Abstract
Evidence suggests that both dissociation and negative affect (NA) may precipitate binge eating. The extent to which dissociation may impact the experience of negative affect around binge eating is unclear. Women with bulimia nervosa completed a two-week ecological momentary assessment protocol of dissociation, NA, and binge eating. Multilevel modeling was used to examine dissociation as a moderator of NA preceding and following binge eating. NA was greater at the time of binge eating for participants higher in average dissociation (between-subjects) and when momentary dissociation was greater than one's average (within-subjects). The trajectory of NA was characterized by a sharper decline after binge eating for participants higher in average dissociation; the NA trajectories were characterized by sharper increases before and decreases after binge eating when momentary dissociation was greater than one's average. Results support the salience of both dissociation and NA in relation to the occurrence of binge eating.
Keywords: binge eating, dissociation, negative affect, bulimia nervosa
Bulimia nervosa (BN) is a serious psychiatric disorder characterized by recurrent binge eating (i.e., eating an unusually large amount of food with a subjective sense of loss of control) and compensatory behaviors (e.g., vomiting, laxative use, excessive exercise). Several theories have been offered to explain the etiology and/or maintenance of bulimic symptoms, particularly binge eating. For instance, escape theory (Heatherton & Baumeister, 1991) proposes that individuals engage in binge eating as a method of escaping from aversive self-awareness. Essentially, binge eating provides an opportunity for individuals to avert their attention from negative affect (NA) and other aversive internal experiences and instead focus attention on food (i.e., an external stimulus) and its consumption. This process can be conceptualized as a form of dissociation from self-awareness in which individuals with BN achieve a low level of cognitive awareness and are less influenced by subjective concerns such as guilt or fear of weight gain (Everill & Waller, 1995). Relatedly, the affect regulation model (Polivy & Herman, 1993) suggests that individuals engage in binge eating to cope with NA, which in turn, functions to reduce NA. Binge eating is therefore theorized to be maintained through negative reinforcement processes. Thus, prominent theories of binge eating emphasize the salience of the experience of both negative affective states and dissociation from self-awareness, or cognitive narrowing.
Negative Affect and Binge Eating
The affect regulation model of binge eating has also been examined in numerous research studies. Most notable is a substantial literature based on studies utilizing ecological momentary assessment (EMA), which is an intensive longitudinal data collection method where participants report on experiences multiple times over the course of a day for a short period of time (e.g., one or two weeks). Such research has sought to evaluate the affect regulation model by examining momentary experiences of negative affective states prior to and following binge eating behaviors in the natural environment. Existing evidence supports the presence of high or increasing NA antecedent to binge eating, although findings based on varying statistical methodologies have been mixed regarding reductions in NA following binge eating (Haedt-Matt & Keel, 2011; Lavender et al., 2016; Smyth et al., 2007). Research utilizing experimental methods has also provided some support for the affect regulation model, particularly in terms of negative affective states as precipitants of binge eating behavior (e.g., Leehr et al., 2015). Consistent with escape theory, the affect regulation model may be enhanced by including dissociation as a moderating factor of the association between negative affect and binge eating.
Dissociation and Binge Eating
Dissociation has been defined as the “lack of the normal integration of thoughts, feelings, and experiences into the stream of consciousness and memory process” (Bernstein, & Putnam, 1986, p. 727). Experimentally-induced dissociation has been shown to impair cognition, including visual memory (Brewin & Mersaditabari, 2013), subjective memory (Kindt, Van den Hout, & Buck, 2005), attention (Brewin, Ma, & Colson, 2013), and cognitive inhibition (Winter et al., 2015). Further, during clinical observations, individuals with BN often report feelings of depersonalization, such as watching oneself from the outside and being unlike one's usual self (Cowan, & Heselmeyer, 2011). Accordingly, individuals with eating disorders have been found to display elevated dissociation, as well as greater avoidance of affect, worse distress tolerance, and reduced emotional clarity and awareness (Demitrack, Brewerton, & Gold, 1990; Lavender et al., 2015).
