Abstract
Background
Mucormycosis is one of the rapidly progressing and lethal form of fungal infection which involves the nose and paranasal sinuses of the head and the neck regions. Mucormycosis also remains a threat to patients with uncontrolled diabetes or other predisposing systemic conditions. It manifests as rhinocerebral, pulmonary, gastrointestinal, cutaneous or disseminated form. The underlying conditions can influence clinical presentation and often delay diagnosis, with resultant poor outcomes.
Case Details
We report a case of rhinocerebral mucormycosis in a 75 year-old diabetic patient with emphasise on diagnosis, treatment and survival options of patient from this potentially fatal fungal infection. Extra oral examination revealed mild non-tender swelling on the face, unable to see from left eye, impaired sense of smell, difficulty in speech and nasal stuffiness. Intra-oral examination showed necrosis of mucosa and underlying bone in relation to canine to the tuberosity area of the left vestibular region of the maxilla.
Conclusion
Timely diagnosis is critical to survival and minimization of morbidity. Institution of surgical and medical therapy is critical in maximizing the likelihood of good outcome.
Keywords: Mucormycosis, fungal, systemic, maxillary sinus
Introduction
Mucormycosis refers to several different diseases caused by infection with fungi in the order of Mucorales. Rhizopus species are the most common causative organisms (1,2). Saprophytic aerobic fungi of the class Phycomycetes (order Mucorales) cause rhinocerebral mucormycosis, also known as phycomycosis. Phycomycetes are ubiquitous in nature commonly found in decaying vegetation, soil and bread mold. They grow rapidly and can release large numbers of airborne spores. Thus, they are frequently found colonizing the oral mucosa, the nose, the paranasal sinuses and the throat (3). Most mucormycosis infections are life-threatening, and risk factors, such as diabetic ketoacidosis and neutropenia are present in most cases which can lead to complications (4). In diabetic patients, especially with elevated blood sugar levels, the spores germinate, hyphae develop and fungi begin an inexorable march through lung tissues, invading blood vessels and surrounding tissues. As blood vessels become involved, thrombosis occurs resulting in tissue necrosis and fungi continue to grow in this devitalised tissue (5). Rhinocerebral mucormycosis (ROCM) is the most common form of mucormycosis in patients with diabetes mellitus. The infection develops after inhalation of fungal sporangio spores into the paranasal sinuses. Rhinocerebral mucormycosis most commonly presents in an acute setting mimicking symptoms of sinusitis or periorbital cellulitis. The pleiotropic clinical manifestations and elusive presentation of mucormycosis often delay diagnosis, with resultant poor outcomes. A high index of suspicion for mucormycosis based on appropriate risk stratification and improved laboratory diagnosis are important for improving the natural history of this devastating infection (5). In the case presented here, the subtler lesion progressed rapidly leading to tissue necrosis and spread to the adjacent structures causing extensive damage.
Case Report
A 75 year-old male edentulous patient reported with complaint of problem in denture wearing and swelling on the face. The patient is edentulous and wearing denture from the past 10 years. The patient is unable to wear denture from the past two months because of some changes in supporting alveolar bone. According to the patient, some discoloration appeared in the left maxillary region on the buccal side of the ridge (∼ 4 months ago) followed by necrosis of underlying bone within two months. There was no pain and no abnormal sensation. The patient was a known diabetic since few years, under medication for the same. He also complained of nasal congestion and headache. He got his right eye operated on for cataract 6 before months and kept on post-operative medication and scheduled to be operated on for the left eye cataract after few days. However, the patient got ulceration in the oral cavity before the operation. He took medication for the same after which he got swelling over the face, on the left part of the face along with protrusion of left eye and impaired visibility. The patient got some tests done; namely, CT scan of the Head and the Orbit, and he was diagnosed with the left orbital cellulitis and the left paranasal sinusitis. He got treatment for the same. He reported back to his eye surgeon and started taking medication, but unfortunately, he got cornea of left eye damaged.
