Abstract
Background
The effects of therapeutic relationship (TR) in elder mental health are understudied. A greater understanding of TR in geriatric psychotherapy is particularly needed for treating late-life depression with executive dysfunction, which predicts poor response to antidepressant medication and presents unique clinical challenges.
Methods
Participants were older patients (N = 220) with major depression and executive dysfunction who received 12 weeks of problem-solving therapy or supportive therapy in a randomized control trial. Multilevel growth curve modeling and latent change scores were used to analyze TR dimensions of Understanding and Accepting at the patient level (individual patient ratings, N = 194) and therapist level (ratings of each therapist averaged across participants, N = 10).
Results
TR predicted reduction of depression in both treatment groups, while treatment × TR interactions were not significant. Patients treated by therapists with higher average Understanding (patient and therapist level) and Accepting (therapist level) ratings had greater decreases in depression. The patient level × therapist level interaction for Understanding approached statistical significance (p = .065), suggesting a synergistic effect on treatment outcome. Together, Understanding and Accepting predicted 21% of variance in depression level changes.
Limitations
TR was not assessed throughout the course of treatment (only after the first therapy session and at post-treatment) and did not include ratings from an objective evaluator.
Conclusions
Assessment of patient's experience of the TR and of therapist ability to foster Understanding and Accepting can play a significant role in the delivery of geriatric psychosocial interventions.
Keywords: therapeutic relationship, treatment outcomes, geriatrics, depression, growth curve modeling
The relationship between therapist and client is a central element in effective psychotherapy (Gelso, 2014; Horvath, Del Re, Fluckiger, and Symonds, 2011), accounting for a large amount of the variance (an estimated 20% to 27%) in outcome (Gelso, 2014; Hovarth, 2005). Therapeutic relationship (TR) has been defined as the feelings and attitudes that the counseling participants have toward one another and the manner in which those are expressed (Gelso, 2014). TR is a “pan-theoretical” change agent because it is applicable to any therapeutic approach (Markin, 2014). Therapists cultivate the TR by applying clear within-session procedures (Arnow et al., 2013) and behaving flexibly and honestly (Ackerman and Hilsenroth, 2003). Early TR variance predicts psychotherapy outcomes based on the impact of therapist skill (Baldwin, Wampold, and Imel, 2007), their implementation of specific techniques (Arnow et al., 2013), and the expectations of clients in therapy (Wampold and Budge, 2012).
Relative to the vast literature on TR in adults (e.g., Arnow et al., 2013; Zuroff et al., 2010), few studies have focused on its association with psychotherapy outcomes in elderly populations and those have produced mixed results. Gaston, Marmar, Gallagher, and Thompson (1991) found a significant association between TR and cognitive therapy outcomes for geriatric depression. In contrast, TR was not significantly related to outcome in a 16-week psychotherapy trial in a different sample of older patients (Beutler and Clarkin, 1990). Nevertheless, increasing patient age has been found to predict stronger TR among depressed outpatients (Arnow et al., 2013), suggesting the importance of focus on this factor in geriatric mental health. Negative preconceptions of TR may also be associated with older adults' low use of psychological services, as anticipated discomfort discussing personal problems with a mental health professional is a predominant predictor of not seeking treatment for late-life mood and anxiety disorders (Byers et al., 2012).
Over the past three decades, psychotherapy has been an increasingly studied treatment for geriatric depression (Blazer, 2003). Psychotherapy is a particularly important treatment option for older adults with executive dysfunction, which is commonly associated with late-life depression (Alexopoulos and Kelly, 2009). This is because executive dysfunction, a neuropsychological manifestation of frontal system impairment, has consistently been shown to predict poor response to antidepressants (Alexopoulos et al., 2004; Alexopoulos et al., 2005; Dunkin et al., 2000; Pimontel et al., 2012; Potter, Kittinger, Wagner, Steffens, and Krishnan, 2004). These patients often have a greater likelihood of psychomotor retardation, lack of insight into their illness, exacerbated disability, and impaired ability to apply adaptive coping strategies (Areán et al., 2010; Krapan et al., 2007).
Older adults with executive dysfunction may be well-suited for psychotherapies that either aim to directly address problem-solving deficits (e.g., problem-solving therapy, PST) or empathic understanding (e.g., supportive therapy, ST) and do not heavily rely on executive functions (Beaudreau et al., 2015). Both forms of treatment have been found to significantly reduce depression severity and lead to high response rates for these patients, with evidence of superiority for PST (Areán et al., 2010). The precise mechanisms related to PST and ST response remain unclear (Blazer, 2003; Kiosses et al., 2011). Recent studies have begun to identify clinical characteristics at baseline that are associated with depression outcomes (Beaudreau et al., 2015; Goodkind et al., 2016; Nelson et al., 2013). Less understood is the extent to which relationship-centered factors, such as the client's perception of the TR and the therapist's skill in fostering TR, predict psychotherapy response for geriatric depression.
Specific to older adults with depression and executive dysfunction, research demonstrating TR quality as a significant contributor to improved psychotherapy outcomes could help clinicians better recognize and treat the unique therapeutic challenges posed by these patients. Identifying patients who may be at risk for poor depression treatment outcomes based on initial assessments of TR may assist clinicians and administrators in providing the appropriate level of resources to meet specific patient needs. Such information could have important ramifications for practitioners' education and training in terms of prioritizing therapist skills and characteristics that cultivate TR. The importance of better understanding factors that influence the success of treatment for geriatric depression is underscored by the rapid growth of the elderly population and the increase and change in their mental health treatment needs (Hybels et al., 2009; Jeste et al., 1999).
The objective of the current study was to determine whether early perceptions of TR, based on individual patient ratings and aggregated ratings that reflect therapist skill (Baldwin et al., 2007), predict depression symptom reduction in response to psychotherapy. Previous research suggests that initial patient perceptions of the TR at the start of treatment may predict outcome better than assessments taken later (Hovarth, 2005). The strength of TR was measured by the multi-dimensional patient-report Client Perception of Therapist scale (CPTS; Lorr, 1965). We examined two CPTS subscales, Understanding and Accepting, to provide insight into specific mechanisms that might predict positive response to geriatric psychotherapy for those with executive deficits. Studying TR involves separating patient and therapist contributions (Baldwin et al., 2007), and their interaction (DeRubeis et al., 2005). Therefore, we used multilevel growth curve modeling to examine both therapist and patient contributions of Understanding and Accepting on change in depression throughout treatment. Given that therapeutic gains tend to parallel TR (Hovarth, 2005), a latent change score approach was also used to examine whether changes in the TR throughout treatment are associated with changes in depression.
