Abstract
Purpose of review
Rest-activity rhythm (RAR) measurements may aid in the detection of depression risk and serve as an important target for depression prevention. This review evaluates the strength of current evidence supporting these potential applications.
Recent findings
Depression is associated with lower activity levels, that is less regularly patterned, and potentially shifted earlier or later in the day. Specific RAR patterns (combinations of several RAR characteristics) in patients with clinical depression may be unique or partially shared across disorders. Longitudinal research is limited but provides initial evidence that multiple distinct RAR patterns are associated with the risk of developing depression symptoms.
Summary
RARs measures provide a comprehensive and objective assessment of depression’s behavioral manifestations, and therefore may be useful as monitoring tool, providing additional information to help clinicians tailor behavioral treatments to specific patients. RARs also appear to contribute to depression risk and may be an important target for depression prevention. But research has not established valid predictive metrics using RARs to diagnose depression or detect depression risk. Future research should prioritize establishing the specific RAR patterns related to depression risk in high risk groups, and should seek to place this risk within the known psychosocial and neurobiological risk architecture of depression.
Keywords: rest-activity rhythms, depression, mood
Activity monitoring devices have recently grown in popularity and ease of use. When worn continuously over 24-hour periods, these devices capture the daily pattern of activity and rest, which is known as the rest-activity rhythm (RAR). The many characteristics and measures of the RAR (described below) provide psychiatry with an objective means for quantifying, both within and across 24-hour periods, the behavioral signatures of mental illness. Recent research suggests it is possible for the clinical utility of objective RAR measures to greatly expand.
Recent literature focused on the relationship between RARs and depression suggests several clinical applications of RAR measurements may be possible, including: (A) RARs could aid in the diagnosis or early detection of depression and (B) certain RARs characteristics or patterns could contribute to the risk of depression and therefore represent a behavioral target for depression prevention.
But to what extent does current evidence support translating these potential uses of RARs into actual clinical practice? This question is addressed by reviewing recent literature, after discussing what RARs are, and how they are measured.
Conceptually Defining RARs
RARs have many characteristics, and conceptually, the most commonly used metrics describe both the RAR’s individual constituents, i.e., characteristics of the active and rest periods, as well as how these periods are patterned and timed. Thus, the concepts measured by some aspects of the RAR overlap with more widely used objective measures of physical activity and sleep, such as the number of sedentary minutes per day or the number of minutes awake at night. But other aspects of RARs characterize unique phenomena that can only be assessed over 24-hour periods, including how stable activity is patterned across days or how long the active period lasts relative to the resting period.
Measuring RARs
Operational definitions of different aspects of the RAR vary by methodological approaches. The most common techniques for measuring RARs are cosine-type modeling and non-parametric approaches. Over the past two decades, both approaches have been developed to accommodate for the fact that, unlike other core daily rhythms, human RARs generally do not follow a simple cosine curve.
Many prominent researchers have favored a non-parametric approach for quantifying RARs. In 1996 van Someren (1) implemented these approaches, which do not make any assumptions about the RAR’s shape. Instead of statistically modeling the observed data, this non-parametric approach calculates metrics based on the level and variability found in activity time-series recordings. Resulting measures include: (A) intradaily variability, defined as the ratio of the hour-to-hour activity variability to the overall activity variability (higher values reflect fragmented RARs with more/larger transitions between activity levels), and (B) interdaily stability, defined as the ratio of variability within the mean 24-hour activity profile to the overall activity variability (higher values indicate the typical 24-hour profile accounts for a greater degree of the overall variability in the time series recording, reflecting greater stability of the mean 24-hour profile across days). Non-parametric methods also provide other measures of both active and resting periods, such as the average activity level during the ten most active hours (reflecting the peak activity level), the average level of activity during the least active five hours (reflecting the level of activity during rest), and the average time that activity reaches its peak (acrophase) and lowest point (nadir).