Extra oral examination revealed mild non-tender swelling on the face, unable to see from the left eye, impaired sense of smell, difficulty in speech and nasal stuffiness (Figure 1). Intra-oral examination showed necrosis of mucosa and underlying bone in relation to canine to tuberosity area of the left vestibular region of maxilla (Figure 2). There was an abnormal communication between vestibule and palate under it due to bone loss in the same region.
Figure 1.
Extra-oral photograph showing swelling over the left part of the face and protrusion of left eye and impaired visibility.
Figure 2.
Intra-oral photograph showing necrosis of mucosa and underlying bone in relation to canine to tuberosity area of left vestibular region of maxilla along with abnormal communication b/w vestibule and palate.
A CT Scan showed a homogeneous density mass involving the greater palatine and the sphenopalatine foramen obliterating the two (Figure 3). The nasal turbinates were bilaterally obliterated. Hard palate osteolysis was seen more on the left side. Radiographic interpretation was suggestive of Rhinocerebral mucoromycosis.
Figure 3.

CT scan showing a homogenous density mass involving maxillary sinus and nasal turbinates bilaterally obliterated.
A biopsy was advised. Hard tissue specimen along with the adjacent soft tissue was excised under local anesthesia and was sent for histopathological examination. Histopathological examination with hematoxylin and eosin stain, identified presence of broad non-septae with branching at right angle along with areas of necrosis (Figure 4).The patient was advised for medication and surgical debridement of the involved area along with administration of antifungal therapy such as liposomal Amphotericin-B 5mg\kg\day intravenously for 10 days, followed by Posaconazole 400mg twice daily.
Figure 4.
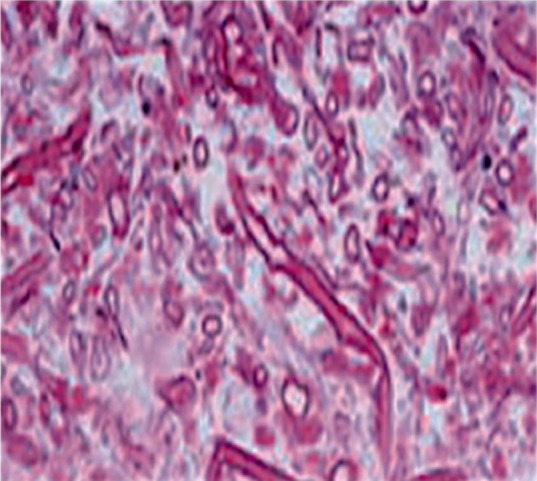
Photomicrograph showing presence of non-septae hyphae branching at right angle along with areas of necrosis (H&E, × 40).
Discussion
Mucormycosis is a serious, relatively uncommon invasive fungal infection and one of the most aggressive and lethal invasive mycoses (5). The predisposing factors for mucormycosis are uncontrolled diabetes (particularly in patients having ketoacidosis), malignancies such as lymphomas and leukemias, renal failure, organ transplant, immunosuppressive therapy, cirrhosis, and AIDS (6). Mucorales species are vasotropic, causing tissue infarctions, and the mucormycosis spectrum ranges from cutaneous, rhinocerebral, and sinopulmonary to disseminated and frequently fatal infections, especially in immune-compromised hosts (7). Reports have suggested that the ability of serum of immuno-compromised patients to inhibit Rhizopus invitro is reduced, which makes them suitable hosts to opportunistic fungal infections (8). In diabetic patients, especially with elevated blood sugar levels, the spores germinate, hypae develop, fungi begin an inexorable march through the tissues as blood vessels become involved, thrombosis occurs, resulting in tissue necrosis and fungi continue to grow in this devitalised tissue causing further damage to surrounding tissues (9). The presence of chronic diabetes in our patient too led to necrosis of palate. Rhinocerebral mucormycosis (ROCM) is the most common form of mucormycosis in patients with diabetes mellitus. The infection develops after inhalation of fungal sporangiospores into the paranasal sinuses. Upon germination, the invading fungus may spread inferiorly to invade the palate, posteriorly to invade the sphenoid sinus, laterally into the cavernous sinus to involve the orbits or cranially to invade the brain which can prove fatal (10). Our patient had uncontrolled diabetes which is a well-known predisposing factor for mucormycosis along with spread of lesion from the palate into adjacent tissues. The initial symptoms of ROCM are consistent with those of sinusitis and periorbital cellulitis and include eye and/or facial pain and facial numbness followed by blurry vision (5,10). Signs and symptoms that suggest mucormycosis in susceptible individuals include, unilateral periorbital facial pain, facial cellulitis, orbital inflammation, eyelid edema, proptosis, acute ocular motility changes, nasal discharge, nasal stuffiness headacheand acute vision loss (5). If blood supply to eye is affected by invasion of retinal artery, blindness develops. A black necrotic eschar is the hallmark of mucormycosis (12,13).