This study analyzed data from a randomized control trial (Areán et al., 2010), which compared the efficacy of PST and ST for treating major depression in older adults with executive dysfunction. We tested four hypotheses: (1) Patient level Understanding and Accepting (i.e., individual patient perceptions of these aspects of TR) will be significantly associated with reductions in depression (i.e., higher TR leads to greater decreases). (2) Higher ratings of Understanding and Accepting, when averaged across all patients (i.e., therapist skill in fostering TR), will impact treatment response in a similar manner. (3) Therapist's ability to foster Understanding and Accepting at the beginning of treatment will interact with patient ratings of Understanding and Accepting (patient level) in predicting decreases in depression, such that high levels of both therapist and client ratings of TR will lead to the greatest decrease in depression. (4) We hypothesized that a treatment × TR interaction predicting that both Understanding and Accepting will be associated more strongly with decreases in depression in PST relative to ST. This was based on recent evidence for a robust TR-outcome association in cognitive-behavioral modalities, suggesting that greater structure contributes to perceptions of therapist competence (Arnow et al., 2103).
Methods
Participants
Participants from the Areán et al. (2010) study were community-dwelling older adults prospectively recruited (12/02 to 11/07) through radio or internet advertisements, senior center and healthcare provider referrals, and community talks. All participants completed written informed consent after receiving a complete description of the study.
Study inclusion criteria required a minimum age of 60, DSM-IV diagnosis of major depressive disorder, a Mini-Mental Status Exam (MMSE; Folstein et al., 1975) score ≥ 24 (to determine a lack of global cognitive impairment or dementia), Initiation/Perseveration subscale of the Mattis Dementia Rating Scale (Mattis, 1988) score < 33, and Stroop Color Word Test (Perret, 1974) scores < 25. The MMSE was chosen because it has documented reliability and validity in older adults, is widely used, and provides a recommended cutoff for determining a lack of global cognitive impairment (Sheehan, 2012). The Initiation/Perseveration and Stroop Color Word Test cutoffs were selected based on their ability to identify executive dysfunction in late-life depression and the correlation of low scores on these measures with poor response to antidepressant medication (Alexopoulos et al., 2005).
Individuals were excluded if they had a severe medical illness (e.g., metastatic cancer), were taking drugs that increase risk for depression (e.g., steroids), required maximum assistance in performing one or more activities of daily living even with assistance (walking with a cane would not constitute as ineligibility), were receiving psychological or pharmacological interventions for depression outside of the study protocol, expressed active suicidal ideation, had a DSM-IV Axis I diagnosis besides generalized anxiety disorder, were current substance abusers, had dementia (MMSE scores < 24 or a DSM-IV diagnosis of dementia), or had a history of head trauma (see Areán et al., 2010 for full criteria). In sum, participants met criteria for major depressive disorder and experienced executive dysfunction in the absence of global dementia.
Two hundred twenty participants were randomized into ST (n = 112) or PST (n = 108) through parallel assignment using random numbers in blocks of five participants at each site (for the participant flow diagram see Areán et al., 2010, p. 1392). Table 1 presents descriptive statistics of participant demographics and clinical characteristics by treatment group. The final sample consisted of 194 (88%) of the intention-to-treat sample who have TR data. Participants without TR data (n = 26) did not significantly differ from those in the final sample on demographic variables of depression severity (p > .05). The use of multilevel growth curve modeling allowed us to include the entire intention-to-treat sample. Participant attrition (n = 35), did not significantly differ by condition. Understanding and Accepting scores were not significantly different between participants who completed treatment and non-completers (ps > .05).
Table 1. Select Demographics and Clinical Characteristics.
| Supportive Therapy (n = 112) | Problem-solving Therapy (n = 108) | p | |
|---|---|---|---|
| Age | 73.16 (SD = 7.93) | 72.77 (SD = 7.57) | .71 |
| Gender | Male (42.9%) | Male (25.9%) | .01* |
| Female (57.1%) | Female (74.1%) | ||
| Race | White (84.8%) | White (89.8%) | .45 |
| Black (9.8%) | Black (4.6%) | ||
| Asian (3.6%) | Asian (4.6%) | ||
| Other (1.8%) | Other (0.9%) | ||
| Ethnicity | Non-Hispanic (95.5%) | Non-Hispanic (90.7%) | .09 |
| Hispanic (3.6%) | Hispanic (9.3%) | ||
| Education | 15.51 years (SD = 2.96) | 14.97 years (SD = 2.59) | .16 |
| Age of depression onset | 53.26 (SD = 23.64, range = 8-86) | 58.33 (SD = 20.92, range = 12-86) | .51 |
| Total depressive episodes | 2.34 (SD = 1.59, range = 1-7) | 2.12 (SD = 2.69, range = 1-25) | .16 |
| Depression | 24.45 (SD = 4.58, range = 19-37) | 24.07 (SD = 3.93, range = 18-40) | .42 |
| Understanding | 36.10 (SD = 5.07, range = 25-45) | 36.91 (SD = 5.07, range = 18-45) | .30 |
| Accepting | 46.18 (SD = 7.72, range = 24-60) | 46.31 (SD = 8.24, range = 13-60) | .91 |
Note.
p < .05.
Depression was measured by the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960). The therapeutic relationship (TR) was assessed by the Understanding and Accepting subscales of the Client Perception of Therapist Scale (CPTS; Lorr, 1965).
Therapists
Therapists consisted of four doctoral-level clinical psychologists and four licensed social workers with at least five years of post-licensure experience who were trained in both therapies (Areán et al., 2010 p. 1393). To control for potential bias from providing both treatments, all therapists attended an extensive two-day training workshop, were closely supervised on three practice cases for both treatments, and were monitored on randomly selected audiotapes by independent experts using standardized adherence scales for PST and ST (Areán et al., 2010). Each therapist treated an average of 22.00 (SD = 23.10) participants, ranging between 1 to 64. Most therapists treated approximately the same number of participants from each group (M = 52% ST clients). In response to an overflow of participants at one point during treatment, two additional doctoral-level clinical psychologists who were experts in PST and ST provided treatment to one participant each, making a total of ten therapists. Social workers and psychologists were distributed evenly between treatment conditions.
