Abstract
Object
To compare the clinical efficacy of titanium mesh cages and autogenous iliac bone graft to restore vertebral height through posterior approach in patients with thoracic and lumbar spinal tuberculosis.
Method
59 patients with spinal tuberculosis underwent interbody fusion and internal fixation through posterior approach in our department from January 2011 to December 2013. In group A, 34 patients obtained titanium mesh for the reconstruction of vertebral height, among them 25 patients (group A1) suffered from single-segment spinal tuberculosis, and 9 patients, (group A2) had multi-segment spinal tuberculosis. In group B, 25 patients got autogenous iliac bone graft to restore vertebral height, including 24 patients with single-segment spinal tuberculosis (group B1), and 1 patient with multi-segment spinal tuberculosis (group B2). The clinical efficacy was evaluated based on average operation time, blood loss, hospital stays, hospitalization expenses, visual analog scale (VAS), Oswestry Disability Index (ODI), erythrocyte sedimentation rate (ESR), C-Reactive protein (CRP), neurological function recovery, bony fusion, intervertebral height, Cobb angle and postoperative complications.
Results
Final follow-up time was an average of 35.5 months ranging from 15 to 56 months. All patients were completely cured and obtained solid bone fusion. The bony fusion time was 9.4±6.1 months in group A1, 10.2±2.7 months in group A2 and 8.7±3.6 months in group B1. There were no significant difference among three groups (P>0.05). The Cobb correction and restoration of intervertebral height significantly improved compared with those in preoperation, but without significant difference among three groups (P>0.05). The loss of angular correction and intervertebral height in group A1 were found to be less than those in group B1 (P<0.05), but with no significant difference between group A1 and group A2, and between group A2 and group B1 (P>0.05). Patients in group B1 got the most loss of angular correction and intervertebral height. In addition, neurological function was revealed to be significantly improved after surgery. There were significant differences of VAS, ODI, ESR and CRP between preoperation and postoperation at the final follow-up time (P<0.05), with no significant difference among three groups (P>0.05). No statistically significant difference was found when analyzing blood loss, hospital stays, hospitalization expenses, and corrective cost among three groups (P>0.05). Complications included cerebrospinal fluid leakage (2 cases in group A1 and group A2), sinus formation (3 cases in group A1, group A2 and group B1), and intervertebral infection (1 case in group B1), but no implant failure or donor site complications was found in any patient.
Conclusions
Titanium mesh cages could obtain good clinical efficacy comparable to autogenous iliac bone graft when treating single-segment spinal tuberculosis, and may be better than autogenous iliac bone graft for treating multi-segment spinal tuberculosis.
Background
Tuberculosis has become increasingly widespread in our country [1, 2]. Bone and Joint tuberculosis (BJTB) constitutes about 10% of total extra-pulmonary TB cases[3], and spinal tuberculosis is known as the most commonly infected site among skeletal tuberculosis (about 44%) [4]. The intervertebral disc and the end plates of the adjacent superior and inferior vertebral bodies are often involved in spinal tuberculosis, and their severe destruction can result in kyphotic deformity and even paraplegia[5]. Various studies have shown that the majority (82–95%) of spinal tuberculosis patients obtain good clinical outcome after receiving current chemotherapy. Surgical intervention is required if the patients suffer from neurologic deficit, big abscess formation, persistent or recurrent infection, severe pain, local kyphosis, and segmental instability[1, 2, 5–7].
Surgical intervention has become an important way of treating serious spinal tuberculosis, and the anterior-posterior approach is known as the gold standard for surgery, but limited by severe trauma, great blood loss, and high risk [2]. Many studies have revealed that posterior approach is able to achieve good clinical outcome when treating spinal tuberculosis [1, 2, 6, 8, 9]. Vertebral height demands reconstruction after surgical debridement, but it is still elusive to select appropriate bone-grafting materials to restore vertebral height [1, 10–13]. In clinical medicine, titanium mesh and autogenous iliac bone graft are ubiquitous. This study is to compare the efficacy between titanium mesh cages and autogenous iliac bone graft to restore vertebral height through posterior approach in patients with spinal tuberculosis.
1 Materials and methods
1.1 Ethics statement
This study was approved by the Institutional Review Board of the First Affiliated Hospital of Chongqing Medical University and conducted according to the principles of the Declaration of Helsinki. All of the participants provided their written informed consent to participate in this study, before their data were stored in the hospital database and used for research purposes.
1.2 Patient population
Inclusion criteria: thoracic and lumbar spinal tuberculosis in adults, posterior approach, internal fixation, and reconstruction using titanium mesh cages or autogenous iliac bone graft. Exclusion criteria: active pulmonary tuberculosis and extrapulmonary tuberculosis, cancer, discontinuous spinal tuberculosis, osteoporosis, traumatic fractures, thoracic and lumbar surgery within 6 months.
