Abstract
OBJECTIVE
To examine whether activity limitation stages were associated with patient-reported trouble getting needed health care among Medicare beneficiaries.
DESIGN
A population-based study (n= 35,912) of Medicare beneficiaries who participated in the Medicare Current Beneficiary Survey (MCBS) for years 2001–2010. Beneficiaries were classified into an activity limitation stage from 0 (no limitation) to IV (complete) derived from self- or proxy-reported difficulty performing activities of daily living (ADLs) and instrumental activities of daily living (IADLs). Beneficiaries reported whether or not they had trouble getting health care in the subsequent year. A multivariable logistic regression model examined the association between activity limitation stages and trouble getting needed care.
RESULTS
Compared to beneficiaries with no limitations (ADL stage 0), the adjusted odds ratios (OR) (95% confidence intervals (CIs)) for stage I (mild) to stage IV (complete) for trouble getting needed health care ranged from OR = 1.53 (95% CI: 1.32–1.76) to OR = 2.86 (95% CI: 1.97–4.14). High costs (31.7%), not having enough money (31.2%), and supplies/services not covered (24.2%) were the most common reasons for reporting trouble getting needed health care.
CONCLUSION
Medicare beneficiaries at higher stages of activity limitations reported trouble getting needed healthcare which was commonly attributed to financial barriers.
Keywords: Disability, Medicare, Access to care, Activity of daily living, Instrumental activity of daily living
Access to health care, the ease with which an individual can obtain needed medical services, is a prominent and pressing issue in the United States (US). Access to health care such as preventive services, is associated with improved functioning, enhanced quality of life, and reduced morbidity and mortality.1,2 Barriers to access to care include high costs, lack of availability of providers and appropriate facilities for care, poor insurance coverage, impaired patient-physician communication, and negative attitudes of health professionals. The Healthy People 2020 initiative aims to eliminate health disparities and improve access to care in the US.
Persons with disabilities are the largest underserved subpopulation in the U.S.3 Problems with access to care are particularly pronounced among persons with multiple chronic conditions and severe disability in comparison to persons without medical conditions or disability.4 The nature of a person’s disability may affect their health care access. Horner-Johnson et al. found that persons in cognitive, physical, and multiple disability type groups were more likely to have problems with receipt of preventive services and healthcare access than persons with other disability types.5 Pandhi et al. reported that hard-of-hearing individuals were more likely to report difficulties in accessing healthcare.6 Spencer et al. found that individuals with blindness and vision impairment reported having more access problems related to cost of care, availability of insurance coverage, transportation issues, and refusal of services by providers.7 In summary, persons with disability are more likely to have unmet health care needs, use fewer preventive services, and to be dissatisfied with services.8–12
Severity of disability, measured by counts of limitations in activities of daily living (ADLs) and instrumental activities of daily living (IADLs) is associated with access to care after adjusting for sociodemographic, behavioral, and system characteristics.13 Some investigators have examined the relationship between access to care and counts of limitations of ADLs.14 However, counts of ADL or IADL limitations do not specify which activities are limited.15 Therefore, we aimed to examine ADL and IADL limitations separately by defined activity limitation stages, which specify activities persons must be able to do without difficulty.16 Stages represent both the types and severities of limitations as well as specify clinically meaningful patterns of increasing difficulty with self-care and domestic management skills. People with substantially different patterns of ADL or IADL limitations may have the same counts. In contrast, stage thresholds are hierarchical in nature, representing the most common patterns of functional recovery and decline as established by ADL and IADL hierarchies.17,18 At mild stages of activity limitation, people are able to carry out all but the “hardest” activities without experiencing difficulty. At more severe stages, the “easiest” activities become limited. Distinguishing between activities people are still able to do without difficulty and those that they find difficult allows for the application of activity limitation stages to provide a framework for discourse about approaches for improving care. Stages may be employed as a tool for screening, evaluation, research, and surveillance that may be useful in guiding care management and service provision. To our knowledge, no previous investigations have examined the relationship between activity limitation stages and reporting trouble obtaining needed health care.
Our goal was to examine the association between ADL and IADL activity limitation stages and trouble getting needed health care in the year subsequent to baseline enrollment among community-dwelling Medicare beneficiaries using data from the Medicare Current Beneficiary Survey (MCBS), a systematic, representative sample. The objectives of the present study were 1) to assess whether activity limitation stage was associated with trouble getting needed health care in the subsequent year and 2) to investigate the reasons for reporting trouble getting needed health care for persons according to activity limitation stages. We hypothesized that Medicare beneficiaries at higher activity limitation stages would report more trouble getting needed health care. Based on our prior qualitative work,19 we postulated that the most common reasons persons with disabilities would report trouble getting needed health care would be issues related to transportation and cost.
