Supplemental Digital Content is available in the text.
Keywords: biomarker, emergency services, intensive care units, procalcitonin, sepsis
Abstract
Objectives:
To prospectively validate that the inability to decrease procalcitonin levels by more than 80% between baseline and day 4 is associated with increased 28-day all-cause mortality in a large sepsis patient population recruited across the United States.
Design:
Blinded, prospective multicenter observational clinical trial following an Food and Drug Administration-approved protocol.
Setting:
Thirteen U.S.-based emergency departments and ICUs.
Patients:
Consecutive patients meeting criteria for severe sepsis or septic shock who were admitted to the ICU from the emergency department, other wards, or directly from out of hospital were included.
Interventions:
Procalcitonin was measured daily over the first 5 days.
Measurements and Main Results:
The primary analysis of interest was the relationship between a procalcitonin decrease of more than 80% from baseline to day 4 and 28-day mortality using Cox proportional hazards regression. Among 858 enrolled patients, 646 patients were alive and in the hospital on day 4 and included in the main intention-to-diagnose analysis. The 28-day all-cause mortality was two-fold higher when procalcitonin did not show a decrease of more than 80% from baseline to day 4 (20% vs 10%; p = 0.001). This was confirmed as an independent predictor in Cox regression analysis (hazard ratio, 1.97 [95% CI, 1.18–3.30; p < 0.009]) after adjusting for demographics, Acute Physiology and Chronic Health Evaluation II, ICU residence on day 4, sepsis syndrome severity, antibiotic administration time, and other relevant confounders.
Conclusions:
Results of this large, prospective multicenter U.S. study indicate that inability to decrease procalcitonin by more than 80% is a significant independent predictor of mortality and may aid in sepsis care.
Early diagnosis and initiation of resuscitation measures, antibiotic treatment and/or source control remains the cornerstone of sepsis care (1). Once treatment is initiated, close monitoring of sepsis patients is of utmost importance to identify patients with adverse disease course who may require alternative therapeutic approaches. Secondarily, monitoring may identify patients with a favorable course trajectory who are at low risk for complications warranting discharge from the ICU and possibly deescalation of antibiotic therapy. Appropriate deescalation of the intensity of care with transfer to the floor setting is an important decision because ICU readmissions due to treatment failure on the floor are associated with adverse prognosis and prolonged in-hospital stay (2). Daily assessment of patient risk using objective prognostic data may aid in these intensification and deescalation decisions.
In addition to clinical signs and symptoms, blood markers may assist in patient monitoring (3–6). While serum lactic acid is a biomarker commonly used to help guide response to resuscitation measures (7), procalcitonin (PCT) has been previously demonstrated to be helpful in antibiotic stewardship decisions (8–10). PCT is a host-response marker that is up-regulated by microbial toxins and certain proinflammatory mediators (e.g., interleukin-1b, tumor necrosis factor-α, interleukin-6) and is down-regulated during recovery (11). The expression of PCT is attenuated by the cytokines typically released in response to a viral infection (e.g., interferon-γ); thus, an elevated PCT is typically indicative of a bacterial infection (12). In addition to its diagnostic value, the kinetics of PCT have also been shown to predict mortality and treatment failure in sepsis (13–19). In a recent retrospective analysis involving 256 sepsis patients from two ICUs in the United States, a lack of PCT decrease by more than 80% over the first 72 hours was associated with an increase in ICU and in-hospital mortality, independent of prognostic ICU risk scores (5).
Prior to this study, Food and Drug Administration (FDA) approved use of PCT was limited to single point measurement in the ICU. Therefore, we sought to expand the indication to apply to serial measurements of severe sepsis and septic shock patients, across all hospital settings. Herein, we performed a large, prospective U.S.-based multicenter study to validate the prognostic accuracy of an inability to decrease PCT by more than 80% from baseline to day 4 to predict 28-day mortality in patients with severe sepsis or septic shock who were being admitted to the ICU from the emergency department (ED) or other wards.
MATERIALS AND METHODS
Study Design
This report adheres to the Reporting of Observational trials (STrengthening the Reporting of OBservational studies in Epidemiology) (20). The study protocol was approved by the U.S. FDA and registered at ClinicalTrials.gov (https://clinicaltrials.gov/ct2/show/NCT01523717, Registration date: January 19, 2012).
Patients
Inclusion criteria for this study were adult patients (age, ≥ 18) who were diagnosed with severe sepsis or septic shock according to adapted American College of Chest Physicians/Society of Critical Care Medicine criteria (21–23) (Supplemental trial definitions, Supplemental Digital Content 1, http://links.lww.com/CCM/C411); patients treated in the ICU or a decision to admit the patient from the ED or other wards; blood sampling performed within 12 hours after diagnosis of severe sepsis or septic shock; and willingness to provide written informed consent. We excluded patients without initial blood draw and patients missing data regarding the primary outcome (28-d mortality). For the intention-to-diagnose (ITD) analysis (analysis mandated by the FDA), patients who died or were discharged from the hospital prior to the day 4 blood draw were also excluded (Supplemental Fig. S1, Supplemental Digital Content 1, http://links.lww.com/CCM/C411). We conducted a sensitivity analysis using the per-protocol population (PP) where we excluded patients who did not meet our sepsis definition or were not transferred to the ICU (Supplemental Fig. S1, Supplemental Digital Content 1, http://links.lww.com/CCM/C411).