The other commonly used method to quantify RARs are an extension of the standard cosine modeling approach. These methods, developed by Marler et al. (2), can accommodate the fact that human RARs usually exhibit more ‘square-like’ rather than ‘cosine-like’ curves. To do so, a series of sigmoidal transformations were applied to the traditional cosine model, resulting in ‘extended cosine models’ that fit human RARs better than the standard cosine curve. These models yield information about RAR characteristics including: (1) height, (2) timing, (3) shape, and (4) robustness. Height parameters include the peak to-nadir difference (amplitude) and middle modeled activity level (mesor); to examine whether the RAR is dampened independent of overall activity level, standardized amplitude can also be calculated as amplitude divided by mesor. Timing parameters include the approximate activity initiation time (up-mesor), the time of the activity peak (acrophase), and the approximate time of activity off-set (down-mesor). The extended cosine model also offers two shape parameters: (A) that allows for individual’s to vary in the relative width of the active to rest periods (known as the alpha parameter), and (B) that allows for individual’s to vary in terms of the steepness of their RARs (known as the beta parameter). Finally, the robustness of the RAR is indicated by the pseudo F-statistic, with lower values indicating the observed data cannot be modeled well and is erratic or irregular. These shape parameters and the pseudo-F are illustrated in Figure 1.
Figure 1.
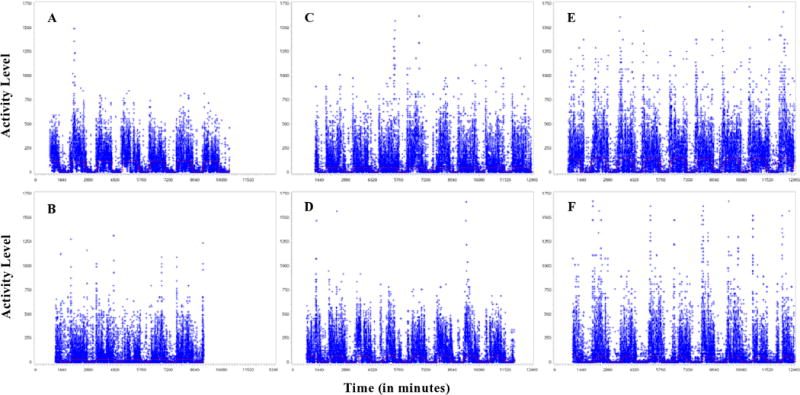
Example recordings illustrating selected measures from the extended cosine model. These recordings are from individual participants in R01HL104607 (PI, Martica Hall, PhD) with: high (A) and low (B) pseudo-F indicating robustness/regularity, high (C) and low (D) beta values indicating the steepness of the curve with higher values indicating more “square-like” curves, low (E) and high (F) alpha indicating the relative width of the active and resting periods with higher values indicating more narrow active periods.
Search method
We performed a PUBMED search with the following terms: (“activity rhythm” or “rest-activity rhythm” or “rest-activity” or “interdaily stability” or “intradaily variability”) and (“mood” or “depression” or “depressed” or “MDD” or “depressive”). Since our focus was on the recent literature, we only included publications filed in PUBMED from 2014 to the time of the search. Thirty-three articles were returned and their titles were evaluated (abstracts as needed) to identify articles meeting the review criteria. Articles were included if they examined RAR measures in relation to a unipolar depressive disorder or depression symptom severity. With the focus on identifying evidence for potentially using RARs to improve depression detection and prevention, articles were excluded if focused mainly on: (A) bipolar disorder or seasonal affective disorder; or (B) clinical treatment outcomes. This resulted in 5 articles, and searching their reference lists yielded an additional 2 articles.
Evidence for RARs as a marker of depression
Six of the identified articles assessed the cross-sectional associations between RAR characteristics and depression (Table 1). Some studies focused on comparing people diagnosed with depression to healthy controls. For example, Hori et al. (3) found that patients with major depressive disorder tended to have lower mesor values (indicating overall lower levels of activity).
Table 1.