METHODS
Study Design and Sample
In this cohort study, we obtained a population-based sample (n= 35,912) of Medicare beneficiaries living in the community who participated in the Medicare Current Beneficiary Survey (MCBS) during calendar years 2001–2010. The MCBS is a nationally representative sample of the Medicare population, which oversamples beneficiaries aged 85 and older and disabled persons.25 The MCBS data were collected by the Centers for Medicare and Medicaid Services through in-person beneficiary or proxy interviews. Sample persons are interviewed three times a year over four years. The MCBS data contains individual-level information on use of health services, access to health care, satisfaction with care, source of care, health, chronic conditions, and sociodemographics. The sample was weighted to be representative of fee-for-service and health maintenance organization Medicare beneficiaries. Interviews were conducted in person, in homes, or in the facility of residence. If a beneficiary was unable to provide a response in English or Spanish, a family member served as a proxy to interpret. We used the Access to Care files. Beneficiaries were excluded if they did not provide complete information for our study analysis. Medicare panels refer to annual supplements to the MCBS. In panel 1, there were 46,842 community living persons interviewed, 22 had missing information for ADLs or IADLs. Of the remaining beneficiaries, 581 were institutionalized, 1,785 died, and 7,410 were lost to follow up during interview panel 2. Furthermore, 1,132 beneficiaries had a missing response (not ascertained, do not know, and refused) for the outcome of whether or not they had trouble getting needed health care. Thus, the remaining 35,912 beneficiaries were included in the final study. This study was approved by the Institutional Review Board at the University of Pennsylvania and study participants provided written informed consent administered by the MCBS. This study adheres to STROBE guidelines and provides the required information (see Supplementary Checklist).
Activity Limitation Stage
As described previously, activity limitation stages were derived to reflect the International Classification of Functioning, Disability and Health for the entire sample.26 Answers to simple questions about difficulties performing basic activities were used to derive standardized activity limitation stages at baseline. These stages were developed in response to the recommendation of the Institute of Medicine to use the ICF as the conceptual framework to develop a comprehensive disability monitoring system.20 The National Committee on Vital and Health Statistics (NCVHS) argued that it is essential to produce comparable functional status measures across care settings that are similar to International Classification of Diseases-9-Clinical Modification and International Classification of Diseases-10 for diagnoses. 21 Thus, a staging system was developed for ADLs, applying terminology from the ICF and data from the second Longitudinal Study of Aging (LSOA II).22
ADL and IADL stages are ordered based on survey respondents’ levels of difficulty (e.g., none to complete) performing each activity except for stage III. For each ADL and IADL activity, respondents are asked, “Because of a health condition, do you have difficulty with [activity]?” The ADL domain activities include self-care tasks: eating, toileting, dressing, bathing/showering, getting in or out of bed/chairs, and walking. The IADL domain activities include domestic management tasks: using the telephone, managing money, preparing meals, doing light housework, shopping for personal items, and doing heavy housework. At stage 0, persons are able to carry out all 6 activities without any difficulty. At stages I and II people have progressively fewer activities that they can carry out without difficulty, starting with the harder and ending with the easiest tasks. At stage IV, persons have difficulty carrying out all 6 ADLs or IADLs. Stage III represents people with uncommon patterns of limitations in which activities that are typically easy may be difficult or vice versa. Detailed methods have been described elsewhere.27,28
Sociodemographic and Clinical Characteristics
Sociodemographics and health-related covariates were assessed at baseline. Sociodemographics included sex, age, race (non-Hispanic white, non-Hispanic black, Hispanic, or other), dual enrollment in Medicare and Medicaid, education (less than high school education or high school diploma and above), living arrangement (alone, with spouse, with children, with others, or in a retirement community), metropolitan setting, and proxy- versus self-response to the survey. Health and clinical characteristics included number of comorbidities (hypertension, myocardial infarction, angina/chronic heart disease, other heart disease, stroke, diabetes mellitus, Parkinson’s disease, emphysema/asthma/chronic obstructive pulmonary disease, rheumatoid arthritis, non-rheumatoid arthritis, osteoporosis/soft bones, cancers other than skin, mental retardation, Alzheimer’s/dementia, and mental/psychiatric disorder), and presence of vision and hearing impairment.
Measurement of Access Barriers: Trouble Getting Needed Health Care
As in prior work,23 as a component of the MCBS, beneficiaries were interviewed approximately one year following the baseline survey. They were asked: “In the last year, have you had trouble getting needed health care?” Respondents who answered “yes” were then asked whether the following factors contributed to their trouble in getting needed health care: not enough money, costs too high, services/supplies not covered, needing transportation, difficulty in getting home health care, no treatment available/doctors won’t treat, waiting too long/doctor too busy, doctor won’t accept Medicare, ineligible for public coverage, difficulty getting appointment/delay because on Medicare, referred specialist, and other.
Statistical Analysis
The analysis proceeded in three phases. In the first phase, we calculated descriptive statistics for the beneficiaries who had trouble getting needed health care and beneficiaries who had no trouble. Comparisons between groups of beneficiaries were made using χ2 tests or t-tests as appropriate for categorical data or differences in means. In the second phase, a multivariable logistic regression model was used to demonstrate the association between activity limitation stages and trouble getting needed health care. The association between activity limitation stages and trouble getting needed health care was assessed first in an unadjusted logistic regression model, and subsequently in a multivariable logistic regression model. Our measure of association was the odds ratio (OR) and 95% confidence interval (CI). These multivariable models were adjusted for sex, age, race, dual enrollment in Medicare and Medicaid, education, living arrangement, metropolitan setting, proxy - versus self-response, number of comorbidities, and vision and hearing impairment. ADL stages (stage 0 as reference) and IADL stages (stage 0 as reference) were analyzed separately because of collinearity between them. The third phase consisted of examining the reasons beneficiaries gave for having trouble getting needed health care. We set alpha at 0.05. All analyses applied sampling weights and accounted for the complex sampling design such as stratification and clustering. Analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC).
RESULTS
Sample characteristics
Our sample consisted of 35,912 beneficiaries living in the community, representing 43.6 million annual beneficiaries nationwide. For the proportion of this population at each of the ADL activity limitation stages, the weighted percentages were 69.4% at stage 0, 16.2% at stage I, 7.3% at stage II, 6.1% at stage III, and 0.9% at stage IV. Table 1 contains the descriptive statistics for the beneficiaries who had trouble getting needed health care and beneficiaries who had no trouble.
