Summary
Ex vivo gene therapy based on CD34+ hematopoietic stem cells (HSCs) has shown promising results in clinical trials, but genetic engineering to high levels and in large scale remains challenging. We devised a sorting strategy that captures more than 90% of HSC activity in less than 10% of mobilized peripheral blood (mPB) CD34+ cells, and modeled a transplantation protocol based on highly purified, genetically engineered HSCs co-infused with uncultured progenitor cells. Prostaglandin E2 stimulation allowed near-complete transduction of HSCs with lentiviral vectors during a culture time of less than 38 hr, mitigating the negative impact of standard culture on progenitor cell function. Exploiting the pyrimidoindole derivative UM171, we show that transduced mPB CD34+CD38− cells with repopulating potential could be expanded ex vivo. Implementing these findings in clinical gene therapy protocols will improve the efficacy, safety, and sustainability of gene therapy and generate new opportunities in the field of gene editing.
Keywords: HSC gene therapy, purified HSCs, HSC expansion, lentiviral vector transduction, prostaglandin E2, UM171
Highlights
-
•
CD34+CD38− cells as an HSC-enriched starting population for ex vivo gene therapy
-
•
Reduced culture time (<38 hr) alleviates negative impact on progenitor cell potency
-
•
Prostaglandin E2 increases LV transduction up to 2× enabling shorter protocols
-
•
UM171 supports ex vivo expansion of mobilized peripheral blood HSCs
In this article, Gentner and colleagues undertake a comprehensive strategy to advance ex vivo genetic engineering of HSCs for gene therapy. They experimentally define an optimal strategy to purify HSCs, which allows uncoupling long-term from short-term hematopoietic reconstitution, and implement ex vivo conditions that best preserve their biological properties applying novel transduction-enhancing compounds and pyrimidoindole derivatives to support HSC expansion.
Introduction
Introduction of the lentiviral vector (LV) platform has spurred applications of gene therapy based on the transplantation of ex-vivo-engineered, autologous hematopoietic stem and progenitor cells (HSPCs) (Naldini, 2015). Recent clinical trials for patients affected by primary immunodeficiencies, hemoglobinopathies, or inborn errors of metabolism have shown high levels of gene transfer into HSPCs, which were stably maintained in multiple hematopoietic lineages until the latest follow-up, reaching up to 9 years in the earliest trial (Cartier et al., 2009, Aiuti et al., 2013, Biffi et al., 2013, Hacein-Bey Abina et al., 2015, Sessa et al., 2016). The post-transplant hematopoiesis reconstituted by polyclonal, gene-marked HSPCs has provided substantial and sustained therapeutic benefit to most treated patients to date. Contrary to the gene therapy trials performed with gamma-retroviral vectors, no adverse events related to insertional mutagenesis of semi-randomly integrating LVs have been reported to date, even though substantial integration loads, typically ranging over 5–20 million integrations per kg body weight, have now been infused into >150 patients. The side effects reported in these gene therapy trials are typically related to the conditioning regimen and include mucositis and temporary bone marrow (BM) aplasia. Trials employing full myeloablation and BM-derived transduced CD34+ cells often showed more prolonged grade 4 neutropenia and thrombocytopenia than allogeneic BM transplantation, despite administering at least similar doses of CD34+ cells/kg (Sessa et al., 2016). Delayed recovery may be caused by the ex vivo culture of the cell therapy product, which typically lasts more than 60 hr (Aiuti et al., 2013, Biffi et al., 2013). Indeed, experimental evidence has accumulated that cultured HSPCs progressively lose engraftment potential by recruitment into cell cycle and loss of adhesion molecules, thus impeding their homing into the niche and driving lineage commitment and differentiation (Glimm et al., 2000, Kallinikou et al., 2012, Larochelle et al., 2012). This notion contrasts with recent reports on successful ex vivo cord blood (CB) expansion leading to accelerated hematologic recovery in patients (reviewed in Kiernan et al., 2016). Differences among HSPC sources (CB versus BM or mobilized peripheral blood [mPB]) may contribute to diverging outcomes, and a complete understanding is key to harnessing emerging CB expansion protocols for ex vivo gene transfer procedures, which utilize BM or mPB HSPCs. Moreover, CD34+ HSPCs comprise a heterogeneous mixture of progenitors at various stages of lineage commitment, the composition of which changes according to age, cell source, and mobilization procedure, and studies investigating the impact of ex vivo culture on defined subpopulations are lacking. Only a minute fraction of these CD34+ cells corresponds to long-term (LT) hematopoietic stem cells (HSCs). Limiting-dilution transplants into immunodeficient mice indicate that no more than 0.1% of lineage-negative CB cells (50%–75% CD34+) engraft longterm (McDermott et al., 2010). In line with an even lower HSC frequency in BM or mPB CD34+ cells, capture/re-capture statistics performed on longitudinally sampled LV integration sites from patients treated by gene therapy indicate that ∼0.01% of the infused CD34+ cells contribute to long-term hematopoiesis (Aiuti et al., 2013, Biffi et al., 2013, Biasco et al., 2015). These data indicate that there is a substantial margin to more precisely tailor gene transfer to LT-HSCs as opposed to the bulk of CD34+ cells, adapting ex vivo manipulation specifically to the requirements of the therapeutically relevant cell subsets. Several landmark studies have identified surface markers that allow prospective isolation of functionally diverse HSPC subsets (Majeti et al., 2007, Notta et al., 2011). However, most of these studies were done on CB cells that did not undergo ex vivo culture, making the results not necessarily representative of the cells typically used in HSPC gene therapy trials. Furthermore, most studies functionally validating HSC markers employed binary sorting gates (markerpositive versus markernegative). Given that antibody staining for many HSPC markers, such as CD38, CD49f, and CD90, results in a gradient of cells with increasing antigen density rather than clearly segregating two populations, large proportions of HSPCs with an intermediate phenotype have not been analyzed in these functional assays.
Here we undertake a comprehensive strategy to advance ex vivo genetic engineering of HSPCs for gene therapy. We experimentally define an optimal, clinically applicable strategy to purify HSCs, which allows uncoupling long-term from short-term hematopoietic reconstitution, and implement ex vivo conditions that best preserve their biological properties applying transduction-enhancing compounds and pyrimidoindole derivatives to support ex vivo HSC expansion.