Cross-sectional studies of associations between RARs with depression
| Authors/Year | Study Design | Sample | RAR measures | Main findings |
|---|---|---|---|---|
| Hori et al., 2016 | Case-controlled clinical sample | 20 outpatients and 20 age/sex matched controls | Standard cosinor | The single best predictor of depression diagnosis was having lower mesor; having greater WASO also added to prediction of cases. |
| Robillard et al., 2014 | Cross-sectional clinical sample | Help-seeking outpatients with a lifetime history of a mood disorder: 127 currently with and 65 currently without clinically significant symptoms. | Extended cosinor | Having current depressive symptoms was associated with having less robust RARs (as measured based on the goodness of fit to the extended cosine model). No interaction was detected between having depressive symptoms and age in association with RAR robustness, but younger adults tended to have more delayed (later) RARs and older adults tended to have lower amplitude and robustness. |
| Robillard et al., 2015 | Cross-sectional clinical sample | Help-seeking outpatients: 135 with unipolar depressive disorder, 80 with bipolar disorder, 56 with anxiety disorder, 30 with psychosis, and 41 healthy controls. | Extended cosinor | Compared with controls: anxiety, bipolar, and depression groups had later acrophase; the psychosis group had more narrow active periods (higher alpha); psychosis, anxiety, and depression groups had less “square-like” rhythms (lower beta). |
| Maglione et al., 2014 | Cross-sectional community-based sample | 3,020 older women (1,961 with “minimal,” 704 with “some,” and 355 with clinically significant depression symptoms). | Extended cosinor | Having low RAR amplitude, mesor, robustness (pseudo F-statistic), and earlier evening settling were independently associated with prevalent depression symptoms. Low standardized amplitude and later-up mesor were also associated with prevalent depression, but these associations were attenuated by adjustment for several health covariates. |
| Smagula et al., 2015 | Cross-sectional community-based sample | 2,892 older men (2,219 with “minimal,” 496 with “some,” and 177 with clinically significant depression symptoms). | Extended cosinor | Low mesor levels and robustness (pseudo F-statistic) were independently associated with prevalent depression symptoms. Low standardized amplitude, later up-mesor, and later acrophase were associated with prevalent depression symptoms, but these associations were attenuated by adjustments for several health covariates. |
| Luik et al., 2015 | Cross-sectional community-based sample | 1,714 middle aged and elderly participants; | Non-parametric: IS and IV | Lower interdaily stability and higher intradaily variability were associated with depression symptom severity, independent of night-time sleep measures and basic health status covariates. |
In a study of people with a history of depression, Robillard et al. (4) found that being currently symptomatic was associated with having less robust or regularly patterned RARs (measured using the extended cosine model goodness of fit). In these participants who have all been exposed to at least one mood disorder episode, RARs differed by age: younger adults tended to have more delayed (later) RARs, and older adults tended to have less robust RARs.
In a different sample, Robillard et al. (5) found that patients with depression tended to have a later acrophase (timing of the activity peaks) and lower beta values (less steep curves and less distinct “square-like” transitions between resting and active periods). Several of these RAR differences with psychiatrically healthy participants were found to be common across disorders: patients with anxiety and bipolar disorder also had a later acrophase, and patients with psychotic symptoms also had lower beta values.
Among community-dwelling older women, Maglione et al. (6) found that having low RAR amplitude, mesor, pseudo F-statistic, and earlier evening settling all marked prevalent depressive symptoms independent of health status covariates. Standardized amplitude and having a later-up mesor were also associated with depression symptoms, but these associations were attenuated by adjustments for covariates. Consistent with these findings, my colleagues and I recently found that community-dwelling older men with low standardized amplitude (indicating a dampened RAR) were more likely to have prevalent depression symptoms, but that this association was completely attenuated after adjusting for concurrent health status measures (7). Later RAR timing (up-mesor and acrophase) was also associated with the presence of depression symptoms, but again, these associations could be explained by adjustments for health status covariates. On the other hand, men with low mesor levels and low pseudo F-statistics had significantly higher odds of prevalent clinically significant depression symptoms, independent of health covariates.
Other epidemiological research has used non-parametric approaches. Building on their previous research (8), Luik et al (9) found that participants with higher levels of depressive symptoms tended to have lower interdaily stability and higher intradaily variability. These associations were independent of both basic health status covariates and night-time sleep measures.