Table 1.
Functional Characteristic and Demographic in the Medicare population of the 2001–2010 Medicare Current Beneficiary Survey Sample stratified by those who had trouble versus those who did not have trouble getting health care in the last year.
| Variable | Total N (weighted %) 35912 |
Had trouble N (column weighted %) 1552 (4.2) |
No trouble N (column weighted %) 35912 (95.8) |
P value |
|---|---|---|---|---|
| Functional Characteristic | ||||
| ADL stage | <.0001 | |||
| 0 | 24222 (69.4) | 708 (2.8) | 23514 (97.2) | |
| I | 6056 (16.2) | 345 (5.8) | 5711 (94.2) | |
| II | 2904 (7.3) | 211 (6.9) | 2693 (93.1) | |
| III | 2354 (6.1) | 239 (10.9) | 2115 (89.1) | |
| IV | 376 (0.9) | 49 (13.3) | 327 (86.7) | |
| IADL stage | <.0001 | |||
| 0 | 20729 (60.8) | 519 (2.4) | 20210 (97.6) | |
| I | 6322 (17.4) | 310 (4.6) | 6012 (95.4) | |
| II | 3413 (9.2) | 295 (9) | 3118 (91) | |
| III | 4675 (10.9) | 354 (8.1) | 4321 (91.9) | |
| IV | 773 (1.7) | 74 (10) | 699 (90) | |
| Demographic | ||||
| Age | <.0001 | |||
| ≤64 | 6405 (16.8) | 804 (11.5) | 5601 (88.5) | |
| 65–74 | 13772 (48.6) | 406 (3) | 13366 (97) | |
| 75–84 | 11811 (27.3) | 264 (2.2) | 11547 (97.8) | |
| ≥85 | 3924 (7.3) | 78 (1.9) | 3846 (98.1) | |
| Age in year, mean (standard error) | 69.8 (0.1) | 61.6 (0.3) | 70.2 (0.1) | <.0001 |
| Gender | 0.10 | |||
| Male | 16306 (45.3) | 701 (3.9) | 15605 (96.1) | |
| Female | 19606 (54.7) | 851 (4.3) | 18755 (95.7) | |
| Race/Ethnicity (Missing = 17) | <.0001 | |||
| Hispanic | 2939 (8.2) | 211 (6.7) | 2728 (93.3) | |
| NH white | 28286 (79) | 1082 (3.7) | 27204 (96.3) | |
| NH Black | 3618 (9.6) | 196 (5.3) | 3422 (94.7) | |
| Other | 1052 (3.2) | 63 (5.7) | 989 (94.3) | |
| Education (Missing = 161) | 0.0004 | |||
| High school diploma or above | 25733 (74.3) | 1046 (3.9) | 24687 (96.1) | |
| No high school diploma | 10018 (25.7) | 502 (4.9) | 9516 (95.1) | |
| Metropolitan Setting (Missing = 6) | 0.68 | |||
| No | 9471 (24.9) | 399 (4) | 9072 (96) | |
| Yes | 26435 (75.1) | 1152 (4.2) | 25283 (95.8) | |
| Duel Insurance | <.0001 | |||
| Medicare only | 28975 (83.5) | 934 (3.2) | 28041 (96.8) | |
| Medicare plus Medicaid | 6937 (16.5) | 618 (8.9) | 6319 (91.1) | |
| Living Arrangement | <.0001 | |||
| Retirement community | 2182 (5.5) | 81 (4) | 2101 (96) | |
| With spouse | 17016 (51.4) | 520 (3) | 16496 (97) | |
| With children | 3689 (9.3) | 237 (6) | 3452 (94) | |
| With others | 3377 (8) | 276 (8) | 3101 (92) | |
| Alone | 9648 (25.8) | 438 (4.7) | 9210 (95.3) | |
| Proxy Responded (Missing = 364) | 0.53 | |||
| No | 32600 (93.2) | 1397 (4.1) | 31203 (95.9) | |
| Yes | 2948 (6.8) | 139 (4.4) | 2809 (95.6) | |
| Medical and disability condition | ||||
| Vision Impairment | <.0001 | |||
| No | 33254 (93.3) | 1319 (3.8) | 31935 (96.2) | |
| Yes | 2658 (6.7) | 233 (9.7) | 2425 (90.3) | |
| Hearing Impairment | 0.0001 | |||
| No | 33430 (93.8) | 1422 (4) | 32008 (96) | |
| Yes | 2482 (6.2) | 130 (5.8) | 2352 (94.2) | |
| * Number of comorbidities, mean (standard error) | 2.4 (0.02) | 2.8 (0.06) | 2.3 (0.02) | <.0001 |
Number of comorbidities including: mental retardation, Alzheimer’s/dementia, mental/psychiatric disorder, hypertension, myocardial infarction, angina/chronic heart disease, other heart disease, stroke, diabetes mellitus, Parkinson’s disease, emphysema/asthma/chronic obstructive pulmonary disease, rheumatoid arthritis, non-rheumatoid arthritis, osteoporosis/soft bones, and other (non-skin) cancer.