Preliminary research has demonstrated the salience of state and momentary dissociation in the context of BN. An experimental study demonstrated that subliminal abandonment cues significantly increased state dissociation among women with BN, but not controls (Hallings-Pott, Waller, Watson, & Scragg, 2005). Additionally, in an EMA study of women with BN, Engelberg, Steiger, Gauvin, and Wonderlich (2007) found that dissociation was elevated prior to binge eating episodes. A separate study in which women with BN completed a dissociation questionnaire before, during, and after a binge eating and purging episode found that depersonalization scores reported just before binge eating were significantly lower than scores during the binge, as well as significantly lower after the binge (but before purging occurred) (McShane & Zirkel, 2008). Empirical findings thus support an association between dissociation and binge eating, and evidence suggests that dissociation may increase from the time before a binge eating episode through the period in which it occurs.
Current Study
Despite significant theoretical and empirical attention to both NA and dissociation in relation to binge eating, further research on potential interactions between these constructs is needed. In particular, there is currently a lack of evidence regarding the role of dissociation from self-awareness in relation to the experience of NA around a binge eating episode in the natural environment. Thus, this investigation used EMA data to examine dissociation scores at the time of binge eating as a moderator of NA trajectories antecedent to and following binge eating. Given that dissociation may operate as mechanism for avoidance of aversive affective experiences, it was hypothesized that higher levels of dissociation at the time of a binge eating episode (within-subjects) would be characterized by significantly greater increases in NA prior to binge eating. Further, because dissociation may provide a temporary relief from negative emotions, it was hypothesized that higher levels of dissociation at the time of a binge eating episode would be characterized significantly greater decreases in NA following binge eating. We also hypothesized that individual differences in dissociation (between-subjects) would be associated with negative affect such that individuals generally higher in dissociation would have greater negative affect. However, how the trajectory of negative affect changed prior to and following binge eating as a function of individual differences in dissociation was an exploratory question.
Method
Participants
Women who met Diagnostic and Statistical Manual of Mental Disorders 4th edition (DSM-IV; American Psychiatric Association, 1994) criteria for BN (N = 133) were recruited through clinical, community, and university advertisements in the Midwestern U. S. Participants were excluded from the study if they were under 18 years of age. Participants had a mean age of 25.3 years (SD = 7.6; Range = 18–55) and a mean body mass index (BMI) of 23.8 kg/m2 (SD = 5.2). Most participants were Caucasian (97.0%), currently employed (73.3%), and had never been married (64.7%). About 19.5% of the sample had a bachelor's degree or higher, 62.4% had some college, 5.3% had a degree from a trade or technical school, and 12.8% had high school or lower. Lifetime rates of Axis I disorders were 87.0% for mood disorders, 59.5% for anxiety disorders, and 54.2% for substance dependence. This sample has previously been reported on in Smyth et al., (2007).
Measures
The current study used EMA data collected via two types of daily self-report methods. Event-contingent reporting involved participants completing an assessment when a binge eating episode occurred. The second method, signal-contingent reporting, required participants to complete an assessment at various times throughout the day in response to six semi-random signals distributed around six anchor points (i.e., 8:30 a.m., 11:10 a.m., 1:50 p.m., 4:30 p.m., 7:10 p.m., and 9:50 p.m.). Participants were asked to rate items assessing NA and dissociation. NA was assessed using 11 items from the Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988): afraid, lonely, irritable, ashamed, disgusted, nervous, dissatisfied with self, jittery, sad, distressed, and angry with self. Dissociation was assessed using three items (“in contact with true self,” “confused as to who I am,” “and out of touch with myself”), which addressed the dissociation constructs of depersonalization/derealization (i.e., feelings of separation from one's sense of self and disembodiment; Sedeño et al., 2014). NA and dissociation items were rated on a Likert-type scale ranging from 1 (not at all) to 5 (extremely). Items were summed to create total NA (alpha = .92) and dissociation (alpha = .83) scores
Procedure
Participants attended an informational meeting during which they were briefed about the study, completed an informed consent, and completed a screening to ensure medical stability. Participants attended two assessment visits. During the initial assessment, structured clinical interviews were conducted to assess eating disorder symptoms and comorbid psychopathology. Also, participants received training in the use of the palmtop computer to complete their EMA reports, were reminded of the goals of the study, and were given the opportunity to ask questions about the study protocol. In addition, participants received training on the definition of a binge eating episode (i.e., “an amount of food that you consider excessive, or an amount of food that others would consider excessive, with an associated loss of control or the feeling of being compelled to eat”). Participants were instructed not to complete entries at times when they felt unable to reply or when safety was a concern (e.g., while driving). However, participants were encouraged to complete the entry as soon as possible when able. Participants completed two practice days of EMA, after which they returned for a visit with study staff in which they received feedback regarding their compliance. Practice data were not used in analyses. Participants then began the two week EMA protocol with the palmtop computer. In order to reduce the chance of lost data, study staff scheduled two visits for each participant during the two week EMA period to collect palmtop data. During these visits, participants were given feedback regarding compliance rates and collected data was stored. Participants received monetary compensation for participating in the study. This research was institutional review board approved and was carried out in accordance with the provisions of the World Medical Association Declaration of Helsinki.
