Summary
This article reviews recently published studies investigating the MRI and sonographic diagnosis of masticatory muscle myalgia in temporomandibular disorder patients. The MRI and sonographic features of muscle after treatment are also discussed. Literature published within the last 15 years was obtained from the PubMed database using the following Mesh terms: magnetic resonance imaging (MRI) or sonography, masticatory muscle pain, and treatment. MRI and sonography enable accurate visualization and evaluation of the masticatory muscles, thereby increasing our understanding of pathology and cause of pain associated with these muscles. Although therapeutic efficacy is often evaluated based on clinical findings, MR and sonographic imaging studies may also be valuable.
Keywords: MRI, Sonography, Masticatory muscle, Myalgia, Splint therapy, Massage therapy
1. Introduction
Masticatory muscles were evaluated using electromyography (EMG) [1], [2], [3], near-infrared spectroscopy (NIRS) [4], and so on, for purpose of evaluation of muscle activities and blood oxygen kinetics. Al-Saleh et al. performed systematic review of two studies (74 patients) that were collected using Mesh terms of TMD, jaw pain and EMG, and stated that the sensitivity of EMG in diagnosing TMD was low (0.25–0.40) [1].
In the recent years, studies using MRI and sonography in patients with masticatory muscle myalgia have frequently been reported, and the newly developed technologies have been introduced [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38]. Muscles after treatment in those patients also have been evaluated using MRI and sonography [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15].
This article reviews recently published studies focusing on the MRI and sonographic diagnosis of masticatory muscle myalgia in temporomandibular disorder (TMD) patients, and shows the intramuscular state, blood flow, and muscle hardness. The MRI and sonographic evaluations in relation to the efficacy of various treatments are also discussed.
2. Methods
Literatures published within the last 15 years were searched from the PubMed database using the following Mesh terms: (1) (MRI or sonography) and masticatory muscle pain; (2) (MRI or sonography) and masticatory muscle pain and treatment. Original papers and review articles published in English and Japanese were adopted. Selection criteria were MRI and sonographic features in diagnosis of masticatory muscle myalgia and in evaluation of muscle after therapy. Studies of neoplastic lesions and case report were excluded.
3. Results
3.1. MRI and sonographic diagnosis of masticatory muscle myalgia in TMD patients
The number of literature that met the mesh terms of (1) and the above-mentioned criteria was 34 [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38].
Most MRI studies in TMD patients evaluated intra-articular changes, such as disk displacement [5], [6], [7], [16], [17], [18], and MRI studies evaluating the masticatory muscles were a few. Zanoteli et al. evaluated changes in the signal intensities of the masticatory muscles in 15 patients with myotonic dystrophy on T1- and T2-weighted images, and diagnosed the presence of a high signal intensity area (fatty replacement) as abnormal [19]. Gregor et al. [20] and Okada et al. [21] investigated masseter muscle metabolism using 31P-magnet resonance spectroscopy. The former revealed a difference in masseter muscle metabolism between 11 dolichofacial and 11 brachyfacial subjects, and the latter showed an increase in masseter muscle metabolism secondary to heat pack use in 12 healthy subjects.
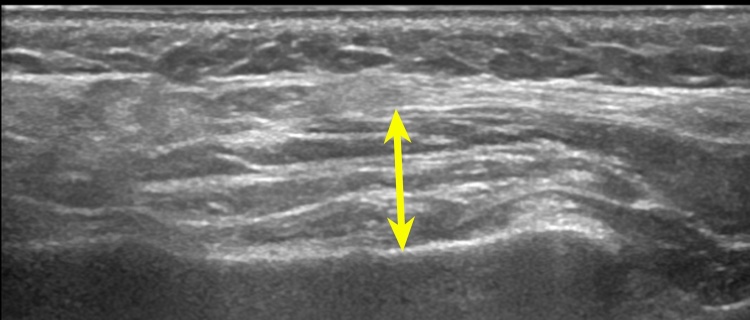
The most common index for evaluation of masticatory muscles in the sonography studies was muscle thickness (Fig. 1) [8], [9], [10], [11], [12], [22], [23], [24], [25], [26], [27], [28], [29]. Ariji et al. showed that the masseter muscle thickness in 25 TMD patients was greater than that of 30 healthy volunteers [22]. Strini et al. showed that the masseter muscle thickness on sonography and the masseter muscle activity on electromyography were positively correlated with occlusal force in 19 TMD patients [23]. Other reports examined the relationship between masseter muscle thickness and facial morphology [24], [25].
Figure 1.
Method for measuring the thickness of the masseter muscle.
