Abstract
Toll-like receptor 4 (TLR4) has been identified as a receptor for lipopolysaccharide. However, the precise role of TLR4 in regulating gene expression in response to an infection caused by gram-negative bacteria has not been fully elucidated. The role of TLR4 signaling in coordinating gene expression was assessed by gene expression profiling in lung tissue in a mouse model of experimental pneumonia with a low-dose infection of Klebsiella pneumoniae. We analyzed four mouse strains: C57BL/6 mice, which are resistant to bacterial dissemination; 129/SvJ mice, which are susceptible; C3H/HeJ mice, which are susceptible and have defective TLR4 signaling; and their respective control strain, C3H/HeN (intermediate resistance). At 4 h after infection, C57BL/6 and C3H/HeN mice demonstrated the greatest number of genes, with 67 shared induced genes which were TLR4 dependent and highly associated with the resistance phenotype. These genes included cytokine and chemokine genes required for neutrophil activation or recruitment, growth factor receptors, MyD88 (a critical adaptor protein for TLR signaling), and adhesion molecules. TLR4 signaling accounted for over 74% of the gene expression in the C3H background. These data suggest that early TLR4 signaling controls the vast majority of gene expression in the lung in response to an infection caused by gram-negative bacteria and that this subsequent gene expression determines survival of the host.
It is now known that recognition of lipopolysaccharide (LPS) by the host is mediated by Toll-like receptor 4 (TLR4) and is responsible for the early innate immune response to this agent (3, 23). However, the precise role that TLR4 plays in coordinating gene expression in response to an intact gram-negative infection where LPS is only one of many virulence factors remains unclear. It has been previously reported in experimental animal models of TLR deficiency that TLR4-deficient mice are more susceptible to Salmonella sp. infection (10) and that TLR2-deficient mice are more susceptible to Staphylococcus aureus infection (29). In both models, reduced survival was associated with uncontrolled bacterial growth.
The genomic response of purified cell populations such as dendritic cells (15) and macrophages (21) in response to purified bacterial ligands like LPS or whole organisms have revealed distinct genetic programs. Huang and colleagues showed that dendritic cells respond to Escherichia coli, Candida albicans, and influenza virus infection with both distinct and shared gene expression profiles. E. coli infection resulted in the greatest number of gene expression changes, with 118 of 685 genes being unique to E. coli and 166 being shared between influenza, C. albicans, and E. coli. Nau and colleagues showed similar findings of shared transcriptional programs in human macrophages but also demonstrated that LPS resulted in a gene expression profile similar to that of live E. coli, suggesting that LPS controls the dominant response in macrophages to this organism (21, 22). Furthermore, that group showed that infection of human peripheral blood mononuclear cells with Mycobacterium tuberculosis poorly induced interleukin-12 (IL-12) p40 and IL-15 compared to E. coli or S. aureus, which may in part explain immune evasion by this organism (21).
Despite these data, it remains unclear on a genomic scale what the contribution of TLR4 signaling is in the lung in response to infection by gram-negative bacteria. To address this question, we performed gene expression profiling using whole lungs of TLR4-deficient C3H/HeJ mice and C3H/HeN mice with intact TLR4 as well as resistant (C57BL/6) and susceptible (129/SvJ) strains of mice in an experimental model of Klebsiella pneumoniae infection. We chose this organism because it is capable of eliciting pneumonia with very small inocula (35, 36), and the growth curves of this bacteria are similar in these mouse strains from time 0 to 16 h, such that changes in gene expression would not be due to changes in organism burden over this time course (36). We chose C3H mice since the C3H/HeJ mutation was initially characterized in these mice by using C3H/HeN as a control which is nearly isogenic, with the exception of the TLR4 mutation (28). TLR4−/− mice have been made on the 129/SvJ background with subsequent backcrossing to C57BL/6; however, significant 129/SvJ alleles still exist in this strain (14). Moreover, since 129/SvJ mice show susceptibility to infections caused by gram-negative bacteria independent of TLR4, as outlined below, data from TLR4−/− mice may be confounded by these 129 alleles.
By using susceptible TLR4 mutant C3H/HeJ mice (23), it was shown that only 42 genes out of 14,700 genes were significantly induced by twofold or more at 4 h compared to a total of 184 genes in resistant C57BL/6 mice or 130 genes in resistant C3H/HeN mice which were induced. These data demonstrate that TLR4 is critical for gene induction and accounts for over 81% of acute gene expression changes in C57BL/6 mice and over 74% of acute gene expression changes in C3H/HeN mice. Moreover, we identified 67 genes that were shared between resistant C57BL/6 and C3H/HeN mice which were clearly TLR dependent. Although TLR4 signaling was critical in early gene expression, hierarchal clustering showed that TLR4 mutant mice “catch up” by 16 h, as evidenced by the fact that gene expression profiles in C3H/HeJ mice at 16 h cluster with C57BL/6 and C3H/HeN mice with intact TLR at 4 h. This result may be due to other TLR pathways such as TLR2 or TLR9 which recognize lipopeptides (25) and CpG DNA (12), respectively.
MATERIALS AND METHODS
Mice.
C3H/HeJ and 129/SvJ male mice (6 to 8 weeks old) were obtained from Jackson Laboratory (Bar Harbor, Maine), while C3H/HeN and C57BL/6 male mice (6 to 8 weeks old) were obtained from the National Cancer Institute (Frederick, Md.). All mice were maintained according to protocol approved by the Institutional Animal Care and Use Committee. Mice were provided with sterile food, water, and filtered air and were housed with 12-h light-dark cycles in the Louisiana State University Health Sciences Center Animal Care Facility.
Bacteria.
K. pneumoniae strain ATCC 43816 serotype 2 (American Type Culture Collection, Rockville, Md.) bacteria were grown in 100 ml of tryptic soy broth (Difco, Sparks, Md.) for 18 h at 37°C. After 18 h, 1 ml of the culture was added to a fresh 100 ml of tryptic soy broth and grown for 2 h at 37°C. The culture was centrifuged at 2,700 × g for 15 min, and the supernatant was discarded. The bacterial pellet was washed twice with phosphate-buffered saline (PBS) and serially diluted to the desired concentration. The concentration of bacteria was measured by calculating the number of CFU on tryptic soy agar plates (Remel, Lenexa, Kans.).
Experimental animal procedures.
All mice were anesthetized with 50 μl of PBS-diluted ketamine-xylazine (50 to 150 mg/kg). The mice were intratracheally inoculated with 104 CFU of K. pneumoniae/ml in a 50-μl volume. At 0, 4, and 16 h postinoculation, the mice were euthanized, the heart and both lungs were excised, and the right ventricle was flushed with PBS. The right lung was isolated, homogenized in 1 ml of Trizol (Invitrogen, Carlsbad, Calif.), and placed at −80°C.
Preparation of labeled cRNA.
RNA was extracted from tissues in Trizol (Invitrogen) according to manufacturer's protocol. The SuperScript Choice system (GIBCO/BRL) in combination with a T7-(T)24 DNA primer (5′-GGCCAGTGAATTGTAATACGACTCACTATAGGGAGGCGG-d(T)24-3′; Integrated DNA Technologies) was used to synthesize cDNA from total RNA. The first-strand DNA synthesis reaction mixture contained 5 μg of total RNA, 100 pmol of T7-(T)24 primer, 500 μM each deoxynucleoside triphosphate, and 200 U of reverse transcriptase (Superscript II Reverse; Gibco/BRL). The reaction mixture was incubated for 1 h at 42°C. Second-strand cDNA synthesis was carried out at 16°C for 2 h in a total volume of 170 μl using 10 U of E. coli DNA ligase, 40 U of E. coli DNA polymerase I, and 2 U of E. coli RNase H in the presence of 200 μM each deoxynucleoside triphosphate. Following the second-strand cDNA synthesis, 10 U of T4 DNA polymerase was added, and the samples were incubated for 5 min at 16°C. The reaction was stopped by the addition of 0.5 M EDTA, and samples were phenol-chloroform extracted by using Phase-Lock gels (Eppendorf 5 Prime, Boulder, Colo.). Samples were then precipitated overnight at −20°C with 0.5 volumes of 7.5 M ammonium acetate and 2.5 volumes of 100% ethanol. With this double-stranded DNA serving as a template, a biotinylated antisense cRNA was synthesized by using the Enzo Bioarray High-Yield RNA transcript labeling kit (Affymetrix). Reactions were run according to the manufacturer's instructions. The reaction mixture was incubated at 37°C for approximately 5 h. Samples were then precipitated overnight at −20°C and subsequently resuspended in 20 μl of diethyl pyrocarbonate-treated water. Forty micrograms of biotinylated antisense cRNA was fragmented by heating the sample to 94°C for 35 min in a volume of 40 μl of fragmentation buffer containing 40 mM Tris-acetate (pH 8.1), 100 mM potassium acetate, and 30 mM magnesium acetate.
Microarray analysis of lung RNA.
To determine which gene expression profiles correlated with host resistance to K. pneumoniae and which of those genes were regulated by TLR4 in the lung, microarray analysis of lung RNA at time points early in the infection (4 and 16 h) was performed. Mice were euthanized at 0, 4, and 16 h (n = 4 to 9 mice per time point) postinoculation, the right lung was harvested and homogenized, and the total RNA was isolated. Replicate samples were individually prepared and hybridized onto separate microarrays as outlined below. Subsequent enzymatic reactions were carried out with 5 μg of total RNA to generate labeled and fragmented cRNA which were then hybridized to Affymetrix MGU74AV2 microarrays.
Microarray processing.
U74Av2 chips (Affymetrix) were prehybridized with 200 μl of 1× hybridization buffer (100 mM MES, 1 M Na+, 20 mM EDTA, 0.01% Tween 20) for 10 min at 45°C in an Affymetrix Genechip Hybridization Oven 640 at 60 rpm. Hybridization was done in a final volume of 300 μl containing 15 μg of fragmented biotinylated cRNA, 50 pmol of control oligonucleotide B2 (Affymetrix), eukaryotic hybridization controls (Affymetrix), 0.1 mg of herring sperm DNA/ml, and 0.5 mg of acetylated bovine serum albumin/ml in 1× hybridization buffer. The samples were heated to 95°C for 5 min and 45°C for an additional 5 min and then briefly spun down. Two hundred microliters of the hybridization cocktail was added to the standard arrays, and hybridizations were carried out for 16 h at 45°C with mixing on a rotisserie at 60 rpm. After hybridization, the solutions were removed, and the arrays were washed by using a fluidics station (Affymetrix). Hybridized arrays were stained for 10 min at 25°C with streptavidin-R phycoerythrin (10 μg/ml; Molecular Probes), followed by staining with biotinylated goat anti-streptavidin antibody (3 μg/ml; Sigma Chemical) for 10 min at 25°C. Genechips were then stained once again with streptavidin-R phycoerythrin for 10 min at 25°C. Probe arrays were scanned with a confocal laser scanner (Agilent) at a wavelength of 570 nm. Pixel intensities were then measured, and expression signals were analyzed by using a commercial software package (Microarray Suite [MAS], version 5.0; Affymetrix). LIMS version 3.0 (Affymetrix), Data Mining Tools (DMT) version 3.0 (Affymetrix), and Genespring version 6.0 (Silicon Genetics) were used to perform data analysis.