Limitation Stages and Trouble Accessing Needed Health Care
Trouble getting needed health care by ADL stages is shown in Table 2, which presents the final models from multiple logistic regression analyses. Compared to beneficiaries with no limitations at ADL stage 0, those at stage I (mild) to stage IV (complete) were more likely to report trouble accessing needed health care. The relationship between ADL activity limitation stage and reporting trouble accessing healthcare increased monotonically. Similarly, compared to beneficiaries with no limitations at IADL stage 0, those at stage I (mild) to stage IV (complete) were more likely to report trouble accessing needed health care. The relationship between IADL activity limitation stage and reporting trouble accessing healthcare increased monotonically. Multivariable models in Table 2 were adjusted for sex, age, race, dual enrollment in Medicare and Medicaid, education, living arrangement, metropolitan setting, proxy- versus self-response, number of comorbidities, and vision and hearing impairment.
Table 2.
Estimates of Adjusted Logistic Regression Models with ADL/IADL stage association with those who had trouble getting health care in the last year.
| Model adjusted with ADL stage | Model adjusted with IADL stage | |||
|---|---|---|---|---|
| Variable | odds ratios (95% CIs) | P value | odds ratios (95% CIs) | P value |
| Functional Characteristic of Stage (reference: Stage 0) | <.0001 | <.0001 | ||
| Stage I | 1.53 (1.32–1.76) | <.0001 | 1.32 (1.12–1.56) | 0.001 |
| Stage II | 1.74 (1.45–2.08) | <.0001 | 2.03 (1.69–2.44) | <.0001 |
| Stage III | 2.47 (1.99–3.06) | <.0001 | 2.05 (1.65–2.54) | <.0001 |
| Stage IV | 2.86 (1.97–4.14) | <.0001 | 2.64 (1.79–3.89) | <.0001 |
| Demographic | ||||
| Age (reference: 65–74) | <.0001 | <.0001 | ||
| <65 | 2.61 (2.24–3.03) | <.0001 | 2.45 (2.08–2.88) | <.0001 |
| 75–84 | 0.61 (0.51–0.73) | <.0001 | 0.61 (0.51–0.73) | <.0001 |
| >=85 | 0.42 (0.32–0.54) | <.0001 | 0.41 (0.32–0.53) | <.0001 |
| Gender (reference: female) | ||||
| Male | 0.93 (0.80–1.08) | 0.32 | 0.94 (0.81–1.09) | 0.40 |
| Race/Ethnicity (reference: non-Hispanic white) | 0.02 | 0.02 | ||
| Hispanic | 1.35 (1.05–1.75) | 0.02 | 1.36 (1.06–1.76) | 0.02 |
| non-Hispanic Black | 0.86 (0.68–1.09) | 0.21 | 0.87 (0.69–1.10) | 0.25 |
| Other | 1.34 (0.90–2.00) | 0.16 | 1.32 (0.88–1.97) | 0.18 |
| Education (reference: High school diploma or above) | ||||
| No high school diploma | 0.96 (0.85–1.09) | 0.56 | 0.96 (0.84–1.09) | 0.51 |
| Metropolitan Setting (reference: Nonmetropolitan) | ||||
| Metropolitan | 1.12 (0.90–1.40) | 0.32 | 0.96 (0.84–1.09) | 0.51 |
| Duel Insurance (reference: Medicare only) | ||||
| Medicare plus Medicaid | 1.42 (1.19–1.68) | <.0001 | 1.12 (0.90–1.40) | 0.31 |
| Living Arrangement (reference: With spouse) | <.0001 | <.0001 | ||
| Retirement community | 1.41 (1.10–1.82) | 0.01 | 1.43 (1.11–1.84) | 0.01 |
| With children | 1.49 (1.21–1.83) | 0.0002 | 1.49 (1.21–1.83) | 0.0002 |
| With others | 1.49 (1.18–1.87) | 0.001 | 1.44 (1.14–1.81) | 0.002 |
| Alone | 1.43 (1.22–1.68) | <.0001 | 1.44 (1.23–1.68) | <.0001 |
| Proxy Responded (reference: Sample person responded) | ||||
| Proxy responded | 0.69 (0.53–0.89) | 0.01 | 0.59 (0.44–0.79) | 0.001 |
| Medical and disability condition | ||||
| Vision Impairment (reference: No) | ||||
| Yes | 1.75 (1.45–2.10) | <.0001 | 1.73 (1.45–2.06) | <.0001 |
| Hearing Impairment (reference: No) | ||||
| Yes | 1.27 (1.05–1.55) | 0.02 | 1.19 (0.96–1.47) | 0.12 |
| * Number of comorbidities | 1.05 (1.01–1.09) | 0.03 | 1.06 (1.02–1.10) | 0.01 |
Number of comorbidities including: mental retardation, Alzheimer’s/dementia, mental/psychiatric disorder, hypertension, myocardial infarction, angina/chronic heart disease, other heart disease, stroke, diabetes mellitus, Parkinson’s disease, emphysema/asthma/chronic obstructive pulmonary disease, rheumatoid arthritis, non-rheumatoid arthritis, osteoporosis/soft bones, and other (non-skin) cancer.
Other Factors Associated with Trouble Accessing Needed Health Care
As shown in Table 2, age, ethnicity, insurance coverage, living arrangement, use of a proxy, and number of comorbidities were significantly associated with trouble accessing needed healthcare. Notably, persons with vision impairment/no usable vision were more likely to report trouble getting needed healthcare both in the model with ADL stages and the model with IADL stages. Persons with hearing impairment/deaf were also more likely to report trouble getting needed healthcare in the model assessing ADL stages.