Among the differential diagnosis, rhinocerebral mucormycosis may initially resemble bacterial sinusitis and may mimic malignancy. Rhinocerebral mucormycosis may be confused with allergic fungal sinusitis, which is caused by phaeohyphomycoses in individuals with histories of allergic rhinitis, elevated immunoglobulin E levels, nasal polyps and recurrent or chronic sinusitis. Allergic fungal sinusitis slowly progresses over months to years, although it causes proptosis and a large rhinocerebral mass, it does not invade tissue or meninges. Aspergillosis can cause a similar disease, with CNS invasion, and carries a poor prognosis. An important difference is that itraconazole may play a role in treatment. Histologic staining can differentiate between the fungi (14). The pleiotropic clinical manifestations with other lesions were ruled out with radiographic and histopathology report. A definitive diagnosis of mucormycosis can be made by tissue biopsy that identifies the characteristic hyphae. In order to differentiate histopathologically from other types of lesions such as aspergillosis, which shows presence of narrow, septae hypae with narrow angle branching was done. In this case, the fungus was identified by hematoxylin and eosin stain.
Treatments of mucormycosis need to be fast and aggressive because by the time even the presumptive diagnosis is made, often the patient has suffered significant tissue damage that cannot be reversed. Most patients require both surgical and medical treatments. The line of treatment for such cases requires aggressive surgical debridement of the infected area; otherwise, the patient is likely to die. Medications also plays an important role. Two main goals are sought at the same time: antifungal medications to slow or halt fungal spread and medications to treat any debilitating underlying diseases. Amphotericin B (initially intravenous) is the usual drug of choice for antifungal treatment. Patients with underlying diseases like diabetes need their diabetes optimally controlled. Patients may need additional surgeries and usually need antifungal therapy for an extended time period (weeks to months) depending on the severity of the disease (15). The prognosis of mucormycosis is usually fair to poor; the prognosis depends on the overall health of the patient, the speed of diagnosis and treatment, the patient's ability to respond to treatments and the complete debridement of the infected body area. In this patient, the line of treatment advised was aggressive surgical debridement of the infected area along with administration of amphotericin B as it is the drug of choice in treatment of mucormycotic infection (2,6,11). The patient was under observation for his ability to respond to treatment due to old age and overall health of patient.
Mucormycosis is a serious, relatively uncommon invasive fungal infection. Early diagnosis is essential because by the time even the presumptive diagnosis is made, often the patient has suffered significant tissue damage that cannot be reversed. The pleiotropic clinical manifestations and elusive presentation of mucormycosis often delay diagnosis, with resultant poor outcomes. Timely diagnosis is critical to survival and minimization of morbidity. Institution of surgical and medical therapy is critical in maximizing the likelihood of good outcome.