Microarray data analysis.
Microarray data were generated by using Affymetrix (http://www.affymetrix.com) protocols. Absolute expression transcript levels were normalized for each chip by globally scaling all probe sets to a target signal intensity of 500. Three statistical algorithms (detection, change call, and signal log ratio) were then used to identify differential gene expression in experimental and control samples. The detection metric (presence, absence, or marginal) for a particular gene was determined by using default parameters of the MAS software. Transcripts that were absent under both control and experimental conditions were eliminated from further consideration. Statistical significance of signals between the control and experimental conditions (P ≤ 0.05) for individual transcripts was determined by using the t test and Mann-Whitney test. Batch analyses in which pairwise comparisons between individual experimental and control chips were made in order to generate a change call and a signal log ratio value for each transcript were performed with MAS. We defined a positive change call as one in which greater than 50% of the change calls for any one transcript were increased or marginally increased for upregulated genes and decreased or marginally decreased for downregulated genes. Finally, the median value of the signal log ratios from each comparison file was calculated. Signal log ratio values were converted from log2 and expressed as fold changes. In addition, only those genes that met the above-mentioned criteria and that had a median signal log ratio of greater than or equal to 1 for upregulated transcripts and less than or equal to 1 for downregulated transcripts were kept in the final list of genes.
For hierarchical clustering, genes were included in the final lists if they passed the following filter requirements when the 4- or 16-h time point was compared to the 0-h controls within the same strain: elimination of Absent to Absent genes (genes denoted to be absent in control and experimental conditions); statistical significance by Student's t test and Mann-Whitney test; change calls of “increased” for upregulated genes and “decreased” for downregulated genes; and a fold change of >3 or <−3. Parametric (t test) and nonparametric (Mann-Whitney test) statistical tests were performed on these data to obtain those genes that were potentially normally distributed across groups and those that were not. Self-organizing maps were generated by using DMT with a subset of genes that were found to be up- and downregulated by the above-described methods in C57BL/6 mice infected with K. pneumoniae at 4 h compared to the 0-h time point. The same subset of genes was used for hierarchical clustering using Genespring version 6.0 on all strains of mice at 0, 4, and 16 h following inoculation.
Alveolar macrophage isolation.
Male C57BL/6, C3H/HeN, C3H/HeJ, or 129/SvJ mice were anesthetized with intraperitoneal pentobarbital and sacrificed by exsanguination. Thereafter, the lungs were lavaged through an intratracheal catheter with prewarmed (37°C) calcium and magnesium-free PBS supplemented with 0.6 mM EDTA. A total of 10 ml was used in each mouse in 0.5-ml increments with a 30-s dwell time. The lavage fluids were pooled and centrifuged at 300 × g for 10 min, and the cells were collected. To ensure that each cell preparation was enriched for macrophages, 10,000 cells were cytospun onto slides and stained with hematoxylin and eosin. Cell preparations were generally >98% enriched for alveolar macrophages.
Cytokine assays.
Alveolar macrophages were isolated from C57BL/6, C3H/HeN, C3H/HeJ, and 129/SvJ mice as described above. Macrophages were adjusted to 5 × 104 in RPMI 1640 medium with 10% fetal bovine serum and 1% PenStrep (Gibco) and added to a volume of 100 μl in individual wells of a 96-well plate (in duplicate). The macrophages were allowed to attach for 1 h at 37°C, and nonadherent cells were washed away. Thereafter, heat-killed K. pneumoniae (70°C for 30 min) was added to experimental wells at 104 CFU/well in a volume of 100 μl of RPMI 1640 medium with 10% fetal bovine serum and 1% PenStrep. Controls included macrophages cultured in the presence of LPS (10 μg/ml; List Biological Laboratories, Campbell, Calif.) or medium alone (control for spontaneous production). The macrophage cultures were allowed to incubate for 6 h at 37°C, 5% CO2, and thereafter, supernatants were harvested for quantification of macrophage inflammatory protein 2 (MIP-2), IL-6, tumor necrosis factor alpha (TNF-α), KC-GRO, and granulocyte colony-stimulating factor (G-CSF) by using the Bio-Plex protein array system (Bio-Rad, Hercules, Calif.) according to the manufacturer's instructions. The concentrations of each cytokine and chemokine were determined by using Bio-Plex Manager version 3.0 software (Bio-Rad). Data are expressed as picograms per milliliter.
Statistical analysis of lung CFU and cytokine protein and fold change data. Data were analyzed by using StatView statistical software (Brainpower Inc., Calabasas, Calif.). Comparisons between groups were analyzed by analysis of variance with a Scheffe follow-up test. Survival was analyzed by log-rank testing. Significance was accepted at a P value of <0.05.
RESULTS
Reduced survival of mice deficient in TLR4 signaling.
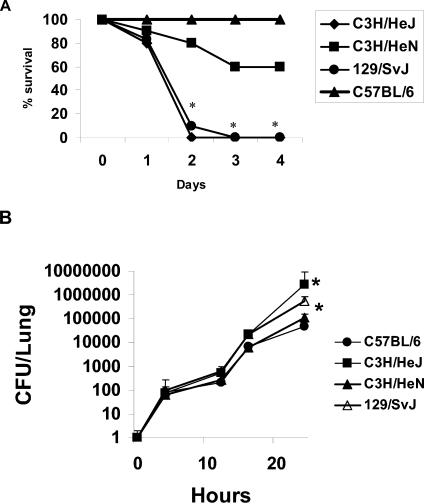
Four strains of mice were chosen to investigate the role of TLR4 signaling in host lung defense in a K. pneumoniae model: C57BL/6, 129/SvJ, C3H/HeN, and C3H/HeJ. The C3H/HeJ strain has a mutant TLR4 allele which results in defective TLR4 signaling, rendering it hyporesponsive to LPS (23), while the C3H/HeN mice have a normal TLR4 allele. Lung inoculums were based on previous pilot studies, whereby the 50% lethal dose at 12 days was determined to be 3 × 104 CFU in C57BL/6 mice (data not shown). Four strains of mice were inoculated intratracheally with 104 CFU of K. pneumoniae (ATCC 43816, serotype 2), and their survival was recorded in 24-h intervals for 96 h. Wild-type control mice, C57BL/6 and C3H/HeN mice, had a 100 and 60% survival rate, respectively, after 96 h, while the remaining susceptible strains had a 100% mortality rate within the same time period. Of these strains, the C3H/HeJ and 129/SvJ mice shared a phenotype of drastically reduced survival, with death resulting 48 to 72 h following inoculation (Fig. 1A). Bacterial lung burdens of K. pneumoniae were determined postinoculation in a separate group of animals at 4, 12, 16, and 24 h (n = 4 to 6 mice per time point) by quantitative culture of lung homogenates (Fig. 1B). As previously described for C57BL/6 and IL-17 receptor knockout mice (36), all mice had similar lung bacterial burdens within the first 16 h, with C3H/HeJ and 129/SvJ mice developing statistically significantly higher lung bacterial burdens at 24 h (Fig. 1B). Moreover, bacterial dissemination was assessed by quantitative cultures of spleen homogenates at the same time points. However, by 24 h, five out of six 129/SvJ, four out of six C3H/HeJ, and two out of six C3H/HeN mice had spleen cultures that were positive for K. pneumoniae, whereas zero out of six C57BL/6 mice were bacteremic at this time point. By 48 h, three out of six C3H/HeN and only one out of six C57BL/6 mice had positive spleen cultures. 129/SvJ and C3H/HeJ mice were moribund at this time point and 100% bacteremic. Thus, as previously observed in this model, mortality was associated with bacterial dissemination from the lungs (36).
FIG. 1.
Panel A: reduced survival of mice deficient in TLR4 signaling. 129/SvJ, C3H/HeJ, C3H/HeN, and C57BL/6N (n = 10 mice per group) were challenged with intratracheal inoculation of 104 CFU of K. pneumoniae, and the survival rate was recorded every 24 h. An * denotes significant difference (P < 0.05; log-rank test) compared to C57BL/6 mice. Panel B: lung bacterial burden in each mouse strain over time (n = 4 to 6 mice per time point). An * indicates a P value of <0.05 compared to C57BL/6 mice.
Microarray analysis of lung homogenates.
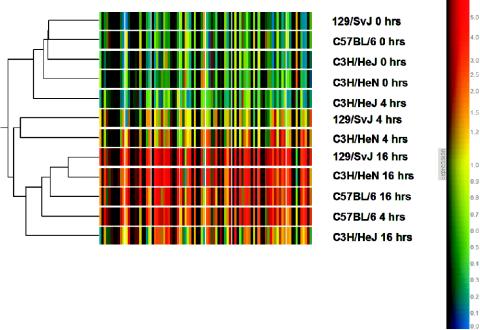
Hierarchal cluster analysis revealed distinct patterns among the four murine strains at 4 h that correlate closely with the survival outcome as seen in Fig. 1. Specifically, the mouse strains with the greatest susceptibility to bacterial dissemination, 129/SvJ and C3H/HeJ, clustered near each other at 4 h. Moreover, as visually seen in the cluster (Fig. 2) the C3H/HeJ mice failed to upregulate a number of genes by 4 h that were observed in C3H/HeN or C57BL/6 mice. The defect in gene expression in C3H/HeJ mice resulted in this strain at 4 h actually clustering with time zero control mice (Fig. 2). The hyporesponsiveness in gene expression observed in C3H/HeJ mice suggests a critical role for TLR4 signaling and subsequent TLR4 gene expression in mediating host resistance to K. pneumoniae infection. The fact that the 129/SvJ strain clustered near C3H/HeJ mice at 4 h also suggests that there may be defects in downstream genes regulated by TLR4 in this mouse strain. This distinction for the 129/SvJ and C3H/HeJ mice was lost at 16 h, as the 129/SvJ mice clustered together with both C3H/HeN and C57BL/6 mice at 16 h. This is despite the fact that there are significant differences in rates of bacteremia at 24 h across these strains. These data suggest that the gene expression profile at 4 h is critical to controlling bacteremia and survival. Lastly, of note is that C3H/HeJ mice at 16 h cluster with C3H/HeN and C57BL/6 mice 4 h into the infection, further suggesting that a defect in LPS recognition delays the gene expression of analogous genes expressed in mice capable of recognizing LPS in response to infection. In 129/SvJ mice, these genes are eventually expressed by 16 h but at a time when it may be too late to affect their survival. Taken together, our results indicate that the expression of critical genes downstream of the TLR4 pathway at 4 h is important in clearing gram-negative infections.