Results
Definition of Functionally Distinct CD34+ Subpopulations in the Setting of Ex Vivo Gene Therapy
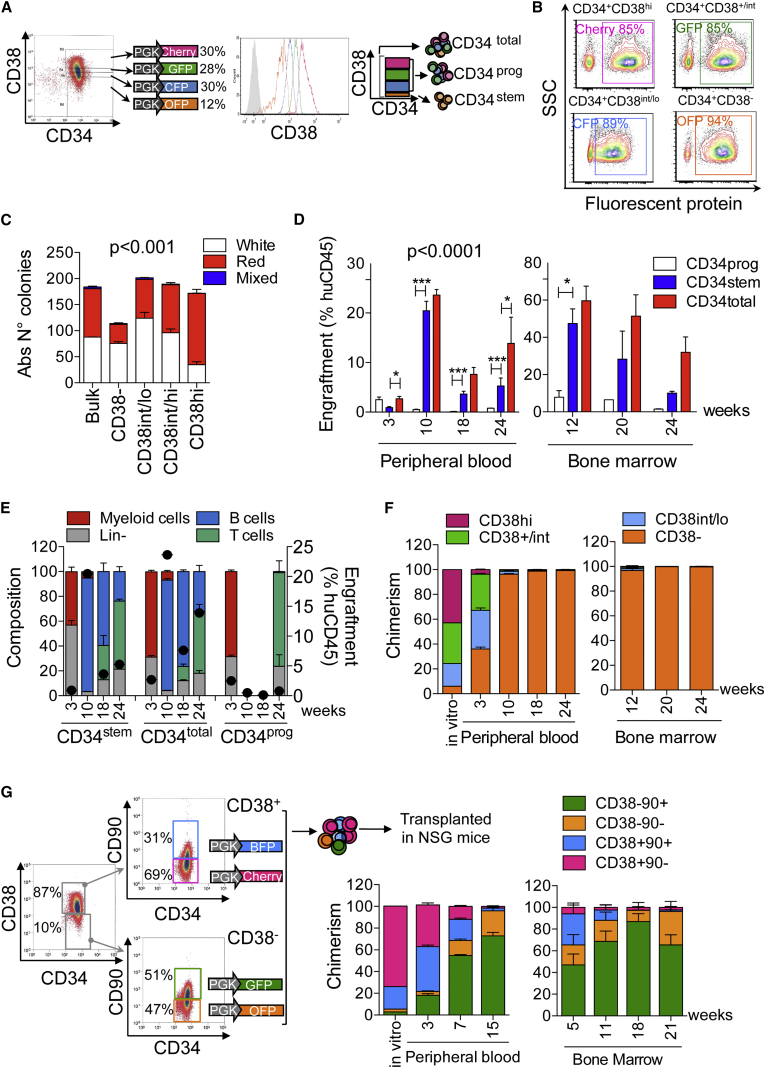
We devised an experimental model that allows tracing the origin of human hematopoiesis to diverse CD34+ HSPC subpopulations, defined at transplantation, in a xenograft over 6 months. First, we sorted CD34+ cells from mPB into four subpopulations according to CD38 expression and stably marked each with a different LV expressing one of the following fluorescent proteins (FP): green FP (GFP), red FP (Cherry), cyan/blue FP (CFP/BFP), or orange FP (OFP) (Figures 1A and S1A). By setting closely spaced sorting gates encompassing the CD38dim populations, we could interrogate the entire CD34+ cell population for differential engraftment potential. In vitro assays confirmed similarly high (>85%) transduction efficiencies for all subpopulations (Figures 1B and S1B) and reduced, myeloid-biased colony-forming capacity within the most primitive CD34+CD38− fraction (Figures 1C and S1C). One day after transduction, we re-assembled the following cell populations for xenotransplantation: CD34total (all four subpopulations re-assembled to the original proportions at sorting), CD34prog (the three CD38+ subpopulations), and CD34stem (the subpopulation with the 10% lowest CD38 expression). CD34stem cells showed little engraftment at 3 weeks but neared the level of the CD34total group 2 months post-transplantation (Figures 1D and S1D). Instead, CD34prog cells were responsible for the majority of short-term engraftment at 3 weeks post-transplant; their myeloid potential extinguished thereafter, with persistence of low lymphoid (mostly T cell) engraftment at the latest time of analysis (Figures 1E and S1E). Within the CD34prog populations, almost no engraftment was derived from the highest CD38 subset, while short-term engraftment (3 weeks) was equally derived from CD38int and CD38low cells (Figures 1F and S1F). Within the CD34total population, the dominance of the CD34+CD38− fraction in mediating nearly all multi-lineage long-term engraftment became evident at 9–10 weeks post-transplant (Figures 1F and S1F). We reached similar conclusions for BM-derived CD34+ cells (Figure S2) and CB cells, where separation into CD38+ and CD38− fractions was carried out with a bead-based sorting procedure (Figure S3).
Figure 1.
In Vivo Tracking of Hematopoietic Reconstitution by CD34+ mPB Subpopulations
(A) Four mPB CD34+ cell subpopulations differing in CD38 expression levels were sorted and transduced with LVs expressing the indicated FPs (PGK, phosphoglycerate kinase promoter). Subpopulation frequency within total CD34+ cells and CD38 expression upon post-sorting re-analysis are shown (histogram plot). The scheme on the right shows how transduced subpopulations were mixed in the three xenotransplantation groups, maintaining their relative frequency at sorting.
(B) Representative transduction efficiency of the indicated subpopulations, as measured in the myeloid colonies after 14 days of culture.
(C) Clonogenic potential of the transduced subpopulations (n = 4 per group). Statistics by one-way ANOVA with Bonferroni's multiple comparison test: white colonies, CD38− versus CD38int/lo∗∗, CD38− versus CD38hi∗; for red colonies, CD38− versus Bulk ∗∗∗, CD38− versus CD38int/lo∗∗, CD38− versus CD38int/hi∗∗∗, CD38− versus CD38hi∗∗∗.
(D) Human CD45+ cell engraftment in PB and BM at the indicated number of weeks post-transplant (n = 4 mice per group). Data were analyzed by two-way ANOVA with Bonferroni's multiple comparison test, significant differences with respect to the CD34stem group are shown.
(E) Lineage composition (left axis) of the human CD45+ cell graft in the PB at the indicated number of weeks post-transplantation. Black dots indicate huCD45+ cell engraftment levels (right axis). B cells, CD19+; myeloid cells, CD13+, T cells, CD3+; Lin−, CD19−, CD13−, CD3− cells.
(F) Distribution of the four FPs in the CD34total group before injection (in vitro) or within human CD45+ cells sampled from the PB and BM at the indicated number of weeks post-transplantation allows back-tracking the origin of hematopoietic reconstitution to the originally transplanted cell subpopulations indicated in the legend.
(G) Four subpopulations differing in CD38 and CD90 expression levels were sorted, transduced with the indicated LVs, mixed back maintaining their relative frequency, and xenografted (n = 9 mice, representative experiment). Hematologic reconstitution at the indicated number of weeks post-transplantation in PB and BM is back-tracked to the population of origin, as in (F).
Error bars represent SEM. See also Figures S1–S3.
A common practice to further enrich for engrafting HSCs is to purify the CD90+ fraction of CD34+CD38− HSPCs. We thus sought to define the engraftment kinetics of CD90+/− subpopulations of short-term (CD34+CD38low/int) or long-term (CD34+CD38−) repopulating HSPCs using a similar marking/re-assembly approach (Figure 1G). Again, long-term engraftment was almost exclusively derived from CD34+CD38− cells. However, approximately one-third originated from the CD90– compartment, indicating that CD90– HSCs contribute to a substantial fraction of the severe combined immunodeficient mouse-repopulating cell (SRC) pool in mPB HSPCs (Figure 1G). CD90 was also expressed on 20%–30% of CD34+CD38+ progenitors, correlated with lower CD38 expression, and defined a population of short-term repopulating HSPCs that showed kinetics similar to CD38low cells.
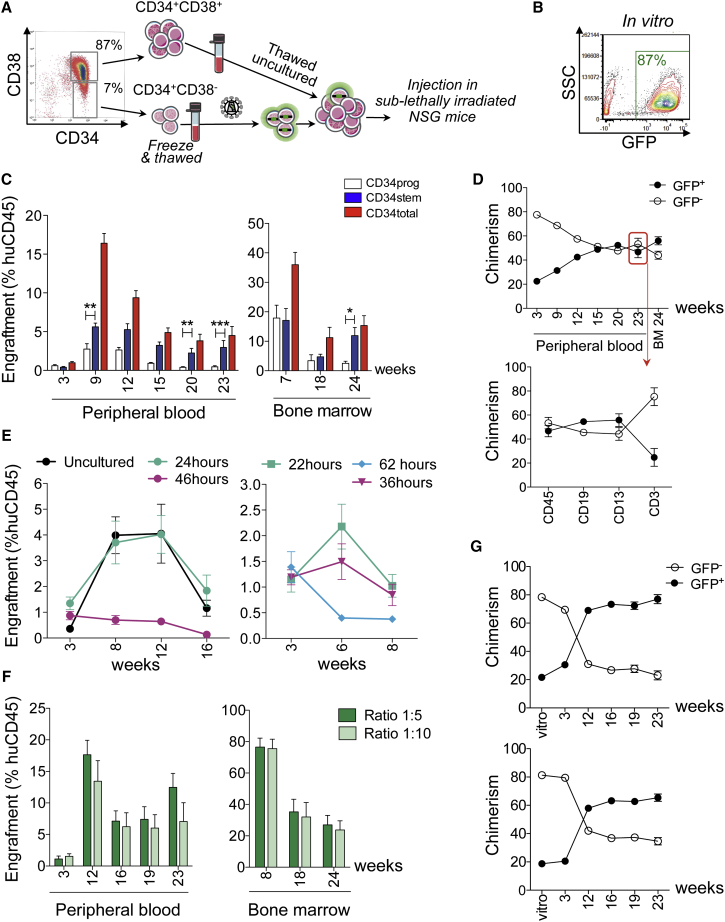
A Gene Therapy Protocol Based on Transducing Purified HSCs
Our modeling suggested that CD34+CD38− cells could substitute CD34+ cells currently used in gene therapy trials when long-term correction of a genetic defect is the ultimate goal. However, CD38int cells may be critical for timely hematopoietic reconstitution following myeloablative conditioning. We therefore simulated a clinical scenario addressing this potential issue by co-transplanting gene-modified CD34+CD38− (CD34stem) cells with uncultured CD34+CD38+ (CD34prog) cells in our xenograft model (Figure 2A). MPB-derived CD34stem cells were transduced with a GFP-expressing vector under saturating conditions resulting in >85% transduction efficiency in vitro (Figure 2B). Mice received either an ex-vivo-modified CD34stem graft, an uncultured CD34prog graft, or a total CD34+ (CD34total) graft re-assembled from the aforementioned two components (CD34stem:CD34prog ratio 1:8). Surprisingly, we found that the CD34prog fraction persisted longer and even retained some long-term repopulating potential. Human cell chimerism of the re-assembled sample was approximately the sum of the CD34stem and CD34prog groups (Figure 2C) and GFP+ cell chimerism in the re-assembled graft stabilized around 50% in all lineages except T cells, where the CD34prog contribution was higher (Figure 2D). This result is in contrast to the experiments described in Figure 1, where similar sorting gates and transduction conditions have been used, except for the transplantation of cultured versus uncultured CD34prog cells.
