Abstract
Objective
There is a high occurrence of sexual assault (SA) and intimate partner violence (IPV) among people with substance use disorders and an established association between substance use and posttraumatic stress disorder (PTSD), but no research has examined associations between combinations of these traumas and PTSD symptom profiles among people who abuse substances. Thus, this study aimed to examine how combinations of SA and IPV histories contribute to the severity of symptoms within PTSD symptom clusters above and beyond the impact of exposure to other traumas in a substance abusing population.
Method
Participants were men and women (N = 219) with trauma histories seeking treatment in a substance abuse facility. MANCOVA analyses examined differences on Clinician Administrated PTSD Scale cluster scores in people with experiences of SA and/or IPV in comparison to people with other types of trauma, controlling for number of PTSD criterion A events.
Results
SA was associated with increased symptom severity across all three PTSD symptom clusters, while IPV was not associated with differences in cluster scores. In addition, survivors of IPV had consistent levels of avoidance symptoms regardless of whether they had also experienced SA, but people who had not experienced IPV only evidenced increased avoidance symptoms when they had experienced SA. Follow-up analyses testing gender differences indicated that these findings were largely similar for men and women.
Conclusions
SA should be assessed in people in substance use treatment settings to conceptualize their unique presentations of PTSD symptoms and inform treatment planning.
Keywords: rape, domestic violence, mental disorders, substance use, posttraumatic stress
Sexual assault (SA) and violence committed by an intimate partner (IPV) are staggeringly common experiences in the lives of people with substance use disorders. In their lifetimes, estimates suggest that 21.7% of US women and 7.3% of men will experience IPV, and 17.6% of women and 3.0% of men will be raped (Tjaden & Thoennes, 2000; 2006). These prevalence rates are even higher among people seeking treatment for substance use disorders: a study of substance-dependent inpatients reported that 69% of women and 17% of men had a history of lifetime SA (Grice, Brady, Dustan, Malcolm & Kilpatrick, 1995), and a review suggested that the rates of past-year IPV among people receiving treatment for alcohol use disorders is four to six times higher than the general population (Klostermann & Fals-Stewart, 2006). In addition, SA and IPV are often overlapping experiences, in that SA is commonly perpetrated by an intimate partner (Basile et al., 2004), and a history of multiple victimization by both IPV and SA is common (Follette, Polusny, Bechtle, & Naugle, 1996).
The prevalence of these experiences among people who abuse substances represents a pressing concern for the treatment of co-occurring disorders. Indeed, people who have experienced IPV and/or SA are more likely to report a wide range of psychopathology, including posttraumatic stress disorder (PTSD), than those without these experiences (see Dworkin, Menon, Bystrynski, & Allen, 2016 and Weaver & Clum, 1995 for reviews). PTSD in particular is much more common in people with substance use disorders than in people without substance use disorders (Mills, Teesson, Ross, & Peters, 2006). Indeed, PTSD appears to have a mutually maintaining relationship with substance use disorders (Kaysen et al., 2011) and is associated with greater symptom severity (Brady, Killeen, Saladin, Dansky, & Becker, 1994) as well as poorer treatment prognosis (Ouimette, Brown, & Najavits, 1998). Thus, it is critically important to understand the role of various types of trauma histories in the clinical presentations of patients seeking treatment for substance use disorders.
Some initial work suggests that SA and IPV may contribute to PTSD over and above other forms of trauma. A recent meta-analysis examining the relationship between SA and multiple forms of psychopathology, including PTSD, found that SA, specifically, is more strongly associated with psychopathology than other forms of trauma, including physical assault (Dworkin et al., 2016). Nationally representative studies assessing a broad range of potential traumas have revealed similar results. For example, Pietrzak, Goldstein, Southwick, and Grant (2011) found that individuals who endorsed SA or physical IPV as their worst traumatic event were at a greater likelihood of having partial and full PTSD than people who had experienced other traumas. Similarly, in a sample of 21,425 European adults, Darves-Bornoz and colleagues demonstrated that criterion-A SA and physical IPV were among the trauma types that contributed the most to the development of PTSD (Darves-Bornoz et al., 2008). However, neither of these studies determined whether these relationships are present among people with co-occurring substance use disorders, compared SA and IPV to each other, or explored the cumulative impact of these experiences. Better understanding how the nature of trauma experiences produces PTSD among people with substance use disorders would provide useful information for theory development as well as assessment and treatment.
The increased risk for PTSD among survivors of SA and/or IPV might be due to their common characteristics. First, SA and IPV are often experienced multiple times in the lifespan (Matlow & DePrince, 2012) and commonly co-occur with other forms of trauma, including natural disasters and child abuse (Breslau, Chilcoat, Kessler, & Davis, 1999; Rees et al., 2001; Schumacher et al., 2010). Experiencing multiple traumas increases risk for post-trauma psychopathology (Green et al., 2000); indeed, a study in a college sample found that physical, sexual, and psychological violence within romantic relationships were not predictive of PTSD symptoms after taking broader trauma history into account (Avant, Swopes, Davis, & Elhai, 2011). Second, both SA and IPV are directly experienced by a victim, which is associated with increased symptoms of PTSD as compared to indirectly experienced traumas (e.g., learning about the sudden violent death of a loved one) (Anders, Frazier & Frankfurt, 2009; Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993). Third, both SA and IPV are intentionally caused, which is associated with worse PTSD outcomes as compared to unintentional traumas (e.g., natural disaster) (Frazier et al., 2009; Zatzick et al., 2007). Finally, unlike other forms of interpersonal trauma like non-intimate physical assault, SA and IPV are associated with consequences which could further increase risk for psychopathology, including guilt and self-blame (Amstadter & Vernon, 2008), alienation from social networks (Lanier & Maume, 2009), and significant resource loss (Beeble, Bybee & Sullivan, 2010). Their unique role in the development of PTSD is thus important to consider above and beyond the impact of non-interpersonal traumas and non-intimate physical assault.