FIG. 2.
Cluster analysis showing relative RNA message levels of genes found differentially expressed in C57BL/6N mice in response to K. pneumoniae intratracheal challenge at 0, 4, and 16 h postchallenge. Gene lists were generated by using algorithms from Affymetrix MAS version 5.0 and mined by using Affymetrix DMT version 3.0, and lists were imported into Genespring version 6.0 in order to generate a cluster. Only those genes that were significantly upregulated and that had a greater than threefold change in gene expression in all strains were used to generate a hierarchical cluster using a standard correlation. A total of 90 genes met these requirements (see Table S1 in the supplemental material [http://www.medschool.lsuhsc.edu/genetics/genechip_record.asp]). All strains at the zero-hour time point clustered together. Overall gene expression is similar for 129/SvJ and C3H/HeJ mice at 4 h in that they share a common node. Interestingly, the 16-h time point for C3H/HeJ shows a gene expression pattern similar to that of C57BL/6N at just 4 h, indicating that key TLR4-dependent immunomodulators produced within 4 h of K. pneumoniae challenge contribute to the overall survival phenotype.
Role of TLR4 signaling and pulmonary gene expression.
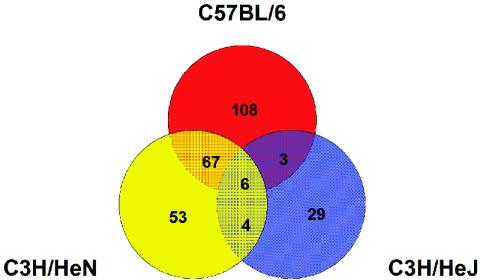
Next, these lists of differentially expressed genes were incorporated into a Venn diagram by using Genespring version 6.0 (Fig. 3) except that genes were now included if they had a fold change of ≥2 or ≤−2 in order to increase sensitivity. Specifically, genes that were found to be upregulated at 4 h following K. pneumoniae infection for strains C57BL/6, C3H/HeN, and C3H/HeJ were compared to each other to observe both shared and unique genes between lists. Key gene lists can be found in Tables 1 to 3, along with information regarding fold changes for each strain at 4 h versus its own 0-h time point. The fold changes for specific genes from certain murine strains were not included in the final lists of differentially expressed transcripts if these genes did not meet the above-mentioned filtering requirements, and the exact reasons for their exclusion are denoted in the tables. The mouse strain most resistant to bacteremia, C57BL/6, showed the greatest number of induced genes (184) meeting at least a twofold change, followed by C3H/HeN and129/SvJ, with 130 and 78 genes, respectively. C3H/HeJ showed the least amount of alteration in gene expression, with only 42 genes changing from 0 to 4 h. Moreover, the two strains showing the greatest level of host resistance shared the greatest number of genes, 67 (Fig. 3). In addition to these 67 common genes, C57BL/6 mice have an additional set of 108 unique genes (Table 4) and C3H/HeN mice had 53 unique genes (Table 5) that were significantly upregulated by 4 h. Because this set of 108 and 53 unique genes may represent TLR4-dependent genes but may be strain specific to C3H or C57, we focused on the 67 shared genes that were not expressed in C3H/HeJ mice as genes that were clearly TLR4 dependent in nature. This set of genes constituted approximately 29% of the genes uniquely upregulated by both control strains, C57BL/6 and C3H/HeN (Table 1). The products of these genes can be categorized by functional ontology, with cytokines/chemokines and receptors constituting the majority of genes found in this group. As expected, several known TLR4-related genes reside in this group of shared genes, including TNF-α, MIP-2 (Cxcl2), IL-1β, IL-6, CD14, and MyD88, further suggesting that the expression of these genes is critical for early infection clearance in the lungs and the ultimate survival of the host. Moreover, this analysis revealed genes that may be critical for host defense but that were heretofore not known to be directly regulated by TLR4, such as G-CSF, a molecule critical for regulating neutrophil responses to bacterial infection (8), and I-TRAF (24), a molecule involved in TNFR II signaling.
FIG. 3.
Venn diagram displaying genes upregulated at 4 h postchallenge that are both common and unique to three strains of mice: C57BL/6N, C3H/HeN, and C3H/HeJ (LPS hyporesponsive). Data were analyzed by using Affymetrix software MAS version 5.0 and DMT version 3.0. Genes that were included had to be significantly upregulated at 4 h versus the zero-hour time point and had to have a fold change between these two conditions of two or higher. Lists were imported into Genespring software version 6.0 (Silicon Genetics) for graphic illustration. The list of 29 genes unique to C3H/HeJ mice are TLR4 independent in nature, whereas the list of 67 genes shared between C57BL/6N and C3H/HeN mice are dependent and should correlate with overall resistance patterns in mice.
TABLE 1.
Mean TLR4-dependent gene fold changes categorized by function
| Affymetrix probe ID | Gene symbol | Genbank accession no. | Change (fold) at 4 vs 0 h
|
Results in C3H/HeJ mice at 4 vs 0 ha | Description | ||
|---|---|---|---|---|---|---|---|
| C57BL/6 | 129/SvJ | C3H/HeN | |||||
| Cytokine/chemokine | |||||||
| 101160_at | Cxcl2 | X53798 | 51.27 | 41.9 | 13.18 | A | Chemokine (C-X-C motif) ligand 2/MIP-2 |
| 102218_at | IL-6 | X54542 | 26.91 | 4.89 | 25.11 | A | IL-6 |
| 102424_at | Ccl3 | J04491 | 8.51 | 3.05 | 3.05 | A | Chemokine (C-C motif) ligand 3/MIP-1α |
| 102629_at | Tnf | D84196 | 9.45 | 5.54 | 3.34 | A | TNF |
| 102736_at | Ccl2 | M19681 | 32.90 | 6.73 | 6.23 | A | Chemokine (C-C motif) ligand 2/MCP-1 |
| 103486_at | IL1b | M15131 | 21.56 | 6.68 | 4.82 | A | Interleukin 1β |
| 104388_at | Ccl9 | U49513 | 4.99 | 1.42 | 2.25 | A | Chemokine (C-C motif) ligand 9 |
| 94755_at | IL1a | M14639 | 9.45 | 5.10 | 4.82 | A | IL-1α |
| 95349_g_at | Cxc11 | J04596 | 61.39 | 25.99 | 25.63 | A | Chemokine (C-X-C motif)/KC-GRO |
| 98772_at | Cxc15 | U27267 | 28.05 | 3.46 | 12.64 | A | Chemokine (C-X-C motif) ligand 5 |
| 94142_at | G-CSF | M13926 | 2.83 | 2.13 | 3.97 | A | Granulocyte colony-stimulating factor |
| 102914_s_at | A1b | U23778 | 3.76 | 1.93 | 2.60 | A | Hematopoietic-specific early response A1-b |
| Receptors | |||||||
| 102658_at | IL-12 | X59769 | 12.38 | 3.39 | 8.63 | A | IL-1 receptor, type II |
| 931198_at | Csf3r | M58288 | 4.41 | 1.58 | 3.20 | A | Colony-stimulating factor 3 receptor (granulocyte) |
| 93430_at | Cmkor1 | AF000236 | 4.06 | 1.67 | 3.78 | A | Chemokine orphan receptor 1 |
| 93871_at | IL-1m | L32838 | 8.06 | 3.18 | 2.89 | A | IL-1 receptor antagonist |
| 102255_at | Osmr | AB015978 | 3.03 | 1.33 | 2.08 | Chg | Oncostatin receptor |
| 102663_at | Plaur | X62700 | 4.03 | 2.19 | 2.77 | NS | Urokinase plasminogen activator receptor |
| 101410_at | mCPE-R | AB000713 | 4.06 | 1.88 | 5.35 | A | CPE receptor |
| 98088_at | CD14 | X13333 | 7.84 | 2.82 | 4.17 | Fld<2 | LPS receptor |
| 99413_at | CCR1 | U29678 | 6.96 | 3.05 | 2.63 | *A | Chemokine (C-C) receptor 1 |
| Apoptosis | |||||||
| 101979_at | Gadd45g | AF055638 | 3.34 | 2.17 | 2.20 | A | Growth arrest and DNA damage-inducible 45 gamma |
| 99392_at | Tnfaip3 | U19463 | 17.75 | 9.45 | 3.76 | A | TNF-α-induced protein 3 |
| Signal/transduction | |||||||
| 102430_at | Myd88 | X51397 | 2.10 | 1.16 | 2.11 | A | Myeloid differentiation primary response gene 88 |
| 96747_at | Arhu | AW121294 | 2.48 | 1.56 | 3.12 | A | ras homolog gene family, member U |
| 98423_at | Gjb2 | M81445 | 2.14 | 2.41 | 4.89 | A | Gap junction membrane channel protein beta 2 |
| 92232_at | SOCS-3 | U88328 | 8.28 | 3.94 | 4.50 | A | Suppressor of cytokine signaling 3 |
| 92534_at | GEM | U10551 | 2.23 | 1.56 | 4.41 | A | GTP binding protein |
| Adhesion | |||||||
| 102805_at | Ceacam1 | M77196 | 2.89 | 1.11 | 3.53 | A | CEA-related cell adhesion molecule 1 |
| 103005_s_at | CD44 | X66084 | 3.07 | 1.48 | 2.08 | A | CD44 antigen |
| 96752_at | Icam1 | M90551 | 2.28 | 1.47 | 2.51 | Fld<2 | Intercellular adhesion molecule |
| Enzymes | |||||||
| 102905_at | Casp4 | Y13089 | 2.57 | 1.05 | 2.25 | A | Caspase 4, apoptosis-related cysteine protease |
| 103341_at | Ctps | U49350 | 2.89 | 1.40 | 2.01 | A | Cytidine 5′-triphosphate synthase |
| 104509_at | Ch25h | AF059213 | 9.25 | 2.19 | 2.75 | A | Cholesterol 25-hydroxylase |
| 104671_at | Ampd3 | D88994 | 3.05 | 1.67 | 2.22 | A | AMP deaminase 3 |
| 99985_at | TxNR | AB027565 | 3.70 | 1.92 | 3.56 | Chg | Thioredoxin reductase 1 |
| 98473_at | Arg2 | AF032466 | 4.20 | 2.39 | 3.89 | A | Arginase type II |
| 94297_at | FK506 binding protein 5 | U16959 | 6.02 | 2.57 | 2.81 | A | FK506 binding protein 5 |
| 103024_at | Adam8 | X13335 | 3.18 | 4.41 | 8.75 | A | A disintegrin and metalloprotease domain 8 |
| Transcriptional factors | |||||||
| 102955_at | NFIL3/E4BP4 | U83148 | 3.03 | 1.89 | 2.55 | A | Nuclear factor, IL-3 regulated |
| 104712_at | C-MYC | L00039 | 6.32 | 2.58 | 5.58 | A | Myelocytomatosis oncogene |
| Other | |||||||
| 102780_at | Tx01 | Z31362 | 3.81 | 3.03 | 3.11 | A | |
| 103887_at | MRP14 | M83219 | 5.86 | 6.36 | 5.03 | NS | Migration inhibitory factor-related protein 14 |
| 92315_at | Slfn4 | AF099977 | 4.20 | 1.13 | 2.17 | A | Schlafen4 |
| 93861_f_at | Endogenous murine leukemia virus modified polytropic provirus | M17327 | 3.05 | 1.16 | 2.33 | A | Endogenous murine leukemia virus modified polytropic provirus |
| 92471_i_at | Slfn2 | AF099973 | 2.36 | 1.95 | 2.30 | A | Schlafen2 |
| 103448_at | MRP8 | M83218 | 5.86 | 6.50 | 4.56 | NS | Intracellular Ca2+ binding protein |
| 93573_at | MT1 | V00835 | 7.89 | 5.70 | 6.23 | Fld<2 | Metallothionein I |
| 99915_at | SDGF | L41352 | 2.46 | 2.33 | 2.53 | A | Amphiregulin |
| 103328_at | I-TRAF | U59864 | 2.39 | 1.62 | 2.33 | A | TRAF-interacting activator |
| 93104_at | BTG1 | Z16410 | 2.07 | 1.48 | 2.38 | Fld<2 | B-cell-transclocation gene 1 protein |
| 98067_at | P21 | U09507 | 2.19 | 2.10 | 2.66 | A | Cyclin-dependent kinase inhibitor 1A |
| 97689_at | Coagulation factor III | M26071 | 3.36 | 3.39 | 2.35 | Chg | Coagulation factor III |
Fold changes were not shown for those genes that had detection calls of absent (A) in the 4-h treated group; that had an inappropriate change call (Chg), such that there was not a call of increased or marginally increased in greater than half of the comparisons made; that had a fold change less than 1 (Fld<2); or that were not determined to be significant (NS) by parametric and nonparametric tests with a P cutoff value of ≤0.05.