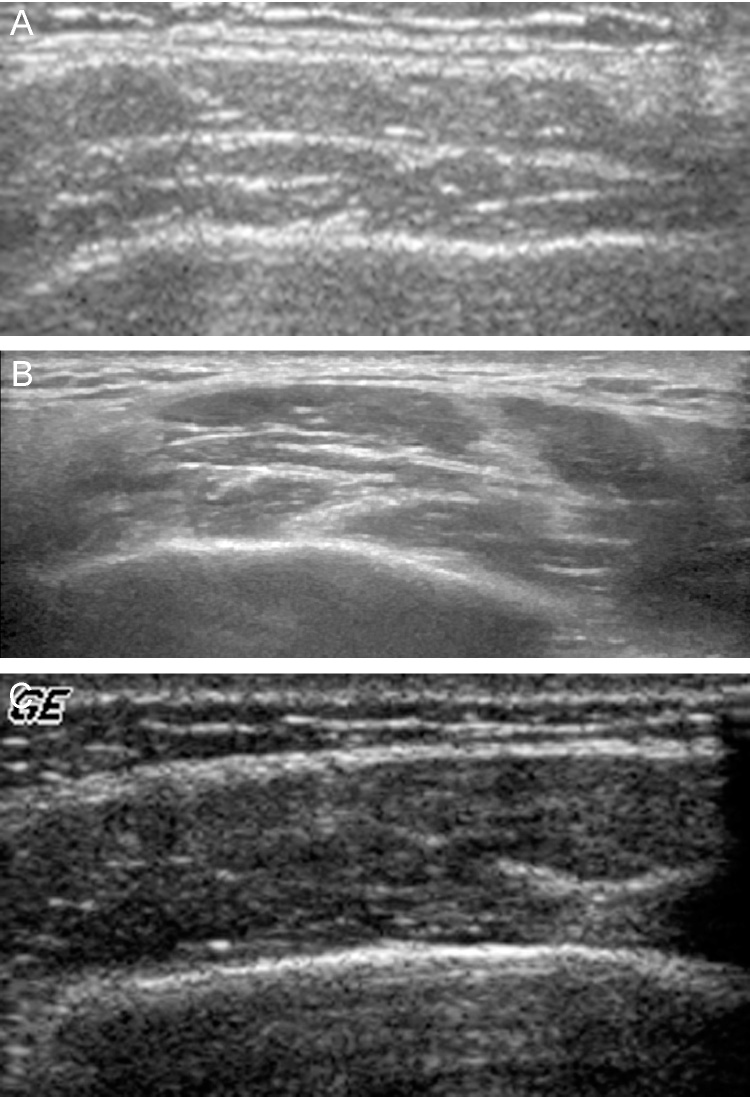
A next focusing index was the appearance of the intramuscular echogenic bands, which correspond to the internal fascia (Fig. 2) [39]. Masseter muscle appearance was classified into three types based on the internal echogenic bands, and it was revealed that the masseter muscles in 25 TMD patients frequently displayed thickened bands or reduction in the number of bands [22].
Figure 2.
Appearance of the intramuscular echogenic bands of the masseter muscle. (A) Fine echogenic bands; (B) thickened bands; (C) Reduction in the number of bands
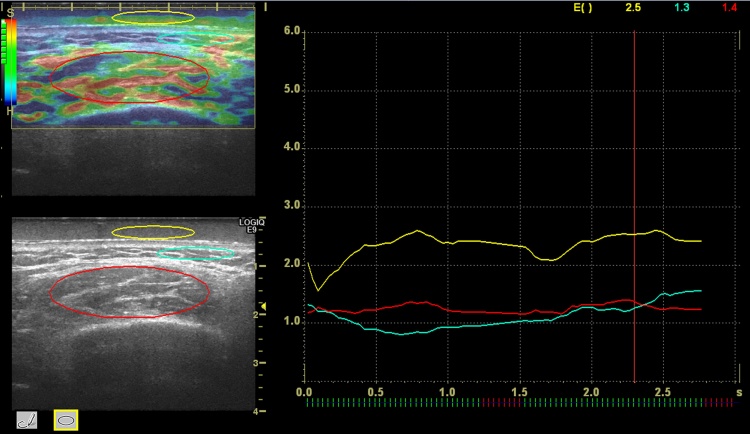
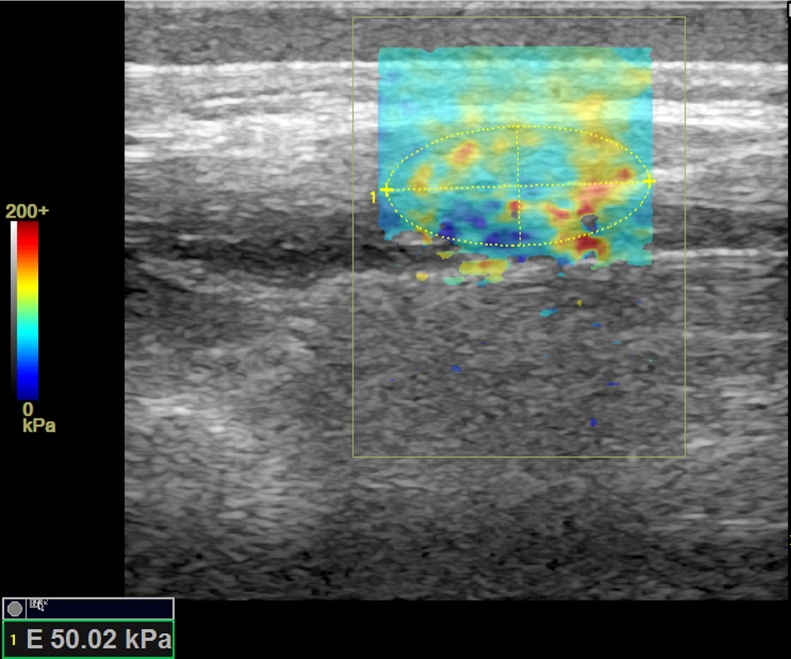
In recent years, sonoelastography has been used to evaluate the skeletal muscles [40], [41], [42], [43]. The principal of sonoelastography can be divided into two types: strain and shear wave elastography [44]. Strain elastography is based on the distortion due to vibration caused by manual pressure. Hardness on strain elastography is displayed as a relative value compared to the reference (Fig. 3). Shear wave elastography is based on the propagation velocity of the shear wave generated by acoustic radiation force. Hardness on shear wave elastography is displayed as the shear wave speed or Young's modulus (Fig. 4).
Figure 3.
Elasticity index of the masseter muscle on strain elastography.
Figure 4.
Young's modulus based on the propagation velocity of the shear wave on shear wave elastography.
Studies regarding the masseter muscle hardness on strain elastography recently have been reported [30], [31]. Hardness on strain elastography is expressed as elasticity index (EI). The EI was originally developed for sonography machine and software, and defined as the strain values of each area compared with the average strain value (EI = 1) of the whole area of interest. The EIs of the softer and harder areas than the average EI were assigned as 0–1 and 1–6, respectively. EI ratio of the masseter muscle was evaluated compared with the reference tissue, such as the subcutaneous fat or coupling agent (Fig. 3). Ariji et al. evaluated the difference in the masseter muscle hardness between eight TMD patients and 35 healthy volunteers using the EI ratios of the masseter muscle against the subcutaneous fat [30]. As a result, there was a significant difference in the EI ratios between the symptomatic and asymptomatic sides in TMD patients. The EI ratio of the symptomatic side in TMD patients was greater than that seen in the healthy volunteers. Nakayama et al. adopted a coupling agent with a known Young's modulus as a reference in order to be generally available to EI ratio, and measured the EI ratio of the masseter muscle against the coupling agent in 25 healthy volunteers [31].
