Abstract
Testosterone induces a lethal outcome in otherwise self-healing blood-stage malaria caused by Plasmodium chabaudi. Here, we examine possible testosterone effects on the antimalaria effectors spleen and liver in female C57BL/6 mice. Self-healing malaria activates gating mechanisms in the spleen and liver that lead to a dramatic reduction in trapping activity, as measured by quantifying the uptake of 3-μm-diameter fluorescent polystyrol particles. However, testosterone delays malaria-induced closing of the liver, but not the spleen. Coincidently, testosterone causes an ∼3- to 28-fold depression of the mRNA levels of nine malaria-responsive genes, out of 299 genes tested, only in the liver and not in the spleen, as shown by cDNA arrays and Northern blotting. Among these are the genes encoding plasminogen activator inhibitor (PAI1) and hydroxysteroid sulfotransferase (STA2). STA2, which detoxifies bile acids, is suppressed 10-fold by malaria and an additional 28-fold by testosterone, suggesting a severe perturbation of bile acid metabolism. PAI1 is protective against malaria, since disruption of the PAI1 gene results in partial loss of the ability to control the course of P. chabaudi infections. Collectively, our data indicate that the liver rather than the spleen is a major target organ for testosterone-mediated suppression of resistance against blood-stage malaria.
Testosterone is known for its immunosuppressive activity (39), and this has often been invoked as the major reason for the higher susceptibility of males to a wide variety of infectious diseases (28, 35). An extreme gender dependence has been described for the experimental malaria parasite Plasmodium chabaudi. Male mice succumb to blood-stage infections, whereas female mice are able to self-heal the same infections (46). However, lowering of testosterone levels by the castration of male mice results in a resistant phenotype, and conversely, testosterone treatment of females or castrated males results in a susceptible phenotype (46, 47).
The spleen is accepted as the major effector of the immune defense against blood-stage malaria (15). Spleen macrophages eliminate Plasmodium-infected erythrocytes via phagocytosis, which occurs predominantly in unique extravascular pathways (43, 50) with arterioles opening directly into the reticular meshwork of the red pulp. This open circulation of the spleen switches to a closed state during the precrisis of acute malaria, presumably controlled by malaria-activated barrier cells (43, 44). The closed state of splenic circulation protects the spleen from malaria parasites, resulting in lower numbers of activated macrophages and allowing erythropoiesis and lymphopoiesis, generation of effector T cells, and affinity maturation of B cells to proceed unperturbed without the devastating effects of uncontrolled inflammation (44, 45).
The liver is known as the site of preerythrocytic development of Plasmodium parasites, but although it is largely forgotten, the liver is also an important effector against malarial blood stages (4, 27). In particular, the reticular endothelial system (RES) of the liver is able to eliminate parasite-derived hemozoin and even Plasmodium-infected erythrocytes through phagocytosis (1). However, it is not yet known whether the liver—similarly to the spleen—also exhibits protective gating mechanisms that prevent uncontrolled inflammation during acute blood-stage malaria.
Both the spleen and the liver are known as target organs for testosterone. Indeed, testosterone has been described as affecting the cellularity of the spleen (8) and even causing carcinomas in the liver (29, 33). Testosterone exerts most of its effects through activation or repression of transcription (26). However, possible testosterone effects on gene expression in the spleen and the liver in the context of defense against blood-stage malaria have not yet been investigated. Here, we show that testosterone affects malaria-induced changes in RES activity and gene expression in the liver, but not in the spleen. Alterations in the liver are therefore critical for the testosterone-induced lethal outcome of P. chabaudi blood-stage malaria.
MATERIALS AND METHODS
Mice.
C57BL/6 mice were bred under specific-pathogen-free conditions at the central animal facilities of our university. PAI1-deficient mice containing the Serpine1tm1Mlg allele on an 87.5% C57BL/6-12.5% 129S2/SvPas background (11), as well as control mice with the same background, were bred at the animal facility of the University of Leuven. Experiments were performed with female mice, which were housed in plastic cages and received a standard diet (Wohrlin, Bad Salzuflen, Germany) and water ad libitum. The experiments were approved by the state authorities and followed German law on animal protection.
Testosterone treatment.
Mice were subcutaneously injected with 100 μl of sesame oil containing 0.9 mg of testosterone (Testoviron-Depot-50; Schering, Berlin, Germany) twice a week for 3 weeks (8, 46). Controls received only the vehicle.
Infections.
Blood stages of P. chabaudi were passaged weekly in NMRI mice (48). C57BL/6 mice were challenged with 106 P. chabaudi-parasitized erythrocytes. Parasitemia was evaluated in Giemsa-stained blood smears. The total number of erythrocytes was determined in a Neubauer chamber.
Determination of particle trapping.
Each mouse was anesthetized, weighed, and then injected with 200 μl of phosphate-buffered saline containing 1.3 × 108 3-μm-diameter green fluorescent beads (Duke Scientific, Palo Alto, Calif.) in the retroorbital plexus according to the method of Pinkerton and Webber (32). After 5 min, the mice were killed by cervical dislocation, and the spleens and parts of the liver lobes were removed. After being weighed, the organs were squeezed with a glass rod in 8 ml of 2.3 M KOH-0.5% Tween 80 in ethanol. Then, 5 × 105 red beads (2.9-μm diameter; Duke Scientific) were added as a control to estimate possible losses during the extraction procedure, and the tissues were dissolved by shaking them at 50°C for 48 h, interrupted several times by vigorous vortexing. Samples were centrifuged at 2,000 × g and 20°C for 20 min, and the pellet with the beads was washed with 8 ml of 1% Triton X-100 and then with 8 ml of phosphate-buffered saline and finally resuspended in 1 ml of distilled water. The fluorescence intensity was measured in a luminescence spectrometer (LS 55; Perkin-Elmer, Langen, Germany) using a 10- by 2-mm quartz precision cell (Hellma, Mühlheim, Germany) at excitation-emission wavelengths of 450-480 and 520-590 nm for green and red beads, respectively.
Liver histology.
Small pieces of the liver were fixed in 10% formalin overnight and embedded in paraffin, and 6-μm-thick sections were stained with hematoxylin-eosin. Histological changes were evaluated using a modified version of the quantitative scoring system of Ishak et al. (22).
RNA isolation.
Spleen and liver pieces were rapidly frozen and stored at −80°C. Total RNA was isolated by standard procedures using a commercially available RNA isolation kit (QIAGEN, Hilden, Germany). Poly A+ RNA was purified using Oligotex (QIAGEN). The quality of the RNA was routinely tested for genomic DNA impurity, the 28S/18S ratio, and the ratio of the optical densities at 280 and 260 nm and for integrity by capillary electrophoresis using a Bioanalyzer 2100 (Agilent Technologies, Palo Alto, Calif.) and a spectrophotometer.
cDNA arrays.