From January 2011 to December 2013 in our department, there were 147 patients with thoracic and lumbar tuberculosis, but 59 patients were included in this study. Of the 59 patients, 25 cases (42.4%) had typical symptoms of tuberculosis, including night fever, loss of weight, fatigue, and back pain. Diagnosis was based on non-specific laboratory and imaging findings, including spinal radiographic films, computed tomography (CT) and magnetic resonance imaging (MRI) in order to verify vertebral body destruction or collapse, intervertebral space narrowing or disappearing and cold abscess. Spinal tuberculosis was examined by postoperative pathological analysis in all patients. 34 cases of 59 patients with spinal tuberculosis in group A obtained titanium mesh cages for reconstruction involving 25 patients with single-segment spinal tuberculosis (group A1) and 9 patients with multi-segment spinal tuberculosis (group A2). In group B, 25 cases got autogenous iliac bone graft for reconstruction including 9 patients with single-segment spinal tuberculosis (group B1) and 1 patients with multi-segment spinal tuberculosis (group B2, 70 years old and T6-8). No significant difference of general datas was found among three groups (P>0.05, Table 1).
Table 1. General data of three groups.
| Items | Group A1 | Group A2 | Group B1 |
|---|---|---|---|
| Age(Y) | 39.2±14.2 | 42.4±12.5 | 41.4±14.3 |
| Sex (M/F) | 13/12 | 7/2 | 9/15 |
| Thoracic | 3 | 4 | 3 |
| Thoracolumbar | 8 | 3 | 7 |
| Lumbar | 14 | 2 | 14 |
| Para-vertebral abscess | 10 | 7 | 14 |
| Psoas abscess | 6 | 2 | 7 |
| Iliac fossa abscess | 3 | 1 | 3 |
Age was expressed as mean±SD, and t-test was performed; P = 0.974. M: male; F: female; n: number of patients.
1.3 Preoperative management
All people had to achieve chemotherapy shortly after clinical diagnosis was suspected. Anti- tuberculosis drugs with HREZ chemotherapy regimen consistingof isoniazid (300 mg/day), rifampicin (450 mg/day), ethambutol (750 mg/day), and pyrazinamide (1500 mg/day) were administered 2–4 weeks before surgery. Surgical management was performed when ESR decreased below 60 mm/h and CRP was progressively decreased..
1.4 Surgical management
In group A, patients were placed in the prone position after administering general endotracheal anesthesia. A posterior midline incision was made following the focus of segmental lesions, and paraspinal muscles were peeled along the debridement side. Wiltse approach was applied on the non-debridement side. Transpedicular screws were fixed in two levels superior and inferior to the level of decompression, and the screws were also placed in the affected vertebrae if the upper part of the vertebrae and pedicle was not involved. A temporary pre-bent rod was installed on the non-debridement side to achieve spine stability. We preferred radical debridement. Streptomycin 1.0 g and isoniazid 0.2 g were administered locally after preparing bone graft bed. The kyphosis was slowly and carefully corrected with the help of the compression and stretching of the internal fixation instrumentation. The specially formed titanium mesh cages (filled with resected cancellous bone containing Streptomycin 1.0 g) were inserted into the bone trough, and had complete connection with upper and lower vertebral end-plates. Negative pressure drainage and incision sutures were performed. In group B, surgical methods were same as group A. After preparing bone graft bed, autogenous iliac was clipped to fit the vertebral defect.
Abscess treatment: For the para-vertebral and psoas abscess, abscess cavity wall, and caseous necrosis and tubercular granulation tissue were eliminated. Large psoas and iliac fossa abscess underwent debridement by extraperitoneal approach, and Streptomycin 1.0 g was used in the lesion site. Effective drainage with a flushing piping and a drainage tube system was applied after debridement. And resected specimens were collected for bacterial culture and pathological diagnosis.
1.5 Postoperative care
The drainage tube was pulled out when drainage volume was less 30 ml/day. Patients obtained oral HREZ chemotherapy postoperatively. 12 months later, pyrazinamide was discontinued. Patients received 18- to 24- month regimens of HRE chemotherapy (12HREZ/18-24HRE). Ambulation was allowed four weeks after surgery. All patients were examined clinically and radiologically in 1 week, and in 3, 6, 12, 18 and 24 months after surgery, and then once a year.
1.6 Evaluating standard
1.6.1 Clinical assessments
For all cases, the following indexes were recorded preoperatively, three months of postoperation, and at follow-up time: (1) average operation time, blood loss, hospital stays, hospitalization expenses, Visual Analogue Scale (VAS), improvement in the postoperative Oswestry Disability Index (ODI) score, (2) recovery of neurologic function, as assessed by the Frankel grade, (3) laboratory tests, including erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).
1.6.2 Radiological assessments
Intervertebral height, kyphotic angle and Cobb angle were recorded. Intervertebral height was defined as the vertical height between superior and inferior vertebral body in coronal plane with fusion zone[14]. Bone grafting fusion was assessed using the radiologic criteria of Bridwell et al[15].
1.7 Statistical analysis
All statistical analyses were performed with SPSS version 22.0 statistical software (SPSS, Inc., Chicago, IL, USA). The paired t test was used to analyze data in each group, and independent sample t-test was performed between groups. Values of P < 0.05 were considered statistically significant.
2. Results
2.1 Clinical assessments
Final follow-up time was an average of 35.5 months (15 to 56 months). VAS, ODI, ESR and CRP were obviously reduced at the final follow-up time than postoperation (P<0.05). The operation time in group A2 was significantly longer than other groups (P < 0.05), but there were no significant difference between group A1 and group B1(P > 0.05, Table 2). 5 patients in group A1, 4 patients in group A2 and 5 patients in group B1 were rated as D grade of neurological function at preoperation, and all patients was improved after surgery apart from 1 case in group B1 who was rated as grade D at the final follow-up.