TABLE 3.
Mean fold changes of upregulated genes common to all strains
| Affymetrix probe ID | Gene symbol | Genbank accession no. | Change (fold) at 4 vs 0 h
|
Results in C3H/HeJ mice at 4 vs 0 h | Description | ||
|---|---|---|---|---|---|---|---|
| C57BL/6 | 129/SvJ | C3H/HeN | |||||
| Enzymes | |||||||
| 102049_at | pdk | AJ001418 | 1.80 | 1.5 | 1.64 | 4.21 | Pyruvate dehydrogenase kinase-like protein |
| 104647_at | griPGHS | M88242 | 1.69 | 0.89 | 1.17 | 3.39 | Glucocortoid-regulated inflammatory prostaglandin G/H synthase |
| 99649_at | GCLC | U85414 | 2.26 | 1.32 | 2.08 | 3.17 | Glutamate cysteine ligase (gammylcysteine synthetase), catalytic |
| Other | |||||||
| 101561_at | MT2 | K02236 | 3.27 | 2.65 | 2.82 | 2.36 | Metallothionein 2 |
| 100325_at | gp49 | M65027 | 3.24 | 1.42 | 2.49 | 1.6 | Glycoprotein 49 |
TABLE 4.
Genes (108) that are upregulated 4 h following K. pneumoniae infection and are unique to C57BL/6 mice
| Affymetrix probe ID | Gene symbol | GenBank accession no. | Mean change (fold) in C57BL/6 mice at 4 vs 0 h | Results in C3H/HeN mice at 4 vs 0 ha | Description |
|---|---|---|---|---|---|
| 102712_at | Saa3 | X03505 | 47.8 | A | Serum amyloid A3 |
| 94769_at | Mmp8 | U96696 | 29.4 | A | Matrix metalloproteinase 8 |
| 92948_at | Csf2 | X03020 | 19.3 | A | Colony-stimulating factor 2 (granulocyte macrophage) |
| 93858_at | Cxcl10 | M33266 | 17.1 | A | Chemokine (C-X-C motif) ligand 10 |
| 160564_at | Lcn2 | X81627 | 11.8 | NS | Lipocalin 2 |
| 95951_at | Clecsf8 | AF061272 | 11.2 | A | C-type lectin |
| 96515_at | Il4i | U70430 | 10.9 | A | IL-4 induced 1 |
| 95303_at | EST | AA144469 | 10.9 | Chg | IMAGE-597616 |
| 103465_f_at | Saa2 | U60438 | 9.3 | A | Serum amyloid A2 |
| 98774_at | Irg1 | L38281 | 9.25 | A | Immunoresponsive gene 1 |
| 96153_at | Ngp | L37297 | 8.8 | A | Neutrophilic granule protein |
| 94688_at | Mad | X83106 | 8.2 | A | Max dimerization protein |
| 97106_at | Map3k8 | D13759 | 8.2 | A | Mitogen-activated protein kinase kinase kinase 8 |
| 97783_at | Ccl17 | AJ242587 | 8.1 | A | Chemokine (C-C motif) ligand 17 |
| 161689_f_at | Il1r2 | AV223216 | 7.6 | NS | IL-1 receptor, type II |
| 162206_f_at | Socs3 | AV374868 | 7.3 | NS | Suppressor of cytokine signaling 3 |
| 104692_at | Selp | M72332 | 7.2 | A | Selectin, platelet |
| 92217_s_at | gp49b | V05265 | 7.2 | NS | Glycoprotein 49B |
| 99333_at | Sele | M80778 | 5.9 | A | Selectin, endothelial cell |
| 102816_at | Serpina 3m | X69832 | 5.9 | A | Serine protease inhibitor, clade A, member 3M |
| 94761_at | Ccl7 | X70058 | 5.0 | A | Chemokine (C-C motif) ligand 7 |
| 95808_g_at | GCSFR | V05894 | 4.9 | A | Colony-stimulating factor, granulocyte receptor pseudogene |
| 101912_at | EST | AI01967 | 4.6 | Chg | IMAGE-1364952 |
| 101800_at | Fprrs2 | AF071180 | 4.6 | NS | N-formylpeptide receptor-like 2 gene |
| 160489_at | Tnfaip2 | L24118 | 4.4 | NS | TNF-α-induced protein 2 |
| 103839_at | SPHK1a | AF068748 | 4.1 | A | Spingosine kinase |
| 160608_at | Rab20 | AI854462 | 3.8 | A | RAB20, member RAS oncogene family |
| 92276_at | Map3k6 | AB021861 | 3.5 | A | Mitogen-activated protein kinase kinase kinase 6 |
| 102114_f_at | Angpt14 | AI326963 | 3.5 | A | Angiopoietin-like 4 |
| 97197_r_at | EST | C78850 | 3.5 | NS | Unknown |
| 96704_at | Sfn | AF058798 | 3.4 | A | Stratifin |
| 101820_at | Ly-6G1 | X70920 | 3.4 | A | Neurotoxin homologue, exons 1-3 |
| 102798_at | Adm | U77630 | 3.4 | Chg | Adrenomedullin |
| 102239_at | Bcl3 | M90397 | 3.3 | A | B-cell leukemia/lymphoma 3 |
| 102921_s_at | Tnfrsf6 | M83649 | 3.3 | Chg | TNF receptor superfamily, member 6 |
| 94147_at | Serpine1 | M33960 | 3.3 | Chg | Serine (or cysteine) proteinase inhibitor, clade E, member 1 |
| 93869_s_at | Ald | U23781 | 3.3 | Fld<2 | Hematopoietic-specific early response A1-d gene |
| 160894_at | Cebpd | X61800 | 3.2 | NS | CCAAT/enhancer binding protein (C/EBP), delta |
| 102707_f_at | Serpina 3C | X61597 | 3.2 | A | Serine (or cysteine) proteinase inhibitor, clade A, member 3C |
| 104333_at | G7e | U69488 | 3.2 | NS | Viral envelope-like |
| 98299_s_at | Slfn3 | AF09997 | 3.2 | A | Schlafen 3 |
| 104374_at | Spi2/eb4 | M64086 | 3.1 | Chg | Spi2 proteinase inhibitor |
| 102337_s_at | FCRII | M31312 | 3.1 | A | Mouse beta Fc receptor type II |
| 94137_at | I18rb | L13239 | 3.0 | A | IL-8 receptor, beta |
| 102021_at | Il4ra | M27960 | 3.0 | Fld<2 | IL-4 receptor, alpha |
| 92472_f_at | Slfn2 | AF099973 | 2.9 | NS | Schlafen 2 |
| 102860_at | Spi2/eb1 | M64085 | 2.9 | A | Spi2 prot |
| 93037_i_at | Anxa1 | M69260 | 2.9 | Chg | Annexin A1 |
| 94747_at | Csf2rb1 | M34397 | 2.9 | A | IL-3 receptor, beta chain 1 |
| 93411_at | EST | AI52789 | 2.8 | Chg | IMAGE-1478197 |
| 95784_at | Pira | U96682 | 2.8 | A | Paired immunoglobulin like receptor A1 |
| 97949_at | Fgl2 | M16238 | 2.7 | Fld<2 | Fibrinogen-like protein 2 |
| 97203_at | Mlp | X61399 | 2.7 | NS | MARCKS-like protein |
| 96119_s_at | Angpt14 | AA797604 | 2.7 | NS | Angiopoietin-like 4 |
| 102313_at | Gch | L09737 | 2.6 | NS | GTP cyclohydrolase 1 |
| 92925_at | Cebpb | M61007 | 2.6 | NS | CCAAT/enhancer binding protein (C/EBP), beta |
| 93058_at | Elf-1A | AF026481 | 2.6 | NS | Eukaryotic translation initiation factor 1A |
| 93860_i_at | M17327 | 2.6 | NS | Mouse endogenous murine leukemia virus modified polytropic provirus | |
| 160353_i_at | Mapkapk2 | X76850 | 2.5 | NS | Map kinase-activated protein kinase 2 |
| 96042_at | Sod2 | L35528 | 2.5 | NS | Superoxide dismutase 2, mitochondrial |
| 99957_at | Mmp9 | X72795 | 2.5 | A | Matrix metalloproteinase 9 |
| 160645_at | Birc2 | U88908 | 2.5 | NS | Baculoviral IAP repeat-containing 2 |
| AFFX-MurFAS_at | Tnfrsf6 | M83649 | 2.5 | NS | TNF receptor superfamily, member 6 |
| 102362_i_at | Junb | U20735 | 2.5 | NS | Jun-B oncogene |
| 104406_at | Ptges | AI060798 | 2.4 | A | Prostaglandin E synthase |
| 160646_at | Gsr | AI851983 | 2.4 | NS | Glutathione reductase I |
| 94351_r_at | Nqo1 | U12961 | 2.4 | A | NAD(P)H dehydrogenase, quinine 1 |
| 97525_at | Gyk | U48403 | 2.4 | NS | Glycerol kinase |
| 97950_at | Xdh | X75129 | 2.4 | NS | Xanthine dehydrogenase |
| 102264_at | Slfn1 | AF099972 | 2.4 | A | Schlafen 1 |
| 94556_at | Snx10 | A1746846 | 2.4 | NS | Sorting nexin 10 |
| 95785_s_at | Rab7 | Y13361 | 2.4 | NS | RAB7, member RAS oncogene family |
| 102957_at | Lcp2 | U20159 | 2.4 | NS | Lymphocyte cytosolic protein 2 |
| 95706_at | Lgals3 | X16834 | 2.4 | NS | Lectin galactose binding soluble 3 |
| 101464_at | Timp1 | V00755 | 2.4 | NS | Immunoresponsive gene 1 |
| 93328_at | Hdc | X57437 | 2.4 | NS | Histidine decarboxylase |
| 160583_at | Xlkd1 | AA880988 | 2.3 | NS | Extracellular link domain-containing 1 |
| 99384_at | Pim1 | M13945 | 2.3 | A | Proviral integration site 1 |
| 102806_g_at | Ceacam1 | M77196 | 2.3 | NS | CEA-related cell adhesion molecule 1 |
| 160975_at | EST | AI504338 | 2.3 | NS | IMAGE-963414 |
| 100328_s_at | Akr1b8 | U96684 | 2.3 | A | Ado-keto reductase family 1, member B8 |
| 92251_f_at | EST | AA960657 | 2.3 | A | IMAGE-2076183 |
| 103091_at | Relb | M83380 | 2.2 | A | Avian reticuloendotheliosis viral (v-rel) oncogene related B |