Reasons for Trouble Getting Needed Health Care
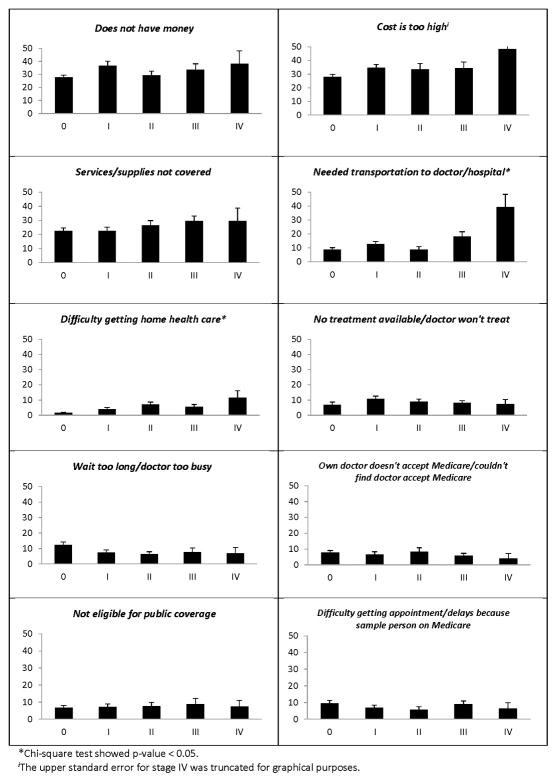
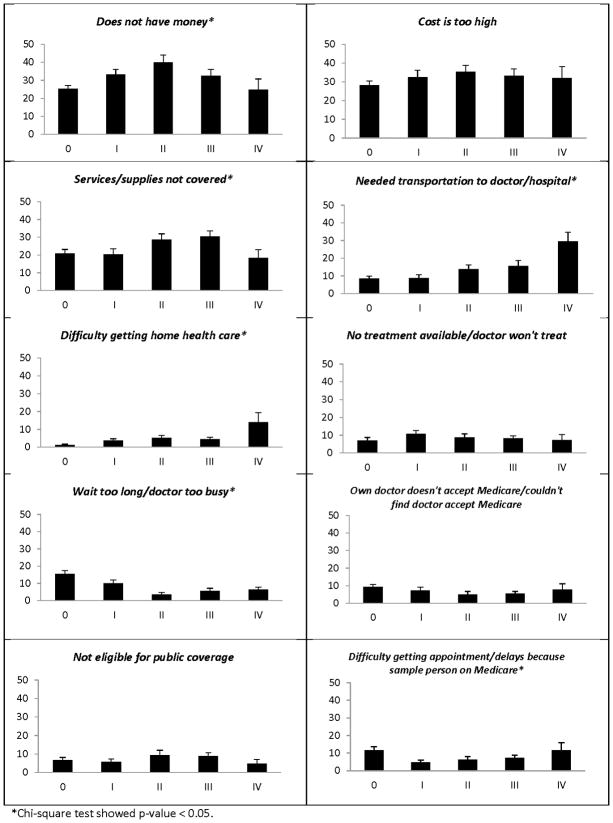
Among 1,552 beneficiaries indicating that they had trouble getting needed health care, corresponding to 1.8 million beneficiaries annually, 57.2% beneficiaries reported a single reason, and 42.8% beneficiaries reported two or more reasons. The beneficiaries gave a variety of reasons but the most common were high costs (31.7%), not having enough money (31.2%), and supplies/services not covered (24.2%). The reasons the beneficiaries gave for trouble getting needed healthcare according to ADL and IADL activity limitation stages are summarized in Figures 1 and 2. Among persons who had trouble getting needed health care, the percentage of beneficiaries reporting that they did not have enough money ranged from a minimum of 25.3% at IADL stage 0 to a maximum of 39.9% at stage II (moderate) (p<.01). The percentage of beneficiaries reporting needed transportation to the doctor/hospital ranged from a minimum of 8.8% at ADL stage 0 to a maximum of 39.3% at stage IV (complete) (p<.001). The percentage of beneficiaries reporting difficulty getting home healthcare ranged from a minimum of 1.6% at ADL stage 0 to a maximum of 11.5% at stage IV (complete) (p<.001) and a minimum of 1.2% IADL stage 0 to a maximum of 14% at stage IV (complete) (p<.001). There was a monotonic increase across IADL activity limitation stages for beneficiaries reporting trouble with needed transportation to doctor/hospital (p<.001).
Figure 1.
Percentages of Medicare Beneficiaries Reporting Specific Reasons for Trouble Getting Needed Healthcare by ADL Stages
Figure 2.
Percentages of Medicare Beneficiaries Reporting Specific Reasons for Trouble Getting Needed Healthcare by IADL Stages
DISCUSSION
Medicare beneficiaries reported that they experienced trouble accessing needed health care especially those at higher activity limitation stages. Specifically, the adjusted relationships between activity limitation stages and reporting trouble accessing needed health care were monotonically increasing for both the ADL and the IADL domain. Commonly cited reasons were costs too high, not having enough money, and services/supplies not covered. Persons at higher ADL activity limitation stages were significantly more likely to report difficulties with transportation and problems getting home healthcare. Persons at higher IADL activity limitation stages were significantly more likely to report that they did not have enough money, difficulties with transportation, and problems getting home healthcare.
While prior work has focused on counts of activity limitations, in this work we focused on activity limitation stages that describe the type as well as the severity of disability, and therefore may provide greater insight into the mechanisms that shape the relationship between poor access and disability. These results suggest that persons even at mild activity limitation stages experience trouble accessing needed health care. This is not surprising given that people at ADL stage I (mild) experience difficulty walking and getting in and out of chairs. These findings emphasize the need for accommodations to improve physical accessibility to needed healthcare. Persons at ADL stage II (moderate) have additional problems dressing and/or bathing, which results in vulnerability and lower quality of life. In terms of IADLs, since people at IADL stage I have difficulty with activities requiring mobility in the community such as shopping, it is not surprising that they would also experience trouble accessing health care.