Custom-designed PIQOR cDNA arrays (Memorec, Cologne, Germany) were constructed on treated glass slides provided with quadruplicate samples of defined 200- to 400-bp cDNA fragments selected from 299 different genes of the mouse. The arrays contained buffer and herring DNA as negative controls, four control RNAs from Escherichia coli, and the six positive control cDNAs GAPDH (glyceraldehyde-3-phosphate dehydrogenase), α actin, α tubulin, β tubulin, cyclophilin, and hypoxanthine-guanine phosphoribosyltransferase.
Labeling and hybridization.
cDNAs were labeled with Cy3-Cy5 and hybridized on the arrays as detailed previously (10). In brief, 100 μg of total RNA was combined with a control RNA of an in vitro-transcribed E. coli genomic DNA with a poly(A)+ tail. After the isolation of mRNA, three different control transcripts were added, and samples were labeled during reverse transcription with Cy3-Cy5-dCTP (Amersham Bioscience, Freiburg, Germany). The labeled samples were cleaned up using QIA Quick spin columns (QIAGEN) and hybridized in a Gene TAC hybridization station (Perkin-Elmer) according to the guidelines of the manufacturer of the arrays (Memorec).
Readout and data analysis.
Image capture and signal quantification of the hybridized arrays were done with the ScanArray 3000 (GSI Lumonics, Watertown, Mass.) and Ima Gene software version 4.1 (Bio-Discovery, Los Angeles, Calif.) as detailed elsewhere (10). The local signal of each spot was measured inside a 300-μm-diameter circle. The local background was determined within 40-μm-wide rings ∼40 μm distant from the signal and subtracted from the local signal intensity to calculate the net signal intensity and the ratio of Cy5 to Cy3. The ratios were normalized to the median of all ratios, considering only those spots with fluorescence intensities three times larger than that of the herring sperm DNA and spotting buffer negative controls. The values represent the means of four single spots and standard deviations.
Northern blot analysis.
RNA (10 μg) was denatured with glyoxal and separated as described previously (24). Hybridization was carried out overnight at 65°C using ExpressHyb solution (Clontech) and [α-32P]dCTP random-primed cDNA fragments. The blots were washed twice with 2× SSC (1× SSC is 0.15 M NaCl plus 0.015 M sodium citrate; pH 7)-0.1% sodium dodecyl sulfate and twice with 0.1× SSC-0.1% sodium dodecyl sulfate at 65°C and exposed at −80°C to Kodak BiomaxMS film with an intensifying screen. The blots were reprobed with an 18S rRNA fragment.
Statistical analysis.
An unpaired Student's t test was used to determine significant differences between groups.
RESULTS
Testosterone prevents self-healing of malaria.
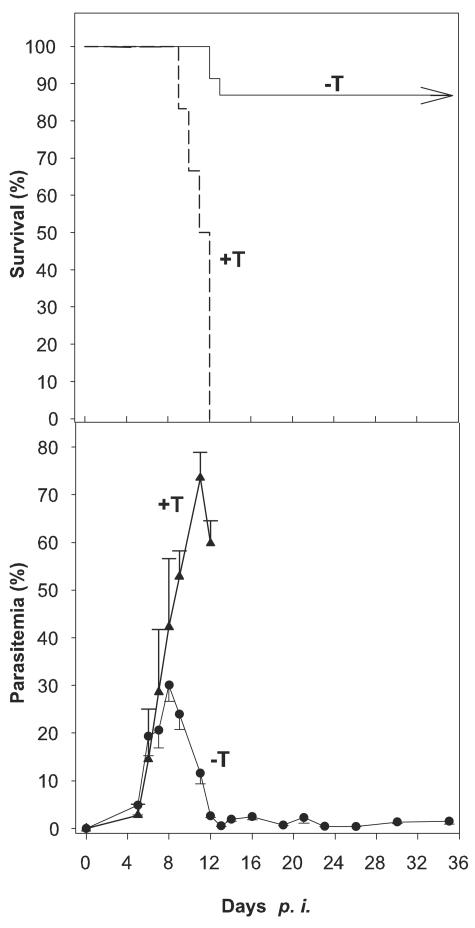
Blood-stage infections with P. chabaudi malaria took a self-healing course in 85% of female C57BL/6 mice (Fig. 1). Precrisis culminated in a maximal parasitemia of ∼30% on day 8 postinfection (p.i.), while the subsequent crisis was characterized by falling parasitemias dropping to <1% on days 13 and 14 p.i. (Fig. 1). However, pretreatment with testosterone caused all of the mice to succumb to infection with delayed and higher peak parasitemias.
FIG. 1.
Survival and parasitemia of female C57BL/6 mice. The mice were pretreated with testosterone (+T) (n = 6) or vehicle (−T) (n = 23) and challenged with 106 P. chabaudi-parasitized erythrocytes. All values are given as means ± half standard deviations.
Testosterone impairs malaria-induced hepatic but not splenic closing.
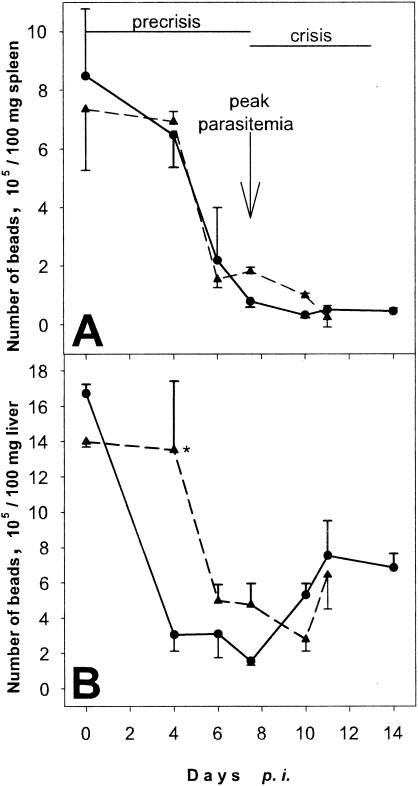
Polystyrol particles were injected to determine the effect of testosterone on the RES activities of the liver and spleen. The spleens of uninfected mice trapped ∼8 × 105 beads/100 mg (Fig. 2). On day 6 p.i., however, there was a dramatic drop in particle trapping. In fact, the spleen was almost closed at peak parasitemia on day 8 p.i. Remarkably, there was no reopening with still higher efficiency of particle trapping during crisis, as previously reported in Plasmodium chabaudi adami infections (2). The P. chabaudi-induced gating mechanism of the spleen was obviously not affected by testosterone (Fig. 2).