SA and IPV also have different characteristics that might afford unique liability for PTSD relative to the other. First, SA can occur during childhood, adolescence, or adulthood, while IPV typically occurs during adolescence or adulthood, so the opportunity for early onset revictimization across life stages in SA may increase the risk of PTSD (Walsh et al., 2012). Second, while SA is most commonly committed by someone known to the victim, IPV is, by definition, committed by a known perpetrator, which may alter the psychological impact of trauma. For example, in a representative sample, Forbes and colleagues (2014) found that violence by an intimate perpetrator (including caregivers and romantic partners) was linked to greater PTSD symptom severity relative to both interpersonal traumatic events by non-intimates and to non-interpersonal event exposure. However, a recent meta-analysis of the psychological impact of SA suggested that stranger-perpetrated SA may be associated with greater symptom severity than SA perpetrated by a known assailant (Dworkin et al., 2016). Experiencing traumas committed by different perpetrators (as in SA revictimization) is associated with the passive avoidance and arousal symptoms of PTSD (Matlow & DePrince, 2012). Third, while both SA and IPV are associated with repeat trauma exposure, IPV is more likely to be chronic (i.e., occurring repeatedly over time), while SA is often acute (i.e., occurring unexpectedly).
One avenue to understand the unique impact of SA and IPV on PTSD among people with substance use disorders is through their differential association with PTSD symptom clusters. Indeed, there is reason to believe that PTSD cluster scores differ based on characteristics of traumas experienced. A large community study of adult trauma survivors found that people reporting distressing combat and sexual traumas evidenced higher hyperarousal and avoidance symptoms than people who reported other distressing traumas groups, including physical assault by any perpetrator (Ullman, 1995). Two studies of undergraduate students identified significantly higher symptoms across all three clusters among women reporting SA as compared to women who had experienced a major accident (Kelley et al., 2009; Lancaster, Melka, Rodriguez, & Bryant, 2014) or the sudden unexpected death of a loved one (Lancaster et al., 2014, cf. Kelley et al., 2009), but these studies did not include participants reporting IPV. One study examined the effect of chronic victimization (i.e., multiple victimization by the same perpetrator, as is more common in IPV) versus revictimization (i.e., multiple victimization by different perpetrators, as is more common in SA) on PTSD symptom clusters, and found that revictimization was associated with passive avoidance and emotional numbing, while chronic victimization was associated with active avoidance (Matlow & DePrince, 2012). While these studies provide initial evidence that different types of trauma experiences are associated with different PTSD symptom profiles, these studies have been limited by their characterization of participants as having experienced only one type of trauma, and a lack of examination of IPV as a unique form of trauma. Understanding the impact of different combinations of trauma types on PTSD symptom clusters, including both SA and IPV, could help to explain the relative impact of these different forms of trauma in a manner that reflects the fact that multiple experiences of trauma are common in the lives of people who abuse substances.
Taken together, the findings of these studies suggest that both SA and IPV could have an additive, deleterious impact on PTSD above and beyond other potentially traumatic life experiences among people who abuse substances, and this impact could differ across PTSD symptom clusters. However, little research has examined the unique association of SA and/or IPV with PTSD symptom clusters, despite calls for more research in this area (Basile et al., 2004), and no research to date has examined these associations within a substance abusing population. In addition, there are several major limitations to this literature. First, although some studies examining associations between IPV and mental disorders have adjusted for some previous trauma exposure (e.g., childhood adversity), they have often not taken a comprehensive range of traumatic events into account. Second, most of these studies have either combined experiences of SA and IPV into interpersonal trauma, or examined either SA or IPV individually while including people who experienced the other form of trauma in their comparison group. This precludes comparisons of the unique impact of SA and IPV as well as the additive impact of combined SA-IPV. Third, few studies have examined the impact of different types of trauma on PTSD symptom clusters. Understanding the unique and additive contributions of SA and IPV to PTSD symptom clusters has the potential to inform both assessment and treatment when people with trauma histories present for treatment as well as support the advancement of theories on the development of PTSD after different forms of trauma. Thus, the current study examined whether IPV alone, SA alone, or combined SA-IPV experiences are associated with symptom severity within PTSD symptom clusters above and beyond the impact of exposure to other traumatic events in a sample of people in residential treatment for substance use disorders. We operationalized IPV as any intimate-partner perpetrator assault, rather than limiting it to physical assault only, to better parse whether the perpetrator or type of violence might be accounting for differences in PTSD. Because of the lack of research on the relative contribution of SA and IPV to PTSD symptom clusters, we chose to approach these analyses in an exploratory manner, rather than making a priori hypotheses.
Method
Participants
Participants were 219 individuals (48.86% women, 51.14% men) who were part of a larger IRB-approved study investigating the effectiveness of an exposure-based intervention for PTSD among people seeking treatment at a residential substance abuse treatment facility. While the larger research project was longitudinal, this study only used data from the initial assessment. All participants in the broader study exceeded the 44-point cut-off score for probable PTSD on the PTSD Checklist-Civilian version (PCL-C; Weathers, Litz, Herman, Huska, & Keane, 1993) and the 8-point cut-off for a probable alcohol problem on the Alcohol Use Disorders Identification Test (Babor, de la Fuente, Saunders, & Grant, 1992). For the purposes of this analysis, participants who reported no lifetime criterion-A events (n = 4) and people who did not complete the clinical interview assessing PTSD (n = 2) were excluded from the original sample of N = 225. The final sample had a mean age of 33.49 (SD = 10.31), with a mean annual household income of $32,585 (SD = $35,173, median = $22,000). Most (78.08%) of the sample was White/Caucasian, with a significant minority reporting that their race was Black/African American (20.09%).