| 93202_at | Nt5e | L12059 | 2.2 | NS | 5′ nucleotidase, ecto |
| 101554_at | Nfkbia | U57524 | 2.2 | Fld<2 | Nuclear factor of kappa light chain gene enhancer in B cells inhibitor, alpha |
| 96562_at | Slc11a1 | L13732 | 2.2 | A | Solute carrier family 11 member 1 |
| 99461_at | Hcls1 | X84797 | 2.2 | A | Lyn substrate 1 |
| 100884_at | U04204 | 2.2 | Chg | Fibroblast growth factor regulated protein | |
| 101908_s_at | Bgp2 | AF101164 | 2.2 | A | Biliary glycoprotein 2 long isoform |
| 162198_f_at | EST | AV373027 | 2.2 | NS | Unknown |
| 94085_at | M34603 | 2.2 | NS | Proteoglycan secretory granule | |
| 160359_at | EST | AI746846 | 2.2 | NS | Unknown |
| 96295_at | Psat1 | AW122030 | 2.1 | NS | Phosphoserine aminotransferase 1 |
| 102310_at | Cc122 | AF052505 | 2.1 | A | Chemokine (C-C motif) ligand 22 |
| 99387_at | Fpr1 | L22181 | 2.1 | NS | Formyl peptide receptor 1 |
| 161132_at | Sce1 | AA727482 | 2.1 | NS | Screllin |
| 99160_s_at | EST | AW227647 | 2.1 | NS | IMAGE-2654099 |
| 93624_at | EST | AI225296 | 2.1 | NS | Unknown |
| 100397_at | Tryrobp | AF024637 | 2.1 | NS | TYRO protein tyrosine kinase binding protein |
| 160108_at | Nupr1 | AI852641 | 2.1 | NS | Nuclear protein 1 |
| 160387_at | EST | AI853900 | 2.1 | NS | Unknown |
| 94821_at | Xbp1 | AW123880 | 2.1 | Fld<2 | X-box binding protein 1 |
| 101923_at | Pla2g7 | U34277 | 2 | A | Phospholipase A2, group VII (platelet-activating factor acetylhydrolase, plasma) |
| 101996_at | Ptpn2 | M80739 | 2.0 | Chg | Protein tyrosine phosphatase, nonreceptor type 2 |
| 94224_s_at | Ifi205 | M74123 | 2.0 | Chg | Interferon-activated gene 205 |
| 92877_at | Tgfbi | L19932 | 2.0 | NS | Transforming growth factor, beta induced |
| 97825_at | Perp-pending | AI854029 | 2.0 | A | p53 apoptosis effector related to Pmp22 |
Fold changes were not shown for those genes that had detection calls of absent (A) in the 4-h treated group; that had an inappropriate change call (Chg), such that there was not a call of increased or marginally increased in greater than half of the comparisons made; that had a fold change less than 1 (Fld<2); or that were not determined to be significant (NS) by parametric and nonparametric tests, with a P cutoff value of ≤0.05.
TABLE 5.
Genes (53) that are upregulated 4 h following K. pneumoniae infection and are unique to C3H/HeN mice
| Affymetrix probe ID | Gene symbol | GenBank accession no. | Mean change (fold) in C3H/HeN mice at 4 vs 0 h | Results in C57BL/6 mice at 4 vs 0 ha | Description |
|---|---|---|---|---|---|
| 99367_at | EST | AA434661 | 9.1 | NS | IMAGE-818356 |
| 94375_at | Hk2 | Y11666 | 4.2 | Fld<2 | Hexokinase 2 |
| 103891_i_at | El12 | AI197161 | 4.1 | Fld<2 | Elongation factor RNA polymerase II |
| 92294_at | EST | AW060793 | 3.6 | NS | Unknown |
| 100302_at | Maff | AB009694 | 3.4 | Chg | v-Maf musculoaponeurotic fibrosarcoma oncogene family, protein F (avian) |
| 104701_at | Bhlhb2 | Y07836 | 3.2 | Fld<2 | Basic helix-loop-helix domain containing, class B2 |
| 103438_at | Dio2 | AF096875 | 2.8 | NS | Deiodinase, iodothyronine, type II |
| 97142_at | EST | C80153 | 2.7 | Chg | Unknown |
| 99864_at | Adora2b | AA608277 | 2.7 | Chg | Adenosine A2b receptor |
| 103892_r_at | EST | AI197161 | 2.6 | Fld<2 | IMAGE-1494691 |
| 99529_f_at | Rnf138 | AB025011 | 2.6 | NS | Ring finger protein 138 |
| 104612_g_at | Wdr26 | AI854008 | 2.6 | Fld<2 | WD repeat domain 26 |
| 92738_at | Gdnf | D49921 | 2.6 | NS | Glial cell line-derived neurotrophic factor |
| 102984_g_at | Madh1 | U58992 | 2.1 | Fld<2 | MAD homolog 1 |
| 160095_at | Lox | D10837 | 2.5 | NS | Lysyl oxidase |
| 95681_f_at | Ppplr2 | AW049584 | 2.5 | Chg | Protein phosphatase I, regulatory subunit 2 |
| 93981_at | Plat | J03520 | 2.4 | Chg | Plasminogen activator |
| 99032_at | Rasd1 | AF009246 | 2.4 | NS | RAS, dexamethasone induced 1 |
| 97740_at | Dusp16 | A1642662 | 2.4 | Fld<2 | Dual specificity phosphatase 16 |
| 95978_at | EST | AA414964 | 2.4 | Chg | Unknown |
| 93882_f_at | Tgoln2 | D50032 | 2.4 | Chg | trans-Golgi network protein 2 |
| 97890_at | Sgk | AW046181 | 2.4 | Fld<2 | Serum/glucocorticoid-regulated kinase |
| 103362_at | Ptger4 | D13458 | 2.4 | Fld<2 | Prostaglandin E receptor 4 (subtype EP4) |
| 94489_at | Prp4aI | U84411 | 2.3 | Fld<2 | Protein tyrosine phosphatase 4a 1 |
| 102292_at | Gadd45a | U00937 | 2.3 | Fld<2 | Growth arrest and DNA-damage-inducible 45 alpha |
| 104534_at | Pgm1 | AA623974 | 2.3 | Fld<2 | Phosphoglucomutase 1 |
| 98892_at | Lpin1 | AI846934 | 2.3 | NS | Lpin1 |
| 104494_at | EST | AI642098 | 2.3 | NS | Unknown |
| 103062_at | Rab33b | AB004664 | 2.3 | NS | RAB33B, member of RAS oncogene family |
| 96777_at | Sf3b1 | AW049372 | 2.2 | NS | Splicing factor 3b, subunit 1 |
| 100065_r_at | Gja1 | M63801 | 2.2 | Fld<2 | Gap junction membrane channel protein alpha 1 |
| 94378_at | Rgs16 | U94828 | 2.2 | Fld<2 | Retinally abundant regulator of G-protein signaling mRGS-r |
| 104257_g_at | Pscdbp | AI120844 | 2.2 | Fld<2 | Pleckstrin homology, Sec7, and coiled-coil domains, binding protein |
| 94088_at | Ptbp2 | AW228429 | 2.2 | Chg | Polypyrimidine tract binding protein 2 |
| 98540_g_at | Cops2 | AF071312 | 2.2 | Chg | COP9 (constitutive photomorphogenic homolog), subunit 2 |
| 94662_at | EST | AA409766 | 2.2 | NS | Unknown |
| 100010_at | Klf3 | U36340 | 2.2 | NS | Kruppel-like factor 3 |
| 98608_at | Etf1 | AI845886 | 2.1 | Fld<2 | Eukaryotic translation termination factor 1 |
| 93471_at | Slc4a7 | AI594427 | 2.1 | Chg | Solute carrier family 4, sodium bicarbonate cotransporter, member 7 |
| 100064_f_at | Gja1 | M63801 | 2.1 | Fld<2 | Gap junction membrane channel protein alpha 1 |
| 100509_at | Rnf19 | AW121012 | 2.1 | Fld<2 | Ring finger protein 19 |
| 92638_at | Ppp2ca | Z67745 | 2.1 | NS | Protein phosphatase 2a, catalytic subunit alpha isoform |
| 103708_at | Eifla | AI132207 | 2.1 | Fld<2 | Eukaryotic translation initiation factor 1A |
| 104340_at | Mbd1 | AF072240 | 2.1 | Fld<2 | Methyl-CpG binding domain protein 1 |
| 101437_at | Stk2 | AF039574 | 2.1 | NS | Serine/threonine kinase 2 |
| 103451_at | Ptk2b | AI835159 | 2.0 | Chg | PTK2 protein tyrosine kinase 2 beta |
| 100297_at | Wdr26 | AA693125 | 2.0 | NS | WD repeat domain 26 |
| 98946_at | Wsb-1 | AF033186 | 2.0 | Fld<2 | WD-40-repeat-containing protein with a SOCS box 1 |
| 99087_at | D10Ertd749e | AW060179 | 2.0 | Chg | DNA segment chromosome 10 |
| 103028_at | Itk | D14042 | 2.0 | NS | IL-2-inducible T-cell kinase |
| 103614_at | Nfkb2 | AW047899 | 2.0 | Fld<2 | Nuclear factor of kappa light polypeptide gene enhancer in B cells 2, p49/p100 |
| 94415_at | EST | AA710439 | 2.0 | Fld<2 | IMAGE-1165752 |
| 103288_at | Nrip1 | AF053062 | 2.0 | NS | Nuclear receptor-interacting protein 1 |
Fold changes were not shown for those genes that had detection calls of absent (A) in the 4-h treated group; that had an inappropriate change call (Chg), such that there was not a call of increased or marginally increased in greater than half of the comparisons made; that had a fold change less than 1 (Fld<2); or that were not determined to be significant by parametric and nonparametric tests with a P cutoff value of ≤0.05.