FIG. 2.
Particle uptake by spleen (A) and liver (B) during P. chabaudi infections. Testosterone-treated (triangles) and vehicle-treated (circles) mice were infected with 106 P. chabaudi-parasitized erythrocytes. All values represent means ± half standard deviations of at least six mice. *, P < 0.05 vs. vehicle-treated control.
The liver displayed twofold-higher efficiency of particle trapping than the spleen (Fig. 2). The specific uptake amounted to ∼1.7 × 106 beads/100 mg in uninfected mice but dropped dramatically during precrisis and was lowest at peak parasitemia, with 1.5 × 105 beads/100 mg. However, liver closing was much less effective than spleen closing, and the liver contained five times more beads than the spleen on day 8 p.i. During crisis, there was a significant reopening, but the liver did not reach its initial particle-trapping capacity again. Testosterone impaired particle trapping by the liver, which became evident as a delay in closing and reopening (Fig. 2). Furthermore, the maximal closing was not as effective as in mice treated only with vehicle. Despite these testosterone effects on particle trapping, we were unable to detect any significant testosterone effects on malaria-induced liver pathology (Table 1).
TABLE 1.
Liver histology of testosterone-treated and control C57BL/6 mice infected with P. chabaudi on days 0 and 8 p.i.
| Liver parametera | Valueb
|
|||
|---|---|---|---|---|
| Uninfected mice
|
Acute-phase malaria
|
|||
| − Testos- terone | + Testos- terone | − Testos- terone | + Testos- terone | |
| Histological activity indexc | 1-3 | 2-3 | 6-10 | 7-11 |
| Inflammatory infiltrates | − | + | ++ | ++ |
| Cytoplasmic vacuolization | − | + | + | + |
| Binucleated cells | − | ++ | ++ | +++ |
| Cell swelling | − | + | + | ++ |
| Apoptosis | − | − | + | ++ |
| Malaria pigment (hemozoin) | − | − | ++ | ++ |
| Hyperplasia of Kupffer cells | − | − | + | ++ |
Paraffin sections (6 μm thick) were stained with hematoxilin-eosin and evaluated.
−, no occurrence; +, rare occurrence; ++, regular occurrence; +++, frequent occurrence.
Modified according to the system of Ishak et al. (22). Score: 1 to 3, minimal; 4 to 8, mild; 9 to 12, moderate; 13 to 18, severe.
Testosterone suppresses malaria-responsive gene expression in the liver but not in the spleen.
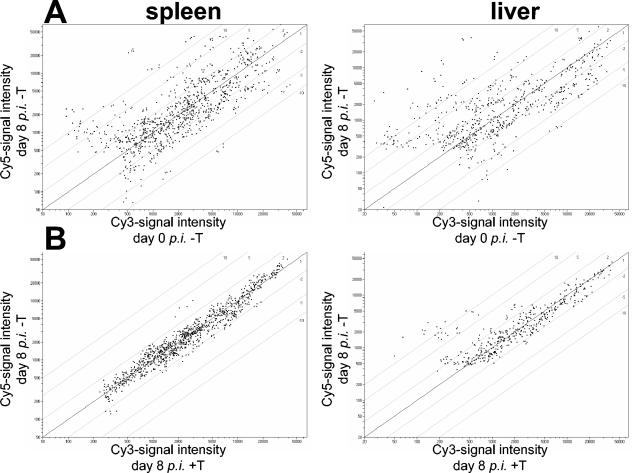
Using cDNA microarrays, gene expression of the spleen and the liver in infected mice on day 8 p.i. was compared with that of uninfected mice and with that of testosterone-treated infected mice on day 8 p.i.
In the spleen, blood-stage malaria caused quite a number of genes to be up- and downregulated, as shown in Fig. 3A. Genes with alterations in expression of at least threefold are listed in Table 2. Increased expression was observed for 23 genes, and decreased expression was observed for 9 genes. It is surprising, however, that testosterone does not essentially alter malaria-induced gene expression in the spleen (Fig. 3B). In the liver, 34 genes were upregulated and 15 were downregulated more than threefold by blood-stage malaria (Table 2). A >10-fold increase in gene expression was still detected for 15 genes, whereas only STA2 and PGHD were downregulated ∼10-fold.
FIG. 3.
Scatter plots of gene expression in spleen and liver. Mice were pretreated with testosterone or vehicle and infected with P. chabaudi. (A) For vehicle-treated mice (−T), gene expression levels on day 0 p.i. and maximal parasitemia on day 8 p.i were compared. (B) The influence of testosterone (+T) was analyzed at maximal parasitemia on day 8 p.i.
TABLE 2.