A few studies on masseter muscle hardness using shear wave elastography were found. Arda et al. reported that the average Young's moduli of the masseter muscles in 127 healthy volunteers was 10.4 ± 3.7 kPa [32]. Ariji et al. measured the average Young's moduli of the masseter muscles in 30 healthy volunteers using the other sonoelastographic device, and reported that it was 42.8 ± 5.56 [33]. Badea et al. found no significant difference in the shear wave velocities of the masseter muscles between 25 healthy volunteers and 13 TMD patients [34]. As such, further research investigating masseter muscle hardness may be required.
Experimental attempts to explore the cause of myalgia using imaging have also been made. Based on the hypothesis that masseter muscle myalgia is partially caused by edematous changes in the masseter muscles, the following studies investigated the water content in the masseter muscles during jaw clenching using MRI: Nagayama et al. adopted magnetization transfer contrast (MTC) imaging, and revealed that the magnetization transfer ratios of masticatory muscles in 50 TMD patients were significantly lower than in 28 healthy volunteers [35]. They concluded that MTC imaging strongly reflected edematous changes in masseter muscle, possibly related to masseter muscle myalgia. Shiraishi et al. examined changes in the diffusion parameters of the masseter muscles in 11 healthy volunteers during jaw opening and clenching on diffusion-tensor imaging [36]. Ariji et al. assessed edematous changes in the masseter muscles of 10 healthy volunteers caused by low-level static contraction on T2-weighted interactive decomposition of water and fat with echo asymmetry and least-square estimation (IDEAL) water images [37]. A similar study was performed using sonoelastography, which showed that the thickness and hardness of the masseter muscles increased immediately after contraction [38]. When changes in the masseter muscles by contraction were compared using MRI and sonoelastography, the soft area ratio of muscle on sonoelastography increased in correlation with increases in water signal on MRI [41]. Therefore, sonoelastography could also evaluate edematous changes in the masseter muscles.