This Venn diagram analysis also revealed a list of 29 TLR4-independent genes that were found to be uniquely upregulated in C3H/HeJ mice at 4 h, including a number of transcriptional factors, enzymes, receptors, and heat shock proteins (HSPs) (Table 2). The 29 genes in Table 2 fall in to two broad categories: ones which are significantly more upregulated in C3H/HeJ mice than controls and genes that are upregulated in C3H/HeJ mice but downregulated at 4 h in the control strains. These latter genes, such as HSP 1A and 1B, appear to be negatively regulated by TLR signaling in control mice (Table 2). Of the 270 genes found in all three lists, only 6 are found to be upregulated by all strains (Table 3) which include a number of transcripts known or believed to be involved in the regulation of glucose (PDK), inflammation (GriPGHS), and glutathione production (GCLC). In addition to these genes, there were genes that were selectively upregulated in C3H/HeN mice compared to C3H/HeJ mice (Table 5). Among these were Rabb33b, which is involved in cellular vesicular transport; Rgs16, a regulator of G protein-coupled receptor signaling which is inducible by LPS and found to be expressed in dendritic cells (26); NF-κB; and IL-2-inducible T-cell kinase (Itk), involved in activation of T cells (34). Taken together, these data suggest that TLR4-mediated recognition of LPS in the lung is critical for the early and coordinated expression of a variety of genes controlling inflammation, granulopoeisis adhesion of neutrophils, and control of genes such as Itk which may be critical for adaptive immunity. We focused our subsequent analysis on a few key transcripts which have been shown to be critical in this model in either knockout or antibody neutralization studies (7, 8, 18, 20).
TABLE 2.
Mean TLR4-independent gene fold changes categorized by functiona
| Affymetrix probe ID | Gene symbol | Genbank accession no. | Change (fold) at 4 vs 0 h
|
Results in C3H/HeJ mice at 4 vs 0 h | Description | ||
|---|---|---|---|---|---|---|---|
| C57BL/6 | 129/SvJ | C3H/HeN | |||||
| Transcriptional Factors | |||||||
| 161348_r_at | Pdlim1 | AV149007 | −0.06 | −0.09 | 0.55 | 2.18 | PDZ and Lim domain 1 (elfin) |
| 104155_f_at | Atf3 | U19118 | 0.8 | 1.74 | −0.07 | 3.54 | Activating transcription factor 3 |
| 96418_r_at | Hox-2.4 | M18399 | −0.02 | 0.22 | 0.73 | 1.87 | Homeobox (Hox2.4) region |
| Enzymes | |||||||
| 161357_r_at | Gstm2 | AV207739 | 0.05 | −0.37 | 0.62 | 3 | Glutathione S-transferase, mu2 |
| 101179_at | DEAD/H | D50494 | −0.53 | −0.22 | −0.16 | 2.98 | Aspartate-glutamate-alanine-aspartate box polypeptide 6 |
| Receptor | |||||||
| 101771_r_at | CNR5 | AB008180 | −0.13 | 0.17 | 0.5 | 3.92 | Cadherin-related neural receptor 5 |
| Heat shock | |||||||
| 100946_at | Hspab | AF109906 | 0.43 | 0.09 | −1.98 | 5.15 | Heat shock protein 1B |
| 93875_at | Hspa1a | M12571 | −0.23 | 0.37 | −1.79 | 4.98 | Heat shock protein 1A |
| 96254_at | Dnajb1 | AB028272 | −0.14 | 0.18 | −0.86 | 2.06 | DNA J homolog, subfamily B, member 1 |
| Other | |||||||
| 92958_at | NA | AI849135 | 0.16 | −0.21 | 0.18 | 1.04 | NA |
| 98590_at | SYND4 | D89571 | 0.16 | −0.35 | 0.48 | 1.13 | Ryudocan core protein |
| 96680_at | NA | AI835630 | 0.6 | −0.19 | 0.51 | 2.2 | NA |
| 162420_r_at | NA | AV290470 | −0.16 | 0.08 | 0.21 | 2.28 | NA |
| 99849_at | NA | C85523 | 0.13 | 0.72 | 0.77 | 1.51 | NA |
| 96526_at | NA | AW228840 | 0.14 | 0.02 | 0.44 | 1.55 | NA |
| 160169_at | NA | AI851407 | 0.69 | −0.01 | 0.14 | 1.96 | NA |
| 104046_at | NA | AI854141 | 0.06 | −0.09 | 0.49 | 1.42 | NA |
| 161348_r_at | NA | AV149007 | −0.06 | −0.09 | 0.55 | 2.18 | NA |
| 160949_at | NA | AI848924 | 0.41 | −0.15 | 0.24 | 2.12 | NA |
| 99162_at | NA | AW122398 | 0.67 | 0.3 | 0.88 | 2.04 | NA |
| 160989_r_at | NA | AA717225 | −0.16 | −0.81 | 1.07 | 2.34 | NA |
| 161561_r_at | NA | AV264321 | −0.63 | 0.04 | 0.31 | 3.9 | NA |
| 160979_at | NA | AW120820 | −0.36 | −0.11 | −0.31 | 1.5 | NA |
| 104343_f_at | NA | AI845798 | 0.38 | 0.58 | 0.38 | 1.44 | NA |
| 102381_at | NA | AA619207 | 0.56 | 0.14 | 0.65 | 1.49 | NA |
| 162496_r_at | NA | AV153195 | 0.04 | 0.42 | 0.55 | 2.82 | NA |
| 161869_s_at | NA | AV265258 | −0.09 | −0.85 | −0.32 | 1.82 | NA |
| 101869_s_at | β-globin | J00413 | −0.41 | −0.61 | −0.87 | 1.68 | β-Globin major gene |
| AFFX-b-ActinMur/M12481_M_st | β-actin | M12481 | −0.14 | −0.36 | 0.06 | 1.53 | Cytoplasmic β-actin |
| 103534_at | β1-globin | V00722 | −0.38 | −0.63 | −0.82 | 2.23 | β-1-globin |
| 102727_at | BDNF | X55573 | 0.18 | −0.07 | −0.06 | 2.22 | Brain-derived neurotrophic factor |
| 99500_at | SLC12A2 | U13174 | 0.37 | 0.09 | 0.43 | 1.11 | Solute carrier family 12, member 2 |
NA, not applicable.
Detection of key TLR4-dependent transcripts.
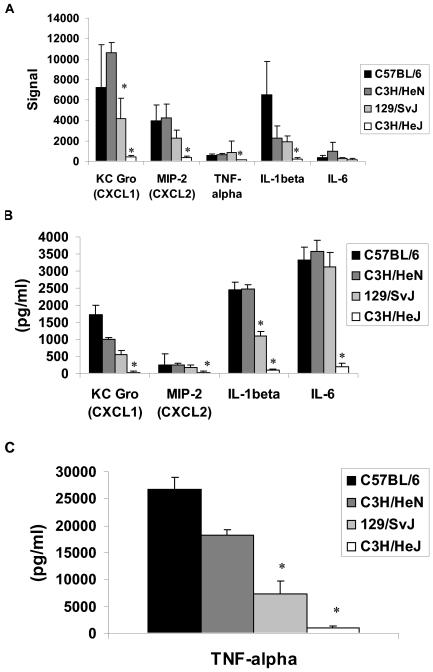
The signal values of several important TLR4-dependent genes were plotted for each strain at the 4-h time point, including TNF-α, IL-1β, IL-6, MIP-2 and KC-GRO (Cxcl1) (Fig. 4A). These values are suggestive of the relative transcript abundance in a sample and were generated with algorithms found in MAS version 5.0 (Affymetrix). The numbers for individual replicates in a group were averaged together and plotted by using Excel software. Both C57BL/6 and C3H/HeN mice showed significantly higher levels of these transcripts at the 4-h time point, while the C3H/HeJ mice showed a minimal signal response. Moreover, the 129/SvJ mice showed lower levels of these transcripts than control mice.
FIG. 4.