Screening Measures
The following measures were administered as brief screening measures to select participants for the study; data from these measures was not retained.
PTSD Checklist-Civilian version (PCL-C; Weathers et al., 1993)
The PCL-C is a highly reliable and valid 17-item self-report measure of DSM-IV PTSD (Wilkins, Lang, & Norman, 2011). We used a cut-off score of 44.
Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 1992)
The AUDIT is a 10-item self-report measure that is commonly used as a screening tool for alcohol problems and was used to screen participants with a score of 8 or above for the current study. It has strong reliability and validity among problem drinkers (Hays, Merz, & Nicholas, 1995).
Research Measures
After obtaining informed consent from participants screening into the study using the previously-described measures, interviewers administered structured and semi-structured clinical interviews and questionnaires to participants in person.
National Women’s Study PTSD Module (NWS-PTSD: Kilpatrick, Resnick, Saunders, & Best, 1989; Resnick, 1996)
The NWS is a structured clinical interview designed to assess lifetime trauma exposure including, among other events, childhood abuse, SA, IPV, and natural disasters. This a modified version of the NWS-PTSD developed by Dansky and colleagues (Dansky, Bryne, & Brady, 1999) to specifically probe a variety of types of interpersonal events: (a) physical attacks using a weapon, (b) physical attacks with intent of causing death or serious injury that did not involve use of a weapon, (c) physical attacks without intent of causing death or serious injury such as hitting, pushing, shoving, kicking, or punching, and (d) sexual violence. For interpersonal events, respondents identified the perpetrator type. Exposure to IPV was defined as an endorsement of completed sexual or physical assault (i.e., types a, b, c, and d of the interpersonal events mentioned previously) where the identified perpetrator was an intimate partner. Exposure to SA was defined as an endorsement of completed vaginal, oral, or anal intercourse, achieved by force or threat of harm, by any perpetrator at any time during the participant’s life.
Clinician Administered PTSD Scale (CAPS; Blake et al., 1995)
Symptom severity (combined frequency and intensity) of PTSD and its symptom clusters were assessed with the CAPS according to DSM-IV criteria. The CAPS is a semi-structured, diagnostic interview and is the benchmark instrument for diagnosing PTSD. It has been demonstrated to have strong reliability and high concurrent validity (Weathers, Keane, & Davidson, 2001). In the current sample, internal consistency reliability was α = 0.88. In addition, 92.23% of participants were given a PTSD diagnosis as assessed by the CAPS, indicating its concurrent validity with the PCL-C. We used continuous variables demonstrating symptom severity of individual PTSD symptom clusters as dependent variables.
Results
See Table 1 for the frequency with which participants experienced SA and IPV. On the NWS-PTSD scale, 65.30% of participants reported experiencing lifetime IPV (referred to as the IPV+ group), while 68.04% reported experiencing lifetime SA (referred to as the SA+ group). Approximately half of the sample (48.86%) had experienced both SA and IPV. Because the SA category addresses trauma type while the IPV category reflects perpetrator type, we explored the extent to which membership in both the SA+ and IPV+ categories reflected characteristics of the same event (i.e., an IPV SA) versus different events (i.e., an IPV physical assault and a non-IPV SA). Of the 143 people who experienced IPV, 25.17% (n = 36) endorsed sexual IPV; however, 31 out of 36 of these individuals reported that they had also experienced SA perpetrated by a non-intimate partner. Thus, in general, membership in the SA+/IPV+ group represents experiencing separate IPV and SA events, although SA was common within the IPV group.
Table 1.
Frequency of Exposure to SA and IPV
| Exposure to SA | |||
|---|---|---|---|
| SA− | SA+ | ||
|
|
|||
| Overall: n = 34/219 (15.53%) | Overall: n = 42/219 (19.18%) | ||
| IPV− | Women: n = 11/107 (10.28%) | Women: n = 4/107 (3.74%) | |
| Men: n = 23/112 (20.54%) | Men: n = 38/112 (33.93%) | ||
| Exposure to IPV | |||
| Overall: n = 36/219 (16.44%) | Overall: n = 107/219 (48.86%) | ||
| IPV+ | Women: n = 18/107 (16.82%) | Women: n = 74/107 (69.16%) | |
| Men: n = 18/112 (16.07%) | Men: n = 33/112 (29.46%) | ||
SA= Sexual assault; IPV = Intimate-partner-perpetrated violence
The mean number of traumas in the sample was 9.34 (SD = 5.38), and included physical assault perpetrated by a nonintimate (42.47%), serious accident (53.42%), natural disaster (33.79%), childhood physical abuse (36.99%), witnessing someone else being seriously hurt or killed (60.27%), or learning that a family member or close friend had been killed in a car accident or through deliberate means (35.16%). All continuous variables (i.e., number of criterion A events, total CAPS score, PTSD symptom cluster scores) were significantly correlated with each other at p < .01 (see Table 2). We conducted bivariate difference tests to assess differences in study variables by history of SA and IPV (see Table 3). People with a history of SA had significantly more criterion-A events than those who did not; the same was true for people with a history of IPV. With regard to symptoms of PTSD, people with a history of SA had significantly higher scores on the re-experiencing, avoidance, and hyperarousal clusters. In contrast, people with a history of IPV had significantly higher scores on the re-experiencing cluster but not the avoidance or hyperarousal clusters.