3.2. MRI and sonographic evaluation of masticatory muscle and therapeutic efficacy
TMD patients with masticatory muscle myalgia were treated by splint therapy [45], [46], [47], medication [48], [49], [50], physical therapy [51], [52], [53] and so on. As an index for evaluating the therapeutic efficacy, the clinical findings, including pain intensity (visual analog scale) [52], [53], pressure pain threshold [50], [52], [53], degree of mouth opening [49], [50], and degree of jaw function impairment [49], [52], [53], were analyzed. Muscle activity was also evaluated using electromyography [1], [2], [3], [51]. To assess the efficacy of massage therapy on the skeletal muscles, muscle hardness was generally evaluated using a muscle hardness meter [54], [55]. Hiraiwa et al. evaluated the change in masseter muscle hardness after massage therapy using a muscle hardness meter, and confirmed that the hardness decreased after massage treatment [56].
As to the evaluation by MRI and sonography, the number of literature that met to the mesh terms of 2 and the previously-mentioned criteria was 11 [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15]. These were studies on the evaluation after the splint or massage therapies. Of them, all 3 MRI studies evaluated changes in disc position after therapy, and did not evaluate changes in the muscles [5], [6], [7]. In studies using sonography, an useful index for therapeutic efficacy is the thickness and intramuscular echo appearance of the masseter muscle following treatment (Figure 1, Figure 2) [8], [9], [10], [11], [12], [13], [14], [15].
A stabilization splint therapy is considered as a therapy of weak recommended level (Grade 2C) for patients with masticatory muscle myalgia, according to the Japanese Society's temporomandibular joint evidence-based clinical guidelines [45]. A systematic review on the efficacy of stabilization splints showed that the use of a stabilization splint aided patients with masticatory muscle myalgia [46], [47]. However, a stabilization splint did not appear to yield a better outcome than a soft splint, a non-occluding palatal splint, physical therapy, or body acupuncture [46]. Following stabilization splint therapy, Aldemir et al. evaluated the changes in the masseter muscle thickness in 35 patients with myofascial pain, and reported that a reduced thickness was found [10]. Bertram et al. evaluated the changes in the masseter muscle thickness in 29 patients and reported that the asymmetry index of thickness decreased [11], [12]. The change in appearance of the intramuscular echogenic bands is controversial; Aldemir et al. found no change [10], whereas Sasaki et al. reported a change in intramuscular echo types in 12 of 40 patients [15].
A few studies performed randomized controlled trials of massage therapy for masticator muscle myalgia [51], [52], [53]. Gomes et al. compared the efficacies among massage therapy, splint therapy, and the combination therapy (n = 15 patients in each group), and showed that the combination of two therapies demonstrated a greater improvement although no significant difference among the groups [51]. De Laat et al. compared the efficacies between 4 weeks and 6 weeks of physical therapies (n = 24 patients in each group) [52], and Craane et al. compared the efficacies between physical therapy (n = 23) and control group (n = 26) [53]. The physical therapy including massage showed improvement in pain and jaw function, but the degree of improvement was not significant between the groups.
In order to adapt of massage therapy to masticatory muscle pain, an oral rehabilitation robot was previously developed [57]. Ariji et al. investigated the safety, a suitable treatment regimen, and the efficacy of masseter and temporal muscle massage treatment using this oral rehabilitation robot (Fig. 5) [8], [13]. No adverse events occurred with any of the treatment sessions. Suitable massage was delivered at a pressure of 10 N for 16 min. The standard treatment regimen was five sessions, spaced 2 weeks apart for a 9.5-week duration. This massage therapy regimen was effective in 70.3% of the patients [8].
Figure 5.
An oral rehabilitation robot for massaging the masseter and temporal muscles.
As to the sonographic evaluation of the masseter muscles after massage therapy, the thickness decreased in all of 41 patients [8], [9], and fine echogenic bands began to appear in 93.3% of the therapy-effective 26 patients [14]. Ariji et al. also evaluated changes in the masseter muscle hardness using sonoelastography (Fig. 4) [14], [30]. The EI ratio decreased after massage therapy. [14], [30] In particular, the EI ratio in the effective-therapy group significantly decreased in early period of treatment, and therefore, the EI ratio may be an effective tool for predicting therapeutic efficacy [14].