Table 2. Comparison of VAS, ODI, ESR, CRP and operation time, blood loss, hospital stay, and hospitalization expenses pre- and postoperatively in and among three groups (X± S).
| Group A1 | Group A2 | Group B1 | PA1-A2 | PA1-B1 | PA2-B1 | |
|---|---|---|---|---|---|---|
| follow-up time | 35.8±11.5 | 36.9±6.7 | 34.8±7.0 | 0.791 | 0.700 | 0.434 |
| Preoperative VAS | 5.9±1.3 | 5.8±1.5 | 5.7±1.3 | 0.844 | 0.560 | 0.832 |
| Follow-up VAS | 1.7±1.4* | 1.8±1.3* | 1.1±0.8* | 0.915 | 0.055 | 0.163 |
| Preoperative ODI | 64.9±15.3 | 69.2±15.2 | 60.8±12.1 | 0.470 | 0.307 | 0.108 |
| Follow-up ODI | 12.8±9.1* | 13.6±7.5* | 13.9±11.4* | 0.826 | 0.728 | 0.947 |
| Preoperative ESR | 41.5±27.8 | 60.8±67.2 | 43.9±26.1 | 0.224 | 0.761 | 0.261 |
| At 3 months postoperative ESR | 13.0±10.6* | 11.1±4.1* | 13.4±9.1* | 0.620 | 0.889 | 0.489 |
| Preoperative CRP | 24.5±18.2 | 34.8±26.0 | 30.1±19.3 | 0.206 | 0.308 | 0.573 |
| At 3 months postoperative CRP | 10.3±4.4* | 8.9±5.3* | 14.3±10.4* | 0.439 | 0.100 | 0.161 |
| Operation time (min) | 240.0±52.5 | 320±77.4# | 240.8±66.2 | 0.016 | 0.961 | 0.006 |
| Blood loss (ml) | 728.0±505.0 | 944.4±600.2 | 518.8±303.2 | 0.302 | 0.085 | 0.071 |
| Hospital stay (days) | 18.7±9.6 | 20.8±6.4 | 17.9±10.1 | 0.550 | 0.776 | 0.428 |
| hospitalization expenses | 73006.0±18860.1 | 66712.2±8618.3 | 76216.5±20894.0 | 0.194 | 0.575 | 0.074 |
*, # Significant difference at P<0.05 compared with pre-operation and group A1, respectively.
2.2 Radiological assessments
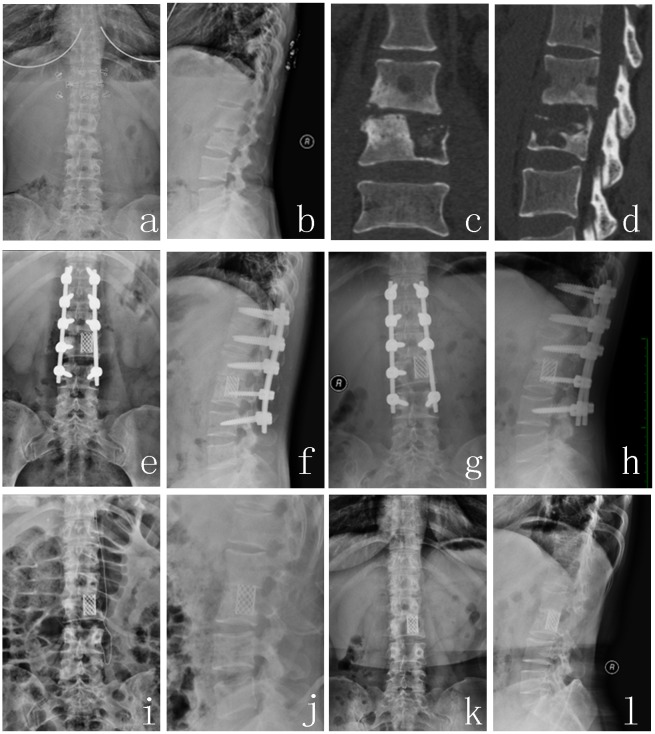
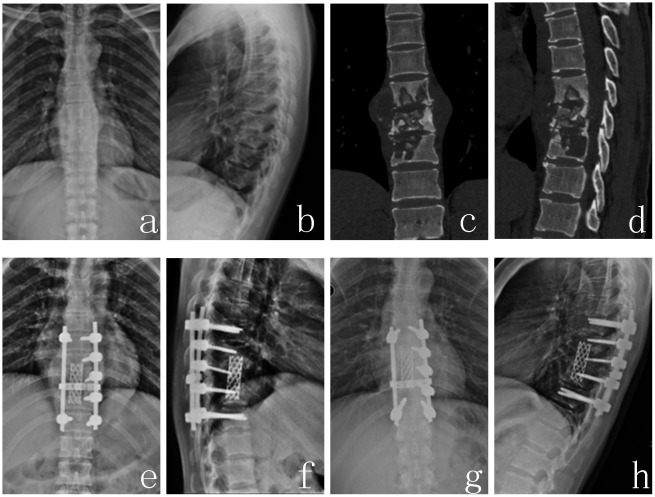
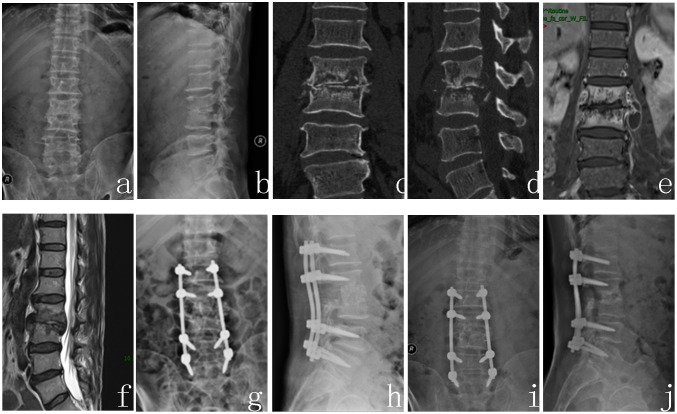
Spinal tuberculosis was completely cured, and the solid bony fusion was achieved for all patients. The bony fusion time was 9.4±6.1 months in group A1 (Fig 1), 10.2±2.7 months in group A2 (Fig 2), 8.7±3.6 months in group B1 (Fig 3). There was no significant difference among three groups (P>0.05). Kyphosis correction was (4.4±8.3) °, (2.3±32.7) ° and (5.4±12.5) ° in group A1, A2 and B1 respectively. And their restoration of intervertebral heights was 1.8±1.1, 2.3±1.4, 1.8±1.1 cm, respectively. There was also no significant difference among three groups (P>0.05). The Cobb angle loss and intervertebral height loss in group A1 were less than that in group B1(P<0.05), but no significant difference was found between group A1 and group A2, and between group A2 and group B1 (P>0.05), and their loss in group B1 was the greatest in the three groups (Table 3).
Fig 1. A 36-year-old female patient with L2-3 spinal tuberculosis (Frankel grade E) obtained formed titanium mesh for reconstruction.