Table 2.
Descriptive Statistics and Intercorrelations for Study Variables
| Correlations | ||||||
|---|---|---|---|---|---|---|
|
|
||||||
| M (SD) | Range | 1 | 2 | 3 | 4 | |
| 1. Number of criterion A events | 9.34 (5.38) | 1-29 | -- | |||
| 2. Total CAPS score | 72.09 (20.93) | 15-114 | .39** | -- | ||
| 3. CAPS reexperiencing | 19.49 (8.73) | 0-36 | .38** | .77** | -- | |
| 4. CAPS avoidance | 29.57 (9.93) | 0-36 | .23** | .83** | .48** | -- |
| 5. CAPS hyperarousal | 22.53 (7.76) | 0-51 | .32** | .76** | .42** | .56** |
SA= Sexual assault; IPV = Intimate-partner-perpetrated violence
p < .01
Table 3.
Bivariate Differences on Study Variables by Trauma Type
| History of sexual assault? | History of intimate partner-perpetrated violence? | |||||||
|---|---|---|---|---|---|---|---|---|
| No (n = 70) |
Yes (n = 149) |
Bivariate difference |
Effect size |
No (n = 76) |
Yes (n = 143) |
Bivariate difference |
Effect size |
|
| Number of criterion A events |
M = 7.44; SD = 4.91 |
M = 10.23; SD = 5.37 |
U = 3555.00** |
d = 0.53 |
M = 7.17; SD = 4.17 |
M = 10.49; SD = 5.60 |
U = 3485.50** |
d = 0.64 |
| Total CAPS score |
M = 62.13; SD = 19.01 |
M = 76.77; SD = 20.19 |
U = 3088.00** |
d = 0.74 |
M = 66.66; SD = 19.11 |
M = 74.97; SD = 21.34 |
U = 4106.00** |
d = 0.40 |
| CAPS reexperiencing |
M = 16.30; SD = 9.16 |
M = 20.99; SD = 8.13 |
U = 3698.50** |
d = 0.55 |
M = 16.43; SD = 8.09 |
M = 21.11; SD = 8.65 |
U = 3810.00** |
d = 0.55 |
| CAPS avoidance |
M = 25.20; SD = 9.40 |
M = 31.62; SD = 9.52 |
U = 3209.00** |
d = 0.68 |
M = 27.97; SD = 9.57 |
M = 30.42; SD = 10.04 |
U = 4670.50 |
d = 0.25 |
| CAPS hyperarousal |
M = 19.61; SD = 8.48 |
M = 23.89; SD = 7.03 |
U = 3712.00** |
d = 0.57 |
M = 21.24; SD = 7.96 |
M = 23.21; SD = 7.59 |
U = 4669.50 |
d = 0.26 |
SA= Sexual assault; IPV = Intimate-partner-perpetrated violence
p < .01
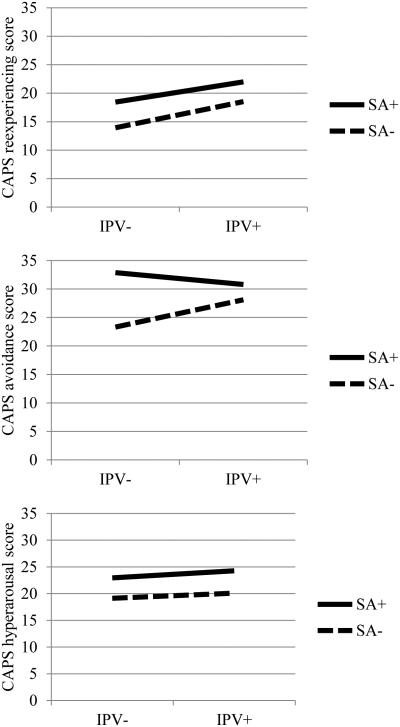
In order to test whether PTSD symptom cluster scores varied by history of SA and/or IPV, we conducted a 2 (SA history) × 2 (IPV history) MANCOVA, controlling for number of criterion A trauma events (see Table 4). Results for Model 1 included a significant omnibus main effect for history of SA, but not history of IPV, which led us to examine between-subjects effects for history of SA in more detail. These results revealed that survivors of SA reported significantly higher symptoms in the re-experiencing, avoidance, and hyperarousal clusters as compared to people without a history of SA. The omnibus interaction effect for SA × IPV was also significant. Examining the moderated between-subjects effects for history of SA × IPV revealed significant differences for avoidance, but not re-experiencing or hyperarousal. On examination of the plots of this moderation (Figure 1) and the confidence intervals of the marginal means, avoidance scores were not significantly different in IPV survivors as a function of SA history. However, for trauma survivors without an IPV history, avoidance scores were significantly higher if they also had a history of SA, M = 32.91, SE = 1.44, 95% CI: 30.07, 35.75, compared to those who did not, M = 23.38, SE = 1.64, 95% CI: 20.14, 26.61.
Table 4.