Statistical Analyses
Multilevel modeling via SPSS version 22 was used to examine within-day relationships between NA, dissociation, and binge eating. NA was examined both antecedent and consequent to binge eating. Multilevel models included a random intercept, fixed effects for the linear (hours), quadratic (hours-squared) and cubic (hours-cubed) time before/after the behavior, and interactions between those time components and a dummy-coded variable representing pre- vs. post-behavior. This allowed us to include both antecedent and consequent NA in one model and to additionally estimate a common intercept for the antecedent and consequence portions of the model. If separate models were estimated for the antecedent and consequence portions, we would obtain two separate, and likely different, intercepts. This would appear to show a precipitous rise or fall in NA immediately at the time of the behavior; although, NA assessments close to the behaviors likely would not show this change. The linear effect allows there to be a constant linear relationship between hours and negative affect. The quadratic effect allows the relationship to curve or bend once and the cubic term allows a second curve or bend.
Between-subjects dissociation was calculated by computing each person's average level of dissociation across all recordings of the EMA protocol. Within-subjects dissociation was calculated by subtracting each person's average level of dissociation across all recordings of the EMA protocol from their level of dissociation at the time of the binge eating episode. Between- and within-subjects dissociation at the time of binge eating were added to the model both as main effects and interactions with other effects in the model, allowing the estimation of separate pre- and post-binge eating trajectories for each level of between- and within subjects dissociation at the time of binge eating. Consistent with previous studies (e.g., Smyth et al., 2007), only the first binge eating event for the day was used when there were multiple events in one day to avoid confounding the effects of NA as an antecedent to the second event with the effects of NA following the event. Otherwise, we used all available data from the EMA data to model the NA curves.
Results
A total of 13,005 ratings were collected over with course of the course of the EMA protocol. Participants’ compliance with signal-contingent ratings averaged 86%. The majority of signal-contingent ratings were made within 5 minutes and 75% were made within 20 minutes of the signal. Women reported an average of 8.65 binges (SD = 6.68; range =1-34) over the course of 2-week EMA protocol. The grand mean of dissociation was 2.58 (SD = 1.06). Results are displayed in Table 1 and Figure 1. NA exhibited a significant increase prior to (linear estimate = −1.54, SE = 0.14, p < .001, 95% CI [−1.80, −1.27]); quadratic estimate = 0.14, SE = 0.02, p < .001, 95% CI [0.10, 0.19]; cubic estimate = −0.004, SE = 0.001, p < .001, 95% CI [−0.006, −.002]) and decrease after (linear estimate = 3.85, SE = 0.21, p < .001, 95% CI [3.44, 4.27]); quadratic estimate = 0.07, SE = 0.3, p =.01, 95% CI [0.02, .12]; cubic estimate = 0.009, SE = 0.001, p < .001, 95% CI [0.007, 0.01]) binge eating.
Table 1.