(a~d) Preoperative X-ray and CT showed that L2 and L3 vertebra body and the intervertebral disc were destroyed, and lumbar instability was formed. (e, f) Postoperative X-ray. (g, h) X-ray at 36 months after surgery. (i, j) Removing the internal fixation at 36 month postoperatively. (k, l) X-ray of 1 year after implant removal showed good location of titanium mesh and lumbar physiological curve.
Fig 2. A 41-year-old female patient with T8,9,10 spinal tuberculosis (Frankel grade E) got formed titanium mesh for reconstruction.
(a~d) Preoperative X-ray and CT demonstrated that T8-10 vertebra body and the intervertebral discs were destroyed and instability was formed. (e, f) Postoperative X-ray, (g, h) A-P and lateral X-ray at 31 months after surgery revealed good location of titanium mesh and lumbar physiological curve.
Fig 3. A 58-year-old male patient with L2-3 spinal tuberculosis (Frankel grade D) achieved autogenous iliac bone graft for reconstruction.
(a~f) Preoperative X-ray, CT, and MRI showed that L2 and L3 vertebra body and the intervertebral disc were destroyed to produce neurological compression and instability. (g, h) Postoperative X-ray. (I, j) A-P and lateral X-ray at 29 months after surgery showed good location of titanium mesh, lumbar physiological curve and neurologic function recovery.
Table 3. All radiological parameters (X ± s).
| Group A1 | Group A2 | Group B1 | PA1-A2 | PA1-B1 | PA2-B1 | |
|---|---|---|---|---|---|---|
| Preoperative kyphosis(°) | 20.3±18.3 | 32.1±17.8 | 24.5±15.3 | 0.795 | 0.722 | 0.985 |
| Postoperative kyphosis(°) | 24.5±17.7* | 21.8±18.7 | 23.8±17.5 | 0.589 | 0.819 | 0.713 |
| Follow-up kyphosis(°) | 25.6±17.8*& | 24.1±18.5& | 26.3±17.6& | 0.582 | 0.885 | 0.675 |
| kyphosis correction(°) | 4.4±8.3 | 2.3±32.7 | 5.4±12.5 | 0.851 | 0.748 | 0.788 |
| Loss of correction (°) | 1.1±1.8* | 2.3±0.8* | 2.5±2.0*# | 0.054 | 0.012 | 0.796 |
| Preoperative intervertebral height(cm) | 11.9±2.4 | 15.4±3.0 | 12.3±1.8 | 0.001 | 0.444 | 0.001 |
| Postoperative intervertebral height(cm) | 13.7±2.6* | 17.7±3.8* | 14.2±2.0* | 0.001 | 0.478 | 0.024 |
| Follow-up intervertebral height (cm) | 12.9±2.5*& | 16.4±4.0*& | 12.0±2.2*& | 0.027 | 0.018 | 0.010 |
| intervertebral height correction (cm) | 1.8±1.1 | 2.3±1.4 | 1.8±1.1 | 0.307 | 0.978 | 0.336 |
| Loss of intervertebral height(cm) | 0.8±0.6* | 1.3±1.0* | 2.2±1.2*# | 0.105 | 0.000 | 0.055 |
| Bone fusion(cm) | 9.4±6.1 | 10.2±2.7 | 8.7±3.6 | 0.714 | 0.594 | 0.254 |
*, &, # Significant difference at P<0.05 compared with pre-operation, post-operation, and group A1, respectively.