Data Collection
In addition to blood specimens, we collected clinical data obtained at admission and during the hospital stay. All participating study centers had evidence-based sepsis protocols in place supported by the latest Surviving Sepsis Campaign guidelines for management of patients with severe sepsis and septic shock (24–26).
Primary Endpoint
The primary endpoint of this study was 28-day all-cause mortality. To verify vital status, patients were followed during the hospital stay and contacted by telephone at day 28.
Sample Collection and PCT Measurement
Blood samples were collected within 12 hours after diagnosis of severe sepsis or septic shock and then daily for a total of 5 days. PCT was measured with the B·R·A·H·M·S PCT sensitive KRYPTOR (B·R·A·H·M·S GmbH, Hennigsdorf, Germany) (27). We tested the prognostic accuracy of a lack in PCT decrease of more than 80% (ΔPCT in %) from baseline to day 4. Because in some patients PCT may still increase within the first 24 hours before reaching the maximum level, we also investigated the kinetics from the maximum level on baseline or days 1–4 (Supplemental trial definitions, Supplemental Digital Content 1, http://links.lww.com/CCM/C411). In addition, we investigated the prognostic ability of baseline PCT levels as well as short-term kinetics of PCT from baseline to day 1 for mortality prediction.
Statistical Considerations
The primary study population was the ITD population. The analysis was repeated in the per-PP excluding patients with protocol violations (Supplemental Fig. S1, Supplemental Digital Content 1, http://links.lww.com/CCM/C411). Based on a previous study that identified a decrease in PCT by 80% or lower as the best threshold for predicting mortality, we designed this study to validate this cutoff (5). Therefore, we hypothesized a priori that an inability to decrease PCT by more than 80% from baseline to day 4 would predict 28-day all-cause mortality. Please see online supplement for the details of the statistical approach and sample size calculations.
RESULTS
Patient Population
From December 2011 to March 2014, 858 patients were enrolled in the study, with 38 patients excluded because of missing or withdrawn written informed consent, missing initial blood draw, or missing information regarding the primary outcome (Supplemental Fig. S1, Supplemental Digital Content 1, http://links.lww.com/CCM/C411). There were another 174 patients who were excluded due to a missing day 4 blood draw (median PCT value at baseline was 7.5 μg/L [interquartile range (IQR), 1.7–21.3 μg/L] for the 73 patients excluded due to death and 1.7 μg/L [IQR, 0.3–11.0 μg/L] for the 101 patients excluded due to hospital discharge prior to day 4 blood draw). The main ITD analysis included 646 patients.
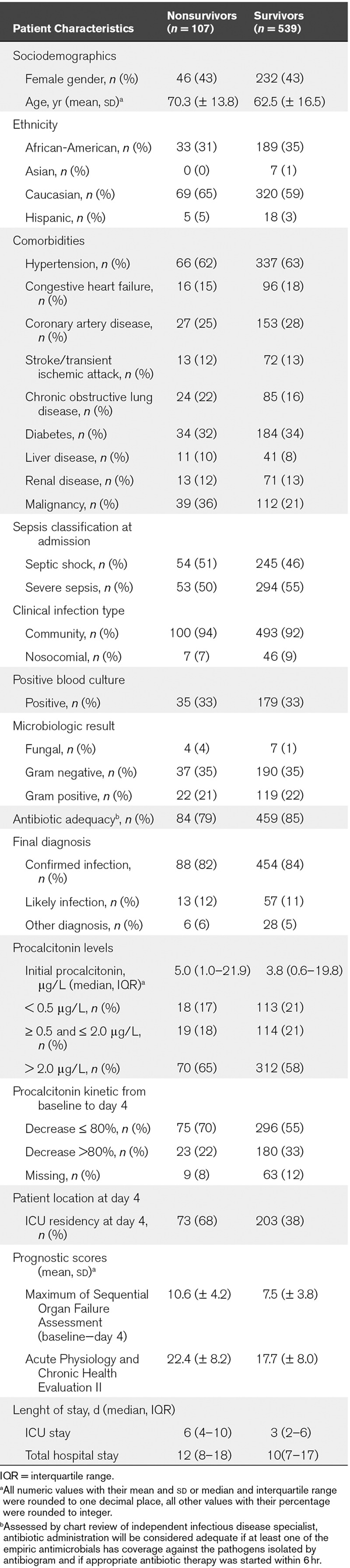
Patients had a mean age of 64 years and 57% were male gender. Infections were mainly community acquired (92%) and slightly more than half of the patients had severe sepsis (54%) when compared with septic shock (46%) (Table 1). Among the 820 patients enrolled were 184 deaths for a 22% all-cause 28-day mortality rate. Among the 646 patients in the ITD population, there were a total of 107 deaths for a 17% overall 28-day mortality rate. The median stay in the ICU was 4 days and patients stayed for a median of 11 days in the hospital. Table 1 shows detailed patient characteristics in the overall ITD population stratified by 28-day survival status. Supplemental Table S1 (Supplemental Digital Content 1, http://links.lww.com/CCM/C411) also shows baseline results in the per-PP and the overall population.
TABLE 1.