Multilevel Models for Negative Affect Before and After Binge Eating Moderated by Dissociation
| Parameter | Estimate | SE | p | 95% CI |
|---|---|---|---|---|
| Intercepts | ||||
| Intercept | 29.59 | .42 | <.001 | [28.76, 30.43] |
| Between-subjects dissociation | 6.48 | .43 | <.001 | [5.62, 7.33] |
| Within-subjects dissociation | 5.19 | .30 | <.001 | [4.60, 5.78] |
| Antecedent Curves | ||||
| (Hours to behavior)*Pre/Post | 3.85 | .21 | <.001 | [3.44, 4.27] |
| (Hours to behavior)2*Pre/Post | .07 | .03 | .01 | [.02, .12] |
| (Hours to behavior)3*Pre/Post | .009 | .001 | <.001 | [.007, .01] |
| (Hours to behavior)*Between-subjects dissociation *Pre/Post | .79 | .22 | <.001 | [.35, 1.23] |
| (Hours to behavior)2*Between-subjects dissociation *Pre/Post | .08 | .03 | .01 | [.02, .13] |
| (Hours to behavior)3*Between-subjects dissociation *Pre/Post | .002 | .001 | .23 | [−.001 .004] |
| (Hours to behavior)*Within-subjects dissociation *Pre/Post | −2.76 | .34 | <.001 | [2.10, 3.43] |
| (Hours to behavior)2*Within-subjects dissociation *Pre/Post | .05 | .04 | .22 | [−.03, .13] |
| (Hours to behavior)3*Within-subjects dissociation *Pre/Post | .008 | .002 | <.001 | [.004, .01] |
| Consequence Curves | ||||
| Hours to behavior | −1.54 | .14 | <.001 | [−1.80, −1.27] |
| Hours to behavior2 | .14 | .02 | <.001 | [.10, .19] |
| Hours to behavior3 | −.004 | .001 | <.001 | [−.006, −.002] |
| (Hours to behavior)*Between-subjects dissociation | −.13 | .15 | .39 | [−.42, .16] |
| (Hours to behavior)2*Between-subjects dissociation | −.005 | .02 | .83 | [−.05, .04] |
| (Hours to behavior)3*Between-subjects dissociation | .0004 | .001 | .66 | [−.001 .002] |
| (Hours to behavior)*Within-subjects dissociation | −1.15 | .22 | <.001 | [−1.57, −.72] |
| (Hours to behavior)2*Within-subjects dissociation | .11 | .04 | .002 | [.04, .18] |
| (Hours to behavior)3*Within -subjects dissociation | −.003 | .001 | .02 | [−.006, .0004] |
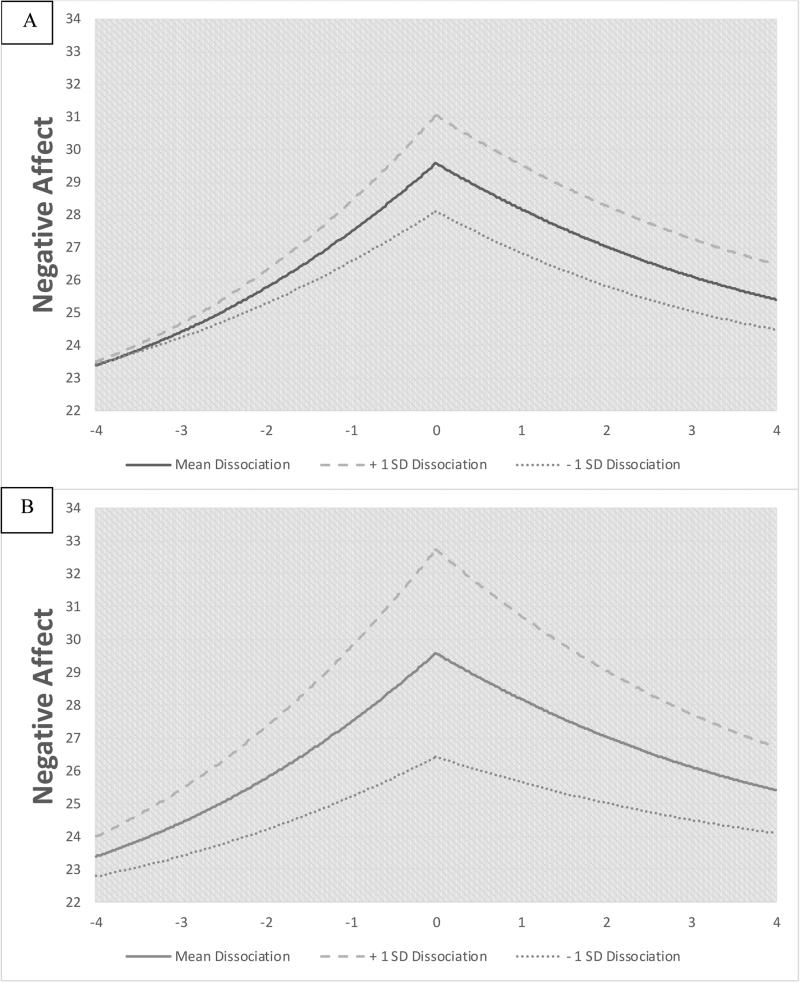
Figure 1.