Procedure
All procedures were approved by the institutional review boards of both study sites: Weill Cornell Medical College and the University of California at San Francisco (Areán et al., 2010). Therapy consisted of 12 weekly individual sessions of either PST or ST. PST focused on reducing stress and helping patients develop greater self-efficacy in confronting and resolving issues in their lives to allay depression (Areán et al., 2010). In PST, “participants set treatment goals, discuss and evaluate different ways to reach goals, create action plans, and evaluate their effectiveness in reaching goals” (Areán et al., 2010, p. 1393). In ST, a manualized (Sachs, 2000) person-centered psychotherapy, “Therapists create a comfortable, nonjudgmental environment by demonstrating genuineness, empathy, and acceptance without imposing any judgments on their decisions” (Areán et al., 2010, p. 1394). In contrast with PST, ST therapists encourage patients to resolve issues through active listening instead of providing direct input. Therapists were aware of participants' randomization status for treatment purposes but not the study hypotheses.
Research assistants, who were blind to treatment assignment and trained under the supervision of clinical psychologists, conducted the assessments. Depression was assessed by the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960) at baseline (Week 0), just before each therapy session (Weeks 1-12), and at follow-up (Week 24 and 36). The CPTS was administered immediately after the first therapy session (Week 1) and just before the last session (Week 12). Participants were compensated for research assessments, but not for therapy sessions.
Measures
Client Perception of Therapist Scale (CPTS)
Lorr (1965) developed the CPTS as a multi-dimensional measure of the client's perception of: (1) the therapist's ability to communicate and understand, (2) emotional distance, and (3) therapist status (superior, equal, subordinate). The CPTS contains Likert ratings of perceived therapist qualities ranging from 1-5, with a score of 1 indicating “Not at All True” and a score of 5 indicating “Extremely True.” Greater scores indicate a more positive impression of the therapist. Each item also includes the response options of 6 or 7 for “Refused” and “Don't know”, respectively.
This investigation focused on the CPTS dimensions of Understanding and Accepting because both have demonstrated the strongest association with patient improvement (Cooley and Lajoy, 1980) and make positive contributions to TR (Ackerman and Hilsenroth, 2003). The 9-item Understanding subscale denotes patient perceptions of the degree to which therapists grasp emotional and cognitive components of patients' experience. For example, participants are asked to rate the extent to which their therapist “Seems to understand how I feel” and “Makes comments that are right in line with what I am saying”. The 12-item Accepting subscale reflects patient perceptions of therapists' attitudes of “interest” and “nurturance” towards patients. Example items include: “Seems to have a real respect for me” and “Makes me feel free to say whatever I think”. Understanding and Accepting have demonstrated concurrent and predictive validity on assessments of therapy satisfaction and on assessments of patient improvement (Cooley and Lajoy, 1980; Lorr, 1965). In this sample, the internal consistency reliability as estimated by Cronbach's alpha was strong for both Understanding (Week 1 = .90, Week 12 = .80) and Accepting (Week 1 = .92, Week 12 = .90).
Severity of Depression
The 24-item version of the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960) was used to measure changes in depression in response to treatment. Items are rated either on a 0-2 or 0-4 point scale (total = 0-76), with greater scores indicating higher severity of depression. HRSD cut scores indicate no (≤ 9), mild (10-19), moderate (20-29), or severe depression (≥ 30). In a large-scale reliability meta-analysis, the HRSD demonstrated adequate inter-rater reliability, test-retest reliability, and internal consistency reliability (Trajković et al., 2011). The HRSD has also been found to be comparable to other commonly used measures for assessing changes in depression among older adults (Heo et al., 2007).
Executive Dysfunction
Data from the Initiation/Perseveration subscale of the Dementia Rating Scale and the Stroop Color Word Test, which were used as eligibility criteria, and the Trail Making Test - Part B (Reitan, 1955) were analyzed to examine if they influenced TR.
Data Analyses
Piecewise multilevel growth curve modeling examined hypotheses regarding change over time in depression (Singer and Willett, 2003). Piecewise growth curve modeling breaks an overall trajectory into separate components. It is increasingly being used to analyze change in outcomes during treatment and follow-up periods of randomized control trials in one model. Multilevel growth curve modeling, conducted in HLM (Version 7.01; Raudenbush et al., 2013), allowed us to examine both therapist and patient level effects of Understanding and Accepting. This study used a three level model with repeated assessments of depression (Model Level 1), nested within patients (Model Level 2), which were in turn nested within therapists (Model Level 3).
Time was modeled as the number of weeks since baseline assessment. Piecewise modeling estimated different slopes from pre- to post-treatment (epoch 1) and post-treatment to long-term follow-up (epoch 2) (Singer and Willett, 2003). Two time variables were entered into the model: (1) the number of weeks (or natural log of number of weeks to test non-linear models) coded as zero at baseline and number of weeks since baseline for each subsequent assessment, and (2) the number of weeks since post-treatment with all assessments from pre-treatment to post-treatment coded as zero and the first and second follow-up assessments coded as 12 and 24, respectively. This model produced three estimates: (1) intercept, representing baseline HRSD scores with time at baseline coded as zero, (2) change during treatment, and (3) the difference in rate of change between treatment and post-treatment.
Understanding and Accepting were added as predictors of each depression change parameter (in separate models). We evaluated a series of models for both TR dimensions (separately). First, we examined patient level (Model Level 2) therapeutic effects by including Understanding and Accepting for each patient as a Model Level 2 predictor of the change parameters. Second, we examined therapist level (Model Level 3) effects by including average Understanding and Accepting across patients, based on the approach taken by Baldwin et al. (2007), for each therapist as a Model Level 3 predictor of the change parameters. Third, we examined therapist and patient level effects simultaneously by including both therapist (Model Level 3) and patient (Model Level 2) Understanding and Accepting scores as predictors of change scores in the same model.
The latent change score approach described by McArdle (2009) using the MPlus software package (Version 7; Muthén and Muthén, 2012) allowed us to examine the relationship between change in depression, as estimated by the multilevel piecewise growth curve modeling described above, and change in TR scores modeled as latent change scores. The first set of latent change score models estimated change in TR scores for each treatment group separately and tested the treatment condition × time interaction by including a dummy coded treatment condition as a predictor of Week 1 Understanding and Accepting scores and the latent change score. The second set of latent change score analyses examined the association between change in Understanding and Accepting and change in depression. These analyses were conducted separately for the two conditions to explore possible treatment condition differences. Therapist level effects could not be accounted for in these final analyses due to a lack of convergence.
Results
Descriptive statistics by treatment group for the measures and participant variables are presented in Table 1. Understanding (M = 36.48, SD = 5.33, range = 18-45) and Accepting (M = 46.24, SD = 7.95, range = 13-60) scores were normally distributed. Average TR ratings for each therapist ranged from 26.00 to 37.91 for Understanding and from 38.00 to 51.18 for Accepting.