4. Discussion and conclusion
This review provides a summary of the literature published within the last 15 years investigating the MRI and sonographic diagnosis of masticatory muscle myalgia in TMD patients. With the recent advances in imaging technology, edematous changes and muscle hardening in patients with masticatory muscle myalgia can be visualized using MRI and sonoelastography.
Evaluation of therapeutic efficacy should be based not only on the clinical findings, but also on imaging findings. Massage therapy using an oral rehabilitation robot would give a certain therapeutic effect. In future, it should be generalized. Sonography will enable the clinician to select the appropriate treatment modalities for managing masticatory muscle myalgia.
Conflict of interest
The authors have no conflicts of interest to declare.
Funding
This study was partially supported by a Grant-in-Aid for Scientific Research (C) (23592785) from the Japan Society for the Promotion of Science.
Acknowledgments
We address special thanks to Dr. Miwa Nakayama, Dr. Nobumi Ogi, Dr. Shigemitsu Sakuma, and Prof. Kenichi Kurita, who are members of the TMD clinic of Aichi-Gakuin University at Nagoya. We also thank Prof. Akitoshi Katsumata of Asahi University at Gifu for the development of the oral rehabilitation robot.
References
- 1.Al-Saleh M.A., Armijo-Olivo S., Flores-Mir C., Thie N.M. Electromyography in diagnosing temporomandibular disorders. J Am Dent Assoc. 2012;143:351–362. doi: 10.14219/jada.archive.2012.0177. [DOI] [PubMed] [Google Scholar]
- 2.Klasser G.D., Okeson J.P. The clinical usefulness of surface electromyography in the diagnosis and treatment of temporomandibular disorders. J Am Dent Assoc. 2006;137:763–771. doi: 10.14219/jada.archive.2006.0288. [DOI] [PubMed] [Google Scholar]
- 3.Suvinen T.I., Kemppainen P. Review of clinical EMG studies related to muscle and occlusal factors in healthy and TMD subjects. J Oral Rehabil. 2007;34:631–644. doi: 10.1111/j.1365-2842.2007.01769.x. [DOI] [PubMed] [Google Scholar]
- 4.Sugisaki M., Misawa A., Ikai A., Young-Sung K., Tanabe H. Sex differences in the hemoglobin oxygenation state of the resting healthy human masseter muscle. J Orofac Pain. 2001;15:320–328. [PubMed] [Google Scholar]
- 5.Summa S., Ursini R., Manicone P.F., Molinari F., Deli R. MRI assessment of temporomandibular disorders: an approach to diagnostic and therapeutic setting. Cranio. 2014;32:131–138. doi: 10.1179/0886963413Z.00000000021. [DOI] [PubMed] [Google Scholar]
- 6.Muhtarogullari M., Avci M., Yuzugullu B. Efficiency of pivot splints as jaw exercise apparatus in combination with stabilization splints in anterior disc displacement without reduction: a retrospective study. Head Face Med. 2014;10:42. doi: 10.1186/1746-160X-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rohida N.S., Bhad W., clinical A. MRI, and EMG analysis comparing the efficacy of twin blocks and flat occlusal splints in the management of disc displacements with reduction. World J Orthod. 2010;11:236–244. [PubMed] [Google Scholar]
- 8.Ariji Y., Nakayama M., Nishiyama W., Ogi N., Sakuma S., Katsumata A. Potential clinical application of masseter and temporal muscle massage treatment using an oral rehabilitation robot in temporomandibular disorder patients with myofascial pain. Cranio. 2015;33:256–262. doi: 10.1080/08869634.2015.1097303. [DOI] [PubMed] [Google Scholar]
- 9.Ariji Y., Katsumata A., Hiraiwa Y., Izumi M., Sakuma S., Shimizu M. Masseter muscle sonographic features as indices for evaluating efficacy of massage treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:517–526. doi: 10.1016/j.tripleo.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Aldemir K., Üstüner E., Erdem E., Demiralp A.S., Oztuna D. Ultrasound evaluation of masseter muscle changes in stabilization splint treatment of myofascial type painful temporomandibular diseases. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:377–383. doi: 10.1016/j.oooo.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Bertram S., Rudisch A., Bodner G., Emshoff R. Effect of stabilization-type splints on the asymmetry of masseter muscle sites during maximal clenching. J Oral Rehabil. 2002;29:447–451. doi: 10.1046/j.1365-2842.2002.00857.x. [DOI] [PubMed] [Google Scholar]
