000 residents in the post-relocation census tract. A third neighborhood characteristic was derived from a survey question that asked participants about their perception of their neighborhood safety on a scale of 1 (“very unsafe”) to 5 (“very safe”). At the individual level, we examined whether an individual had health insurance at follow-up (versus being uninsured).
Analytic Approach
We compared healthcare access and use across the two time points using Stata’s equality of proportions test (StataCorp 2013). We subsequently described changes in the outcomes using the categorical measures to assess the proportion of participants for whom access improved or declined.
Finally, we examined the association between enabling characteristics and changes in access and utilization across waves. Bivariate associations were assessed using chi-squared tests and one-way analysis of variance tests. We also estimated multinomial logistic regression models, which included the enabling characteristics, individual-level predisposing characteristics (age and gender), need-related characteristics at baseline [a dichotomous indicator of fair or poor self-reported health status (versus good, very good, or excellent) and a scale of substance use behaviors (Knight, Simpson, and Morey 2002)], and the local road distance participants had moved. Standard errors were clustered at the pre-relocation census tract. We present marginal effects, which were estimated at the reference category of insurance status (i.e., uninsured) and the mean value of other covariates. The marginal effect indicates the percentage point difference in the likelihood that an individual falls into one of the outcome categories associated with a one unit increase in a given covariate. Continuous measures were standardized in each sample such that a one unit increase corresponds to a one standard deviation increase in the measure above its mean value.
In sensitivity analyses, we also included measures of physical health symptoms (Ware, Kosinski, and Keller 1994) and depressive symptoms at baseline (Radloff 1977), as well measures of the change in need-related measures between baseline and follow-up. Key findings from these supplemental analyses were qualitatively similar in direction and magnitude.
Results
Approximately 55% of the sample was female, and the mean age was 43.0 years (Appendix Table A). On average, participants moved to less impoverished tracts (p<0.001) that they perceived to be safer (p<0.001) (Table 1). However, the new tracts had fewer primary care physicians per capita compared to the prior tracts (p<0.05).
Table 1.
Healthcare access, healthcare utilization, and enabling characteristics among participants in a public housing relocation program, at baseline and follow-up§
| Baseline | Follow-up | p-value† | |
|---|---|---|---|
| Individual-Level Healthcare Access and Utilization | |||
| Has Usual Source of Care (n=137), % | 75.2 | 73.7 | 0.782 |
| Has Unmet Need (n=134), % | 28.4 | 20.9 | 0.156 |
| Had Medical Exam (n=139), % | 72.7 | 69.1 | 0.509 |
| Neighborhood-Level Enabling Characteristics | |||
| Percentage living in poverty in the census tract, mean (SD) | 41.0 (11.3) | 31.9 (12.8) | <0.001 |
| Number of primary care physicians per1,000 residents in the census tract, mean (SD) | 1.8 (3.2) | 0.9 (2.6) | 0.003 |
| Perceived neighborhood safety (1–5 Scale, 5 is Most Safe), mean (SD) | 3.9 (0.9) | 4.3 (0.7) | <0.001 |
| Individual-Level Enabling Characteristic | |||
| Has health insurance (versus uninsured), % | 65.6 | 74.1 | 0.132 |
Notes:
Median interview dates were June 30, 2009 at baseline and May 16, 2011 at follow-up.
Bivariate comparisons between the value of each measure at baseline and follow-up were conducted with equality of proportions tests and t-tests. Bivariate comparisons for neighborhood- and individual-level enabling characteristics use the largest sample (i.e., those who had complete data for the medical exam question; n=139).
Aggregate measures of individual-level healthcare access or health insurance status did not differ statistically across waves (Table 1). However, there were notable changes in all three measures for individual participants (Table 2). For example, 12.4% gained a USOC, while 13.9% lost a USOC between baseline and follow-up.
Table 2.