A) Temporal association between negative affect and binge eating moderated by between-subjects dissociation; B) Temporal association between negative affect and binge eating moderated by within-subjects dissociation.
Within-Subjects Moderation
Episodes where individuals reported more dissociation compared to their individual average (within-subjects dissociation) were characterized by greater NA at the time of binge eating (intercept estimate = 5.19, SE = 0.30, p < .001, 95% CI [4.60, 5.78]). Furthermore, antecedent NA increased more rapidly prior to binge eating (linear estimate = −1.15, SE = 0.22, p < .001, 95% CI [−1.57, −0.72]; quadratic estimate = 0.11, SE = 0.04, p = .002, 95% CI [0.04, 0.18]; cubic estimate = −0.003, SE = 0.001, p = .02, 95% CI [−0.006, 0.0004]) and decreased more rapidly after binge eating (linear estimate = −2.76, SE = 0.34, p < .001, 95% CI [2.10, 3.43]) on those occasions in which they experienced higher than average levels of dissociation. Figure 1B displays the negative affect trajectory at three levels of within-subjects dissociation: one SD above the mean, the mean, and one SD below the mean).
Between-Subjects Moderation
Individuals generally higher in dissociation (between-subjects dissociation) displayed higher NA at the time of binge eating (intercept estimate = 6.48, SE = 0.43, p < .001, 95% CI [5.62, 7.33]). Antecedent NA did not differ as a function of between-subjects dissociation, although NA decreased more rapidly after binge eating for individuals higher in dissociation (linear by between-subject dissociation by pre-post estimate = 0.79, SE = 0.22, p < .001, 95% CI [0.35, 1.23]; quadratic by between-subject dissociation by pre-post estimate = 0.08, SE = 0.03, p = .01, 95% CI [0.02, 0.13]). Figure 1A displays the negative affect trajectory at three levels of between-subjects dissociation: one SD above the mean, the mean, and one SD below the mean).
Discussion
The current study found that the trajectory of NA prior to binge eating was moderated by within-subjects levels of dissociation, whereas the trajectory of NA after binge eating was moderated by both between- and within-subjects levels of dissociation. These results extend the findings of a previous EMA study that found that NA and dissociation were antecedents of binge eating in women with BN (Engelberg et al., 2007). The current findings revealed that individuals who tend to dissociate more at the time of binge eating show a steeper decline in NA after binge eating, whereas those who tend to dissociate less show a slightly lower decline in NA after binge eating. A more pronounced difference in NA trajectories was found as a function of within-subjects dissociation. Episodes of binge eating wherein individuals reported higher dissociation compared to their average were preceded by a more rapid increase in NA, peaked at a higher level of NA, and had a steeper drop in NA afterwards. Episodes of binge eating where individuals reported lower dissociation compared to their average were preceded by a smaller increase in NA, which dropped to pre-binge eating levels of NA subsequent to the binge.