Several preliminary analyses were conducted to examine the relationship between participant variables and study measures. At baseline, Understanding was significantly associated with Accepting (r = .73, p < .001) and HRSD scores (r = -.16, p = .03). Accepting was not significantly associated with HRSD scores at the start of treatment (r = -.13, p = .08), but had a weak association with age (r = .159, p = .029). African-American participants (M = 39.37, SD = 5.32) rated their therapists as more Understanding than Caucasian participants (M = 36.23, SD = 5.32; F (1,183) = 2.51, p =.032). Understanding and Accepting were not significantly associated with gender, marital status, ethnicity, education, number of depressive episodes, or Mini-Mental Status Exam scores (ps > .10). The proportion of male and female participants were significantly different between the ST and PST groups, χ² (1, 220) = 6.97, p = .01. However, gender was not systematically related to HRSD at any assessment period (ps > .05). Finally, none of the executive dysfunction measures significantly predicted Understanding (R2 = .04, F (3, 156) = .49, p = .69) or Accepting (R2 = .01, F (3, 154) = .46, p = .71) in separate regression analyses. Thus, the participant variables and executive dysfunction measures were not considered further in statistical modeling as a result of the pre-analysis.
Prior to examining Understanding and Accepting as predictors of depression in response to treatment, multiple unconditional change models were evaluated to determine the optimal method for modeling HRSD scores over time. A non-linear piecewise model fit the data best and accounted for 51% of the within-subjects variance in HRSD scores. This pattern of change was characterized by strong initial decreases in depression during the beginning of treatment that flattened out over time with no significant change during the follow-up period. The Analysis 1 section of Table 2 presents the regression coefficients for this model, and the solid black line in Figure 1 depicts this pattern of change. As depicted in Figure 1, the follow-up period data are not reported on further, as it added little after consideration of treatment phase data.
Table 2. Regression Coefficients and Effects Sizes for Piecewise Growth Curve Models.
| Baseline Assessment | Change During Treatment | |||||||
|---|---|---|---|---|---|---|---|---|
| (Analysis #) Model | b | (95% CI) | t | d | b | (95% CI) | t | d |
| (1) Entire Sample | 24.7 5* | (23.09, 26.39) | 29. 42 | 19. 61 | -3.82* | (-4.22, -3.42) | -18.68 | -12.54 |
| (2) TR (Patient Level) × Time | ||||||||
| (3a) Understanding | -0.02 | (-0.21, 0.17) | -0.21 | -.02 | -0.12* | (-0.2, -0.04) | -2.87 | -.30 |
| (3b) Accepting | -0.07 | (-0.19, 0.06) | -1.07 | -.11 | -0.02 | (-0.08, 0.03) | -0.79 | -.08 |
| (3) TR (Therapists Level) × Time | ||||||||
| (2a) Understanding | -0.72 | (-1.49, 0.05) | -1.82 | -.19 | -0.34* | (-0.62, -0.06) | -2.40 | -.25 |
| (2b) Accepting | -0.24 | (-0.81, 0.33) | -0.84 | -.09 | -0.26* | (-0.47, -0.05) | -2.39 | -.25 |
| (4) TR (Therapist and Patient Level; main effects) × Time | ||||||||
| (4a) Understanding (Therapist) | -0.2 | (-0.95, 0.56) | -0.51 | -.05 | -0.32 | (-0.6, -0.03) | -2.15 | -.22 |
| (4a) Understanding (Patient) | -0.03 | (-0.22, 0.16) | -0.30 | -.03 | -0.1* | (-0.18, -0.02) | -2.35 | -.24 |
| (4b) Accepting (Therapist) | 0.21 | (-0.36, 0.79) | 0.7 2 | .07 | -0.32* | (-0.54, -0.1) | -2.82 | -.29 |
| (4b) Accepting (Patient) | -0.08 | (-0.19, 0.04) | -1.31 | -.14 | -0.01 | (-0.07, 0.05) | -0.24 | -.02 |
| (5) TR (Therapist and Patient Level; interaction) × Time | ||||||||
| (5a) Understanding (Therapist × Patient) | 0.13* | (0.05, 0.2) | 3.2 8 | .34 | -0.05 | (-0.09, 0) | -2.13 | -.22 |
| (5b) Accepting (Therapist × Patient) | 0.07* | (0.02, 0.11) | 2.7 9 | .29 | -0.02 | (-0.05, 0.01) | -1.47 | -.15 |
Note.
= p < .05;
TR = therapeutic relationship (Client Perception of Therapist Scale; Lorr, 1965); b = unstandardized regression coefficient; d = Cohen's d , .25, .50, and .80 for small, medium, and large effect sizes respectively (Cohen, 1988). For the TR × Time interactions, only the interaction terms are presented (the main effects were included in the model; however, only the coefficients for TR domains predicting the time parameters are displayed for brevity). Similarly, only the TR × Condition × Time coefficients are reported for the TR × Condition interactions despite including all main effects and two way interactions in the model.
Figure 1.
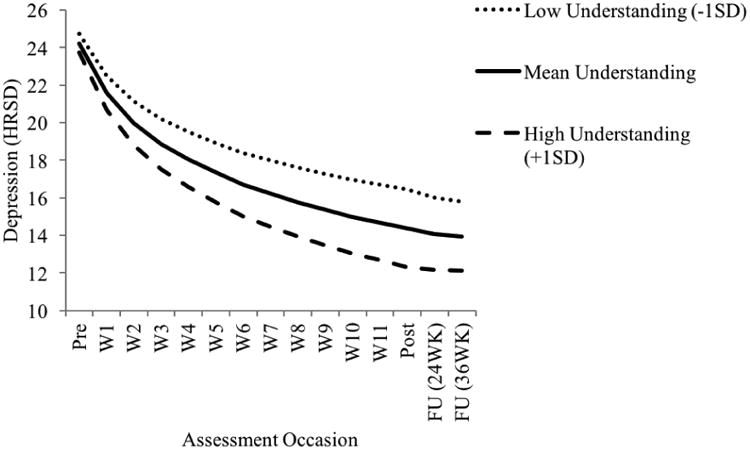
Depression trajectories as a function of Week 1 Client Perception of Therapist Scale (CPTS; Lorr, 1965) Understanding subscale levels. Depression was measured by the Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960). Pre = Pre-treatment session, W1-W11 = treatment session assessments, post = post-treatment, FU = follow-up, WK = week.
Hypothesis Testing
Table 2 presents the estimates of Understanding and Accepting predicting each of the depression change parameters at the baseline assessment and during the treatment period.7 Table 3 presents the percentage of variance in change in depression during treatment accounted for by Understanding and Accepting.