Changes in individual-level healthcare access and utilization among participants in a public housing relocation program
| Changes in Access/UseBetween Baseline & Follow-up | |||||
|---|---|---|---|---|---|
|
| |||||
| Has access/use both waves a | Improved | Declined | No access/use both waves | Total | |
| Has Usual Source of Care (n=137) | 61.3 | 12.4 | 13.9 | 12.4 | 100.0 |
| Has Unmet Need (n=134) | 59.7 | 19.4 | 11.9 | 9.0 | 100.0 |
| Had Medical Exam (n=139) | 56.8 | 12.2 | 15.8 | 15.1 | 99.9† |
Note:
For the measure of unmet need, this category includes those that reported no unmet need at baseline and follow-up.
Total number does not equal 100.0 due to rounding of the estimate to a single decimal place.
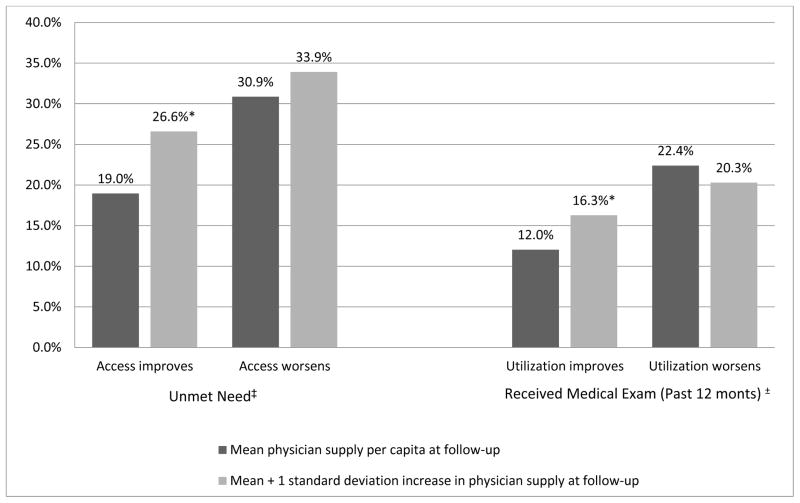
In bivariate comparisons, the association between primary care physicians per capita in the post-relocation census tract and two outcome measures (changes in unmet need and receipt of a physical exam) approached statistical significance (p<0.10). In multivariate comparisons, the supply of primary care physicians per capita in the post-relocation tract was significantly associated with improvements in both of these outcomes across waves (Panel B, p<0.05) (Figure 1).
Figure 1.
Adjusted percentage of adult participants in public housing relocation program that experienced changes in healthcare access and utilization between baseline and follow-up, by physician supply
Note: Results come from multinomial regression models adjusted for age, gender, baseline health status, insurance status at follow-up, neighborhood enabling characteristics at follow-up, and distance moved. Significance refers to the difference in the adjusted percentage of participants that experienced an improvement in access/utilization, by physician supply at follow-up.
*p<0.05. ‡ N=134, ± N=139 African American adult participants in public housing relocation program.
There was no association between census tract-level poverty rates and any of the outcome measures in the bivariate comparisons (Table 3, Panel A). Results from the multivariate models (Table 3, Panel B), however, indicate that residents who move to poorer areas were more likely to have improvements in unmet needs and less likely to have a decline in utilization (i.e., medical exam).
Table 3.