Patient Characteristics of the Overall Intention-to-Diagnose Population (n = 646) Stratified by Survival Status
PCT Kinetics and 28-Day Mortality
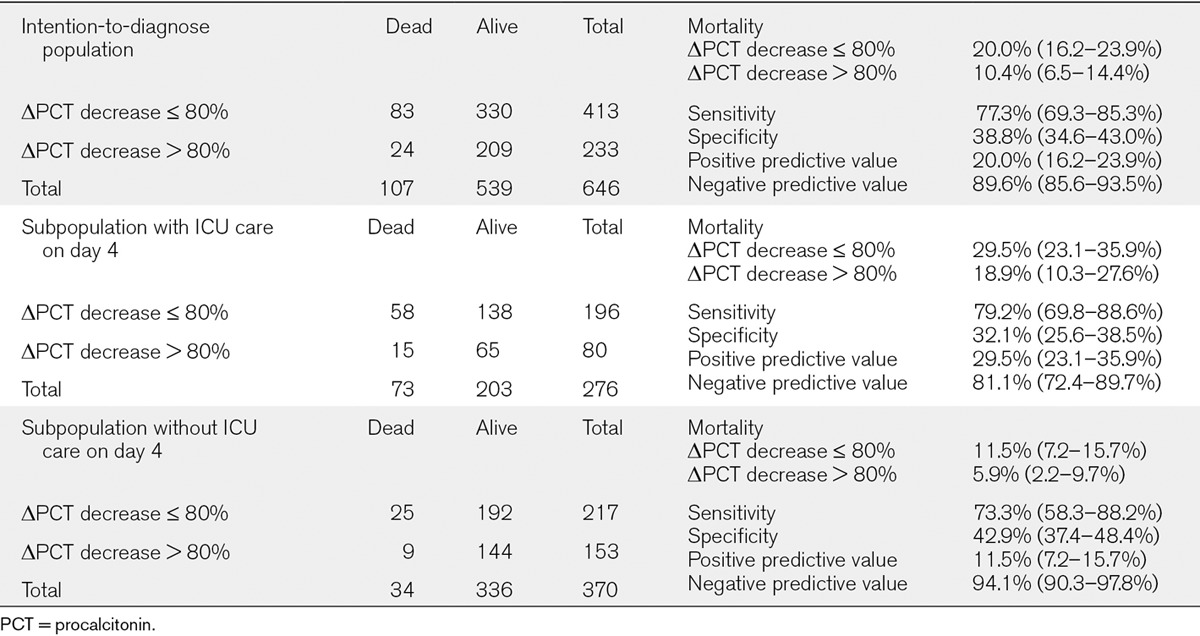
In regard to the primary hypothesis, the mortality rate was nearly double for those who did not decrease their PCT by more than 80% from baseline to day 4 when compared with those who did decrease by more than 80% (20% vs 10%; p = 0.001) (Table 2). The prognostic measures at this cutoff showed a sensitivity of 77% (95% CI, 69–85%) with a specificity of 39% (35–43%), a negative predictive value of 90% (86–94%), and a positive predictive value of 20% (16–24%). In our sensitivity analysis, comparable results were obtained in the per-protocol patient population (Supplemental Fig. S2, a–c, Supplemental Digital Content 1, http://links.lww.com/CCM/C411).
TABLE 2.
Cross Tables and Prognostic Performance of Procalcitonin Decrease (Baseline to Day 4)
Kaplan-Meier and Cox Regression Analysis
Results were further analyzed in a time-to-event analysis. Figure 1 shows Kaplan-Meier plots for the overall population and stratified by patient location at day 4. Again, the 80% PCT decrease cutoff from baseline to day 4 significantly separated survivors from nonsurvivors.
Figure 1.
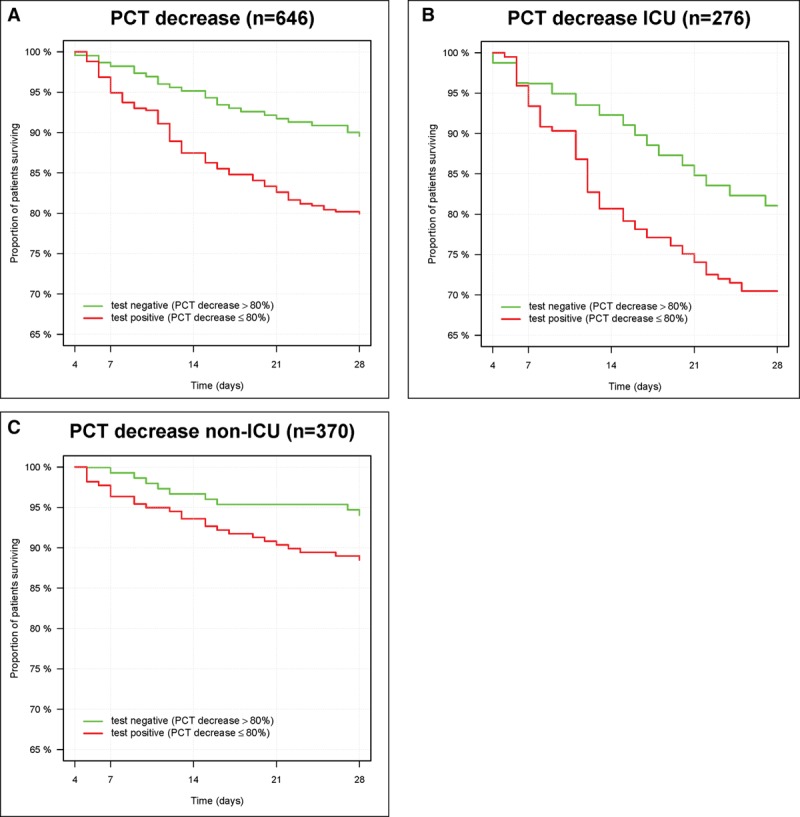
Kaplan-Meier survival curves comparing the survival of patients with procalcitonin (PCT) decrease of at least 80% (red, high-risk group) and patients with PCT decrease > 80% (green, low-risk group) in the overall population (A), in patients in the ICU at day 4 (B) and in patients discharged from the ICU to the hospital ward on or prior to day 4 (C). (Per study methodology patients were excluded who died or went home until day 4.)