Table 3. Amount of Variance Accounted for (R2) in Change in Depression During Treatment by TR domain.
| TR domain | Patient level | Therapist level | Combined | Interaction |
|---|---|---|---|---|
| Understanding | .081* | .064* | .118 | 0.147* |
| Accepting | .016 | .052* | .057 | .073 |
Note.
= p < .05.
TR = therapeutic relationship (Client Perception of Therapist Scale; Lorr, 1965). All values are variance accounted for (R2) estimates or reduction of variance in change in depression during treatment when the predictor(s) was (were) added to the model.
At the patient level (Model Level 2), Understanding significantly predicted change in depression during treatment (Table 2, Analysis #2). Consistent with the first hypothesis, patients who reported high levels of Understanding by their therapists at Week 1 exhibited significantly larger decreases in depression during treatment than patients reporting low levels of Understanding (d = -.30). In contrast, Accepting did not significantly predict change in depression at the patient level.
At the therapist level (Model Level 3), Understanding (d = -.25) and Accepting (d = -.25) were significantly associated with change in depression during treatment, consistent with hypothesis two (Table 2, Analysis #3). Patients who were treated by therapists with high average Understanding ratings exhibited greater decreases in depression compared to therapists with low average Understanding ratings. This therapist level effect was also found for Accepting. Figure 1 illustrates this effect for Understanding (and not Accepting) for brevity.
The coefficients for TR dimensions × time interactions when including Understanding and Accepting scores at both the therapist and patient level are depicted in the Analysis #4 section of Table 2. When examined simultaneously, the coefficient for the time × Understanding interaction at the patient level remained statistically significant (p = .043, d = -.24), but fell just below the p < .05 threshold at the therapist level (p = .063, d = -.22). However, given the almost identical effect size estimates and the relatively small number of therapists, the most prudent interpretation of this finding is that Understanding demonstrated a small but potentially meaningful effect on change in depression during treatment at both the patient and therapist level. For Accepting, including both patient and therapist effects in the same model did not impact the results as only the therapist level effect of Accepting remained significant (p = .012, d = -.29).
For Understanding, a patient level × therapist level × time three-way interaction (Table 2, Analysis #5) approached statistical significance (p = .065, d = -.22). Given the difficulty in detecting interactions (McClelland and Judd, 1993), particularly a three-way cross level interaction that accounts for an additional three percent of the variance in change in depression during treatment, we contend that it is worthy of consideration. Visual inspection of this interaction reveals the largest decrease in depression was exhibited by patients who rated their therapists as high in Understanding and who were treated by therapists whose patients on average rated them high on Understanding, consistent with hypothesis three. This suggests that there is a synergistic effect between rating of Understanding by patients and therapist skill in fostering Understanding.8
Table 4 depicts the estimates derived from the latent change score analyses. Both treatment conditions exhibited statistically significant increases in Understanding and Accepting from Week 1 to Week 12. The last column of Table 4 summarizes the results of the multivariate change models estimating the association between change in depression and change in the TR dimensions during treatment. The association between change in Understanding and change in depression was negative (r = -.12) approached statistical significance (p = .070) indicating a trend for increases in Understanding to be associated with decreases in depression. Evidence for hypothesis four was not found as the overlap among the 95% intervals suggested that association between changes in Understanding and Accepting and depression did not significantly differ between the two conditions.
Table 4. Summary of the Latent Change Score Models Evaluating Change in TR domain from Week 1 to Week 12.
| TR domain | Week 1 | Week 12 | Latent Change | rz with Δ Depression | ||
|---|---|---|---|---|---|---|
| Condition/Effect | Estimate (95% CI) | Estimate (95% CI) | Estimate (95% CI) | d | Condition | r (95% CI) |
| Understanding | Overal l | -.12 (-.25, .01)a | ||||
| ST | 36.04 (35.02, 37.06) | 38.03 (37.04, 39.02) | 1.99 (0.78, 3.19)* | 0.37 | ST | -.06 (-.20, .11) |
| PST | 37.00 (35.89, 38.10) | 39.69 (38.64, 40.74) | 2.70 (1.39, 4.00)* | 0.51 | PST | -.15 (-.34, .04) |
| TX Difference | 0.95 (-0.55, 2.46) | 1.66 (0.22, 3.11)* | 0.71 (-1.07, 2.49) | 0.13 | ||
| Tx Difference (res. Δ) | 0.95 (-0.55, 2.46) | 0.18 | ||||
| Accepting | Overal l | -.09 (-.22, .04) | ||||
| ST | 46.04 (44.49, 47.59) | 48.8 (47.28, 50.32) | 2.76 (1.10, 4.42)* | 0.35 | ST | -.01 (-.17, .15) |
| PST | 46.59 (44.95, 48.22) | 50.65 (49.04, 52.25) | 4.06 (2.28, 5.84)* | 0.51 | PST | -.14 (-.34, .06) |
| TX Difference | 0.55 (-1.71, 2.80) | 1.85 (-0.37, 4.06) | 1.3 (-1.14, 3.74) | 0.16 | ||
| Tx Difference (res. Δ) | 1.6 (-0.43, 3.63) | 0.20 | ||||
Note.
= p < .05,
= p = .07.
TR = therapeutic relationship (Client Perception of Therapist Scale; Lorr, 1965). Tx (Treatment) Difference denotes estimates when evaluating the raw change score. Tx Difference (res. Δ) denotes the results of examining treatment conditions in change when controlling for Week 1 scores. CI = Confidence Interval; d = Cohen's d . .
Post-hoc Analysis
To understand the overall effect size of the significant TR domains on outcome, we entered Understanding and Accepting simultaneously and found they predict 21% of the variance in depression level changes.
Discussion
The principal finding of this study is that patient perception of TR, and therapist skill in engendering TR, significantly predicted reduction of geriatric depression. Understanding and Accepting predicted 21% of the variance in depression level changes, which aligns with the variance in psychotherapy outcomes accounted for by TR in non-geriatric samples (Gelso, 2014; Horvath et al., 2011). While negative preconceptions might impact treatment seeking among the elderly (Byers et al., 2012), it apparently does not undermine the robustness of the TR itself once the process has begun. Latent change score results correspond with conclusions from meta-analyses that the strength of TR is independent of treatment modality (Flückiger, et al., 2012; Horvath, et al., 2011; Martin et al., 2000). TR assessment preceded all but the first therapy session, indicating that TR exerted influence on therapy outcome rather than being a function of that outcome (Barber et al., 2000; DeRubeis et al., 2005). The use of multilevel growth curve modeling, which allowed us to explore the effects of patients and therapists simultaneously, addressed methodological and conceptual concerns raised in this literature (Crits-Christoph et al., 2011; DeRubeis et al., 2005).