Summary of the evidence for RARs as a clinically useful marker of depression
Clinicians may find it useful to monitor their patients’ RARs using actigraphy to gain an objective assessment of their behavioral patterns. Current evidence suggests that depression is associated with lower RAR height (3, 6, 7) and alterations to normal RAR timing (4–7). However, some of these associations may be due to other aspects of health that differ between people with and without depression, e.g., differences in the level of daytime activity, lifestyle factors, or the presence of physical co-morbidities (6, 7). Since these RAR characteristics appear to be marking other factors that often co-occur with, but are not unique to depression, they are likely of limited stand-alone value as diagnostic aids.
Having lower RAR robustness or irregular RARs (measured with the pseudo F-statistic (6, 7), lower interdaily stability, and higher intra-daily variability (8)) does appear to be associated with depression independent of confounding health characteristics. However, as pointed out by Rollibard (5), the specific RARs characteristics associated with depression are not necessarily unique to depression. Even if an RAR characteristic is associated with depression independent of other health factors, the same RAR factor could also be associated with other disorders. Therefore, it seems that no single RAR metric will be able to produce adequate discriminative validity (such as sensitivity and positive predictive validity) in detecting depression or depression risk. Instead, multiple RAR metrics may be needed to arrive at a clinically useful RAR signature of depression, or of a group of disorders that share a RAR profile with depression (e.g., one with a combination of altered timing, lower activity levels, less “square-like” shapes, and less regularity).
Presenting an additional challenge towards the goal of developing clinically useful RAR markers of depression, it is unlikely that all patients with depression are characterized by a single RAR profile. For example, patients with MDD may have either timing advances or delays. RAR characteristics differ across the lifespan in patients with (4) and without (8) a history of depression. As a result, the RAR signals associated with depression may be difficult to identify using methods that rely on averaging within heterogeneous groups affected by depression. Indeed, important criteria for establishing screening tools include that the screening instrument applies to a clearly defined target population and a disease outcome that has a known natural history (10). Thus, any clinically useful “RAR signature of depression” may actually vary by depression phenotype, stage, or population sub-group. Future research should therefore seek to establish the RAR profile(s) associated with depression in clearly defined populations, the highest priority of which may be sub-groups at known risk for depression.
Evidence for RARs as a risk factor for depression
Only limited literature has investigated whether RAR measures are associated with prospectively assessed depression risk, i.e., the new incidence of clinically significant depression symptoms or longitudinal changes in depression severity. In the same report on community-dwelling older men discussed above (7), my colleagues and I also assessed whether RARs were associated with the development of clinically significantly depression symptoms about 1 year later. These analyses were conducted among men free of significant depression symptoms at the initial visit (n=2,124). Although men with low amplitude or low standardized amplitude had a greater likelihood of developing depression symptoms, these associations were attenuated to non-significance by adjustment for traditional health risk factors. On the other hand, having a low pseudo F-statistic (indicating RAR robustness) was independently associated with over twice the odds of developing depression.
Following-up in the same cohort of older men (11), we next used a data-driven approach to investigate whether RAR disturbances tended to cluster within people. This identified sub-groups who shared similar RAR characteristics. We then evaluated whether being in any sub-group was associated with exercising faster increases in depression symptom severity over about five years.
When compared with a subgroup that was normative on all RAR parameters (that made up 32% or n=963 of the sample), several of the identified subgroups experienced faster increases in depressive symptom severity over time (Figure 2). One of these sub-groups made up 10.5% of the sample (n=302) and had lower RAR amplitude and robustness (pseudo F-statistic), but appeared normative on the other RAR parameters. Being in this group was associated with having faster increases in depression symptom severity over time, but this association was attenuated after adjustment for health status covariates.
Figure 2.