Figure 2.
Co-transplantation of Gene-Modified, Long-Term Repopulating Cells with Uncultured Short-Term Progenitors
(A) Batches of CD34+CD38+ and CD34+CD38− cells were generated and cryopreserved. As shown in the scheme, CD34+CD38− (CD34stem) cells were LV transduced and xenotransplanted with or without uncultured CD34+CD38+ (CD34prog) cells.
(B) Representative transduction efficiency of CD34+CD38− cells, as measured in the myeloid progeny after 14 days of culture.
(C) Human CD45+ cell engraftment in PB and BM following transplantation of 50,000 GFP LV-transduced CD34stem cells (46 hr culture protocol; n = 5 mice), 350,000 uncultured CD34prog cells (n = 5 mice), or a mix of both (CD34total cells, stem:prog ratio 1:8; n = 6 mice). Significant differences with respect to the CD34stem group are shown (two-way ANOVA with Bonferroni's multiple comparison test).
(D) Top: GFP+ and GFP− cell chimerism in PB and BM within the human CD45+ cell compartment following transplantation of CD34total cells. Red arrow: GFP+/GFP− cell chimerism in CD19+ B cells, CD13+ myeloid cells, and CD3+ T cells (PB, 23 weeks post-transplant).
(E) Left: mice were xenotransplanted with CD34+CD38+ cells that were uncultured (n = 4 mice), or cultured for 24 hr (n = 5 mice) or 46 hr (n = 4 mice) under standard conditions. Human CD45+ cell engraftment in the PB is shown. Right (replicate experiment): PB engraftment of CD34+CD38+ cells cultured for 22 hr (n = 4 mice), 36 hr (n = 6 mice), or 62 hr (n = 3).
(F) Mice were xenotransplanted with CD34total cells composed of 50,000 GFP LV-transduced CD34stem cells (24 hr ex vivo protocol, no IL-3) and 200,000 uncultured CD34prog cells (ratio 1:5, n = 5 mice) or 450,000 uncultured CD34prog cells (ratio 1:10, n = 6 mice). Human CD45+ cell engraftment in PB and BM is shown.
(G) GFP+ and GFP− cell chimerism of the transplanted CD34total cells (in vitro) or the resulting human CD45+ cell graft in the PB at the indicated time points post-transplant for the 1:5 (top) or 1:10 (bottom) stem:prog ratio.
Error bars represent SEM.
These data suggest that fresh CD34prog cells (likely, within the CD38low cell fraction) contain some long-term repopulating capacity, which is lost during 2 days of ex vivo culture. To directly test this hypothesis, we xenotransplanted mPB CD34prog cells (the same donor and sorted aliquot as in the experiment shown in Figures 2B–2D) that were either uncultured, or cultured and transduced with a GFP LV during a 24 hr or a 48 hr ex vivo protocol. While engraftment at 3 weeks was similar or slightly better for the cultured cells, the 46 hr ex vivo group showed no short- or long-term engraftment thereafter, at variance to the uncultured group (Figure 2E). Interestingly, the shorter 24 hr ex vivo culture time restored engraftment potential to similar levels seen in uncultured cells. We repeated the experiment with CD38prog cells from a different donor, confirming that short-term engraftment potential starts to decrease after 36 hr of culture (Figure 2E). These findings provide a strong rationale to reduce ex vivo culture times to improve progenitor cell potency in gene therapy products.
We thus reasoned that CD34stem HSPCs might better compete with uncultured progenitor cells when their ex vivo culture is reduced to 24 hr. In addition, we eliminated interleukin-3 (IL-3) from the culture medium, given that it stimulates progenitors rather than HSCs and has recently been implicated in accelerated loss of short-term repopulation potential (Miller et al., 2016). Using mPB CD34stem and CD34prog aliquots from the same donor and a sorting strategy as in the experiment shown in Figures 2B–2D, we co-transplanted mPB CD34stem cells transduced with GFP LV according to the optimized and shortened ex vivo protocol with uncultured CD34prog cells mixed in a 1:5 ratio or a 1:10 ratio. The fraction of GFP+ cells scored in vivo was used as a surrogate marker for CD34+CD38−-derived hematopoiesis, assuming that most CD34stem cells were transduced even under the shortened 24 hr ex vivo culture protocol. Engraftment levels were similar between the 1:5 and 1:10 groups (Figure 2F). Importantly, up to 80% and 70% of hematopoietic progeny were stably gene marked in vivo, respectively, and equilibrium was reached between 3 and 4 months post-transplantation (Figure 2G). We conclude that shortening the culture time of CD34+CD38− cells to 24 hr in an IL-3-free medium significantly enhanced progenitor fitness within the gene-modified CD34+CD38− cells allowing a contribution of up to 80% of the long-term graft even when large amounts of uncultured CD34+CD38+ progenitor cells were co-infused.
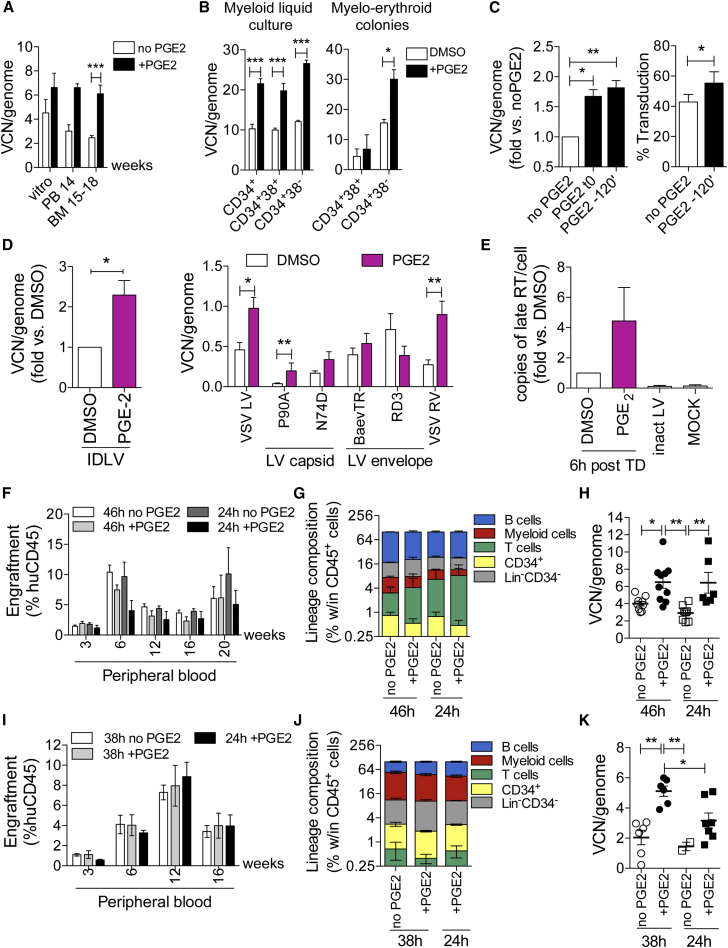
Robust HSC Gene Transfer Using Short Culture Time and Prostaglandin E2
To date, most clinical protocols employ culture times of more than 60 hr and multiple exposures to LV (in general, two transduction cycles). Therefore, a significant challenge when implementing shorter transduction protocols in the clinic is to achieve sufficiently high levels of gene transfer with large-scale LV preparations produced under good manufacturing practice (GMP). Unexpectedly, we found that the more primitive CD34+CD38− cells were transduced to almost 2-fold-higher vector copy number per genome (VCN) than the more committed counterparts after a single LV exposure (Figure S4). This phenomenon may facilitate gene transfer when manipulating more purified HSC populations.