Associations between enabling characteristics and changes in healthcare access and utilization, among participants in a public housing relocation program
| PANEL A: BIVARIATE RESULTS
| |||||
|---|---|---|---|---|---|
| Changes in Access/Use | |||||
|
| |||||
| Has access/use both waves a | Improved | Declined | Pooraccess/use both waves | p-value | |
| Has Usual Source of Care (n=137) | |||||
|
| |||||
| Neighborhood-Level Enabling Characteristics | |||||
| Percentage living in poverty (mean) | 33.7 | 28.4 | 30.1 | 33.5 | 0.275 |
| Physicians per 1,000 Residents (mean) | 1.1 | 0.3 | 0.3 | 0.4 | 0.170 |
| Perceived neighborhood safety, 1–5 (mean) | 4.4 | 4.4 | 4.4 | 4.4 | 0.999 |
| Individual-Level Enabling Characteristic | |||||
| Has health insurance (%) | 72.6% | 82.4% | 42.1% | 41.2% | 0.006 |
|
| |||||
| Unmet Need (n=134) | |||||
|
| |||||
| Neighborhood-Level Enabling Characteristics | |||||
| Percentage living in poverty (mean) | 32.1 | 33.9 | 34.4 | 32.6 | 0.867 |
| Physicians per 1,000 Residents (mean) | 0.7 | 1.8 | 0.5 | 0.2 | 0.086 |
| Perceived neighborhood safety, 1–5 (mean) | 4.4 | 4.3 | 4.4 | 4.3 | 0.976 |
| Individual-Level Enabling Characteristic | |||||
| Has health insurance (%) | 77.5% | 69.2% | 25.0% | 58.3% | <0.001 |
|
| |||||
| Had Medical Exam (n=139) | |||||
|
| |||||
| Neighborhood-Level Enabling Characteristics | |||||
| Percentage living in poverty (mean) | 33.0 | 32.2 | 27.4 | 32.1 | 0.448 |
| Physicians per 1,000 Residents (mean) | 0.9 | 1.8 | 0.5 | 0.3 | 0.066 |
| Perceived neighborhood safety, 1–5 (mean) | 4.4 | 4.4 | 4.2 | 4.3 | 0.770 |
| Individual-Level Enabling Characteristic | |||||
| Has health insurance (%) | 82.3.% | 70.6% | 68.2% | 52.4%b | 0.065 |
|
| |||||
| PANEL B: MULTIVARIATE RESULTS, PRESENTED AS MARGINAL EFFECTS [M.E.]b | |||||
|
| |||||
| M.E. | M.E. | M.E. | M.E. | ||
|
| |||||
| Has Usual Source of Care [intercept] | 51.7 | 5.2 | 22.1 | 21.0 | |
|
| |||||
| Neighborhood-Level Enabling Characteristics | |||||
| Percentage living in povertyc | 7.2 | −4.8 | −2.7 | 0.2 | |
| Physicians per 1,000 residentsc | 14.5** | −11.8 | −2.1 | −0.6 | |
| Perceived neighborhood safety, 1–5 | 0.9 | −1.5 | −0.9 | 1.5 | |
| Individual-Level Enabling Characteristic | |||||
| Has health insurance | 10.5*** | 13.2*** | −11.9 | −11.8* | |
|
| |||||
| Unmet Need [intercept] | 40.0 | 19.0 | 30.9 | 10.1 | |
|
| |||||
| Neighborhood-Level Enabling Characteristics | |||||
| Percentage living in povertyc | −2.4 | 4.4* | −0.9 | −1.2 | |
| Physicians per 1,000 residentsc | −4.6 | 7.6* | 3.1 | −6.1 | |
| Perceived neighborhood safety, 1–5 | −0.9 | −4.3 | 6.0 | −0.9 | |
| Individual-Level Enabling Characteristic | |||||
| Has health insurance (%) | 25.7** | −1.5 | −21.5*** | −2.7 | |
|
| |||||
| Had Medical Exam [intercept] | 35.6 | 12.0 | 22.4 | 30.0 | |
|
| |||||
| Neighborhood-Level Enabling Characteristics | |||||
| Percentage living in povertyc | 5.3 | 2.3 | −6.4*** | −1.2 | |
| Physicians per 1,000 residentsc | 8.5 | 4.2* | −2.1 | −10.7 | |
| Perceived neighborhood safety, 1–5 | −4.9 | −1.2 | 4.9 | 1.2 | |
| Individual-Level Enabling Characteristic | |||||
| Has health insurance (%) | 27.1* | −0.5 | −9.4 | −17.2*** | |
Notes: Bivariate analyses were conducted with one-way ANOVA analyses and chi-squared tests. Multivariate analyses were conducted with multinomial logistic regression models that also control for age, gender, self-rated health, substance use behaviors, and the distance participants moved.
For the measure of unmet need, this category includes those that reported no unmet need at baseline and follow-up.