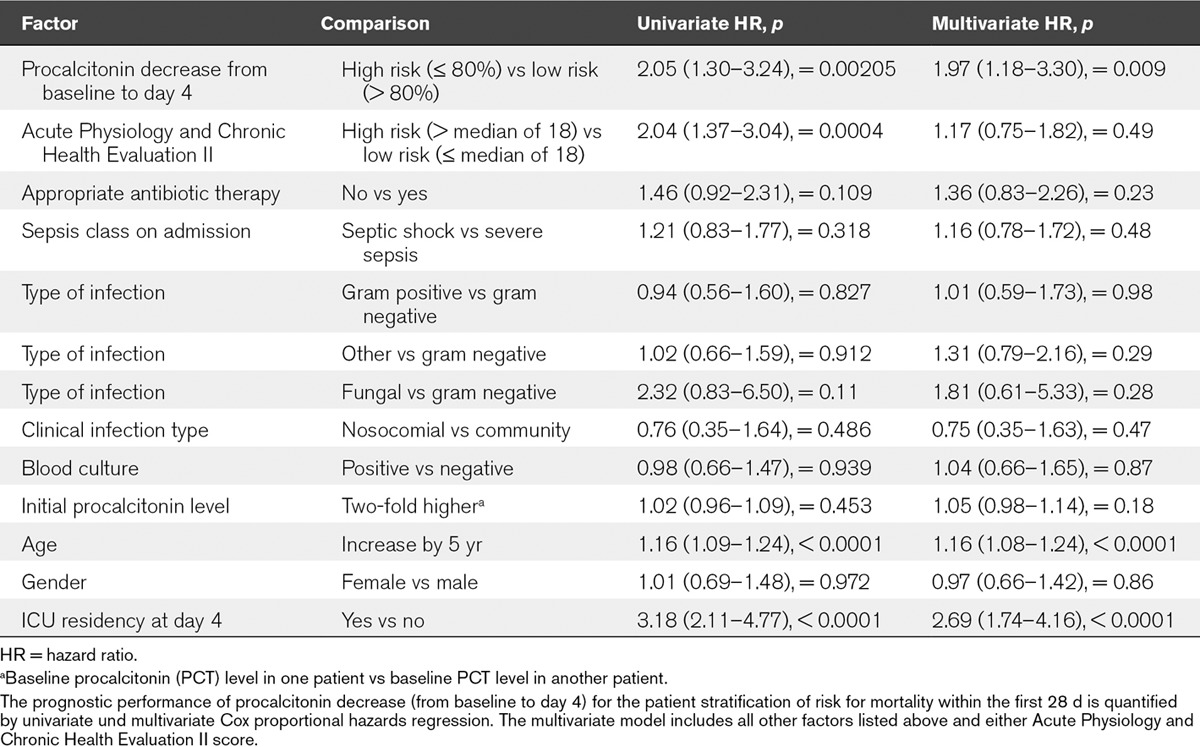
To assess whether the PCT decrease provides prognostic information beyond that of other clinical outcome predictors, we calculated multivariate Cox regression models including Acute Physiology and Chronic Health Evaluation (APACHE) II or maximum Sequential Organ Failure Assessment (SOFA) score, as well as nine clinical variables associated with severity and/or adverse outcome (appropriateness of antibiotic therapy, sepsis syndrome, microbiology, nosocomial vs community infection, blood culture positivity, initial PCT level, age, gender, and patient location at day 4). In the unadjusted analysis, the hazard ratio (HR) for 28-day mortality of patients without a PCT decrease of more than 80% until day 4 was 2.05 (95% CI, 1.30–3.24) (Table 3). This result remained robust in the model including adjustment for APACHE II and nine other variables with a HR of 1.97 (95% CI, 1.18–3.30; p < 0.01). Results were similar when using maximum SOFA score instead of APACHE II in the fully adjusted model (Supplemental Table S2, Supplemental Digital Content 1, http://links.lww.com/CCM/C411). Furthermore, PCT remains a significant predictor in models incorporating change in WBC count between baseline and day 4 (Supplemental Table S3, Supplemental Digital Content 1, http://links.lww.com/CCM/C411), as well as a model incorporating change in SOFA score between baseline and day 4 (Supplemental Table S4, Supplemental Digital Content 1, http://links.lww.com/CCM/C411). We also note that the maximum SOFA score over the first 4 days (stratified by maximum SOFA, > 8) is also associated with a approximately two-fold mortality risk (Supplemental Table S2, Supplemental Digital Content 1, http://links.lww.com/CCM/C411). We repeated the same analyses in the per-protocol patient population and achieved comparable results (Supplemental Table S5, Supplemental Digital Content 1, http://links.lww.com/CCM/C411).
TABLE 3.