Multivariate Analysis of Covariance of Differences in PTSD Symptom Clusters by Trauma History
| Overall Model | Reexperiencing | Avoidance | Hyperarousal | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Wilks’ lambda |
F | Effect size (η2p) |
F | Effect size (η2p) |
F | Effect size (η2p) |
F | Effect size (η2p) |
|
| Model 1 | |||||||||
| Intercept | .29 | 170.87*** | .71 | 168.12*** | .44 | 417.80*** | .66 | 338.09*** | .61 |
| Main effects | |||||||||
| Number of criterion A events | .88 | 9.48*** | .12 | 21.30*** | .09 | 6.11* | .03 | 15.93*** | .07 |
| IPV | .98 | 1.75 | .02 | 4.70* | .02 | 0.77 | .00 | 0.00 | .00 |
| SA | .92 | 6.41** | .08 | 5.79* | .03 | 18.49*** | .08 | 8.06** | .04 |
| Interaction effects | |||||||||
| IPV × SA | .96 | 2.81* | .04 | 0.30 | .00 | 6.03* | .03 | 0.01 | .00 |
| Model 2 | |||||||||
| Intercept | .32 | 145.18*** | .68 | 134.48*** | .39 | 360.33*** | .63 | 281.11*** | .57 |
| Main effects | |||||||||
| Gender | .99 | 0.82 | .01 | 0.00 | .00 | 0.79 | .00 | 0.45 | .00 |
| Number of criterion A events | .87 | 10.16*** | .13 | 22.18*** | .10 | 7.82** | .04 | 18.27*** | .08 |
| IPV | .98 | 1.31 | .02 | 3.84 | .02 | 0.22 | .00 | 0.17 | .00 |
| SA | .92 | 5.68** | .08 | 2.78 | .01 | 15.93*** | .07 | 8.86** | .04 |
| Interaction effects | |||||||||
| IPV × SA | .97 | 1.93 | .03 | 0.00 | .00 | 4.38* | .02 | 0.07 | .00 |
| IPV × gender | .99 | 0.78 | .01 | 0.00 | .00 | 0.09 | .00 | 1.32 | .01 |
| SA × gender | .99 | 0.84 | .01 | 1.35 | .01 | 1.34 | .01 | 0.00 | .00 |
| IPV × SA × gender | .96 | 2.62 | .04 | 0.00 | .00 | 3.38 | .02 | 6.32* | .03 |
SA= Sexual assault; IPV = Intimate-partner-perpetrated violence
p < .001
p < .01
p < .05
η2p = Partial eta squared
Figure 1. Interactions of SA with IPV in the Multivariate Model.
SA+ = Sexual assault; SA− = No sexual assult; IPV+ = Intimate-partner-perpetrated violence; IPV− = No intimate-partner-perpetrated violence.
PTSD symptom values for each combination of SA/IPV reflect marginal means within the multivariate MANCOVA and control for number of criterion A traumas.
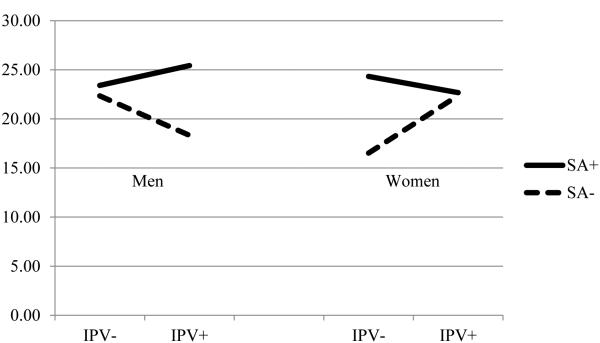
Since our sample was comprised of near-equal proportions of men and women and there is no literature to date that has tested gender differences in the relative association of trauma experiences with PTSD symptom clusters, we conducted a follow-up analysis involving the addition of main and interaction effects for gender to determine whether the effects identified in Model 1 significantly differed by gender. See Table 1 for the frequency of IPV/SA experiences in men and women. Notably, there were only four women in the IPV−/SA+ group. In MANOVA, there must be more dependent variables than participants for each cell (Tabachnick & Fidell, 1996) so that cells do not become singular. Having only one more participant than dependent variable in the IPV−/SA+ cell means that there is a potential violation of the assumption of homogeneity of covariance matrices, but results from Levene’s test suggest that no such violation occurred. This small cell size also raises concerns about Type I error. Results for Model 2 indicated no main effect for gender, and were otherwise largely similar to Model 1 in terms of main effects, although the 2-way interaction for IPV × SA was no longer significant (Table 4). A trend towards significance was identified for the omnibus three-way SA × IPV × gender interaction (Figure 2). Examination of this trend indicated that an experience of SA was associated with statistically significantly increased hyperarousal scores for IPV+ men, M = 25.44, SE = 1.25, 95% CI: 22.97, 27.91, as compared to IPV+ men without a history of SA, M = 18.32, SE = 1.69, 95% CI: 14.99, 21.66. In contrast, a history of SA was not associated with significant differences in hyperarousal for either IPV+ or IPV− women.
Figure 2. SA × IPV × Gender Interaction for Hyperarousal.
SA+ = Sexual assault; SA− = No sexual assult; IPV+ = Intimate-partner-perpetrated violence; IPV− = No intimate-partner-perpetrated violence.
PTSD symptom values for each combination of SA/IPV reflect marginal means within the multivariate MANCOVA and control for number of criterion A traumas.