References
- 1.Dimaka K, Mallis A, Naxakis SS, Marangos M, Papadas TA, Stathas T, et al. Chronic rhinocerebral mucormycosis: a rare case report and review of the literature. Mycoses. 2014;57:699–702. doi: 10.1111/myc.12219. [DOI] [PubMed] [Google Scholar]
- 2.Kwon-Chung KJ. Taxonomy of fungi causing mucormycosis and entomophthoramycosis (zygomycosis) and nomenclature of the disease: molecular mycologic perspectives. Clin Infect Dis. 2012;54(1):S8–S15. doi: 10.1093/cid/cir864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Margo CE, Linden C, Strickland-Marmol LB, Denietolis AL, McCaffrey JC, Kirk N. Rhinocerebral mucormycosis with perineural spread. Ophthal Plast Reconstr Surg. 2007;23:326–327. doi: 10.1097/IOP.0b013e318070855b. [DOI] [PubMed] [Google Scholar]
- 4.Berdai MA, Labib S, Harandou M. Rhinocerebral mucormycosis complicating ketoacidosis diabetes. Presse Med. 2016;45:145–146. doi: 10.1016/j.lpm.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Reddy SS, Rakesh N, Chauhan P, Sharma S. Rhinocerebral Mucormycosis Among Diabetic Patients: An Emerging Trend. Mycopathologia. 2015;180:389–396. doi: 10.1007/s11046-015-9934-x. [DOI] [PubMed] [Google Scholar]
- 6.Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatment. Clin Microbiol Infect. 2004;10(1):31–47. doi: 10.1111/j.1470-9465.2004.00843.x. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez CE, Rinaldi MG, Sugar AM. Zygomycosis. Infect Dis Clin North Am. 2002;16:895–914. doi: 10.1016/s0891-5520(02)00037-5. [DOI] [PubMed] [Google Scholar]
- 8.Aras MH, Kara MI, Erkiliç S, Ay S. Mandibular mucormycosis in immunocompromised patients: report of 2 cases and review of the literature. J Oral Maxillofac Surg. 2012;70:1362–1368. doi: 10.1016/j.joms.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 9.Chakrabarti A, Das A, Mandal J. The rising trend of invasive mucormycosis in patients with uncontrolled diabetes mellitus. Med Mycol. 2006;44:335–342. doi: 10.1080/13693780500464930. [DOI] [PubMed] [Google Scholar]
- 10.Hosseini SM, Borghei P. Rhinocerebral mucormycosis: pathways of spread. Eur Arch Otorhinolaryngol. 2005;262:932–938. doi: 10.1007/s00405-005-0919-0. [DOI] [PubMed] [Google Scholar]
- 11.Kömür S, İnal AS, Kurtaran B, Ulu A, Uğuz A, Aksu HS, et al. Mucormycosis: a 10-year experience at a tertiary care center in Turkey. Turk J Med Sci. 2016;46:58–62. doi: 10.3906/sag-1409-137. [DOI] [PubMed] [Google Scholar]
- 12.Monteagudo M, Palazón-García E, Lozano-Setién E, García-García J. The ‘black turbinate sign’ in a case of rhinocerebral mucormycosis. Rev Neurol. 2014;58:234–235. [PubMed] [Google Scholar]
- 13.Orguc S, Yuceturk AV, Demir MA, Goktan C. Rhinocerebral mucormycosis: perineural spread via the trigeminal nerve. J Clin Neurosci. 2005;12:484–486. doi: 10.1016/j.jocn.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 14.Walsh TJ. Rhino-orbital-cerebral mucormycosis. Curr Infect Dis Rep. 2012;14:423–434. doi: 10.1007/s11908-012-0272-6. [DOI] [PubMed] [Google Scholar]
- 15.Sun HY, Singh N. Mucormycosis: Its Contemporary Face and Management. Lancet Infect Dis. 2011;11:301–311. doi: 10.1016/S1473-3099(10)70316-9. [DOI] [PubMed] [Google Scholar]