Emotion dysregulation is a common feature of BN (Lavender et al., 2015) and is manifested in various ways (e.g., poor distress tolerance, emotion suppression, lack of emotional clarity, etc.). Further, prominent theories of binge eating emphasize the relevance of both momentary dissociation and negative affective states in terms of the occurrence of binge eating. The current results demonstrated that on occasions when individuals reported levels of dissociation that were higher than their average, their NA prior to binge eating had increased more sharply compared to episodes with lower levels of dissociation, perhaps indicating that dissociation is most typical in moments of heightened aversive affect and reduces awareness of these negative internal experiences. Thus, consistent with escape theory, escape theory, lowered self-awareness (akin to dissociation) may lead to loss of control over eating. While our study examined the interactional relationship between NA and dissociation predicting binge eating, it is important to note that a previous EMA study found that concurrent momentary dissociation and NA both uniquely predicted binge eating (Engelberg et al., 2007), suggesting the potential for independent contributions of these two constructs.
We also found that the NA steadily decreases after binge eating regardless of dissociation. Thus, dissociation appears to be a short-term cognitive process that occurs before binge eating and dissipates afterwards. It is possible that binge eating brings the individual “back to reality.” For example, after binge eating, individuals may begin to feel physical discomfort or bloating (Abraham & Beumont, 1982), which they are not able to ignore. In addition, because NA decreased more sharply when dissociation was higher than average, dissociation may help avoid emotional experiences by impairing cognitive processing (Brewin, Ma, & Colson, 2013; Brewin & Mersaditabari, 2013; Kindt, Van den Hout, & Buck, 2005).
Strengths and Limitations
An important strength of this study was the use of EMA methodology to examine experiences of dissociation and NA in the natural environment. In the present study, the momentary nature of the data minimized recall bias, and also allowed for the examination of how dissociation moderated the temporal associations (both antecedent and consequent) between NA and bulimic behaviors. However, even with these strengths, there were limitations of this investigation that must be considered. First, although participants were largely compliant with the EMA protocol, it is possible that not all binge eating episodes were recorded, which could bias the results. Second, a three item scale was developed for this study to assess dissociation in daily life, which demonstrated excellent reliability. This was helpful in reducing burden on respondents who were completing multiple reports each day, but a longer measure may have been more psychometrically sound. Third, given that dissociation is a process involving low self-awareness, it is unclear what effect completing the EMA measures had on self-awareness. Finally, while our results indicate that the experience of dissociation around the time of an eating binge is related to antecedent and/or consequent NA following a binge, these results do not speak to the extent to which NA fosters dissociation, dissociation fosters NA, or both. Future studies should address this separate, but potentially useful, research question. Finally, some conceptualizations of dissociation include loss of control as an explicit component of dissociation (Vanderlinden, van Dyck, Vandereycken, Vertommen, & Verkees, 1993). More research is needed to clarify how loss of control is similar and different to other aspects of dissociation.
Clinical Implications
These results highlight the potential utility of psychotherapeutic interventions that focus on effective and adaptive emotion regulation, as well as remaining self-aware even when emotionally distressed, in order to prevent binge eating. For instance, one major clinical target in Integrative Cognitive-Affective Therapy (ICAT) for BN (Wonderlich, Peterson, Smith, Klein, Mitchell, & Crow, 2015) is to help individuals to develop skills to effectively cope with momentary emotions and prevent the occurrence of rash behaviors such as binge eating. In addition, several therapies integrate tenets of mindfulness training to help individuals remain aware and present in their environment and to reduce the emotional intensity of negative experiences (Singh, Lancioni, Wahler, Winton, & Singh, 2008).
Footnotes
There are no conflicts of interest to report.