- 12.Bertram S., Rudisch A., Bodner G., Emshoff R. The short-term effect of stabilization-type splints on the local asymmetry of masseter muscle sites. J Oral Rehabil. 2001;28:1139–1143. doi: 10.1046/j.1365-2842.2001.00787.x. [DOI] [PubMed] [Google Scholar]
- 13.Ariji Y., Katsumata A., Ogi N., Izumi M., Sakuma S., Iida Y. An oral rehabilitation robot for massaging the masseter and temporal muscles: a preliminary report. Oral Radiol. 2009;25:53–59. doi: 10.1111/j.1365-2842.2009.01977.x. [DOI] [PubMed] [Google Scholar]
- 14.Ariji Y., Nakayama M., Nishiyama W., Ogi N., Sakuma S., Katsumata A. Can sonographic features be efficacy predictors of robotic massage treatment for masseter and temporal muscle in patients with temporomandibular disorder with myofascial pain? Cranio. 2016;34:13–19. doi: 10.1179/2151090314Y.0000000037. [DOI] [PubMed] [Google Scholar]
- 15.Sasaki J., Ariji Y., Sakuma S., Katsuno R., Kurita K., Ogi N. Ultrasonography as a potential tool for the evaluation of treatment effect in the masseter muscle of patients with temporomandibular disorder associated with myofascial pain. Oral Radiol. 2006;22:52–57. [Google Scholar]
- 16.Özkan N.C., Ozkan F. The relationship of temporomandibular disorders with headaches: a retrospective analysis. Agri. 2011;23:13–17. doi: 10.5505/agri.2011.48615. [DOI] [PubMed] [Google Scholar]
- 17.Matheus R.A., Ramos-Perez F.M., Menezes A.V., Ambrosano G.M., Haiter-Neto F., Bóscolo F.N. The relationship between temporomandibular dysfunction and head and cervical posture. J Appl Oral Sci. 2009;17:204–208. doi: 10.1590/S1678-77572009000300014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ohlmann B., Rammelsberg P., Henschel V., Kress B., Gabbert O., Schmitter M. Prediction of TMJ arthralgia according to clinical diagnosis and MRI findings. Int J Prosthodont. 2006;19:333–338. [PubMed] [Google Scholar]
- 19.Zanoteli E., Yamashita H.K., Suzuki H., Oliveira A.S., Gabbai A.A. Temporomandibular joint and masticatory muscle involvement in myotonic dystrophy: a study by magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94:262–271. doi: 10.1067/moe.2002.124580. [DOI] [PubMed] [Google Scholar]
- 20.Gregor C., Hietschold V., Harzer W. A 31P-magnet resonance spectroscopy study on the metabolism of human masseter in individuals with different vertical facial pattern. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:406–414. doi: 10.1016/j.oooo.2012.11.017. [DOI] [PubMed] [Google Scholar]
- 21.Okada K., Yamaguchi T., Komatsu K., Matsuki T., Gotouda A., Minowa K. The influence of tissue blood flow volume on energy metabolism in masseter muscles. Cranio. 2005;23:166–173. doi: 10.1179/crn.2005.024. [DOI] [PubMed] [Google Scholar]
- 22.Ariji Y., Sakuma S., Izumi M., Sasaki J., Kurita K., Ogi N. Ultrasonographic features of the masseter muscle in female patients with temporomandibular disorder associated with myofascial pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:337–341. doi: 10.1016/j.tripleo.2004.06.068. [DOI] [PubMed] [Google Scholar]
- 23.Strini P.J., Strini P.J., Barbosa Tde S., Gavião M.B. Assessment of thickness and function of masticatory and cervical muscles in adults with and without temporomandibular disorders. Arch Oral Biol. 2013;58:1100–1108. doi: 10.1016/j.archoralbio.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 24.Rohila A.K., Sharma V.P., Shrivastav P.K., Nagar A., Singh G.P. An ultrasonographic evaluation of masseter muscle thickness in different dentofacial patterns. Indian J Dent Res. 2012;23:726–731. doi: 10.4103/0970-9290.111247. [DOI] [PubMed] [Google Scholar]
- 25.Farella M., Bakke M., Michelotti A., Rapuano A., Martina R. Masseter thickness, endurance and exercise-induced pain in subjects with different vertical craniofacial morphology. Eur J Oral Sci. 2003;111:183–188. doi: 10.1034/j.1600-0722.2003.00035.x. [DOI] [PubMed] [Google Scholar]
- 26.Imanimoghaddam M., Davachi B., Madani A.S., Nemati S. Ultrasonographic findings of masseter muscle in females with temporomandibular disorders. J Craniofac Surg. 2013;24:e108–e112. doi: 10.1097/SCS.0b013e3182646af0. [DOI] [PubMed] [Google Scholar]