The marginal effect indicates the adjusted percentage point difference in the likelihood that an individual falls into a specific outcome category associated with a one unit increase in a given covariate. Marginal effects were estimated using the reference category of insurance status (i.e., uninsured) and the mean value of other covariates.
Measures were standardized in the multivariate model such that the marginal effect corresponds to a one standard deviation increase in the measure above its mean value.
p<0.05,
p<0.01,
p<0.001.
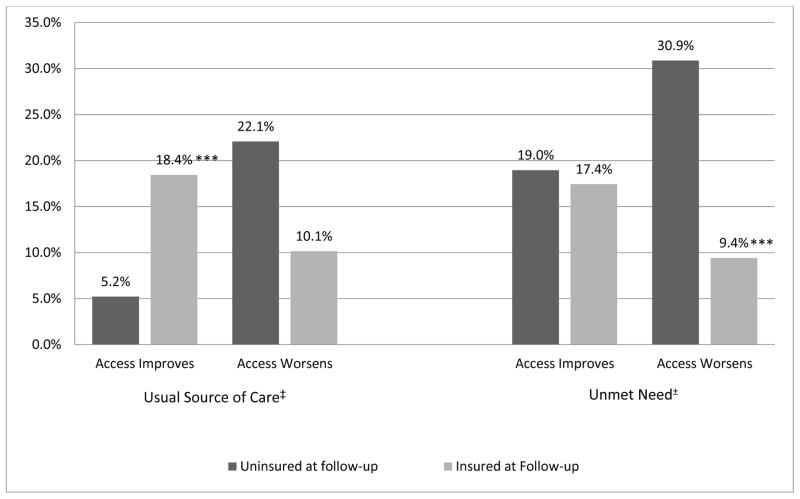
Individual-level health insurance (versus being uninsured) at follow-up was strongly associated with changes in having a USOC and having an unmet need for healthcare in the bivariate (p<0.01) and multivariate analyses (p<0.05) (Table 3, Figure 2). The marginal effect indicates that the model adjusted percentage of those who gained a USOC was 13.2 percentage points greater (p<0.001) for those with health insurance (18.4%) compared to those without health insurance (5.2%) at follow-up. In addition, the model adjusted percentage of those who experienced a decline in access assessed by unmet need was 21.5 percentage points lower (p<0.001) among those with health insurance (9.4%) compared to those without health insurance (30.9%).
Figure 2.
Adjusted percentage of adult participants in public housing relocation program that experienced changes in healthcare access between baseline and follow-up, by individual health insurance status
Notes: Results come from multinomial regression models adjusted for age, gender, baseline health status, insurance status at follow-up, neighborhood enabling characteristics at follow-up, and distance moved. Significance refers to the difference in the adjusted percentage of participants that experienced an improvement or decline in access, by insurance status at follow-up. ***p<0.001. ‡ N=137, ± N=134 African American adult participants in public housing relocation program. For the measure of unmet need, participants who reported an unmet need at baseline, but none at follow-up, were classified as having an improvement in access.
Conclusions
On average, participants in this public housing program moved to safer, less impoverished neighborhoods. Although some participants experienced improvements in access and utilization after relocating, others participants experienced declines in these outcomes. Our results identified several enabling factors that were associated with these changes in access and utilization post-relocation.
Understanding the factors that improve individual-level access for some relocators may inform programs and policies to yield better outcomes for future relocation programs. Results indicated that, on average, participants in this relocation program moved to neighborhoods with a lower supply of physicians, which is consistent with prior research reporting that spatial access to safety-net resources declines post-relocation (Cooper et al. 2012). However, those who did move to a neighborhood with a more primary care physicians were more likely to experience improvements in access (i.e., no unmet need) and utilization (i.e., receiving a medical exam). Given the health risks experienced by this population, future relocation efforts may seek to assist individuals with choosing a new neighborhood that has accessible healthcare resources for low-income populations.