Geriatric Depression
This is the first study to demonstrate an effect of TR on the efficacy of psychotherapy in depressed older adults with executive dysfunctions. Our findings are consistent with a previous investigation of depressed older adults who were not selected for the presence of executive dysfunction (Gaston et al., 1991). As in our study, participant perception of the quality of the therapeutic alliance was a predictor of response to cognitive therapy. However, therapeutic alliance assessed with a modified version of the Systematic Treatment Selection Framework (Beutler and Clarkin, 1990) did not predict outcomes throughout a 16-week psychotherapy trial in a different sample of older patients. Methodological differences may explain these divergent findings. Gaston et al. (1991) and our study investigated geriatric depression severity, while Beutler and Clarkin (1990) examined patient-rated distress level and quality of life.
Our findings suggest that therapists of depressed older adults should actively monitor their contribution to TR (e.g., Baldwin et al., 2007; Norcross, 2010), and clinics should provide feedback to therapists about TR formation. Educators in elder mental health should focus on therapist characteristics (e.g., honesty, respectfulness, warmth) and techniques (e.g., exploration, reflection, accurate interpretation) known to positively contribute to TR (Ackerman and Hilsenroth, 2003). Specific to older patients who have depression and executive dysfunction, forming a TR ultimately rests upon establishing structure, clarity, and consistency (Campbell et al., 1994). An emphasis should be placed on assessing both patient perceptions of TR and the therapist ability to foster TR. The current study underscores the importance of explicitly monitoring and integrating client and relationship-centered concepts (Sachs, 2000) into the delivery of skills-based approaches (Areán et al., 2010).
Treatment Mechanisms
This investigation of TR took place in the context of a clinical trial in which PST was found to be more effective than ST (Areán et al., 2010). Recent studies have also demonstrated a robust association between therapeutic alliance and outcomes in cognitive behavioral modalities, such as PST (Arnow et al., 2103). For this reason, we predicted that TR would be more robust in PST than ST. Instead, the relationship-centered value of the client's perception of therapist grasp on the client's situation, and therapist skill in fostering both Understanding and Accepting, predicted the outcome of depressive symptoms regardless of treatment modality. Understanding and Accepting are efficacious factors operating across treatment modalities as they influenced outcome despite therapeutic and technical differences (Krupnick et al., 1996; Markin, 2014; Wolfe and Goldfried, 1988).
A potential mechanism accounting for the robust association of TR and outcome of depression is that individuals in both treatment groups received a lot of support and validation throughout psychotherapy perhaps because of their executive dysfunction. In PST, the TR-outcome association may be related to robust within-session procedures, an increased sense of encouragement, and an expert-orientation. For ST, therapists' support, enablement, and empowerment of clients in making their own life decisions could have contributed to the TR-outcome association. We did not find a significant association between executive function and patients' ratings of Understanding and Accepting in this sample. However, future research is needed to investigate whether more robust assessments (e.g., longitudinal designs and objective ratings) or other patient populations would evidence executive function as a predictor of TR.
Higher Understanding (patient and therapist level) and Accepting (therapist level) ratings resulted in significantly greater decreases in depression. This finding is consistent with previous studies which demonstrated that Understanding and Accepting are meaningfully related to outcome in non-elderly patients (Cooley and Lajoy, 1980; Lorr, 1965). Understanding and Accepting may have exerted their influence by promoting social connection and creation of positive expectations, factors common to PST and ST (Wampold and Budge, 2012). Our observations suggest that the interaction of therapist skill and patient perception is a significant source of variance in psychotherapy outcome (Baldwin et al., 2007; DeRubeis et al., 2005). The Understanding subscale may be an especially important component of the early TR because it likely involves the therapist-client exchange and agreement on tasks and goals, which has been found to predict outcome at both early and late points in cognitive therapy for depression (Webb et al., 2011). The quality of the communication and empathy perceived by patients, as denoted by the Understanding subscale, should be carefully attended to by therapists working with older adults with depression and executive dysfunction.
Limitations
Several study limitations are worth noting. First, the CPTS was developed prior to Bordin's (1979) model that serves as the basis of widely used, present-day measures of TR (e.g., Working Alliance Inventory; Horvath and Greenberg, 1994). Nevertheless, this study demonstrated that the CPTS is a viable measure of TR domains for predicting psychotherapy outcomes. Second, the CPTS was only administered early in treatment and at post-treatment but not during the course of treatment as in other investigations (e.g., Barber et al., 2000; Krupnick et al., 1996). While initial patient perceptions may be a stronger predictor of the outcome of depression than assessments taken later (Hovarth, 2005), future research should assess TR multiple times during treatment. This would allow for a more nuanced investigation of the developing TR as a mediator of treatment outcome and allow for aggregation across sessions to increase measurement dependability (Crits-Christoph et al., 2011). Additionally, only patient level effects (and not therapist level effects) converged in the latent change score examining the TR as a psychotherapy outcome. Third, we were unable to include assessments of TR by an objective evaluator. Therapist level ratings were computed by aggregating TR ratings across patients to control for effects of idiosyncratic individual patient ratings (Baldwin et al., 2007). A more comprehensive investigation of therapist level effects should include TR ratings from an objective rater. Finally, our sample consisted of predominately Caucasian and highly educated participants, making it difficult to generalize our findings to more diverse patients with geriatric depression.
Despite these limitations, our findings underscore the importance of TR in psychotherapy for older adults. The identification of understanding and accepting as significant qualities of the early TR, impacting treatment outcome across different types of psychotherapy, can inform the development and implementation of successful treatments for geriatric depression with executive dysfunction.
Highlights.
Therapeutic relationship (TR) is an important factor in treating elder depression.
TR predicted reduction of depression in both psychotherapy treatment groups.
The influence of TR was affected by patient and therapist contribution levels.
Higher TR (Understanding and Accepting) let to greater decreases in depression.
Understanding and Accepting predicted 21% of variance in depression level changes.
Footnotes
For all models, the main effects of Time and TR were included. We only report estimates for the Time × TR interactions to facilitate interpretability and because our main hypotheses involved examining the impact of Understanding and Accepting on change over time.