- 27.Kant P., Bhowate R.R., Sharda N. Assessment of cross-sectional thickness and activity of masseter, anterior temporalis and orbicularis oris muscles in oral submucous fibrosis patients and healthy controls: an ultrasonography and electromyography study. Dentomaxillofac Radiol. 2014;43:20130016. doi: 10.1259/dmfr.20130016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gaszynska E., Godala M., Szatko F., Gaszynski T. Masseter muscle tension, chewing ability, and selected parameters of physical fitness in elderly care home residents in Lodz, Poland. Clin Interv Aging. 2014;9:1197–1203. doi: 10.2147/CIA.S66672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tircoveluri S., Singh J.R., Rayapudi N., Karra A., Begum M., Challa P. Correlation of masseter muscle thickness and intermolar width – an ultrasonography study. J Int Oral Health. 2013;5:28–34. [PMC free article] [PubMed] [Google Scholar]
- 30.Ariji Y., Gotoh A., Hiraiwa Y., Kise Y., Nakayama M., Nishiyama W. Sonographic elastography for evaluation of masseter muscle hardness. Oral Radiol. 2013;29:64–69. [Google Scholar]
- 31.Nakayama M., Ariji Y., Nishiyama W., Ariji E. Evaluation of the masseter muscle elasticity with the use of acoustic coupling agents as references in strain sonoelastography. Dentomaxillofac Radiol. 2015;44:20140258. doi: 10.1259/dmfr.20140258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arda K., Ciledag N., Aribas B.K., Aktas E., Köse K. Quantitative assessment of normal soft-tissue elasticity using shear-wave ultrasound elastography. Am J Roentgenol. 2011;197:532–536. doi: 10.2214/AJR.10.5449. [DOI] [PubMed] [Google Scholar]
- 33.Ariji Y., Nakayama M., Nishiyama W., Nozawa M., Ariji E. Shear-wave sonoelastography for assessing masseter muscle hardness in comparison with strain sonoelastography: study with phantoms and healthy volunteers. Dentomaxillofac Radiol. 2016;45:20150251. doi: 10.1259/dmfr.20150251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Badea I., Tamas-Szora A., Chiorean I., Fildan F., Ciulea E., Badea M. Quantitative assessment of the masseter muscle's elasticity using Acoustic Radiation Force Impulse. Med Ultrason. 2014;16:89–94. doi: 10.11152/mu.201.3.2066.162.ib1asz2. [DOI] [PubMed] [Google Scholar]
- 35.Nagayama K., Suenaga S., Nagata J., Takada H., Majima H.J., Miyawaki S. Clinical significance of magnetization transfer contrast imaging for edematous changes in masticatory muscle. J Comput Assist Tomogr. 2010;34:233–241. doi: 10.1097/RCT.0b013e3181bb2002. [DOI] [PubMed] [Google Scholar]
- 36.Shiraishi T., Chikui T., Inadomi D., Kagawa T., Yoshiura K., Yuasa K. Evaluation of diffusion parameters and T2 values of the masseter muscle during jaw opening, clenching, and rest. Acta Radiol. 2012;53:81–86. doi: 10.1258/ar.2011.110136. [DOI] [PubMed] [Google Scholar]
- 37.Gotoh A., Ariji Y., Hasegawa T., Nakayama M., Kise Y., Matsuoka M. Sonographic elastography for assessing changes in the masseter muscle elasticity after low-level static contraction. Oral Radiol. 2013;29:140–145. [Google Scholar]
- 38.Ariji Y., Nakayama M., Taguchi A., Gotoh A., Kise Y., Katsumata A. Intramuscular changes of soft and hard areas after low-level static contraction of the masseter muscle and the correlations with muscle hardness and increase in water content: evaluations with sonographic elastography and magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:354–361. doi: 10.1016/j.oooo.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 39.Ariji E., Ariji Y., Yoshiura K., Kimura S., Horinouchi Y., Kanda S. Ultrasonographic evaluation of inflammatory changes in the masseter muscle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1994;78:797–801. doi: 10.1016/0030-4220(94)90098-1. [DOI] [PubMed] [Google Scholar]
- 40.Muro-Culebras A., Cuesta-Vargas A.I. Sono-myography and sono-myoelastography of the tender points of women with fibromyalgia. Ultrasound Med Biol. 2013;39:1951–1957. doi: 10.1016/j.ultrasmedbio.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 41.Lee S.Y., Park H.J., Choi Y.J., Choi S.H., Kook S.H., Rho M.H. Value of adding sonoelastography to conventional ultrasound in patients with congenital muscular torticollis. Pediatr Radiol. 2013;43:1566–1572. doi: 10.1007/s00247-013-2750-x. [DOI] [PubMed] [Google Scholar]