Furthermore, we sought to enhance transduction by small-molecule compounds. While employing 16,16-dimethyl prostaglandin E2 (PGE2) as an anti-apoptotic agent in ex vivo HSC gene-editing protocols, we noted that it increased gene-targeting efficiency (Genovese et al., 2014). We hypothesized that PGE2 may also increase transduction by integrating LV. Indeed, pre-stimulating CB CD34+ HSPCs with 10 μM PGE2 before transduction increased VCN in the progeny ∼1.5-fold in vitro, an increase that was maintained or increased after xenotransplantation (Figure 3A). PGE2 also enhanced transduction of CD34+ cells from BM (Figure 3B), including the more primitive CD34+CD38− subset, and mPB, whereby the timing of PGE2 stimulation was flexible (Figure 3C). At non-saturating LV doses, PGE2 also increased the fraction of transduced cells, not only VCN (Figure 3C). We then tested whether PGE2 increased transduction by vector variants to determine a mechanism of action. Gene transfer was increased when using vesicular stomatitis virus G protein (VSV-G)-pseudotyped, integrase-deficient LV, or gamma-retroviral vectors, and also in the case of HIV1 capsid mutants that reduce interaction with cyclophilin A (P90A) or CPSF6 (N74) during uncoating (Figure 3D). On the other hand, when pseudotyping LVs with alternative, non-endocytosis-dependent envelopes, we could not appreciate a significant impact of PGE2 on transduction. Quantification of reversely transcribed vector DNA intermediates 6 hr post-transduction further indicated that PGE2 acted during the early steps of transduction (Figure 3E).
Figure 3.
Prostaglandin E2 Enables Efficient HSC Transduction with Shortened Ex Vivo Protocols
(A) CB CD34+ cells were transduced with LVs in the presence or absence of 10 μM PGE2. VCN was measured in the progeny after >7 days culture (n = 5) or in the human CD45+ cell xenograft harvested from the PB (n = 2 experiments, blood from individual mice was pooled) or BM (2 experiments, n = 13 mice in the no PGE2 group, n = 10 mice in PGE2 group, statistics by Student's t test).
(B) BM CD34+ subpopulations (n = 3 donors) were transduced with GFP LV (MOI = 100) + 10 μM PGE2 or DMSO, and VCN was measured in the myeloid progeny after 14 days of culture or on myelo-erythroid colonies obtained from clonogenic assay. Statistics by two-way ANOVA with Bonferroni's multiple comparison test.
(C) mPB CD34+ cells (n = 8 donors) were transduced with GFP LV (38 hr protocol) ± 10 μM PGE2 added at the beginning of culture (t0) or during pre-stimulation, 120 min before LV addition (−120′). Transduction was evaluated after 14 days in culture. Left: VCN relative to the no PGE2 group (statistics by Wilcoxon signed rank test). Right: transduction efficiency measured by flow cytometry (n = 6) (statistics by Student's t test).
(D) mPB CD34+ cells (n = 3 donors, with two replicates each) were transduced with GFP-expressing LV variants after adding PGE2 or DMSO (−120′). IDLV, integrase-deficient, VSV-G pseudotyped LV; VSV LV, integration-competent, VSV-G-pseudotyped LV; P90A and N74D, VSV-G-pseudotyped LV with capsid mutants; BaEV-TR and RD114-TR, integration-competent LV pseudotyped with the BaEV-TR and RD114-TR envelopes, respectively. VCN were measured by specific droplet digital PCR assays. Statistics were performed by Mann-Whitney test.
(E) Quantification of late reverse-transcription DNA intermediates (late-RT) in mPB CD34+ cells (n = 6 donors), 6 hr after transduction (TD) in PGE2 or DMSO.
(F–H) mPB CD34+ cells were transduced with gp91phox-expressing LVs (MOI = 100) using a 24 or 46 hr ex vivo protocol ± 10 μM PGE2, and xenotransplanted with the day 0 equivalent of 500,000 cells (n = 6–9 mice/group). (F) Human CD45+ cell engraftment in the PB. (G) Lineage composition of the human CD45+ cell graft in the BM at 20 weeks post-xenotransplantation. B cells, CD19+; myeloid cells: CD33+; T cells: CD3+; CD34+: HSPCs; Lin−CD34−: CD19− CD33−CD3−CD34− cells. (H) VCN in the human graft recovered from the BM at 20 weeks post-xenotransplantation. Statistics by one-way ANOVA with Bonferroni's multiple comparison test.
(I–K) mPB CD34+CD38− cells were transduced with purified Globe LV (MOI = 100) using a 24 or 38 hr ex vivo protocol ±10 μM PGE2, and xenotransplanted with the day 0 equivalent of 50,000 cells (experiment 1: 38 hr no PGE2, n = 4; 38 hr + PGE2, n = 4; 24 hr + PGE2, n = 5; experiment 2: 38 hr no PGE2, n = 4; 38 hr + PGE2, n = 4; 24 hr no PGE2, n = 5; 24 hr + PGE2, n = 4). (I) Human CD45+ cell engraftment in the PB. (J) Lineage composition of the human CD45+ cell graft in the BM at 20 weeks post-xenotransplantation (representative mice from experiment 1). (K) VCN in the human graft recovered from the BM at 18 weeks (experiment 2) or 20 weeks (experiment 1) post-xenotransplantation. Statistics by one-way ANOVA with Bonferroni's multiple comparison test.
Error bars represent SEM. See also Figure S4.
We then performed in vivo repopulation assays on CD34+ mPB cells transduced in the presence or absence of PGE2 using either a 46 hr or an ultra-short 24 hr ex vivo culture protocol. Despite injecting fewer cells in the 24 hr protocol groups (the yield of 500,000 plated CD34+ cells was lower after 24 hr with respect to 46 hr, because of less proliferation during the shorter ex vivo culture), huCD45+ cell engraftment was equivalent to the 46 hr protocol (Figure 3F). PGE2 treatment had no overall effect on ex vivo proliferation, colony-forming potential (Figure S4D), or engraftment levels (Figure 3F), nor did it alter the lineage composition of the human graft (Figure 3G). At the experimental endpoint (20–24 weeks post-transplant), we noted significantly higher VCN in the PGE2 groups (Figure 3H).
Next, we transduced CD34+CD38− mPB cells with a purified LV expressing a therapeutic gene. We tested the impact of PGE2 on gene transfer efficiency in the context of a short 38 hr or an ultra-short 24 hr ex vivo culture protocol. In vitro results of VCN in liquid cultures established from CD34+CD38− cells showed that exposure to PGE2 doubled VCN (Figure S4E). Following transplantation, we detected no statistically significant differences in engraftment or graft composition (Figures 3I and 3J). Importantly, differences in VCN were maintained in the human graft at 18–20 weeks post-transplant, confirming that PGE2 increased gene transfer into long-term repopulating cells (Figure 3K).
Taken together, these results suggest that a minimal ex vivo manipulation protocol, as short as 24 hr, can achieve substantial levels of gene transfer by therapeutic LVs in human HSCs from clinically relevant sources. The effect of PGE2 was particularly robust for the 38 hr protocol in CD34+CD38− cells, motivating its clinical implementation.