Genes regulated at least threefold by P. chabaudi infection or testosterone in spleen or liver
| Gene name | UNIPROTa | Spleen
|
Liver
|
||
|---|---|---|---|---|---|
| Day 8 p.i./day 0b (%) | Day 8 p.i. −T/ day 8 p.i. +Tc (%) | Day 8 p.i./day 0 (%) | Day 8 p.i. −T/ day 8 p.i. +T (%) | ||
| Cytokines, chemokines, growth factors, and their receptors | |||||
| Interleukin 10 (IL-10) | P18893 | 16.35/32 | 1.21/24 | ||
| Tumor necrosis factor alpha (TNF-α) | P06804 | 0.89/9 | 0.90/8 | 22,26/85 | |
| Gamma interferon (IFN-γ) | P01580 | 8.89/7 | 0.75/4 | ||
| Interleukin 1 receptor type II | P27931 | 5.26/15 | 1.22/4 | ||
| Cytokine receptor common β chain | P26955 | 1.38/5 | 0.95/4 | 3.50/6 | 1.42/11 |
| Lymphptoxin α | P09225 | 0.23/24 | 0.86/- | ||
| Lymphptoxin β | P41155 | 0.15/6 | 0.57/7 | ||
| C-C chemokine receptor 1 | P51675 | 2.20/6 | 0.79/5 | 10.88/82 | |
| Chemokine (C-C motif) ligand 2; MCP-1 | Q9QYD7 | 5.83/13 | 0.69/2 | 7.00/40 | |
| Chemokine (C-C motif) ligand 4; MIP-1β | P14097 | 8.75/14 | 0.89/5 | 6.05/32 | |
| Chemokine (C-C motif) ligand 5; RANTES | P30882 | 1.08/3 | 1.04/5 | 6.19/8 | 1.08/8 |
| Chemokine (C-C motif) ligand 6; MRP-1 | Q99M24 | 5.57/9 | 0.86/9 | 14.02/71 | 1.52/- |
| Chemokine (C-X-C motif) ligand 1; GRO1 | P12850 | 8.83/37 | 2.12/- | ||
| Chemokine (C-X-C motif) ligand 10; γ-IP10 | P17515 | 4.78/6 | 0.66/4 | 10.97/12 | 4.32/9 |
| Chemokine (C-X-C motif) ligand 9; MIG | P18340 | 11.80/10 | 1.04/13 | 30.62/24 | 0.77/10 |
| Growth differentiation factor 3; GDF3 | Q07104 | 4.38/8 | 1.73/7 | ||
| Bone morphogenetic protein 11; BMP11 | Q9QX55 | 0.14/9 | 0.66/- | ||
| Cysteine-rich angiogenic inducer 61; Cyr61 | P18406 | 0.41/7 | 0.51/9 | 4.49/8 | 8.99/16 |
| Insulin-like growth factor binding protein 1 | P47876 | 12.06/16 | 19.30/23 | ||
| Insulin-like growth factor 1 | P05018 | 1.04/5 | 1.09/5 | 0.25/6 | 0.85/4 |
| ECMd components and regulators; coagulation | |||||
| Tissue inhibitor of metalloproteinases 1 | P12032 | 3.02/4 | 0.80/11 | ||
| Matrix metalloproteinase-13 | P33435 | 20.96/19 | 1.60/5 | 16.68/15 | 2.57/7 |
| Syndecan 3 | Q64519 | 1.23/4 | 0.58/5 | 4.08/6 | 1.11/12 |
| Osteopontin | P10923 | 3.60/- | 0.70/7 | 0.63/5 | 0.82/13 |
| Plasminogen activator inhibitor; Serpine 1 | P22777 | 2.07/9 | 1.21/20 | 106.45/57 | 14.22/22 |
| Urokinase-type plasminogen activator receptor; CD87 | P35456 | 0.86/10 | 1.03/6 | 8.40/43 | |
| Coagulation factor F5 | O88783 | 0.39/3 | 0.25/6 | 1.12/18 | |
| Latent transforming growth factor-β-binding protein | Q8K4G1 | 0.09/8 | 0.70/5 | 0.18/37 | |
| GTPases | |||||
| IFNγ-inducible 47 kDa GTPase IF147, IRG-47 | Q61635 | 5.33/1 | 1.07/8 | 4.25/5 | 0.55/9 |
| IFNγ-induced isoprenylated 67-kDa GTPase; MGBP-2; GBP2 | Q9Z0E6 | 13.85/1 | 1.14/4 | 12.16/7 | 1.05/7 |
| IFNγ-induced GTPase IFII | Q60766 | 5.54/11 | 1.14/5 | 2.71/14 | 0.59/7 |
| IFNγ-induced GTPase IGTP | Q9DCE9 | 7.61/4 | 1.17/2 | 5.45/5 | 0.56/18 |
| IFNγ-induced GTPase IIGP | Q9Z1M3 | 7.89/21 | 0.93/9 | 1.79/8 | 0.50/7 |
| IFNγ-induced GTPase TGTP | Q60711 | 6.32/10 | 1.10/3 | 15.19/10 | 0.52/3 |
| Signal transduction proteins and transcription factors | |||||
| Protein kinase C-ɛ | P16054 | 0.40/6 | 1.04/14 | 0.26/- | |
| B lymphoid kinase | P16277 | 0.25/8 | 1.31/4 | ||
| Suppressor of cytokine signaling 1 | O35716 | 2.61/7 | 0.50/4 | 11.35/16 | 0.71/6 |
| Suppressor of cytokine signaling 2 | O35717 | 1.95/1 | 1.09/13 | 0.23/6 | |
| Suppressor of cytokine signaling 3 | P97803 | 2.18/4 | 0.64/4 | 5.51/12 | 1.45/10 |
| Dual-specificity protein phosphatase 1; MKP1 | P28563 | 2.14/2 | 3.28/11 | 2.75/5 | 6.41/10 |
| Dual-specificity protein phosphatase 2; PAC1 | Q05922 | 0.66/5 | 1.32/9 | 5.83/20 | 1.34/2 |
| NFIL3/E4BP4 transcription factor | O08750 | 3.30/16 | 1.14/10 | 1.86/9 | 2.27/12 |
| Activating transcription factor 3 | Q60765 | 4.02/12 | 0.74/6 | 18.97/25 | 7.05/19 |
| JunB oncogene; junB | P09450 | 0.48/3 | 0.48/3 | 3.38/4 | 3.10/7 |
| Fos-related antigen 2 | P47930 | 1.49/6 | 0.52/9 | 3.50/13 | 2.59/12 |
| Avian reticuloendotheliosis viral oncogene-related B (relB) | Q04863 | 0.33/10 | 0.70/6 | ||
| NFκB p49/p100 | Q9WTK5 | 0.32/9 | 0.65/12 | 1.79/18 | |
| Innate immunity; acute phase | |||||
| Complement C1q subcomponent γ | Q02105 | 2.04/5 | 1.18/7 | 3.97/11 | 1.50/5 |
| Complement factor B | P04186 | 3.19/6 | 0.76/4 | 0.89/6 | 0.79/3 |
| Serum amyloid A1/2 | P05366 | 0.79/15 | 64.03/17 | 0.89/3 | |
| P05367 | |||||
| Serum amyloid A3 | Q62201 | 42.22/4 | 1.56/8 | 80.12/11 | 0.72/7 |
| Liver metabolic enzymes | |||||
| Cytochrome p450 1A2 | P00186 | 0.20/4 | 0.89/9 | ||
| Cytochrome p450 2E1 | Q05421 | 0.25/5 | 0.82/4 | ||
| Microsomal GST; GST-3 | Q9CPU4 | 0.88/4 | 0.97/4 | 0.22/11 | |
| Alcohol dehydrogenase 1 | P00329 | 0.22/10 | 0.81/6 | ||
| Cytochrome p450 2C38 | P56656 | 0.12/33 | |||
| Hydroxysteroid sulfotransferase; Sth2; STA2 | P50236 | 0.10/8 | 27.88/70 | ||
| Miscellaneous | |||||
| Heat shock protein 1B; Hspa1b; HSP70 | P17879 | 1.96/14 | 0.70/4 | 11.18/9 | 1.30/14 |
| Prostaglandin-H2 d isomerase; PGHD | O09114 | 0.12/45 | 0.09/47 | ||
| Bone marrow stromal cell antigen 1; BST1; CD157 | Q64277 | 0.93/3 | 0.74/11 | 36.90/113 | |
| Apolipoprotein M; apoM | Q9Z1R3 | 0.29/2 | 0.79/5 | ||
| Transferrin | Q92111 | 0.25/12 | 1.09/11 | 0.88/5 | 1.03/4 |
| Superoxide dismutase 1 | P08228 | 1.23/3 | 1.61/8 | 0.30/11 | 0.88/9 |
| B-cell differentiation antigen CD72 | P21855 | 0.40/2 | 1.11/7 | 3.73/16 | |
| Sialophorin; CD43 | P15702 | 1.01/3 | 0.71/10 | 3.68/21 | |
| Mitochondrial superoxide dismutase 2 | Q8VEM5 | 3.05/7 | 1.13/5 | 0.93/3 | 0.92/15 |
| Growth arrest and DNA damage-inducible protein 45 | P48316 | 0.89/4 | 1.41/5 | 4.83/6 | 9.65 15 |
UNIPROT, protein database of the European Bioinformatics Institute.