2.3 Complications
No implant failure or donor site complications were found in any patient. There were 20 kinds of complications in 15 patients, such as intervertebral infection, sinus formation, combined bacterial infection, liver and kidney dysfunction. Two cases suffered from cerebrospinal fluid leakage. 1 case in group A1 had tuberculosis meningitis after 1 year (Table 4).
Table 4. Complications.
| Postoperative Complications | In total | Group A1 | Group A2 | Group B1 |
|---|---|---|---|---|
| Cerebrospinal Fluid Leakage | 2 | 1 | 1 | 0 |
| Drug-induced liver Dysfunction | 4 | 2 | 0 | 2 |
| Drug-induced Kidney Dysfunction | 7 | 4 | 1 | 2 |
| Postoperative Infection | 7 | 3 | 2 | 2 |
| Sinus Formation | 3 | 1 | 1 | 1 |
| Bacterial Meningitis | 2 | 1 | 1 | 0 |
| Intervertebral Infection | 1 | 0 | 0 | 1 |
| Tuberculous Meningitis | 1 | 1 | 0 | 0 |
| In total | 20 | 10 | 4 | 6 |
2.4. Typical case analysis (Figs 1, 2, 3)
3 Discussions
Tuberculosis has become increasingly widespread in china. Various studies have shown that the majority (82–95%) of spinal tuberculosis patients resulted in good clinical outcome after current chemotherapy[16]. Duration of antituberculous treatment remained controversial. Existing guidelines recommended the treatment duration ranging from 6 to 24 months. Van Loenhout-Rooyackers et al.[17] suggested that 6-month antituberculous treatment is probably sufficient. World Health Organization recommends 9 months of treatment for patients with osteoarticular tuberculosis[18]. The American Thoracic Society recommends 6 months of chemotherapy for spinal tuberculosis in adults and 12 months in children[19]. The British Thoracic Society recommends 6 months of daily treatment (2HREZ/4HR), irrespective of age[20]. Due to the serious risk of disability and the difficulty in assessing treatment response, many experts still preferred 12–24 months of antituberculous treatment based on radiological change and inflammatory markers [16, 17, 21]. Duration of antituberculous treatment in China varied from 15 to 36 months (6-12HREZ/9-24HRE)[1, 6, 22–25]. Clinic Society of Chinese Antituberculosis Association doesn’t recommend a short period chemotherapy for patients after surgery[26]. Certainly, anti-tuberculosis drugs should be changed when encountering multidrug-resistant TB.
Preoperative managements are very important for perioperative period care. The ESR and CRP are of a high level, which represent that the tuberculosis bacillus are active and TB toxicity symptoms are serious. ESR and CRP can’t return to normal within 2–4 weeks after chemotherapy, because of abscesses persisting, but TB toxicity symptoms may be relieved. When ESR decreased below 40–80 mm/h or returned to normal, and CRP was progressively decreased[22, 24, 27, 28], the surgery was recommended. In addition, if the patients encountered neural function aggravation, defecation function disturbance, and paraplegia, the surgical intervention should be perfomed immediately.
Surgical treatment methods for spinal tuberculosis mainly included anterior approach, staged or simultaneous anterior decompression combined with posterior stabilization, as well as posterior approach. Anterior approach allowed direct access to the lesion site and was beneficial to debridement and convenient bone grafting[29], but with high risk of pseudarthrosis and ineffective correction of kyphosis. Moreover, the anterior exposure of the upper thoracic spinal region showed some difficulty because of the barrier of thoracic bones, clavicle, costal bone and superior mediastinum organs[8, 29–31]. Anterior approach was limited by long operation time, large amount of bleeding, large wounds, and prolonged bed rest[32]. With the development of pedicle screws and bone fusion, posterior approach had become widespread and benefited to correction of kyphosis and spinal stability [1, 6, 31]. Our research showed that the posterior approach allowed the sufficient decompression of spinal cord and nerve, and bone fusion and good clinical outcome were available using titanium mesh cages or autogenous iliac bone graft combined with fixation instrumentation. Kyphosis correction effect was obviously improved and maintained at the final follow-up. The solid bony fusion was achieved for all patients. Fewer complications related to operation occurred than anterior approach [6, 7, 10].
According to the three column theory of Denis[33], it’s very important to integrate anterior column and middle column for improving spinal stability. Spinal tuberculosis often destroyed spinal anterior column and middle column to reduce stability. Autogenous iliac bone graft was known as the gold standard to repair bone defects due to good osteogenesis, bone induction, bone conductibility and biocompatibility [10]. Recently, many studies report that titanium mesh cages showed an important potential in reliable spinal reconstruction, high bone fusion, sufficient sagittal profile maintenance and low implant-related problems[6, 10, 34, 35].