- 42.Kuo W.H., Jian D.W., Wang T.G., Wang Y.C. Neck muscle stiffness quantified by sonoelastography is correlated with body mass index and chronic neck pain symptoms. Ultrasound Med Biol. 2013;39:1356–1361. doi: 10.1016/j.ultrasmedbio.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 43.Botar Jid C., Vasilescu D., Damian L., Dumitriu D., Ciurea A., Dudea S.M. Musculoskeletal sonoelastography. Pictorial essay. Med Ultrason. 2012;14:239–245. [PubMed] [Google Scholar]
- 44.Nakashima K., Shiina T., Sakurai M., Enokido K., Endo T., Tsunoda H. JSUM ultrasound elastography practice guidelines: breast. J Med Ultrason. 2013;40:359–391. doi: 10.1007/s10396-013-0457-0. [DOI] [PubMed] [Google Scholar]
- 45.Yuasa H., Kino K., Kubota E., Kakudo K., Sugisaki M., Nishiyama A. Primary treatment of temporomandibular disorders: the Japanese Society for the temporomandibular joint evidence-based clinical practice guidelines. 2nd edition. Jpn Dent Sci Rev. 2013;49:89–98. [Google Scholar]
- 46.Türp J.C., Komine F., Hugger A. Efficacy of stabilization splints for the management of patients with masticatory muscle pain: a qualitative systematic review. Clin Oral Investig. 2004;8:179–195. doi: 10.1007/s00784-004-0265-4. [DOI] [PubMed] [Google Scholar]
- 47.Al-Ani M.Z., Davies S.J., Gray R.J., Sloan P., Glenny A.M. Stabilisation splint therapy for temporomandibular pain dysfunction syndrome. Cochrane Database Syst Rev. 2004;(1):CD002778. doi: 10.1002/14651858.CD002778.pub2. [DOI] [PubMed] [Google Scholar]
- 48.Gonzalez-Perez L.M., Infante-Cossio P., Granados-Nunez M., Urresti-Lopez F.J., Lopez-Martos R., Ruiz-Canela-Mendez P. Deep dry needling of trigger points located in the lateral pterygoid muscle: efficacy and safety of treatment for management of myofascial pain and temporomandibular dysfunction. Med Oral Patol Oral Cir Bucal. 2015;20:e326–e333. doi: 10.4317/medoral.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clark G.T., Baba K., McCreary C.P. Predicting the outcome of a physical medicine treatment for temporomandibular disorder patients. J Orofac Pain. 2009;23:221–229. [PubMed] [Google Scholar]
- 50.Cairns B.E. Pathophysiology of TMD pain – basic mechanisms and their implications for pharmacotherapy. J Oral Rehabil. 2010;37:391–410. doi: 10.1111/j.1365-2842.2010.02074.x. [DOI] [PubMed] [Google Scholar]
- 51.Gomes C.A., Politti F., Andrade D.V., de Sousa D.F., Herpich C.M., Dibai-Filho A.V. Effects of massage therapy and occlusal splint therapy on mandibular range of motion in individuals with temporomandibular disorder: a randomized clinical trial. J Manip Physiol Ther. 2014;37:164–169. doi: 10.1016/j.jmpt.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 52.De Laat A., Stappaerts K., Papy S. Counseling and physical therapy as treatment for myofascial pain of the masticatory system. J Orofac Pain. 2003;17:42–49. [PubMed] [Google Scholar]
- 53.Craane B., Dijkstra P.U., Stappaerts K., De Laat A. One-year evaluation of the effect of physical therapy for masticatory muscle pain: a randomized controlled trial. Eur J Pain. 2012;16:737–747. doi: 10.1002/j.1532-2149.2011.00038.x. [DOI] [PubMed] [Google Scholar]
- 54.Yang J.L., Chen S.Y., Hsieh C.L., Lin J.J. Effects and predictors of shoulder muscle massage for patients with posterior shoulder tightness. BMC Musculoskelet Disord. 2012;13:46. doi: 10.1186/1471-2474-13-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zheng Z., Wang J., Gao Q., Hou J., Ma L., Jiang C. Therapeutic evaluation of lumbar tender point deep massage for chronic non-specific low back pain. J Tradit Chin Med. 2012;32:534–537. doi: 10.1016/s0254-6272(13)60066-7. [DOI] [PubMed] [Google Scholar]
- 56.Hiraiwa Y., Ariji Y., Kise Y., Sakuma S., Kurita K., Ariji E. Efficacy of massage treatment technique in masseter muscle hardness: robotic experimental approach. Cranio. 2013;31:291–299. doi: 10.1179/crn.2013.31.4.007. [DOI] [PubMed] [Google Scholar]
- 57.Koga H., Usuda Y., Matsuno M., Ogura Y., Ishii H., Solis J. Proceeding 2004 IEEE. 2004. Development of oral rehabilitation robot for massage therapy; pp. 2492–2497. [Google Scholar]