For brevity and readability, the full results of the treatment condition × TR or follow-up analyses are not presented but can be obtained from the corresponding author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ackerman SJ, Hilsenroth MJ. A review of therapist characteristics and techniques positively impacting the TA. Clin Psychol Rev. 2003;23:1–33. doi: 10.1016/S0272-7358(02)00146-0. [DOI] [PubMed] [Google Scholar]
- Alexopoulos G, Kelly RE., Jr Research advances in geriatric depression. World Psychiatry. 2009;8:140–149. doi: 10.1002/j.2051-5545.2009.tb00234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexopoulos G, Kiosses DN, Heo M, Murphy CF, Shanmugham B, Gunning-Dixon F. Executive dysfunction and the course of geriatric depression. Biol Psychiat. 2005;58:204–210. doi: 10.1016/j.biopsych.2005.04.024. [DOI] [PubMed] [Google Scholar]
- Alexopoulos G, Kiosses DN, Murphy C, Heo M. Executive dysfunction, heart disease burden, and remission of geriatric depression. Neuropsychopharmacology. 2004;29:2278–2284. doi: 10.1038/sj.npp.1300557. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Meyers BS, Young RC, Kalayam B, Kakuma T, Gabriele M, Sirey JA, Hull J. Executive dysfunction and long-term outcomes of geriatric depression. Arch Gen Psychiat. 2000;57:285–290. doi: 10.1001/archpsyc.57.3.285. [DOI] [PubMed] [Google Scholar]
- Areán PA, Raue P, Mackin S, Kanellopoulos D, McCulloch C, Alexopoulos GS. Problem Solving therapy and supportive therapy ST in older adults with major depression and executive dysfunction. Am J Psychiat. 2010;167:1391–1398. doi: 10.1176/appi.ajp.2010.09091327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnow BA, Steidtmann D, Blasey C, Manber R, Constantino MJ, Klein DN, Markowitz JC, Rothbaum BO, Thase ME, Fisher AJ, Kocsis JH. The Relationship Between the Therapeutic Alliance and Treatment Outcome in Two Distinct Therapies for Chronic Depression. J Consult Clin Psych. 2013;81:627–638. doi: 10.1037/a0031530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin SA, Wampold BE, Imel ZE. Untangling the Alliance-Outcome Correlation: Exploring the Relative Importance of Therapist and Patient Variability in the Alliance. J Consult Clin Psych. 2007;75:842–852. doi: 10.1037/0022-006X.75.6.842. [DOI] [PubMed] [Google Scholar]
- Barber JP, Connolly MB, Crits-Christoph P, Gladis L, Siqueland L. Alliance Predicts Patients Outcome Beyond In-treatment Change in Symptoms. J Consult Clin Psych. 2000;68:1027–1032. doi: 10.1037/0022-006X.68.6.1027. [DOI] [PubMed] [Google Scholar]
- Beaudreau SA, Rideaux T, O'Hara R, Areán P. Does cognition predict treatment response and remission in psychotherapy for late-life depression? Am J Geriat Psychiat. 2015;23:215–219. doi: 10.1016/j.jagp.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beutler LE, Clarkin JF. Systematic treatment selection: Toward targeted interventions. Philadelphia, PA: Brunner/Mazel; 1990. [Google Scholar]
- Blazer DG. Depression in Late Life: Review and Commentary. J Gerontol A Biol Sci Med Sci. 2003;58A:249–265. doi: 10.1093/gerona/58.3.M249. [DOI] [PubMed] [Google Scholar]
- Bordin E. The generalizability of the psychoanalytic concept of the working alliance. Psychol Psychother T. 1979;16:252–260. [Google Scholar]
- Byers AL, Areán PA, Yaffe K. Low Use of Mental Health Services among Older Americans with Mood and Anxiety Disorders. Psychiat Serv. 2012;63:66–72. doi: 10.1176/appi.ps.201100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JJ, Duffy JD, Salloway SP. Treatment Strategies for Patients with Dysexecutive Syndromes. J Neuropsych Clin N. 1994;6:411–418. doi: 10.1176/jnp.6.4.411. [DOI] [PubMed] [Google Scholar]
- Cooley EJ, Lajoy R. Therapeutic relationship and improvement as perceived by clients and their therapists. J Clin Psychol. 1980;36:562–570. doi: 10.1002/jclp.6120360230. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Gibbons MBC, Hamilton J, Ring-Kurtz S, Gallop R. The Dependability of Alliance Assessments: The Alliance-Outcome Correlation is Larger Than You Might Think. J Consult Clin Psych. 2011;79:267–278. doi: 10.1037/a0023668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRubeis RJ, Brotman MA, Gibbons CJ. A conceptual and methodological analysis of the nonspecific argument. Clin Psychol Sci Pract. 2005;12:174–183. doi: 10.1093/clipsy.bpi022. [DOI] [Google Scholar]
- Dunkin JJ, Leuchter AF, Cook IA, Kasl-Godley JE, Abrams M, Rosenberg-Thompson S. Executive dysfunction predicts nonresponse to fluoxetine in major depression. J Affect Disorders. 2000;60:13–23. doi: 10.1016/S0165-0327(99)00157-3. [DOI] [PubMed] [Google Scholar]
- Flückiger C, Del Re AC, Wampold BE, Symonds D, Horvath AO. How central is the alliance in psychotherapy: A multilevel longitudinal meta-analysis. J Couns Psychol. 2012;59:10–17. doi: 10.1037/a0025749. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gaston L, Marmar CR, Gallagher D, Thompson L. Alliance prediction of outcome beyond in-treatment symptomatic change as psychotherapy processes. Psychother Res. 1991;1:104–112. doi: 10.1080/10503309112331335531. [DOI] [Google Scholar]
- Gelso C. A tripartite model of the therapeutic relationship: Theory, research, and practice. Psychother Res. 2014;24:117–131. doi: 10.1080/10503307.2013.845920. [DOI] [PubMed] [Google Scholar]
- Goodkind MS, Gallagher-Thompson D, Thompson LW, Kesler SR, Anker L, Flournoy J, Berman MP, Holland JM, O'Hara RM. The impact of executive function on response to cognitive behavioral therapy in late-life depression. Int J Geriatr Psych. 2016;31:334–339. doi: 10.1002/gps.4325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton MA. A rating scale for depression. J Neurol Neurosur Ps. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horvath AO. The therapeutic relationship: Research and Theory – An introduction to the Special Issue. Psychother Res. 2005;15:3–7. doi: 10.1080/10503300512331339143. [DOI] [Google Scholar]
- Horvath AO, Del Re AC, Flückiger C, Symonds D. Alliance in Individual Psychotherapy. Psychother. 2011;48:9–16. doi: 10.1037/a0022186. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. The working alliance: Theory, research, and practice. In: Weiner IB, Horvath AO, Greenberg LS, editors. Wiley series on personality processes. New York: John Wiley & Sons Inc; 1994. [Google Scholar]