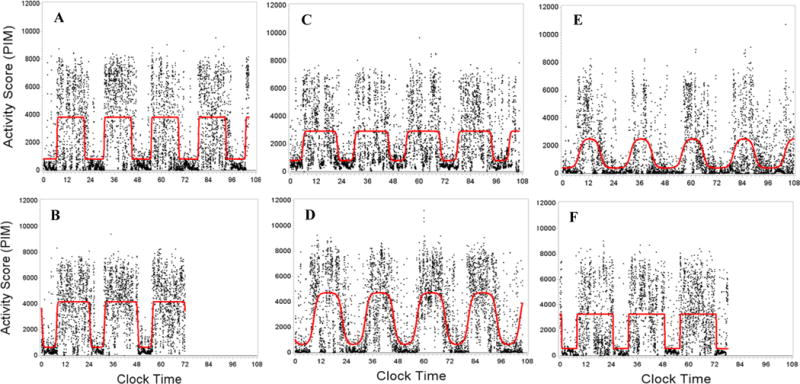
Example recordings illustrating RAR profiles associated with faster increases in depression symptoms in the Outcomes of Sleep Disorders in Older Men Study (MrOS Sleep): (A) normative on all parameters (the reference group), (B) later timing only, (C) lower rhythm height only, (D) later timing with a more narrow active period (high alpha), (E) earlier timing with a more narrow active periods (high alpha) and dampened rhythm (low standardized amplitude), and (F) later timing with lower rhythm height. These groups experienced faster increases in depression symptoms compared with (A), and this was only attenuated by adjustment for health covariates in the case of group C. MrOS Sleep was supported by R01 HL071194, R01 HL070848, R01 HL070847, R01 HL070842, R01 HL070841, R01 HL070837, R01 HL070838, and R01 HL070839. A version of this figure was previously published in (11).
In contrast, four other sub-groups of older men experienced faster increases in depression symptom severity that were independent of adjustments for relevant covariates including physical activity and sleep measures. Two of these groups tended to have lower RAR robustness and height (marked by the pseudo-F statistic, amplitude, and mesor levels): one of these groups had later timing (8.2% or n=247 of the sample), while the other had earlier timing plus a relatively narrow active period (high alpha) and a dampened rhythm (low standardized amplitude; 6.8%, n=204 of the sample). The other two sub-groups who experienced faster increases in depression symptoms, independent of covariates, were: one with only later timing (14.5% or n=434 of the sample), and one with later timing plus low alpha (a relatively shorter active compared with resting period; 8.2% or n=247 of the sample).
Summary of the evidence that RARs represent a depression risk factor and prevention target
These longitudinal findings suggests RARs may be a novel risk factor for depression that acts independent of many relevant covariates including sleep and physical activity. Therefore, RARs represent a potentially important behavioral target for depression prevention. Initially (7), we only found depression risk associated with a measure of rhythm robustness or regularity (the pseudo F-statistic). But our later work (11) revealed that low pseudo F-statistics tended to only be found when overall activity was also low, and that this occurred in diverse groups – those with earlier, normative, and later timing.
Furthermore, only sub-groups with lower levels of RAR robustness/height plus extreme timing (both earlier and later) had faster increases in depression symptom severity independent of relevant covariates. Thus, the pseudo-F statistic may be a general marker of heterogeneous RAR-related depression risk, which is only conferred when co-occurring with other RAR characteristics. The heterogeneity of RAR-related depression risk in this sample of older men was further highlighted by two groups who experienced faster increases in depression symptom severity, but did not have low amplitude or pseudo F-statistic measures; these were the subgroup that had later timing alone and the sub-group with late timing plus a shorter active (compared with resting) period.
Conclusion
RARs provide an objective measure of the behavioral sleep-wake patterns associated with depression. Notably, these include reduced activity levels and regularity as well as differences in activity timing. However, current evidence does not support the use of RAR measures alone for the early detection or diagnosis of depression. Multivariate approaches may be necessary to establish acceptable levels of discriminative utility using RARs to detect depression or depression risk. Since RAR-related depression risk appears to be heterogeneous, future studies (especially those limited in terms of sample size) should minimize this heterogeneity by examining RARs within well-defined populations who are thought share a similar etiologic pathway to depression.