In this research, the single-segment titanium mesh group and autogenous iliac bone group achieved solid bone fusion, and neurological function in all patients was obviously improved after surgery apart from 1 case in group B1 who was rated as grade D at the final follow-up. Cobb angle loss and intervertebral height loss in group A1 were less when compared with that in group B1. Our results were consistent with previously published results[2, 5, 34]. On the one hand, titanium mesh cages allowed tailored design of shape corresponding to individual bone defects. Titanium mesh cages was filled with resected cancellous bone, which consisted of excised vertebral lamina and articular process, and the donor site complications were avoided. And its insertion to the resection site provided a large interbody—bone interface beneficial to improve spinal stability. Posterior instrumentation and titanium mesh cages were used in our patients to enforce operative segments stability, induce deformity correction and maintenance, bone fusion and prevention of bone resorption. Cobb angle loss and intervertebral height loss using autogenous iliac bone graft were revealed to be greater than that using titanium mesh cages, which may be mediated by bone resorption. In the current study, solid bony fusion, good clinical outcomes as well as improvement of neurologic function were achieved in single-segment titanium mesh group and autogenous iliac bone group, and a small loss of kyphosis and intervertebral height correction was acceptable[7].
The autogenous iliac bone graft showed the risk of stress fractures, fixation failure and severe loss of correction of kyphosis when treating multi-segment spinal tuberculosis which demanded bone grafts with strong mechanical force for spinal stability [29]. The donor site complications included chronic pain (up to 40% of cases) and infection [34, 36]. Zeng et al[1] and Korovessis et al[12] reported that a long-segment bone graft was more prone to result in delayed stress fractures, poor correction and implant failure. In previous studies[13, 25, 29, 37, 38] and our research, titanium mesh was found to provide better structural support, solid bony fusion, kyphosis and intervertebral height correction, the smaller loss of angular correction and intervertebral height than autogenous iliac bone when treating multi-segment spinal tuberculosis. Bone tablets grafts harvested from intraoperative biting were sufficient to fill the titanium mesh for stimulating bone fusion.
One patient in group A1 suffered from tuberculosis meningitis 1 year post-operation.. Drug-induced liver and kidney dysfunction, tuberculosis and bacterial meningitis, intervertebral infection, sinus formation and combined staphylococcus aureus were cured by debridement, antibiotics and the symptomatic methods. That complications may be related with irregular anti-TB drugs treatments, drug-resistance, malnutrition, poor immunity and so on.
4 Conclusion
Titanium mesh cages was found to be a good alternative to autogenous iliac bone graft for restoring vertebral height when treating single-segment spinal tuberculosis and might obtained better clinical efficacy than autogenous iliac bone graft for treating multi-segment spinal tuberculosis. Some potential shortcomings of our study should be considered. Many studies involve anterior and posterior multi-segment autogenous iliac bone and titanium mesh bone graft, and combined anterior and posterior approaches are necessary. Further, a larger number of patients and longer follow-ups would be required.
Supporting information
It contains the Ethical Approval Form and translation document.
(ZIP)
It’s a informed consent form template for clinical trials.
(ZIP)
Acknowledgments
The authors wish to thank Mr. Yong Zhu, and Mr. Zenghui Zhao, of the Department of Orthopedics, the First Affiliated Hospital of Chongqing Medical University, Chongqing, China, for their advice and supervision with regards to the statistical analysis and modification of the manuscript.
Data Availability
Data contains confidential participant information and cannot be shared publicly, in accordance with the restrictions of the Institutional Review Board of the First Affiliated Hospital of Chongqing Medical University, which approved this study. Readers may request access to data and direct questions about the data availability to the IRB at 1262744150@qq.com.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Zeng H, Zhang P, Shen X, Luo C, Xu Z, Zhang Y, et al. One-stage posterior-only approach in surgical treatment of single-segment thoracic spinal tuberculosis with neurological deficits in adults: a retrospective study of 34 cases. BMC Musculoskelet Disord. 2015;16(186). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang HQ, Li JS, Zhao SS, Shao YX, Liu SH, Gao Q, et al. Surgical management for thoracic spinal tuberculosis in the elderly: posterior only versus combined posterior and anterior approaches. Arch Orthop Trauma Surg. 2012;132(12):1717–23. 10.1007/s00402-012-1618-0 [DOI] [PubMed] [Google Scholar]