At first glance, the positive association between neighborhood poverty at follow-up and improvements in access (i.e, having no unmet need) may seem counterintuitive. However, this finding comes from a multivariate model that controlled for the supply primary care physicians and perceptions of neighborhood safety. One possible explanation for this residual association could be that some of those who moved to relatively poorer neighborhoods had greater access to a healthcare provider or clinic that offered services for low-income populations. As another possibility, those who moved to relatively poorer neighborhoods may have had greater access to non-medical social services that target these communities (Allard 2008), which could have facilitated healthcare system navigation.
Results also indicated that health insurance status was strongly associated with changes in access to care for program participants. Being uninsured at one or both time periods was a common occurrence in this sample, experienced by nearly half of participants (data not shown). The Patient Protection and Affordable Care Act provides an opportunity for states to expand their Medicaid program and provide insurance coverage for all adults with income below 133% of the federal poverty level (U.S. Centers for Medicare & Medicaid Services. 2014). State participation in the Medicaid expansion would help stabilize health insurance status for low-income adults. As of November 2015, 31 states (not including Georgia) and Washington D.C. have opted to participate in the expansion (Kaiser Family Foundation 2015).
Several study limitations are noted. First, the sample is small and was obtained via a convenience sampling process to recruit individuals with high-risk behaviors, which might limit the generalizability of our findings to other groups affected by housing relocation changes. Second, there was no control group of non-relocators available for comparison. A third limitation is that more detailed geospatial measures of healthcare resource availability for low-income populations, such as the distance to providers that offer reduced cost or free services, were not available. Lastly, additional pathways beyond those examined in this study may be associated with changes in healthcare access and utilization for relocators, such as changes in social support, health behaviors, health status, or relationships with healthcare providers. Future research may examine whether these other pathways have implications for how program participants interact with the healthcare system after relocation.
Notwithstanding limitations, this study offers an important foundation for future research by providing the first examination of changes in individual-level healthcare access and utilization for public housing relocators. Our findings highlight the importance of bolstering the public housing relocation initiatives with additional policies to reduce barriers to care and help facilitate connections to healthcare resources in new communities for program participants.
Supplementary Material
Highlights.
We examined changes in healthcare access and use for public housing relocators
Some relocators had improvements in outcomes whereas others had declines
Enabling resources were associated with improvements in healthcare access and use
Acknowledgments
This work was supported by the National Institute of Drug Abuse (R21DA027072; R01DA029513), and a CFAR03 grant awarded by the Emory Center for AIDS Research (P30 AI050409). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Agency for Healthcare Research and Quality. National Healthcare Quality Report, 2011. [accessed on December, 2014];Chapter 9: Access to Health Care. 2014 Available at: http://www.ahrq.gov/research/findings/nhqrdr/nhqr11/chap9.html.
- Allard SW. The Colors of Poverty: Why Racial and Ethnic Disparities Persist. Russell Sage Foundation; 2008. Retrieved from http://www.jstor.org/stable/10.7758/9781610447249. [Google Scholar]
- Andersen RM. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Cooper HL, Bonney LE, Ross Z, Karnes C, Hunter-Jones J, Kelley ME, Rothenberg R. The aftermath of public housing relocation: relationship to substance misuse. Drug Alcohol Depend. 2013;133(1):37–44. doi: 10.1016/j.drugalcdep.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Haley DF, Linton S, Hunter-Jones J, Martin M, Kelley ME, Karnes C, Ross Z, Adimora AA, Del Rio C, Rothenberg R, Wingood GM, Bonney LE. Impact of Public Housing Relocations: Are Changes in Neighborhood Conditions Related to STIs Among Relocaters? Sex Transm Dis. 2014;41(10):573–9. doi: 10.1097/OLQ.0000000000000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Wodarski S, Cummings J, Hunter-Jones J, Karnes C, Ross Z, Druss B, Bonney LE. Public housing relocations in Atlanta, Georgia, and declines in spatial access to safety net primary care. Health & place. 2012;18(6):1255–60. doi: 10.1016/j.healthplace.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culhane-Pera K, Ellmore D, Wessel LA. Primary care in public housing: voices of clinicians. J Health Care Poor Underserved. 2007;18(4):735–43. doi: 10.1353/hpu.2007.0105. [DOI] [PubMed] [Google Scholar]
- Digenis-Bury EC, Brooks DR, Chen L, Ostrem M, Horsburgh CR. Use of a Population-Based Survey to Describe the Health of Boston Public Housing Residents. Am J Public Health. 2008;98(1):85–91. doi: 10.2105/AJPH.2006.094912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fauth RC, Leventhal T, Brooks-Gunn J. Short-term effects of moving from public housing in poor to middle-class neighborhoods on low-income, minority adults’ outcomes. Soc Sci Med. 2004;59(11):2271–84. doi: 10.1016/j.socscimed.2004.03.020. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Thorpe RJ, McGinty EE, Bower K, Rohde C, Young JH, LaVeist TA, Dubay L. Disparities in Diabetes: The Nexus of Race, Poverty, and Place. Am J Public Health. 2013;104(11):2147–55. doi: 10.2105/AJPH.2013.301420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources and Services Administration. [accessed on 2014];Primary Care Service Area Data Download – 2010 (Census Tract Basis) 2014 Available at: http://datawarehouse.hrsa.gov/Data/datadownload/pcsa2010Download.aspx.