Results of the Univariate and Multivariate Cox Proportional Hazards Regression Based on the Intention-to-Diagnose Patient Population
Secondary Analysis
Shorter Term Change in PCT (Baseline to Day 1) and Baseline PCT. In addition to the primary analysis where we analyzed the prognostic value of a PCT decrease of more than 80% between baseline and day 4, we assessed the prognostic value of a shorter term change of PCT between baseline and day 1. Among the 752 patients available for analysis, patients who died have an average mean increase of 30% (95% CI, 15–47%) when compared with 0% (95% CI, –7% to +6%) for those who survived (p < 0.001). The area under the curve (AUC) for the short-term increase was 0.64 (95% CI, 0.59–0.69). When simply stratifying by patients with an initial increase in PCT from baseline to day 1 (n = 323) when compared with a decrease (n = 429), patients with a PCT increase had an almost three-fold higher mortality (mortality, 29% vs 12%; p < 0.0001).
In addition to the concept of serial PCT measurements, we investigated the ability of a single PCT value to predict 28-day all-cause mortality at baseline (n = 820). Although nonsurvivors had higher mean baseline PCT levels compared with survivors (5.2 μg/L [95% CI, 3.9–7.0 μg/L] vs 3.4 μg/L [95% CI, 2.8–4.0 μg/L]; p < 0.02), a single PCT value at baseline was less predictive for 28-day mortality than serial measurements (Supplemental Table S6, Supplemental Digital Content 1, http://links.lww.com/CCM/C411). The AUC for baseline PCT as a predictor of mortality was 0.56 (95% CI, 0.51–0.60). Furthermore, when comparing the PCT values over the first 5 days among survivors versus nonsurvivors, the PCT values for the nonsurvivors were higher and stayed higher on all days 1–5 (Fig. 2).
Figure 2.
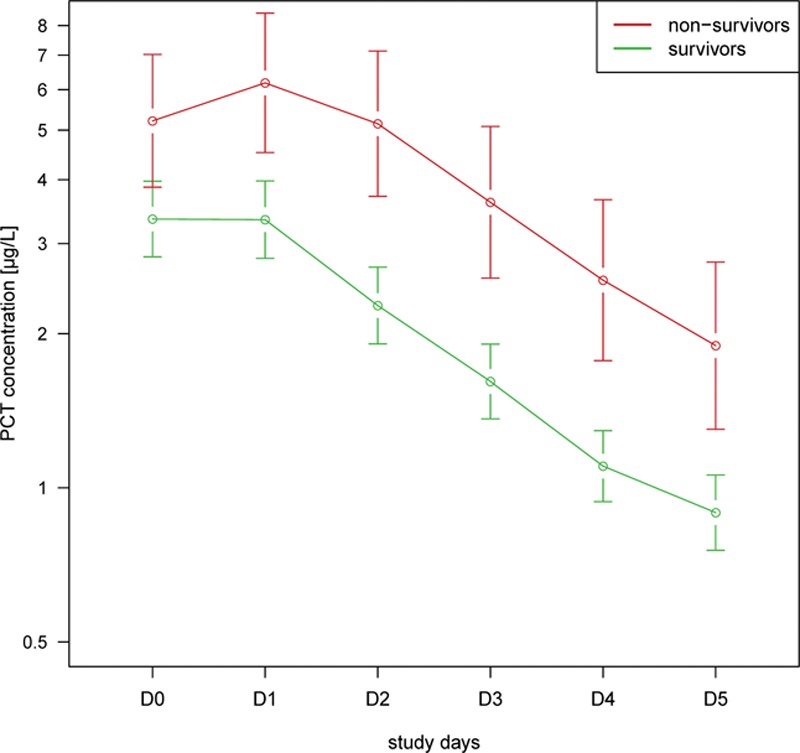
Course of all available procalcitonin (PCT) concentrations (means and 95% CIs) grouped by 28-d outcome (red—nonsurvivors; green—survivors) and study day.
Combined Initial PCT, PCT Change, and ICU Status. As an additional exploratory analysis requested by the FDA, we assessed whether the prognostic performance of our main covariate of interest, PCT reduction of more than 80% at day 4, was different when stratified by patient location at day 4 (ICU vs non-ICU) (Table 2). Mortality was higher in patients still hospitalized in the ICU at day 4 (26%) than in those patients already discharged to the floor at day 4 (9%). Among patients discharged from the ICU by day 4 who had a high baseline PCT value of greater than 2 μg/L, mortality was more than three-fold increased if PCT did not drop by more than 80% (19% vs 5%) (Supplemental Table S7, Supplemental Digital Content 1, http://links.lww.com/CCM/C411). Similarly, for patients still residing in the ICU at day 4 and low baseline PCT of less than or equal to 2 μg/L, mortality was about three-fold higher if PCT did not drop by more than 80% compared with PCT that decreased by more than 80% (26% vs 10%).
DISCUSSION
Within this large, multicenter study including 13 study sites across the United States, we found that kinetics of PCT over the first 4 days were predictive for survival of patients diagnosed with severe sepsis or septic shock. These results remained significant after multivariate adjustment for other known prognostic variables and risk factors. These findings validate previous retrospective research from the United States (5), as well as other smaller studies (14, 16–19). In addition to daily routine clinical assessment, monitoring of PCT in this patient population was demonstrated to aid in risk assessment, which may translate into better informed clinical decisions regarding intensification of care or ICU discharge.