- 3.Chen ST., Zhao LP, Dong WJ, Gu YT, Li YX, Dong LL, et al. The Clinical Features and Bacteriological Characterizations of Bone and Joint Tuberculosis in China. Sci Rep. 2015;5:11084 10.1038/srep11084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sandher DS, Al-Jibury M, Paton RW, Ormerod LP. Bone and joint tuberculosis: cases in Blackburn between 1988 and 2005. J Bone Joint Surg Br. 2007;89(10):1379–81. 10.1302/0301-620X.89B10.18943 [DOI] [PubMed] [Google Scholar]
- 5.Yin XH, Zhou ZH, Yu HG, Hu XK, Guo Q, Zhang HQ. Comparison between the antero-posterior and posterior only approaches for treating thoracolumbar tuberculosis (T10-L2) with kyphosis in children: a minimum 3-year follow-up. Childs Nerv Syst. 2016;32(1):127–33. 10.1007/s00381-015-2935-8 [DOI] [PubMed] [Google Scholar]
- 6.Zhang H, Zeng K, Yin X, Huang J, Tang M, Guo C. Debridement, internal fixation, and reconstruction using titanium mesh for the surgical treatment of thoracic and lumbar spinal tuberculosis via a posterior-only approach: a 4-year follow-up of 28 patients. J Orthop Surg Res. 2015;10(150). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tosun B, Erdemir C, Yonga O, Selek O. Surgical treatment of thoracolumbar tuberculosis: a retrospective analysis of autogenous grafting versus expandable cages. Eur Spine J. 2014;23(11):2299–306. 10.1007/s00586-014-3565-7 [DOI] [PubMed] [Google Scholar]
- 8.Shen XJ, Liu HZ, Wang GP, Liu XY. Single-stage posterior-only approach treating single-segment thoracic tubercular spondylitis. Int J Clin Exp Pathol. 2015;8(9):11051–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Sahoo MM, Mahapatra S, Sethi GC. Posterior-only Approach Surgery for Fixation and Decompression of Thoracolumbar Spinal Tuberculosis. J Spinal Disord Tech. 2013;25:217–23. [DOI] [PubMed] [Google Scholar]
- 10.Sundararaj GD, Amritanand R, Venkatesh K, Arockiaraj J. The use of titanium mesh cages in the reconstruction of anterior column defects in active spinal infections: can we rest the crest? Asian Spine J. 2011;5(3):155–61. 10.4184/asj.2011.5.3.155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gong K, Wang Z, Luo Z. Single-stage posterior debridement and transforaminal lumbar interbody fusion with autogenous bone grafting and posterior instrumentation in the surgical management of lumbar tuberculosis. Arch Orthop Trauma Surg. 2011;131(2):217–23. 10.1007/s00402-010-1138-8 [DOI] [PubMed] [Google Scholar]
- 12.Korovessis P, Petsinis G, Koureas G, Iliopoulos P, Zacharatos S. Anterior surgery with insertion of titanium mesh cage and posterior instrumented fusion performed sequentially on the same day under one anesthesia for septic spondylitis of thoracolumbar spine: is the use of titanium mesh cages safe? Spine 2006;31(9):1014–9. 10.1097/01.brs.0000215049.08622.9d [DOI] [PubMed] [Google Scholar]
- 13.Ozdemir HM, Us AK, Oğün T. The role of anterior spinal instrumentation and allograft fibula for the treatment of pott disease. Spine. 2003;28(5):474–9. 10.1097/01.BRS.0000048666.17934.17 [DOI] [PubMed] [Google Scholar]
- 14.Wang B, Lv G, Liu W, Cheng I. Anterior radical debridement and reconstruction using titanium mesh cage for the surgical treatment of thoracic and thoracolumbar spinal tuberculosis: minimium five-year follow-up. Turk Neurosurg. 2011;21(4):575–81. [PubMed] [Google Scholar]
- 15.Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine. 1995;20(12):1410–8. [PubMed] [Google Scholar]
- 16.Garg RK, Somvanshi DS. Spinal tuberculosis: a review. J Spinal Cord Med. 2011;34(5):440–54. 10.1179/2045772311Y.0000000023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Loenhout-Rooyackers JH, Verbeek AL, Jutte PC. Chemotherapeutic treatment for spinal tuberculosis. Int J Tuberc Lung Dis. 2002;6(3):259–65. [PubMed] [Google Scholar]
- 18.Organization. WH. Treatment of tuberculosis: guidelines. 4th ed (WHO/HTM/TB/2009.420) World Health Organization; 2010. [assessed on 2011 Apr 16].(http://whqlibdoc.who.int/publications/2010/9789241547833_eng.pdf). [Google Scholar]
- 19.Bass JB Jr., Farer LS, Hopewell PC, O'Brien R, Jacobs RF, Ruben F, et al. Treatment of tuberculosis and tuberculosis infection in adults and children. American Thoracic Society and The Centers for Disease Control and Prevention. Am J Respir Crit Care Med. 1994;149(5):1359–74. 10.1164/ajrccm.149.5.8173779 [DOI] [PubMed] [Google Scholar]
- 20.Joint Tuberculosis Committee of the British Thoracic Society Chemotherapy and management of tuberculosis in the United Kingdom: recommendations 1998. Thorax. 1998;53(7):536–48. [PMC free article] [PubMed] [Google Scholar]
- 21.Donald PR. The chemotherapy of osteo-articular tuberculosis with recommendations for treatment of children. J Infect. 2011;62(6):411–39. 10.1016/j.jinf.2011.04.239 [DOI] [PubMed] [Google Scholar]