Ratio of expression in mRNA of vehicle-treated mice on days, 0 and 8 p.i.
Ratio of expression in mRNA of infected mice on day 8 p.i. treated with vehicle (−T) or testosterone (+T).
ECM, extracellular matrix.
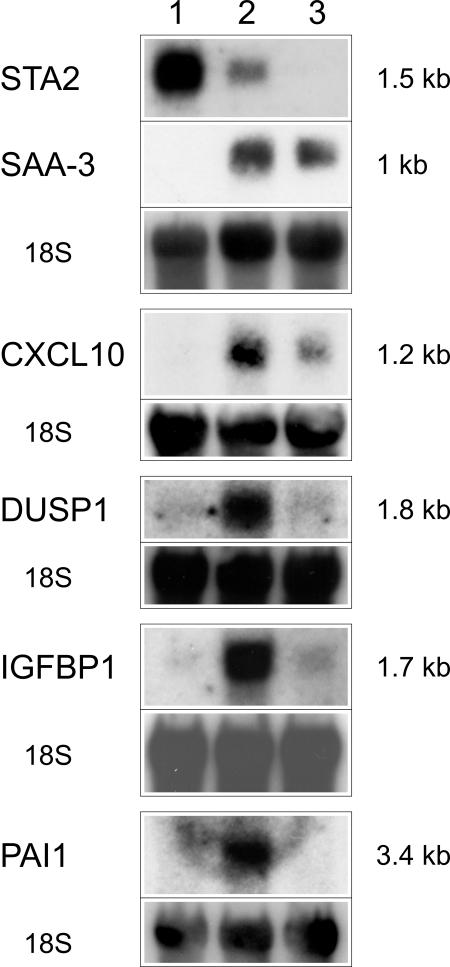
Most conspicuously, however, testosterone caused dramatic downregulation of the malaria-induced PAI1, Cyr61, IGFBP1, GADD45α, DUSP1, junB, and ATF3 genes. In addition, STA2 was further suppressed ∼28-fold after testosterone treatment. Testosterone-induced suppression of the STA2, CXCL10, DUSP1, IGFBP1, and PAI1 genes, as well as the testosterone nonresponsiveness of SAA3, was confirmed by Northern blotting (Fig. 4).
FIG. 4.
Northern blot analysis with RNAs from livers of female C57BL/6 mice. RNAs from vehicle-treated and uninfected mice (lane 1), RNAs from vehicle-treated mice at peak parasitemia (lane 2), and RNAs from testosterone-treated mice at peak parasitemia (lane 3) were hybridized to the indicated probes.
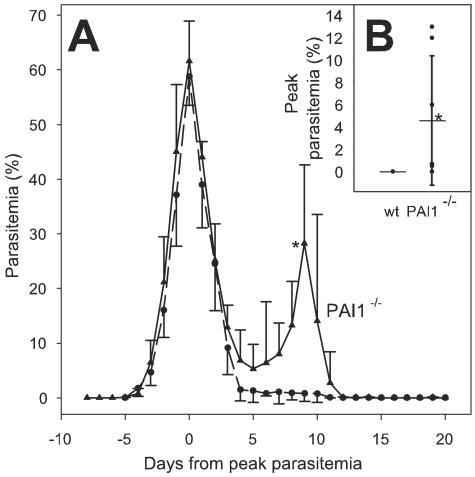
Decreased malaria resistance of PAI1-deficient mice.
In order to evaluate any relevance of testosterone-suppressed genes for the control of resistance to P. chabaudi, we analyzed the course of P. chabaudi infections in PAI1-deficient mice. One of the infected PAI1−/− mice died at peak parasitemia, whereas all infected control mice survived. Infections in these mice developed peak parasitemias of ∼60% between days 6 and 12 in PAI1−/− mice, while peak parasitemias were observed in control mice between days 7 and 9. In Fig. 5A, the course of infection has been normalized to the first parasitemia peak for better comparison. Surprisingly, ∼9 days after the first peak, all PAI1-deficient mice developed an unusually high second peak, with parasitemias of ∼30%. Even after homologous reinfection of immune PAI1−/− mice, obtained after curing primarily infected mice with chloroquine, parasites were detectable in peripheral blood in 70% of the PAI1−/− mice but in none of the control mice (Fig. 5B).
FIG. 5.
Increased susceptibility of PAI1-deficient mice to P. chabaudi blood-stage malaria. (A) PAI1−/− (triangles; n = 8) and control (circles; n = 8) mice were infected with 106 P. chabaudi-parasitized erythrocytes. All values are given as means ± half standard deviations. The time course was normalized to the day of the first peak parasitemia to compensate for the different time points of peak parasitemia due to different periods of time until parasites were detected in peripheral blood. (B) Immune mice were reinfected, and individual peak parasitemias and means (horizontal lines) ± standard deviations are shown. *, P < 0.05 vs. wild-type (wt) control.
DISCUSSION
This study is the first to provide evidence that testosterone impairs protective responses of the liver rather than of the spleen to P. chabaudi blood-stage malaria, as indicated by changes in particle trapping and gene expression. This is astonishing, since the spleen is accepted not only as the major effector site against blood-stage malaria but also as an organ with cells able to respond to testosterone by different signaling pathways mediated through either classical nuclear androgen receptors, as in B cells (5), or unconventional surface androgen receptors, as in T cells (6, 7, 49) and macrophages (9, 18), presumably G protein-coupled receptors.