Previous Related PCT Studies
Several studies have investigated the prognostic utility of PCT in systemic infection and sepsis (reviewed in [15]). In one retrospective analysis from the United States, PCT change over the first 72 hours was also a predictor for ICU and in-hospital mortality in sepsis patients, independent of ICU risk scores (APACHE IV and Simplified Acute Physiology Score II) (5). In addition to general sepsis, studies also found PCT to improve risk stratification in respiratory infections, mainly community-acquired pneumonia and chronic obstructive pulmonary disease exacerbation (15, 16). An individual patient data meta-analysis including more than 4,000 patients from 14 trials found an association between admission PCT levels and treatment failure across different types of respiratory infections and treatment settings (16). In a large U.S. pneumonia cohort (28), the greatest benefit of PCT was found in patients classified as high risk by the pneumonia severity index. A PCT level less than 0.1 μg/L virtually excluded mortality in these high-risk patients. Our current analysis is in line with these previous investigations and supports the prognostic utility of PCT when measured serially.
Implications of Findings
Early recognition and the start of appropriate antibiotic treatment, fluid resuscitation, source control, and close patient monitoring remain the cornerstone of care to lower sepsis related morbidity and mortality (1). In real-life practice, this remains challenging because clinical variables lack specificity for sepsis etiology and prognosis (29). Additionally, microbiologic diagnostics have low sensitivity and modalities such as cultures do not provide needed information in a timely fashion. Therefore, sepsis biomarkers are promising tools to help monitor patient response to therapy and may help guide therapeutic decisions in individual patients. It is particularly challenging during initial patient evaluation to determine which patients with sepsis will not respond well to therapeutic measures, and thus will have worsening of their clinical status. Specifically, the development of new or worsening organ dysfunction portends poor outcome and is a common pathway to death in these patients (30, 31). Novel strategies that improve a clinician’s ability to accurately risk stratify patients with suspected sepsis facilitate early and appropriate therapeutic intervention, improve important triage decisions (e.g., admission to the hospital vs discharge home, or admission to ICU vs non-ICU bed, or continuation of care in the ICU vs discharge to the hospital ward), and provide a means to follow response to therapy, including antibiotic stewardship (32). PCT has generated much interest as a sepsis biomarker that is associated with increased risk and severity of bacterial infection. PCT has also been found to correlate with risk of culture-proven bacteremia (33). Although the biological function of PCT in host defense is incompletely understood, this peptide influences the immune system in various ways including a decrease in phagocytic and candidacidal activity of neutrophils and also leads to an increase in the concentration of intracellular calcium ions (34, 35) which facilitate the host response.
Importantly, previous research demonstrates that PCT can be used to inform antibiotic stewardship decisions, mainly by reducing antibiotic initiation in low-risk patients (i.e., bronchitis, upper respiratory infection) and by early stoppage of antibiotics in patients with pneumonia and sepsis (10, 32, 36). A recent 1,500 patient multicenter, ICU trial from the Netherlands which included more than 1,500 patients with suspected or confirmed infection found a significant reduction in antibiotic use and a mortality in the group that followed a PCT-based antibiotic stewardship algorithm (37, 38). Our observation that a drop in PCT of at least 80% was associated with survival outcomes further supports the approach of monitoring PCT levels over time. Interestingly, our secondary analysis identified that simply assessing whether PCT decreases or increases from baseline to day 1 revealed a three-fold higher mortality in patients with a short-term increase in PCT levels. This simple finding could prove particularly useful during early critical care management. However, while PCT may contribute to prognosis, it is not able to identify nonsurvivors such that one would, for example, withdraw care if the PCT level does not decrease by more than 80%. Still, beyond antibiotic deescalation in patients with clinical improvement and decreasing PCT levels, it remains unclear which therapeutic and/or diagnostic measures should be used in patients with nondecreasing PCT levels to improve outcomes (39, 40). One large critical care trial investigating whether PCT-guided initiation and escalation of antimicrobial therapy would improve survival did not find any outcomes benefit for this strategy (13). However, further interventional studies are needed to investigate whether monitoring of PCT kinetics over longer time periods will improve outcomes in patients with sepsis. Such a study should also investigate costs of PCT measurement and possible costs savings. Based on a literature review, a previous study has estimated of the total cost of performing a PCT assay, including assay material, reagents, technician time, purchase, maintenance of a bench top analyzer, and overhead, to be approximately Can$49.42 (approximately $50 USD) per test (41).
Strengths and Limitations
The strengths of this study are the rigorous study design with a large sample size, prospective inclusion of patients being treated for sepsis in different experienced centers across the United States, and the relatively low number of patients who were lost to follow-up. The study hypothesis was defined a priori, based on retrospective data (5), which strengthens our conclusions and provides external validation. As a limitation, we were not able to use patients who died or were discharged prior to the day 4 blood draw in our main analysis and the prognostic accuracy in these patients is not clearly defined. Also, as an observational study, we cannot make conclusions about clinical effects of using a PCT algorithm for patient care. An interventional study is needed to test the hypothesis that serial monitoring of PCT will improve clinical decisions and outcomes (10, 40).
CONCLUSIONS
The results of this large, U.S.-based prospective multicenter study in several U.S. hospitals indicate that inability to decrease PCT by at least 80% is a significant independent predictor of mortality and may aid in sepsis care.
ACKNOWLEDGMENTS
We are grateful to all the physicians, nursing staff, and patients who participated in this study.
Supplementary Material
Footnotes
Trial registration: https://clinicaltrials.gov/ct2/show/NCT01523717. Registered: January 19, 2012.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
B·R·A·H·M·S GmbH funded the trial and the institutions of all authors received research funding to support the conduct of this trial.