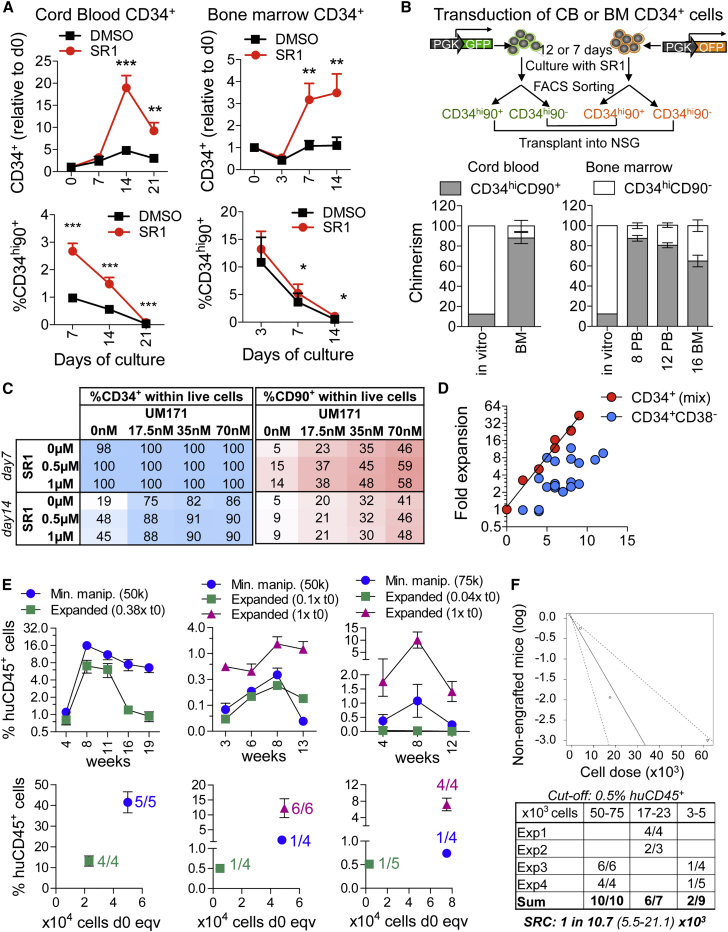
Ex Vivo Expansion of CD34+CD38− Cells from mPB in the Presence of Pyrimidoindole Derivatives
Based on our finding that short-term engrafting cells are particularly sensitive to ex vivo culture, we hypothesized that HSC expansion protocols could be more suitably applied to highly purified HSC fractions. First, we set out to functionally validate surface markers that prospectively identify SRC after 1–2 weeks of expansion culture. BM or CB CD34+ cells were cultured in the presence or absence of the arylhydrocarbon receptor antagonist StemRegenin 1 (SR1) (Boitano et al., 2010). Serial flow cytometric analysis indicated that CD38 expression was rapidly lost in culture, while a fraction of cells maintained a CD34highCD90+ phenotype. This fraction was higher when cells were cultured with SR1, especially for CB (Figure 4A). Peak expansion of CD34highCD90+ cells occurred around 2 weeks for CB and 1 week for BM. In a separate experiment, we transduced 50% of CB or BM CD34+ cells with a GFP-expressing LV, while the other 50% were transduced with an OFP-expressing LV. Both GFP+ and OFP+ cells were expanded for 12 days (CB) or 7 days (BM) in the presence of SR1. To test whether CD90 expression could be useful to enrich for engrafting cells following prolonged ex vivo culture, we sorted the cultures into CD34highCD90+ or CD34highCD90– fractions, mixed the GFP+CD90+ cells with the OFP+CD90– cells and vice versa without altering their original ratio (CD90+ cells constituted 10%–20% of the CD34high cells or 1%–5% of the total cells) and xenotransplanted them (Figure 4B). Both for CB and BM, most long-term engraftment derived from the CD34highCD90+ fraction.
Figure 4.
Ex Vivo Expansion of Gene-Modified HSCs Supported by Small-Molecule Compounds
(A) LV-transduced CB (left panel, n = 6 donors) or BM (right panel, n = 5 donors) CD34+ HSPCs were expanded ex vivo in the presence of vehicle (DMSO) or StemRegenin 1 (SR1, 1 μM), as described by Boitano et al. (2010). The fraction of CD34highCD90+ cells in the culture at the indicated number of days is shown (statistics by matched two-way ANOVA with Bonferroni's multiple comparison test).
(B) CB or BM CD34+ cells were divided into equal fractions and transduced with GFP- or OFP- expressing LVs. GFP+ and OFP+ cells were expanded for 12 days (CB) and 7 days (BM) in the presence of SR1, followed by sorting of each group into a CD34highCD90+ and CD34+CD90− fractions. Each GFP+ fraction was then re-combined with the complementary OFP+ CD34+ cell fraction and xenotransplanted. The fraction of CD34hiCD90+ cells in vitro after re-combining, as well as the in vivo output deriving from this fraction tracked by expression of the associated FP (CB CD34+ cells: BM at 20 weeks post-xenografting; BM CD34+ cells: PB and BM up to 16 weeks) are shown. CB, n = 6 mice; BM, n = 6 mice.
(C) mPB CD34+CD38− cells were expanded ex vivo in the presence of increasing concentrations of SR1, UM171 or combinations of both. Reported are the percentages of CD34+ and CD90+ cells in the culture at 7 and 14 days.
(D) Growth kinetics of total CD34+ versus CD34+CD38− mPB cells expanded in the presence of UM171 (35 nM).
(E) mPB CD34+CD38− cells were LV transduced and xenotransplanted after <36 hr ex vivo (minimally manipulated cells, 50,000–75,000 cells/mouse) or after an additional 7–8 days of expansion in 35 nM UM171. Injected cell dose is indicated relative to the minimally manipulated cell dose (t0 equivalent). Upper graphs show the percentage of huCD45+ cells in the PB. Lower graphs show BM engraftment relative to administered cell dose (t0 cell equivalents) at the experimental endpoint, 20 weeks (left) or 13–14 weeks (middle and right graphs) post-transplant. The number of engrafted mice (>0.5% huCD45+ and both myeloid and lymphoid reconstitution in BM at the endpoint) is indicated.
(F) Estimation of SRC frequency in ex-vivo-expanded CD34+CD38− cells by extreme limiting dilution statistics, considering the t0 cell dose equivalents (62,500–20,000–4,000) transplanted in four independent experiments (Exp).
Error bars represent SEM.
Using the CD34 and CD90 markers as surrogates for SRC, we next screened different expansion conditions for mPB CD34+CD38− cells by varying the concentrations of SR1 and/or the pyrimidoindole derivative UM171 (Fares et al., 2014). Notably, CD34+CD38− cells proliferated little during the first week and homogeneously maintained CD34 expression. UM171 substantially increased the fraction and number of CD90+ cells over control cultures or cells cultured with SR1, while combination of UM171 and SR1 had additive effects during the first week of culture (Figure 4C). We then compared the growth characteristics of transduced CD34+ and CD34+CD38− mPB cells during expansion culture (Figure 4D). CD34+CD38− cells generally showed little growth in the first days of ex vivo culture and then expanded at variable rates, which differed by donor and experiment. On the other hand, CD34+ cells steadily duplicated every 2 days, likely reflecting the progenitors responding to cytokine stimulation. This overgrowth of progenitors rapidly drove up culture volumes while keeping the concentration of CD34+ cells stable, highlighting a substantial practical advantage of the CD34+CD38− cultures. To functionally test the repopulation potential of UM171-expanded, genetically engineered HSPCs, we xenotransplanted LV-transduced CD34+CD38− cells either after a minimal, 24–36 hr ex vivo culture (minimally manipulated cells) or after an additional 7–8 days of ex vivo expansion (Figure 4E). When matching transplanted cell number according to the same “t0 equivalent” (1× t0), we found higher engraftment in the ex vivo expanded sample (Figure 4E, pink dots). When the transplanted cell dose was matched according to the post-culture counts, ex vivo expanded cells showed lower engraftment compared with minimally manipulated cells, consistent with the 3- to 25-fold lower “t0 equivalent” cell dose (0.38–0.04× t0) injected (Figure 4E, green dots). To estimate the frequency of SRC in UM171-expanded CD34+CD38− HSPCs, we performed limiting-dilution statistics on the “t0 equivalent” cell doses that were transplanted in four replicate experiments (Figure 4F). Estimated SRC frequency was 1 in 10,700 (95% confidence interval: 5,500–21,100), which compares with a recently reported SRC frequency of ∼1 in 141,203 in uncultured CD34+ cells from G-CSF-mPB (Lidonnici et al., 2016). Taken together, these data indicate that our protocol allows ex vivo expansion of genetically engineered mPB CD34+CD38− cells with SCID-repopulating potential and warrants further protocol optimization for clinical application.
Discussion
Transplantation of genetically engineered, autologous HSPCs is emerging as a less risky and potentially more efficacious alternative to allogeneic transplantation for a series of non-malignant indications (Naldini, 2015). To fully harness the advantages of gene therapy, genetic engineering of HSPCs must be developed into a standardized and sustainable method. To reach this objective, key challenges include improving LV transduction, minimizing the negative impact of ex vivo culture to ensure faster and more polyclonal long-term reconstitution, and alleviating the safety concerns related to insertional mutagenesis. Here we developed a series of readily translatable strategies that overcome these hurdles and help to establish gene therapy as a widely available standard treatment.
