Abstract
Mediastinal liposarcoma (ML) is a rare mesenchymal tumor, accounting for less than 1% of mediastinal tumors. They have a slow growth, so they may not give symptoms for a long time, until the tumor produces compression of close structures. The treatment of choice is surgery, which can be combined with chemo-radiotherapy. We present a case in which the diagnosis of a ML was made in a 30-year-old woman with dyspnea and chest pain.
Keywords: Liposarcoma, Mediastinal tumor, Mesenchymal tumor
1. Background
Liposarcomas are malignant tumors with a mesenchymal origin. The most frequent locations are the lower limbs and retroperitoneum. Mediastinal liposarcoma (ML) is a rare entity, accounting for less than 1% of mediastinal tumors, and 2% of liposarcomas [1], [2]. ML has been described in all mediastinal compartments, but it seems to have a certain predominance in the posterior mediastinum [3].
Their growth is slow, so they may not give symptoms for a long time. Symptoms usually appear when the tumor has already reached a large size and produces compression of neighboring structures. It has been described that they can initially originate as lipomas, which eventually malignize [4].
The treatment of choice is surgery, which must be exhaustive in order to achieve a complete resection, since ML tend to be recurrent [5].
The most important prognostic factors are size, degree of differentiation, location and complete resection [6].
2. Case presentation
We present the case of a 30-year-old woman who came to the hospital emergency department in September 2015, referring a week of progressive dyspnea, accompanied by sharp pain in left hemithorax and chest tightness. She didn't refer other symptoms.
She had multiple food allergies, controlled by the Allergology department, and allergic rhinitis and asthma that was treating with terbutaline and antihistamines on demand. She has never had toxic habits, and works as a graphic designer at a printing press.
Physical examination only highlighted an abolition of the vesicular murmur and vocal vibrations in the left lung base.
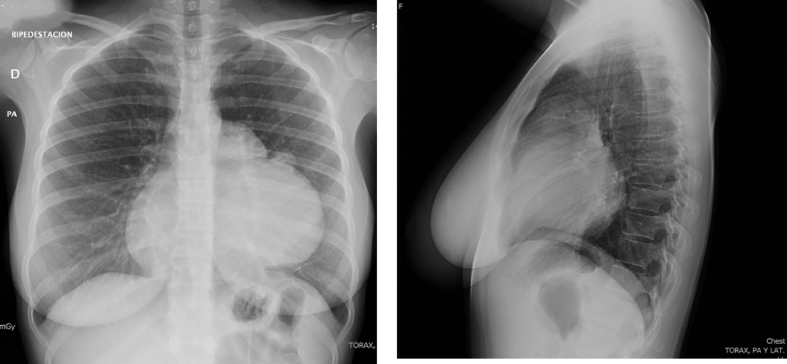
The blood test performed in the emergency room was strictly normal. In the chest X-ray, a large left paracardiac mass was observed, which in the lateral projection was located in the anterior mediastinum (Fig. 1). Thoracic echography revealed a paracardiac mass of about 10 cm in diameter.
Fig. 1.
The chest X-ray showed a big mass located in anterior mediastinum.
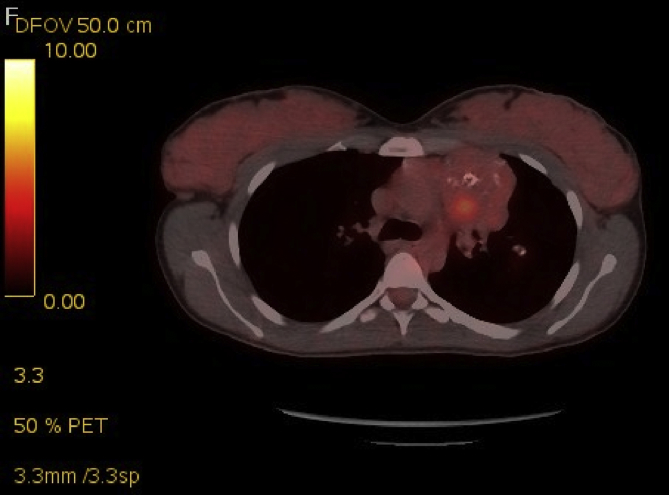
The patient was admitted to the Pneumology Service with the suspicion of an anterior mediastinal tumor. During admission, a CT scan of chest, abdomen and pelvis was performed, confirming the presence in the left anterior mediastinum of a 10 × 11 cm of diameter tumor located to the left of the heart and in front of the left lung. The lesion had an intimate contact with the adjacent pericardium with effacement of the fat planes (Fig. 2). A CT-guided needle biopsy was performed. The biopsy was informed as compatible with a low grade myofibroblastic tumor. During admission, a PET-CT was performed, which showed that the mass had a heterogeneous metabolic behavior, with a SUV max. of 4.83 g/mL. The remaining structures showed no increase in glucose metabolism (Fig. 3). Thoracic MRI was also performed, which showed that the tumor had a broad contact with the pericardium, but without signs of infiltration.