While activity limitations may reduce an individual’s ability to obtain needed health care by making physical barriers insurmountable, other mechanisms may also play a role. Findings suggest that despite legislation to promote equal access to employment for persons with disability, higher levels of disability are associated with lower employment status and income.24 An examination over the past two decades found that there has been little improvement in the economic well-being of people with disabilities and that such persons remain at very low levels of economic well-being despite relative levels of privilege (e.g. college degree).25 It is also notable that many beneficiaries may be ineligible for employment because they are receiving social security income (SSI) or social security disability (SSD) income. With inadequate health insurance coverage, financial costs may inhibit the ability to obtain needed health care. Beatty et. al. found in a sample of people with chronic or disabling conditions, respondents with the poorest health and with the lowest incomes were the least likely to receive all health services examined.4 While persons with chronic or disabling conditions may require more health care than the average consumer they often face more difficulties in obtaining such care. Even in a relatively well insured population such as that covered by Medicare, disability leads to fewer resources, and finding care too costly or not having enough money to pay for co-payments. There is a need for reform of the current coverage and delivery systems in order to meet the needs of persons who require the most intensive array of care.
Consistent with prior studies, age was associated with trouble accessing needed healthcare. Medicare beneficiaries who were younger than 65 years old were more likely to report trouble getting needed health care in comparison with persons aged 65 to 74 years old. In contrast, beneficiaries who were aged 75 to 84 years old or 85 years old and older and were significantly less likely to report trouble getting needed health care in comparison with persons aged 65 to 74 years old. Medicare beneficiaries aged younger than 65 years old experience significant vulnerability and a high burden of medical conditions. Because younger beneficiaries are often eligible for benefits based on medical illness and/or disability as opposed to age-based eligibility for those 65 years or older, younger beneficiaries are more likely to have worse self-reported health, and higher rates of medical conditions and disability.26 Our findings are consistent with reports that beneficiaries under age 65 are an increasingly vulnerable population with Medicare reform having largely focused on meeting the needs of the aged. The aged are the largest and most visible segment of the Medicare population and in turn appear to have garnered the most attention and support for reform.27 Further investigation is warranted to examine the differences between those who are age-based eligible in comparison to those who are eligible based on disability status. Type of disability may serve as particularly insightful elucidating access to care.
Hispanic beneficiaries were more likely to report trouble obtaining healthcare compared to non-Hispanic whites. This is consistent with recent findings that among Medicare beneficiaries, trouble accessing health care is greatest among Hispanics (9%).28 There was no adjusted association between being non-Hispanic black race/ethnicity and trouble obtaining needed healthcare. According to the Panel on Hispanics in the US of the National Research Council, Hispanics face substantial barriers in obtaining high quality health care as a result of low socioeconomic status and other specific features of the Hispanic population such as degree of acculturation, language fluency, and immigration status. Low income among Hispanics and occupational characteristics are associated with lower rates of health insurance coverage, thus subjecting persons to high out-of-pocket costs which may be prohibitive in accessing health care. Furthermore, lower educational attainment may impair navigation of a complex health care system and communication with health care professionals.29 Further research is needed to evaluate the mechanisms that shape the relationship between race and ethnicity and trouble getting needed health care.
As expected, Medicaid enrollment, living arrangement and proxy respondent to the survey were significantly associated with trouble getting needed healthcare. Persons without adequate health insurance coverage are much less likely to receive preventive services and are more likely to delay or forego visits with physicians.30 Living arrangements other than living with a spouse, such as living alone and living with an adult child, have been associated with worse health care access.31 Given the importance of surveys for assessing health care provision and aging of the population, the examination of proxy respondents has been an important area of study. Proxy respondents have been found to provide less positive evaluations of beneficiary health care experiences on subjective global ratings. However, reports from spouse proxies were found to be more similar to what would have been reported by beneficiaries themselves.32
In addition, the presence of vision impairment or hearing impairment was strongly associated with trouble getting needed health care. These findings are consistent with studies demonstrating gaps in care experienced by persons with vision or hearing impairments.6,7 Persons with vision impairment may struggle to find a chair or navigate furniture, make eye contact when talking, or may fail to respond when they have been handed something. Persons with hearing impairment may have difficulty interacting with office staff and providers and may lack a response when asked questions and presented with information.33 These signs may be too subtle for ascertainment by health professionals in usual clinical settings. Interventions specifically tailored to the needs of persons with these sensory limitations are needed. Findings from this study may be relevant for similar populations, particularly Medicare beneficiaries. However, the validity of our findings in other samples is an important area of further inquiry.
An important goal of our study was to examine the reasons for reporting trouble getting needed health care. While beneficiaries offered a variety of reasons, the most common ones were high costs, not having enough money, and services/supplies not covered. The Institute of Medicine provided a framework in which three broad categories: structural, financial, and personal/cultural factors influence access to care. These factors entail a complex interplay in which barriers overlap and interact with one another.34 Financial barriers play a significant role in diminishing access to care for persons with disabilities as individuals with disabilities may need additional health care services and accommodations. However, persons with minimal insurance or a lack of coverage may not be able to afford out-of-pocket costs for uncovered services. Costs of care have been associated with significant difficulties in accessing health care such as home health care, prescription drugs, mental health services, and necessary equipment among persons with disability.35 Financial barriers have been found to be particularly pronounced among the uninsured and Medicare beneficiaries. Accommodations in the office (e.g., space for wheelchairs, exam tables, mammography machines) and home settings (e.g., basic equipment) are often absent and may be related to insurance coverage.36 Transportation may be problematic as persons may be unable to obtain needed conveyance or effectively find their way to health care facilities.37 Other factors contributing to poor access include insufficient knowledge, misconceptions about persons with disability, and insensitivity.38 Our findings indicate that financial barriers were the most common issues faced by beneficiaries although transportation services and home healthcare services were especially cited as by persons at more advanced activity limitation stages as reasons for trouble getting needed health care.