Only limited research has investigated whether RARs are prospectively associated with the development of depression symptoms (7, 11). Initial findings indicate that different combinations of RAR characteristics (or RAR profiles) may increase depression risk. Thus, RAR characteristics may serve as important targets for depression prevention, but replication is needed. This will further clarify which RARs profiles or individual characteristics (e.g., timing delays) uniquely increase depression risk, thus providing interventionists with detailed information regarding the behavioral patterns that must be modified to reduce depression incidence and/or persistence. In addition, there is a need for mechanistically-oriented research to understand the psychosocial and neurobiological meaning of RARs across the course of mood disorders. Mapping objective RAR measures against clinically relevant psychological and biological measures, as they change during depression development, will greatly clarify where best to intervene.
Conclusion
In conclusion, current literature demonstrates that RARs measures provides details regarding behavioral patterns that are not captured using any single sleep or physical activity measures alone. Therefore, RAR measures have an important role helping to characterizing the behavioral changes that are associated with depression and depression risk. But substantial gaps in the literature remain, including the need for detailed and replicable information regarding which specific RAR characteristics, and combinations of characteristics, hasten the development of depression in populations known to be at risk.
As evidence grows, activity monitoring may become useful as a standard clinical practice supporting precisely targeted approaches to prevent depression. But it may be years before additional longitudinal observational studies, replication, and clinical trials can demonstrate the viability of specific RAR targets for depression prevention. While these research activities are underway, clinicians may find it useful to monitor their patients’ RARs and deliver individually tailored advisement based on the recent evidence discussed above, other important work outside the scope of this review (12–16), and their clinical experience.
Key points.
Rest-activity rhythms (RAR) measures provide a comprehensive and objective assessment of behavioral patterns associated with depression, notably including reduced activity levels, that is less regularly patterned, and potentially shifted earlier or later.
The RAR patterns associated with depression may be heterogeneous (multiple patterns may be associated with depression, e.g., differing by patient age or depression phenotype) and/or non-specific (shared across similar disorders or due to depression’s co-travelers).
RARs may serve as a useful tool for clinicians to monitor individual patients, but current evidence does not provide normative data or any valid method for using RARs to diagnosis depression or detect depression risk.
There is a need for further research to define the specific RAR patterns related to developing depression in highly at risk groups and to understand their psychosocial and neurobiological meaning.
Acknowledgments
None
Funding support: SFS is currently supported by a training grant from the National Institute of Mental Health (T32MH19986).
Footnotes
Conflicts of interest: None
References
- 1.van Someren EJ, Hagebeuk EE, Lijzenga C, Scheltens P, de Rooij SE, Jonker C, et al. Circadian rest-activity rhythm disturbances in Alzheimer’s disease. Biological psychiatry. 1996;40(4):259–70. doi: 10.1016/0006-3223(95)00370-3. [DOI] [PubMed] [Google Scholar]
- 2.Marler MR, Gehrman P, Martin JL, Ancoli-Israel S. The sigmoidally transformed cosine curve: a mathematical model for circadian rhythms with symmetric non-sinusoidal shapes. Statistics in medicine. 2006;25(22):3893–904. doi: 10.1002/sim.2466. [DOI] [PubMed] [Google Scholar]
- 3.Hori H, Koga N, Hidese S, Nagashima A, Kim Y, Higuchi T, et al. 24-hour activity rhythm and sleep in depressed outpatients. Journal of psychiatric research. 77:27–34. doi: 10.1016/j.jpsychires.2016.02.022. [DOI] [PubMed] [Google Scholar]