Discussion
This study examined the relative contribution of SA and IPV to PTSD symptom clusters in a traumatized, substance-abusing, mixed-gender sample. In general, experiencing SA was associated with higher symptomatology across symptom clusters, while experiencing IPV was not. This is consistent with past research indicating that SA is a uniquely deleterious form of trauma in non-treatment-seeking populations (Dworkin et al., 2016; Frazier et al., 2009; Kessler et al., 1995) that evidences increased symptoms across clusters (Kelley et al., 2009; Lancaster et al., 2014; Ullman, 1995), while the effect of IPV on psychopathology might depend on abuse type (e.g., psychological, physical, sexual) (Pico-Alfonso et al., 2006; Street & Arias, 2001; cf. Basile et al., 2004) or chronicity (Matlow & DePrince, 2012), or might be better accounted for by the multiple experiences of trauma in the lives of people experiencing IPV (Avant et al., 2011). Indeed, SA is more likely to have a number of characteristics that increase risk for PTSD, including the possibility of a stranger perpetrator (Dworkin et al., 2016), the greater likelihood of acute traumas with revictimization across the lifespan rather than chronic, repeated traumas with a single perpetrator (Walsh et al., 2012), and the potential for earlier onset of trauma (McCutcheon et al., 2010). Regardless, these findings should not be taken as evidence of the lack of impact of IPV on survivors, but of the similarity in psychological consequences between IPV and non-IPV traumas in substance abusing populations. It is also important to note that IPV has been associated with numerous non-PTSD-related psychological outcomes, including depression, anxiety, substance abuse, and suicidality (Coker et al., 2002; Pico-Alfonso et al., 2006) as well as social, economic, and health consequences (Beeble et al., 2010; Coker et al., 2002) not examined here.
It appears that, among treatment-seeking people with problem substance use, combinations of SA and IPV histories differ in terms of their association with PTSD symptom clusters. Moderation analyses revealed that avoidance symptoms differed as a function of whether survivors had experienced SA and/or IPV. Among people who had not experienced IPV, people who also had a history of SA had higher avoidance symptoms as compared to people who did not. However, this difference by SA status was not present for people who had experienced IPV, who reported moderate levels of avoidance relative to the other trauma groups regardless of SA status. One potential explanation for this finding is that people who have experienced IPV may be more avoidant of internal triggers (e.g., thoughts and emotions related to the trauma)—for example, through the use of substances—but less avoidant of external triggers (e.g., people, places, and situations related to the trauma) in order to maintain a relationship with a perpetrator (Waldrop & Resick, 2004). In contrast, sexual victimization might be associated with increased avoidance of both internal and external triggers. The group that experienced neither IPV nor SA would thus be expected to have the lowest avoidance, the group that experienced IPV but not SA would be expected to have higher internal but not external avoidance, and both the group that experienced IPV and SA and the group that experienced SA only would be expected to have higher internal and external avoidance (and thus, the highest overall avoidance). While we did not test differences in external versus internal avoidance, the magnitude of avoidance scores identified in this study is generally consistent with this pattern.
Our exploratory follow-up analysis found that men and women evidence similar relationships with regard to the association between trauma history and symptom severity across PTSD clusters. Although these findings appear to be different than those of Lancaster and colleagues (2014), who found significant differences in the association between trauma type and PTSD symptom profile for undergraduate women but not undergraduate men, Lancaster and colleagues did not statistically compare men and women in terms of their association between trauma type and PTSD symptom profile, and they had a small sample of men who had experienced SA. The current findings might also be specific to people seeking treatment for problem substance use. However, there was one exception to this lack of a gender difference in the current study: an experience of SA was associated with increased hyperarousal scores for IPV+ men only. While this finding must be interpreted with caution, since the significance of the omnibus test was at trend level, the small sample size (and, correspondingly, low power to detect effects) for these analyses suggests that these findings might be worth consideration. Since SA and IPV are generally narrated as being perpetrated by men against women, men who have experienced both traumas might develop expanded schemas regarding the likelihood and source of violence being perpetrated against them, leading to symptoms in the hyperarousal cluster including hypervigilance and difficulty concentrating. Women, on the other hand, might see SA and IPV as potential threats to their safety as women and may not be as likely as men to overaccommodate their worldview in response. These findings require replication in future research, which should use larger sample sizes and explore the potential mechanisms of these effects.
These findings have several clinical implications. First, providers offering substance use and PTSD services should consistently screen for SA history, as these patients are likely to be experiencing particularly severe symptoms of PTSD. Understanding the unique presentations of their symptom clusters and how they interact with substance use could inform treatment planning. For example, it is possible that symptoms of avoidance are particularly likely to be present for treatment-seeking survivors of SA (and, to a lesser extent, people who have experienced both SA and IPV), so practitioners may want to probe whether trauma reminders are a trigger for substance use as an avoidance strategy. Second, it is important for settings that are focused on serving survivors of SA (e.g., rape crisis centers) to ensure that they have resources available to meet the unique needs of their population. For example, since men with SA and IPV histories evidenced high symptoms of hyperarousal, settings should ensure that their outreach efforts are reaching men in need of services, identify referrals to therapists that offer services targeted towards hyperarousal symptoms (e.g., cognitive behavioral therapy for insomnia), or train their in-house clinicians in this modality.
This study had a number of limitations that should be addressed in future research. First, we did not test the chronicity of traumas or the co-occurrence of SA and IPV with other traumas in relation to PTSD symptom clusters, which we posit may be related to the differential effects of SA and IPV. Future research could assess the chronicity of a recent focal event in relation to a prospective assessment of PTSD symptoms. Second, we used a DSM-IV-TR conceptualization of PTSD symptom clusters, which has changed in DSM-5 to include a greater emphasis on cognitive symptoms. Research is needed to clarify whether these findings apply to this altered conceptualization of symptom clusters. Third, relatively small effect sizes were identified, particularly when examining sex differences, which suggests that additional research is needed to account for variance in symptom presentation across clusters. Finally, while selecting a traumatized substance-abusing population helped provide evidence that could inform future research on interactions between substance use and various symptom clusters as a function of trauma history, additional research is needed to determine whether these findings hold in populations that have not been selected for PTSD or substance use disorders.