Dr. Schuetz received support from B·R·A·H·M·S GmbH and bioMérieux to attend meetings and fulfill speaking engagements and received research grants from these two firms. Dr. Birkhahn’s institution received funding from Alere. Dr. Singer received support for article research from Thermo Fisher Scientific. Dr. Runyon’s institution received funding from National Institute of General Medical Sciences of the National Institutes of Health (NIH), Center for Disease Control and Prevention, and National Highway Traffic Safety Administration. He disclosed other support from MedEvac Foundation, Carolinas Trauma Network Research Center of Excellence, Janssen Pharmaceutical Companies, Emergency MCG USA, Siemens Healthcare Diagnostics, Boehringer Ingelheim Pharmaceuticals, Trinity Biotech, Durata Therapeutics International, Abbott Fund, and Bristol- Myers Squibb. Dr. Self received funding from B·R·A·H·M·S/ThermoFisher (funding to conduct the study reported in this article). He received funding from Bio-Fire (consultant fees), Abbott POC (consultant fee), and Venaxis (consultant fees). He disclosed other support from Pfizer (funding for clinical research), Venaxis (funding for clinical research), RPS (funding for clinical research), Kypha (funding for clinical research), and BioAegis (funding for clinical research). He received support for article research from the NIH. Drs. Ebmeyer, Johannes, Wiemer, and Schwabe are employees of B·R·A·H·M·S GmbH, which is the company that sponsored the trial reported in this article and manufacturer of B·R·A·H·M·S PCT sensitive Kryptor. Dr. Shapiro has received consulting and speaking fees from B·R·A·H·M·S GmbH and Siemens Medical. He received funding from Cheetah Medical and Cumberland Pharma. He disclosed other support from rapid pathogen screening and nanomix. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Dellinger RP, Levy MM, Rhodes A, et al. Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup: Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 2013; 39:165–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ouanes I, Schwebel C, Français A, et al. Outcomerea Study Group: A model to predict short-term death or readmission after intensive care unit discharge. J Crit Care 2012; 27:422.e1–422.e9 [DOI] [PubMed] [Google Scholar]
- 3.Jun KR, Lee JN, Song SA, et al. Serial changes in serum procalcitonin, interleukin 6, and C-reactive protein levels according to non-specific surgical stimulation. Clin Chem Lab Med 2015; 53:549–558 [DOI] [PubMed] [Google Scholar]
- 4.Henriquez-Camacho C, Losa J.Biomarkers for sepsis. Biomed Res Int 2014; 2014:547818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schuetz P, Maurer P, Punjabi V, et al. Procalcitonin decrease over 72 hours in US critical care units predicts fatal outcome in sepsis patients. Crit Care 2013; 17:R115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schuetz P, Litke A, Albrich WC, et al. Blood biomarkers for personalized treatment and patient management decisions in community-acquired pneumonia. Curr Opin Infect Dis 2013; 26:159–167 [DOI] [PubMed] [Google Scholar]
- 7.Jones AE, Shapiro NI, Trzeciak S, et al. Emergency Medicine Shock Research Network (EMShockNet) Investigators: Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: A randomized clinical trial. JAMA 2010; 303:739–746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schuetz P, Mueller B.Procalcitonin: An effective screening tool and safe therapeutic decisionmaking aid for emergency department patients with suspected sepsis. Ann Emerg Med 2015; 66:318–319 [DOI] [PubMed] [Google Scholar]
- 9.Schuetz P, Mueller B.Biomarker-guided de-escalation of empirical therapy is associated with lower risk for adverse outcomes. Intensive Care Med 2014; 40:141. [DOI] [PubMed] [Google Scholar]
- 10.Schuetz P, Briel M, Christ-Crain M, et al. Procalcitonin to guide initiation and duration of antibiotic treatment in acute respiratory infections: An individual patient data meta-analysis. Clin Infect Dis 2012; 55:651–662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schuetz P, Albrich W, Mueller B.Procalcitonin for diagnosis of infection and guide to antibiotic decisions: Past, present and future. BMC Med 2011; 9:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linscheid P, Seboek D, Schaer DJ, et al. Expression and secretion of procalcitonin and calcitonin gene-related peptide by adherent monocytes and by macrophage-activated adipocytes. Crit Care Med 2004; 32:1715–1721 [DOI] [PubMed] [Google Scholar]
- 13.Jensen JU, Hein L, Lundgren B, et al. Procalcitonin And Survival Study (PASS) Group: Procalcitonin-guided interventions against infections to increase early appropriate antibiotics and improve survival in the intensive care unit: A randomized trial. Crit Care Med 2011; 39:2048–2058 [DOI] [PubMed] [Google Scholar]
- 14.Karlsson S, Heikkinen M, Pettilä V, et al. Finnsepsis Study Group: Predictive value of procalcitonin decrease in patients with severe sepsis: A prospective observational study. Crit Care 2010; 14:R205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schuetz P, Amin DN, Greenwald JL.Role of procalcitonin in managing adult patients with respiratory tract infections. Chest 2012; 141:1063–1073 [DOI] [PubMed] [Google Scholar]
- 16.Kutz A, Briel M, Christ-Crain M, et al. Prognostic value of procalcitonin in respiratory tract infections across clinical settings. Crit Care 2015; 19:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruiz-Rodríguez JC, Caballero J, Ruiz-Sanmartin A, et al. Usefulness of procalcitonin clearance as a prognostic biomarker in septic shock. A prospective pilot study. Med Intensiva 2012; 36:475–480 [DOI] [PubMed] [Google Scholar]