Surprisingly, our data indicated that the liver is provided with a gating mechanism similar to that in the spleen that protects against malaria-induced damage to the spleen, though significant differences exist in gating between the spleen, with its extravascular beds in the red pulp, and the liver, with its completely intravascular circulation. The major difference was that testosterone impaired the malaria-induced closing process only in the liver. In consequence, testosterone caused the liver to be exposed longer to parasites and their toxic products, such as the malaria pigment hemozoin. Hemozoin is produced by Plasmodium parasites to detoxify the highly lytic ferriprotoporphyrin IX released during parasitic digestion of a host's hemoglobin (19). Hemozoin has been described as being avidly phagocytosed by cells such as neutrophils, monocytes, and macrophages both in vitro and in vivo (3, 42). Accordingly, we observed the hemozoin to be almost exclusively phagocytosed by Kupffer cells, the number of which even increases slightly at peak parasitemia (Table 2). Though this suggests a higher phagocytic activity of the Kupffer cell-based RES of the liver, just the opposite may occur. Indeed, it has been shown in vitro that hemozoin accumulation in macrophages diminishes and eventually paralyses their activity (3, 34, 37, 38, 41, 42). It appears rather likely that the testosterone-impaired closing of the liver is not able to efficiently restrain inundation with toxic parasite substances and inflammatory mediators, resulting in failure of the liver RES to act as an effector against P. chabaudi blood stages.
Moreover, our data demonstrate that testosterone-impaired closing coincides with suppression of malaria-responsive gene expression in the liver, but not in the spleen. It is clear that testosterone affected only a small fraction of the malaria-responsive genes in the liver, indicating that the testosterone-induced suppression is specific and is not due to a general dampening of transcription possibly caused by testosterone-induced general liver failure. In particular, testosterone impaired the malaria-induced upregulation of the seven Cyr61, IGFBP1, GADD45α, DUSP1, ATF3, junB, and PAI1 genes. All of these genes are stress responsive and are described as being involved in the control of specific aspects of the cell cycle and apoptosis. It is therefore not improbable that at least some of these stress-responsive genes might be involved in the control of host resistance to malaria. Indeed, we could show that at least the PAI1 gene plays a vital role in the control of blood-stage malaria.
The serpine PAI1 has been shown not only to be involved in regulation of fibrinolysis, cell adhesion, and cell migration (21) but also to exhibit angiogenic properties (16) and to inhibit the activation of the potent hepatocyte apoptogen and immunomodulatory Th2 cytokine latent transforming growth factor β by plasminogen activators (20). The antiparasite effector function of PAI1 became evident in PAI1-deficient mice, which displayed a partial loss of the ability to control the course of infection. In contrast to wild-type controls, PAI1−/− mice exhibited high malaria recrudescence ∼9 days after the first peak parasitemia, and immune PAI1-deficient mice developed a patent infection upon homologous rechallenge. A protective function of PAI1 induction in blood-stage malaria is consistent with previous data showing an involvement of the plasminogen activator system in the antimalaria response, using mice deficient for urokinase-type plasminogen activator (uPA) or its receptor (uPAR) (30, 31). Both mutant mouse strains display enhanced resistance to cerebral malaria caused by Plasmodium berghei ANKA. This phenotype is associated with amelioration of thrombocytopenia and thrombocyte sequestration in brain capillaries (30). Furthermore, fewer apoptotic cells can be found in the spleen and lymph nodes of both strains during P. berghei infection (31). It is well known that PAI1 interacts with the uPA/uPAR complex and regulates its activity by inhibiting the enzymatic activity of uPA and enhancing internalization of the complex (21), thus decreasing local remodeling of the extracellular matrix. In addition, active, but not uPA-bound, PAI1 is able to directly bind to fibronectin and to inhibit integrin-dependent cell attachment to vibronectin. Obviously, the plasminogen activator system is strongly involved in the regulation of cell migration, a hallmark of the progression of inflammatory responses as induced by blood-stage malaria.
The STA2 gene was the gene in the liver with the most prominent downregulation (28-fold) by testosterone. Since STA2 was already suppressed by P. chabaudi infection (10-fold), the STA2 mRNA levels in testosterone-treated mice were >250-fold lower at peak parasitemia than in uninfected mice. Testosterone-dependent downregulation of STA2 in rodent hepatocytes is known from several previous studies (13, 14, 25, 40) showing, e.g., fourfold-lower levels of STA2 mRNA in male than in female mice (14). STA2 encodes a cytosolic hydroxysteroid-specific sulfotransferase, which is involved in limiting the amount of active androgens in cells (12) and also in detoxification of cholestatic hydroxylated bile acids, such as lithocholic acid (23, 36). In humans, low levels of hydroxysteroid sulfotransferase activity were shown to correlate with chronic liver diseases, such as primary biliary cirrhosis, primary sclerosing cholangitis, chronic active hepatitis, and alcoholic cirrhosis (17). Thus, STA2 may be important for detoxification of bile acids originally derived from cholesterol, which is released in excess from malaria-destroyed erythrocytes during the crisis of infections. Indeed, the severely swollen gall bladder induced by P. chabaudi blood-stage malaria indicates an extreme perturbation of bile acid metabolism during crisis, the period when most testosterone-treated mice succumb to P. chabaudi infection.
Collectively, our data indicate that the liver plays a protective role against blood stages of malaria and that the liver is more critical than the spleen for mediating suppressive effects of testosterone on resistance to malaria. In particular, the testosterone-induced changes in the activity of the RES and the dramatic suppression of the malaria-protective PAI1 gene and the STA2 gene suggest that dysregulation of liver effector functions toward malarial blood stages critically contributes to the testosterone-induced lethal outcome of blood-stage malaria.
Editor: W. A. Petri, Jr.
REFERENCES
- 1.Aikawa, M., M. Suzuki, and Y. Gutierrez. 1980. Pathology of malaria, p. 47-102. In J. P. Kreier (ed.), Malaria, vol. 2. Academic Press, New York, N.Y.