A: presence of key TLR4-dependent transcripts in lung samples generated in four different strains of mice 4 h after intratracheal challenge with K. pneumoniae. Signal values were generated by using algorithms found in MAS software version 5.0 (Affymetrix), and biological replicates for each strain were averaged together and plotted by using Excel. Control strains, C57BL/6 and C3H/HeN, showed higher signal values, while the 129/SvJ strain showed lower levels of signal for almost all genes displayed. The C3H/HeJ strain showed a minimal signal response for these genes, as expected. Data are expressed as means ± standard errors of the means (SEM) (n = 4 to 9 mice per group; an * denotes a P value of <0.05 compared to C57BL/6 mice). B: protein concentrations in macrophage supernatants by Bio-Plex assay of four TLR4-dependent immune factors in four strains of mice after 6 h of ex vivo incubation with heat-killed K. pneumoniae. These levels are consistent with the RNA expression patterns established in the signal plot for the same factors, thus confirming that RNA levels may be predictive of a survival phenotype. Data are expressed as means ± SEM (n = 4 to 6 mice per group; an * denotes a P value of <0.05 compared to C57BL/6 mice). C: presence of TNF-α protein as measured by enzyme-linked immunosorbent assay in supernatants of macrophages isolated from four strains of mice and incubated with K. pneumoniae for 6 h. Data are expressed as means ± SEM (n = 4 to 6 mice per group; an * denotes a P value of <0.05 compared to C57BL/6 mice).
Detection of key TLR4-dependent proteins from isolated macrophages.
TLR4 is most abundantly expressed on alveolar macrophages and dendritic cells (1, 16, 32). As these are some of the first cells to encounter an invading pathogen in the lung and to verify that changes in signal levels were reflected at the protein level, we examined protein production for TLR4-dependent transcripts in ex vivo-treated alveolar macrophages. In these studies, 50,000 alveolar macrophages from each murine strain were harvested, plated, and incubated with heat-killed K. pneumoniae for 6 h, and cytokines and chemokines were measured by using a Bio-Plex 18 assay as described in Materials and Methods. The trends identified by surveying the signal values of specific genes were replicated in these protein assays. Specifically, C57BL/6 and C3H/HeN strains showed higher levels of MIP-2, IL-6, KC-GRO, G-CSF (Fig. 4B), and TNF-α (Fig. 4C) in culture supernatants, as opposed to that of the TLR4 mutant C3H/HeJ. The 129/SvJ mice had lower levels of these proteins at the same time point, consistent with the signal value trends seen in Fig. 4A. E. coli LPS-treated cells were also included as positive controls in this study and showed levels of cytokine/chemokine production across mouse strains similar to those found with heat-killed K. pneumoniae (data not shown). Control wells lacking any stimulus revealed cytokine/chemokine levels of <50 pg/ml.
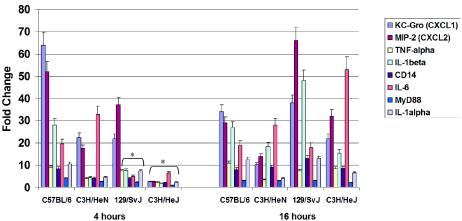
Comparison of fold change values over time for key transcripts.
Although TLR4 is critical for early gene expression, TLR4-deficient mice clustered with mice with intact TLR4 at 16 h (Fig. 2), suggesting that they have a delayed response. To confirm this hypothesis, we analyzed eight known genes related to or regulated by TLR4 (TNF-α, IL-1β, IL-6, MIP-2, KC-GRO, CD14, and Myd88) and graphed their fold change from time zero by strain and experimental time point (Fig. 5). As illustrated, C3H/HeJ mice had significantly lower fold change values for all genes at 4 h than mice with intact TLR4 (P < 0.001; analysis of variance) compared to those at 16 h (Fig. 5), where they had a fold induction similar to that of a strain with intact TLR4 at 4h. The results for C3H/HeN and 129/SvJ at 4 h gave similar expression patterns which were also depicted in the hierarchical cluster, whereby these two strains at this time point clustered together. This graph also demonstrated the same trends seen in the hierarchical cluster, where C3H/HeN, 129/SvJ, and C3H/HeJ showed delayed expression in these genes at 4 h but at 16 h appeared to catch up to the expression values seen at the 4-h time point in C57BL/6 mice. Thus, this analysis independently confirms data from hierarchical clustering (Fig. 2).
FIG. 5.
Analysis of eight known related genes regulated by TLR4 by strain. In order to verify our hierarchical clustering, we plotted the average fold change values of eight highly expressed TLR4-related genes (KC-GRO, MIP-2, TNF-α, IL-1β, CD14, IL-6, MyD88, and IL-1α) by strain and time. Data are expressed as means ± SEM (an * denotes a P value of <0.05 compared to C57BL/6 mice).
DISCUSSION
The development of pneumonia is a complex interaction between virulence factors of the invading pathogen, the inoculum size, and host factors. The results outlined in these studies suggest that TLR4 recognition of invading pathogens is a critical early response pathway that regulates genes ultimately responsible for successful host defense against gram-negative bacteria.
TLR4 signaling was responsible for a diverse set of genes involved in innate immunity, such as IL-1β and TNF-α; chemokines involved in host defense and granulopoeisis, including MIP-2, KC-GRO, MIP-1α, and G-CSF (6, 19); and receptors expressed in lung cells and recruited immune cells. Further support of our data is provided by the fact that antibody neutralization or genetic disruption of MIP-2 (8), TNF (17, 20), MIP-1α (18), or the urokinase receptor (9) results in impaired host defense against gram-negative bacteria. Some of the genes in Table 1, such as CD14, MyD88, and CD44, may be upregulated due to cell recruitment into the lung rather than a true increase in endogenous gene expression. We chose 4 h for our first time point since this time point represents the beginning of significant neutrophil recruitment into the lung, and we postulated that this time point would largely represent endogenous genes, but we cannot exclude an effect of marginated cells in the lung that may account for this set of genes appearing in our list of TLR-dependent genes. Furthermore, our data show that TLR was required for nearly all of the cytokine/chemokine gene expression at 4 h in our model, as these growth factors are notably absent in our TLR4-independent or shared genes (Tables 2 and 3). Moreover, this microarray analysis revealed that TLR4 appears to be critical for downregulation of HSPs (Table 2). Recent evidence supports HSP 70 as an endogenous stimulus for TLR signaling (2, 5, 31), and downregulation of HSPs in the control strains may occur in an effort to downregulate the inflammatory response.
Studies in this model have suggested that macrophages which express TLR4 are critical to early host defense (4). To confirm some of these critical genes at the protein level, we performed ex vivo stimulations with macrophages from the mouse strains. These ex vivo experiments confirmed the role of TLR4 in the protein production of cytokines and chemokines. However, our data do not allow us to determine the role of resident alveolar macrophages in the overall production of the TLR4 pathway in the lung. Using microarray analysis, Weighardt and colleagues have recently shown that over 40% of the gene expression in purified dendritic cells is Trif dependent rather than MyD88 dependent (33). Moreover, 129/SvJ mice have also been reported to have a defect in the upregulation of costimulatory molecules on dendritic cells in response to double-stranded RNA, and this appears to be due to a single gene defect (13). As this strain clearly also has attenuated host defense against K. pneumoniae and has altered expression of genes downstream of TLR4, this phenotype may be explained by a defective adaptor protein that plays a role in host defense against gram-negative bacteria and recognition of double-stranded RNA. Moreover, due to these defects in the 129/SvJ mice, phenotypes obtained in knockout mice backcrossed to C57BL/6 mice must be interpreted with caution until these 129/SvJ alleles are elucidated (13).
Of note, TLR4-deficient mice clustered with mice with intact TLR4 at 16 h, suggesting that they have a delayed response. As TLR4 is the critical LPS receptor, we speculate that this change in gene expression at 16 h may involve other MyD88-dependent pathways such as TLR2 (25, 30) or TLR9 (12) which could come into play later in this model of infection. In support of this speculation, it has been recently been reported that MyD88 knockout mice fail to upregulate TNF-α even 24 h after a pulmonary challenge with Pseudomonas aeruginosa, suggesting that mice lacking MyD88 signaling do not show this catch-up phenomenon (27). Additionally, the whole organ gene expression profiling approach clearly misses some genes with are indirectly TLR dependent. For example, IL-17A and IL-17F, which regulate lung neutrophil recruitment into the lung and host defense in this model, were absent on the chip algorithm but have been demonstrated to be TLR dependent by a Taqman approach (11). Thus, our approach is biased towards the most abundantly expressed transcripts and does not exclude more subtly expressed genes that may be equally critical for host defense. Moreover, our data are limited to one strain of K. pneumoniae, and some of the TLR4-dependent genes may be under indirect control of TLR4 signaling via TLR4-dependent activation of a signaling molecule or transcription factor. Nevertheless, these data do show that TLR4 signaling is a critical early response pathway and accounts for 120 of the 162 genes that change in 4 h in C3H mice or 74% of gene expression. This coordinated gene expression plays a key role in determining lung host defense to live gram-negative bacteria. We postulate that the ability to rapidly express TLR4-related genes in response to a bacterial challenge permits containment of infection and survival, while delayed expression of these genes results in bacterial dissemination and mortality.
Acknowledgments
This work was supported by Public Health Service grants AA010384, HL061271 (J.K.K.), and AI051677 (J.E.S.) and the Louisiana Gene Therapy Research Consortium.