In conclusion, among people with trauma histories in a substance use facility, SA was associated with higher PTSD symptomatology across symptom clusters when controlling for number of past traumas, while IPV was not. Additive experiences of SA appear to be associated with increased avoidance symptoms among trauma survivors without an IPV history, while additive experiences of SA do not appear to have the same association for survivors of IPV.
Acknowledgments
This research was supported in part by grants from the National Institute on Alcohol Abuse and Alcoholism (R01AA016816, PI: S. Coffey; T32AA007455-33, PI: M. Larimer) and the National Institute on Minority Health and Health Disparities (K99MD010468, PI: C. Vinci)
References
- Amstadter AB, Vernon LL. Emotional reactions during and after trauma: A comparison of trauma types. Journal of Aggression, Maltreatment, & Trauma. 2008;16(4):391–408. doi: 10.1080/10926770801926492. doi:10.1080/10926770801926492.Emotional. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anders SL, Frazier PA, Frankfurt SB. Variations in Criterion A and PTSD rates in a community sample of women. Journal of Anxiety Disorders. 2011;25(2):176–184. doi: 10.1016/j.janxdis.2010.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avant EM, Swopes RM, Davis JL, Elhai JD. Psychological abuse and posttraumatic stress symptoms in college students. Journal of Interpersonal Violence. 2011;26:3080–3097. doi: 10.1177/0886260510390954. [DOI] [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, Grant M. The Alcohol Use Disorders Identification Test. Guidelines for use in primary health care. World Health Organization; Geneva, Switzerland: 1992. [Google Scholar]
- Basile KC, Arias I, Desai S, Thompson MP. The differential association of intimate partner physical, sexual, psychological, and stalking violence and posttraumatic stress symptoms in a nationally representative sample of women. Journal of Traumatic Stress. 2004;17(5):413–421. doi: 10.1023/B:JOTS.0000048954.50232.d8. [DOI] [PubMed] [Google Scholar]
- Beeble ML, Bybee D, Sullivan CM. The impact of resource constraints on the psychological well-being of survivors of intimate partner violence over time. Journal of Community Psychology. 2010;38(8):943–959. doi:10.1002/jcop. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 2006;8(1):75–90. doi: 10.1007/BF02105408. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Brady KT, Killeen T, Dansky B, Becker S. Comorbid substance abuse and PTSD: Characteristics of women in treatment. The American Journal on Addictions. 1994;3:160–164. [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: Results from the Detroit Area Survey of Trauma. The American Journal of Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, Smith PH. Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine. 2002;23(4):260–268. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- Dansky BS, Bryne CA, Brady KT. Intimate violence and post-traumatic stress disorder among individuals with cocaine dependence. American Journal of Drug and Alcohol Abuse. 1999;25:257–268. doi: 10.1081/ada-100101859. [DOI] [PubMed] [Google Scholar]
- Darves-Bornoz J-M, Alonso J, de Girolamo G, de Graaf R, Haro J-M, Kovess-Masfety V-K, et al. Main traumatic events in Europe: PTSD in the European Study of the Epidemiology of Mental Disorders Survey. Journal of Traumatic Stress. 2008;21(5):455–462. doi: 10.1002/jts.20357. [DOI] [PubMed] [Google Scholar]
- Dworkin ER, Menon S, Bystrynski J, Allen NE. Associations between sexual assault and psychopathology: A meta-analysis. 2016 Manuscript in preparation. [Google Scholar]
- Follette VM, Polusny MA, Bechtle AE, Naugle AE. Cumulative trauma: The impact of child sexual abuse, adult sexual assault, and spouse abuse. Journal of Traumatic Stress. 1996;9(1):25–35. doi: 10.1007/BF02116831. doi:10.1016/S0140-6736(01)05622-7. [DOI] [PubMed] [Google Scholar]
- Forbes D, Parslow R, Creamer M, Allen N, McHugh T, Hopwood M. Mechanisms of anger and treatment outcome in combat veterans with posttraumatic stress disorder. Journal of Traumatic Stress. 2008;21(2):142–149. doi: 10.1002/jts.20315. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Anders S, Perera S, Tomich P, Tennen H, Park C, Tashiro T. Traumatic events among undergraduate students: Prevalence and associated symptoms. Journal of Counseling Psychology. 2009;56(3):450–460. doi:10.1037/a0016412. [Google Scholar]
- Green BL, Goodman LA, Krupnick JL, Corcoran CB, Petty RM, Stockton P, Stern NM. Outcomes of single versus multiple trauma exposure in a screening sample. Journal of Traumatic Stress. 2000;13(2):271–286. doi: 10.1023/A:1007758711939. doi:10.1023/A:1007758711939. [DOI] [PubMed] [Google Scholar]
- Grice DE, Brady KT, Dustan LR, Malcolm R, Kilpatrick DG. Sexual and physical assault history and posttraumatic stress disorder in substance-dependent Individuals. The American Journal on Addictions. 1995;4:297–305. [Google Scholar]
- Kaysen D, Atkins DC, Moore SA, Lindgren KP, Dillworth T, Simpson T. Alcohol use, problems, and the course of posttraumatic stress disorder: A prospective study of female crime victims. Journal of Dual Diagnosis. 2011;7(4):262–279. doi: 10.1080/15504263.2011.620449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley LP, Weathers FW, McDevitt-Murphy ME, Eakin DE, Flood AM. A comparison of PTSD symptom patterns in three types of civilian trauma. Journal of Traumatic Stress. 2009;22(3):227–235. doi: 10.1002/jts.20406. doi:10.1002/jts. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, Sonnega A, Nelson CB. Posttraumatic stress disorder in the National Comorbity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Saunders BE, Best CL. The National Women's Study PTSD module. National Crime Victims Research and Treatment Center, Medical University of South Carolina; Charleston, SC: 1989. [Google Scholar]