Study Limitations
Several study limitations are important for consideration. First, self-reports were utilized which may have varying reliability due to recall, social desirability and other biases. Second, the MCBS data were obtained through self-or proxy responses. The proxy-related answers to questions may differ from answers provided by the sampled beneficiaries; however, we included proxy responses because substantial bias can be introduced when proxy responses are excluded.39 Third, even with a high degree of confidence in our measurements, the potential of misspecification of the model remains possible, such as when relevant variables may not have been incorporated. However, we carefully selected our variables when adjusting our estimates of association for potentially influential characteristics. Finally, our findings may not be generalizable to all Medicare beneficiaries or other groups. Further work is needed to explore the significance of our findings in other populations.
CONCLUSIONS
A critical priority noted by the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the National Institutes of Health is to reduce health disparities between the most and least vulnerable groups. Our findings contribute to a growing knowledge base suggesting that those with greater functional limitations may have more trouble getting needed health care services. With new findings elucidating factors influencing trouble getting needed health care, we may be able to develop and implement approaches to overcome barriers and improve access and health outcomes. Our findings highlight a need for interventions targeting persons with disabilities, particularly persons at higher activity limitation stages. Alerting providers to activity limitation stages of their patients and incorporating patient evaluations and perceptions into strategies for improving access to care may be important next steps. Such approaches to enhance access for persons with disabilities may ultimately improve both the quality and outcomes of care.
Supplementary Material
Acknowledgments
The authors thank Dr. Margaret G. Stineman, MD for her contributions to study development.
Footnotes
Author Disclosures: The authors have no financial or any other kind of conflicts of interest to declare. This work was supported through a Patient-Centered Outcomes Research Institute PCORI Project Program Award AD-12-11-4567 and by the National Institutes of Health (R01AG040105 and R01HD074756). Dr. Bogner was supported by an American Heart Association Award #13GRNT17000021.
References
- 1.Goldberg TH, Chavin SI. Preventive medicine and screening in older adults. J Am Geriatr Soc. 1997;45:344–354. doi: 10.1111/j.1532-5415.1997.tb00952.x. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease C, Prevention. Pneumococcal and influenza vaccination levels among adults aged > or = 65 years--United States, 1995. MMWR Morb Mortal Wkly Rep. 1997;46:913–919. [PubMed] [Google Scholar]
- 3.Drum C, McClain M, Horner-Johnson W, et al. Health Disparities Chart Book on Disability and Racial and Ethnic Status in the United States. Durham, NH: 2011. [Google Scholar]
- 4.Beatty PW, Hagglund KJ, Neri MT, et al. Access to health care services among people with chronic or disabling conditions: patterns and predictors. Archives of physical medicine and rehabilitation. 2003;84:1417–1425. doi: 10.1016/s0003-9993(03)00268-5. [DOI] [PubMed] [Google Scholar]
- 5.Horner-Johnson W, Dobbertin K, Lee JC, et al. Disparities in health care access and receipt of preventive services by disability type: analysis of the medical expenditure panel survey. Health Serv Res. 2014;49:1980–1999. doi: 10.1111/1475-6773.12195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pandhi N, Schumacher JR, Barnett S, et al. Hearing loss and older adults’ perceptions of access to care. J Community Health. 2011;36:748–755. doi: 10.1007/s10900-011-9369-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spencer C, Frick K, Gower EW, et al. Disparities in access to medical care for individuals with vision impairment. Ophthalmic Epidemiol. 2009;16:281–288. [PubMed] [Google Scholar]
- 8.Diab ME, Johnston MV. Relationships between level of disability and receipt of preventive health services. Archives of physical medicine and rehabilitation. 2004;85:749–757. doi: 10.1016/j.apmr.2003.06.028. [DOI] [PubMed] [Google Scholar]
- 9.Haggstrom DA, Bindman AB. The influence of care management tools on physician practice change across organizational settings. Jt Comm J Qual Patient Saf. 2007;33:672–680. doi: 10.1016/s1553-7250(07)33077-8. [DOI] [PubMed] [Google Scholar]
- 10.Bogner HR, de Vries McClintock HF, Hennessy S, et al. Patient Satisfaction and Perceived Quality of Care Among Older Adults According to Activity Limitation Stages. Archives of physical medicine and rehabilitation. 2015;96:1810–1819. doi: 10.1016/j.apmr.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahmoudi E, Meade MA. Disparities in access to health care among adults with physical disabilities: analysis of a representative national sample for a ten-year period. Disability and health journal. 2015;8:182–190. doi: 10.1016/j.dhjo.2014.08.007. [DOI] [PubMed] [Google Scholar]
- 12.Chan L, Doctor JN, MacLehose RF, et al. Do Medicare patients with disabilities receive preventive services? A population-based study. Archives of physical medicine and rehabilitation. 1999;80:642–646. doi: 10.1016/s0003-9993(99)90166-1. [DOI] [PubMed] [Google Scholar]