We revealed the PGE2-enhanced transduction of human HSPCs by VSV-G-pseudotyped LV, possibly by acting on the endocytosis-dependent entry pathway. Applying PGE2 makes shorter ex vivo manipulation protocols that feature a single transduction cycle clinically viable, mitigating the negative effect of prolonged culture on progenitor cell engraftment and allowing to double the number of patients that can be treated with a given vector batch with respect to current clinical standards. Importantly, the enhancing effect of PGE2 on LV transduction has recently been reported by an independent group (Heffner et al., 2016). In contrast to other pharmacological interventions that enhance transduction but may also have broader effects on HSC biology and/or cause toxicity (Wang et al., 2014, Petrillo et al., 2015), PGE2 was non-toxic, did not change the biological properties of the cells, and has already been safely employed in an ex vivo setting to increase CB engraftment in patients (Cutler et al., 2013). We did not note a significant increase in engraftment levels in the PGE2 groups, as could be expected from published data (Goessling et al., 2011). Further studies on diverse cell sources employing ultra-short ex vivo protocols are warranted to understand whether the promoting effects of PGE2 on LV transduction and engraftment capacity are functionally linked to a common mechanism and whether both effects can be exploited contemporaneously. The shortened PGE2 protocol can be readily applied to current ex vivo gene therapy trials and should translate clinically into accelerated hematologic recovery.
We provide evidence here that CD34+CD38− cells transduce at higher levels than total CD34+ cells, consistent with a recent report (Baldwin et al., 2015). In vitro, the effect was most robust (1) when cell populations were sorted before transduction (Figure S4C), (2) when saturating vector doses were used (Figure S4B), and (3) when PGE2 was employed (Figure 3B). We hypothesize that the lack of cell division of CD34+CD38− cells during the first days of culture (Figure 4F) may give more time for infecting LV to complete integration before DNA replication, thus transmitting a copy of each provirus to both daughter cells, whereas the rapidly dividing CD38+ progenitors may randomly sort the LV pre-integration complexes between the two daughter cells. Considering that PGE2 relieves an early transduction block, applying it to purified CD34+CD38− cells may provide added benefits in terms of gene transfer efficiency. Robust gene transfer into HSCs may allow reducing the intensity of the conditioning regimen and implementing non-genotoxic and stem cell-specific conditioning strategies (Palchaudhuri et al., 2016). Regarding safety, avoiding the infusion of CD38+ progenitors carrying semi-random LV integrations would reduce the integration load 10-fold, thereby decreasing the chances of gain-of-function events due to insertional mutagenesis, which may originate from immortalized progenitor cells (Cavazzana-Calvo et al., 2010, Stein et al., 2010, Braun et al., 2014).
We argue that gene therapy based on transduced, purified CD34+CD38− cells is clinically feasible and offers advantages over alternative strategies that have previously been employed in clinical trials to obtain HSC-enriched cell populations, including positive selection for CD133+ cells (Gordon et al., 2003) or CD34+CD90+ cells (Michallet et al., 2000, Negrin et al., 2000). Combining a negative (CD38) with a positive (CD34) selection marker allows using a sequential, bead-based selection procedure that can be made GMP compliant and implemented in centers that already possess standard cell separation equipment. The 10-fold gain in HSC purity with respect to CD34+ cells is higher than what can be achieved with the CD133+ (2×) or the CD34+CD90+ (up to 5×) selection strategies. Furthermore, we show that almost all long-term repopulation activity is captured within the CD34+CD38− fraction, while, in agreement with CB data (Notta et al., 2011), substantial numbers of HSCs are contained within the CD34+CD90– fraction of mPB, which would be discarded in the case of a CD34+CD90+ selection. While more stringent gating on CD90high cells may increase HSC purity, it would at the same time aggravate the loss of CD90–/low HSCs.
Our functional analyses showed that CD38 expression inversely correlated with time of onset and persistence of the graft, confirming and extending published results obtained in xenograft models (Glimm et al., 2001, Kerre et al., 2001, Mazurier et al., 2003). Interestingly, analysis of clonal dynamics by LV integration sites in a clinical gene therapy trial pointed to two distinct waves of repopulation, switching between the third and sixth month post-transplant, which may correspond to the waves generated by CD34+CD38int/+ and CD34+CD38− cells, respectively (Biasco et al., 2015). Transplantation of genetically engineered CD34+CD38− cells may repopulate patients following the kinetics of the second wave resulting in a fully established transgenic hematopoiesis beyond 3 months after transplantation. While this may be suboptimal for genetic diseases with an urgent transplant indication such as PIDs, it may be acceptable for chronic conditions such as hemoglobinopathies. Considering the timing of repopulation by CD34+CD38− cells, co-infusion of progenitor cells is advisable when a fully myeloablative conditioning regimen is applied to facilitate short-term engraftment. These short-term engrafting progenitors can be conveniently obtained from the CD38int/+ fraction left over from the negative selection step and cryopreserved as a whole, without further ex vivo manipulation. Infusing uncultured progenitors may be particularly beneficial for hematologic recovery, considering their selective vulnerability to ex vivo culture. Low CD38 expression on CB HSPCs has been associated with stem cell activation and recruitment into the G1 phase of the cell cycle (McKenzie et al., 2007). Unbalanced stimulation by high doses of cytokines may irreversibly push these cells to differentiate resulting in a loss of self-renewal potential and premature exhaustion in vivo.
On the contrary, the more primitive CD34+CD38− mPB cells appeared to be more tolerant to ex vivo culture. Using the shortened transduction protocol, we effectively alleviated competition from a 10-fold excess of uncultured progenitors. Moreover, we demonstrate that, with the help of the pyrimidoindole derivative UM171 (Fares et al., 2014), the culture time of mPB CD34+CD38− cells can extend beyond 7 days, with evidence for SRC expansion. We foresee numerous applications for ex vivo expansion of postnatally derived HSCs in the gene therapy field. This technology can overcome disease- or patient-specific cell shortages, allow more complex genetic manipulations such as serial transductions by multiple vectors, possibly with selection of engineered cells, and enable therapeutic application of emerging gene-editing technologies (Naldini, 2015). The use of purified CD34+CD38− cells and the associated reduction in culture volumes and vector amount promises substantial cost savings and quality improvements, also considering that differentiating progenitor and mature cell populations may give rise to inhibitory feedback and differentiation signaling exhausting the long-term repopulating potential of the more primitive cells in the culture (Csaszar et al., 2012).
In conclusion, our data support the stepwise introduction of incremental improvements in the ex vivo HSPC engineering process into clinical testing, ultimately fulfilling the promise of gene therapy to the community.
Experimental Procedures
Mice
NOD.Cg-PrkdcscidIL2rgtm1Wjl/SzJ (NSG) mice were acquired from the Jackson Laboratory. All animal procedures were performed according to protocols approved by the Institutional Animal Care and Use Committee (IACUC 618) and communicated to the Ministry of Health and local authorities according to the Italian law. Eight week old mice were sublethally irradiated (200–220 cGy) and transplanted with human HSPCs by tail vein injection. All mice were randomized into different HSC transplantation groups. On the basis of a standard backward sample size calculation, we transplanted at least three to ten mice per condition and performed at least two independent experiments to obtain a sufficient number of mice to perform statistical analysis. Human cell engraftment was blindly assessed by serial bleeding or BM aspirates, as described in the Supplemental Experimental Procedures.
Procurement, Culture, and Transduction of Human HSPCs
Human CB, BM, or mPB was purchased from commercial sources (Lonza, HemaCare, or All Cells). CD34+ or CD34+CD38− cells were pre-stimulated in serum-free medium supported with early-acting human cytokines (SCF, FLT3L, or TPO with or without IL-3 or IL-6), and transduced with concentrated LV at an MOI of 100, unless otherwise indicated. Where indicated, 10 μM 16,16-dimethyl-prostaglandin E2 (Cayman Chemical) was added before LV transduction. Additional details can be found in the Supplemental Experimental Procedures.
Cell Sorting and Flow Cytometry
Sorting for CD34+ cells (and CD38− cells, where indicated) was performed by magnetic beads (Miltenyi). Fluorescence-activated cell sorting for CD38 and CD90 subpopulations was performed on a MoFlo XDP sorter (Beckman Coulter). Analytical flow cytometry was performed on a FACSCanto II or LSR II Fortessa instrument (BD Bioscience). Details on protocols and reagents can be found in the Supplemental Experimental Procedures.