Editor: F. C. Fang
REFERENCES
- 1.Arbour, N. C., E. Lorenz, B. C. Schutte, J. Zabner, J. N. Kline, M. Jones, K. Frees, J. L. Watt, and D. A. Schwartz. 2000. TLR4 mutations are associated with endotoxin hyporesponsiveness in humans. Nat. Genet. 25:187-191. [DOI] [PubMed] [Google Scholar]
- 2.Asea, A., M. Rehli, E. Kabingu, J. A. Boch, O. Bare, P. E. Auron, M. A. Stevenson, and S. K. Calderwood. 2002. Novel signal transduction pathway utilized by extracellular HSP70: role of Toll-like receptor (TLR) 2 and TLR4. J. Biol. Chem. 277:15028-15034. [DOI] [PubMed] [Google Scholar]
- 3.Beutler, B., K. Hoebe, X. Du, and R. J. Ulevitch. 2003. How we detect microbes and respond to them: the Toll-like receptors and their transducers. J. Leukoc. Biol. 74:479-485. [DOI] [PubMed] [Google Scholar]
- 4.Broug-Holub, E., G. B. Toews, J. F. van Iwaarden, R. M. Strieter, S. L. Kunkel, R. Paine III, and T. J. Standiford. 1997. Alveolar macrophages are required for protective pulmonary defenses in murine Klebsiella pneumonia: elimination of alveolar macrophages increases neutrophil recruitment but decreases bacterial clearance and survival. Infect. Immun. 65:1139-1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen, M., F. Aosai, K. Norose, H. S. Mun, O. Takeuchi, S. Akira, and A. Yano. 2002. Involvement of MyD88 in host defense and the down-regulation of anti-heat shock protein 70 autoantibody formation by MyD88 in Toxoplasma gondii-infected mice. J. Parasitol. 88:1017-1019. [DOI] [PubMed] [Google Scholar]
- 6.Dale, D. C., W. C. Liles, W. R. Summer, and S. Nelson. 1995. Review: granulocyte colony-stimulating factor—role and relationships in infectious diseases. J. Infect. Dis. 172:1061-1075. [DOI] [PubMed] [Google Scholar]
- 7.Greenberger, M. J., S. L. Kunkel, R. M. Strieter, N. W. Lukacs, J. Bramson, J. Gauldie, F. L. Graham, M. Hitt, J. M. Danforth, and T. J. Standiford. 1996. IL-12 gene therapy protects mice in lethal Klebsiella pneumonia. J. Immunol. 157:3006-3012. [PubMed] [Google Scholar]
- 8.Greenberger, M. J., R. M. Strieter, S. L. Kunkel, J. M. Danforth, L. L. Laichalk, D. C. McGillicuddy, and T. J. Standiford. 1996. Neutralization of macrophage inflammatory protein-2 attenuates neutrophil recruitment and bacterial clearance in murine Klebsiella pneumonia. J. Infect. Dis. 173:159-165. [DOI] [PubMed] [Google Scholar]
- 9.Gyetko, M. R., S. Sud, T. Kendall, J. A. Fuller, M. W. Newstead, and T. J. Standiford. 2000. Urokinase receptor-deficient mice have impaired neutrophil recruitment in response to pulmonary Pseudomonas aeruginosa infection. J. Immunol. 165:1513-1519. [DOI] [PubMed] [Google Scholar]
- 10.Hagberg, L., D. E. Briles, and C. S. Eden. 1985. Evidence for separate genetic defects in C3H/HeJ and C3HeB/FeJ mice, that affect susceptibility to gram-negative infections. J. Immunol. 134:4118-4122. [PubMed] [Google Scholar]
- 11.Happel, K. I., M. Zheng, E. Young, L. J. Quinton, E. Lockhart, A. J. Ramsay, J. E. Shellito, J. R. Schurr, G. J. Bagby, S. Nelson, and J. K. Kolls. 2003. Cutting edge: roles of Toll-like receptor 4 and IL-23 in IL-17 expression in response to Klebsiella pneumoniae infection. J. Immunol. 170:4432-4436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hemmi, H., O. Takeuchi, T. Kawai, T. Kaisho, S. Sato, H. Sanjo, M. Matsumoto, K. Hoshino, H. Wagner, K. Takeda, and S. Akira. 2000. A Toll-like receptor recognizes bacterial DNA. Nature 408:740-745. [DOI] [PubMed] [Google Scholar]
- 13.Hoebe, K., E. M. Janssen, S. O. Kim, L. Alexopoulou, R. A. Flavell, J. Han, and B. Beutler. 2003. Upregulation of costimulatory molecules induced by lipopolysaccharide and double-stranded RNA occurs by Trif-dependent and Trif-independent pathways. Nat. Immunol. 4:1223-1229. [DOI] [PubMed] [Google Scholar]
- 14.Hoshino, K., O. Takeuchi, T. Kawai, H. Sanjo, T. Ogawa, Y. Takeda, K. Takeda, and S. Akira. 1999. Cutting edge: Toll-like receptor 4 (TLR4)-deficient mice are hyporesponsive to lipopolysaccharide: evidence for TLR4 as the Lps gene product. J. Immunol. 162:3749-3752. [PubMed] [Google Scholar]
- 15.Huang, Q., D. Liu, P. Majewski, L. C. Schulte, J. M. Korn, R. A. Young, E. S. Lander, and N. Hacohen. 2001. The plasticity of dendritic cell responses to pathogens and their components. Science 294:870-875. [DOI] [PubMed] [Google Scholar]
- 16.Kaisho, T., and S. Akira. 2000. Critical roles of Toll-like receptors in host defense. Crit. Rev. Immunol. 20:393-405. [PubMed] [Google Scholar]
- 17.Laichalk, L. L., S. L. Kunkel, R. M. Strieter, J. M. Danforth, M. B. Bailie, and T. J. Standiford. 1996. Tumor necrosis factor mediates lung antibacterial host defense in murine Klebsiella pneumonia. Infect. Immun. 64:5211-5218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindell, D. M., T. J. Standiford, P. Mancuso, Z. J. Leshen, and G. B. Huffnagle. 2001. Macrophage inflammatory protein 1α/CCL3 is required for clearance of an acute Klebsiella pneumoniae pulmonary infection. Infect. Immun. 69:6364-6369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mehrad, B., and T. J. Standiford. 1999. Role of cytokines in pulmonary antimicrobial host defense. Immunol. Res. 20:15-27. [DOI] [PubMed] [Google Scholar]
- 20.Moore, T. A., H. Y. Lau, A. L. Cogen, C. L. Monteleon, and T. J. Standiford. 2003. Anti-tumor necrosis factor-alpha therapy during murine Klebsiella pneumoniae bacteremia: increased mortality in the absence of liver injury. Shock 20:309-315. [DOI] [PubMed] [Google Scholar]
- 21.Nau, G. J., J. F. Richmond, A. Schlesinger, E. G. Jennings, E. S. Lander, and R. A. Young. 2002. Human macrophage activation programs induced by bacterial pathogens. Proc. Natl. Acad. Sci. USA 99:1503-1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nau, G. J., A. Schlesinger, J. F. Richmond, and R. A. Young. 2003. Cumulative Toll-like receptor activation in human macrophages treated with whole bacteria. J. Immunol. 170:5203-5209. [DOI] [PubMed] [Google Scholar]
- 23.Poltorak, A., X. He, I. Smirnova, M. Y. Liu, C. V. Huffel, X. Du, D. Birdwell, E. Alejos, M. Silva, C. Galanos, M. Freudenberg, P. Ricciardi-Castagnoli, B. Layton, and B. Beutler. 1998. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science 282:2085-2088. [DOI] [PubMed] [Google Scholar]
- 24.Rothe, M., J. Xiong, H. B. Shu, K. Williamson, A. Goddard, and D. V. Goeddel. 1996. I-TRAF is a novel TRAF-interacting protein that regulates TRAF-mediated signal transduction. Proc. Natl. Acad. Sci. USA 93:8241-8246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schwandner, R., R. Dziarski, H. Wesche, M. Rothe, and C. J. Kirschning. 1999. Peptidoglycan- and lipoteichoic acid-induced cell activation is mediated by Toll-like receptor 2. J. Biol. Chem. 274:17406-17409. [DOI] [PubMed] [Google Scholar]
- 26.Shi, G. X., K. Harrison, S. B. Han, C. Moratz, and J. H. Kehrl. 2004. Toll-like receptor signaling alters the expression of regulator of G protein signaling proteins in dendritic cells: implications for G protein-coupled receptor signaling. J. Immunol. 172:5175-5184. [DOI] [PubMed] [Google Scholar]
- 27.Skerrett, S. J., H. D. Liggitt, A. M. Hajjar, and C. B. Wilson. 2004. Cutting edge: myeloid differentiation factor 88 is essential for pulmonary host defense against Pseudomonas aeruginosa but not Staphylococcus aureus. J. Immunol. 172:3377-3381. [DOI] [PubMed] [Google Scholar]
- 28.Suzuki, K., and M. Taniike. 1995. Murine model of genetic demyelinating disease: the twitcher mouse. Microsc. Res. Technol. 32:204-214. [DOI] [PubMed] [Google Scholar]
- 29.Takeuchi, O., K. Hoshino, and S. Akira. 2000. Cutting edge: TLR2-deficient and MyD88-deficient mice are highly susceptible to Staphylococcus aureus infection. J. Immunol. 165:5392-5396. [DOI] [PubMed] [Google Scholar]
- 30.Takeuchi, O., K. Hoshino, T. Kawai, H. Sanjo, H. Takada, T. Ogawa, K. Takeda, and S. Akira. 1999. Differential roles of TLR2 and TLR4 in recognition of gram-negative and gram-positive bacterial cell wall components. Immunity 11:443-451. [DOI] [PubMed] [Google Scholar]
- 31.Vabulas, R. M., P. Ahmad-Nejad, S. Ghose, C. J. Kirschning, R. D. Issels, and H. Wagner. 2002. HSP70 as endogenous stimulus of the Toll/interleukin-1 receptor signal pathway. J. Biol. Chem. 277:15107-15112. [DOI] [PubMed] [Google Scholar]
- 32.Visintin, A., A. Mazzoni, J. H. Spitzer, D. H. Wyllie, S. K. Dower, and D. M. Segal. 2001. Regulation of Toll-like receptors in human monocytes and dendritic cells. J. Immunol. 166:249-255. [DOI] [PubMed] [Google Scholar]
- 33.Weighardt, H., G. Jusek, J. Mages, R. Lang, K. Hoebe, B. Beutler, and B. Holzmann. 2004. Identification of a TLR4- and TRIF-dependent activation program of dendritic cells. Eur. J. Immunol. 34:558-564. [DOI] [PubMed] [Google Scholar]
- 34.Wilcox, H. M., and L. J. Berg. 2003. Itk phosphorylation sites are required for functional activity in primary T cells. J. Biol. Chem. 278:37112-37121. [DOI] [PubMed] [Google Scholar]
- 35.Ye, P., P. B. Garvey, P. Zhang, S. Nelson, G. Bagby, W. R. Summer, P. Schwarzenberger, J. E. Shellito, and J. K. Kolls. 2001. Interleukin-17 and lung host defense against Klebsiella pneumoniae infection. Am. J. Respir. Cell Mol. Biol. 25:335-340. [DOI] [PubMed] [Google Scholar]
- 36.Ye, P., F. H. Rodriguez, S. Kanaly, K. L. Stocking, J. Schurr, P. Schwarzenberger, P. Oliver, W. Huang, P. Zhang, J. Zhang, J. E. Shellito, G. J. Bagby, S. Nelson, K. Charrier, J. J. Peschon, and J. K. Kolls. 2001. Requirement of interleukin 17 receptor signaling for lung CXC chemokine and granulocyte colony-stimulating factor expression, neutrophil recruitment, and host defense. J. Exp. Med. 194:519-528. [DOI] [PMC free article] [PubMed] [Google Scholar]