- 13.Chan L, Beaver S, Maclehose RF, et al. Disability and health care costs in the Medicare population. Archives of physical medicine and rehabilitation. 2002;83:1196–1201. doi: 10.1053/apmr.2002.34811. [DOI] [PubMed] [Google Scholar]
- 14.Maclachlan M, Mannan H, McAuliffe E. Access to health care of persons with disabilities as an indicator of equity in health systems. Open medicine : a peer-reviewed, independent, open-access journal. 2011;5:e10–12. [PMC free article] [PubMed] [Google Scholar]
- 15.Lubitz J, Cai L, Kramarow E, et al. Health, life expectancy, and health care spending among the elderly. N Engl J Med. 2003;349:1048–1055. doi: 10.1056/NEJMsa020614. [DOI] [PubMed] [Google Scholar]
- 16.Stineman MG, Streim JE, Pan Q, et al. Establishing an Approach to Activity of Daily Living and Instrumental Activity of Daily Living Staging in the United States Adult Community-Dwelling Medicare Population. PM & R. 2014 doi: 10.1016/j.pmrj.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 18.Katz S, Ford AB, Moskowitz RW, et al. Studies of Illness in the Aged. The Index of Adl: A Standardized Measure of Biological and Psychosocial Function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 19.de Vries McClintock HF, Barg FK, Katz SP, et al. Health care experiences and perceptions among people with and without disabilities. Disability and health journal. 2016;9:74–82. doi: 10.1016/j.dhjo.2015.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Committee on Disability in America. The future of disability in America. Washington, D.C: National Academies Press; 2007. [PubMed] [Google Scholar]
- 21.Iezzoni LI, Greenberg MS. Capturing and classifying functional status information in administrative databases. Health Care Financ Rev. 2003;24:61–76. [PMC free article] [PubMed] [Google Scholar]
- 22.Stineman MG, Henry-Sanchez JT, Kurichi JE, et al. Staging activity limitation and participation restriction in elderly community-dwelling persons according to difficulties in self-care and domestic life functioning. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists. 2012;91:126–140. doi: 10.1097/PHM.0b013e318241200d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kennedy J, Gimm G, Blodgett E. Return to work: a critical aspect of care coordination for younger dual eligibles. Disability and health journal. 2013;6:95–99. doi: 10.1016/j.dhjo.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Randolph DS. Predicting the effect of disability on employment status and income. Work. 2004;23:257–266. [PubMed] [Google Scholar]
- 25.Drew JA. Disability, Poverty, and Material Hardship since the Passage of the ADA. Disability studies quarterly. 2015:35. doi: 10.18061/dsq.v35i3.4947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cubanski J, Neuman P. Medicare doesn’t work as well for younger, disabled beneficiaries as it does for older enrollees. Health Aff (Millwood) 2010;29:1725–1733. doi: 10.1377/hlthaff.2009.0962. [DOI] [PubMed] [Google Scholar]
- 27.Riley GF, Lubitz JD, Zhang N. Patterns of health care and disability for Medicare beneficiaries under 65. Inquiry : a journal of medical care organization, provision and financing. 2003;40:71–83. doi: 10.5034/inquiryjrnl_40.1.71. [DOI] [PubMed] [Google Scholar]
- 28.Profile of Medicare Beneficiaries by Race and Ethnicity. [Accessed April 7, 2016];A Chartpack. 2016 http://kff.org/medicare/report/profile-of-medicare-beneficiaries-by-race-and-ethnicity-a-chartpack/
- 29.Tienda M, Mitchell F, editors. Hispanics and the Future of America. Washington (DC): 2006. [PubMed] [Google Scholar]
- 30.America’s uninsured crisis: consequences for health and health care. Washington, D.C: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 31.Lau DT, Kirby JB. Living arrangement and colorectal cancer screening: updated USPSTF guidelines. Am J Public Health. 2009;99:1733–1734. doi: 10.2105/AJPH.2009.172916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Elliott MN, Beckett MK, Chong K, et al. How do proxy responses and proxy-assisted responses differ from what Medicare beneficiaries might have reported about their health care? Health Serv Res. 2008;43:833–848. doi: 10.1111/j.1475-6773.2007.00820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cupples ME, Hart PM, Johnston A, et al. Improving healthcare access for people with visual impairment and blindness. BMJ. 2012;344:e542. doi: 10.1136/bmj.e542. [DOI] [PubMed] [Google Scholar]
- 34.Institute of Medicine. Access to healthcare in America. Washington, DC: 1993. [Google Scholar]
- 35.Kennedy J, Erb C. Prescription noncompliance due to cost among adults with disabilities in the United States. Am J Public Health. 2002;92:1120–1124. doi: 10.2105/ajph.92.7.1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Story MF, Kailes JI, Donald CM. The ADA in action at health care facilities. Disability and health journal. 2010;3:245–252. doi: 10.1016/j.dhjo.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 37.Taylor B, Taylor A. Social work with transport disabled persons: a wayfinding perspective in health care. Social work in health care. 1996;23:3–19. doi: 10.1300/J010v23n04_02. [DOI] [PubMed] [Google Scholar]
- 38.Sanchez J, Byfield G, Brown TT, et al. Perceived accessibility versus actual physical accessibility of healthcare facilities. Rehabil Nurs. 2000;25:6–9. doi: 10.1002/j.2048-7940.2000.tb01849.x. [DOI] [PubMed] [Google Scholar]
- 39.Stineman MG, Ross RN, Maislin G. Functional status measures for integrating medical and social care. Int J Integr Care. 2005;5:e07. doi: 10.5334/ijic.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.