- 18.Suberviola B, Castellanos-Ortega A, González-Castro A, et al. [Prognostic value of procalcitonin, C-reactive protein and leukocytes in septic shock]. Med Intensiva 2012; 36:177–184 [DOI] [PubMed] [Google Scholar]
- 19.Pieralli F, Vannucchi V, Mancini A, et al. Procalcitonin kinetics in the first 72 hours predicts 30-day mortality in severely ill septic patients admitted to an intermediate care unit. J Clin Med Res 2015; 7:706–713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, et al. Iniciativa STROBE: [The Strengthening the Reporting of Observational Studies in Epidemiology [STROBE] statement: Guidelines for reporting observational studies]. Gac Sanit 2008; 22:144–150 [DOI] [PubMed] [Google Scholar]
- 21.Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003; 31:1250–1256 [DOI] [PubMed] [Google Scholar]
- 22.Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992; 101:1644–1655 [DOI] [PubMed] [Google Scholar]
- 23.Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996; 22:707–710 [DOI] [PubMed] [Google Scholar]
- 24.Shapiro NI, Howell M, Talmor D.A blueprint for a sepsis protocol. Acad Emerg Med 2005; 12:352–359 [DOI] [PubMed] [Google Scholar]
- 25.Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: Results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med 2010; 36:222–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dellinger RP, Levy MM, Carlet JM, et al. International Surviving Sepsis Campaign Guidelines Committee; American Association of Critical-Care Nurses; American College of Chest Physicians; American College of Emergency Physicians; Canadian Critical Care Society; European Society of Clinical Microbiology and Infectious Diseases; European Society of Intensive Care Medicine; European Respiratory Society; International Sepsis Forum; Japanese Association for Acute Medicine; Japanese Society of Intensive Care Medicine; Society of Critical Care Medicine; Society of Hospital Medicine; Surgical Infection Society; World Federation of Societies of Intensive and Critical Care Medicine: Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 2008; 36:296–32718158437 [Google Scholar]
- 27.Christ-Crain M, Jaccard-Stolz D, Bingisser R, et al. Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: Cluster-randomised, single-blinded intervention trial. Lancet 2004; 363:600–607 [DOI] [PubMed] [Google Scholar]
- 28.Huang DT, Weissfeld LA, Kellum JA, et al. GenIMS Investigators: Risk prediction with procalcitonin and clinical rules in community-acquired pneumonia. Ann Emerg Med 2008; 52:48–58.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vincent JL.Dear SIRS, I’m sorry to say that I don’t like you. Crit Care Med 1997; 25:372–374 [DOI] [PubMed] [Google Scholar]
- 30.Abraham E, Laterre PF, Garg R, et al. Administration of Drotrecogin Alfa (Activated) in Early Stage Severe Sepsis (ADDRESS) Study Group: Drotrecogin alfa (activated) for adults with severe sepsis and a low risk of death. N Engl J Med 2005; 353:1332–1341 [DOI] [PubMed] [Google Scholar]
- 31.Shapiro N, Howell MD, Bates DW, et al. The association of sepsis syndrome and organ dysfunction with mortality in emergency department patients with suspected infection. Ann Emerg Med 2006; 48:583–90, 590.e1 [DOI] [PubMed] [Google Scholar]
- 32.Schuetz P, Chiappa V, Briel M, et al. Procalcitonin algorithms for antibiotic therapy decisions: A systematic review of randomized controlled trials and recommendations for clinical algorithms. Arch Intern Med 2011; 171:1322–1331 [DOI] [PubMed] [Google Scholar]
- 33.Laukemann S, Kasper N, Kulkarni P, et al. Can we reduce negative blood cultures with clinical scores and blood markers? results from an observational cohort study. Medicine (Baltimore) 2015; 94:e2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Christ-Crain M, Müller B.Calcitonin peptides–the mediators in sepsis or just another fairy tale? Crit Care Med 2008; 36:1684–1687 [DOI] [PubMed] [Google Scholar]
- 35.Becker KL, Snider R, Nylen ES.Procalcitonin in sepsis and systemic inflammation: A harmful biomarker and a therapeutic target. Br J Pharmacol 2010; 159:253–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bouadma L, Luyt CE, Tubach F, et al. PRORATA trial group: Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): A multicentre randomised controlled trial. Lancet 2010; 375:463–474 [DOI] [PubMed] [Google Scholar]
- 37.de Jong E, van Oers JA, Beishuizen A, et al. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: A randomised, controlled, open-label trial. Lancet Infect Dis 2016; 16:819–827 [DOI] [PubMed] [Google Scholar]
- 38.Schuetz P, Mueller B.Procalcitonin in critically ill patients: Time to change guidelines and antibiotic use in practice. Lancet Infect Dis 2016; 16:758–760 [DOI] [PubMed] [Google Scholar]
- 39.Schuetz P, Mueller B.To escalate or to de-escalte–that is the question. Crit Care Med 2011; 39:2590; author reply 2591 [DOI] [PubMed] [Google Scholar]
- 40.Jensen JU, Heslet L, Jensen TH, et al. Procalcitonin increase in early identification of critically ill patients at high risk of mortality. Crit Care Med 2006; 34:2596–2602 [DOI] [PubMed] [Google Scholar]
- 41.Heyland DK, Johnson AP, Reynolds SC, et al. Procalcitonin for reduced antibiotic exposure in the critical care setting: A systematic review and an economic evaluation. Crit Care Med 2011; 39:1792–1799 [DOI] [PubMed] [Google Scholar]