- 22.Yin XH, Liu SH, Li JS, Chen Y, Hu XK, Zeng KF, et al. The role of costotransverse radical debridement, fusion and postural drainage in the surgical treatment of multisegmental thoracic spinal tuberculosis: a minimum 5-year follow-up. Eur Spine J. 2016;25(4):1047–55. 10.1007/s00586-015-4283-5 [DOI] [PubMed] [Google Scholar]
- 23.Mei G, Luo F, Zhang Z, Dai F, Zhou Q, He Q, et al. Treatment Experiences and Management Outcomes for Skipped Multisegmental Spinal Tuberculosis. Orthopedics. 2016;39(1):e19–25. 10.3928/01477447-20151218-04 [DOI] [PubMed] [Google Scholar]
- 24.Gao Z, Wang M, Zhu W, Zheng G, Meng Y. Tuberculosis of ultralong segmental thoracic and lumbar vertebrae treated by posterior fixation and cleaning of the infection center through a cross-window. Spine J. 2015;15(1):71–8. 10.1016/j.spinee.2014.06.025 [DOI] [PubMed] [Google Scholar]
- 25.Yin XH, Liu SH, Li JS, Chen Y, Hu XK, Zeng KF, et al. The role of costotransverse radical debridement, fusion and postural drainage in the surgical treatment of multisegmental thoracic spinal tuberculosis: a minimum 5-year follow-up. Eur Spine J. 2015. [DOI] [PubMed] [Google Scholar]
- 26.TANG S. Annual Report on Clinical Diagnosis and Treatment Progress of Tuberculosis(2012)(Part 2 Clinical Treatment). Chin J Antituberc. 2013;35(7):488–510. [Google Scholar]
- 27.Shi J, Tang X, Xu Y, Zhou T, Pan X, Lin H, et al. Single-stage internal fixation for thoracolumbar spinal tuberculosis using 4 different surgical approaches. J Spinal Disord Tech. 2014;27(7):E247–57. 10.1097/BSD.0000000000000100 [DOI] [PubMed] [Google Scholar]
- 28.Pang X, Shen X, Wu P, Luo C, Xu Z, Wang X. Thoracolumbar spinal tuberculosis with psoas abscesses treated by one-stage posterior transforaminal lumbar debridement, interbody fusion, posterior instrumentation, and postural drainage. Arch Orthop Trauma Surg. 2013;133(6):765–72. 10.1007/s00402-013-1722-9 [DOI] [PubMed] [Google Scholar]
- 29.Qureshi MA, Khalique AB, Afzal W, Pasha IF, Aebi M. Surgical management of contiguous multilevel thoracolumbar tuberculous spondylitis. Eur Spine J. 2013;22 Suppl 4:618–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang HQ, Lin MZ, Shen KY, Ge L, Li JS, Tang MX, et al. Surgical management for multilevel noncontiguous thoracic spinal tuberculosis by single-stage posterior transforaminal thoracic debridement, limited decompression, interbody fusion, and posterior instrumentation (modified TTIF). Arch Orthop Trauma Surg. 2012;132(6):751–7. 10.1007/s00402-012-1473-z [DOI] [PubMed] [Google Scholar]
- 31.Panchmatia JR, Lenke LG, Molloy S, Cheung KM, Kebaish KM. Review article: Surgical approaches for correction of post-tubercular kyphosis. J Orthop Surg (Hong Kong). 2015;23(3):391–4. [DOI] [PubMed] [Google Scholar]
- 32.Yin XH, Zhou ZH, Yu HG, Hu XK, Guo Q, Zhang HQ. Comparison between the antero-posterior and posterior only approaches for treating thoracolumbar tuberculosis (T10-L2) with kyphosis in children: a minimum 3-year follow-up. Child's nervous system: ChNS: official journal of the International Society for Pediatric Neurosurgery. 2016;32(1):127–33. [DOI] [PubMed] [Google Scholar]
- 33.Azam MQ, Sadat-Ali M. The Concept of Evolution of Thoracolumbar Fracture Classifications Helps in Surgical Decisions. Asian Spine Journal. 2015;9(6):984–94. 10.4184/asj.2015.9.6.984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang B, L G, Liu W, Cheng I. Anterior radical debridement and reconstruction using titanium mesh cage for the surgical treatment of thoracic and thoracolumbar spinal tuberculosis: minimium five-year follow-up. Turk Neurosurg. 2011;21(4):575–81. [PubMed] [Google Scholar]
- 35.Oga M, Arizono T, Takasita M, Sugioka Y. Evaluation of the risk of instrumentation as a foreign body in spinal tuberculosis. Clinical and biologic study. Spine. 1993;18(13):1890–4. [DOI] [PubMed] [Google Scholar]
- 36.Arrington ED, Smith WJ, Chambers HG, Bucknell AL, Davino NA. Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res. 1996;(329):300–9. [DOI] [PubMed] [Google Scholar]
- 37.Christodoulou AG, Givissis P, Karataglis D, Symeonidis PD, Pournaras J. Treatment of tuberculous spondylitis with anterior stabilization and titanium cage. Clin Orthop Relat Res. 2006;444:60–5. 10.1097/01.blo.0000201175.87635.28 [DOI] [PubMed] [Google Scholar]
- 38.Erturer E, Tezer M, Aydogan M, Mirzanli C, Ozturk I. The results of simultaneous posterior-anterior-posterior surgery in multilevel tuberculosis spondylitis associated with severe kyphosis. Eur Spine J. 2010;19(12):2209–15. 10.1007/s00586-010-1481-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
It contains the Ethical Approval Form and translation document.
(ZIP)
It’s a informed consent form template for clinical trials.
(ZIP)
Data Availability Statement
Data contains confidential participant information and cannot be shared publicly, in accordance with the restrictions of the Institutional Review Board of the First Affiliated Hospital of Chongqing Medical University, which approved this study. Readers may request access to data and direct questions about the data availability to the IRB at 1262744150@qq.com.