- Henry KA, Sherman RL, McDonald K. Associations of census-tract poverty with subsite-specific colorectal cancer incidence rates and stage of disease at diagnosis in the United States. J Cancer Epidemiol. 2014;2014:823484. doi: 10.1155/2014/823484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang HJ, Begun JW. Dynamics of change in local physician supply: an ecological perspective. Social science & medicine. 2002;54(10):1525–41. doi: 10.1016/s0277-9536(01)00132-0. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. Status of State Action on the Medicaid Expansion Decision. 2015. [Google Scholar]
- Kirby JB, Kaneda T. Neighborhood Socioeconomic Disadvantage and Access to Health Care. Journal of Health and Social Behavior. 2005;46(1):15–31. doi: 10.1177/002214650504600103. [DOI] [PubMed] [Google Scholar]
- Kling JR, Liebman JB, Katz LF, Sanbonmatsu L. Moving to opportunity and tranquility: Neighborhood effects on adult economic self-sufficiency and health from a randomized housing voucher experiment. National Bureau of Economic Research; 2006. [Google Scholar]
- Knight K, Simpson DD, Morey JT. An evaluation of the TCU Drug Screen. Washington, DC: National Institute of Justice, Office of Justice Programs, US Department of Justice; 2002. [Google Scholar]
- Krieger J, Higgins DL. Housing and Health: Time Again for Public Health Action. Am J Public Health. 2002;92(5):758–68. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, Kessler RC, Kling JR, Lindau ST, Whitaker RC, McDade TW. Neighborhoods, Obesity, and Diabetes — A Randomized Social Experiment. New England Journal of Medicine. 2011;365(16):1509–19. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May JH, Cunningham PJ, Hadley J. Most uninsured people unaware of health care safety net providers. [accessed on 2004];2004 Available at: http://www.hschange.com/CONTENT/718/ [PubMed]
- Millman M. Access to health care in America. Committee on Monitoring Access to Personal Health Care Services, Institute of Medicine; Washington, DC: National Academy Press; 1993. [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- U.S. Census Bureau. [accessed on 2015];2012 American Community Survey. 2015 Available at: http://factfinder2.census.gov.
- U.S. Centers for Medicare & Medicaid Services. [accessed on 2014];Medicaid expansion & what it means for you. 2014 Available at: https://www.healthcare.gov/medicaid-chip/medicaid-expansion-and-you.
- U.S. Department of Housing and Urban Development. [accessed on 2014];Moving to Opportunity for Fair Housing. 2014 Available at: http://portal.hud.gov/hudportal/HUD?src=/programdescription/mto.
- Ware J, Kosinski M, Keller S. Physical and mental health summary scales—a user’s manual. Boston, MA: New England Medical Center; 1994. [Google Scholar]
- Wight RG, Cummings JR, Karlamangla AS, Aneshensel CS. Urban neighborhood context and mortality in late life. J Aging Health. 2010;22(2):197–218. doi: 10.1177/0898264309355980. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.