Fig. 2.
The chest CT scan revealed a 10 × 11 cm mass located in the anterior mediastinum, to the left of the heart. The tumor had two components: a bigger part with an intense peripheral contrast uptake and necrotic center, and a smaller part with presence of multiple calcifications.
Fig. 3.
The PET-CT revealed that the tumor had a heterogeneous metabolic behavior, with a SUV max of 4.83 g/mL.
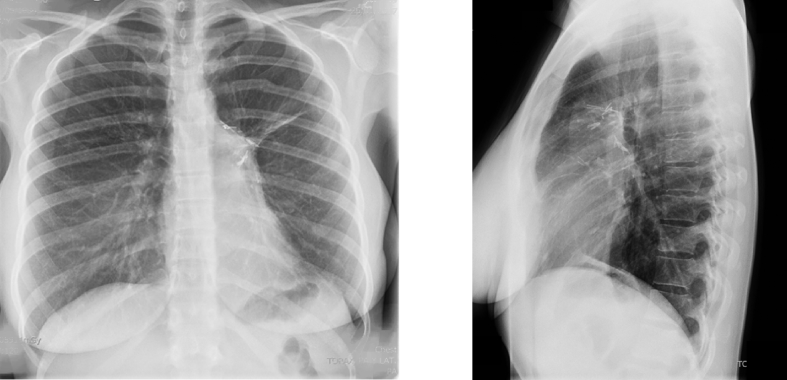
With the diagnose of a low grade myofibroblastic tumor, the patient was referred to the Thoracic Surgery Service. A thoracoplasty was performed, dissecting the mass and part of the pericardium where it was not possible to dissect. The main complication was an intense bleeding which needed the transfusion of 2 units of red blood cells. The resected piece was submitted to the Pathological Anatomy Service and analyzed by the same team of the previous needle biopsy, which provided the definitive diagnosis of a dedifferentiated liposarcoma with bone metaplasia. The surgical margins were free of tumor and no lymphatic or vascular invasion was identified. The chest X-ray two months before surgery can be observed in Fig. 4.
Fig. 4.
Chest X-ray performed two months after surgery.
After surgery, the patient was referred to the Medical Oncology Service, who proposed her to start adjuvant chemotherapy treatment with four cycles of ifosfamide-adriamycin. The possibility of concomitant local radiotherapy was considered, but it was rejected because of the high risk of toxicity and sequelae.
The chemotherapeutic treatment was administrated between December 2015 and April 2016. One month later, a new PET-CT scan was performed, which showed no increase in glycolic metabolism at any level.
The patient currently follows periodic check-ups at the Medical Oncology Service, performing chest CT every 6 months. The last one was performed in February 2017, and was strictly normal. Until date, she has not developed a recurrence of the ML.
3. Discussion
ML are very rare tumors. They account for less than 1% of mediastinal tumors, and comprise approximately 2% of liposarcomas [1], [2]. A certain predominance has been observed in males between the second and seventh decades of life [7], [8]. They are slow-growing tumors, which usually only produce symptoms when they reach a large size, due to the compression of neighboring mediastinal structures. The presence of superior vena cava syndrome has been associated with early mortality [9], [10].
The diagnosis of suspicion arises from CT images, in which a large mass is usually observed, which combines fat densities, with attenuations similar to other soft tissues [4], [5], [9]. The definitive diagnosis is based on the anatomopathological study of the lesion. In the case of our patient initially a diagnosis of low grade myofibroblastic tumor was established, which was modified to a dedifferentiated mediastinal liposarcoma with bone metaplasia, after analyzing the surgical specimen. Probably, due to the heterogeneous nature of these tumors, a single percutaneous biopsy is not enough to establish a diagnosis of certainty.
The treatment of choice is resection surgery. A complete excision of the lesion should always be attempted [5], [11]. Radiotherapy seems to decrease recurrences, but has not been shown to have an effect on survival. Chemotherapy is used in combination with radiotherapy as a neoadjuvant treatment, as well as to prevent recurrences in the postoperative period. The choice scheme is the combination of ifosfamide with adriamycin [12]. The possibility of an immunomodulatory and molecular therapy-based treatment is being studied, but further studies are still needed to clarify its efficacy [13], [14]. Our patient received adjuvant chemotherapy with ifosfamide-adriamycin to avoid recurrences, but, radiotherapy was rejected because the risks were supposed to be greater than the potential benefits, although she is a young woman with no associated comorbidities. Attending to the available bibliography, we consider that our patient would have benefited from the radiotherapeutic treatment in order to decrease the risk of recurrences.