Ex Vivo HSPC Expansion
Expansion cultures were set up in serum-free medium (StemSpan, STEMCELL Technologies or StemMacs, Miltenyi) containing, unless otherwise indicated, 100 ng/mL SCF, 100 ng/mL FLT3L, 50 ng/mL TPO, 50 ng/mL IL-6, 35 nM UM171 (STEMCELL Technologies), and/or 1 μM SR1 (BioVision Technologies). Starting cell density was 1 × 105 cells/mL, and fresh medium was manually added as needed, to keep cell concentration always below 1 × 106 cells/mL. Cultures were kept at 37°C, 5% CO2 under normoxia.
LV Production, Titration, and Molecular Analysis of Gene Transfer Efficiency
Purified vectors (Globe LV, some batches of PGK.GFP LV) were produced and titered by MolMed, according to the GMP process employed in our clinical trials (Biffi et al., 2013, Aiuti et al., 2013). Lab-grade vectors were produced and titered on 293T cells according to standard lab protocols, as described previously. Molecular quantification of gene transfer efficiency was performed using specific qPCR assays, as detailed in the Supplemental Experimental Procedures.
Statistical Analysis
In all studies, values are expressed as means ± SEM, unless otherwise indicated. Statistical analyses were performed by Mann-Whitney test, Student's t test, Wilcoxon signed rank test, or ANOVA test as indicated. Percentages were converted into log odds for statistical analysis. Significance levels are coded as follows throughout the manuscript: ∗p < 0.05, ∗∗p < 0.01, ∗∗∗p < 0.001.
Author Contributions
E.Z. performed experiments, analyzed the data, and contributed to writing the manuscript. G.D., F.E.B., C.P., and M.R.L. performed experiments. A.K.R. provided intellectual input and supervised C.P. A.A. and G.F. provided intellectual input, reagents, and protocols. L.N. supported the project, provided research infrastructure, gave intellectual input, and edited the manuscript. B.G. designed and coordinated the research, analyzed the data, and wrote the manuscript.
Acknowledgments
We thank Oriana Meo, Matteo Maria Naldini, Andrea Cosentino, Cheruku Patali Shikhi, Lucia Sergi Sergi, Ivan Cuccovillo, and Tiziana Plati for help with experiments; C. Villa, E. Canonico, M. Romanó, M. Zambelli, and C. Parisi for help with sorting and cell manipulation; MolMed S.p.A. for providing the lentiviral vector pseudotyped with RD114-TR envelope; François-Loic Cosset from Inserm-ENS Lyon, France, for the BaEV-TR envelope construct; Guy Sauvageau for friendly discussions on HSC expansion. This research was supported by grants from the Telethon Foundation (TELE16-C1 to B.G., TELE16-C3 to A.K.R.), the Telethon-GSK Alliance (AGSK-HSC), the Italian Ministry of Health (NET-2011-02350069) and a John Goldman Clinical Research Fellowship from the European Hematology Association to B.G.
Published: March 16, 2017
Footnotes
Supplemental Information includes Supplemental Experimental Procedures, four figures, and one table and can be found with this article online at http://dx.doi.org/10.1016/j.stemcr.2017.02.010.
Supplemental Information
References
- Aiuti A., Biasco L., Scaramuzza S., Ferrua F., Cicalese M.P., Baricordi C., Dionisio F., Calabria A., Giannelli S., Castiello M.C. Lentiviral hematopoietic stem cell gene therapy in patients with Wiskott-Aldrich syndrome. Science. 2013;341:1233151. doi: 10.1126/science.1233151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin K., Urbinati F., Romero Z., Campo-Fernandez B., Kaufman M.L., Cooper A.R., Maziuk K., Hollis R.P., Kohn D.B. Enrichment of human hematopoietic stem/progenitor cells facilitates transduction for stem cell gene therapy. Stem Cells. 2015;33:1532–1542. doi: 10.1002/stem.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biasco L., Pellin D., Scala S., Dionisio F., Basso-Ricci L., Leonardelli L., Scaramuzza S., Baricordi C., Ferrua F., Cicalese M.P. In vivo tracking of human hematopoiesis reveals patterns of clonal dynamics during early and steady-state reconstitution phases. Cell Stem Cell. 2015;19:107–119. doi: 10.1016/j.stem.2016.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biffi A., Montini E., Lorioli L., Cesani M., Fumagalli F., Plati T., Baldoli C., Martino S., Calabria A., Canale S. Lentiviral hematopoietic stem cell gene therapy benefits metachromatic leukodystrophy. Science. 2013;341:1233158. doi: 10.1126/science.1233158. [DOI] [PubMed] [Google Scholar]
- Boitano A.E.A., Wang J., Romeo R., Bouchez L.C., Parker A.E., Sutton S.E., Walker J.R., Flaveny C.A., Perdew G.H., Denison M.S. Aryl hydrocarbon receptor antagonists promote the expansion of human hematopoietic stem cells. Science. 2010;329:1345–1348. doi: 10.1126/science.1191536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun C.J., Boztug K., Paruzynski A., Witzel M., Schwarzer A., Rothe M., Modlich U., Beier R., Göhring G., Steinemann D. Gene therapy for Wiskott-Aldrich syndrome – long-term efficacy and genotoxicity. Sci. Transl. Med. 2014;6:227ra33. doi: 10.1126/scitranslmed.3007280. [DOI] [PubMed] [Google Scholar]
- Cartier N., Hacein-Bey-Abina S., Bartholomae C.C., Veres G., Schmidt M., Kutschera I., Vidaud M., Abel U., Dal-Cortivo L., Caccavelli L. Hematopoietic stem cell gene therapy with a lentiviral vector in x-linked adrenoleukodystrophy. Science. 2009;326:818–823. doi: 10.1126/science.1171242. [DOI] [PubMed] [Google Scholar]
- Cavazzana-Calvo M., Payen E., Negre O., Wang G., Hehir K., Fusil F., Down J., Denaro M., Brady T., Westerman K. Transfusion independence and HMGA2 activation after gene therapy of human β-thalassaemia. Nature. 2010;467:318–322. doi: 10.1038/nature09328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csaszar E., Kirouac D.C., Yu M., Wang W., Qiao W., Cooke M.P., Boitano A.E., Ito C., Zandstra P.W. Rapid expansion of human hematopoietic stem cells by automated control of inhibitory feedback signaling. Cell Stem Cell. 2012;10:218–229. doi: 10.1016/j.stem.2012.01.003. [DOI] [PubMed] [Google Scholar]
- Cutler C., Multani P., Robbins D., Kim H.T., Le T., Hoggatt J., Pelus L.M., Desponts C., Chen Y.B. Prostaglandin-modulated umbilical cord blood hematopoietic stem cell transplantation. Blood. 2013;122:3074–3081. doi: 10.1182/blood-2013-05-503177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fares I., Chagraoui J., Gareau Y., Gingras S., Ruel R., Mayotte N., Csaszar E., Knapp D.J.H.F., Miller P., Ngom M. Cord blood expansion. Pyrimidoindole derivatives are agonists of human hematopoietic stem cell self-renewal. Science. 2014;345:1509–1512. doi: 10.1126/science.1256337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genovese P., Schiroli G., Escobar G., Di Tomaso T., Firrito C., Calabria A., Moi D., Mazzieri R., Bonini C., Holmes M.C. Targeted genome editing in human repopulating haematopoietic stem cells. Nature. 2014;510:235–240. doi: 10.1038/nature13420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glimm H., Oh I.H., Eaves C.J. Human hematopoietic stem cells stimulated to proliferate in vitro lose engraftment potential during their S/G(2)/M transit and do not reenter G(0) Blood. 2000;96:4185–4193. [PubMed] [Google Scholar]