- 2.Alves, H. J., W. Weidanz, and L. Weiss. 1996. The spleen in murine Plasmodium chabaudi adami malaria: stromal cells, T lymphocytes, and hematopoiesis. Am. J. Trop. Med. Hyg. 55:370-378. [DOI] [PubMed] [Google Scholar]
- 3.Amodu, O. K., A. A. Adeyemo, P. E. Olumese, and R. A. Gbadegesin. 1998. Intraleucocytic malaria pigment and clinical severity of malaria in children. Trans. R. Soc. Trop. Med. Hyg. 92:54-56. [DOI] [PubMed] [Google Scholar]
- 4.Balmer, P., J. Alexander, and R. S. Phillips. 2000. Protective immunity to erythrocytic Plasmodium chabaudi AS infection involves IFN-γ-mediated responses and a cellular infiltrate to the liver. Parasitology 121:473-482. [DOI] [PubMed] [Google Scholar]
- 5.Benten, W. P. M., C. Stephan, and F. Wunderlich. 2002. B cells express intracellular but not surface receptors for testosterone and estradiol. Steroids 67:647-654. [DOI] [PubMed] [Google Scholar]
- 6.Benten, W. P. M., M. Lieberherr, C. E. Sekeris, and F. Wunderlich. 1997. Testosterone induces Ca2+ influx via non-genomic surface receptors in activated T cells. FEBS Lett. 407:211-214. [DOI] [PubMed] [Google Scholar]
- 7.Benten, W. P. M., M. Lieberherr, G. Giese, C. Wrehlke, O. Stamm, C. E. Sekeris, H. Mossmann, and F. Wunderlich. 1999. Functional testosterone receptors in plasma membranes of T cells. FASEB J. 13:123-133. [DOI] [PubMed] [Google Scholar]
- 8.Benten, W. P. M., U. Bettenhaeuser, F. Wunderlich, E. van Vliet, and H. Mossmann. 1991. Testosterone-induced abrogation of self-healing of Plasmodium chabaudi malaria in B10 mice: mediation by spleen cells. Infect. Immun. 59:4486-4490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benten, W. P. M., M. Lieberherr, O. Stamm, C. Wrehlke, Z. Guo, and F. Wunderlich. 1999. Testosterone signaling through internalizable surface receptors in androgen receptor-free macrophages. Mol. Biol. Cell. 10:3113-3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bosio, A., C. Knorr, U. Janssen, S. Gebel, H. J. Haussmann, and T. Müller. 2002. Kinetics of gene expression profiling in Swiss 3T3 cells exposed to aqueous extracts of cigarette smoke. Carcinogenesis 23:741-748. [DOI] [PubMed] [Google Scholar]
- 11.Carmeliet, P., L. Kieckens, L. Schoonjans, B. Ream, A. van Nuffelen, G. Prendergast, M. Cole, R. Bronson, D. Collen, and R. C. Mulligan. 1993. Plasminogen activator inhibitor-1 gene-deficient mice. I. Generation by homologous recombination and characterization. J. Clin. Investig. 92:2746-2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chan, J., C. S. Song, R. J. Matusik, B. Chatterjee, and A. K. Roy. 1998. Inhibition of androgen action by dehydroepiandrosterone sulfotransferase transfected in PC-3 prostate cancer cells. Chem. Biol. Interact. 109:267-278. [DOI] [PubMed] [Google Scholar]
- 13.Chatterjee, B., D. Majumdar, O. Ozbilen, C. V. Murty, and A. K. Roy. 1987. Molecular cloning and characterization of cDNA for androgen-repressible rat liver protein, SMP-2. J. Biol. Chem. 262:822-825. [PubMed] [Google Scholar]
- 14.Chatterjee, B., C. S. Song, M. H. Jung, S. Chen, C. A. Walter, D. C. Herbert, F. J. Weaker, M. A. Mancini, and A. K. Roy. 1996. Targeted overexpression of androgen receptor with a liver-specific promoter in transgenic mice. Proc. Natl. Acad. Sci. USA 93:728-733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chotivanich, K., R. Udomsangpetch, R. McGready, S. Proux, P. Newton, S. Pukrittayakamee, S. Looareesuwan, and N. J. White. 2002. Central role of the spleen in malaria parasite clearance. J. Infect. Dis. 185:1538-1541. [DOI] [PubMed] [Google Scholar]
- 16.Devy, L., S. Blacher, C. Grignet-Debrus, K. Bajou, V. Masson, R. D. Gerard, A. Gils, G. Carmeliet, P. Carmeliet, P. J. Declerck, A. Noel, and J. M. Foidart. 2002. The pro- or antiangiogenic effect of plasminogen activator inhibitor 1 is dose dependent. FASEB J. 16:147-154. [DOI] [PubMed] [Google Scholar]
- 17.Elekima, O. T., C. O. Mills, A. Ahmad, G. R. Skinner, D. B. Ramsden, J. Bown, T. W. Young, and E. Elias. 2000. Reduced hepatic content of dehydroepiandrosterone sulphotransferase in chronic liver diseases. Liver 20:45-50. [DOI] [PubMed] [Google Scholar]
- 18.Guo, Z., W. P. M. Benten, J. Krücken, and F. Wunderlich. 2002. Nongenomic testosterone calcium signaling: genotropic actions in androgen receptor-free macrophages. J. Biol. Chem. 277:29600-29607. [DOI] [PubMed] [Google Scholar]
- 19.Hempelmann, E., and T. J. Egan. 2002. Pigment biocrystallization in Plasmodium falciparum. Trends Parasitol. 18:11. [DOI] [PubMed] [Google Scholar]
- 20.Hertig, A., J. Berrou, Y. Allory, L. Breton, F. Commo, M. A. Costa De Beauregard, P. Carmeliet, and E. Rondeau. 2003. Type 1 plasminogen activator inhibitor deficiency aggravates the course of experimental glomerulonephritis through overactivation of transforming growth factor beta. FASEB J. 17:1904-1906. [DOI] [PubMed] [Google Scholar]
- 21.Irigoyen, J. P., P. Munoz-Canoves, L. Montero, M. Koziczak, and Y. Nagamine. 1999. The plasminogen activator system: biology and regulation. Cell. Mol. Life Sci. 56:104-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ishak, K., A. Baptista, L. Bianchi, F. Callea, J. De Groot, F. Gudat, H. Denk, V. Desmet, G. Korb, R. N. M. MacSween, M. J. Phillips, B. G. Portmann, H. Poulsen, P. J. Scheuer, M. Schmid, and H. Thaler. 1995. Histological grading und staging of chronic hepatitis. J. Hepatol. 22:696-699. [DOI] [PubMed] [Google Scholar]
- 23.Kitada, H., M. Miyata, T. Nakamura, A. Tozawa, W. Honma, M. Shimada, K. Nagata, C. J. Sinal, G. L. Guo, F. J. Gonzalez, and Y. Yamazoe. 2003. Protective role of hydroxysteroid sulfotransferase in lithocholic acid-induced liver toxicity. J. Biol. Chem. 278:17838-17844. [DOI] [PubMed] [Google Scholar]
- 24.Krücken, J., H.-P. Schmitt-Wrede, U. Markmann-Mulisch, and F. Wunderlich. 1997. Novel gene expressed in spleen cells mediating acquired testosterone-resistant immunity to Plasmodium chabaudi malaria. Biochem. Biophys. Res. Commun. 230:167-170. [DOI] [PubMed] [Google Scholar]