- Hybels CF, Blazer DG, Hays RN. Demography and epidemiology of psychiatric disorders in late-life. In: Blazer DG, Steffens DC, editors. Textbook of Geriatric Psychiatry. Arlington: American Psychiatric Publishing, Inc; 2009. pp. 19–43. [Google Scholar]
- Jeste DV, Alexopoulos GS, Bartels SJ, Cummings JL, Gallo JJ, Gottlieb GL, Halpain MC, Palmer BW, Patterson TL, Reynolds CF, 3rd, Lebowitz BD. Consensus statement on the upcoming crisis in geriatric mental health. Arch Gen Psychiat. 1999;56:848–853. doi: 10.1001/archpsyc.56.9.848. [DOI] [PubMed] [Google Scholar]
- Kalayam B, Alexopoulos GS. Prefrontal dysfunction and treatment response in geriatric depression. Arch Gen Psychiat. 1999;56:713–718. doi: 10.1001/archpsyc.56.8.713. [DOI] [PubMed] [Google Scholar]
- Kim BSK, Ng GF, Ahn AJ. Effects of Client Expectation for Counseling Success, Client-Counselor Worldview Match, and Client Adherence to Asian and European American Cultural Values on Counseling Process with Asian Americans. J Couns Psychol. 2005;52:67–76. [Google Scholar]
- Kiosses DN, Leon AC, Areán PA. Psychosocial interventions for late-life major depression: evidence-based treatments, predictors of treatment outcomes, and moderators of treatment effects. Psychiat Clin N Am. 2011;34:377–401. doi: 10.1016/j.psc.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krapan KM, Levine B, Stuss DT, Dawson DR. Executive function and coping at one-year post traumatic brain injury. J Clin Exp Neuropsyc. 2007;29:36–46. doi: 10.1080/13803390500376816. [DOI] [PubMed] [Google Scholar]
- Krupnick JL, Sotsky SM, Elkin I, Simmens S, Moyer J, Watkins J, Pilkonis PA. The Role of the Therapeutic Alliance in Psychotherapy and Psychotherapy Outcome: Findings in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. J Consult Clin Psych. 1996;64:532–539. doi: 10.1037/0022-006X.64.3.532. [DOI] [PubMed] [Google Scholar]
- Lorr M. Client perceptions of therapists: A study of the therapeutic relation. J Consult Psychol. 1965;29:146–149. doi: 10.1037/h0021924. [DOI] [PubMed] [Google Scholar]
- Markin R. Toward a common identity for relationally oriented clinicians: A place to hand one's hat. Psychother. 2014;51:327–333. doi: 10.1037/a0037093. [DOI] [PubMed] [Google Scholar]
- Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. J Consult Clin Psych. 2000;68:438–450. doi: 10.1037/0022-006X.68.3.438. [DOI] [PubMed] [Google Scholar]
- Mattis S. Dementia Rating Scale. Odessa, Fla: Psychological Assessment Resources; 1989. [Google Scholar]
- McArdle JJ. Latent variable modeling of differences and changes with longitudinal data. Annu Rev Psychol. 2009;60:577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychol Bull. 1993;114:376. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- mHeo M, Murphy CF, Meyers BS. Relationship between the Hamilton Depression Rating Scale and the Montgomery-Asberg Depression Rating scale in depressed elderly: A meta-analysis. Am J Geriat Psychiat. 2007;15:899–905. doi: 10.1097/JGP.0b013e318098614e. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User's Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- Nelson JC, Delucchi KL, Scneider LS. Moderators of Outcome in Late-Life Depression: A Patient-Level Meta-Analysis. Am J Psychiat. 2013;170:651–659. doi: 10.1176/appi.ajp.2012.12070927. [DOI] [PubMed] [Google Scholar]
- Norcross JC. Evidence-Based Therapy Relationships Substance Abuse and Mental Health Services Administration Publishing Service. 2010 http://www.nrepp.samhsa.gov/Norcross.aspx.
- Perret E. The left frontal lobe of man and the suppression of habitual responses in verbal categorical behavior. Neuropsychologia. 1974;12:323–330. doi: 10.1016/0028-3932(74)90047-5. [DOI] [PubMed] [Google Scholar]
- Pimontel MA, Culang-Reinlieb ME, Morimoto SS, Sneed JR. Executive dysfunction and treatment response in late-life depression. Int J Geriatr Psychiatry. 2012;27:893–899. doi: 10.1002/gps.2808. [DOI] [PubMed] [Google Scholar]
- Potter GG, Kittinger JD, Wagner HR, Steffens DC, Krishnan KRR. Prefrontal Neuropsychological Predictors of Treatment Remission in Late-Life Depression. Neuropsychopharmacol. 2004;29:2266–2271. doi: 10.1038/sj.npp.1300551. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. HLM 7 01 for Windows. Skokie, IL: Scientific Software International, Inc; 2013. Computer software. [Google Scholar]
- Reitan RM. The relation of the Trail Making Test to organic brain damage. J Consult Psychol. 1955;44:393–394. doi: 10.1037/h0044509. [DOI] [PubMed] [Google Scholar]
- Sachs MH. Manual for supportive therapy. New York: Cornell University; 2000. [Google Scholar]
- Sheehan B. Assessment scales in dementia. Ther Adv Neurol Disord. 2012;5:349–358. doi: 10.1177/1756285613489764. http://doi.org/10.1177/1756285612455733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modelling Change and Event Occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Trajković G, Vladan S, Latas M, Leštarević M, Ille T, Bukumirić Z, Marinković J. Reliability of the Hamilton Rating Scale for Depression: A meta-analysis over a period of 49 years. Psychiat Res. 2011;189:1–9. doi: 10.1016/j.psychres.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Wampold BE, Budge SL. The Relationship–and its Relationship to the Common and Specific Factors of Psychotherapy. Couns Psychol. 2012;40:601–623. doi: 10.1177/0011000011432709. [DOI] [Google Scholar]
- Webb CA, DeRubeis RJ, Amsterdam JD, Shelton RC, Hollon SD, Dimidjian S. Two Aspects of the Therapeutic Alliance: Differential Relations with Depressive Symptom Change. J Consult Clin Psych. 2011;79:279–283. doi: 10.1037/a0023252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfe BE, Goldfried M. Research on psychotherapy integration: Recommendations and conclusions from an NIMH workshop. J Consult Clin Psych. 1988;56:448–451. doi: 10.1037/0022-006X.56.3.448. [DOI] [PubMed] [Google Scholar]
- Zuroff DC, Kelly AC, Leybman MJ, Blatt SJ, Wampold BE. Between-Therapist and Within-Therapist Differences in the Quality of the Therapeutic Relationship: Effects on Maladjustment and Self-Critical Perfectionism. J Clin Psychol. 2010;66:681–697. doi: 10.1002/jclp.20683. [DOI] [PubMed] [Google Scholar]