- Glimm H., Eisterer W., Lee K., Cashman J., Holyoake T.L., Nicolini F., Shultz L.D., Von Kalle C., Eaves C.J. Previously undetected human hematopoietic cell populations with short-term repopulating activity selectively engraft NOD/SCID-2 microglobulin-null mice. J. Clin. Invest. 2001;107:199–206. doi: 10.1172/JCI11519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goessling W., Allen R.S., Guan X., Jin P., Uchida N., Dovey M., Harris J.M., Metzger M.E., Bonifacino A.C., Stroncek D. Prostaglandin E2 enhances human cord blood stem cell xenotransplants and shows long-term safety in preclinical nonhuman primate transplant models. Cell Stem Cell. 2011;8:445–458. doi: 10.1016/j.stem.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon P.R., Leimig T., Babarin-Dorner A., Houston J., Holladay M., Mueller I., Geiger T., Handgretinger R. Large-scale isolation of CD133+ progenitor cells from G-CSF mobilized peripheral blood stem cells. Bone Marrow Transpl. 2003;31:17–22. doi: 10.1038/sj.bmt.1703792. [DOI] [PubMed] [Google Scholar]
- Hacein-Bey Abina S., Gaspar H.B., Blondeau J., Caccavelli L., Charrier S., Buckland K., Picard C., Six E., Himoudi N., Gilmour K. Outcomes following gene therapy in patients with severe Wiskott-Aldrich syndrome. JAMA. 2015;313:1550–1563. doi: 10.1001/jama.2015.3253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heffner G., Bonner M., Campbell D., Christiansen L., Pierciey F.J., Zhang W., Lewis G., Smurnyy Y., Hamel A., Shah S. PGE2 increases lentiviral vector transduction efficiency of human HSC. Mol. Ther. 2016;24(S1):229. doi: 10.1016/j.ymthe.2017.09.025. (abstract) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kallinikou K., Anjos-Afonso F., Blundell M.P., Ings S.J., Watts M.J., Thrasher A.J., Linch D.C., Bonnet D., Yong K.L. Engraftment defect of cytokine-cultured adult human mobilized CD34+ cells is related to reduced adhesion to bone marrow niche elements. Br. J. Haematol. 2012;158:778–787. doi: 10.1111/j.1365-2141.2012.09219.x. [DOI] [PubMed] [Google Scholar]
- Kerre T.C., De Smet G., De Smedt M., Offner F., De Bosscher J., Plum J., Vandekerckhove B. Both CD34+38+ and CD34+38− cells home specifically to the bone marrow of NOD/LtSZ scid/scid mice but show different kinetics in expansion. J. Immunol. 2001;167:3692–3698. doi: 10.4049/jimmunol.167.7.3692. [DOI] [PubMed] [Google Scholar]
- Kiernan J., Damien P., Monaghan M., Shorr R., McIntyre L., Fergusson D., Tinmouth A., Allan D. Clinical studies of ex vivo expansion to accelerate engraftment after umbilical cord blood transplantation: a systematic review. Transfus. Med. Rev. 2016 doi: 10.1016/j.tmrv.2016.12.004. [DOI] [PubMed] [Google Scholar]
- Larochelle A., Gillette J.M., Desmond R., Ichwan B., Cantilena A., Cerf A., Barrett A.J., Wayne A.S., Lippincott-Schwartz J., Dunbar C.E. Bone marrow homing and engraftment of human hematopoietic stem and progenitor cells is mediated by a polarized membrane domain. Blood. 2012;119:1848–1855. doi: 10.1182/blood-2011-08-371583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lidonnici M.R., Aprile A., Frittoli M.C., Mandelli G., Paleari Y., Spinelli A., Gentner B., Zambelli M., Parisi C., Bellio L. Plerixafor and G-CSF combination mobilizes hematopoietic stem and progenitors cells with a distinct transcriptional profile and a reduced in vivo homing capacity compared to Plerixafor alone. Haematologica. 2016 doi: 10.3324/haematol.2016.154740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majeti R., Park C.Y., Weissman I.L. Identification of a hierarchy of multipotent hematopoietic progenitors in human cord blood. Cell Stem Cell. 2007;1:635–645. doi: 10.1016/j.stem.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazurier F., Doedens M., Gan O.I., Dick J.E. Rapid myeloerythroid repopulation after intrafemoral transplantation of NOD-SCID mice reveals a new class of human stem cells. Nat. Med. 2003;9:959–963. doi: 10.1038/nm886. [DOI] [PubMed] [Google Scholar]
- McDermott S.P., Eppert K., Lechman E.R., Doedens M., Dick J.E. Comparison of human cord blood engraftment between immunocompromised mouse strains. Blood. 2010;116:193–200. doi: 10.1182/blood-2010-02-271841. [DOI] [PubMed] [Google Scholar]
- McKenzie J.L., Gan O.I., Doedens M., Dick J.E. Reversible cell surface expression of CD38 on CD34-positive human hematopoietic repopulating cells. Exp. Hematol. 2007;35:1429–1436. doi: 10.1016/j.exphem.2007.05.017. [DOI] [PubMed] [Google Scholar]
- Michallet M., Philip T., Philip I., Godinot H., Sebban C., Salles G., Thiebaut A., Biron P., Lopez F., Mazars P. Transplantation with selected autologous peripheral blood CD34+Thy1+ hematopoietic stem cells (HSCs) in multiple myeloma: impact of HSC dose on engraftment, safety, and immune reconstitution. Exp. Hematol. 2000;28:858–870. doi: 10.1016/s0301-472x(00)00169-7. [DOI] [PubMed] [Google Scholar]
- Miller P.H., Knapp D.J.H.F., Beer P.A., MacAldaz M., Rabu G., Cheung A.M.S., Wei L., Eaves C.J. Early production of human neutrophils and platelets posttransplant is severely compromised by growth factor exposure. Exp. Hematol. 2016;44:635–640. doi: 10.1016/j.exphem.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Naldini L. Gene therapy returns to centre stage. Nature. 2015;526:351–360. doi: 10.1038/nature15818. [DOI] [PubMed] [Google Scholar]
- Negrin R.S., Atkinson K., Leemhuis T., Hanania E., Juttner C., Tierney K., Hu W.W., Johnston L.J., Shizurn J.A., Stockerl-Goldstein K.E. Transplantation of highly purified CD34+Thy-1+ hematopoietic stem cells in patients with metastatic breast cancer. Biol. Blood Marrow Transpl. 2000;6:262–271. doi: 10.1016/s1083-8791(00)70008-5. [DOI] [PubMed] [Google Scholar]
- Notta F., Doulatov S., Laurenti E., Poeppl A., Jurisica I., Dick J.E. Isolation of single human hematopoietic stem cells capable of long-term multilineage engraftment. Science. 2011;333:218–221. doi: 10.1126/science.1201219. [DOI] [PubMed] [Google Scholar]
- Palchaudhuri R., Saez B., Hoggatt J., Schajnovitz A., Sykes D., Tate T., Czechowicz A., Kfoury Y., Ruchika F., Rossi D. Non-genotoxic conditioning for hematopoietic stem cell transplantation using a hematopoietic-cell-specific internalizing immunotoxin. Nat. Biotechnol. 2016;34:738–747. doi: 10.1038/nbt.3584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrillo C., Cesana D., Piras F., Bartolaccini S., Naldini L., Montini E., Kajaste-Rudnitski A. Cyclosporin a and rapamycin relieve distinct lentiviral restriction blocks in hematopoietic stem and progenitor cells. Mol. Ther. 2015;23:352–362. doi: 10.1038/mt.2014.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sessa M., Lorioli L., Fumagalli F., Acquati S., Redaelli D., Baldoli C., Canale S., Lopez I.D., Morena F., Calabria A. Lentiviral haemopoietic stem-cell gene therapy in early-onset metachromatic leukodystrophy: an ad-hoc analysis of a non-randomised, open-label, phase 1/2 trial. Lancet. 2016;388:476–487. doi: 10.1016/S0140-6736(16)30374-9. [DOI] [PubMed] [Google Scholar]
- Stein S., Ott M.G., Schultze-Strasser S., Jauch A., Burwinkel B., Kinner A., Schmidt M., Krämer A., Schwäble J., Glimm H. Genomic instability and myelodysplasia with monosomy 7 consequent to EVI1 activation after gene therapy for chronic granulomatous disease. Nat. Med. 2010;16:198–204. doi: 10.1038/nm.2088. [DOI] [PubMed] [Google Scholar]
- Wang C.X., Sather B.D., Wang X., Adair J., Khan I., Singh S., Lang S., Adams A., Curinga G., Kiem H.P. Rapamycin relieves lentiviral vector transduction resistance in human and mouse hematopoietic stem cells. Blood. 2014;124:913–923. doi: 10.1182/blood-2013-12-546218. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.