- 25.Labrie, Y., J. Couet, J. Simard, and F. Labrie. 1994. Multihormonal regulation of dehydroepiandrosterone sulfotransferase messenger ribonucleic acid levels in adult rat liver. Endocrinology 134:1693-1699. [DOI] [PubMed] [Google Scholar]
- 26.Lee, H. J., and C. Chang. 2003. Recent advances in androgen receptor action. Cell. Mol. Life Sci. 60:1613-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mannoor, M. K., R. C. Halder, S. R. Morshed, A. Ariyasinghe, H. Y. Bakir, H. Kawamura, H. Watanabe, H. Sekikawa, and T. Abo. 2000. Essential role of extrathymic T cells in protection against malaria. J. Immunol. 169:301-306. [DOI] [PubMed] [Google Scholar]
- 28.Müller, H. E. 1992. The more effective immune system of women against infectious agents. Wien Med. Wochenschr. 142:389-395. [PubMed] [Google Scholar]
- 29.Nagasue, N., and H. Kohno. 1992. Hepatocellular carcinoma and sex hormones. HPB Surg. 6:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Piguet, P. F., C. da Laperrousaz, C. Vesin, F. Tacchini-Cottier, G. Senaldi, and G. E. Grau. 2000. Delayed mortality and attenuated thrombocytopenia associated with severe malaria in urokinase- and urokinase receptor-deficient mice. Infect. Immun. 68:3822-3829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Piguet, P. F., C. da Laperrousaz, C. Vesin, and Y. Donati. 2001. Incidence of apoptosis in the lymphoid organs of normal or malaria infected mice is decreased in CD18 and urokinase-receptor (UPAR, CD87) deficient mice. Dev. Immunol. 8:183-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pinkerton, W., and M. Webber. 1964. A method of injecting small laboratory animals by opthalmic plexus route. Proc. Soc. Exp. Biol. Med. 116:959-961. [DOI] [PubMed] [Google Scholar]
- 33.Poole, T. M., and N. R. Drinkwater. 1996. Strain dependent effects of sex hormones on hepatocarcinogenesis in mice. Carcinogenesis 17:191-196. [DOI] [PubMed] [Google Scholar]
- 34.Prada, J., J. Malinowski, S. Müller, U. Bienzle, and P. G. Kremsner. 1996. Effects of Plasmodium vinckei hemozoin on the production of oxygen radicals and nitrogen oxides in murine macrophages. Am. J. Trop. Med. Hyg. 54:620-624. [DOI] [PubMed] [Google Scholar]
- 35.Roberts, C. W., W. Walker, and J. Alexander. 2001. Sex-associated hormones and immunity to protozoan parasites. Clin. Microbiol. Rev. 14:476-488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saini, S. P., J. Sonoda, L. Xu, D. Toma, H. Uppal, Y. Mu, S. Ren, D. D. Moore, R. M. Evans, and W. Xie. 2004. A novel constitutive androstane receptor-mediated and CYP3A-independent pathway of bile acid detoxification. Mol. Pharmacol. 65:292-300. [DOI] [PubMed] [Google Scholar]
- 37.Schwarzer, E., and P. Arese. 1996. Phagocytosis of malarial pigment hemozoin inhibits NADPH-oxidase activity in human monocyte-derived macrophages. Biochim. Biophys. Acta 1316:169-175. [DOI] [PubMed] [Google Scholar]
- 38.Scorza, T., S. Magez, L. Brys, and P. de Baetselier. 1999. Hemozoin is a key factor in the induction of malaria-associated immunosuppression. Parasite Immunol. 21:545-554. [DOI] [PubMed] [Google Scholar]
- 39.Seli, E., and A. Arici. 2002. Sex steroids and the immune system. Immunol. Allergy Clin. N. Am. 22:407-408. [Google Scholar]
- 40.Song, C. S., M. H. Jung, S. C. Kim, T. Hassan, A. K. Roy, and B. Chatterjee. 1998. Tissue-specific and androgen-repressible regulation of the rat dehydroepiandrosterone sulfotransferase gene promoter. J. Biol. Chem. 273:21856-21866. [DOI] [PubMed] [Google Scholar]
- 41.Taramelli, D., S. Recalcati, N. Basilico, P. Olliaro, and G. Cairo. 2000. Macrophage preconditioning with synthetic malaria pigment reduces cytokine production via heme iron-dependent oxidative stress. Lab. Investig. 80:1781-1788. [DOI] [PubMed] [Google Scholar]
- 42.Turrini, F., E. Schwarzer, and P. Arese. 1993. The involvement of hemozoin toxicity in depression of cellular immunity. Parasitol. Today 9:297-300. [DOI] [PubMed] [Google Scholar]
- 43.Weiss, L. 1991. The spleen in malaria: the role of barrier cells. Immunol. Lett. 25:165-172. [DOI] [PubMed] [Google Scholar]
- 44.Weiss, L., U. Geduldig, and W. Weidanz. 1986. Mechanisms of splenic control of murine malaria: reticular cell activation and the development of a blood-spleen barrier. Am. J. Anat. 176:251-285. [DOI] [PubMed] [Google Scholar]
- 45.Weiss, L. 1989. Mechanisms of splenic control of murine malaria: cellular reactions of the spleen in lethal (strain 17XL) Plasmodium yoelii malaria in BALB/c mice, and the consequences of pre-infective splenectomy. Am. J. Trop. Med. Hyg. 41:144-160. [DOI] [PubMed] [Google Scholar]
- 46.Wunderlich, F., H. Mossmann, M. Helwig, and G. Schillinger. 1988. Resistance to Plasmodium chabaudi in B10 mice: influence of the H-2 complex and testosterone. Infect. Immun. 6:2400-2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wunderlich, F., P. Marinovski, W. P. M. Benten, H. P. Schmitt-Wrede, and H. Mossmann. 1991. Testosterone and other gonadal factor(s) restrict the efficacy of genes controlling resistance to Plasmodium chabaudi malaria. Parasite Immunol. 13:357-367. [DOI] [PubMed] [Google Scholar]
- 48.Wunderlich, F., H. Stübig, and E. Königk. 1982. Development of Plasmodium chabaudi in mouse red blood cells: structural properties of the host and parasite membranes. J. Protozool. 29:60-66. [DOI] [PubMed] [Google Scholar]
- 49.Wunderlich, F., W. P. M. Benten, M. Lieberherr, Z. Guo, O. Stamm, C. Wrehlke, C. E. Sekeris, and H. Mossmann. 2002. Testosterone signaling in T cells and macrophages. Steroids 67:535-538. [DOI] [PubMed] [Google Scholar]
- 50.Yadava, A., S. Kumar, J. A. Dvorak, G. Milon, and L. H. Miller. 1996. Trafficking of Plasmodium chabaudi adami-infected erythrocytes within the mouse spleen. Proc. Natl. Acad. Sci. USA 93:4595-4599. [DOI] [PMC free article] [PubMed] [Google Scholar]