References
- Abraham SF, Beumont PJV. How patients describe bulimia or binge eating. Psychol Med. 1982;12:625–635. doi: 10.1017/s0033291700055732. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis. 1986;174:727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Ma BY, Colson J. Effects of experimentally induced dissociation on attention and memory. Conscious Cogn. 2013;22:315–323. doi: 10.1016/j.concog.2012.08.005. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Mersaditabari N. Experimentally-induced dissociation impairs visual memory. Conscious Cogn. 2013;22:1189–1194. doi: 10.1016/j.concog.2013.07.007. [DOI] [PubMed] [Google Scholar]
- Cowan E, Heselmeyer R. Bulimia and dissociation: A developmental perspective. J Ment Health Couns. 2011;33:128–143. [Google Scholar]
- Demitrack MA, Brewerton TD, Gold PW. Relation of clinical variables to dissociative phenomena in eating disorders. Am J Psychiatry. 1990;147:1184–1188. doi: 10.1176/ajp.147.9.1184. [DOI] [PubMed] [Google Scholar]
- Engelberg MJ, Steiger H, Gauvin L, Wonderlich SA. Binge antecedents in bulimic syndromes: An examination of dissociation and negative affect. Int J Eat Disorder. 2007;40:531–536. doi: 10.1002/eat.20399. [DOI] [PubMed] [Google Scholar]
- Everill JT, Waller G. Dissociation and bulimia: Research and theory. Eur Eat Disord Rev. 1995;3:129–147. [Google Scholar]
- Foa E, Hembree E, Rothbaum BO. Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences therapist guide. Oxford University Press; 2007. [Google Scholar]
- Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychol Bull. 2011;137:660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallings-Pott C, Waller G, Watson D, Scragg P. State dissociation in bulimic eating disorders: An experimental study. Int J Eat Disorder. 2005;38:37–41. doi: 10.1002/eat.20146. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychol Bull. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Polivy J, Herman CP, Baumeister RF. Self-awareness, task failure, and disinhibition: How attentional focus affects eating. J Pers. 1993;61:49–61. doi: 10.1111/j.1467-6494.1993.tb00278.x. [DOI] [PubMed] [Google Scholar]
- Kindt M, Van den Hout M, Buck N. Dissociation related to subjective memory fragmentation and intrusions but not to objective memory disturbances. J Behav Ther Exp Psy. 2005;36:43–59. doi: 10.1016/j.jbtep.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Lavender JM, Utzinger LM, Cao L, Wonderlich SA, Engel SG, Mitchell JE, Crosby RD. Reciprocal associations between negative affect, binge eating, and purging in the natural environment in women with bulimia nervosa. J Abnor Psychol. 2016;125:381–386. doi: 10.1037/abn0000135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clin Psychol Rev. 2015;40:111–122. doi: 10.1016/j.cpr.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leehr EJ, Krohmer K, Schag K, Dresler T, Zipfel S, Giel KE. Emotion regulation model in binge eating disorder and obesity-a systematic review. Neurosci Biobehav R. 2015;49:125–134. doi: 10.1016/j.neubiorev.2014.12.008. [DOI] [PubMed] [Google Scholar]
- McShane JM, Zirkel S. Dissociation in the binge–purge cycle of bulimia nervosa. J Trauma Dissociation. 2008;9:463–479. doi: 10.1080/15299730802225680. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman CP. Etiology of binge eating: Psychological mechanisms. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. Guilford Press; New York, NY, US: 1993. pp. 173–205. [Google Scholar]
- Sedeño L, Couto B, Melloni M, Canales-Johnson A, Yoris A, Baez S, Esteves S, Velásquez M, Barttfeld P, Sigman M, Kichic R. How do you feel when you can't feel your body? Interoception, functional connectivity and emotional processing in depersonalization-derealization disorder. PloS one. 2014;9:e98769. doi: 10.1371/journal.pone.0098769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh NN, Lancioni GE, Wahler RG, Winton AS, Singh J. Mindfulness approaches in cognitive behavior therapy. Behav Cogn Psychoth. 2008;36:659–666. [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. J Consult Clin Psychol. 2007;75:629. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Stice E. A prospective test of the dual-pathway model of bulimic pathology: mediating effects of dieting and negative affect. J Abnor Psychol. 2001;110:825–848. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Winter D, Krause-Utz A, Lis S, Chiu CD, Lanius RA, Schriner F, Bohus M, Schmahl C. Dissociation in borderline personality disorder: Disturbed cognitive and emotional inhibition and its neural correlates. Psychiat Res-Neuroim. 2015;233:339–351. doi: 10.1016/j.pscychresns.2015.05.018. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Peterson CB, Smith TL, Klein MH, Mitchell JE, Crow SJ. Integrative cognitive-affective therapy for bulimia nervosa: A treatment manual. Guilford Publication; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]