- 4.Robillard R, Naismith SL, Smith KL, Rogers NL, White D, Terpening Z, et al. Sleep-Wake Cycle in Young and Older Persons with a Lifetime History of Mood Disorders. PloS one. 2014;9(2):e87763. doi: 10.1371/journal.pone.0087763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **5.Robillard R, Hermens DF, Naismith SL, White D, Rogers NL, Ip TK, et al. Ambulatory sleep-wake patterns and variability in young people with emerging mental disorders. Journal of psychiatry & neuroscience: JPN. 2015;40(1):28–37. doi: 10.1503/jpn.130247. This article compared RARs between patients with depression and other mental disorders, demonstrating some RAR characteristics are unique and some are shared across disorders. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maglione JE, Ancoli-Israel S, Peters KW, Paudel ML, Yaffe K, Ensrud KE, et al. Depressive Symptoms and Circadian Activity Rhythm Disturbances in Community-Dwelling Older Women. The American journal of geriatric psychiatry: official journal of the American Association for Geriatric Psychiatry. 2013 doi: 10.1016/j.jagp.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *7.Smagula SF, Ancoli-Israel S, Blackwell T, Boudreau R, Stefanick ML, Paudel ML, et al. Circadian rest-activity rhythms predict future increases in depressive symptoms among community-dwelling older men. The American journal of geriatric psychiatry: official journal of the American Association for Geriatric Psychiatry. 2015;23(5):495–505. doi: 10.1016/j.jagp.2014.06.007. This was the first report demonstrating that RAR measures predict the future development of clinically significant depression symptoms. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luik AI, Zuurbier LA, Hofman A, Van Someren EJ, Tiemeier H. Stability and fragmentation of the activity rhythm across the sleep-wake cycle: the importance of age, lifestyle, and mental health. Chronobiology international. 2013;30(10):1223–30. doi: 10.3109/07420528.2013.813528. [DOI] [PubMed] [Google Scholar]
- 9.Luik AI, Zuurbier LA, Direk N, Hofman A, Van Someren EJ, Tiemeier H. 24-hour activity rhythm and sleep disturbances in depression and anxiety: a population-based study of middle-aged and older persons. Depression and anxiety. 2015 doi: 10.1002/da.22355. [DOI] [PubMed] [Google Scholar]
- 10.Andermann A, Blancquaert I, Beauchamp S, Déry V. Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bulletin of the World Health Organization. 2008;86(4):317–9. doi: 10.2471/BLT.07.050112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **11.Smagula SF, Boudreau RM, Stone K, Reynolds CF, 3rd, Bromberger JT, Ancoli-Israel S, et al. Latent activity rhythm disturbance sub-groups and longitudinal change in depression symptoms among older men. Chronobiology international. 2015;32(10):1427–37. doi: 10.3109/07420528.2015.1102925. This article demonstrated that the nature of RAR related depression risk among older men may be heterogeneous, with multiple distinct combinations of RARs (RAR patterns) being related to changes in symptoms over time. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raoux N, Benoit O, Dantchev N, Denise P, Franc B, Alliale J-F, et al. Circadian pattern of motor activity in major depressed patients undergoing antidepressant therapy: Relationship between actigraphic measures and clinical course. Psychiatry research. 1994;52(1):85–98. doi: 10.1016/0165-1781(94)90122-8. [DOI] [PubMed] [Google Scholar]
- 13.Baune BT, Caliskan S, Todder D. A case series on the development of rest-activity rhythm and quality of sleep in patients hospitalized for treatment of uni- or bipolar depression: a potential role for quetiapine. International journal of psychiatry in clinical practice. 2006;10(4):269–75. doi: 10.1080/13651500600736726. [DOI] [PubMed] [Google Scholar]
- 14.Kasper S, Hajak G, Wulff K, Hoogendijk WJ, Montejo AL, Smeraldi E, et al. Efficacy of the novel antidepressant agomelatine on the circadian rest-activity cycle and depressive and anxiety symptoms in patients with major depressive disorder: a randomized, double-blind comparison with sertraline. The Journal of clinical psychiatry. 2010;71(2):109–20. doi: 10.4088/JCP.09m05347blu. [DOI] [PubMed] [Google Scholar]
- 15.Novak D, Albert F, Spaniel F. Analysis of actigraph parameters for relapse prediction in bipolar disorder: a feasibility study; Conference proceedings : Annual International Conference of the IEEE Engineering in Medicine and Biology Society IEEE Engineering in Medicine and Biology Society Annual Conference; 2014. pp. 4972–5. [DOI] [PubMed] [Google Scholar]
- 16.McCall WV. A rest-activity biomarker to predict response to SSRIs in major depressive disorder. Journal of psychiatric research. 2015;64:19–22. doi: 10.1016/j.jpsychires.2015.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]