The most important prognostic factors are size, degree of differentiation, location and complete resection. Due to the high recurrence rate, patients should be monitored in the long term [5]. Our patient, after 1.5 years of follow-up, persists without data of tumor recurrence. However, we must be cautious and keep the medical checks over several years.
4. Conclusions
The mediastinal liposarcoma is a rare mesenchymal tumor, usually diagnosed when it has reached a big size and produces symptoms because of the compression of neighboring structures. The ideal treatment is surgical resection, which can be combined with chemo-radiotherapy to reduce the risk of recurrences, which usually are frequent.
Declaration of interest
The authors declare that no conflicts of interest exist. The authors alone are responsible for the content and writing of the paper.
Acknowledgements
The authors gratefully acknowledge the financial support provided by Sociedad Asturiana de Patología Respiratoria (ASTURPAR) and Fundación AIRE under project “Experimental and numerical study of a three-dimensional model of an asthmatic patient airways reconstructed from CT or MR images”.
Contributor Information
Ana Fernández-Tena, Email: tenaana@uniovi.es.
Francisco Julián López-González, Email: fjlopezglez@gmail.com.
References
- 1.Enzinger F.M., Weiss S.W., editors. Liposarcoma. Soft Tissue Tumors. third ed. Mosby; St. Louis: 1995. pp. 431–466. [Google Scholar]
- 2.Razuk M.A., Urschel H.C., Race G.J., Kingsley W.B., Paulson D.L. Liposarcoma of the mediastinum. J. Thorac. Cardiovasc Surg. 1971;61:819–826. [PubMed] [Google Scholar]
- 3.Grewai R.G., Prager K., Austin J.H. Long-term survival in non-encapsulated primary liposarcoma ofthe mediastinum. Thorax. 1993;48 doi: 10.1136/thx.48.12.1276. 1.276-1.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rivo J.E., Cañizares M.A., García-Fontán E., Albort J., González-Piñeiro A., Peñalver R. Liposarcomas mediastínicos de localización atípica. Aportación de 2 casos. Cir. Esp. 2005;77(2):99–101. doi: 10.1016/s0009-739x(05)70816-2. [DOI] [PubMed] [Google Scholar]
- 5.Morcillo A., Calvo V., Pastor J. Liposarcoma mediastínico recidivante. Arch. Bronconeumol. 1998;34:273. doi: 10.1016/s0300-2896(15)30442-7. [DOI] [PubMed] [Google Scholar]
- 6.Mier J.M., Molins L., Mazarro A., Sebastian E., Fibla J.J., Vidal G. Liposarcoma mediastínico gigante. A propósito de un caso. Neumol. Cir. Torax. 2008;67(3):148–150. [Google Scholar]
- 7.Standerfer R.J., Armistead S.H., Paneth M. Liposarcoma of the mediastinum: report of two cases and review of the literature. Thorax. 1981;36:639–694. doi: 10.1136/thx.36.9.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacLean T.R., Almassi G.H., Hackbath D.A., Janjan N.A., Potish R.A. Mediastinal involvement by mixoid liposarcoma. Ann. Thorac. Surg. 1989;47:920–921. doi: 10.1016/0003-4975(89)90038-6. [DOI] [PubMed] [Google Scholar]
- 9.Ruiz L.A., Camino J., Cabriada V., Campo A., Pascal y I., Zalacain R. Liposarcoma mediastínico. A propósito de 2 casos. Arch. Bronmneiimol. 1999;35:189–191. doi: 10.1016/s0300-2896(15)30278-7. [DOI] [PubMed] [Google Scholar]
- 10.Attal H., Jensen J., Reyes C. Myxoid liposarcoma of the anterior mediastinum: diagnosis by fine needle aspiration biopsy. Acta Cytol. 1995;39:511–513. [PubMed] [Google Scholar]
- 11.Álvarez-Sala R., Casadevall J., Caballero P., Prados C., Ortega B. Long-term survival in a surgically treated non-capsulated mediastinal primary liposarcoma. J. Cardiovasc Surg. 1995;36:199–200. [PubMed] [Google Scholar]
- 12.Skubitz K., DÁdamo D. Sarcoma. Mayo Clin. Proc. 2007;82(11):1409–1432. doi: 10.4065/82.11.1409. [DOI] [PubMed] [Google Scholar]
- 13.Conyers R., Young S., Thomas D.M. Liposarcoma: molecular genetics and therapeutics. Sarcoma. 2011;2011:483154. doi: 10.1155/2011/483154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Italiano A., Bianchini L., Gjernes E. Clinical and biological significance of CDK4 amplification in well-differentiated and dedifferentiated liposarcomas. Clin. Cancer Res. 2009;15:5696. doi: 10.1158/1078-0432.CCR-08-3185. [DOI] [PubMed] [Google Scholar]