- Klostermann KC, Fals-Stewart W. Intimate partner violence and alcohol use: Exploring the role of drinking in partner violence and its implications for intervention. Aggression and Violent Behavior. 2006;11:587–597. doi:10.1016/j.avb.2005.08.008. [Google Scholar]
- Lancaster SL, Melka SE, Rodriguez BF, Bryant AR. PTSD symptom patterns following traumatic and nontraumatic events. Journal of Aggression, Maltreatment & Trauma. 2014;23:414–429. [Google Scholar]
- Lanier C, Maume MO. Intimate partner violence and social isolation across the rural/urban divide. Violence Against Women. 2009;15(11):1311–1330. doi: 10.1177/1077801209346711. [DOI] [PubMed] [Google Scholar]
- Matlow RB, DePrince AP. The influence of victimization history on PTSD symptom expression in women exposed to intimate partner violence. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;5(3):241–250. doi:10.1037/a0027655. [Google Scholar]
- McCutcheon VV, Sartor CE, Pommer NE, Bucholz KK, Nelson EC, Madden PAF, Heath AC. Age at trauma exposure and PTSD risk in young adult women. Journal of Traumatic Stress. 2010;23(6):811–814. doi: 10.1002/jts.20577. doi: http://dx.doi.org/10.1002/jts.20577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, Peters L. Trauma, PTSD, and substance use disorders: Findings from the Australian National Survey of Mental Health and Well-Being. American Journal of Psychiatry. 2006;163:651–658. doi: 10.1176/ajp.2006.163.4.652. doi:10.1176/appi.ajp.163.4.652. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Brown PJ, Najavits LM. Course and treatment of patients with both substance use and posttraumatic stress disorders. Addictive Behaviors. 1998;23(6):785–795. doi: 10.1016/s0306-4603(98)00064-1. [DOI] [PubMed] [Google Scholar]
- Pico-Alfonso MA, Garcia-Linares MI, Celda-Navarro N, Blasco-Ros C, Echeburúa E, Martinez M. The impact of physical, psychological, and sexual intimate male partner violence on women’s mental health: Depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. Journal of Women’s Health. 2006;15(5):599–611. doi: 10.1089/jwh.2006.15.599. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders. 2011;25:456–465. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees S, Silove D, Chey T, Ivancic L, Steel Z, Creamer M, et al. Lifetime prevalence of gender-based violence in women and the relationship with mental disorders and psychosocial function. Journal of the American Medical Association. 2011;306:513–521. doi: 10.1001/jama.2011.1098. [DOI] [PubMed] [Google Scholar]
- Resnick H. Psychometric review of National Women’s Study (NWS) event history—PTSD module. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Sidran; Lutherville, MD: 1996. pp. 214–217. [Google Scholar]
- Resnick H, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61(6):984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Schumacher JA, Coffey SF, Norris F, Tracy M, Clements K, Galea S. Intimate partner violence and Hurricane Katrina: Predictors and associated mental health outcomes. Violence and Victims. 2010;25:588–603. doi: 10.1891/0886-6708.25.5.588. PMCID: PMC3394178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street AE, Arias I. Psychological abuse and posttraumatic stress disorder in battered women: Examining the roles of shame and guilt. Violence and Victims. 2001;16:65–78. [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 3rd HarperCollins; New York: 1996. [Google Scholar]
- Tjaden P, Thoennes N. Prevalence and consequences of male-to-female and female-to-male intimate partner violence as measured by the National Violence Against Women Survey. Violence Against Women. 2000;6(2):142–161. doi:10.1177/10778010022181769. [Google Scholar]
- Tjaden P, Thoennes N. Extent, nature, and consequences of rape victimization: Findings from the National Violence Against Women Survey. Washington, D. C.: 2006. [Google Scholar]
- Ullman SE. Adult trauma survivors and post-traumatic stress sequelae: An analysis of reexperiencing, avoidance, and arousal criteria. Journal of Traumatic Stress. 1995;8:179–188. doi: 10.1007/BF02105416. [DOI] [PubMed] [Google Scholar]
- Waldrop AE, Resick PA. Coping among adult female victims of domestic violence. Journal of Family Violence. 2004;19(5):291–302. [Google Scholar]
- Walsh K, Danielson CK, McCauley JL, Saunders BE, Kilpatrick DG, Resnick HS. National prevalence of posttraumatic stress disorder among sexually revictimized adolescent, college, and adult household-residing women. Archives of General Psychiatry. 2012;69(9):935–942. doi: 10.1001/archgenpsychiatry.2012.132. doi:10.1001/archgenpsychiatry.2012.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT. Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13(3):132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist(PCL): Reliability, validity, and diagnostic utility; Paper presented at the Annual Meeting of International Society for Traumatic Stress Studies; San Antonio, TX. Oct, 1993. [Google Scholar]
- Weaver TL, Clum GA. Psychological distress associated with interpersonal violence: A meta-analysis. Clinical Psychology Review. 1995;15(2):115–140. [Google Scholar]
- Zatzick DF, Rivara FP, Nathens AB, Jurkovich GJ, Wang J, Fan M-Y, Mackenzie EJ. A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychological Medicine. 2007;37:1469–1480. doi: 10.1017/S0033291707000943. [DOI] [PubMed] [Google Scholar]